Education of healthcare professionals for preventing pressure ulcers
Abstract
Background
Pressure ulcers, also known as bed sores or pressure sores, are localised areas of tissue damage arising due to excess pressure and shearing forces. Education of healthcare staff has been recognised as an integral component of pressure ulcer prevention. These educational programmes are directed towards influencing behaviour change on the part of the healthcare professional, to encourage preventative practices with the aim of reducing the incidence of pressure ulcer development.
Objectives
To assess the effects of educational interventions for healthcare professionals on pressure ulcer prevention.
Search methods
In June 2017 we searched the Cochrane Wounds Specialised Register; the Cochrane Central Register of Controlled Trials (CENTRAL); Ovid MEDLINE (including In‐Process & Other Non‐Indexed Citations); Ovid Embase and EBSCO CINAHL Plus. We also searched clinical trials registries for ongoing and unpublished studies, and scanned reference lists of relevant included studies as well as reviews, meta‐analyses and health technology reports to identify additional studies. There were no restrictions with respect to language, date of publication or study setting.
Selection criteria
We included randomised controlled trials (RCTs) and cluster‐RCTs, that evaluated the effect of any educational intervention delivered to healthcare staff in any setting to prevent pressure ulceration.
Data collection and analysis
Two review authors independently assessed titles and abstracts of the studies identified by the search strategy for eligibility. We obtained full versions of potentially relevant studies and two authors independently screened these against the inclusion criteria.
Main results
We identified five studies that met the inclusion criteria for this review: four RCTs and one cluster‐RCT. The study characteristics differed in terms of healthcare settings, the nature of the interventions studied and outcome measures reported. The cluster‐RCT, and two of the RCTs, explored the effectiveness of education delivered to healthcare staff within residential or nursing home settings, or nursing home and hospital wards, compared to no intervention, or usual practices. Educational intervention in one of these studies was embedded within a broader, quality improvement bundle. The other two individually randomised controlled trials explored the effectiveness of educational intervention, delivered in two formats, to nursing staff cohorts.
Due to the heterogeneity of the studies identified, pooling was not appropriate and we have presented a narrative overview. We explored a number of comparisons (1) education versus no education (2) components of educational intervention in a number of combinations and (3) education delivered in different formats. There were three primary outcomes: change in healthcare professionals' knowledge, change in healthcare professionals' clinical behaviour and incidence of new pressure ulcers.
We are uncertain whether there is a difference in health professionals' knowledge depending on whether they receive education or no education on pressure ulcer prevention (hospital group: mean difference (MD) 0.30, 95% confidence interval (CI) ‐1.00 to 1.60; 10 participants; nursing home group: MD 0.30, 95% CI ‐0.77 to 1.37; 10 participants). This was based on very low‐certainty evidence from one study, which we downgraded for serious study limitations, indirectness and imprecision.
We are uncertain whether there is a difference in pressure ulcer incidence with the following comparisons: training, monitoring and observation, versus monitoring and observation (risk ratio (RR) 0.63, 95% CI 0.37 to 1.05; 345 participants); training, monitoring and observation, versus observation alone (RR 1.21, 95% CI 0.60 to 2.43; 325 participants) or, monitoring and observation versus observation alone (RR 1.93, 95% CI 0.96 to 3.88; 232 participants). This was based on very low‐certainty evidence from one study, which we downgraded for very serious study limitations and imprecision. We are uncertain whether multilevel intervention versus attention control makes any difference to pressure ulcer incidence. The report presented insufficient data to enable further interrogation of this outcome.
We are uncertain whether education delivered in different formats such as didactic education versus video‐based education (MD 4.60, 95% CI 3.08 to 6.12; 102 participants) or e‐learning versus classroom education (RR 0.92, 95% CI 0.80 to 1.07; 18 participants), makes any difference to health professionals' knowledge of pressure ulcer prevention. This was based on very low‐certainty evidence from two studies, which we downgraded for serious study limitations and study imprecision.
None of the included studies explored our other primary outcome: change in health professionals' clinical behaviour. Only one study explored the secondary outcomes of interest, namely, pressure ulcer severity and patient and carer reported outcomes (self‐assessed quality of life and functional dependency level respectively). However, this study provided insufficient information to enable our independent assessment of these outcomes within the review.
Authors' conclusions
We are uncertain whether educating healthcare professionals about pressure ulcer prevention makes any difference to pressure ulcer incidence, or to nurses' knowledge of pressure ulcer prevention. This is because the included studies provided very low‐certainty evidence. Therefore, further information is required to clarify the impact of education of healthcare professionals on the prevention of pressure ulcers.
PICOs
Plain language summary
Educating healthcare staff to prevent pressure ulcers
Background
Pressure ulcers, also known as bed sores or pressure sores, are often experienced by those who find it difficult to walk and spend long periods of time sitting or lying down. Pressure ulcers can range from patches of discoloured, painful skin, to open wounds that can take a long time to heal. Pressure ulcers are prone to infection and have a great impact on people's health and well being. To stop these ulcers from developing in people who are at risk, healthcare staff need to be well informed about how to prevent them. It is important to understand what type of information healthcare staff need, how it might best be delivered to them and whether education can prevent pressure ulcers from developing.
Review question
We reviewed the evidence about the effect of the education of healthcare professionals on the prevention of pressure ulcers. We explored all types of education regardless of how it was delivered as long as it focused on preventing pressure ulcers. Healthcare staff included all staff working in pressure ulcer prevention from any professional background. Settings where the care was provided included hospital inpatient and outpatient departments, community clinics, patients' own homes, and residential or nursing care homes.
What we found
In June 2017 we searched for studies evaluating the effect of the education of healthcare professionals on pressure ulcer prevention, and found five relevant studies. Two studies explored the impact of education on the prevention of pressure ulcers. We are uncertain whether education of healthcare professionals makes any difference to the number of new pressure ulcers that develop. This is because the certainty of the evidence within the studies was very low.
Three studies explored the impact of education on staff knowledge of pressure ulcer prevention. The studies compared: education versus no education; components of educational intervention in a number of combinations; and education delivered in different formats. We are uncertain whether education makes any difference to staff knowledge of pressure ulcer prevention, or to the number of new pressure ulcers that develop. This is because the certainty of the evidence within the studies was very low. No study explored the impact of education on the treatment provided by health professionals. Only one study explored the secondary outcomes of interest: pressure ulcer severity, patients' views on their quality of life and carers' views on the patients' ability to carry out daily tasks independently. However, there was not enough information provided within the study to enable our independent assessment of these outcomes.
We examined the certainty of the evidence using the GRADE approach and concluded that all of the evidence was of very low certainty. Therefore we are unable to determine whether education can prevent pressure ulcers. We are also unable to determine whether education affects the knowledge that healthcare staff possess about preventing pressure ulcers.
The evidence of this review is up‐to‐date as of 12 June 2017.
Authors' conclusions
Summary of findings
| Education compared to no education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No education | Education | |||||
| Knowledge in hospital group | Mean knowledge score with no education was 5.7 | Mean knowledge score was 0.30 units higher (1.0 lower to 1.6 higher) | 10 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in health professionals' knowledge depending on whether they receive education or no education on pressure ulcer prevention | |
| Knowledge in nursing‐home group | Mean knowledge score with no education was 5.1 | Mean knowledge score was 0.30 units higher (0.77 lower to 1.37 higher) | 10 | ⊕⊝⊝⊝ | ||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded four times: serious limitations due to performance bias, detection bias and attrition bias; indirectness due to use of a non validated instrument to assess knowledge; serious imprecision due to a wide confidence interval and small sample size. | ||||||
| Training, monitoring and observation compared to monitoring and observation for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Monitoring and observation | Training, monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 0.63 | 345 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with monitoring and observation | |
| 183 per 1000 | 115 per 1000 | |||||
| Severity of new pressure ulcers | No data were presented by the study author | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Training, monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Training monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.21 | 325 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with observation alone | |
| 94 per 1000 | 114 per 1000 | |||||
| Severity of new pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.93 | 232 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as monitoring and observation compared with observation alone | |
| 94 per 1000 | 182 per 1000 | |||||
| Severity of new pressure ulcers | No data are presented by the study author | |||||
| Patient reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitation due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Education versus video for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Comparison: didactic lecture | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Didactic education | Video education | |||||
| Change in health professionals' knowledge | Mean knowledge score with didactic education was 84.62 | Mean knowledge score was 4.60 units higher (3.8 units to 6.12 units higher) | 102 | ⊕⊝⊝⊝ | It is uncertain whether education delivered in different formats such as didactic or video‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitation due to unclear risk of selection, performance and detection bias; very serious imprecision due to small sample size and wide confidence intervals. | ||||||
| E‐learning compared with classroom education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Settings: hospitals and nursing homes Intervention: e‐learning Comparison: classroom education | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Classroom education | E‐learning | |||||
| Knowledge of pressure ulcer classification | Study population | RR 0.92 (0.80 to 1.07) | 18 participants | very low1 | It is uncertain whether education delivered in different formats such as e‐learning or classroom‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| 694 per 1000 | 638 per 1000 | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitations due to high risk of attrition and selective reporting bias; unclear risk of performance, selection, detection and other bias; serious imprecision due to small sample size and wide confidence intervals. | ||||||
Background
Description of the condition
A pressure ulcer (also known as a bed sore, pressure sore, decubitus ulcer or pressure injury) is "a localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear" (NPUAP/EPUAP/PPPIA 2014). A common international pressure ulcer classification exists that categorises pressure ulcers into four categories or stages of injury, ranging from non‐blanching erythema of the skin (tissue redness that does not turn white when pressure is applied) (stage 1) to full‐thickness tissue loss (stage 4), and two other levels of 'unstageable' and 'deep tissue injury' (NPUAP/EPUAP/PPPIA 2014).
A number of risk factors are associated with pressure ulcer development, most recently presented in a theoretical causal pathway and pressure ulcer conceptual framework (Coleman 2014). Recognising that no single factor can explain pressure ulcer susceptibility, factors such as immobility and poor perfusion have been described as direct causal factors, and factors such as moisture, poor sensory perception and nutrition have been described as indirect causal factors. These factors interplay to make some individuals particularly vulnerable or 'at risk' to pressure ulceration, however, the exact mechanisms by which this happens and which factors are of greatest importance remains unknown. Those more 'at risk' of pressure ulceration include individuals who spend prolonged periods of time sitting or lying, wheelchair users, sedentary elderly or those who are immobile (Bates‐Jensen 2009; Gunningberg 2008; Thomas 2010). Pressure ulcers occur due to prolonged unrelieved exposure to externally applied mechanical forces (Gefen 2008). Those who are vulnerable to exposure to this pressure are the immobile, with older people demonstrating the highest propensity to mobility problems (Moore 2011).
Pressure ulceration has a profound impact on the health, rehabilitation, and quality of life of the individuals suffering from them (Anderson 2008; Bates‐Jensen 2009; Ryan 2006; Shapcott 1999). Despite this, the prevalence of pressure ulceration remains unacceptably high, ranging from 9% in Ireland (Moore 2011); 5% to 32% in the UK (Kaltenthaler 2001); 18% in Europe (Vanderwee 2007); and 12.3% in the USA (VanGilder 2009). Pressure ulcers occur in all clinical settings: acute care (mean prevalence of 21%); long‐stay (mean prevalence of 12%); hospices (35.7% prevalence); and community care (prevalence varies from 0.04% to 4%) (Moore 2013). Prevalence of pressure ulcers in an intensive care setting in Australia has been shown to be as high as 50% (Elliott 2008). Such prevalence poses a significant financial impact on healthcare services in treatment and staff costs. International studies have consistently demonstrated the high cost of treating pressure ulceration. It has been estimated that the annual cost of treating pressure ulcers is GBP 1.4 to 2.1 billion in the UK (Bennett 2004); EUR 205 million per annum in Ireland (Gethin 2005); EUR 461 million per annum in Spain (Agreda 2007); AUD 285 million per annum in Australia (Graves 2005); and USD 11 billion in the USA (Reddy 2006). In the USA, the average cost of treating a stage 4 hospital‐acquired pressure ulcer alone, has been reported as being USD 129,248 and a stage 4 community‐acquired pressure ulcer as USD 124,327 (Brem 2010).
Governments have recently adopted more robust positions on the prevention of pressure ulceration, for example, in the UK, pressure ulceration incidence has become a key clinical indicator in ensuring patient safety and infection control (NPSA 2010). The spotlight on pressure ulcers provides a renewed impetus to address the challenges and complexities of pressure ulceration prevention in health and social care services. It is proposed that a focus on preventative healthcare interventions would yield a more efficient use of resources, whilst also minimising the negative health and social consequences experienced by individuals ‘at risk’ of pressure ulceration. For example, in the USA, it has been estimated that treating people with spinal cord injuries and pressure ulceration costs USD 1.2 billion annually, as opposed to prevention, which is estimated to cost one‐tenth of this sum (Byrne 1996). Given that it is thought that the majority of all pressure ulcers are preventable (DoH 2009; Pope 1999), and that prevention costs less than treatment (Stroupe 2011), a focus on preventative measures may be more cost‐effective to health services (Stinson 2013).
Description of the intervention
Education of healthcare staff has been recognised as an integral component of pressure ulcer prevention (Dealey 2007). The Royal College of Nursing (RCN 2001) in their recommendations for clinical practice guidelines on pressure ulcer risk assessment and prevention, considered that education programmes should include a wide range of factors to reflect the multi‐factorial and complex nature of pressure ulceration. Programmes should include information such as: risk factors and the pathophysiology of pressure ulcer development; the limitations and potential applications of risk assessment tools; skin assessment; skin care; selection, use and maintenance of pressure redistributing equipment; methods of documenting risk assessments and prevention activities; positioning to minimise pressure, shear and friction damage (including the correct use of manual handling devices); roles and responsibilities of inter‐disciplinary team members in pressure ulcer management; and patient education and information giving. More recent international guidelines have been developed that broadly group the key components of preventative pressure ulceration care required by all vulnerable individuals (NPUAP/EPUAP/PPPIA 2014). The key components are classified within these guidelines as being fourfold: skin and pressure ulcer risk assessment; nutrition; repositioning; and support surfaces (bed/chair/mattress/cushion). The National Pressure Ulcer Advisory Panel has expanded upon these to develop a competency‐based curriculum for use in pressure ulcer prevention (NPUAP 2013). Similarly, the Surfaces, Keep moving, Incontinence, Nutrition (SKIN) or Surfaces, Skin, Keep moving, Incontinence, Nutrition (SSKIN) care bundles offer a classification that defines and ties together best practice components in preventative pressure ulcer care (HIS 2011). These components routinely form the core aspects upon which educational interventions in pressure ulcer preventative care practices are based (Demarre 2011; Kwong 2011; Thomas 2012; Tweed 2008). However, the effectiveness of such educational programmes, what they optimally comprise, and in what format, are yet to be established.
How the intervention might work
Education is central in developing and maintaining competency, an integral component of the professional code of conduct of all health professionals (NPUAP 2013). Education also provides practitioners with the knowledge and skills needed to make well‐informed clinical decisions. Prevention of pressure ulcers is attainable through the adoption of evidence‐based guidelines and high standards of care NPUAP 2013. However, in order to meet these clinical demands, healthcare professionals require specific skills and knowledge (Beeckman 2008). Educational programmes are ultimately directed towards influencing behavioural change on the part of the recipient. Thus, the underlying premise is that providing education to healthcare professionals may have the potential to enhance their knowledge and skills in pressure ulcer prevention and bring about a positive change in their clinical behaviour.
Why it is important to do this review
Education programmes may help elicit behavioural change by the healthcare professional and so support an overall reduction in the incidence and prevalence of pressure ulcer development. Studies have been conducted that report educational interventions eliciting changes across a range of constructs, such as knowledge of pressure ulcer prevention (Kwong 2011; Thomas 2012; Tweed 2008); pressure ulcer classification (Beeckman 2008); compliance with pressure ulcer clinical guidelines (Demarre 2011); and pressure ulcer risk assessment (Magnan 2008). Education of healthcare professionals in pressure ulcer prevention may, therefore, elicit positive changes in the knowledge and clinical behaviours of those individuals, leading to enhanced compliance with 'best practice' and yielding an overall reduction in prevalence and incidence of pressure ulceration. However, to date there has not been a synthesis of the evidence pertaining to the impact of education of health professionals for preventing pressure ulcers. Reviewing the evidence in order not only to determine whether education programmes for healthcare professionals can help prevent pressure ulceration, but also to understand whether the educational content, mode of delivery, and intensity and duration of input have an effect on outcomes is thus of key importance.
Objectives
To assess the effects of educational interventions for healthcare professionals on pressure ulcer prevention.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and cluster‐RCTs. In the absence of this type of evidence we planned to include non‐randomised controlled trials (NRCTs), controlled before‐after (CBA) studies and interrupted‐time‐series (ITS) studies. We excluded all other types of studies. We did not place any restrictions upon language or date of publication.
Types of participants
All healthcare staff involved in frontline pressure ulcer prevention, including medical and nursing staff, allied health professionals and healthcare assistants, based in all healthcare settings including hospital inpatients and outpatients, community‐based clinics and domiciliary home care, delivering regular care to any patient group deemed 'at risk' of pressure ulceration. We excluded papers reporting upon educational interventions imparted to groups of students in any of these professions or settings.
Types of interventions
We considered all educational programmes aimed at improving clinician knowledge, changing clinical behaviour and reducing pressure ulcer incidence. These may have taken the form of direct teaching, online teaching, blended learning, workshops, short courses (series or stand alone), written educational materials, or self‐directed education. We included studies describing any of the following:
-
educational intervention compared with no intervention or usual practice;
-
comparisons between different components of educational intervention;
-
comparisons between different formats of educational intervention (e.g. face‐to‐face training, webinars, e‐learning).
Types of outcome measures
Primary outcomes
-
Change in healthcare professionals' knowledge (pre‐ and post‐test assessment following intervention, as defined by each study).
-
Change in healthcare professionals' clinical behaviour, as defined by each study (e.g. performing routine skin inspections, enhanced repositioning or mobilisation schedules, changing sitting or lying surfaces, educating patients on skin care, instruction in pressure relief manoeuvres and transfers).
-
Incidence of new pressure ulcers (as reported by each study using numerical counts, or percentages of patients developing any pressure ulcer of any stage).
Secondary outcomes
-
Severity of new pressure ulcers (as reported by each study e.g. using International Pressure Ulcer Classification Scale (NPUAP/EPUAP/PPPIA 2014).
-
Patient‐reported outcomes, as defined by each study using validated outcome measures (decreased pain e.g. McGill Pain Questionnaire, Melzack 1975); (quality of life e.g. Euroqol, EQ‐5D, Oemar 2013).
-
Carer‐reported outcomes (enhanced independence e.g. Barthel Self Care Index, Mahoney 1965).
Search methods for identification of studies
Electronic searches
We searched the following electronic databases to identify reports of RCTs and cluster‐RCTs:
-
Cochrane Wounds Specialised Register (searched 12 June 2017);
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 5) in the Cochrane Library (searched 12 June 2017);
-
Ovid MEDLINE including In‐Process & Other Non‐Indexed citations (1946 to 12 June 2017);
-
Ovid Embase (1974 to 12 June 2017);
-
EBSCO CINAHL Plus (1937 to 12 June 2017).
The search strategies for the Cochrane Wounds Specialised Register, CENTRAL, Ovid MEDLINE, Ovid Embase and EBSCO CINAHL Plus can be found in Appendix 1. We combined the Ovid MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (2008 revision) (Lefebvre 2011). We combined the Embase search with the Ovid Embase filter developed by the UK Cochrane Centre (Lefebvre 2011). We combined the CINAHL Plus searches with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN 2018). There were no restrictions with respect to language, date of publication or study setting.
We also searched the following clinical trials registries:
-
ClinicalTrials.gov (www.clinicaltrials.gov/) (searched February 2018);
-
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/Default.aspx) (searched February 2018);
-
EU Clinical Trials Register (www.clinicaltrialsregister.eu/ctr‐search/search) (searched February 2018).
Search strategies for clinical trials registries can be found in Appendix 1.
Searching other resources
We searched the bibliographies of all included trials identified by the above strategies for further relevant studies.
Data collection and analysis
We carried out data collection and analysis according to methods stated in a published protocol (Porter‐Armstrong 2015).
Selection of studies
Cochrane Wounds' Information Specialist ran the electronic searches. Two review authors (APA, ZM) independently screened all titles and abstracts retrieved by the searches and excluded those that did not meet the inclusion criteria given above. If no abstract was available, we obtained the full paper and assessed it. Two review authors (APA, ZM) retrieved and assessed for eligibility the full texts of all trials classified as relevant. Disagreement between review authors was resolved by consensus, or third party adjudication (SMcD). All full papers retrieved, but subsequently excluded, are disclosed in the Characteristics of excluded studies table, with full reasons given. A PRISMA flowchart of the data management phase of the review is shown in Figure 1 (Liberati 2009).

Study Flow Diagram
Data extraction and management
We modified the data extraction forms developed by the Effective Practice and Organisation of Care Group (EPOC 2018) and used them to extract the data from the selected studies. Two review authors (APA, ZM) independently extracted the data. We piloted the data extraction forms with a small number of studies to ensure that the correct type and level of information was being recorded. We extracted data on:
-
author, title and source;
-
date of study, country of origin;
-
study design type and details;
-
inclusion and exclusion criteria;
-
details about the intervention (e.g. format of delivery, composition of programme, length of programme, setting);
-
participant characteristics (e.g. number, education, professional training, professional background, practice setting);
-
trial quality (e.g. allocation method, outcome assessment, completeness of reporting);
-
all primary and secondary outcomes;
-
statistical analysis used;
-
outcomes data for primary and secondary outcomes;
-
funding source;
-
conflicts of interest.
We resolved any differences in opinion between the two review authors by consensus. Where necessary, we made contact with trial authors for clarification of study characteristics and data.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the following criteria and resolved any disagreements through consensus.
For all included studies we used the Cochrane tool for assessing risk of bias (Higgins 2011a). This tool addresses six specific domains, namely sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other issues (e.g. extreme baseline imbalance), see Appendix 2 for details of criteria on which we based judgements. For trials using cluster randomisation, we specifically considered recruitment bias, baseline imbalance, loss of clusters, incorrect analysis and comparability with individually randomised trials (Appendix 3). We assessed blinding and completeness of outcome data separately for each outcome. We completed a 'Risk of bias' table for each eligible study. We present assessment of risk of bias using a 'Risk of bias' summary figure (Figure 2), which presents all of the judgements in a cross‐tabulation of study by entry. This display of internal validity indicates the weight the reader may give the results of each study.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
For controlled before‐after (CBA) studies and interrupted‐time‐series (ITS) studies we planned to use the 'Risk of bias' tool from the Cochrane EPOC group (EPOC 2013) to assess risk based upon (where appropriate to study design) allocation sequence; allocation concealment; similarity of outcome measurement; similarity of baseline characteristics; incomplete outcome data; allocation blinding; contamination; selective reporting; and other bias.
Where information on risk of bias related to unpublished data or correspondence with a trial author, we planned to note this in the 'Risk of bias' table.
Measures of treatment effect
Dichotomous data
For dichotomous data, we made 2 x 2 contingency tables for each study, showing the number of participants with each outcome event and calculated risk ratios (RRs) with 95% confidence intervals (CIs).
Continuous data
We analysed continuous data if means and standard deviations were available, on the scale chosen in the original publication. For continuous outcomes measured identically across studies, we calculated an overall mean difference (MD) and 95% CI. If only median and interquartile ranges were presented, we converted these to estimated mean and variance, assuming normality. Otherwise, we calculated standardised mean difference (SMD) and 95% CI (Higgins 2011b).
Ordinal data
We planned to analyse ordinal (ordered categorical) data depending on the data presented in the original reports. If sufficient data were available from individual reports, we planned to analyse the data as ordinal data using proportional odds regression.
Unit of analysis issues
Cluster‐RCTs
If cluster‐RCTs had been included in the meta‐analysis, we planned to first seek evidence in the publication that the authors made appropriate adjustments in their analysis to account for the clustering of data. In doubtful cases, we planned to contact the trial authors. If the error estimate had not been corrected, and necessary data were available to allow this, we planned to attempt to make the correction – if necessary using intraclass correlation coefficient estimates from other published studies. However, because there was only one cluster trial (Van Gaal 2010) we were unable to undertake meta‐analysis. Therefore, we reported results for the outcomes of this review without meta analysis.
Multiple trial arms
For studies with multiple intervention groups, we made multiple pair‐wise comparisons between all possible pairs of intervention groups, which were presented as separate analyses.
Interrupted time series studies
If required, and if sufficient data were available in the published study or from the original trial authors, we planned to re analyse results to account for unit of analysis errors in ITS designs.
Dealing with missing data
If summary items such as standard errors were missing from the published report, we contacted the trial authors in order to verify key study characteristics and obtain missing numerical outcome data where possible. If missing data were unobtainable, we planned to present the available‐cases result together with two alternatives; first imputing missing data by the treatment arm mean, and second imputing missing data by the control arm mean. In both cases, we planned to analyse data outside of Review Manager 5 (Review Manager 2014) to allow study weights from the available‐cases analysis to be used in order to avoid inflating the apparent precision of the estimates.
Where the missing data were thought likely to introduce a risk of bias, we noted this in the 'Risk of bias' table and planned to explore the impact of including such studies in the overall assessment of results by a sensitivity analysis.
Assessment of heterogeneity
We planned to use the I² statistic (Higgins 2003) to measure heterogeneity among the trials in each analysis and would have reported our findings for each analysis. If we identified unexplained heterogeneity, that is, Chi² test significant at the level of 0.1, I² greater than 50%, and changes in direction of effect, we planned to first explore clinical explanations for such heterogeneity, for example with important subgroups. If we were unable to explain the heterogeneity clinically, then we planned to use random‐effects analysis or narrative review.
Assessment of reporting biases
We planned to assess reporting bias using Cochrane guidelines (Sterne 2010). If sufficient studies were found (at least 10), we planned to use funnel plots to investigate asymmetry in respect of publication and selective reporting bias and conduct Egger Tests to assess for bias.
Data synthesis
We planned to use Review Manager 5 (Review Manager 2014) to perform meta‐analysis of the included studies separately for continuous, dichotomous and ordinal outcomes, and planned to present the meta‐analysis using forest plots and statistical summaries. We planned to use a fixed‐effect model unless there were clinical or statistical reasons (I² statistic greater than 50%) to suspect significant heterogeneity, in which case we planned to use random‐effects analysis (I²≤ 75%) or narrative review (I² > 75% or clinical heterogeneity).
Subgroup analysis and investigation of heterogeneity
We planned to analyse potential sources of heterogeneity using the following subgroup analyses:
-
type of setting (community, hospital, inpatient, outpatient);
-
type of healthcare professional (medical staff, nursing staff, allied health professional);
-
type of education approach (face‐to‐face, e‐learning, webinars).
Sensitivity analysis
We planned to perform sensitivity analyses to examine how the results of any meta‐analysis would change under the following assumptions:
-
we planned to assess the robustness of results by only including studies assessed as low risk of bias. We planned to exclude trials deemed most susceptible to bias based upon the quality assessment, particularly those with inadequate allocation concealment, uncertain or unblinded outcome assessment, or incomplete outcome data;
-
we planned to explore the effect of inadequate correction for clustering by varying the assumed intracluster correlation coefficient, and by omitting studies whose primary report had apparently failed to correct for clustering;
-
we planned to explore the effect of inadequate correction for auto correlation in ITS studies by omitting studies whose primary report had apparently failed to correct for auto correlation;
-
we planned to assess the effect of missing data by, where possible (a) restricting the analysis to only studies without missing data, and (b) restricting the analysis to complete studies plus those that had attempted to adjust for missing data.
'Summary of findings' tables
We have presented 'Summary of findings' tables for the following primary outcomes: healthcare professionals' knowledge (pre‐ and post‐test assessment following intervention, and comparisons between the control and experimental group post‐test), health professionals' clinical behaviour, and pressure ulcer incidence (proportion of patients developing a new ulcer). We have also included the following secondary outcomes in the 'Summary of findings' tables: severity of new pressure ulcers, patient‐reported outcomes and carer‐reported outcomes. We assessed the quality of the published evidence using the GRADE protocol (Guyatt 2011) against the following five key issues:
-
limitations in the design and implementation of available studies suggesting high likelihood of bias;
-
indirectness of evidence (indirect population, intervention, control, outcomes);
-
unexplained heterogeneity or inconsistency of results (including problems with subgroup analyses);
-
imprecision of results (including wide confidence intervals);
-
high probability of publication bias (Schünemann 2011).
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies.
Results of the search
The search yielded 282 citations. Two review authors examined the abstracts of all the papers, independently, to assess for potential relevance. Of these, we retrieved eleven studies for further assessment and after examination, five studies met the inclusion criteria (Bredesen 2016; Hayes 1994; James 1998; Rantz 2012; Van Gaal 2010); four studies were excluded (Danchaivijitr 1995; Esche 2015; Rantz 2001; Shannon 2012); and two trials were retrieved through searching of trial registers and identified as relevant ongoing studies (IRCT2017080935602N1; NCT02270385), refer to Characteristics of ongoing studies for more details about these trials. See PRISMA flow chart (Figure 1).
Included studies
We have included five studies in this review (Bredesen 2016; Hayes 1994; James 1998; Rantz 2012; Van Gaal 2010). See Characteristics of included studies. Three studies purported to be cluster‐RCTs, conducted in the Netherlands (Van Gaal 2010), the UK (James 1998), and the USA (Rantz 2012); of which only one was truly a cluster‐RCT (Van Gaal 2010), and two were parallel group RCTs (James 1998; Rantz 2012). The other two studies were also parallel‐group RCTs undertaken in the USA (Hayes 1994) and Norway (Bredesen 2016).
Populations
The studies were undertaken in the following settings: two acute care hospitals and four nursing homes in Norway (Bredesen 2016), an urban acute care hospital in the USA (Hayes 1994), 37 residential homes in the UK (James 1998), 58 nursing homes in the USA (Rantz 2012), and 20 hospital and nursing home wards in the Netherlands (Van Gaal 2010).
In Bredesen 2016, Hayes 1994 and Van Gaal 2010, the participants were nursing staff (registered nurses, licensed practical nurses and nursing assistants) and James 1998 described the participants as nursing staff. In Rantz 2012, the participants were owners of facilities, nursing and administrative facility staff, and direct‐care staff. However, the intervention was directed at the leaders of the facilities.
James 1998 and Rantz 2012 did not provide information pertaining to the sample size of the intervention target population. The mean sample size in the remaining three studies (Bredesen 2016; Hayes 1994; Van Gaal 2010) was 327 participants (SD 361; min 44, max 837).
Neither James 1998 nor Rantz 2012 provided data regarding the age or gender distribution of the intervention target participants. In Hayes 1994, the mean age of the participants was 33.3 years (SD 10.3 years, min 20 years, max 69 years), and 81.2% (n = 91) were female. In Van Gaal 2010, the mean age of the participants was 38 years (SD 10.7 years), and 89% (n = 411) were female. Bredesen 2016, provided data on gender distribution only and 97.7% (n = 43) of the participants were female.
Interventions
Bredesen 2016 randomly assigned nurses to one of two groups. Each participant in the e‐learning group completed an individual, computer‐based training module on pressure ulcer risk assessment and classification. The classroom group received the same training module content on pressure ulcer risk assessment and classification, delivered through a 45‐minute lecture format by an experienced nurse using a PowerPoint presentation. Similarly, Hayes 1994 randomly assigned nurses to one of two groups. The intervention group received a 40‐minute instructional educational session, based on pressure ulcer prevention and treatment information, and the control group viewed a 25‐minute video on general skin care for hospitalised patients.
In James 1998, there were three study groups, and nursing homes were randomised to one of the three groups. Although termed as a cluster randomised trial, this was a parallel RCT with the outcomes of interest at a nursing home level, rather than at the level of the individual patient, and nursing homes were the unit of randomisation.The intervention group received three elements: training, monitoring and observation. Training comprised a two‐hour, interactive educational session delivered by a district nurse covering pressure ulcer risk assessment, grading and preventative strategies including nutrition, continence, mobility, and moving and handling. Monitoring comprised a district nurse‐led educational session on pressure ulcer risk assessment and grading only. Observation comprised data collection via a point prevalence assessment at baseline, six, 12 and 18 months.
Rantz 2012 was also termed a cluster randomised trial, however similar to James 1998, this was a parallel RCT as the outcomes were measured at the nursing home level and the unit of randomisation was the nursing homes. Outcomes were compared between the control or intervention groups of the study. The multilevel intervention targeted three levels of staff responsible for operating a nursing facility: owners, nursing and administrative facility staff, and direct‐care staff. Owners were asked, at least for the duration of the study, to (1) provide consistent nursing and administrative leadership, (2) adopt the elements of change (EC) into their management practices, and to actively support and encourage (3) the use of team and group processes for decision‐making affecting resident care, (4) the use of a quality‐improvement programme and (5) the efforts of staff to focus on performing the basics of care, including ambulation, nutrition and hydration, toileting, bowel regularity, preventing skin breakdown and managing pain. The trial investigators provided a detailed intervention manual and two text books to the leaders of each intervention facility. The research nurse observed direct‐care staff at work and then met with them and nursing administrative staff in quality‐improvement teams. These groups tailored care systems and practices outlined in the intervention manual to fit their situation, anchoring them into their facility's care routines.
Van Gaal 2010 used cluster randomisation to allocate five hospital wards and five nursing home wards to the intervention group, and five hospital wards and five nursing home wards to the control group. The intervention consisted of small‐scale, educational meetings, educational materials and outreach visits, delivered to all nurses in the participating wards in the intervention group. Outcomes were measured at the individual patient level.
Comparisons
The control group in the original protocol of Bredesen 2016 were to receive no additional education. However, due to "massive dropout" (p 192) this control group was excluded from the study and was not reported upon. The control group in Hayes 1994 received monthly, videotaped, in‐service training and reading materials about aging and physical assessment of elderly residents, topics that were not directly related to quality‐improvement strategies.
James 1998 used two control groups, one of monitoring and observation, and one of observation only, as the comparators. Monitoring comprised a district nurse‐led educational session on pressure ulcer risk assessment and grading only. Observation comprised data collection via a point prevalence assessment at baseline, six, 12 and 18 months.
The control group in Rantz 2012 received a monthly mailing of general educational material pertaining to elderly care, alongside a monthly telephone call from the co‐investigator to answer any questions relating to the materials, whereas the Van Gaal 2010 control group received no intervention at all.
Outcomes
All studies reported at least one of the primary outcomes of interest for this review. However, these outcomes varied across all five studies and included pressure ulcer development (Rantz 2012); pressure ulcer development, functional dependency and self‐reported quality of life (James 1998); and knowledge of pressure ulcer risk, classification, assessment and treatment (Bredesen 2016; Hayes 1994; Van Gaal 2010).
Excluded studies
We excluded four studies from this review: two studies because they were not RCT design (Danchaivijitr 1995; Esche 2015), one because the study purpose was different from the focus of this review (Rantz 2001), and the other as trial participants in both groups received the educational intervention before the study began (Shannon 2012). See Characteristics of excluded studies.
Risk of bias in included studies
All five studies were at high or unclear risk of bias. We have presented details in separate 'Risk of bias' tables for each of the five studies (see Characteristics of included studies) and in a summary table and graph (Figure 2; Figure 3). As no meta‐analyses were performed, the one cluster randomised controlled trial was assessed against the first 4 of the 5 additional risk of bias criteria for cluster trials (Appendix 3).
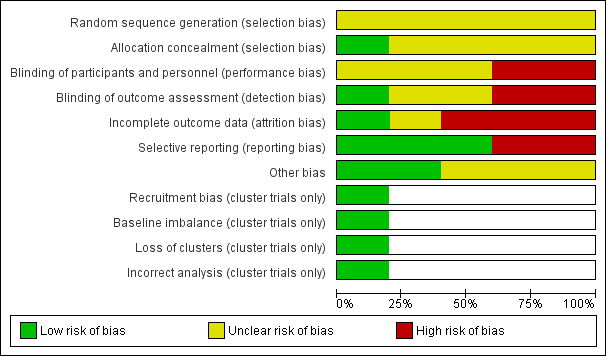
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Allocation
All five studies reported methods of randomisation. In Bredesen 2016, the principal investigator assigned participants using block randomisation to the e‐learning or classroom‐based group. Similarly in Hayes 1994, one of the investigators assigned participants randomly to the experimental or control group. In James 1998, allocation to study group was at the level of the nursing home which was also the unit of analysis. Rantz 2012 randomised owners of nursing homes to either the intervention or control group, then randomly invited individual nursing homes to participate and if they agreed, assigned them to the group designation based upon the owner; again the nursing home was the unit of analysis. Van Gaal 2010 used cluster randomisation, where allocation was by ward, stratified by centre and type of ward.
Allocation concealment was reported in Bredesen 2016 through the use of closed, opaque, numbered envelopes to conceal group allocation. The other four studies did not report allocation concealment.
Blinding
James 1998 disclosed that participating staff were aware of group allocation and we thus judged it to be at high risk for performance bias. Similarily judged as high risk was Van Gaal 2010, as participants would have known their group allocation based upon whether they received the educational intervention or not. It is unclear whether blinding of participants occurred in Bredesen 2016; Hayes 1994 or Rantz 2012.
It is reasonable to assume that blinding of participants and staff would have been difficult to achieve, as it would have been clear which group the participant was in. Nonetheless, blinded outcome assessment would have been possible in terms of pressure ulcer development, functional dependency, self‐reported quality of life and knowledge scores, as these outcomes were gathered using data‐collection instruments, which could have been anonymised regarding study allocation.
Blinding of outcome assessment was reported in only one study (Rantz 2012). One study reported that they did not undertake blinded outcome assessment (James 1998). We judged Van Gaal 2010 to be at high risk as, at each ward, one nurse was responsible for the distribution and collection of the questionnaires, so we judged it likely that this nurse knew group allocation. Blinding of outcome assessment was not reported in Bredesen 2016 or Hayes 1994 and we thus judged them to be at unclear risk of bias.
Incomplete outcome data
We judged Van Gaal 2010 to be at high risk of attrition bias, as the actual attrition rates in the study were judged to be higher than acceptable. In the pre‐intervention phase, the response rates for the questionnaires were: 80% intervention group and 72% control (hospital wards), and 66% intervention group and 71% control (nursing home wards). In the postintervention phase, the response rates for the questionnaires were: 49% intervention group and 87% control (hospital wards), and 58% intervention group and 56% control (nursing home wards). In Rantz 2012, there was also a dropout rate for response to the survey employed (intervention group 71% baseline and 63% study end; control group 65% baseline; 53% study end), thus we judged it to be at high risk of attrition bias. Similarily, we also judged Bredesen 2016 to be at high risk of attrition bias, with an overall drop out rate of 59% at the three‐month, postintervention phase (e‐learning group 52% baseline and 23% study end; classroom group 48% baseline and 18% study end). We judged James 1998 as unclear as there was insufficient information provided to make a full assessment. Only Hayes 1994 was judged to be at low risk of attrition bias.
Selective reporting
We judged Bredesen 2016 at high risk of selective reporting bias as the study authors excluded the original control group comprising no additional education from the study report due to dropout and only reported on the two active education arms of the study. Further, whilst the study protocol stated that they had planned a 24‐week measurement, they did not report it. Another study did not report all the outcomes described in the methods section in sufficient detail to allow full interrogation of the data, therefore we have scored this accordingly, at high risk of bias (James 1998). The other three studies (Hayes 1994; Rantz 2012; Van Gaal 2010) reported on all the outcomes measured and therefore we judged them to be at low risk of reporting bias.
Other potential sources of bias
No other potential sources of bias were apparent from two of the studies (Hayes 1994; Rantz 2012). Participants in Bredesen 2016 were not asked about their computer proficiency in using an e‐learning platform to access training and thus, as a potential source of bias, we assessed it as unclear. James 1998 provided limited information pertaining to the characteristics of the nursing staff participants and thus, as a potential source of bias, we assessed it as unclear. Van Gaal 2010 used a non‐standardised outcome measure to gather data and thus, as a potential source of bias, we assessed it as unclear.
Effects of interventions
See: Summary of findings for the main comparison Education compared to no education for preventing pressure ulcers; Summary of findings 2 Training, monitoring and observation compared to monitoring and observation for preventing pressure ulcers; Summary of findings 3 Training, monitoring and observation compared to observation alone for preventing pressure ulcers; Summary of findings 4 Monitoring and observation compared to observation alone for preventing pressure ulcers; Summary of findings 5 Didactic education versus video education for preventing pressure ulcers; Summary of findings 6 E‐learning versus classroom education for preventing pressure ulcers
Comparison 1. Education versus no education (1 trial, 20 wards from 4 hospitals and 6 nursing homes)
Primary outcome
Changes in health professionals' knowledge
One study (Van Gaal 2010) reported the primary outcome: change in healthcare professionals' knowledge.
Van Gaal 2010 evaluated change in nurses' knowledge using a 20‐item pressure ulcer knowledge test developed for the study, at baseline and one year post baseline. Due to differences in nurses' characteristics between hospitals and nursing homes, the study authors analysed the data for hospital wards and nursing home wards separately. The study authors did not undertake any analysis for the effect of clustering. We have reported the data from the study as further analysis was not possible. We classed this study at high risk of bias, since the 95% CIs would be narrower than they would have been had the correct analysis been undertaken. It is unclear whether education versus no education makes any difference to health professionals' knowledge, as we assessed the certainty of the evidence as very low (downgraded twice for serious limitations due to performance bias, detection bias and attrition bias, and downgraded twice for indirectness due to use of a non validated instrument to assess knowledge, and imprecision due to a wide confidence interval) see summary of findings Table for the main comparison. The mean knowledge score for the hospital participants was 6 (SD: 1.1) for the education group and 5.7 (SD: 0.99) for the no‐education group (MD 0.30, 95% CI ‐1.00 to 1.60; 10 participants; Analysis 1.1). The mean post‐test knowledge score for the nursing home participants was 5.4 (SD: 0.96) for the education group and 5.1 (SD: 0.76) for the no‐education group (MD 0.30, 95% CI ‐0.77 to 1.37; 10 participants; Analysis 1.2) (pre‐test knowledge scores were 5.0 (0.84) and 4.8 (0.78) respectively).
Changes in health professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
Not reported
Secondary outcomes
Severity of new pressure ulcers
Not reported
Patient‐reported outcomes
Not reported
Carer‐reported outcomes
Not reported
Comparison 2. Comparisons between different components of educational intervention: training, monitoring and observation versus monitoring and observation (1 trial, 37 residential homes with 345 residents)
Primary outcomes
Change in health professionals' knowledge
Not reported
Change in health professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
One study (James 1998) reported the primary outcome: incidence of pressure ulcers.
James 1998 used the Norton scale (Norton 1975) and research nurse skin assessments at baseline, 6, 12 and 18 months, to calculate incidence of pressure ulcers. It is unclear whether training, monitoring and observation versus monitoring and observation makes any difference to pressure ulcer incidence, as we assessed the certainty of the evidence as very low (downgraded twice for serious limitations due to performance bias, detection bias and outcome reporting bias, and downgraded once for imprecision due to a wide confidence interval) see summary of findings Table 2. In the training, monitoring and observation group, 11.4% of patients (25/219) developed a pressure ulcer during the study period, whereas in the monitoring and observation group 18% of patients (23/125) developed a pressure ulcer during the study period (RR 0.63, 95% CI 0.37 to 1.05; 345 participants; Analysis 2.1).
Secondary outcomes
James 1998 measured the following secondary outcomes.
Severity of new pressure ulcers
James 1998 measured severity of pressure sores using the David classification of pressure sore severity (David 1983), a four‐stage grading system, used weekly by the staff and recorded by the research nurse assessor at baseline, 6, 12 and 18 months. The study report did not present any data on this outcome to enable further evaluation.
Patient‐reported outcomes
James 1998 used Euroqol (Oemar 2013) to measure the self‐assessed quality of life of the residents at all four time points and reported no differences in scores between the groups of residents during the 18‐month study period. The report presented insufficient data to enable further interrogation of this outcome.
Carer‐reported outcomes
James 1998 used the Bathel Index (Mahoney 1965) to measure the functional dependency level of the residents at all four time points throughout the study. The trial author reported no differences, but there were insufficient data within the report to further interrogate this outcome.
Comparison 3. Comparisons between different components of educational intervention: training, monitoring and observation versus observation alone (1 trial, 37 residential homes with 325 residents)
Primary outcomes
Change in health professionals' knowledge
Not reported
Change in health professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
One study (James 1998) reported the primary outcome: incidence of pressure ulcers.
James 1998 used the Norton scale (Norton 1975) and research nurse skin assessments at baseline, 6, 12 and 18 months, to calculate incidence of pressure ulcers. It is unclear whether training, monitoring and observation versus observation alone makes any difference to pressure ulcer incidence, as we assessed the certainty of the evidence as very low (downgraded twice for serious limitations due to performance bias, detection bias and outcome reporting bias, and downgraded once for imprecision due to a wide confidence interval) see summary of findings Table 3. In the training, monitoring and observation group 11.4% of patients (25/219) developed a pressure ulcer during the study period, whereas in the observation group 10% of patients (10/106) developed a pressure ulcer during the study period (RR 1.21, 95% CI 0.60 to 2.43; 325 participants); Analysis 3.1).
Secondary outcomes
James 1998 measured the following secondary outcomes.
Severity of new pressure ulcers
James 1998 measured severity of pressure ulcers using the David classification of pressure sore severity (David 1983), a four‐stage grading system, used weekly by the staff and recorded by the research nurse assessor at baseline, 6, 12 and 18 months. The study report did not present any data on this outcome to enable further evaluation.
Patient‐reported outcomes
James 1998 used Euroqol (Oemar 2013) to measure the self‐assessed quality of life of the residents at all four time points and reported no differences in scores between the groups of residents during the 18‐month study period. The report presented insufficient data to enable further interrogation of this outcome.
Carer‐reported outcomes
James 1998 used the Bathel Index (Mahoney 1965) to measure the functional dependency level of the residents at all four time points throughout the study. The trial author reported no differences, but the report presented insufficient data to further interrogate this outcome.
Comparison 4. Comparisons between different components of educational intervention: monitoring and observation versus observation alone (1 trial, 37 residential homes with 232 residents)
Primary outcomes
Change in health professionals' knowledge
Not reported
Change in health professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
One study (James 1998) reported the primary outcome: incidence of pressure ulcers.
James 1998 used the Norton scale (Norton 1975) and research nurse skin assessments at baseline, 6, 12 and 18 months, to calculate incidence of pressure ulcers. It is unclear whether monitoring and observation versus observation alone makes any difference to pressure ulcer incidence, as we assessed the certainty of the evidence as very low (downgraded twice for serious limitations due to performance bias, detection bias and outcome reporting bias, and downgraded once for imprecision due to a wide confidence interval) see summary of findings Table 4. In the monitoring and observation group 18% of patients (23/125) developed a pressure ulcer during the study period, whereas in the observation group 10% of patients (10/106) developed a pressure ulcer during the study period (RR 1.93, 95% CI 0.96 to 3.88; 232 participants; Analysis 4.1).
Secondary outcomes
James 1998 measured the following secondary outcomes.
Severity of new pressure ulcers
James 1998 measured severity of pressure ulcers using the David classification of pressure sore severity (David 1983), a four‐stage grading system, used weekly by the staff and recorded by the research nurse assessor at baseline, 6, 12 and 18 months. The study report did not present any data on this outcome to enable further evaluation.
Patient‐reported outcomes
James 1998 used Euroqol (Oemar 2013) to measure the self‐assessed quality of life of the residents at all four time points and reported no differences in scores between the groups of residents during the 18‐month study period. The report presented insufficient data to enable further interrogation of this outcome.
Carer‐reported outcomes
James 1998 used the Bathel Index (Mahoney 1965) to measure the functional dependency level of the residents at all four time points throughout the study. The trial author reported no differences, but the report presented insufficient data to further interrogate this outcome.
Comparison 5. Comparisons between different components of educational intervention: multilevel intervention versus attention control (1 trial, 58 nursing homes)
Primary outcomes
Change in health professionals' knowledge
Not reported
Change in health professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
One study (Rantz 2001) reported the primary outcome: odds of pressure ulcer development.
Rantz 2012 used repeated measures analysis and applied a logistic regression model to calculate the odds ratio of pressure ulcer development between the study groups. The trial authors reported a reduction in pressure ulcer incidence, however, the report presented insufficient data to enable further interrogation of this outcome. Using the GRADE assessment, this was assessed as low certainty evidence (downgraded twice for multiple issues with risk of bias).
Secondary outcomes
Severity of new pressure ulcers
Not reported
Patient‐reported outcomes
Not reported
Carer‐reported outcomes
Not reported
Comparison 6. Comparison between different formats of education: didactic education versus video education (1 trial, 102 participants)
Primary outcome
Change in healthcare professionals' knowledge
One study (Hayes 1994) reported the primary outcome: change in healthcare professionals' knowledge.
Hayes 1994 evaluated changes in nurses' knowledge of pressure ulceration using a 100‐item, true‐false questionnaire developed for the study pre‐ and postintervention, a higher score indicated better knowledge. It is unclear whether education delivered via didactic lecture versus education delivered via video makes any difference to health professionals' knowledge, as we assessed the certainty of the evidence as very low (downgraded once for serious limitations due to unclear risk of selection bias, performance bias and detection bias, and downgraded twice for serious imprecision due to small sample size and a wide confidence interval) see summary of findings Table 5. The mean knowledge score for the didactic lecture group was 84.62 (SD: 4.01) and for the video education group was 89.22 (SD: 3.80); (MD 4.60, 95% CI 3.08 to 6.12; 102 participants; Analysis 5.1).
Change in healthcare professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
Not reported
Secondary outcomes
Severity of new pressure ulcers
Not reported
Patient‐reported outcomes
Not reported
Carer‐reported outcomes
Not reported
Comparison 7. Comparison between different formats of education: education delivered via e‐learning versus classroom education (1 trial, 18 participants)
Primary outcome
Change in healthcare professionals' knowledge
One study (Bredesen 2016) reported the primary outcome: change in healthcare professionals' knowledge.
Bredesen 2016 evaluated changes in nurses' knowledge of pressure ulcer classification, using 40 photos of pressure ulcers representing different categories (normal skin, categories 1 to 4), a higher score indicated better knowledge. It is unclear whether education delivered via e‐learning versus education delivered via the classroom makes any difference to health professionals' knowledge, as we assessed the certainty of the evidence as very low (downgraded twice for serious limitations due to high risk of attrition and selective reporting bias, and unclear risk of selection, performance, detection and other bias, and downgraded once for serious imprecision due to small sample size) see summary of findings Table 6. Participants in the e‐learning group correctly classified 64% of photographs (128/200), participants in the classroom education group correctly classified 69% of photographs (111/160); (RR 0.92, 95% CI 0.80 to 1.07; 18 participants; Analysis 6.1).
Bredesen 2016 also evaluated changes in nurses' knowledge of pressure ulcer risk assessment, using the Braden pressure ulcer risk assessment tool (Bergstrom 1987). No summative scores are provided by the study authors, however, they report that there were no differences found in Braden sub scale scores between the e‐learning group and the classroom group. The report provides insufficient data to further interrogate this outcome.
Change in healthcare professionals' clinical behaviour
Not reported
Incidence of new pressure ulcers
Not reported
Secondary outcomes
Severity of new pressure ulcers
Not reported
Patient‐reported outcomes
Not reported
Carer‐reported outcomes
Not reported
Discussion
Summary of main results
We identified five studies that met the inclusion criteria for this review (Bredesen 2016; Hayes 1994; James 1998; Rantz 2012; Van Gaal 2010). Due to the heterogeneity of the studies identified, pooling was not appropriate and we presented a narrative overview. We explored three key comparisons (1) education versus no education (2) components of educational intervention in a number of combinations and (3) education delivered in different formats.
We are uncertain whether there is a difference in health professionals' knowledge depending on whether they receive education or no education on pressure ulcer prevention. This was based on very low‐certainty evidence from one study, Van Gaal 2010. We downgraded the evidence for serious study limitations, indirectness, and imprecision.
We are uncertain whether there is a difference in pressure ulcer incidence when using different components of educational interventions such as combinations of training, monitoring and observation or multilevel interventions versus control. This is based upon very low‐certainty evidence from two studies (James 1998; Rantz 2012). We downgraded the evidence for serious study limitations and study imprecision.
We are uncertain whether education delivered in different formats such as didactic education and video‐based education or e‐learning and classroom education, makes any difference to health professionals' knowledge of pressure ulcer prevention. This is based upon very low‐certainty evidence from two studies (Bredesen 2016; Hayes 1994). We downgraded the evidence for serious study limitations and study imprecision.
No studies explored our other primary outcome of interest, changes in health professionals' clinical behaviour.
Only one study (James 1998) explored the secondary outcomes of interest, namely; pressure ulcer severity, patient‐reported quality of life and carer‐reported functional dependency level. However, the study provided insufficient information to enable our independent assessment of these outcomes within the review.
Overall these findings reflect the sparseness of the evidence base that exists in this area, and the uncertainty of the existing evidence. In summary, we are unable to determine whether educating healthcare professionals about pressure ulcer prevention makes any difference to pressure ulcer incidence, or to nurses' knowledge of pressure ulcer prevention, or healthcare professionals' clinical behaviour. This is because the studies we included were at unclear, or high risk of bias and GRADE assessment determined that all studies provided very low‐certainty evidence. Therefore, further information is required to clarify the impact of education of healthcare professionals on the prevention of pressure ulcers.
Overall completeness and applicability of evidence
Delivery of education to healthcare professionals to prevent pressure ulcers has only been evaluated in five, small, randomised or cluster‐randomised controlled trials. This resulted in very limited evidence. We were unable to undertake any meta‐analyses or subgroup analyses due to the heterogeneity of the included studies. All five studies investigated a different healthcare setting, from nursing homes (Rantz 2012) and residential homes (James 1998) to hospital‐based wards (Van Gaal 2010) and staff (Bredesen 2016; Hayes 1994). None of the studies used the same outcome measures to assess efficacy. All five studies delivered different formats and educational content. This wide variation in setting, outcome assessment, format and content led to ineligibility of direct comparisons. None of the five studies delivered education to staff from outside a nursing background or nursing role.
The incongruity between targeting an intervention at healthcare staff and measuring outcomes and anticipating changes at patient level (pressure ulcer incidence) must be acknowledged. In addition, in some of the trials, patients were included in the trials regardless of their risk of pressure ulceration. This could explain small or absent effects, as those without risk are not going to benefit from this intervention. One way to address this would be to recruit individuals 'at risk' and then monitor whether the educational intervention changed the risk of developing pressure ulcers. To design appropriately powered studies to explore the effects of healthcare interventions directly on pressure ulcer incidence would require very large clinical populations, potentially resulting in unfeasible and non‐pragmatic trials. Thus, pressure ulcer studies such as those contained within this review select interim or proxy outcomes that may represent a precursor to the development of new pressure ulcers, or provide evidence to support preventative practices in the area, or both.
A further layer of disassociation between the intervention at staff level and the real outcome of interest (pressure ulcer incidence) occurs due to the use of the cluster‐RCT design adopted by one of the five studies in this review. This study randomised groups of healthcare staff based upon the care setting in which the healthcare staff were employed. The care recipients were, by default, recruited to participate in the study by virtue of their care placement and not primarily upon their 'risk' of developing a pressure ulcer. Thus measuring for any intervention effect at patient level using this design is further obscured.
Quality of the evidence
Overall, the evidence was assessed as being of very low certainty for the key outcomes of pressure ulcer incidence and healthcare professionals' knowledge.
Given the heterogeneity of the study outcomes and the inability to pool data, we applied the GRADE criteria to each study individually, as opposed to a combined body of evidence pertaining to key outcomes. Further, we were only able to partially apply the GRADE criteria listed in the methods section; of the five key criteria listed, we could not assess the evidence for inconsistency or for publication bias due to the absence of meta‐analysis and the very small number of studies reviewed (n = 5). However, we did apply the GRADE criteria against the issues of study limitations, indirectness and imprecision (see summary of findings Table for the main comparison; summary of findings Table 2; summary of findings Table 3; summary of findings Table 4; summary of findings Table 5; summary of findings Table 6). The most serious limitation and reason for downgrading the certainty of the evidence across all five studies was risk of bias and study imprecision. Further research is therefore very likely to have an important impact on the confidence of the estimates of effect for these measured outcomes.
Issues such as poor reporting of randomisation methods, absence of allocation concealment and blinded outcome assessment, the lack of intention‐to‐treat analysis, attrition and small sample sizes means that there is no strong evidence upon which to base our knowledge and practices in this area. High‐quality RCTs, with sample sizes of sufficient power to detect clinically important differences between groups with improved methodology and reporting, and a more standardised content and format of delivery involving a multi‐disciplinary healthcare staff are required. This type of evidence to underpin the education of healthcare professionals to prevent pressure ulcers will help to direct effective programmes that will ultimately enhance patient care in this area.
Potential biases in the review process
This review considered all the evidence that met the review criteria. We were only able to access the study by James 1998 from the study authors in original, full‐report form. The report contained limited data on the secondary outcomes of interest, however, data were available for the primary outcome and we included them in the review.
Agreements and disagreements with other studies or reviews
There are no other systematic reviews of RCTs relating to education of healthcare professionals to prevent pressure ulcers. All the available RCTs to date have been scrutinised for this review.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
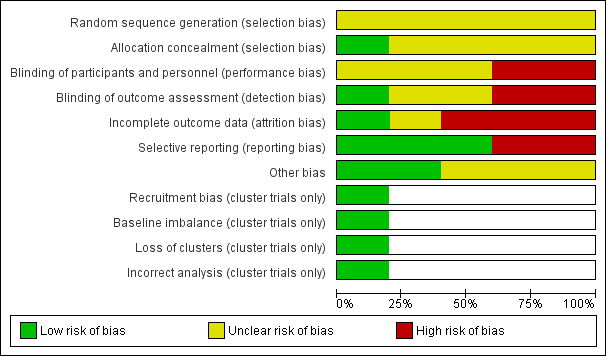
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
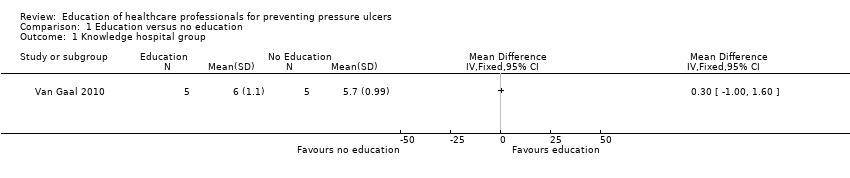
Comparison 1 Education versus no education, Outcome 1 Knowledge hospital group.

Comparison 1 Education versus no education, Outcome 2 Knowledge nursing‐home group.

Comparison 2 Training, monitoring and observation vs monitoring and observation, Outcome 1 Pressure ulcer developed.

Comparison 3 Training monitoring and observation vs observation alone, Outcome 1 Pressure ulcer developed.

Comparison 4 Monitoring and observation vs observation alone, Outcome 1 Pressure ulcer developed.

Comparison 5 Education via didactic lecture versus video, Outcome 1 Knowledge.
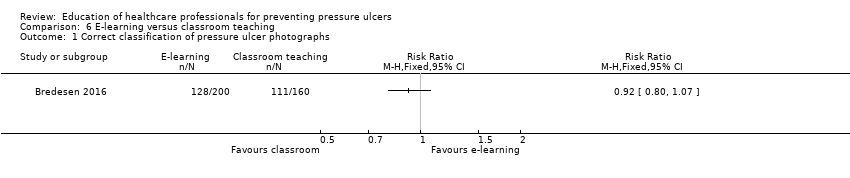
Comparison 6 E‐learning versus classroom teaching, Outcome 1 Correct classification of pressure ulcer photographs.
| Education compared to no education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No education | Education | |||||
| Knowledge in hospital group | Mean knowledge score with no education was 5.7 | Mean knowledge score was 0.30 units higher (1.0 lower to 1.6 higher) | 10 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in health professionals' knowledge depending on whether they receive education or no education on pressure ulcer prevention | |
| Knowledge in nursing‐home group | Mean knowledge score with no education was 5.1 | Mean knowledge score was 0.30 units higher (0.77 lower to 1.37 higher) | 10 | ⊕⊝⊝⊝ | ||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded four times: serious limitations due to performance bias, detection bias and attrition bias; indirectness due to use of a non validated instrument to assess knowledge; serious imprecision due to a wide confidence interval and small sample size. | ||||||
| Training, monitoring and observation compared to monitoring and observation for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Monitoring and observation | Training, monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 0.63 | 345 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with monitoring and observation | |
| 183 per 1000 | 115 per 1000 | |||||
| Severity of new pressure ulcers | No data were presented by the study author | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Training, monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Training monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.21 | 325 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with observation alone | |
| 94 per 1000 | 114 per 1000 | |||||
| Severity of new pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.93 | 232 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as monitoring and observation compared with observation alone | |
| 94 per 1000 | 182 per 1000 | |||||
| Severity of new pressure ulcers | No data are presented by the study author | |||||
| Patient reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitation due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Education versus video for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Comparison: didactic lecture | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Didactic education | Video education | |||||
| Change in health professionals' knowledge | Mean knowledge score with didactic education was 84.62 | Mean knowledge score was 4.60 units higher (3.8 units to 6.12 units higher) | 102 | ⊕⊝⊝⊝ | It is uncertain whether education delivered in different formats such as didactic or video‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitation due to unclear risk of selection, performance and detection bias; very serious imprecision due to small sample size and wide confidence intervals. | ||||||
| E‐learning compared with classroom education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Settings: hospitals and nursing homes Intervention: e‐learning Comparison: classroom education | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Classroom education | E‐learning | |||||
| Knowledge of pressure ulcer classification | Study population | RR 0.92 (0.80 to 1.07) | 18 participants | very low1 | It is uncertain whether education delivered in different formats such as e‐learning or classroom‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| 694 per 1000 | 638 per 1000 | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitations due to high risk of attrition and selective reporting bias; unclear risk of performance, selection, detection and other bias; serious imprecision due to small sample size and wide confidence intervals. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Knowledge hospital group Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Knowledge nursing‐home group Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Knowledge Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Correct classification of pressure ulcer photographs Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

