Palliative care interventions for people with multiple sclerosis
Abstract
Background
People with multiple sclerosis (MS) have complex symptoms and different types of needs. These demands include how to manage the burden of physical disability as well as how to organise daily life, restructure social roles in the family and at work, preserve personal identity and community roles, keep self‐sufficiency in personal care, and how to be part of an integrated care network. Palliative care teams are trained to keep open full and competent lines of communication about symptoms and disease progression, advanced care planning, and end‐of‐life issues and wishes. Teams create a treatment plan for the total management of symptoms, supporting people and families on decision‐making. Despite advances in research and the existence of many interventions to reduce disease activity or to slow the progression of MS, this condition remains a life‐limiting disease with symptoms that impact negatively the lives of people with it and their families.
Objectives
To assess the effects (benefits and harms) of palliative care interventions compared to usual care for people with any form of multiple sclerosis: relapsing‐remitting MS (RRMS), secondary‐progressive MS (SPMS), primary‐progressive MS (PPMS), and progressive‐relapsing MS (PRMS) We also aimed to compare the effects of different palliative care interventions.
Search methods
On 31 October 2018, we conducted a literature search in the specialised register of the Cochrane MS and Rare Diseases of the Central Nervous System Review Group, which contains trials from CENTRAL, MEDLINE, Embase, CINAHL, LILACS, Clinical trials.gov and the World Health Organization International Clinical Trials Registry Platform. We also searched PsycINFO, PEDro and Opengrey. We also handsearched relevant journals and screened the reference lists of published reviews. We contacted researchers in palliative care and multiple sclerosis.
Selection criteria
Randomised controlled trials (RCTs) and cluster randomised trials were eligible for inclusion, as well as the first phase of cross‐over trials. We included studies that compared palliative care interventions versus usual care. We also included studies that compared palliative care interventions versus another type of palliative interventions.
Data collection and analysis
We used standard Cochrane methodological procedures. We summarised key results and certainty of evidence in a 'Summary of Finding' table that reported outcomes at six or more months of post‐intervention.
Main results
Three studies (146 participants) met our selection criteria. Two studies compared multidisciplinary, fast‐track palliative care versus multidisciplinary standard care while on a waiting‐list control, and one study compared a multidisciplinary palliative approach versus multidisciplinary standard care at different time points (12, 16, and 24 weeks). Two were RCTs with parallel design (total 94 participants) and one was a cross‐over design (52 participants). The three studies assessed palliative care as a home‐based intervention. One of the three studies included participants with 'neurodegenerative diseases', with MS people being a subset of the randomised population. We assessed the risk of bias of included studies using Cochrane's 'Risk of Bias' tool.
We found no evidence of differences between intervention and control groups in long‐time follow‐up (> six months post‐intervention) for the following outcomes: mean change in health‐related quality of life (SEIQoL ‐ higher scores mean better quality of life; MD 4.80, 95% CI ‐12.32 to 21.92; participants = 62; studies = 1; very low‐certainty evidence), serious adverse events (RR 0.97, 95% CI 0.44 to 2.12; participants = 76; studies = 1, 22 events, low‐certainty evidence) and hospital admission (RR 0.78, 95% CI 0.24 to 2.52; participants = 76; studies = 1, 10 events, low‐certainty evidence).
The three included studies did not assess the following outcomes at long term follow‐up (> six months post intervention): fatigue, anxiety, depression, disability, cognitive function, relapse‐free survival, and sustained progression‐free survival.
We did not find any trial that compared different types of palliative care with each other.
Authors' conclusions
Based on the findings of the RCTs included in this review, we are uncertain whether palliative care interventions are beneficial for people with MS. There is low‐ or very low‐certainty evidence regarding the difference between palliative care interventions versus usual care for long‐term health‐related quality of life, adverse events, and hospital admission in patients with MS. For intermediate‐term follow‐up, we are also uncertain about the effects of palliative care for the outcomes: health‐related quality of life (measured by different assessments: SEIQoL or MSIS), disability, anxiety, and depression.
PICO
Plain language summary
Palliative care interventions for people with multiple sclerosis
Objective
To assess the effects (benefits and harms) of palliative care interventions compared to usual care for people with any form of multiple sclerosis: relapsing‐remitting MS (RRMS), secondary‐progressive MS (SPMS) and primary‐progressive MS (PPMS). We also aimed to compare the effects of different palliative care interventions.
Background
Multiple sclerosis (MS) is a chronic, disabling and progressive condition that affects around 2.3 million people worldwide. The many symptoms of MS create emotional, psychosocial and physical burdens for those affected. Palliative care is defined as the active and total care of pain and psychological, spiritual and social problems of people with a disease that does not respond to curative treatments. Palliative care includes the relief of pain and other stressor symptoms, the promotion of the concept of life and death as something natural, promoting respect for the natural course of death, the integration of psychological and spiritual aspects into patient care, and the preservation of an active life for as long as possible.
Study characteristics
Three studies involving 146 participants were included in this review. All three studies compared palliative care delivered in home visits versus usual care for people with MS. Two studies included only participants with MS. The third study (Ne‐PAL) included participants with MS and other neurodegenerative diseases. In all three studies, interventions focused on assessment and management of symptoms and end‐of‐life planning. We did not find studies that compared different types of palliative care with each other.
Key results
We are uncertain about differences between palliative care versus usual care for the following outcomes assessed at long‐term follow‐up (> six months post‐intervention): change in health‐related quality of life, adverse events and hospital admission. The included studies did not assess fatigue, cognitive function, relapse‐free survival or sustained progression‐free survival.
Quality of the evidence
We are uncertain whether palliative care interventions are beneficial for people with MS. There is low‐ or very low‐certainty evidence regarding the difference between palliative care interventions versus usual care for long‐term health‐related quality of life, adverse events and hospital admission.
Currentness of evidence
This evidence is up‐to‐date as of 31 October 2018.
Authors' conclusions
Summary of findings
| Palliative care compared to usual care (long time) for people with multiple sclerosis | ||||||
| Patient or population: Adults people with multiple sclerosis (including RRMS, SPMS, PPMS, PRMS)1 | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with control group (long time) | Risk with Palliative care | |||||
| Health‐related quality of life Assessed by: SeiQoL‐DW (higher scores mean better quality of life) Follow‐up: long‐term (24 weeks) | The mean change of the SeiQoL score in the control group was ‐4.0 | The mean difference of the SeiQoL score in palliative group was 4.8 higher (‐12.43 lower to 22.03 higher) | 58 | ⊕⊝⊝⊝ | ||
| Serious adverse events Assessed by: number of participants presenting at least one serious adverse event Follow‐up: long‐term (24 weeks) | 269 per 1.000 | 261 per 1.000 | RR 0.97 | 76 | ⊕⊕⊝⊝ LOW 3.4 | |
| Hospital admission Assessed by: number of participants admitted in hospital Follow‐up: long‐term (24 weeks) | 154 per 1.000 | 120 per 1.000 | RR 0.78 | 76 | ⊕⊕⊝⊝ LOW 3,4 | |
| Fatigue ‐ Not reported at long term follow‐up | ||||||
| Disability ‐ Not reported at long term follow‐up | ||||||
| Anxiety ‐ Not reported at long term follow‐up | ||||||
| Depression ‐ Not reported at long term follow‐up | ||||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 RRMS: Relapsing‐remitting Multiple Sclerosis; SPMS: Secondary‐progressive Multiple Sclerosis; PPMS: Primary‐progressive Multiple Sclerosis; PRMS: Progressive‐relapsing Multiple Sclerosis. 2 Downgraded two levels due to risk of bias (unblinded participants and outcome liable to participant subjective judgement and incomplete outcome data). 3 Downgraded one level due to imprecision (low number of participants and wide confidence interval crossing the null). 4 Downgraded one level for risk of selective reporting (2/3 studies did not report health‐related quality of life measured by SeiQoL‐DW at 24 weeks). | ||||||
Background
Description of the condition
Multiple sclerosis (MS) is a chronic, disabling and progressive condition that affects around 2.3 million people worldwide (Browne 2014). The disease is characterised by an autoimmune, inflammatory and demyelinating [when the myelin sheath of the neurons are affected causing problems at the conduction of signs, damaging functions as movement and cognition] process of the brain and spinal cord with progressive loss of neurons [nervous system cells] and axons [part of neurons responsible for the conduction of nerve impulses] (Nylander 2012).
The progressive course of MS and the related functional damage substantially affect a persons' daily activities, autonomy and quality of life. The disease is associated with high emotional, social and physical impacts for people, caregivers and health systems (Chiaravalloti 2008; Fox 2012; Khan 2007; Multiple Sclerosis International Federation 2010).
People are diagnosed with MS when they are in an economically active phase of their lives and are looking for economic self‐sufficiency or need to support their families.
The course of the disease is unpredictable. According to the most recent classification, the following patterns are reported: clinically isolated syndromes (CIS); radiologically isolated syndrome (RIS); relapsing‐remitting MS (RRMS); secondary‐progressive MS (SPMS); and primary‐progressive MS (PPMS) (Lublin 2014).
Description of the intervention
Palliative care is defined as the active care of pain, psychological, spiritual and social problems of people with a disease that does not respond to curative treatments (EAPC 1998). Palliative care aims to improve the quality of life of both patients and families. As it is the combination of several components, it may be defined as a complex intervention (Craig 2008).
The objectives of palliative care include the relief of pain and other stressor symptoms; promotion of the concept of life and death as something natural; promotion of respect for the natural course of death; the integration of psychological and spiritual aspects into patient care; the preservation of an active life for as long as possible; assistance to families in supporting people during the illness and after that; and the improvement of quality of life positively influencing the course of disease and promoting the discussion of advance care planning with the patient and his/her family (Haun 2017; Hui 2013;WHOQOL Group 1998; WHO 2018).
Palliative care can be delivered by a team of multidisciplinary specialists (medical doctors, nurses, social workers, chaplains, physiotherapists, occupational therapists, dentists, psychologists and psychiatrists) or through an approach coordinated by a specialised professional (usually nurses). Palliative care usually takes place in different settings, such as the community, hospitals, hospices, day‐care units, outpatient clinics and the patient's home (Huan 2014).
Palliative care may be divided into three categories: 'early palliative care', palliative care administered early in the beginning of the disease; 'palliative care' focus on symptom management and quality of life; and 'end‐of‐life care', care provided for the terminally ill, when the person is living the last days of life (Haun 2017, NICE 2004, Turner‐Stokes 2008).
How the intervention might work
There is some evidence about the benefits of palliative care for people with cancer (Gomes 2013; Higginson 2003), but there is a lack of evidence for other conditions, such as neurodegenerative diseases [diseases in which the progressive and irreversible destruction of neurons happens gradually affecting motor, physiological and cognitive functions] (Karam 2016; Murphy 2016). We believe that this type of care may have a positive impact on the quality of life for people with MS, regardless of disease activity, although the strategy offered during different periods will vary according to their symptoms and needs. Different strategies may be planned to deal with pain and other symptoms, psychosocial and economic issues, end‐of‐life care planning, and advance directives (Edmonds 2010; Murphy 2016).
People with MS present with complex symptoms (Strupp 2016), giving rise to different types of demands. These demands include how to manage the burden of physical disability as well as how to organise daily life, restructure social roles in family and at work, preserve personal identity and community roles, keep self‐sufficiency in personal care, and how to be part of an integrated care network (Strupp 2016).
Palliative care teams are trained to keep open, full and competent lines of communication about symptoms and disease progression, advanced care planning, and end‐of‐life issues and wishes (Buecken 2012; Strupp 2016).
Taking care of family needs is also a task for palliative care teams. When a MS family member dies, many feelings emerge, including grief and relief: grief about the loss of a loved relative and relief because that family member is no longer suffering (Wollin 2006). The management of families that live with a person suffering from a chronic progressive disease can prevent the development of complicated or anticipatory grief or depression (Lobb 2006; Wittouck 2011).
Why it is important to do this review
Despite research and the development of many interventions aimed at reducing disease activity or slowing the progression of MS, this condition remains life‐threatening with highly damaging symptoms for people with it and their families.
Some primary studies have assessed the effectiveness of palliative care for people with MS (Strupp 2016). A comprehensive synthesis of primary studies of palliative care for people with MS will help health care professionals, patients and families to make informed treatment choices when considering palliative care for MS.
Objectives
To assess the effects (benefits and harms) of palliative care interventions for people with MS types: relapsing‐remitting MS (RRMS), secondary‐progressive MS (SPMS), and primary‐progressive MS (PPMS). We also aim to compare the effects of different palliative care interventions considering delivery settings and categories, i.e. early palliative care, palliative care, or end‐of‐life care.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and cluster randomised trials were eligible for inclusion, as well as the first phase of cross‐over trials. We considered studies reported as full texts, as abstract only, and unpublished reports.
Types of participants
We included adults diagnosed with MS according to the McDonald or Poser criteria (McDonald 2001; Polman 2011; Poser 1983; Thompson 2018). We considered participants with the following forms of MS: relapsing‐remitting MS (RRMS), secondary‐progressive MS (SPMS), primary‐progressive MS (PPMS), and progressive‐relapsing MS (PRMS) (Lublin 2014), regardless of gender, time of diagnosis or degree of functionality.
Types of interventions
We considered for inclusion any type of palliative care intervention, given in any scheme, alone or associated with medications, for any period of time. The primary study had to define the intervention as palliative in order to be included in this review. Possible types of interventions included (but were not limited to): multidisciplinary team work aiming at the management of physical, spiritual and psychosocial symptoms; management on how to live with a life‐threatening disease; and advanced care including the discussion of advanced life support (Murphy 2016).
Palliative care is defined a type of treatment intending to improve the quality of life of patients and families facing a life‐threatening illness, through early identification, prevention and treatment of pain, psychosocial, physical and spiritual suffering. It may help the person to live as functional and independent as possible until death. It should be integrated into countries' health systems and offered early in the beginning of the disease progression. It is usually delivered by a multidisciplinary team and in different levels of care (home‐based, community care and specialist palliative care services) (NICE 2004; WHO 2018).
Comparisons
-
Palliative care interventions versus usual care interventions.
-
Palliative care intervention versus another type of palliative care intervention, considering delivery settings (for example, home‐based versus hospice palliative care interventions).
Types of outcome measures
Primary outcomes
-
Health‐related quality of life.
-
Adverse events.
Secondary outcomes
-
Fatigue.
-
Cognitive function.
-
Disability.
-
Anxiety.
-
Depression.
-
Hospital admission.
-
Relapse‐free survival.
-
Sustained progression‐free survival.
Method and timing of outcome measurement
-
Health‐related quality of life: assessed by the Multiple Sclerosis Quality of Life scale (MSQOL‒54) (Vickrey 1995); the Multiple Sclerosis Quality of Life Inventory (MSQLI) (Fischer 1999); or other validated tools, as the SEIQoL‐DW scale (O'Boyle 1995).
-
Adverse events: number of participants with at least one adverse event, including (but not limited to) complaints by participants, pain, sleep disturbance or any event considered as adverse by the participant.
-
Fatigue: assessed by the Fatigue Severity Scale or the Fatigue Index Scale (Krupp 1989); or any other validated tool.
-
Cognitive function: assessed by any validated tool, including the Multiple Sclerosis Neuropsychological Questionnaire (Benedict 2003); and the Wechsler Adult Intelligence Scale (WAIS, Wechsler 1997).
-
Disability: change in disability as assessed by the Expanded Disability Status Scale (EDSS, Kurtzke 1983).
-
Anxiety and depression as assessed by the subscales of the Delusion‐States‐Symptoms Inventory (Bedford 1978); or any other validated tool.
-
Hospital admission: number of participants experiencing at least one hospital admission.
-
Relapse‐free survival: defined as newly developed or recently worsened symptoms of neurological dysfunction, lasting longer than 24 hours and objectively confirmed. However, we considered less stringent criteria (as defined by the author from the primary study) and we intended to assess these criteria separately.
-
Sustained progression‐free survival: progression was defined as a ≥ 1.0‐point increase in the Expanded Disability Status Scale (EDSS) score for participants with a baseline score ≤ 5.0; or a ≥ 0.5‐point increase for participants with a baseline score ≥ 5.5 points; confirmed at six months (Kurtzke 1983). We considered a 1.0‐point increase in EDSS score confirmed at three months' follow‐up as a surrogate outcome measure of progression.
We measured the prespecified outcomes at the following time‐point intervals: short‐term (less than one month post‐intervention), intermediate (one month to less than six months post‐intervention), and long‐term (≥ six months post‐intervention). When a study measured an outcome more than once during the same time‐point interval, we considered the last measure for analysis, to avoid double counting of participants.
Search methods for identification of studies
We conducted a sensitive literature search to identify studies. The search strategy was not limited by year of publication, language or publication type.
Electronic searches
The Information Specialist searched on the specified dates the Trials Register of the Cochrane Multiple Sclerosis and Rare Diseases of the CNS Group, which, among other sources, contains trials from:
-
Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library (2018, issue 10);
-
MEDLINE (www.nlm.nih.gov/bsd/pmresources.html) (1966 to 31 October 2018);
-
Embase (www.elsevier.com/solutions/embase‐biomedical‐research) (1974 to 31 October 2018);
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL; www.ebscohost.com/nursing/products/cinahl‐databases/cinahl‐complete) (1981 to 31 October 2018);
-
Latin American and Caribbean Health Science Information Database (LILACS; lilacs.bvsalud.org/en/) (1982 to 31 October 2018);
-
ClinicalTrials.gov (clinicaltrials.gov); and
-
World Health Organization (WHO) International Clinical Trials Registry Platform (apps.who.int/trialsearch).
See Appendix 1 for the list of keywords used in the search.
In addition we searched:
-
PsycINFO (American Psychological Association (APA) (from inception to 31 October 2018); www.apa.org/pubs/databases/psycinfo/index.aspx); (Appendix 2);
-
PEDro (Physiotherapy Evidence Database; www.pedro.org.au) (from inception to 31 October 2018); (Appendix 3);
-
Opengrey (European Association for Grey Literature Exploitation ‒ EAGLE; www.opengrey.eu) (from inception to 31 October 2018); (Appendix 4).
Information on the Group's Trials Register and details of search strategies used to identify trials can be found in the 'Specialised Register' section within the Cochrane Multiple Sclerosis and Rare Diseases of the CNS Group's website (https://msrdcns.cochrane.org/).
Searching other resources
We screened the reference lists of published reviews to identify RCTs that we may not have identified through our electronic searches. We also handsearched the annals of national and international conferences, such as America's Committee for Treatment and Research in Multiple Sclerosis; Congress of the European Committee for Treatment and Research in Multiple Sclerosis; International Congress on Palliative Care; European Association for Palliative Care; and MS and palliative care societies. We contacted specialists in MS and in palliative care to find additional information.
Data collection and analysis
Selection of studies
Two review authors (COCL and RLP) independently screened all references retrieved by the search and selected studies for full‐text reading from the titles and abstracts. They consulted a third author (ALCM) in case of disagreement. Two independent authors (COCL and RLP) read the full texts of potentially relevant studies. They included those that fulfilled the aforementioned selection criteria. When necessary, a third author (DVP) resolved disagreements. We recorded the reasons for exclusion of each study.
Data extraction and management
The records retrieved by the search were entered into a reference manager program (Mendeley 2017) and this information was transferred to the Rayyan platform (Ouzzani 2016). We identified and excluded duplicates and collated multiple reports of the same study so that each study, rather than each report, was the unit of interest in the review. We recorded the selection process in sufficient detail and completed a PRISMA flow diagram (Moher 2010), and a 'Characteristics of excluded studies' table.
Two review authors (COCL and RLP) independently extracted data from each included RCT using a standardised data extraction form. In case of disagreements, a third author (RR) was involved to reach consensus. When available data were insufficient, we contacted the authors of included studies to obtain additional information (Latorraca 2018 [pers comm]; Latorraca 2018a [pers comm]; Latorraca 2018b [pers comm]; Latorraca 2018c [pers comm]; Latorraca 2018d [pers comm]; Latorraca 2019 [pers comm] ). We extracted the following information from each study.
-
Study identification: title, year of publication, contact authors, and publication status (abstract or full‐text report).
-
Methods: ethical approval, objectives, study design, duration of study and follow‐up period, number and location of centres, setting, methods and unit of randomisation, allocation, concealment, blinding.
-
Participants: inclusion and exclusion criteria, method of recruitment, informed consent obtained, total number randomised, baseline imbalances, withdrawals and losses to follow‐up, age, gender, race/ethnicity, type of MS, previous treatments, comorbidities, diagnostic criteria, and other relevant social and demographic data.
-
Interventions: number randomised in each group, dose, duration of treatment period, delivery setting, co‐interventions, and compliance.
-
Outcomes: primary and secondary outcomes specified and collected, results for all these outcomes (absolute and relative number and rates), definition of outcomes, timing measured and reported, outcome assessors, imputation of missing data, and number of participants in each arm at the end of the study.
-
Notes: funding source, declaration of interest.
Assessment of risk of bias in included studies
Two review authors (COCL and RLP) independently evaluated risk of bias of each included study according to Cochrane's tool for assessing risk of bias (chapter 8.5, Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011)). They involved a third author (RR) to reach consensus, when necessary. The 'Risk of bias' tool covers the following seven domains.
-
Sequence generation: was the allocation sequence adequately generated?
-
Allocation concealment: was allocation adequately concealed?
-
Blinding of participants and personnel: was knowledge of the allocated interventions adequately prevented during the study?
-
Blinding of outcome assessors: was knowledge of the allocated interventions adequately prevented during the study?
-
Incomplete outcome data: were outcome data adequately assessed and accounted for?
-
Selective outcome reporting: were the reports of the study free of any suggestion of selective outcome reporting?
-
Other potential threats to validity: was the study apparently free from other problems that could put it at risk of bias?
Judgement of risk of bias for each domain involves classification into one of three categories: (1) low risk of bias, when we consider the domain described by the study to be adequate; (2) high risk of bias, when we consider the domain described by the study to be inadequate; and (3) unclear risk of bias, when the study does not provide enough information for judgement. For the domains 'blinding of participants and personnel', 'blinding of outcome assessors' and 'incomplete outcome data', we planned to judge different outcomes separately. However, we judged blinding of participants and personnel, blinding of outcome assessment and incomplete outcome data at outcome level, but we presented it gathered by study as it was more readable.
We summarised the overall risk of bias for each outcome, following the criteria below:
-
Low risk of bias (plausible bias unlikely to seriously alter the results) when all the criteria were classified as at low risk of bias.
-
Unclear risk of bias (plausible bias that raises some doubt about the results) when one or more criteria were classified as at unclear risk of bias in the absence of any criteria classified as high risk of bias.
-
High risk of bias (plausible bias that seriously weakens confidence in the results) when one or more criteria were classified as at high risk of bias.
Measures of treatment effect
For each outcome, we calculated a summary estimate of treatment effects with 95% confidence intervals (CIs) for each comparison. We reported continuous data as mean differences (MDs) and, if the outcome was measured in different scales, standardised mean differences (SMDs). We planned to summarise dichotomous outcomes as risk ratios (RRs) and time‐to‐event outcomes as hazard ratios (HRs).
Unit of analysis issues
The analysis was made at the individual allocation level regardless of study design, parallel or cross‐over. We did not find any cluster‐randomised trials or studies with multiple treatment groups that assessed palliative care interventions for MS.
Dealing with missing data
In cases of missing or unavailable data, we contacted the corresponding authors of the primary studies for further information. We recorded the answers obtained and the dates of our contacts. We searched for protocols or additional articles (or both) related to the included trials. Where data were missing to the extent that we could not include the study in the meta‐analysis, and attempts to retrieve data were exhausted, we presented the results as qualitative syntheses.
Assessment of heterogeneity
We assessed the following among studies:
-
Clinical heterogeneity: we assessed included studies based on characteristics of participants (MS types, comorbidity, and treatments that participants were probably receiving on trial entry); characteristics of the intervention (delivery setting, timing of palliative care, treatment duration); and outcomes (measurement tools and timing).
-
Methodological heterogeneity: we assessed the randomisation process, study quality, and analytical methods of the included studies.
-
Statistical heterogeneity: we used the Chi² test and the I² statistic. I² values equal to or higher than 50% were considered as indicative of significant heterogeneity between studies in a meta‐analysis (Higgins 2011).
Assessment of reporting biases
We did not perform a funnel plot analysis because fewer than ten trials were included in the review (Egger 1997).
Data synthesis
We planned to apply a random‐effects model by default. To assess the robustness of our findings, we planned to conduct sensitivity analyses for primary outcomes using fixed‐effect models (Review Manager 2014). In case of inconsistency between the two models, we planned to present both results; otherwise, we would present only results from the random‐effects model. For outcomes where we could not provide a quantitative analysis, we presented the results of individual studies in a narrative synthesis (qualitative analysis).
Subgroup analysis and investigation of heterogeneity
For the primary outcomes, we planned to perform the following subgroup analyses to verify the consistency of results in different subgroups.
-
Disease type: relapsing‐remitting, primary‐progressive or secondary‐progressive.
-
Setting of palliative care: home‐based, hospice‐based, day care‐based, hospital‐based, ambulatory‐based.
Due to the scarcity of studies included in the meta‐analyses, we could not conduct subgroup analyses.
Sensitivity analysis
If a sufficient number of studies had been included, we would have undertaken sensitivity analyses, for the primary outcomes, to assess the strength of the results by:
-
Excluding from the meta‐analysis studies judged to be at 'high risk of bias' and 'unclear risk of bias' as defined in Assessment of risk of bias in included studies section.
-
Excluding from the meta‐analysis unpublished studies.
-
Using fixed‐effect models.
'Summary of findings' table
We created a 'Summary of findings' table for the following outcomes at long‐term follow‐up (≥ six months):
-
Health‐related quality of life.
-
Adverse events.
-
Fatigue.
-
Disability.
-
Anxiety
-
Depression.
-
Hospital admission.
We assessed the five GRADE parameters for each outcome (risk of bias, inconsistency, imprecision, indirectness, and publication bias) to evaluate the quality of the body of evidence as it related to the studies that contributed data to the meta‐analyses (GRADE 2013). We based the grading of the evidence related to the risk of bias on all domains of the 'Risk of Bias' table. We used the methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011); and used GRADEpro software (GRADEprofiler 2011). We justified all decisions to downgrade the quality of the evidence in the footnotes.
Results
Description of studies
We summarised the characteristics of participants, interventions, and outcomes of the included studies in the Characteristics of included studies table.
Results of the search
The search strategy identified 735 records (up to 31 October 2018). An additional 80 records were retrieved through other sources. After removing duplicates, two review authors (COCL and RLP) independently screened the titles and abstracts of 659 records, excluded 646 records and selected 13 for full‐text reading. Two of these were excluded (Campbell 2010; Strupp 2016) because they were narrative reviews. Three studies, that were reported in 11 articles were included (Edmonds 2010; NE‐PAL 2015; PeNSAMI 2018). Figure 1 presents the process of study identification and selection.

Study flow diagram.
Included studies
Date of publication
The included trials were published between 2010 and 2018 (Edmonds 2010; NE‐PAL 2015; PeNSAMI 2018).
Design and setting
Two studies were single‐centre randomised clinical trials: one with a parallel‐group design (NE‐PAL 2015) and one with a cross‐over design (Edmonds 2010). The third study was a multicentric randomised controlled parallel‐group trial (PeNSAMI 2018), conducted in three Italian centres (Milan, Rome and Catania). Two studies were conducted in Italy (NE‐PAL 2015; PeNSAMI 2018) and one in the United Kingdom (Edmonds 2010).
Sample size
Overall, 146 participants with MS were randomised (52 from Edmonds 2010, 18 from NE‐PAL 2015 and 76 from PeNSAMI 2018) and 136 (92%) were available for analysis.
Participants
Overall, 91 participants were female and 55 were male, with a mean age of 57.5 years.
One study (NE‐PAL 2015) included participants with different neurodegenerative disorders: amyotrophic lateral sclerosis (ALS), multiple sclerosis (MS) and Parkinson's disease (PD). We contacted the authors to obtain separate data for participants with MS. Two studies (Edmonds 2010; PeNSAMI 2018) included only participants with severe MS defined as a mean Expanded Disability Status Scale (EDSS) score ≥ 8.0.
Interventions and controls
All three studies assessed home‐based palliative care team visits. Palliative care was offered to all participants allocated to the control group at the end of the studies. In two studies (Edmonds 2010; NE‐PAL 2015), the control group was on a waiting list while in PeNSAMI 2018, the control group was usual care.
Edmonds 2010 included 52 participants with MS from South East London. The duration of the intervention was 12 weeks (first period) and 24 weeks (second period). Participants were assessed at baseline, 6 weeks, 12 weeks, 18 weeks and 24 weeks from intervention. We included only the first period of the cross‐over (12 weeks ‐ intermediate‐term follow‐up). The participants in the intervention group (called Fast track (FT)) received palliative care team visits, 3 visits in 12 weeks, to evaluate and manage their main symptoms. The participants in the control group received standard best practice while they were on a waiting list. The participants in this group received the usual care for MS available in London at that time.
The Ne‐PAL study (NE‐PAL 2015) was conducted in Turin, Italy and included 50 participants in total: 18 with MS, 16 with ALS and 16 with PD. The intervention duration was 16 weeks. Participants were assessed at baseline and at the end of the intervention (week 16), which we considered as intermediate‐term follow‐up. The Intervention group was called Specialist Palliative Care Service (SPSC) ‐ Fast track (FT). Participants in this group received palliative care team visits, at weekly intervals, to assess and manage symptoms. The MS participants in the control group received usual care.
The PeNSAMI study (PeNSAMI 2018) included a total of 76 participants with MS. The intervention duration was 24 weeks. Participants were assessed at baseline, 6 weeks, 12 weeks, 18 weeks (only for the control group) and 26 weeks. The study provided data for the primary outcomes at 12 weeks and 26 weeks (intermediate‐term and long‐term follow‐up). Intervention group participants received home‐based visits from a palliative care team to assess and manage their symptoms. During the first 12 weeks, the participants received team visits every two weeks; during the second 12 weeks period, the visits were scheduled whenever necessary. The participants in the control group received usual care for MS according to local practice.
Outcomes
According to these review outcomes, the studies that evaluated each outcome were:
-
Health‐related quality of life: Edmonds 2010; NE‐PAL 2015; PeNSAMI 2018;
-
Adverse events: PeNSAMI 2018;
-
Fatigue: no included study assessed this outcome;
-
Cognitive function: no included study assessed this outcome;
-
Disability: NE‐PAL 2015;
-
Anxiety: NE‐PAL 2015;
-
Depression: NE‐PAL 2015;
-
Hospital admission: PeNSAMI 2018;
-
Relapse‐free survival: no included study assessed this outcome;
-
Sustained progression‐free survival: no included study assessed this outcome.
Ongoing studies
No ongoing study was identified.
Excluded studies
Two narrative reviews were excluded (Campbell 2010; Strupp 2016) (see Characteristics of excluded studies tables).
Risk of bias in included studies
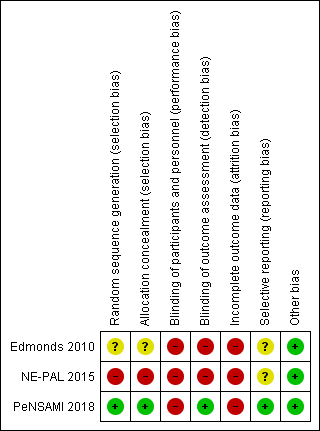
Risk of bias of included studies was evaluated with the Cochrane 'Risk of Bias' tool. Domains were classified as having a 'low risk', 'high risk' and 'unclear risk of bias' (Higgins 2011). We contacted the first or senior authors of all three studies. We asked the authors of PeNSAMI 2018 to provide additional methodological details not reported in the article. To date, two authors (Edmonds 2010; NE‐PAL 2015) responded to our requests and provided additional information. See: Characteristics of included studies, Figure 2 and Figure 3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
PeNSAMI 2018 reported adequate methods for sequence generation and allocation concealment (low risk); NE‐PAL 2015 reported inadequate methods for both domains (high risk); and Edmonds 2010 did not provide enough information to assess sequence generation and allocation concealment (unclear risk).
Blinding
All the three studies reported that participants and investigators were not blinded (high risk). Two studies (Edmonds 2010; NE‐PAL 2015) were at high risk of detection bias (no blinding of outcome assessors) and one study (PeNSAMI 2018) was at low risk.
Incomplete outcome data
We judged all three included studies at high risk because they reported unbalanced numbers across intervention groups with different reasons for loss to follow‐up. No reasonable explanation was given.
Selective reporting
One study (PeNSAMI 2018) reported all prespecified primary outcomes (low risk). The other two included studies did not provide enough information to assess reporting bias (unclear risk).
Other potential sources of bias
No other source of potential bias was found in all three studies and we judged them as having a low risk of bias for this domain.
Effects of interventions
Summary of findings table 1 provides estimates of treatment effects on health‐related quality of life, adverse events and hospital admission at long‐term follow‐up (24 weeks), along with certainty of available evidence for each outcome. Data needed to estimate treatment effects on fatigue, cognitive function, disability, anxiety and depression were not available.
Comparison: Palliative care versus usual care
Primary outcomes
Health‐related quality of life (HRQoL)
All included studies assessed this outcome.
Two studies (NE‐PAL 2015; PeNSAMI 2018) used the Schedule for the Evaluation of Individual Quality of Life Direct Weight (SEiQOL‐DW, higher scores mean better quality of life) tool to assess this outcome at intermediate‐term follow‐up (one month to less than six months post‐intervention).
After our contact, the authors of one study provided additional data (NE‐PAL 2015). Until the publication of this review, PeNSAMI 2018 authors did not reply to our contact, therefore we performed a meta‐analysis with the available data. No difference was observed between the treatment groups for change in HRQoL from baseline to 12 weeks (MD 6.07, 95% CI ‐4.91 to 17.06; participants = 76; studies = 2; I2 = 0%) (Analysis 1.1).
Edmonds 2010 used the Multiple Sclerosis Impact Scale (MSIS, higher scores mean worse quality of life) and presented the data separately for the score change from baseline to 12 weeks for physical and psychological subscales (intermediate‐term follow‐up). The authors found no differences between groups in both subscales: physical score (MD 6.80, 95% CI ‐11.16 to 24.76; participants = 23; studies = 1) (Analysis 1.2) and psychological score (MD 0.90, 95% CI ‐3.12 to 4.92; participants = 38; studies = 1) (Analysis 1.3).
No difference between the treatment groups was also found at long‐term follow‐up, measured with the mean change from baseline to six months, with data available from only one study (PeNSAMI 2018) (MD 4.80, 95% CI ‐12.32 to 21.92; participants = 62; studies = 1; very low‐certainty of evidence) (see summary of findings Table for the main comparison; Analysis 2.1).
Adverse events
One study (PeNSAMI 2018) assessed 'serious adverse events'. Among the 76 participants included, 20 of them reported 22 serious adverse events. There were no differences between groups (13/50 in the palliative care group versus 7/26 in the control group; (RR 0.97, 95% CI 0.44 to 2.12; participants = 76; studies = 1; low‐certainty evidence) (see summary of findings Table for the main comparison; Analysis 2.2).
Secondary outcomes
Fatigue
No included study assessed this outcome.
Cognitive function
No included study assessed this outcome.
Disability
All studies assessed disability using the Expanded Disability Status Scale (EDSS, higher scores mean worse symptoms). However, two studies reported the data incompletely (Edmonds 2010; PeNSAMI 2018). We contacted authors from both studies to request data on this outcome. Edmonds 2010 answered that the EDSS was used to assess the participants at baseline and was not used as an outcome measure. PeNSAMI 2018 did not provide data to date. Therefore, only one study contributed to the analysis of this outcome (NE‐PAL 2015). After our contact, the authors of the NE‐PAL 2015 study provided additional data that we included in the analysis. There were no differences between groups at intermediate‐term follow‐up (MD 0.13, 95% CI ‐0.44 to 0.70; participants = 16; studies = 1) (Analysis 1.4).
Anxiety
Two studies assessed anxiety but reported the results incompletely (NE‐PAL 2015, PeNSAMI 2018). After our contact, the authors of one study provided additional data (NE‐PAL 2015) that we included in the analysis. This study assessed 16 participants.
For anxiety, measured with the Hospital Anxiety and Depression Scale ‐ Anxiety (HADS‐A, higher scores mean worse symptoms), there were no differences between groups at intermediate‐term follow‐up (MD 2.50, 95% CI ‐0.94 to 5.94; participants = 16; studies = 1) (Analysis 1.5).
Depression
Two studies assessed depression (NE‐PAL 2015; PeNSAMI 2018), but only one provided data after contact with authors (NE‐PAL 2015).
For depression, measured with the Hospital Anxiety and Depression Scale ‐ Depression (HADS‐D, higher scores mean worse symptoms), there were no differences between groups at intermediate‐term follow‐up (MD ‐0.50, 95% CI ‐4.14 to 3.14; participants = 16; studies = 1) (Analysis 1.6).
Hospital admission
One study, including 76 participants, assessed this outcome (PeNSAMI 2018). The proportion of participants hospitalised was similar between groups (6/50 in the palliative care group versus 4/26 in the control group; RR 0.78, 95% CI 0.24 to 2.52; participants = 76; studies = 1, low‐certainty evidence) (see summary of findings Table for the main comparison; Analysis 2.3).
Relapse‐free survival
No included study assessed this outcome.
Sustained progression‐free disease survival
No included study assessed this outcome.
Discussion
Summary of main results
This systematic review aimed to evaluate the effects (benefits and harms) of palliative care interventions for people with MS. The results of three RCTs, including a total of 146 participants, indicate that we are uncertain about the effects of palliative care on quality of life, disability, anxiety and depression when compared to usual care. The results of this review reflect the shortage of studies in this area.
The overall very low certainty of evidence (summary of findings Table for the main comparison) for the primary outcomes (health‐related quality of life and adverse events) showed that, for these outcomes, no difference was observed between groups.
Only one included study (PeNSAMI 2018) assessed adverse events and hospital admission. The low number of events and wide confidence intervals crossing null for both outcomes indicates that, based on the current available data, there does not appear to be a difference between the two interventions.
Overall completeness and applicability of evidence
We found three studies that assessed different palliative care interventions in people with MS and EDSS scores ≥ 8.0 at baseline .The participants in the intervention groups received weekly visits from a palliative care team during 12 weeks (first phase of a cross‐over trial), 16 weeks (one RCT), 12 and 24 weeks (one RCT). The participants in the control groups received usual care and were on a waiting list.
In the three studies, the palliative care team included different health professionals that visited the participant at home or wherever the participant was located. The palliative care teams of the three studies had a physician and a nurse, the teams from two studies also had psychologists (NE‐PAL 2015, PeNSAMI 2018), but an administrator (Edmonds 2010), a social worker (PeNSAMI 2018) and a physiotherapist (NE‐PAL 2015) were found in only one study each. Identifying all components of this complex intervention is necessary for its proper implementation and the reproducibility of these findings. The available information did not allow us to identify all components of this complex intervention that is needed for its proper implementation and reproducibility.
None of the palliative care schemes reported in the three studies clearly included physical activities and exercises, which are interventions that could provide some benefit (Amatya 2018, Kumar 2010).
Some limitations can impact the applicability of evidence including the low number of included participants, high disability score of participants at baseline, and the country‐related restriction of the included studies (to Italy and UK).
There is a lack of studies assessing the following outcomes:
-
fatigue: a symptom that affects almost 80% of persons with MS and is also described as one of the worst symptoms they experience was not considered by any of the included studies (Khan 2014).
-
cognitive function: cognitive impairment has been well documented to have a negative impact on employment, social, and avocational activity (Benedict 2002).
Relapse‐free survival and sustained progression‐free survival were not considered as primary outcomes for this review (as the aim of palliative care is not to improve them) and none of the included studies evaluated these outcomes.
Quality of the evidence
This review identified only three trials with only 146 participants. We are uncertain about the effectiveness of palliative care for quality of life when compared to usual care for people with multiple sclerosis.
The overall methodological quality of the included studies was affected by selection, performance, detection and attrition biases. The outcomes of interest were subjective and therefore susceptible to bias related to unblinded outcome assessors. As presented in summary of findings Table for the main comparison, the certainty of the body of evidence was very low for long‐term health‐related quality of life and adverse events. We downgraded the certainty of the evidence because of poor methodological quality of the primary studies and imprecision (small numbers of studies and participants).
Potential biases in the review process
We followed the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) in all steps of this review to minimise bias.The search strategy was broad and sensitive and it is likely that all randomised controlled trials were identified. This can be considered one of the strengths of this review. Limitations of the review include the lack of some outcome data of included studies: among the nine outcomes of interest for this review, we found data for five outcomes only. The data available were sufficient for meta‐analysis for only one outcome. Furthermore, although studies about palliative care usually consider patient and caregiver outcomes, our review focused only on patient outcomes.
The POS‐MS‐S (Palliative care Outcome Scale ‐ Multiple Sclerosis ‐ Symptoms, Sleeman 2013) was a primary outcome in two included studies (Edmonds 2010; PeNSAMI 2018). However, we did not plan to evaluate this measure as an outcome of interest of this review; instead, we decided to assess the symptoms separately (e.g. fatigue, disability, anxiety).
Agreements and disagreements with other studies or reviews
We found no other systematic review that assessed the same clinical question addressed here. One consensus review about palliative care for people with neurological diseases found limited evidence of palliative care for people with MS in terms of symptoms and quality of life improvement (Oliver 2016). This consensus review concluded that further research is needed to evaluate treatment effects in the area of palliative care.

Study flow diagram.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Palliative care versus usual care (intermediate‐term, one month to less than six months post‐intervention), Outcome 1 Health‐related quality of life (SeiQoL‐DW, higher scores means better quality of life) ‐ Change from baseline to 12 weeks.

Comparison 1 Palliative care versus usual care (intermediate‐term, one month to less than six months post‐intervention), Outcome 2 Health‐related quality of life (Multiple Sclerosis Impact Scale, higher scores means worst quality of life) ‐ Change in physical score from baseline to 12 weeks.

Comparison 1 Palliative care versus usual care (intermediate‐term, one month to less than six months post‐intervention), Outcome 3 Health‐related quality of life (Multiple Sclerosis Impact Scale, higher scores means worst quality of life) ‐ Change in psychological score from baseline to 12 weeks.

Comparison 1 Palliative care versus usual care (intermediate‐term, one month to less than six months post‐intervention), Outcome 4 Disability (EDSS, higher scores mean worst symptoms) ‐ Change in disability score from baseline to 16 weeks.
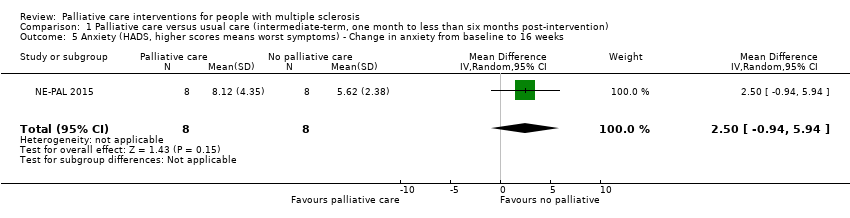
Comparison 1 Palliative care versus usual care (intermediate‐term, one month to less than six months post‐intervention), Outcome 5 Anxiety (HADS, higher scores means worst symptoms) ‐ Change in anxiety from baseline to 16 weeks.

Comparison 1 Palliative care versus usual care (intermediate‐term, one month to less than six months post‐intervention), Outcome 6 Depression (HADS, higher scores means worst symptoms) ‐ Change in depression from baseline to 16 weeks.

Comparison 2 Palliative care versus usual care (long‐term, ≥ six months post‐intervention), Outcome 1 Change in the health‐related quality of life (SeiQoL‐DW, higher scores means better quality of life) ‐ Change from baseline to 24 weeks.

Comparison 2 Palliative care versus usual care (long‐term, ≥ six months post‐intervention), Outcome 2 Serious adverse events.

Comparison 2 Palliative care versus usual care (long‐term, ≥ six months post‐intervention), Outcome 3 Hospital admission.
| Palliative care compared to usual care (long time) for people with multiple sclerosis | ||||||
| Patient or population: Adults people with multiple sclerosis (including RRMS, SPMS, PPMS, PRMS)1 | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with control group (long time) | Risk with Palliative care | |||||
| Health‐related quality of life Assessed by: SeiQoL‐DW (higher scores mean better quality of life) Follow‐up: long‐term (24 weeks) | The mean change of the SeiQoL score in the control group was ‐4.0 | The mean difference of the SeiQoL score in palliative group was 4.8 higher (‐12.43 lower to 22.03 higher) | 58 | ⊕⊝⊝⊝ | ||
| Serious adverse events Assessed by: number of participants presenting at least one serious adverse event Follow‐up: long‐term (24 weeks) | 269 per 1.000 | 261 per 1.000 | RR 0.97 | 76 | ⊕⊕⊝⊝ LOW 3.4 | |
| Hospital admission Assessed by: number of participants admitted in hospital Follow‐up: long‐term (24 weeks) | 154 per 1.000 | 120 per 1.000 | RR 0.78 | 76 | ⊕⊕⊝⊝ LOW 3,4 | |
| Fatigue ‐ Not reported at long term follow‐up | ||||||
| Disability ‐ Not reported at long term follow‐up | ||||||
| Anxiety ‐ Not reported at long term follow‐up | ||||||
| Depression ‐ Not reported at long term follow‐up | ||||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 RRMS: Relapsing‐remitting Multiple Sclerosis; SPMS: Secondary‐progressive Multiple Sclerosis; PPMS: Primary‐progressive Multiple Sclerosis; PRMS: Progressive‐relapsing Multiple Sclerosis. 2 Downgraded two levels due to risk of bias (unblinded participants and outcome liable to participant subjective judgement and incomplete outcome data). 3 Downgraded one level due to imprecision (low number of participants and wide confidence interval crossing the null). 4 Downgraded one level for risk of selective reporting (2/3 studies did not report health‐related quality of life measured by SeiQoL‐DW at 24 weeks). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Health‐related quality of life (SeiQoL‐DW, higher scores means better quality of life) ‐ Change from baseline to 12 weeks Show forest plot | 2 | 76 | Mean Difference (IV, Random, 95% CI) | 6.07 [‐4.91, 17.06] |
| 2 Health‐related quality of life (Multiple Sclerosis Impact Scale, higher scores means worst quality of life) ‐ Change in physical score from baseline to 12 weeks Show forest plot | 1 | 23 | Mean Difference (IV, Random, 95% CI) | 6.8 [‐11.16, 24.76] |
| 3 Health‐related quality of life (Multiple Sclerosis Impact Scale, higher scores means worst quality of life) ‐ Change in psychological score from baseline to 12 weeks Show forest plot | 1 | 38 | Mean Difference (IV, Random, 95% CI) | 0.9 [‐3.12, 4.92] |
| 4 Disability (EDSS, higher scores mean worst symptoms) ‐ Change in disability score from baseline to 16 weeks Show forest plot | 1 | 16 | Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.44, 0.70] |
| 5 Anxiety (HADS, higher scores means worst symptoms) ‐ Change in anxiety from baseline to 16 weeks Show forest plot | 1 | 16 | Mean Difference (IV, Random, 95% CI) | 2.50 [‐0.94, 5.94] |
| 6 Depression (HADS, higher scores means worst symptoms) ‐ Change in depression from baseline to 16 weeks Show forest plot | 1 | 16 | Mean Difference (IV, Random, 95% CI) | ‐0.5 [‐4.14, 3.14] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in the health‐related quality of life (SeiQoL‐DW, higher scores means better quality of life) ‐ Change from baseline to 24 weeks Show forest plot | 1 | 62 | Mean Difference (IV, Random, 95% CI) | 4.8 [‐12.32, 21.92] |
| 2 Serious adverse events Show forest plot | 1 | 76 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.44, 2.12] |
| 3 Hospital admission Show forest plot | 1 | 76 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.24, 2.52] |

