Physical training for asthma
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised controlled trial with a run‐in period | |
| Participants | 48 asthmatic subjects aged 12 to 17 years performed both a maximal incremental exercise test on a cycle ergometer and 20‐MST. Ten of the subjects were then randomly chosen and trained three times per week at their ventilatory threshold (Vth) intensity level for three months. Another group of ten asthmatic subjects served as control subjects. Training intensity was adjusted monthly. There were twenty asthmatic subjects (10 in the intervention group and 10 in the control group). | |
| Interventions | The training group participated in 36 sessions (3 d/wk for 3 months) of running on an outdoor track. Each session lasted 1 hour during which the children ran for 10min, 3 times, at their own predetermined ventilatory threshold. | |
| Outcomes | VO2max, Vth, HRmax, Wmax, maximum oxygen pulse. | |
| Notes | Lung function testing was done for the whole sample (of all possible 48 subjects) after the run‐in period and before training but not after training. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available |
| Methods | Patients were randomly allocated to either the training or the control group. A six week run‐in period preceded training. | |
| Participants | 36 adults (14 male, 22 female) aged 16‐40 years, with chronic asthma of mild to moderate severity as defined by a requirement for regular prophylactic treatment and reproducible airways obstruction when treatment withdrawn. | |
| Interventions | 30 minute training sessions, 3 times a week for 3 months. | |
| Outcomes | FEV1, VO2max, VEmax, maximum oxygen pulse, HRmax, RR, Vth and VE/VO2max | |
| Notes | The mean number of training sessions undertaken by each patient was 36 (range was 19‐42 sessions). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available |
| Methods | Randomised controlled trial with no run in period. | |
| Participants | 16 male asthmatic children aged 10‐16 years were randomly assigned to a control group (n=7) or a training group (n=9) however two of the training group did not complete the study & results are only presented for the 7 participants in the training group who did complete the study. Nine of the 14 children were taking inhaled steroids. All participants underwent pulmonary function tests and aerobic fitness testing at the start of the study and had acclimatised to altitude (1400m) for at least 1 month. The study took place in a small city in the Pyrenees Mountains. | |
| Interventions | The training group exercised by continuous cycling 3 times weekly for 6 weeks, 45 minutes each session. The target heart rate was individualised and corresponded to the anaerobic threshold level. Training sessions were supervised. | |
| Outcomes | PEFR, FEV1, FVC, FRC, VEmax, HRmax, VO2, Episodes of Wheeze (days), Work capacity W, FRC%, maximal aerobic power, ventilatory reserve, aerobic threshold | |
| Notes | Testing was done blindly regarding the training groups. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available |
| Methods | Randomised controlled trial with no run‐in period. | |
| Participants | 26 asthmatic volunteers aged between 10 and 14 years were selected to participate in the study. The 1962 American Thoracic Society definition of asthma was utilised. 10 of the children formed the training group while the other 16 formed the control group. | |
| Interventions | Warm‐ups (i.e. jogging, callisthenics), followed by running sports (i.e. soccer, netball, volleyball, interval and continuous sprints). Intensity was at 75% of target heart rate. | |
| Outcomes | PEFR, HRmax and VO2max | |
| Notes | Nil | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available |
| Methods | Randomised controlled trial with a run‐in period. | |
| Participants | Media solicitations for asthmatics to volunteer for an experimental breathing study yielded 274 respondents. 150 eliminated, eventually 92 volunteers remained. Of these 67 were randomly allocated to one of three groups. Mean age varied from 28‐33 years. | |
| Interventions | No details provided in published paper, written to author for information. Intensity level not mentioned. | |
| Outcomes | No details provided in published paper, written to author for information, no reply to date. | |
| Notes | We ignored the deep diaphragmatic breathing data and only used the control and physical training data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Investigators unaware as to order of randomisation |
| Methods | Randomised controlled trial with no run in period. | |
| Participants | 45 asthmatic children aged 6‐12 years were randomly assigned to a control group (n=45) matched for age, sex & severity of asthma to a training group (n=45). All participants underwent a pre‐enrolment physical, evaluation of pulmonary function with a peak flow meter every three months, and monitoring of clinical progress. | |
| Interventions | Swimming training conducted 3 times a week for an hour each session over an 8 week period. | |
| Outcomes | Clinical progress was assessed by school absenteeism, emergency room visits, hospitalizations, days requiring daily medications and days of wheezing during a period of 12 months after the swimming sessions. | |
| Notes | A total of 63 children had participated in training sessions but the results presented only include the 45 children who had attended all the sessions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available |
| Methods | Randomised controlled trial with no run in period. | |
| Participants | 16 children with severe asthma diagnosed according to the ATS criteria aged 8‐12 years were randomly assigned to a control group (n=8) or a training group (n=8). No participants were taking oral steroids and other medication was not modified during the study period. The aerobic capacity of each child was determined at the start of the study. An evaluation of exercise induced bronchoconstriction and a histamine challenge test were also conducted. | |
| Interventions | A swimming ergometer was used to assess work rate and corresponding heart rate at 125% of the lactate threshold. The training intensity was set to 125% of the lactate threshold for each participant individually. Training took place for 6 weeks in a heated indoor pool for 2 periods of 15 minutes on 6 days each week. A 10 minute break was taken between the two 15 min training periods. Training intensity was increased as necessary to remain at 125% of the lactate threshold. | |
| Outcomes | Aerobic capacity of the subjects in both training and control groups was assessed again after the training period. Histamine responsiveness was also reassessed. Outcomes include change in work load during cycle test, % fall in FEV1 during swimming & cycle tests, changes in concentrations of histamine required to provoke a fall in FEV1 of 20% or more. | |
| Notes | The mean duration of swimming training was 31.4 days (SD 3.2) and the mean distance swum per day was 851.5m (SD 52.2). The mean total distance achieved during the entire training period was 26,675m (SD 2827.6). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available |
| Methods | Randomised controlled trial. No run‐in period was used. | |
| Participants | 26 asthmatic children aged between 9‐13 years selected for the study from patients attending the pediatric allergy clinics of Charity Hospital. | |
| Interventions | Breathing control swimming, callisthenics, tumbling, parallel bars, rope climbing, abdominal strengthening, wall ladder, running. Three times a week for 2 hours per session, 39 sessions in total. | |
| Outcomes | Wheezy days, FVC, FEV1 and PEFR. | |
| Notes | Attendance at training sessions varied from 22‐39 sessions with an average attendance of 33 sessions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | Randomisation not concealed. |
| Methods | Randomised controlled trial with a run‐in period. | |
| Participants | Children attending the asthma clinic with proven exercise‐induced bronchospasm (>20% fall in PEFR after exercise). Children aged between 7‐14 years in the control group and between 8‐13 years in the exercise group. | |
| Interventions | Warm‐ups, squat thrusts, star jumps, sit‐ups and press‐ups. Exercise loads were increased at each session. Twice a week for 3 months. | |
| Outcomes | Minimum PEFR | |
| Notes | All children were given sodium cromoglycate by Spinhaler, 15 minutes before exercise. Wrote to author to find out the duration of the training, received no reply to date. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available |
| Methods | Randomised controlled trial with no run in period. | |
| Participants | 47 children with asthma aged 8‐13 years were randomly assigned to a control group (n=24) or a training group (n=23). Participants were recruited from an asthma centre (n=9), following an advertisement in a local paper (n=19), and from a special school (n=20). One child in the experimental group dropped out because of a physical problem not related to asthma & was omitted from further analysis. Severity of asthma was diagnosed using the questionnaire of the classification of the Dutch Central Advisory Committee for Peer Review. | |
| Interventions | The 3 month exercise programme consisted of group exercises twice a week for one hour in a gymnasium and one 20‐minute exercise session per week at home. The gym sessions started with 10 minutes warming up, 20 minutes of fitness training then 15‐20minutes different physical activities followed. The training group also received information about asthma and exercise to improve coping behaviour with asthma. Medication was taken before training as prescribed by the child's paediatrician. If wheezing following exercise occurred this was relieved by inhalation of salbutamol. Children in the control group did not receive an extra care or treatment. | |
| Outcomes | A maximum incremental exercise test was used to determine maximum workload, HR, minute ventilation, oxygen uptake, CO2 production and a treadmill endurance test at submaximal heart rate was also taken. A translated version of the Self‐Perception Profile for Children was used to measure perceived competence and the Asthma Coping Test was also administered. Lung function measures (FCV, FEV1, PEF) were recorded and exercise provocation was measured on a treadmill. | |
| Notes | Assessments took place immediately before and after the intervention. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | Information not available |
| Methods | Randomised controlled trial with no run‐in period. Authors update: randomisation was ensured by drawing lots. | |
| Participants | Atopic asthmatic children were divided into 2 groups, control subjects (7) and swimmers (7). All 14 subjects were known to have recurrent reversible wheezing episodes and were required to fulfil at least 3 of the 4: clinical, allergic, immunological or functional (improvement of > 15% in FEV1 after bronchodilator) criteria. | |
| Interventions | Indoor swimming pool training, twice a week for 3 months. Each session lasted for an hour (i.e. 10 minutes on and 10 minutes off). | |
| Outcomes | FEV1 and FVC | |
| Notes | Study had 2 stages and went for 6 months but we only used the first 3 months data, because the second 3 months was specialised high intensity training. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Investigators unaware as to order of randomisation |
| Methods | Randomised controlled trial with no run‐in period. Authors update: randomisation was ensured by drawing lots. | |
| Participants | Subjects included presented a functional improvement of 15% at least in FEV1 by inhaling a bronchodilator. In addition all subjects were required to fulfil: clinical, allergic and immunological criteria. Eighteen asthmatic children (7 boys and 2 girls in each group), mean age was 10.3 for the exercise group and 11.7 for the control group. Authors update: Age range in both groups was 9‐13 years. | |
| Interventions | Indoor swimming pool, individualised training intensity was used during the sessions. Twice a week for 3 months with each session lasting for total 30 minutes for an hour (i.e. 10 minutes on and 10 minutes off). Individualised training intensity used during study for each subject. | |
| Outcomes | VO2max and Vth | |
| Notes | Nil | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Investigators unaware as to order of randomisation |
| Methods | Randomised controlled trial with no run‐in period. | |
| Participants | Subjects were recruited from the Medical College of Georgia Pediatric Pulmonary Allergy/Immunology and General Pediatric clinics. Children included in the study were between 7 and 14 years of age. The study was performed from August 2001 to May 2002. Criteria for inclusion was moderate persistent asthma according to symptom criteria and a need for preventive daily asthma therapy. Exclusion criteria were other comorbidities that would make training unsafe or difficult, asthma therapy changed during trial duration or if an exacerbation occurred during the trial period. Mean baseline values: FEV1 (L) 1.44 (training group), 1.19 (control); FVC (L) 1.84; 1.45; PEFR (L/s) 3.47, 2.89; age 8.4, 7.3. | |
| Interventions | Swimming training according to the child's ability. Lessons were conducted twice per week for 5 to 6 weeks, depending on the time of the year, for 45 minutes each. Lessons were taught by certified swim lesson instructors who were not aware of the child's involvement in the study. Children were excluded from the study if the did not attend at least 80% of the lessons. however, all children assigned to the swim group met this attendance requirement. | |
| Outcomes | FEV1 | |
| Notes | Randomisation was conducted using random number table. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | Investigators unaware as to order of randomisation |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Not an RCT but a CCT (controlled clinical trial with randomisation). | |
| Study does not included physical training using whole body. | |
| Both the groups were trained and the only difference was the intensity of training with no difference in duration or frequency of training. | |
| Study included a composite intervention and included both subjects with asthma and COPD. A physiotherapist run program included breathing retraining, mucus evacuation and exercise. | |
| Not an RCT. | |
| The study was too short, being only for 5 days. | |
| Duration did not meet our minimum. Subjects only exercised once per week . | |
| Follow up analysis where either all groups had physical training or where study was a before & after assessment. Also includes retrospective interview results. | |
| Not an RCT. a review. | |
| All patients had already undergone an 8 week rehabilitation program training prior to being included in the current trial. | |
| Study was not truly randomised. Allocation was based on who lived closer to the gymnasium and this group being included in the exercise training arm. | |
| Health control subjects used, not participants with asthma. | |
| Subjects are said to be randomly choosen but the intervention group of 28 were choosen from a total of 42 because they were inactive in sports and related physical games and had poor physical fitness. Control groups were more physically active than the subjects in the intervention group. | |
| Mentioned as randomised, but all patients who were in hospital were assigned to the control group. Subjects who had severe asthma were assigned to the control group. | |
| Not an RCT. | |
| Not an RCT. | |
| not an RCT, but a long term observational study. | |
| Not an RCT, but a questionnaire based study. | |
| Not an RCT. | |
| Questionnaire based study. | |
| Not an RCT and composite patient group and not able to obtain data for asthma patients only. | |
| Study not randomised, subjects were consecutively allocated to the training and placebo groups, where the first 26 subjects were allocated to the training group and the next 16 to the placebo group. | |
| Not truly randomised, subjects were assigned to groups according to the availability of transport. | |
| Both study groups underwent physical training. One had intermittent training and the other group had aerobic training. | |
| Not an RCT but a CCT. | |
| Not an RCT. | |
| Not an RCT. | |
| Exercise prescription is of too short a duration. | |
| Not an RCT. | |
| Not a truly randomised study. Participants were randomised on the basis of distance from training centre. | |
| Recommendations for sports training in asthma, not a RCT. | |
| Not randomised since the subjects could choose which one of the four groups they would like to be in. | |
| Not an RCT. | |
| Not an RCT, but a before and after study. | |
| Not an RCT. | |
| Not an RCT. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PEFR‐l/min Show forest plot | 4 | 103 | Mean Difference (IV, Fixed, 95% CI) | ‐5.47 [‐27.55, 16.60] |
| Analysis 1.1  Comparison 1 Physical Training vs Control, Outcome 1 PEFR‐l/min. | ||||
| 2 FEV1‐litres Show forest plot | 5 | 129 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.14, 0.16] |
| Analysis 1.2  Comparison 1 Physical Training vs Control, Outcome 2 FEV1‐litres. | ||||
| 3 FVC‐litres Show forest plot | 4 | 93 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.12, 0.30] |
| Analysis 1.3  Comparison 1 Physical Training vs Control, Outcome 3 FVC‐litres. | ||||
| 4 VEmax‐l/min Show forest plot | 4 | 111 | Mean Difference (IV, Fixed, 95% CI) | 6.00 [1.57, 10.43] |
| Analysis 1.4  Comparison 1 Physical Training vs Control, Outcome 4 VEmax‐l/min. | ||||
| 5 HRmax (bpm) Show forest plot | 5 | 121 | Mean Difference (IV, Fixed, 95% CI) | 7.70 [5.57, 9.83] |
| Analysis 1.5  Comparison 1 Physical Training vs Control, Outcome 5 HRmax (bpm). | ||||
| 6 VO2max‐ml/kg/min Show forest plot | 7 | 175 | Mean Difference (IV, Fixed, 95% CI) | 5.43 [4.24, 6.61] |
| Analysis 1.6  Comparison 1 Physical Training vs Control, Outcome 6 VO2max‐ml/kg/min. | ||||
| 7 Episodes of Wheeze (days) Show forest plot | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐7.5 [‐22.42, 7.42] |
| Analysis 1.7  Comparison 1 Physical Training vs Control, Outcome 7 Episodes of Wheeze (days). | ||||
| 8 Work Capacity‐W Show forest plot | 3 | 83 | Mean Difference (IV, Fixed, 95% CI) | 14.95 [11.52, 18.38] |
| Analysis 1.8  Comparison 1 Physical Training vs Control, Outcome 8 Work Capacity‐W. | ||||

Comparison 1 Physical Training vs Control, Outcome 1 PEFR‐l/min.

Comparison 1 Physical Training vs Control, Outcome 2 FEV1‐litres.
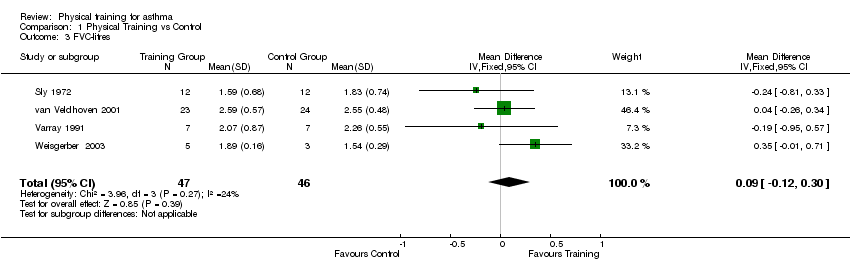
Comparison 1 Physical Training vs Control, Outcome 3 FVC‐litres.

Comparison 1 Physical Training vs Control, Outcome 4 VEmax‐l/min.

Comparison 1 Physical Training vs Control, Outcome 5 HRmax (bpm).
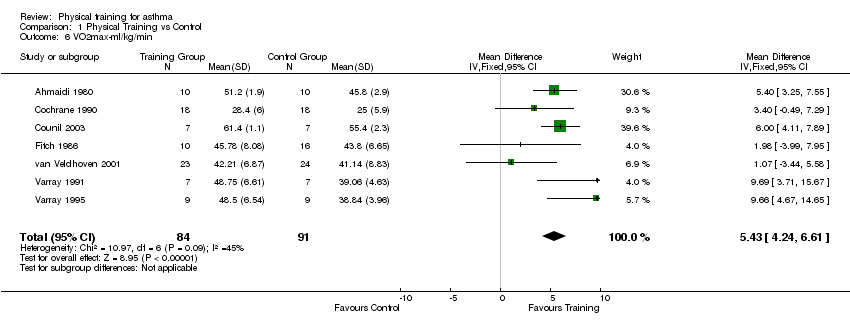
Comparison 1 Physical Training vs Control, Outcome 6 VO2max‐ml/kg/min.
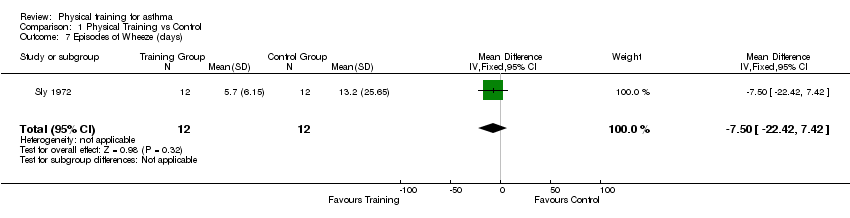
Comparison 1 Physical Training vs Control, Outcome 7 Episodes of Wheeze (days).

Comparison 1 Physical Training vs Control, Outcome 8 Work Capacity‐W.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PEFR‐l/min Show forest plot | 4 | 103 | Mean Difference (IV, Fixed, 95% CI) | ‐5.47 [‐27.55, 16.60] |
| 2 FEV1‐litres Show forest plot | 5 | 129 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.14, 0.16] |
| 3 FVC‐litres Show forest plot | 4 | 93 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.12, 0.30] |
| 4 VEmax‐l/min Show forest plot | 4 | 111 | Mean Difference (IV, Fixed, 95% CI) | 6.00 [1.57, 10.43] |
| 5 HRmax (bpm) Show forest plot | 5 | 121 | Mean Difference (IV, Fixed, 95% CI) | 7.70 [5.57, 9.83] |
| 6 VO2max‐ml/kg/min Show forest plot | 7 | 175 | Mean Difference (IV, Fixed, 95% CI) | 5.43 [4.24, 6.61] |
| 7 Episodes of Wheeze (days) Show forest plot | 1 | 24 | Mean Difference (IV, Fixed, 95% CI) | ‐7.5 [‐22.42, 7.42] |
| 8 Work Capacity‐W Show forest plot | 3 | 83 | Mean Difference (IV, Fixed, 95% CI) | 14.95 [11.52, 18.38] |

