Formación de los profesionales de la asistencia sanitaria en la prevención de las úlceras por presión
Información
- DOI:
- https://doi.org/10.1002/14651858.CD011620.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 25 mayo 2018see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Heridas
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Alison Porter‐Armstrong: co‐ordinated and developed the review; extracted data; checked the quality of data extraction; analysed and interpreted data; completed the first draft of the review; contributed to writing and editing the review, approved the final version prior to submission; and is a guarantor of the review.
Zena Moore: extracted data, checked the quality of data extraction, analysed and interpreted data; contributed to writing and editing the review; advised on the review; and approved the final version of the review prior to submission.
Ian Bradbury: advised on statistical analysis of the review; and approved the final version of the review prior to submission.
Suzanne McDonough: undertook and checked quality assessment; contributed to writing and editing the review; advised on the review; and approved the final version of the review prior to submission.
Contributions of editorial base:
Julie Bruce (Editor): edited the protocol, advised on methodology, interpretation and protocol content; approved the final protocol prior to publication.
Gill Norman (Editor): edited the review, advised on methodology, interpretation and review content; approved the final review prior to publication.
Gill Rizzello (Managing Editor): co‐ordinated the editorial process; advised on interpretation and content, and edited the review.
Amanda Briant, Reetu Child and Naomi Shaw (Information Specialists): designed the search strategy; edited the search methods section and ran the searches.
Ursula Gonthier (Editorial Assistant): edited the Plain Language Summary and reference section of the review.
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
The HSC Research and Development Division of the Public Health Agency (Northern Ireland), UK.
Cochrane Fellowship Funding Award for Dr Alison Porter‐Armstrong
-
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Wounds. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health, UK.
Declarations of interest
Alison Porter‐Armstrong: received Cochrane Fellowship funding from the HSC Research and Development Division of the Public Health Agency (Northern Ireland) to perform this review.
Zena Moore: received honoraria for speaking at professional meetings for 3M, Molnlycke and Smith & Nephew.
Ian Bradbury: none known.
Suzanne McDonough: none known.
Acknowledgements
The authors would like to acknowledge the assistance of the Cochrane Wounds editorial team and the contribution of peer reviewers Sonya Osborne, Giovanni Casazza, Damian Francis, Victoria Steelman, Ajima Olaghere and Ruth Ropper for their comments on the protocol; and of Andrea Nelson, Zipporah Iheozor‐Ejiofor, Carolina Weller and Janet Gunderson for their feedback on the review. Thanks are also due to copy‐editors Clare Dooley and Denise Mitchell.
Version history
| Published | Title | Stage | Authors | Version |
| 2018 May 25 | Education of healthcare professionals for preventing pressure ulcers | Review | Alison P Porter‐Armstrong, Zena EH Moore, Ian Bradbury, Suzanne McDonough | |
| 2015 Apr 01 | Education of healthcare professionals for preventing pressure ulcers | Protocol | Alison P Porter‐Armstrong, Zena EH Moore, Ian Bradbury, Suzanne McDonough | |
Differences between protocol and review
We planned to compare treatments using the change in knowledge from pre‐treatment values. However, this proved impossible because of the way results were reported in the primary publications, and so we made the post‐hoc decision to report instead differences in post‐treatment levels of knowledge. The protocol did not specify methods for assessing risk of bias in cluster randomised controlled trials. We conducted that assessment using the wounds group template (Appendix 3).
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Humans;
PICO

Study Flow Diagram
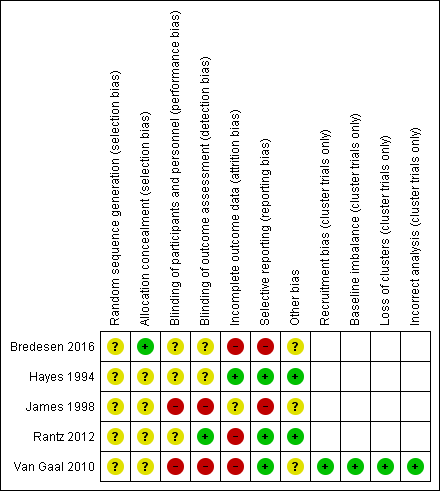
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
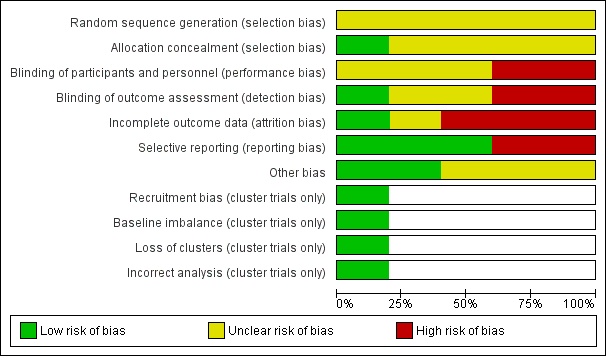
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
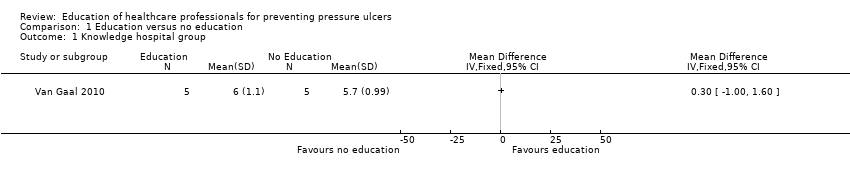
Comparison 1 Education versus no education, Outcome 1 Knowledge hospital group.

Comparison 1 Education versus no education, Outcome 2 Knowledge nursing‐home group.
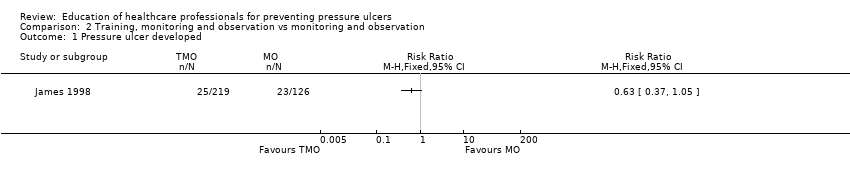
Comparison 2 Training, monitoring and observation vs monitoring and observation, Outcome 1 Pressure ulcer developed.
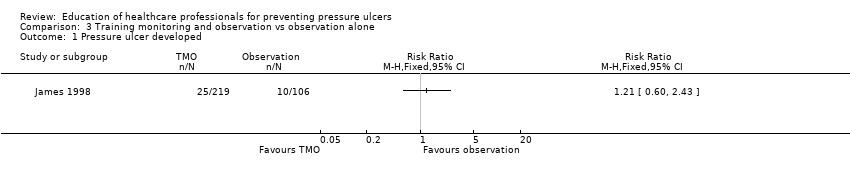
Comparison 3 Training monitoring and observation vs observation alone, Outcome 1 Pressure ulcer developed.
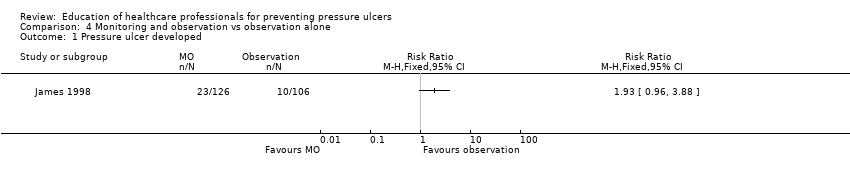
Comparison 4 Monitoring and observation vs observation alone, Outcome 1 Pressure ulcer developed.
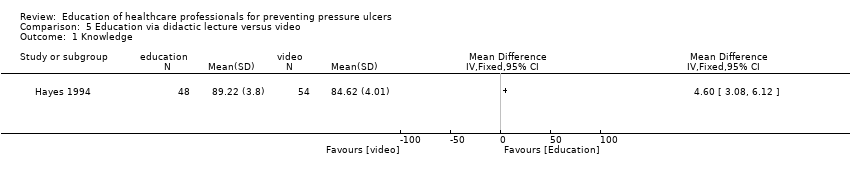
Comparison 5 Education via didactic lecture versus video, Outcome 1 Knowledge.
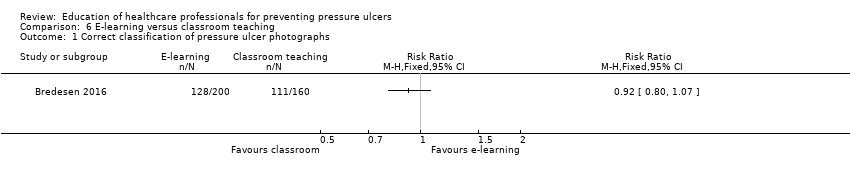
Comparison 6 E‐learning versus classroom teaching, Outcome 1 Correct classification of pressure ulcer photographs.
| Education compared to no education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No education | Education | |||||
| Knowledge in hospital group | Mean knowledge score with no education was 5.7 | Mean knowledge score was 0.30 units higher (1.0 lower to 1.6 higher) | 10 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in health professionals' knowledge depending on whether they receive education or no education on pressure ulcer prevention | |
| Knowledge in nursing‐home group | Mean knowledge score with no education was 5.1 | Mean knowledge score was 0.30 units higher (0.77 lower to 1.37 higher) | 10 | ⊕⊝⊝⊝ | ||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded four times: serious limitations due to performance bias, detection bias and attrition bias; indirectness due to use of a non validated instrument to assess knowledge; serious imprecision due to a wide confidence interval and small sample size. | ||||||
| Training, monitoring and observation compared to monitoring and observation for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Monitoring and observation | Training, monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 0.63 | 345 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with monitoring and observation | |
| 183 per 1000 | 115 per 1000 | |||||
| Severity of new pressure ulcers | No data were presented by the study author | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Training, monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Training monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.21 | 325 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with observation alone | |
| 94 per 1000 | 114 per 1000 | |||||
| Severity of new pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.93 | 232 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as monitoring and observation compared with observation alone | |
| 94 per 1000 | 182 per 1000 | |||||
| Severity of new pressure ulcers | No data are presented by the study author | |||||
| Patient reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitation due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Education versus video for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Comparison: didactic lecture | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Didactic education | Video education | |||||
| Change in health professionals' knowledge | Mean knowledge score with didactic education was 84.62 | Mean knowledge score was 4.60 units higher (3.8 units to 6.12 units higher) | 102 | ⊕⊝⊝⊝ | It is uncertain whether education delivered in different formats such as didactic or video‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitation due to unclear risk of selection, performance and detection bias; very serious imprecision due to small sample size and wide confidence intervals. | ||||||
| E‐learning compared with classroom education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Settings: hospitals and nursing homes Intervention: e‐learning Comparison: classroom education | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Classroom education | E‐learning | |||||
| Knowledge of pressure ulcer classification | Study population | RR 0.92 (0.80 to 1.07) | 18 participants | very low1 | It is uncertain whether education delivered in different formats such as e‐learning or classroom‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| 694 per 1000 | 638 per 1000 | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitations due to high risk of attrition and selective reporting bias; unclear risk of performance, selection, detection and other bias; serious imprecision due to small sample size and wide confidence intervals. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Knowledge hospital group Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Knowledge nursing‐home group Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Knowledge Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Correct classification of pressure ulcer photographs Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

