Formación de los profesionales de la asistencia sanitaria en la prevención de las úlceras por presión
Resumen
Antecedentes
Las úlceras por presión, también conocidas como úlceras de decúbito o úlceras por compresión, son áreas localizadas de daño tisular que surgen debido a la presión excesiva y a las fuerzas de rozamiento. La formación del personal de asistencia sanitaria se ha reconocido como un componente integral de la prevención de las úlceras por presión. Estos programas educacionales se dirigen a influir en el cambio de comportamiento por parte del profesional de la asistencia sanitaria, para promover prácticas preventivas con la intención de reducir la incidencia del desarrollo de úlceras por presión.
Objetivos
Evaluar los efectos de las intervenciones educacionales para los profesionales de la asistencia sanitaria sobre la prevención de las úlceras por presión.
Métodos de búsqueda
En junio 2017, se hicieron búsquedas en el registro especializado del Grupo Cochrane de Heridas (Cochrane Wounds Specialised Register); Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials, CENTRAL); Ovid MEDLINE (incluyendo In‐Process & Other Non‐Indexed Citations); Ovid EMBASE y EBSCO CINAHL Plus. Para identificar estudios adicionales, también se buscó en los registros de ensayos clínicos de estudios en curso y no publicados, y se revisaron las listas de referencias de los estudios relevantes incluidos, así como de las revisiones, los metanálisis y los informes de tecnología de la salud. No hubo ninguna restricción en cuanto al idioma, la fecha de publicación o el ámbito de los estudios.
Criterios de selección
Se incluyeron los ensayos controlados aleatorios (ECA) y ECA con asignación al azar grupal, que evaluaron el efecto de cualquier intervención educacional administrada al personal de asistencia sanitaria en cualquier ámbito para prevenir la úlcera por presión.
Obtención y análisis de los datos
Dos autores de la revisión, de forma independiente, evaluaron la elegibilidad de los títulos y resúmenes de los estudios identificados mediante la estrategia de búsqueda. Se obtuvo el texto completo de los estudios potencialmente pertinentes y dos autores de la revisión los revisaron de forma independiente sobre la base de los criterios de inclusión.
Resultados principales
Se identificaron cinco estudios que cumplieron los criterios de inclusión para esta revisión: cuatro ECA y un ECA con asignación al azar grupal. Las características de los estudios difirieron con respecto a los ámbitos de asistencia sanitaria, la naturaleza de las intervenciones estudiadas y las medidas de resultado informadas. El ECA con asignación al azar grupal, y dos de los ECA, exploraron la efectividad de la educación proporcionada al personal de asistencia sanitaria dentro de los ámbitos de hogares de atención residencial o residencias geriátricas, o residencias geriátricas y salas de hospital, en comparación con ninguna intervención, o las prácticas habituales. En uno de estos estudios la intervención educacional se integró en un paquete más amplio para mejorar la calidad. Los otros dos ensayos controlados con asignación al azar individual exploraron la efectividad de la intervención educacional, proporcionada en dos formatos, a las cohortes del personal de enfermería.
Debido a la heterogeneidad de los estudios identificados, no fue apropiado realizar el agrupamiento y se ha presentado un resumen narrativo. Se exploraron algunas de comparaciones (1) educación versus ninguna educación (2) componentes de la intervención educacional en varias combinaciones y (3) educación proporcionada en diferentes formatos. Hubo tres resultados primarios: cambio en el conocimiento de los profesionales de la asistencia sanitaria, cambio en el comportamiento clínico de los profesionales de la asistencia sanitaria e incidencia de nuevas úlceras por presión.
No existe seguridad con respecto a si hay una diferencia en el conocimiento de los profesionales de la salud en dependencia de si reciben educación o no sobre la prevención de las úlceras por presión (grupo del hospital: diferencia de medias [DM] 0,30; intervalo de confianza [IC] del 95%: ‐1,00 a 1,60; 10 participantes; grupo de residencias geriátricas: DM 0,30; IC del 95%: ‐0,77 a 1,37; 10 participantes). Este resultado se basó en evidencia de muy baja certeza a partir de un estudio, la que se disminuyó debido a las limitaciones graves del estudio, la imposibilidad para generalizar la evidencia y la imprecisión.
No existe seguridad con respecto a si hay una diferencia en la incidencia de las úlceras por presión con las comparaciones siguientes: entrenamiento, monitorización y observación, versus monitorización y observación (cociente de riesgos [CR] 0,63; IC del 95%: 0,37 a 1,05; 345 participantes); entrenamiento, monitorización y observación, versus observación sola (CR 1,21; IC del 95%: 0,60 a 2,43; 325 participantes) o, monitorización y observación versus observación sola (CR 1,93; IC del 95%: 0,96 a 3,88; 232 participantes). Este resultado se basó en evidencia de muy baja certeza de un estudio, que se disminuyó debido a limitaciones muy graves del estudio y a imprecisión. No existe seguridad con respecto a si la intervención multinivel versus control de atención logra algún cambio en la incidencia de la úlcera por presión. El informe no presentó datos suficientes para permitir una investigación adicional en cuanto a este resultado.
No existe seguridad con respecto a si la educación proporcionada en diferentes formatos como la educación didáctica versus la educación basada en video (DM 4,60; IC del 95%: 3,08 a 6,12; 102 participantes) o la educación a distancia versus la educación en el aula (CR 0,92; IC del 95%: 0,80 a 1,07; 18 participantes), logra algún cambio en el conocimiento de los profesionales de la salud en cuanto a la prevención de las úlceras por presión. Este resultado se basó en evidencia de muy baja certeza de dos estudios, la que se disminuyó debido a las limitaciones graves y a la imprecisión de los estudios.
Ninguno de los estudios incluidos exploró el otro resultado primario: cambio en el comportamiento clínico de los profesionales de la salud. Solamente un estudio exploró los resultados secundarios de interés, a saber, la gravedad de la úlcera por presión y los resultados informados por el paciente y el cuidador (calidad de vida autoevaluada y nivel de dependencia funcional respectivamente). Sin embargo, este estudio no proporcionó información suficiente para poder evaluar de forma independiente estos resultados dentro de la revisión.
Conclusiones de los autores
No existe seguridad con respecto a si la educación de los profesionales de la asistencia sanitaria acerca de la prevención de las úlceras por presión logra algún cambio en la incidencia de la úlcera por presión o en el conocimiento del personal de enfermería sobre la prevención de las úlceras por presión. Lo anterior se debe a que los estudios incluidos aportaron evidencia de muy baja certeza. Por lo tanto, se necesita más información para aclarar el impacto de la educación de los profesionales de la asistencia sanitaria en la prevención de las úlceras por presión.
PICO
Resumen en términos sencillos
Formación del personal de asistencia sanitaria en la prevención de las úlceras por presión
Antecedentes
Las úlceras por presión, también conocidas como úlceras de decúbito o úlceras por compresión, suelen presentarse en los pacientes que tienen dificultades para caminar y pasan períodos prolongados sentados o acostados. Las úlceras por presión pueden variar desde manchas decoloradas y dolorosas en la piel, hasta heridas que pueden tomar mucho tiempo en cicatrizar. Las úlceras por presión son propensas a la infección y tienen un gran impacto sobre la salud y el bienestar del paciente. Para impedir que se desarrollen estas úlceras en los pacientes que están en riesgo, el personal de asistencia sanitaria debe estar bien informado acerca de cómo prevenirlas. Es importante comprender qué tipo de información necesita el personal de asistencia sanitaria, cómo se les puede proporcionar de la mejor manera y si la educación puede prevenir el desarrollo de las úlceras por presión.
Pregunta de la revisión
Se examinó la evidencia acerca del efecto de la educación de los profesionales de la asistencia sanitaria sobre la prevención de las úlceras por presión. Se exploraron todos los tipos de educación, independientemente de cómo se proporcionaron, siempre que se centraran en la prevención de las úlceras por presión. El personal de asistencia sanitaria incluyó todo el personal que trabajaba en la prevención de las úlceras por presión con cualquier experiencia profesional. Los ámbitos donde se proporcionó la atención incluyeron los servicios de atención hospitalaria o ambulatoria, consultorios comunitarios, el propio hogar del paciente y los hogares de atención residencial o residencias geriátricas.
Datos encontrados
En junio de 2017 se realizaron búsquedas de estudios que evaluaran el efecto de la educación de los profesionales de la asistencia sanitaria en la prevención de las úlceras por presión, y se encontraron cinco estudios relevantes. Dos estudios exploraron el impacto de la educación sobre la prevención de las úlceras por presión. No existe seguridad con respecto a si la educación de los profesionales de la asistencia sanitaria logra algún cambio en la cantidad de nuevas úlceras por presión que se desarrollan. Lo anterior se debe a que la certeza de la evidencia dentro de los estudios fue muy baja.
Tres estudios exploraron el impacto de la educación en el conocimiento del personal sobre la prevención de las úlceras por presión. Los estudios compararon: educación versus no educación; componentes de la intervención educacional en varias combinaciones; y educación proporcionada en diferentes formatos. No existe seguridad con respecto a si la educación logra algún cambio en el conocimiento del personal sobre la prevención de las úlceras por presión o en la cantidad de nuevas úlceras por presión que se desarrollan. Lo anterior se debe a que la certeza de la evidencia dentro de los estudios fue muy baja. Ningún estudio exploró la repercusión de la educación en el tratamiento proporcionado por los profesionales de la salud. Sólo un estudio exploró los resultados secundarios de interés: gravedad de la úlcera por presión, opinión de los pacientes de su calidad de vida y opinión de los cuidadores sobre la capacidad de los pacientes de realizar las tareas diarias de forma independiente. Sin embargo, en el estudio no se proporcionó información suficiente para poder realizar una evaluación independiente de estos resultados.
La certeza de la evidencia se examinó mediante el enfoque GRADE y se concluyó que toda la evidencia fue de certeza muy baja. Por lo tanto, no es posible determinar si la educación puede prevenir las úlceras por presión. Tampoco es posible determinar si la educación afecta el conocimiento que posee el personal de asistencia sanitaria acerca de la prevención de las úlceras por presión.
La evidencia de esta revisión está actualizada hasta el 12 de junio de 2017.
Conclusiones de los autores
Summary of findings
| Education compared to no education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No education | Education | |||||
| Knowledge in hospital group | Mean knowledge score with no education was 5.7 | Mean knowledge score was 0.30 units higher (1.0 lower to 1.6 higher) | 10 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in health professionals' knowledge depending on whether they receive education or no education on pressure ulcer prevention | |
| Knowledge in nursing‐home group | Mean knowledge score with no education was 5.1 | Mean knowledge score was 0.30 units higher (0.77 lower to 1.37 higher) | 10 | ⊕⊝⊝⊝ | ||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded four times: serious limitations due to performance bias, detection bias and attrition bias; indirectness due to use of a non validated instrument to assess knowledge; serious imprecision due to a wide confidence interval and small sample size. | ||||||
| Training, monitoring and observation compared to monitoring and observation for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Monitoring and observation | Training, monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 0.63 | 345 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with monitoring and observation | |
| 183 per 1000 | 115 per 1000 | |||||
| Severity of new pressure ulcers | No data were presented by the study author | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Training, monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Training monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.21 | 325 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with observation alone | |
| 94 per 1000 | 114 per 1000 | |||||
| Severity of new pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.93 | 232 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as monitoring and observation compared with observation alone | |
| 94 per 1000 | 182 per 1000 | |||||
| Severity of new pressure ulcers | No data are presented by the study author | |||||
| Patient reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitation due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Education versus video for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Comparison: didactic lecture | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Didactic education | Video education | |||||
| Change in health professionals' knowledge | Mean knowledge score with didactic education was 84.62 | Mean knowledge score was 4.60 units higher (3.8 units to 6.12 units higher) | 102 | ⊕⊝⊝⊝ | It is uncertain whether education delivered in different formats such as didactic or video‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitation due to unclear risk of selection, performance and detection bias; very serious imprecision due to small sample size and wide confidence intervals. | ||||||
| E‐learning compared with classroom education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Settings: hospitals and nursing homes Intervention: e‐learning Comparison: classroom education | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Classroom education | E‐learning | |||||
| Knowledge of pressure ulcer classification | Study population | RR 0.92 (0.80 to 1.07) | 18 participants | very low1 | It is uncertain whether education delivered in different formats such as e‐learning or classroom‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| 694 per 1000 | 638 per 1000 | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitations due to high risk of attrition and selective reporting bias; unclear risk of performance, selection, detection and other bias; serious imprecision due to small sample size and wide confidence intervals. | ||||||
Antecedentes
Descripción de la afección
Una úlcera por presión (también conocida como úlcera de decúbito, úlcera por compresión, o lesión por presión) es "una lesión localizada en la piel o el tejido subyacente generalmente sobre una prominencia ósea, como resultado de la presión, o de la presión en combinación con el rozamiento" (NPUAP/EPUAP/PPPIA 2014). Existe una clasificación común internacional de las úlceras por presión que categoriza las úlceras por presión en cuatro categorías o estadios de la lesión, que varían del eritema no blanqueable de la piel (enrojecimiento tisular que no se vuelve blanco cuando se aplica presión) (estadio 1) hasta la pérdida tisular de espesor total (estadio 4), y otros dos niveles de lesión tisular "inestadiable" y "profunda" (NPUAP/EPUAP/PPPIA 2014).
Existen varios factores de riesgo asociados con la aparición de úlceras por presión, que recientemente se presentaron en una vía causal teórica y un marco conceptual de la úlcera por presión (Coleman 2014). Al reconocer que ningún factor único puede explicar la susceptibilidad a las úlceras por presión, factores como la inmovilidad y la perfusión deficiente se han descrito como factores causales directos, y factores como la humedad, la percepción sensorial deficiente y la nutrición deficiente se han descrito como factores causales indirectos. Estos factores interaccionan y dan lugar a que algunos individuos sean particularmente vulnerables o estén "en riesgo" de presentar úlceras por presión; sin embargo, aún no se conocen los mecanismos exactos por los cuales sucede lo anterior, ni qué factores son de mayor importancia. Las personas "en riesgo" mayor de úlcera por presión incluyen los individuos que pasan períodos prolongados sentados o acostados, los que utilizan sillas de ruedas, las personas sedentarias de edad más avanzada o las que se encuentran inmóviles (Bates‐Jensen 2009; Gunningberg 2008; Thomas 2010). Las úlceras por presión ocurren debido a la exposición prolongada sin alivio a fuerzas mecánicas aplicadas de forma externa (Gefen 2008). Las personas vulnerables a la exposición a dicha presión son las que se encuentran inmóviles, y las de edad más avanzada demuestran la propensión más alta a problemas de movilidad (Moore 2011).
La úlcera por presión tiene una repercusión profunda sobre la salud, la rehabilitación y la calidad de vida de los individuos que las presentan (Anderson 2008; Bates‐Jensen 2009; Ryan 2006; Shapcott 1999). A pesar de lo anterior, la prevalencia de la úlcera por presión todavía es inaceptablemente alta, y varía del 9% en Irlanda (Moore 2011); el 5% al 32% en el Reino Unido (Kaltenthaler 2001); 18% en Europa (Vanderwee 2007); y el 12,3% en los EE.UU. (VanGilder 2009). Las úlceras por presión ocurren en todos los ámbitos clínicos: cuidados intensivos (prevalencia media del 21%); estancias prolongadas (prevalencia media del 12%); hospicios (prevalencia del 35,7%); y atención comunitaria (la prevalencia varía del 0,04% al 4%) (Moore 2013). Se ha demostrado que la prevalencia de las úlceras por presión en un ámbito de cuidados intensivos en Australia alcanza el 50% (Elliott 2008). Dicha prevalencia impone un impacto económico significativo sobre los servicios de asistencia sanitaria en cuanto a los costos del tratamiento y del personal. Estudios internacionales han demostrado de forma consistente el costo elevado del tratamiento de la úlcera por presión. Se ha calculado que el costo anual del tratamiento de las úlceras por presión es de GBP 1 400 000 000 a 2 100 000 000 en el Reino Unido (Bennett 2004); EUR 205 000 000 por año en Irlanda (Gethin 2005); EUR 461 000 000 por año en España (Agreda 2007); AUD 285 000 000 por año en Australia (Graves 2005); y USD 11 000 000 000 en los EE.UU. (Reddy 2006). En los EE.UU. se ha informado que el costo promedio del tratamiento de una sola úlcera por presión de estadio 4 adquirida en el hospital es de USD 129 248 y el de una úlcera por presión de estadio 4 adquirida en la comunidad es de USD 124 327 (Brem 2010).
Recientemente los gobiernos han adoptado posiciones más consistentes sobre la prevención de la úlcera por presión, por ejemplo, en el Reino Unido, la incidencia de úlcera por presión se ha convertido en un indicador clínico clave para garantizar la seguridad del paciente y el control de las infecciones (NPSA 2010). El interés del que son objeto las úlceras por presión proporciona un impulso renovado para considerar los retos y las complejidades de la prevención de la úlcera por presión en los servicios de salud y de atención social. Se plantea que el énfasis en las intervenciones preventivas de atención sanitaria daría lugar a un uso más efectivo de los recursos, a la vez que también se reducirían al mínimo las enfermedades y las consecuencias sociales presentadas por los individuos "en riesgo" de úlcera por presión. Por ejemplo, en los EE.UU., se ha calculado que el tratamiento de los pacientes con lesiones de la médula espinal y úlcera por presión cuesta USD 1 200 000 000 anualmente, en contraposición con la prevención, que se calcula que cuesta un décimo de esta suma (Byrne 1996). Debido a que se considera que la mayoría de todas las úlceras por presión son prevenibles (DoH 2009; Pope 1999) y que la prevención cuesta menos que el tratamiento (Stroupe 2011), un énfasis en las medidas preventivas puede ser más efectivo en función de los costos para los servicios sanitarios (Stinson 2013).
Descripción de la intervención
La formación del personal de asistencia sanitaria se ha reconocido como un componente integral de la prevención de las úlceras por presión (Dealey 2007). El Royal College of Nursing (RCN 2001) en sus recomendaciones para las guías de práctica clínica sobre la evaluación y la prevención del riesgo de úlceras por presión, consideró que los programas de educación deben incluir una variedad amplia de factores para reflejar la naturaleza multifactorial y compleja de la úlcera por presión. Los programas deben incluir información como: factores de riesgo y fisiopatología del desarrollo de las úlceras por presión; limitaciones y aplicaciones potenciales de las herramientas de evaluación del riesgo; evaluación de la piel; cuidado de la piel; selección, uso y mantenimiento del equipo de redistribución de la presión; métodos de documentación de las evaluaciones del riesgo y de las actividades de prevención; posicionamiento para disminuir el daño por presión, rozamiento y fricción (incluido el uso correcto de los dispositivos de manipulación manual); funciones y responsabilidades de los miembros de los equipos interdisciplinarios en el tratamiento de las úlceras por presión; y educación del paciente y provisión de información. Se han desarrollado guías internacionales más recientes que agrupan ampliamente los componentes clave de la atención preventiva de la úlcera por presión requerida por todos los individuos vulnerables (NPUAP/EPUAP/PPPIA 2014). Los componentes clave se clasifican dentro de estas guías como cuádruples: evaluación de la piel y del riesgo de úlceras por presión; nutrición; reposicionamiento; y superficies de apoyo (cama/silla/colchón/cojín). El National Pressure Ulcer Advisory Panel los ha ampliado para desarrollar un programa basado en la competencia para el uso en la prevención de las úlceras por presión (NPUAP 2013). De igual manera, los paquetes de atención Surfaces, Keep moving, Incontinence, Nutrition (SKIN) o Surfaces, Skin, Keep moving, Incontinence, Nutrition (SSKIN) ofrecen una clasificación que define y agrupa los componentes de la mejor práctica en la atención preventiva de las úlceras por presión (HIS 2011). Estos componentes forman de manera sistemática los aspectos centrales sobre los que se basan las intervenciones educacionales para la práctica de la atención preventiva de la úlcera por presión (Demarre 2011; Kwong 2011; Thomas 2012; Tweed 2008). Sin embargo, aún se debe establecer la efectividad de dichos programas educacionales, qué incluyen de forma óptima y en qué formato.
De qué manera podría funcionar la intervención
La educación es fundamental en el desarrollo y el mantenimiento de la competencia, un componente integral del código de conducta profesional de todos los profesionales de la salud (NPUAP 2013). La educación también proporciona a los profesionales el conocimiento y las aptitudes necesarias para tomar decisiones clínicas bien informadas. La prevención de las úlceras por presión es alcanzable a través de la adopción de guías basadas en la evidencia y estándares altos de atención NPUAP 2013. Sin embargo, para satisfacer estas demandas clínicas, los profesionales de la asistencia sanitaria requieren aptitudes y conocimientos específicos (Beeckman 2008). Los programas educacionales están dirigidos en último término a influir en el cambio conductual del receptor. Por lo tanto, la premisa fundamental es que la provisión de educación a los profesionales de la asistencia sanitaria puede tener el potencial de mejorar su conocimiento y aptitudes en la prevención de las úlceras por presión y producir un cambio positivo en su comportamiento clínico.
Por qué es importante realizar esta revisión
Los programas de educación pueden ayudar a producir un cambio conductual en el profesional de la asistencia sanitaria y así apoyar la reducción general de la incidencia y la prevalencia del desarrollo de las úlceras por presión. Se han realizado estudios que informan que las intervenciones educacionales producen cambios a través de un rango de construcciones, como el conocimiento de la prevención de las úlceras por presión (Kwong 2011; Thomas 2012; Tweed 2008); la clasificación de las úlceras por presión (Beeckman 2008); el cumplimiento de las guías clínicas sobre las úlceras por presión (Demarre 2011); y la evaluación del riesgo de úlceras por presión (Magnan 2008). Por lo tanto, la educación de los profesionales de la asistencia sanitaria con respecto a la prevención de las úlceras por presión puede producir cambios positivos en el conocimiento y en los comportamientos clínicos de dichos individuos, lo que da lugar a mejoras en el cumplimiento de la "práctica adecuada" y provoca una reducción general en la prevalencia y la incidencia de la úlcera por presión. Sin embargo, hasta la fecha no se ha realizado una síntesis de la evidencia relevante sobre el impacto de la educación de los profesionales de la salud en la prevención de las úlceras por presión. Por lo tanto, es de gran importancia la revisión de la evidencia no sólo para determinar si los programas de educación para los profesionales de la asistencia sanitaria pueden ayudar a prevenir la úlcera por presión, sino también para comprender si el contenido educacional, la forma de proporcionarlo, y la intensidad y la duración de su administración tienen un efecto sobre los resultados.
Objetivos
Evaluar los efectos de las intervenciones educacionales para los profesionales de la asistencia sanitaria sobre la prevención de las úlceras por presión.
Métodos
Criterios de inclusión de estudios para esta revisión
Tipos de estudios
Se incluyeron ensayos controlados aleatorios (ECA) y ECA grupales. A falta de este tipo de evidencia se planificó incluir ensayos controlados no aleatorios (ECNA), estudios controlados tipo antes y después (CAD) y estudios de series de tiempo interrumpido (STI). Se excluyeron todos los otros tipos de estudios. No se realizaron restricciones de idioma ni de fecha de publicación.
Tipos de participantes
Todo el personal de asistencia sanitaria involucrado en la prevención de las úlceras por presión de primera línea, que incluye el personal médico y de enfermería, los profesionales paramédicos y los asistentes sanitarios, de todos los ámbitos de asistencia sanitaria que incluyen el ámbito hospitalario y ambulatorio, los consultorios comunitarios y la atención domiciliaria, que prestara asistencia regular a cualquier grupo de pacientes considerado "en riesgo" de úlcera por presión. Se excluyeron los artículos que informaron sobre intervenciones educacionales impartidas a grupos de estudiantes en cualquiera de estas profesiones o ámbitos.
Tipos de intervenciones
Se consideraron todos los programas educacionales dirigidos a mejorar el conocimiento clínico, cambiar el comportamiento clínico y reducir la incidencia de las úlceras por presión. Los mismos pueden haber adoptado la forma de enseñanza directa, enseñanza en línea, aprendizaje combinado, talleres, cursos cortos (series o independientes), materiales didácticos escritos, o educación autodirigida. Se incluyeron los estudios que describían cualquiera de los siguientes:
-
intervención educacional en comparación con ninguna intervención o con la práctica habitual;
-
comparaciones entre diferentes componentes de la intervención educacional;
-
comparaciones entre diferentes formatos de intervención educacional (p.ej. entrenamiento presencial, seminarios en línea, educación a distancia).
Tipos de medida de resultado
Resultados primarios
-
Cambio en el conocimiento de los profesionales de la asistencia sanitaria (examen de evaluación previo y posterior a la intervención, como se definió en cada estudio).
-
Cambio en el comportamiento clínico de los profesionales de la asistencia sanitaria, como se definió en cada estudio (p.ej. inspecciones habituales de la piel, programas mejorados de reposicionamiento o de movilización, cambio en las superficies donde el paciente permanece sentado o acostado, educación del paciente sobre el cuidado de la piel, instrucción en maniobras de alivio de la presión y traslados).
-
Incidencia de nuevas úlceras por presión (como se informó en cada estudio mediante recuentos numéricos o porcentajes de pacientes que desarrollaron cualquier úlcera por presión de cualquier estadio).
Resultados secundarios
-
Gravedad de las nuevas úlceras por presión (como se informó en cada estudio p.ej. mediante la International Pressure Ulcer Classification Scale (NPUAP/EPUAP/PPPIA 2014).
-
Resultados informados por el paciente, como se definió en cada estudio con el uso de medidas de resultado validadas (reducción del dolor, p.ej. McGill Pain Questionnaire, Melzack 1975); (calidad de vida, p.ej. Euroqol, EQ‐5D, Oemar 2013).
-
Resultados informados por el cuidador (mejora en la independencia, p.ej. Barthel Self Care Index, Mahoney 1965).
Métodos de búsqueda para la identificación de los estudios
Búsquedas electrónicas
We searched the following electronic databases to identify reports of RCTs and cluster‐RCTs:
-
Cochrane Wounds Specialised Register (searched 12 June 2017);
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 5) in the Cochrane Library (searched 12 June 2017);
-
Ovid MEDLINE including In‐Process & Other Non‐Indexed citations (1946 to 12 June 2017);
-
Ovid Embase (1974 to 12 June 2017);
-
EBSCO CINAHL Plus (1937 to 12 June 2017).
The search strategies for the Cochrane Wounds Specialised Register, CENTRAL, Ovid MEDLINE, Ovid Embase and EBSCO CINAHL Plus can be found in Appendix 1. We combined the Ovid MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (2008 revision) (Lefebvre 2011). We combined the Embase search with the Ovid Embase filter developed by the UK Cochrane Centre (Lefebvre 2011). We combined the CINAHL Plus searches with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN 2018). There were no restrictions with respect to language, date of publication or study setting.
We also searched the following clinical trials registries:
-
ClinicalTrials.gov (www.clinicaltrials.gov/) (searched February 2018);
-
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/Default.aspx) (searched February 2018);
-
EU Clinical Trials Register (www.clinicaltrialsregister.eu/ctr‐search/search) (searched February 2018).
Search strategies for clinical trials registries can be found in Appendix 1.
Búsqueda de otros recursos
We searched the bibliographies of all included trials identified by the above strategies for further relevant studies.
Obtención y análisis de los datos
We carried out data collection and analysis according to methods stated in a published protocol (Porter‐Armstrong 2015).
Selección de los estudios
Cochrane Wounds' Information Specialist ran the electronic searches. Two review authors (APA, ZM) independently screened all titles and abstracts retrieved by the searches and excluded those that did not meet the inclusion criteria given above. If no abstract was available, we obtained the full paper and assessed it. Two review authors (APA, ZM) retrieved and assessed for eligibility the full texts of all trials classified as relevant. Disagreement between review authors was resolved by consensus, or third party adjudication (SMcD). All full papers retrieved, but subsequently excluded, are disclosed in the Characteristics of excluded studies table, with full reasons given. A PRISMA flowchart of the data management phase of the review is shown in Figure 1 (Liberati 2009).
Extracción y manejo de los datos
We modified the data extraction forms developed by the Effective Practice and Organisation of Care Group (EPOC 2018) and used them to extract the data from the selected studies. Two review authors (APA, ZM) independently extracted the data. We piloted the data extraction forms with a small number of studies to ensure that the correct type and level of information was being recorded. We extracted data on:
-
author, title and source;
-
date of study, country of origin;
-
study design type and details;
-
inclusion and exclusion criteria;
-
details about the intervention (e.g. format of delivery, composition of programme, length of programme, setting);
-
participant characteristics (e.g. number, education, professional training, professional background, practice setting);
-
trial quality (e.g. allocation method, outcome assessment, completeness of reporting);
-
all primary and secondary outcomes;
-
statistical analysis used;
-
outcomes data for primary and secondary outcomes;
-
funding source;
-
conflicts of interest.
We resolved any differences in opinion between the two review authors by consensus. Where necessary, we made contact with trial authors for clarification of study characteristics and data.
Evaluación del riesgo de sesgo de los estudios incluidos
Two review authors independently assessed risk of bias for each study using the following criteria and resolved any disagreements through consensus.
For all included studies we used the Cochrane tool for assessing risk of bias (Higgins 2011a). This tool addresses six specific domains, namely sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other issues (e.g. extreme baseline imbalance), see Appendix 2 for details of criteria on which we based judgements. For trials using cluster randomisation, we specifically considered recruitment bias, baseline imbalance, loss of clusters, incorrect analysis and comparability with individually randomised trials (Appendix 3). We assessed blinding and completeness of outcome data separately for each outcome. We completed a 'Risk of bias' table for each eligible study. We present assessment of risk of bias using a 'Risk of bias' summary figure (Figure 2), which presents all of the judgements in a cross‐tabulation of study by entry. This display of internal validity indicates the weight the reader may give the results of each study.
For controlled before‐after (CBA) studies and interrupted‐time‐series (ITS) studies we planned to use the 'Risk of bias' tool from the Cochrane EPOC group (EPOC 2013) to assess risk based upon (where appropriate to study design) allocation sequence; allocation concealment; similarity of outcome measurement; similarity of baseline characteristics; incomplete outcome data; allocation blinding; contamination; selective reporting; and other bias.
Where information on risk of bias related to unpublished data or correspondence with a trial author, we planned to note this in the 'Risk of bias' table.
Medidas del efecto del tratamiento
Dichotomous data
For dichotomous data, we made 2 x 2 contingency tables for each study, showing the number of participants with each outcome event and calculated risk ratios (RRs) with 95% confidence intervals (CIs).
Continuous data
We analysed continuous data if means and standard deviations were available, on the scale chosen in the original publication. For continuous outcomes measured identically across studies, we calculated an overall mean difference (MD) and 95% CI. If only median and interquartile ranges were presented, we converted these to estimated mean and variance, assuming normality. Otherwise, we calculated standardised mean difference (SMD) and 95% CI (Higgins 2011b).
Ordinal data
We planned to analyse ordinal (ordered categorical) data depending on the data presented in the original reports. If sufficient data were available from individual reports, we planned to analyse the data as ordinal data using proportional odds regression.
Cuestiones relativas a la unidad de análisis
Cluster‐RCTs
If cluster‐RCTs had been included in the meta‐analysis, we planned to first seek evidence in the publication that the authors made appropriate adjustments in their analysis to account for the clustering of data. In doubtful cases, we planned to contact the trial authors. If the error estimate had not been corrected, and necessary data were available to allow this, we planned to attempt to make the correction – if necessary using intraclass correlation coefficient estimates from other published studies. However, because there was only one cluster trial (Van Gaal 2010) we were unable to undertake meta‐analysis. Therefore, we reported results for the outcomes of this review without meta analysis.
Multiple trial arms
For studies with multiple intervention groups, we made multiple pair‐wise comparisons between all possible pairs of intervention groups, which were presented as separate analyses.
Interrupted time series studies
If required, and if sufficient data were available in the published study or from the original trial authors, we planned to re analyse results to account for unit of analysis errors in ITS designs.
Manejo de los datos faltantes
If summary items such as standard errors were missing from the published report, we contacted the trial authors in order to verify key study characteristics and obtain missing numerical outcome data where possible. If missing data were unobtainable, we planned to present the available‐cases result together with two alternatives; first imputing missing data by the treatment arm mean, and second imputing missing data by the control arm mean. In both cases, we planned to analyse data outside of Review Manager 5 (Review Manager 2014) to allow study weights from the available‐cases analysis to be used in order to avoid inflating the apparent precision of the estimates.
Where the missing data were thought likely to introduce a risk of bias, we noted this in the 'Risk of bias' table and planned to explore the impact of including such studies in the overall assessment of results by a sensitivity analysis.
Evaluación de la heterogeneidad
We planned to use the I² statistic (Higgins 2003) to measure heterogeneity among the trials in each analysis and would have reported our findings for each analysis. If we identified unexplained heterogeneity, that is, Chi² test significant at the level of 0.1, I² greater than 50%, and changes in direction of effect, we planned to first explore clinical explanations for such heterogeneity, for example with important subgroups. If we were unable to explain the heterogeneity clinically, then we planned to use random‐effects analysis or narrative review.
Evaluación de los sesgos de notificación
We planned to assess reporting bias using Cochrane guidelines (Sterne 2010). If sufficient studies were found (at least 10), we planned to use funnel plots to investigate asymmetry in respect of publication and selective reporting bias and conduct Egger Tests to assess for bias.
Síntesis de los datos
We planned to use Review Manager 5 (Review Manager 2014) to perform meta‐analysis of the included studies separately for continuous, dichotomous and ordinal outcomes, and planned to present the meta‐analysis using forest plots and statistical summaries. We planned to use a fixed‐effect model unless there were clinical or statistical reasons (I² statistic greater than 50%) to suspect significant heterogeneity, in which case we planned to use random‐effects analysis (I²≤ 75%) or narrative review (I² > 75% or clinical heterogeneity).
Análisis de subgrupos e investigación de la heterogeneidad
We planned to analyse potential sources of heterogeneity using the following subgroup analyses:
-
type of setting (community, hospital, inpatient, outpatient);
-
type of healthcare professional (medical staff, nursing staff, allied health professional);
-
type of education approach (face‐to‐face, e‐learning, webinars).
Análisis de sensibilidad
We planned to perform sensitivity analyses to examine how the results of any meta‐analysis would change under the following assumptions:
-
we planned to assess the robustness of results by only including studies assessed as low risk of bias. We planned to exclude trials deemed most susceptible to bias based upon the quality assessment, particularly those with inadequate allocation concealment, uncertain or unblinded outcome assessment, or incomplete outcome data;
-
we planned to explore the effect of inadequate correction for clustering by varying the assumed intracluster correlation coefficient, and by omitting studies whose primary report had apparently failed to correct for clustering;
-
we planned to explore the effect of inadequate correction for auto correlation in ITS studies by omitting studies whose primary report had apparently failed to correct for auto correlation;
-
we planned to assess the effect of missing data by, where possible (a) restricting the analysis to only studies without missing data, and (b) restricting the analysis to complete studies plus those that had attempted to adjust for missing data.
'Summary of findings' tables
We have presented 'Summary of findings' tables for the following primary outcomes: healthcare professionals' knowledge (pre‐ and post‐test assessment following intervention, and comparisons between the control and experimental group post‐test), health professionals' clinical behaviour, and pressure ulcer incidence (proportion of patients developing a new ulcer). We have also included the following secondary outcomes in the 'Summary of findings' tables: severity of new pressure ulcers, patient‐reported outcomes and carer‐reported outcomes. We assessed the quality of the published evidence using the GRADE protocol (Guyatt 2011) against the following five key issues:
-
limitations in the design and implementation of available studies suggesting high likelihood of bias;
-
indirectness of evidence (indirect population, intervention, control, outcomes);
-
unexplained heterogeneity or inconsistency of results (including problems with subgroup analyses);
-
imprecision of results (including wide confidence intervals);
-
high probability of publication bias (Schünemann 2011).
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies.
Results of the search
The search yielded 282 citations. Two review authors examined the abstracts of all the papers, independently, to assess for potential relevance. Of these, we retrieved eleven studies for further assessment and after examination, five studies met the inclusion criteria (Bredesen 2016; Hayes 1994; James 1998; Rantz 2012; Van Gaal 2010); four studies were excluded (Danchaivijitr 1995; Esche 2015; Rantz 2001; Shannon 2012); and two trials were retrieved through searching of trial registers and identified as relevant ongoing studies (IRCT2017080935602N1; NCT02270385), refer to Characteristics of ongoing studies for more details about these trials. See PRISMA flow chart (Figure 1).
Included studies
We have included five studies in this review (Bredesen 2016; Hayes 1994; James 1998; Rantz 2012; Van Gaal 2010). See Characteristics of included studies. Three studies purported to be cluster‐RCTs, conducted in the Netherlands (Van Gaal 2010), the UK (James 1998), and the USA (Rantz 2012); of which only one was truly a cluster‐RCT (Van Gaal 2010), and two were parallel group RCTs (James 1998; Rantz 2012). The other two studies were also parallel‐group RCTs undertaken in the USA (Hayes 1994) and Norway (Bredesen 2016).
Populations
The studies were undertaken in the following settings: two acute care hospitals and four nursing homes in Norway (Bredesen 2016), an urban acute care hospital in the USA (Hayes 1994), 37 residential homes in the UK (James 1998), 58 nursing homes in the USA (Rantz 2012), and 20 hospital and nursing home wards in the Netherlands (Van Gaal 2010).
In Bredesen 2016, Hayes 1994 and Van Gaal 2010, the participants were nursing staff (registered nurses, licensed practical nurses and nursing assistants) and James 1998 described the participants as nursing staff. In Rantz 2012, the participants were owners of facilities, nursing and administrative facility staff, and direct‐care staff. However, the intervention was directed at the leaders of the facilities.
James 1998 and Rantz 2012 did not provide information pertaining to the sample size of the intervention target population. The mean sample size in the remaining three studies (Bredesen 2016; Hayes 1994; Van Gaal 2010) was 327 participants (SD 361; min 44, max 837).
Neither James 1998 nor Rantz 2012 provided data regarding the age or gender distribution of the intervention target participants. In Hayes 1994, the mean age of the participants was 33.3 years (SD 10.3 years, min 20 years, max 69 years), and 81.2% (n = 91) were female. In Van Gaal 2010, the mean age of the participants was 38 years (SD 10.7 years), and 89% (n = 411) were female. Bredesen 2016, provided data on gender distribution only and 97.7% (n = 43) of the participants were female.
Interventions
Bredesen 2016 randomly assigned nurses to one of two groups. Each participant in the e‐learning group completed an individual, computer‐based training module on pressure ulcer risk assessment and classification. The classroom group received the same training module content on pressure ulcer risk assessment and classification, delivered through a 45‐minute lecture format by an experienced nurse using a PowerPoint presentation. Similarly, Hayes 1994 randomly assigned nurses to one of two groups. The intervention group received a 40‐minute instructional educational session, based on pressure ulcer prevention and treatment information, and the control group viewed a 25‐minute video on general skin care for hospitalised patients.
In James 1998, there were three study groups, and nursing homes were randomised to one of the three groups. Although termed as a cluster randomised trial, this was a parallel RCT with the outcomes of interest at a nursing home level, rather than at the level of the individual patient, and nursing homes were the unit of randomisation.The intervention group received three elements: training, monitoring and observation. Training comprised a two‐hour, interactive educational session delivered by a district nurse covering pressure ulcer risk assessment, grading and preventative strategies including nutrition, continence, mobility, and moving and handling. Monitoring comprised a district nurse‐led educational session on pressure ulcer risk assessment and grading only. Observation comprised data collection via a point prevalence assessment at baseline, six, 12 and 18 months.
Rantz 2012 was also termed a cluster randomised trial, however similar to James 1998, this was a parallel RCT as the outcomes were measured at the nursing home level and the unit of randomisation was the nursing homes. Outcomes were compared between the control or intervention groups of the study. The multilevel intervention targeted three levels of staff responsible for operating a nursing facility: owners, nursing and administrative facility staff, and direct‐care staff. Owners were asked, at least for the duration of the study, to (1) provide consistent nursing and administrative leadership, (2) adopt the elements of change (EC) into their management practices, and to actively support and encourage (3) the use of team and group processes for decision‐making affecting resident care, (4) the use of a quality‐improvement programme and (5) the efforts of staff to focus on performing the basics of care, including ambulation, nutrition and hydration, toileting, bowel regularity, preventing skin breakdown and managing pain. The trial investigators provided a detailed intervention manual and two text books to the leaders of each intervention facility. The research nurse observed direct‐care staff at work and then met with them and nursing administrative staff in quality‐improvement teams. These groups tailored care systems and practices outlined in the intervention manual to fit their situation, anchoring them into their facility's care routines.
Van Gaal 2010 used cluster randomisation to allocate five hospital wards and five nursing home wards to the intervention group, and five hospital wards and five nursing home wards to the control group. The intervention consisted of small‐scale, educational meetings, educational materials and outreach visits, delivered to all nurses in the participating wards in the intervention group. Outcomes were measured at the individual patient level.
Comparisons
The control group in the original protocol of Bredesen 2016 were to receive no additional education. However, due to "massive dropout" (p 192) this control group was excluded from the study and was not reported upon. The control group in Hayes 1994 received monthly, videotaped, in‐service training and reading materials about aging and physical assessment of elderly residents, topics that were not directly related to quality‐improvement strategies.
James 1998 used two control groups, one of monitoring and observation, and one of observation only, as the comparators. Monitoring comprised a district nurse‐led educational session on pressure ulcer risk assessment and grading only. Observation comprised data collection via a point prevalence assessment at baseline, six, 12 and 18 months.
The control group in Rantz 2012 received a monthly mailing of general educational material pertaining to elderly care, alongside a monthly telephone call from the co‐investigator to answer any questions relating to the materials, whereas the Van Gaal 2010 control group received no intervention at all.
Outcomes
All studies reported at least one of the primary outcomes of interest for this review. However, these outcomes varied across all five studies and included pressure ulcer development (Rantz 2012); pressure ulcer development, functional dependency and self‐reported quality of life (James 1998); and knowledge of pressure ulcer risk, classification, assessment and treatment (Bredesen 2016; Hayes 1994; Van Gaal 2010).
Excluded studies
We excluded four studies from this review: two studies because they were not RCT design (Danchaivijitr 1995; Esche 2015), one because the study purpose was different from the focus of this review (Rantz 2001), and the other as trial participants in both groups received the educational intervention before the study began (Shannon 2012). See Characteristics of excluded studies.
Risk of bias in included studies
All five studies were at high or unclear risk of bias. We have presented details in separate 'Risk of bias' tables for each of the five studies (see Characteristics of included studies) and in a summary table and graph (Figure 2; Figure 3). As no meta‐analyses were performed, the one cluster randomised controlled trial was assessed against the first 4 of the 5 additional risk of bias criteria for cluster trials (Appendix 3).
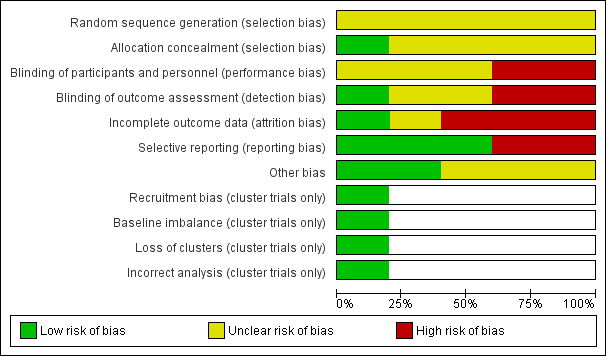
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
All five studies reported methods of randomisation. In Bredesen 2016, the principal investigator assigned participants using block randomisation to the e‐learning or classroom‐based group. Similarly in Hayes 1994, one of the investigators assigned participants randomly to the experimental or control group. In James 1998, allocation to study group was at the level of the nursing home which was also the unit of analysis. Rantz 2012 randomised owners of nursing homes to either the intervention or control group, then randomly invited individual nursing homes to participate and if they agreed, assigned them to the group designation based upon the owner; again the nursing home was the unit of analysis. Van Gaal 2010 used cluster randomisation, where allocation was by ward, stratified by centre and type of ward.
Allocation concealment was reported in Bredesen 2016 through the use of closed, opaque, numbered envelopes to conceal group allocation. The other four studies did not report allocation concealment.
Blinding
James 1998 disclosed that participating staff were aware of group allocation and we thus judged it to be at high risk for performance bias. Similarily judged as high risk was Van Gaal 2010, as participants would have known their group allocation based upon whether they received the educational intervention or not. It is unclear whether blinding of participants occurred in Bredesen 2016; Hayes 1994 or Rantz 2012.
It is reasonable to assume that blinding of participants and staff would have been difficult to achieve, as it would have been clear which group the participant was in. Nonetheless, blinded outcome assessment would have been possible in terms of pressure ulcer development, functional dependency, self‐reported quality of life and knowledge scores, as these outcomes were gathered using data‐collection instruments, which could have been anonymised regarding study allocation.
Blinding of outcome assessment was reported in only one study (Rantz 2012). One study reported that they did not undertake blinded outcome assessment (James 1998). We judged Van Gaal 2010 to be at high risk as, at each ward, one nurse was responsible for the distribution and collection of the questionnaires, so we judged it likely that this nurse knew group allocation. Blinding of outcome assessment was not reported in Bredesen 2016 or Hayes 1994 and we thus judged them to be at unclear risk of bias.
Incomplete outcome data
We judged Van Gaal 2010 to be at high risk of attrition bias, as the actual attrition rates in the study were judged to be higher than acceptable. In the pre‐intervention phase, the response rates for the questionnaires were: 80% intervention group and 72% control (hospital wards), and 66% intervention group and 71% control (nursing home wards). In the postintervention phase, the response rates for the questionnaires were: 49% intervention group and 87% control (hospital wards), and 58% intervention group and 56% control (nursing home wards). In Rantz 2012, there was also a dropout rate for response to the survey employed (intervention group 71% baseline and 63% study end; control group 65% baseline; 53% study end), thus we judged it to be at high risk of attrition bias. Similarily, we also judged Bredesen 2016 to be at high risk of attrition bias, with an overall drop out rate of 59% at the three‐month, postintervention phase (e‐learning group 52% baseline and 23% study end; classroom group 48% baseline and 18% study end). We judged James 1998 as unclear as there was insufficient information provided to make a full assessment. Only Hayes 1994 was judged to be at low risk of attrition bias.
Selective reporting
We judged Bredesen 2016 at high risk of selective reporting bias as the study authors excluded the original control group comprising no additional education from the study report due to dropout and only reported on the two active education arms of the study. Further, whilst the study protocol stated that they had planned a 24‐week measurement, they did not report it. Another study did not report all the outcomes described in the methods section in sufficient detail to allow full interrogation of the data, therefore we have scored this accordingly, at high risk of bias (James 1998). The other three studies (Hayes 1994; Rantz 2012; Van Gaal 2010) reported on all the outcomes measured and therefore we judged them to be at low risk of reporting bias.
Other potential sources of bias
No other potential sources of bias were apparent from two of the studies (Hayes 1994; Rantz 2012). Participants in Bredesen 2016 were not asked about their computer proficiency in using an e‐learning platform to access training and thus, as a potential source of bias, we assessed it as unclear. James 1998 provided limited information pertaining to the characteristics of the nursing staff participants and thus, as a potential source of bias, we assessed it as unclear. Van Gaal 2010 used a non‐standardised outcome measure to gather data and thus, as a potential source of bias, we assessed it as unclear.
Effects of interventions
See: Summary of findings for the main comparison Education compared to no education for preventing pressure ulcers; Summary of findings 2 Training, monitoring and observation compared to monitoring and observation for preventing pressure ulcers; Summary of findings 3 Training, monitoring and observation compared to observation alone for preventing pressure ulcers; Summary of findings 4 Monitoring and observation compared to observation alone for preventing pressure ulcers; Summary of findings 5 Didactic education versus video education for preventing pressure ulcers; Summary of findings 6 E‐learning versus classroom education for preventing pressure ulcers
Comparison 1. Education versus no education (1 trial, 20 wards from 4 hospitals and 6 nursing homes)
Primary outcome
Changes in health professionals' knowledge
One study (Van Gaal 2010) reported the primary outcome: change in healthcare professionals' knowledge.
Van Gaal 2010 evaluated change in nurses' knowledge using a 20‐item pressure ulcer knowledge test developed for the study, at baseline and one year post baseline. Due to differences in nurses' characteristics between hospitals and nursing homes, the study authors analysed the data for hospital wards and nursing home wards separately. The study authors did not undertake any analysis for the effect of clustering. We have reported the data from the study as further analysis was not possible. We classed this study at high risk of bias, since the 95% CIs would be narrower than they would have been had the correct analysis been undertaken. It is unclear whether education versus no education makes any difference to health professionals' knowledge, as we assessed the certainty of the evidence as very low (downgraded twice for serious limitations due to performance bias, detection bias and attrition bias, and downgraded twice for indirectness due to use of a non validated instrument to assess knowledge, and imprecision due to a wide confidence interval) see summary of findings Table for the main comparison. The mean knowledge score for the hospital participants was 6 (SD: 1.1) for the education group and 5.7 (SD: 0.99) for the no‐education group (MD 0.30, 95% CI ‐1.00 to 1.60; 10 participants; Analysis 1.1). The mean post‐test knowledge score for the nursing home participants was 5.4 (SD: 0.96) for the education group and 5.1 (SD: 0.76) for the no‐education group (MD 0.30, 95% CI ‐0.77 to 1.37; 10 participants; Analysis 1.2) (pre‐test knowledge scores were 5.0 (0.84) and 4.8 (0.78) respectively).
Changes in health professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
Not reported
Secondary outcomes
Severity of new pressure ulcers
Not reported
Patient‐reported outcomes
Not reported
Carer‐reported outcomes
Not reported
Comparison 2. Comparisons between different components of educational intervention: training, monitoring and observation versus monitoring and observation (1 trial, 37 residential homes with 345 residents)
Primary outcomes
Change in health professionals' knowledge
Not reported
Change in health professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
One study (James 1998) reported the primary outcome: incidence of pressure ulcers.
James 1998 used the Norton scale (Norton 1975) and research nurse skin assessments at baseline, 6, 12 and 18 months, to calculate incidence of pressure ulcers. It is unclear whether training, monitoring and observation versus monitoring and observation makes any difference to pressure ulcer incidence, as we assessed the certainty of the evidence as very low (downgraded twice for serious limitations due to performance bias, detection bias and outcome reporting bias, and downgraded once for imprecision due to a wide confidence interval) see summary of findings Table 2. In the training, monitoring and observation group, 11.4% of patients (25/219) developed a pressure ulcer during the study period, whereas in the monitoring and observation group 18% of patients (23/125) developed a pressure ulcer during the study period (RR 0.63, 95% CI 0.37 to 1.05; 345 participants; Analysis 2.1).
Secondary outcomes
James 1998 measured the following secondary outcomes.
Severity of new pressure ulcers
James 1998 measured severity of pressure sores using the David classification of pressure sore severity (David 1983), a four‐stage grading system, used weekly by the staff and recorded by the research nurse assessor at baseline, 6, 12 and 18 months. The study report did not present any data on this outcome to enable further evaluation.
Patient‐reported outcomes
James 1998 used Euroqol (Oemar 2013) to measure the self‐assessed quality of life of the residents at all four time points and reported no differences in scores between the groups of residents during the 18‐month study period. The report presented insufficient data to enable further interrogation of this outcome.
Carer‐reported outcomes
James 1998 used the Bathel Index (Mahoney 1965) to measure the functional dependency level of the residents at all four time points throughout the study. The trial author reported no differences, but there were insufficient data within the report to further interrogate this outcome.
Comparison 3. Comparisons between different components of educational intervention: training, monitoring and observation versus observation alone (1 trial, 37 residential homes with 325 residents)
Primary outcomes
Change in health professionals' knowledge
Not reported
Change in health professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
One study (James 1998) reported the primary outcome: incidence of pressure ulcers.
James 1998 used the Norton scale (Norton 1975) and research nurse skin assessments at baseline, 6, 12 and 18 months, to calculate incidence of pressure ulcers. It is unclear whether training, monitoring and observation versus observation alone makes any difference to pressure ulcer incidence, as we assessed the certainty of the evidence as very low (downgraded twice for serious limitations due to performance bias, detection bias and outcome reporting bias, and downgraded once for imprecision due to a wide confidence interval) see summary of findings Table 3. In the training, monitoring and observation group 11.4% of patients (25/219) developed a pressure ulcer during the study period, whereas in the observation group 10% of patients (10/106) developed a pressure ulcer during the study period (RR 1.21, 95% CI 0.60 to 2.43; 325 participants); Analysis 3.1).
Secondary outcomes
James 1998 measured the following secondary outcomes.
Severity of new pressure ulcers
James 1998 measured severity of pressure ulcers using the David classification of pressure sore severity (David 1983), a four‐stage grading system, used weekly by the staff and recorded by the research nurse assessor at baseline, 6, 12 and 18 months. The study report did not present any data on this outcome to enable further evaluation.
Patient‐reported outcomes
James 1998 used Euroqol (Oemar 2013) to measure the self‐assessed quality of life of the residents at all four time points and reported no differences in scores between the groups of residents during the 18‐month study period. The report presented insufficient data to enable further interrogation of this outcome.
Carer‐reported outcomes
James 1998 used the Bathel Index (Mahoney 1965) to measure the functional dependency level of the residents at all four time points throughout the study. The trial author reported no differences, but the report presented insufficient data to further interrogate this outcome.
Comparison 4. Comparisons between different components of educational intervention: monitoring and observation versus observation alone (1 trial, 37 residential homes with 232 residents)
Primary outcomes
Change in health professionals' knowledge
Not reported
Change in health professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
One study (James 1998) reported the primary outcome: incidence of pressure ulcers.
James 1998 used the Norton scale (Norton 1975) and research nurse skin assessments at baseline, 6, 12 and 18 months, to calculate incidence of pressure ulcers. It is unclear whether monitoring and observation versus observation alone makes any difference to pressure ulcer incidence, as we assessed the certainty of the evidence as very low (downgraded twice for serious limitations due to performance bias, detection bias and outcome reporting bias, and downgraded once for imprecision due to a wide confidence interval) see summary of findings Table 4. In the monitoring and observation group 18% of patients (23/125) developed a pressure ulcer during the study period, whereas in the observation group 10% of patients (10/106) developed a pressure ulcer during the study period (RR 1.93, 95% CI 0.96 to 3.88; 232 participants; Analysis 4.1).
Secondary outcomes
James 1998 measured the following secondary outcomes.
Severity of new pressure ulcers
James 1998 measured severity of pressure ulcers using the David classification of pressure sore severity (David 1983), a four‐stage grading system, used weekly by the staff and recorded by the research nurse assessor at baseline, 6, 12 and 18 months. The study report did not present any data on this outcome to enable further evaluation.
Patient‐reported outcomes
James 1998 used Euroqol (Oemar 2013) to measure the self‐assessed quality of life of the residents at all four time points and reported no differences in scores between the groups of residents during the 18‐month study period. The report presented insufficient data to enable further interrogation of this outcome.
Carer‐reported outcomes
James 1998 used the Bathel Index (Mahoney 1965) to measure the functional dependency level of the residents at all four time points throughout the study. The trial author reported no differences, but the report presented insufficient data to further interrogate this outcome.
Comparison 5. Comparisons between different components of educational intervention: multilevel intervention versus attention control (1 trial, 58 nursing homes)
Primary outcomes
Change in health professionals' knowledge
Not reported
Change in health professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
One study (Rantz 2001) reported the primary outcome: odds of pressure ulcer development.
Rantz 2012 used repeated measures analysis and applied a logistic regression model to calculate the odds ratio of pressure ulcer development between the study groups. The trial authors reported a reduction in pressure ulcer incidence, however, the report presented insufficient data to enable further interrogation of this outcome. Using the GRADE assessment, this was assessed as low certainty evidence (downgraded twice for multiple issues with risk of bias).
Secondary outcomes
Severity of new pressure ulcers
Not reported
Patient‐reported outcomes
Not reported
Carer‐reported outcomes
Not reported
Comparison 6. Comparison between different formats of education: didactic education versus video education (1 trial, 102 participants)
Primary outcome
Change in healthcare professionals' knowledge
One study (Hayes 1994) reported the primary outcome: change in healthcare professionals' knowledge.
Hayes 1994 evaluated changes in nurses' knowledge of pressure ulceration using a 100‐item, true‐false questionnaire developed for the study pre‐ and postintervention, a higher score indicated better knowledge. It is unclear whether education delivered via didactic lecture versus education delivered via video makes any difference to health professionals' knowledge, as we assessed the certainty of the evidence as very low (downgraded once for serious limitations due to unclear risk of selection bias, performance bias and detection bias, and downgraded twice for serious imprecision due to small sample size and a wide confidence interval) see summary of findings Table 5. The mean knowledge score for the didactic lecture group was 84.62 (SD: 4.01) and for the video education group was 89.22 (SD: 3.80); (MD 4.60, 95% CI 3.08 to 6.12; 102 participants; Analysis 5.1).
Change in healthcare professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
Not reported
Secondary outcomes
Severity of new pressure ulcers
Not reported
Patient‐reported outcomes
Not reported
Carer‐reported outcomes
Not reported
Comparison 7. Comparison between different formats of education: education delivered via e‐learning versus classroom education (1 trial, 18 participants)
Primary outcome
Change in healthcare professionals' knowledge
One study (Bredesen 2016) reported the primary outcome: change in healthcare professionals' knowledge.
Bredesen 2016 evaluated changes in nurses' knowledge of pressure ulcer classification, using 40 photos of pressure ulcers representing different categories (normal skin, categories 1 to 4), a higher score indicated better knowledge. It is unclear whether education delivered via e‐learning versus education delivered via the classroom makes any difference to health professionals' knowledge, as we assessed the certainty of the evidence as very low (downgraded twice for serious limitations due to high risk of attrition and selective reporting bias, and unclear risk of selection, performance, detection and other bias, and downgraded once for serious imprecision due to small sample size) see summary of findings Table 6. Participants in the e‐learning group correctly classified 64% of photographs (128/200), participants in the classroom education group correctly classified 69% of photographs (111/160); (RR 0.92, 95% CI 0.80 to 1.07; 18 participants; Analysis 6.1).
Bredesen 2016 also evaluated changes in nurses' knowledge of pressure ulcer risk assessment, using the Braden pressure ulcer risk assessment tool (Bergstrom 1987). No summative scores are provided by the study authors, however, they report that there were no differences found in Braden sub scale scores between the e‐learning group and the classroom group. The report provides insufficient data to further interrogate this outcome.
Change in healthcare professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
Not reported
Secondary outcomes
Severity of new pressure ulcers
Not reported
Patient‐reported outcomes
Not reported
Carer‐reported outcomes
Not reported
Discusión
Resumen de los resultados principales
Se identificaron cinco estudios que cumplieron los criterios de inclusión para esta revisión (Bredesen 2016; Hayes 1994; James 1998; Rantz 2012; Van Gaal 2010). Debido a la heterogeneidad de los estudios identificados, no fue apropiado realizar el agrupamiento y se presentó un resumen narrativo. Se exploraron tres comparaciones clave (1) educación versus ninguna educación (2) componentes de la intervención educacional en varias combinaciones y (3) educación proporcionada en diferentes formatos.
No existe seguridad con respecto a si hay una diferencia en el conocimiento de los profesionales de la salud, en dependencia de si reciben educación o no, sobre la prevención de las úlceras por presión. Lo anterior se basó en evidencia de muy baja certeza de un estudio, Van Gaal 2010. La evidencia se disminuyó debido a las limitaciones graves de los estudios, la imposibilidad de generalizar la evidencia y la imprecisión.
No existe seguridad con respecto a si hay una diferencia en la incidencia de las úlceras por presión cuando se utilizan diferentes componentes de las intervenciones educacionales como combinaciones de entrenamiento, monitorización y observación o intervenciones multinivel versus control. Lo anterior se basa en evidencia de muy baja certeza de dos estudios (James 1998; Rantz 2012). La evidencia se disminuyó debido a las limitaciones graves y a la imprecisión de los estudios.
No existe seguridad con respecto a si la educación proporcionada en diferentes formatos como la educación didáctica y la educación basada en videos o la educación a distancia y la educación en el aula, logran algún cambio en el conocimiento de los profesionales de salud sobre la prevención de las úlceras por presión. Lo anterior se basa en evidencia de muy baja certeza de dos estudios (Bredesen 2016; Hayes 1994). La evidencia se disminuyó debido a las limitaciones graves y a la imprecisión de los estudios.
Ningún estudio exploró el otro resultado primario de interés, cambios en el comportamiento clínico de los profesionales de la salud.
Solamente un estudio (James 1998) exploró los resultados secundarios de interés, a saber; gravedad de la úlcera por presión, calidad de vida informada por el paciente y nivel de dependencia funcional informada por el cuidador. Sin embargo, el estudio no proporcionó información suficiente para permitir la evaluación independiente de estos resultados dentro de la revisión.
En general estos hallazgos reflejan la escasez de la base de evidencia que existe en esta área, y la incertidumbre de la evidencia existente. En resumen, no es posible determinar si la educación de los profesionales de la asistencia sanitaria acerca de la prevención de las úlceras por presión logra algún cambio en la incidencia de las úlceras por presión, en el conocimiento del personal de enfermería sobre la prevención de las úlceras por presión o en el comportamiento clínico de los profesionales de la asistencia sanitaria. Lo anterior se debe a que los estudios incluidos tuvieron riesgo incierto o alto de sesgo y la evaluación GRADE determinó que todos los estudios proporcionaron evidencia de muy baja certeza. Por lo tanto, se necesita más información para aclarar el impacto de la educación de los profesionales de la asistencia sanitaria en la prevención de las úlceras por presión.
Compleción y aplicabilidad general de las pruebas
La provisión de educación a los profesionales de la asistencia sanitaria para prevenir las úlceras por presión sólo se ha evaluado en cinco ensayos controlados aleatorios pequeños con asignación al azar grupal. Este hecho dio lugar a evidencia muy limitada. No fue posible realizar metanálisis ni análisis de subgrupos debido a la heterogeneidad de los estudios incluidos. Los cinco estudios investigaron ámbitos de asistencia sanitaria diferentes, desde residencias geriátricas (Rantz 2012) y hogares de atención residencial (James 1998) hasta salas de hospitales (van Gaal 2010) y diferente personal (Bredesen 2016; Hayes 1994). Ninguno de los estudios utilizó las mismas medidas de resultado para evaluar la eficacia. Los cinco estudios administraron diferentes formatos y contenido educacional. Esta amplia variación en el ámbito, la evaluación de los resultados, el formato y el contenido dio lugar a que no fuera posible realizar comparaciones directas. Ninguno de los cinco estudios proporcionó educación a otro personal que no perteneciera al área de enfermería o no realizara la función de enfermería.
Se debe reconocer la incongruencia entre dirigir una intervención al personal de asistencia sanitaria y medir los resultados y prever los cambios a nivel del paciente (incidencia de las úlceras por presión). Además, en algunos de los ensayos, los pacientes se incluyeron independientemente del riesgo de úlcera por presión. Este hecho podría explicar los efectos pequeños o ausentes, debido a que los pacientes sin riesgo no se van a beneficiar con esta intervención. Una manera de considerar lo anterior sería reclutar a individuos "en riesgo" y luego monitorizar si la intervención educacional cambió el riesgo de desarrollar úlceras por presión. Para diseñar estudios con el poder estadístico apropiado para explorar los efectos de las intervenciones de asistencia sanitaria directamente sobre la incidencia de las úlceras por presión se necesitarían poblaciones clínicas muy grandes, lo que posiblemente daría lugar a ensayos no factibles y no pragmáticos. Por lo tanto, los estudios de las úlceras por presión como los incluidos en esta revisión seleccionan resultados provisionales o sustitutos que puedan representar un precursor del desarrollo de nuevas úlceras por presión o aportar evidencia para apoyar las prácticas preventivas en el área, o ambos.
Se observa una capa adicional de disociación entre la intervención a nivel del personal y el resultado real de interés (incidencia de las úlceras por presión) debido al uso del diseño de ECA con asignación al azar grupal adoptado por uno de los cinco estudios de esta revisión. Este estudio asignó al azar a los grupos de personal de asistencia sanitaria según el ámbito de atención en el cual trabajaban. Los que recibieron la atención, por defecto, se seleccionaron para participar en el estudio en virtud del lugar en el que recibían la atención y no principalmente por su "riesgo" de desarrollar una úlcera por presión. Por lo tanto, la medición de cualquier efecto de la intervención a nivel del paciente mediante este diseño se complica aún más.
Calidad de la evidencia
En términos generales, la evidencia se consideró de certeza muy baja para los resultados clave de incidencia de la úlcera por presión y conocimiento de los profesionales de la asistencia sanitaria.
Debido a la heterogeneidad de los resultados de los estudios y a la imposibilidad de agrupar los datos, se aplicaron los criterios GRADE a cada estudio de forma individual, en contraposición con un grupo de evidencia combinado concerniente a los resultados clave. Además, sólo fue posible aplicar de forma parcial los criterios GRADE enumerados en la sección de métodos; de los cinco criterios clave enumerados, no fue posible evaluar la evidencia sobre la inconsistencia ni sobre el sesgo de publicación debido a la ausencia de un metanálisis y al número muy pequeño de estudios examinados (n = 5). Sin embargo, se aplicaron los criterios GRADE a los aspectos limitaciones de los estudios, imposibilidad para generalizar la evidencia e imprecisión (ver Resumen de los hallazgos, tabla 1; Resumen de los hallazgos, tabla 2; Resumen de los hallazgos, tabla 3; Resumen de los hallazgos, tabla 4; Resumen de los hallazgos, tabla 5; Resumen de los hallazgos, tabla 6). La limitación más grave, así como la razón para la disminución de la certeza de la evidencia entre los cinco estudios, estuvo relacionada con el riesgo de sesgo y la imprecisión de los estudios. Por lo tanto, es probable que estudios de investigación adicionales tengan una marcada repercusión sobre la confianza de las estimaciones del efecto para todos los resultados medidos.
Aspectos como el informe deficiente de los métodos de asignación al azar, la falta de ocultación de la asignación y el cegamiento de la evaluación de resultados, la falta de un análisis de intención de tratar, la deserción y los tamaños de la muestra pequeños significan que no hay evidencia sólida sobre la cual basar el conocimiento y las prácticas en esta área. Se necesitan ECA de alta calidad, con tamaños de la muestra de poder estadístico suficiente para detectar diferencias clínicamente importantes entre los grupos, con una mejor metodología e informe y un contenido y formato de administración más estandarizados que involucren al personal multidisciplinario de asistencia sanitaria. Este tipo de evidencia para respaldar la educación de los profesionales de la asistencia sanitaria y prevenir las úlceras por presión ayudará a dirigir programas efectivos que al final mejorarán la asistencia al enfermo en esta área.
Sesgos potenciales en el proceso de revisión
Esta revisión consideró toda la evidencia que cumplió con los criterios de la revisión. Sólo fue posible tener acceso al informe original completo del estudio James 1998 a partir de sus autores. El informe incluyó datos limitados sobre los resultados secundarios de interés; sin embargo, estuvieron disponibles datos del resultado primario que se incluyeron en la revisión.
Acuerdos y desacuerdos con otros estudios o revisiones
No hay otra revisión sistemática de ECA relacionada con la educación de los profesionales de la asistencia sanitaria para prevenir las úlceras por presión. Para esta revisión se revisaron todos los ECA disponibles hasta la fecha.

Study Flow Diagram
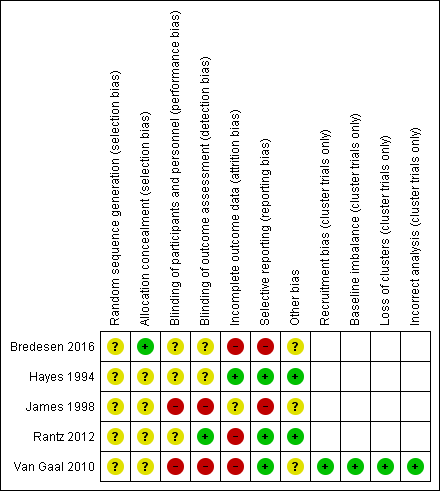
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
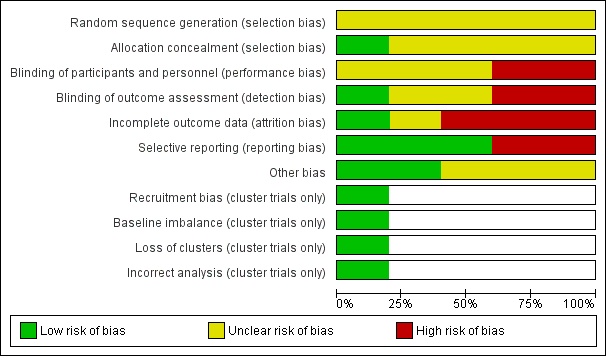
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
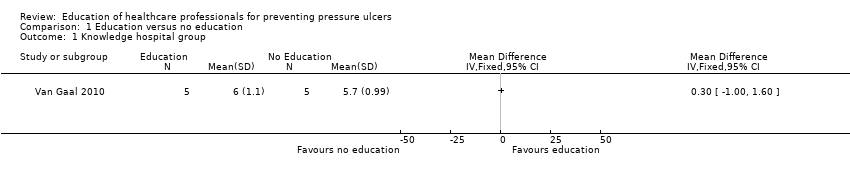
Comparison 1 Education versus no education, Outcome 1 Knowledge hospital group.

Comparison 1 Education versus no education, Outcome 2 Knowledge nursing‐home group.
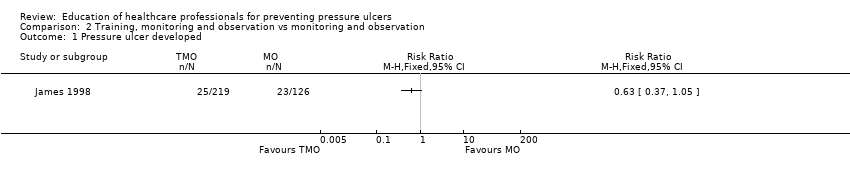
Comparison 2 Training, monitoring and observation vs monitoring and observation, Outcome 1 Pressure ulcer developed.
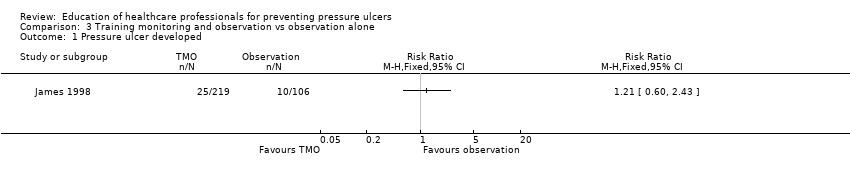
Comparison 3 Training monitoring and observation vs observation alone, Outcome 1 Pressure ulcer developed.
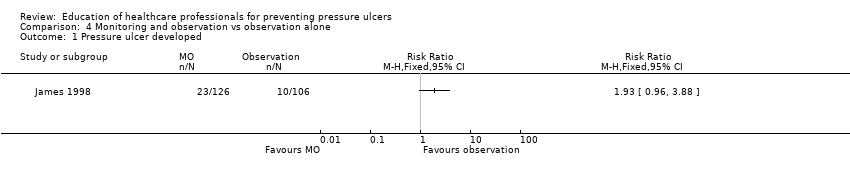
Comparison 4 Monitoring and observation vs observation alone, Outcome 1 Pressure ulcer developed.
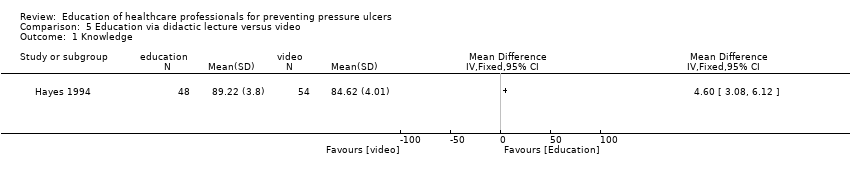
Comparison 5 Education via didactic lecture versus video, Outcome 1 Knowledge.
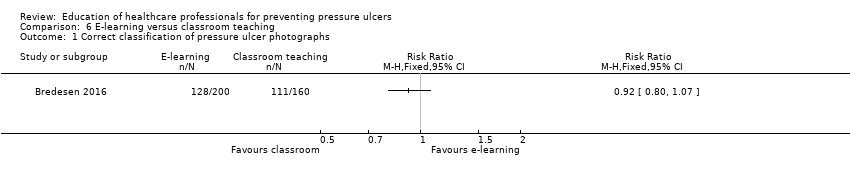
Comparison 6 E‐learning versus classroom teaching, Outcome 1 Correct classification of pressure ulcer photographs.
| Education compared to no education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No education | Education | |||||
| Knowledge in hospital group | Mean knowledge score with no education was 5.7 | Mean knowledge score was 0.30 units higher (1.0 lower to 1.6 higher) | 10 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in health professionals' knowledge depending on whether they receive education or no education on pressure ulcer prevention | |
| Knowledge in nursing‐home group | Mean knowledge score with no education was 5.1 | Mean knowledge score was 0.30 units higher (0.77 lower to 1.37 higher) | 10 | ⊕⊝⊝⊝ | ||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded four times: serious limitations due to performance bias, detection bias and attrition bias; indirectness due to use of a non validated instrument to assess knowledge; serious imprecision due to a wide confidence interval and small sample size. | ||||||
| Training, monitoring and observation compared to monitoring and observation for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Monitoring and observation | Training, monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 0.63 | 345 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with monitoring and observation | |
| 183 per 1000 | 115 per 1000 | |||||
| Severity of new pressure ulcers | No data were presented by the study author | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Training, monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Training monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.21 | 325 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with observation alone | |
| 94 per 1000 | 114 per 1000 | |||||
| Severity of new pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.93 | 232 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as monitoring and observation compared with observation alone | |
| 94 per 1000 | 182 per 1000 | |||||
| Severity of new pressure ulcers | No data are presented by the study author | |||||
| Patient reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitation due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Education versus video for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Comparison: didactic lecture | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Didactic education | Video education | |||||
| Change in health professionals' knowledge | Mean knowledge score with didactic education was 84.62 | Mean knowledge score was 4.60 units higher (3.8 units to 6.12 units higher) | 102 | ⊕⊝⊝⊝ | It is uncertain whether education delivered in different formats such as didactic or video‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitation due to unclear risk of selection, performance and detection bias; very serious imprecision due to small sample size and wide confidence intervals. | ||||||
| E‐learning compared with classroom education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Settings: hospitals and nursing homes Intervention: e‐learning Comparison: classroom education | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Classroom education | E‐learning | |||||
| Knowledge of pressure ulcer classification | Study population | RR 0.92 (0.80 to 1.07) | 18 participants | very low1 | It is uncertain whether education delivered in different formats such as e‐learning or classroom‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| 694 per 1000 | 638 per 1000 | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitations due to high risk of attrition and selective reporting bias; unclear risk of performance, selection, detection and other bias; serious imprecision due to small sample size and wide confidence intervals. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Knowledge hospital group Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Knowledge nursing‐home group Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Knowledge Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Correct classification of pressure ulcer photographs Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

