Hybrid repair versus conventional open repair for aortic arch dissection
Abstract
Background
A dissection of the aorta is a separation or tear of the intima from the media. This tear allows blood to flow not only through the original aortic flow channel (known as the true lumen), but also through a second channel between the intima and media (known as the false lumen). Aortic dissection is a life‐threatening condition which can be rapidly fatal. There is debate on the optimal surgical approach for aortic arch dissection. People with ascending aortic dissection have poor rates of survival. Currently open surgical repair is regarded as the standard treatment for aortic arch dissection. We intend to review the role of hybrid and open repair in aortic arch dissection.
Objectives
To assess the effectiveness and safety of a hybrid technique of treatment over conventional open repair in the management of aortic arch dissection.
Search methods
The Cochrane Vascular Information Specialist searched the Cochrane Vascular Specialised Register, CENTRAL, MEDLINE, Embase, CINAHL and AMED databases and World Health Organization International Clinical Trials Registry Platform and ClinicalTrials.gov trials registers to 8 February 2021. We also undertook reference checking for additional studies.
Selection criteria
We included randomised controlled trials (RCTs) and clinical controlled trials (CCTs), which compared the effects of hybrid repair techniques versus open surgical repair of aortic arch dissection. Outcomes of interest were dissection‐related mortality and all‐cause mortality, neurological deficit, cardiac injury, respiratory compromise, renal ischaemia, false lumen thrombosis (defined by partial or complete thrombosis) and mesenteric ischaemia.
Data collection and analysis
Two review authors independently screened all records identified by the literature searches to identify those that met our inclusion criteria. We planned to undertake data collection and analysis in accordance with recommendations described in the Cochrane Handbook for Systematic Reviews of Interventions. We planned to assess the certainty of the evidence using GRADE.
Main results
We identified one ongoing study and two unpublished studies that met the inclusion criteria for the review. Due to a lack of study data, we could not compare the outcomes of hybrid repair to conventional open repair for aortic arch dissection.
Authors' conclusions
This review revealed one ongoing RCT and two unpublished RCTs evaluating hybrid versus conventional open repair for aortic arch surgery. Observational data suggest that hybrid repair for aortic arch dissection could potentially be favourable, but conclusions can not be drawn from these studies, which are highly selective, and are based on the clinical status of the patient, the presence of comorbidities and the skills of the operators. However, a conclusion about its definitive benefit over conventional open surgical repair cannot be made from this review without published RCTs or CCTs.
Future RCTs or CCTs need to have adequate sample sizes and follow‐up, and assess clinically‐relevant outcomes, in order to determine the optimal treatment for people with aortic arch dissection. It must be noted that this may not be feasible, due to the reasons mentioned.
PICO
Plain language summary
Hybrid versus conventional open repair for aortic arch dissection
Background
A dissection of the aorta is a separation or tear of the intima from the media. This tear allows blood to flow not only through the original aortic flow channel (known as the true lumen), but also through a second channel between the intima and media (known as the false lumen). A dissection can then develop along the artery, secondary to the blood flowing into the space. Aortic dissection is a life‐threatening condition which can rapidly be fatal. Aortic dissection that affects the ascending aorta, aortic arch and the descending aorta is a challenge for physicians. There is debate on the best surgical approach for aortic arch dissection. People with ascending aortic dissection have poor rates of survival. Currently, open surgical repair is regarded as the standard treatment for aortic arch dissection.
Study characteristics and key results
We searched medical databases for clinical trials that compared the use of a hybrid technique versus open surgical technique for people who suffered from arterial dissection of the aortic arch (last search February 2021). We identified one ongoing study and two unpublished studies, which met the inclusion criteria for the review. However, due to a lack of published study data, we could not compare the outcomes of hybrid repair to conventional open repair for aortic arch dissection.
Certainty of the evidence
In the absence of study data for those identified as eligible for inclusion in the review, it was not possible to assess the certainty of the evidence.
Conclusion
There is an absence of data for patients with this type of condition. Reasons may include its acute nature, and the need to intervene quickly in a surgical environment; patients with aortic arch dissection often suffer from many other conditions, which prevent them having particular surgeries; and often centres and surgical expertise may be lacking in this area, leading to a culture of using conventional rather than contemporary methods.
Future studies need to have adequate sample sizes and follow‐up, and assess clinically relevant outcomes, in order to determine the best treatment for people with aortic arch dissection. It must be noted that this may not be feasible due to the reasons mentioned.
Authors' conclusions
Background
See Appendix 1 for Glossary of terms.
Description of the condition
The aorta is the main artery in the body. It originates in the heart and supplies blood to all parts of the body. The aorta consists of three layers: the intima, which is the innermost layer; the media, which is the middle layer; and the adventitia, which is the outermost layer. A dissection of the aorta is a separation or tear of the intima from the media. This tear allows blood to flow not only through the original aortic flow channel (known as the true lumen), but also through a second channel along the medial layers (known as the false lumen) (Tran 2009). A dissection can then propagate along the artery, secondary to the blood flowing into the space. Aortic dissection is a life‐threatening condition which can be rapidly fatal. It occurs more frequently in men, and uncontrolled blood pressure (hypertension) is a leading risk factor (Nienaber 2004). Predominate risk factors include genetic or familial aortopathies and connective tissue disorders such as Loeys‐Dietz syndrome, Marfan syndrome, and Ehlers‐Danlos syndrome (Murphy‐Ryan 2010).
According to the reporting standards for thoracic endovascular aortic repair, the aorta is divided into 12 treatment zones, zone 0 to zone 11. Aortic arch dissection occurs between zone 0 and zone 4 (Fillinger 2010). Zone 0 refers to an area between the aortic sinus and the brachiocephalic artery origin; zone 1 is distal to the brachiocephalic artery but proximal to the left common carotid artery origin; zone 2 is distal to the left common carotid artery but proximal to the subclavian artery; zone 3 is within 2 cm of the left subclavian artery without covering it; and zone 4 refers to an area 2 cm or more distal to the left subclavian artery and ends within the proximal half of the descending thoracic aorta (Fillinger 2010).
There are two classification systems for aortic dissection:
-
the Stanford classification, which categorises dissection into Type A and Type B (Daily 1970; DeBakey 1966). Type A occurs in the ascending aorta or aortic arch, or both, with possible involvement of the descending aorta. Type B occurs in the descending aorta, beyond the left subclavian artery; and
-
the DeBakey classification, which categorises dissection into Type I, Type II, and Type III. Type I involves the ascending and descending aorta (Stanford Type A), Type II involves the ascending aorta only (Stanford Type A), and Type III involves the descending aorta only, beginning after the left subclavian artery (Stanford Type B) (Daily 1970; DeBakey 1966).
Aortic dissection is also classified based on the age of the dissection (chronicity), as the mortality rates vary with chronicity (Wong 2008). These classifications are, from the onset of symptoms: less than 24 hours (hyper‐acute); less than 2 weeks (acute); 2 to 6 weeks (sub‐acute); and more than 6 weeks (chronic) (Nienaber 2011). As the dissection progresses in chronicity, the separated arterial layers that divide the true and false lumen (the intraluminal septum) increase in rigidity and reduce in elasticity and mobility, causing the septum to become stiff.
Description of the intervention
Aortic dissection that affects the ascending aorta, aortic arch and the descending aorta is a challenging pathology for physicians. People with this type of aortic disease pose a surgical challenge in this area of continuing development and innovation (Cochennec 2013; Kurimoto 2015; Lu 2013). Treatment of aortic dissection can be by open repair, endovascular repair, or a hybrid repair (Antoniou 2010; Cao 2012; Cochennec 2013; Murphy 2012; O'Callaghan 2014). There is debate on the optimal surgical approach for aortic arch dissection. People with ascending aortic dissection have poor rates of survival. Currently, open surgical repair (OSR) is regarded as the standard treatment for aortic arch dissection (DeBakey 1966; Suzuki 2003).
Open surgical repair
Current treatment for complex aortic arch dissection depends on the distal extent of the dissection, the location of the intimal tear, the diameter of the distal aortic arch and the relative fitness of the patient. The mainstay of treatment for type A dissection is complete resection of the intimal tear and replacement of the ascending aorta with a prosthetic graft. However, if the dissection extends into the aortic arch more extensive resections and aortic graft replacement may be required. A hemi‐arch repair can be undertaken if the dissection does not extend beyond the proximal arch, if the intimal tear is on the inner curve and does not involve the supra‐aortic vessels, if the distal aortic arch is not aneurysmal, or if the patient is unfit for extensive repair (Yang 2019). This involves removal of the ascending portion of the aorta and the proximal aortic arch, and replacement and open proximal and distal anastomosis (connection) with a surgical graft. This is carried out under artificially‐induced circulatory arrest (a method of temporarily stopping the blood flow completely, to create a bloodless field) with varying degrees of hypothermia (cooling of core body temperature), and a selection of cerebral protection techniques, including antegrade or retrograde cerebral perfusion, or deep hypothermia alone. Potential complications of open surgical repair include stroke, cardiac arrhythmia (irregular heartbeat), coagulopathy (failure to clot, or inappropriate clotting of blood), and hypokalaemia (lower than normal level of potassium in the blood) (Groysman 2011). This type of repair is high‐risk and carries a mortality risk of 21.6%, even with the use of circulatory arrest and cerebral perfusion techniques (Patel 2011).
In cases where the intimal dissection cannot be adequately treated by replacement of a hemi‐arch, or where the arch is aneurysmal or there is malperfusion of the supra‐aortic vessels, a more aggressive total arch replacement is warranted (Yang 2019). Surgical grafts with sidearms for the supra‐aortic branches and a perfusion branch reduce the number of surgical anastomoses required. In cases in which there is no evidence of supra‐aortic malperfusion and the supra‐aortic arteries are not dissected, the supra‐aortic vessel can be reimplanted en bloc (island) to the aortic graft, reducing the number of individual anastomoses (Shrestha 2014). Although total arch repair operative time is longer and requires more experience and surgical skill, it is associated with a reduced risk of aortic rupture, a lower stroke rate and a reduction in aortic re‐intervention rates (Smith 2017).
Hybrid repair
Hybrid techniques use a combination of endovascular approaches (intervention through the arteries using wires to carry grafts) and open surgical approaches to treat arch pathologies. These methods are designed to be less invasive than conventional open techniques and may permit more extensive arch repair in those unfit for open total arch repair (Smith 2017). The aorta is treated with a surgical graft in combination with the less invasive approach of endovascular implantation of an aortic stent endograft. Purely endovascular implantation of an endograft in the aorta is made through peripheral arterial access sites such as the femoral arteries, with no invasive surgical intervention. However, techniques for total endovascular repair, although promising, are still in their infancy (Nordon 2012), and reports estimate that in anatomical terms only 30% to 50% of patients with Stanford Type A aortic dissection are suitable for total endovascular repair with current technologies (Moon 2011; Sobocinski 2011).
Hybrid repair involves surgical arch debranching of the supra‐aortic vessels, thereby creating a proximal landing zone of adequate length, followed by endovascular stent graft insertion in the surgically‐constructed landing zone within the aortic arch.
Complete debranching of the aortic arch consists of revascularisation (restoring blood to the vessel) of at least the brachiocephalic artery and the left common carotid artery via a prosthetic bypass from the ascending aorta. After induction of pharmacologic hypotension (inducing a state of low blood pressure to reduce blood loss), the ascending aorta is clamped tangentially and the proximal end of a prosthetic graft sutured in an end‐to‐side anastomosis (Tominaga 2003). The left subclavian artery is revascularised through the sternotomy (division of the chest bone) or through an incision above the clavicle (collar bone). Aortic arch branch vessels can be bypassed with a singular, bifurcated (two branches) or trifurcated (three branches) tube graft.
Alternatively, cervical debranching can be performed through cervicotomies (incision in the neck) and consists of retro‐oesophageal right common carotid‐to‐left common carotid artery bypass using a Dacron graft. Depending on the surgeon's preference, the left subclavian artery can be ligated (tied up) or revascularised via a transposition into the left common carotid artery or a carotid artery bypass (Cochennec 2013).
During hybrid repair the endovascular intervention can be carried out in isolation or concurrently with the surgical intervention. In people with extensive disease of the thoracic arch and descending aorta, a single‐stage approach under circulatory arrest shows promising results (Jakob 2011; Sun 2011).
Hybrid approaches are classified into three types according to the extent of the aortic arch lesion and presence of the proximal and distal landing zones (Moulakakis 2013):
-
Type I: the debranching procedure consists of brachiocephalic bypass and endovascular repair of the aortic arch. This approach is reserved for people with isolated disease exhibiting an adequate proximal landing zone in the ascending aorta and a distal landing zone in the descending thoracic aorta (Stanford Type A/DeBakey Type II);
-
Type II: an open ascending aorta reconstruction that creates an appropriate proximal landing zone, supra‐aortic vessel revascularisation, and endoluminal dissection coverage. This approach is designed for people with ascending aortic lesions with a limited extension into the distal arch (Stanford Type A/DeBakey Type I); and
-
Type III: an elephant trunk procedure with a complete endovascular repair of the thoracoabdominal aorta. This technique is reserved for people with extensive aortic lesions that involve the ascending, transverse arch, and descending thoracic aorta (Stanford Type A/DeBakey Type I). This type III hybrid approach requires total open arch replacement and so falls outside the remit of this review, and is described here for the sake of complete description of the Moulakakis classification.
How the intervention might work
Although to date trial results using hybrid repair techniques for aortic arch dissection are promising, opinion is divided on its efficacy among the wider vascular surgery community (Kurimoto 2015). The aim of both hybrid repair and OSR is to stop further dissection progression in the aortic artery by covering the dissection entry points and also by promoting false lumen thrombosis; OSR is regarded as the standard for aortic arch dissection. Intervention for aortic arch dissection with a hybrid approach could reduce the incidence of highly invasive surgery when compared to OSR, while duration of cardiopulmonary bypass, hypothermic circulatory arrest and antegrade/retrograde cerebral perfusion can be reduced. Cardiopulmonary bypass is a technique that temporarily takes over the function of the heart and lungs during surgery, maintaining the circulation of blood and oxygen in the body. Hypothermic circulatory arrest temporarily suspends blood flow under very cold body temperatures. Antegrade cerebral perfusion involves sewing a small graft to the axillary/brachiocephalic artery or left common carotid artery. The graft is connected to a heart‐lung machine, and allows blood to flow through the brain during complex surgery of the aorta. Retrograde cerebral perfusion requires cannulation of the vena cava with perfusion pressures not exceeding 25 mmHg. Antegrade perfusion permits blood flow through the arterial system, allowing for varying temperature control. Retrograde perfusion permits blood flow through the venous system. The high associated risks using these methods including mortality (death) (6.6% to 9.9%), stroke (2.7% to 6.6%), paraplegia (18%), cardiac arrhythmia (irregular heartbeat), venous congestion and cerebral oedema would therefore be reduced or negated by using hybrid repair (Estrera 2003; Kamiya 2007; Okita 2001).
Why it is important to do this review
To date, no Cochrane Review has assessed the effectiveness of hybrid repair compared to the standard OSR. There is an agreement that intervention is necessary for aortic arch dissection, but complex open aortic arch repair still carries a high degree of health risks and death due to the use of cardiopulmonary bypass, hypothermic circulatory arrest, and antegrade or retrograde cerebral perfusion during the procedure (Lu 2013; Murphy 2012; Rampoldi 2007; Vohra 2012). Deciding if a person will undergo a hybrid versus an open repair depends on their fitness and comorbidity, surgical skill and physician preference, the overall quality of the supra‐aortic vessels (the brachiocephalic artery, the left common carotid artery, and subclavian artery) and the ability to clamp them, and whether cerebral perfusion can be maintained adequately.
We undertook this review as there is a critical need within the cardiovascular community for a synthesis of high‐quality evidence to inform decisions on optimal management of aortic arch dissection. Our systematic review focuses on aortic arch dissection treatments (specifically of Stanford Type A, i.e. DeBakey Type I and Type II) using hybrid and open repair.
Objectives
To assess the effectiveness and safety of a hybrid technique of treatment over conventional open repair in the management of aortic arch dissection.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and controlled clinical trials (CCTs) assessing the effects of hybrid repair techniques compared to open surgical repair (OSR) of aortic arch dissection.
Types of participants
We include all participants with a diagnosis of aortic arch dissection. This includes classifications of dissection according to Stanford Type A (DeBakey Type I and Type II). Diagnosis was made by relevant diagnostic modalities, i.e. computed tomography (CT) or magnetic resonance imaging (MRI), or both. There was no limitation by participant gender, age, ethnicity, treatment setting (e.g. elective versus emergency repair), or dissection chronicity (acute or chronic). We excluded patients requiring a concomitant aortic valve repair.
Types of interventions
We include the following comparisons:
-
Type I hybrid repair versus OSR;
-
Type II hybrid repair versus OSR.
Types of outcome measures
Outcomes were guided and defined by the International Aortic Arch Surgery Study Group (Yan 2014; see also Table 1 for more details).
| Types of outcome measures | Defined by | Including |
|---|---|---|
| Primary outcomes | ||
| Mortality | Dissection related and all causes | (Grade V) All deaths at 30 days and 12 months |
| Neurological deficit | Global events | (Grade I ‐ IV) Postoperative agitation, delirium, obtundation, or myoclonic movements, without localised cerebral neurological signs |
| Focal events | (Grade I ‐ IV) Lateralising sensory or motor deficit or focal seizure activity | |
| Spinal neurological events | (Grade I ‐ IV) Paraplegia, paraparesis | |
| Cardiac injury | Myocardial ischaemia | (Grade I ‐ IV) |
| Low cardiac output syndrome | (Grade I ‐ IV) | |
| Arrhythmia | (Grade I ‐ IV) | |
| Pericardial effusion | (Grade I ‐ IV) | |
| Respiratory compromise | Parenchymal complications | (Grade I ‐ IV) Atelectasis, pneumonia, pulmonary oedema, and acute respiratory distress syndrome |
| Pleural complications | (Grade I ‐ IV) Pneumothorax, pleural effusion | |
| Renal ischaemia | Modified RIFLE classification (Bellomo 2004): Risk (I), Injury (II), Failure (III), Loss/End‐Stage Kidney Dysfunction (IV) | (Grade I ‐ IV) Serum creatinine increase, glomerular filtration rate (GFR) decrease, anuria, haemodialysis |
| Secondary outcomes | ||
| False lumen thrombosis | Partial or complete thrombosis | ‐ |
| Mesenteric ischaemia | Gut complications | (Grade I ‐ IV) Ileus or gastric paresis, gut ischaemia manifested as metabolic acidosis or increased lactate |
| Grades as defined by Yan 2014: Grade I: any deviation from the normal postoperative course but self‐limiting or requiring simple therapeutic regimens (including antiemetics, antipyretics, analgesics, electrolytes, and physiotherapy); Grade II: complications requiring pharmacological treatment for resolution; Grade III: complications requiring surgical, endoscopic, or radiological intervention but not requiring regional or general anaesthesia or requiring interdisciplinary intervention; Grade IV: complications requiring surgical, endoscopic, or radiological intervention under regional or general anaesthesia, or requiring new intensive care unit (ICU) admission or ongoing ICU management for > 7 days or hospitalisation for > 30 days, or causing secondary organ failure; Grade V: death caused by a complication. | ||
Primary outcomes
-
Dissection‐related mortality and all‐cause mortality at 30 days and 12 months (Grade V)
-
Neurological deficit (defined by global, focal and spinal events, Grade I to IV)
-
Cardiac injury (defined by myocardial ischaemia, low cardiac output syndrome, arrhythmia, pericardial effusion, Grade I to IV)
-
Respiratory compromise (defined by parenchymal and pleural complications, Grade I to IV)
-
Renal ischaemia (defined by RIFLE classification Bellomo 2004, Grade I to IV)
Secondary outcomes
-
False lumen thrombosis (defined by partial or complete thrombosis)
-
Mesenteric ischaemia (defined by gastrointestinal complications, Grade I to IV)
Search methods for identification of studies
Electronic searches
The Cochrane Vascular Information Specialist conducted systematic searches of the following databases for randomised controlled trials and controlled clinical trials without language, publication year or publication status restrictions.
-
the Cochrane Vascular Specialised Register via the Cochrane Register of Studies (CRS‐Web searched from inception to 8 February 2021).
-
the Cochrane Central Register of Controlled Trials (CENTRAL) Cochrane Register of Studies Online (CRSO 2021, Issue 1).
-
MEDLINE (Ovid MEDLINE® Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE® Daily and Ovid MEDLINE®) (searched to 8 February 2021).
-
Embase Ovid (searched 8 February 2021).
-
CINAHL Ebsco (searched to 8 February 2021).
-
AMED Ovid (searched to 8 February 2021).
The Information Specialist modelled search strategies for other databases on the search strategy designed for CENTRAL. Where appropriate, they were combined with adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials (as described in the Cochrane Handbook for Systematic Reviews of Interventions Chapter 6, Lefebvre 2011). Search strategies for major databases are provided in Appendix 2.
The Information Specialist also searched the following trials registries on 8 February 2021.
-
ClinicalTrials.gov (clinicaltrials.gov).
-
World Health Organization International Clinical Trials Registry Platform (who.int/trialsearch).
For the purpose of this review, we also included studies published as abstracts only, if we could extract sufficient information. In cases where insufficient data were published, we first contacted the trial authors to access the required information. If data remained insufficient after contacting the trial authors, we excluded the study from our review.
Searching other resources
We searched the reference lists of all included studies.
Data collection and analysis
Selection of studies
Two review authors (EPK and AE) independently assessed the titles and abstracts of each identified study. Both review authors (EPK and AE) assessed the full texts of all studies categorised as included or unclear at title/abstract screening. If the review authors disagreed on the inclusion or exclusion of a study, we discussed the reasons. If there was no agreement between the two review authors, then we discussed with a third review author (NH). We recorded reasons for exclusions in the Characteristics of excluded studies table. We describe the selection process in an adapted PRISMA flow chart (Liberati 2009).
Data extraction and management
We obtained full‐text reports of the studies selected, and two review authors (EPK and AE) independently extracted data using an adapted data extraction form provided by Cochrane Vascular. If there was disagreement between the two review authors, we resolved issues by discussion with a third review author (NH). For studies with duplicate or multiple publications (or both), we collated all available data, and presented them as one study data set.
We aimed to describe the studies according to the following:
-
trial design;
-
diagnosis of aortic arch dissection;
-
demographic characteristics of participants;
-
type of intervention (hybrid and open repair); and
-
frequency of primary and secondary outcomes.
Assessment of risk of bias in included studies
Two review authors (EPK and AE) planned to independently assess the potential risks of bias in all included RCTs and CCTs using the Cochrane risk of bias tool (Higgins 2011). We planned to judge each domain as low risk, high risk, or unclear risk of bias and provide a statement to support each judgement. If there was disagreement between the two review authors, we planned to resolve these by consensus, and when necessary, by discussion with a third review author (NH).
We assessed the risk of bias in the following domains:
-
selection bias (random sequence generation and allocation concealment);
-
performance bias (blinding of participants and personnel);
-
detection bias (blinding of outcome assessors);
-
attrition bias (incomplete outcome data);
-
reporting bias (selective outcome reporting); and
-
other sources of bias.
Measures of treatment effect
Dichotomous data
We planned to express the results for dichotomous outcomes as risk ratios (RRs) with 95% confidence intervals (CIs), to reflect uncertainty of the point estimate of effects.
Continuous data
We planned to express the results for continuous scales of measurement as mean differences (MDs), standard deviations (SDs) and associated 95% CIs. Where there was a difference in scales for the same outcome, we used the standardised mean difference (SMD) with a 95% CI to combine the outcomes.
Time‐to‐event data
We aimed to use survival analysis to present time‐to‐event data expressed as hazard ratios (HRs) with 95% CIs. Methods used to analyse time‐to‐event outcomes were guided by those described by Parmar 1998 and Tierney 2007, and as detailed in Chapter 7, section 7.7.6 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Unit of analysis issues
We considered the unit of analysis within each trial to be each participant.
Dealing with missing data
In studies that had incomplete data, we contacted the study authors to seek additional data. For all outcomes, we aimed to carry out analyses as far as possible on an intention‐to‐treat basis (i.e. based on the initial treatment assignment and not on the treatment eventually received).
Assessment of heterogeneity
We planned to evaluate clinical heterogeneity based on participant data, the intervention and outcomes of each study. Our aim was to assess the degree of heterogeneity by visual inspection of forest plots and by examining the Chi2 test for heterogeneity. We planned to use the I2 statistic, Tau2 statistic and Chi2 test to determine statistical heterogeneity among studies, according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
We would have rated statistical heterogeneity as substantial if an I2 were greater than 50% and either the Tau2 was greater than zero, or there was a low P value (less than 0.10) in the Chi2 test for heterogeneity. If we had identified substantial heterogeneity, we planned to explore possible reasons using subgroup analyses.
We did not undertake an assessment of heterogeneity, since we identified one ongoing study and two unpublished studies only, so results could not be pooled.
Assessment of reporting biases
We planned to address publication bias and other reporting biases (such as multiple publication bias) using funnel plots, in line with Cochrane Vascular guidelines, if there were 10 or more included studies (Higgins 2011).
This review has no included studies, so we did not investigate publication bias or other reporting bias using funnel plots.
Data synthesis
We planned to enter the collected data into Review Manager 5 software (Review Manager 2020). We planned to use a fixed‐effect meta‐analysis for synthesising data where it is reasonable to assume that trials are estimating the same underlying treatment effect. If clinical heterogeneity was sufficient to expect that the underlying treatment effects differ between trials, or if we detected substantial statistical heterogeneity, we planned to use a random‐effects meta‐analysis to produce an overall summary where the average treatment effect is clinically meaningful. If we identified clinical, methodological or statistical heterogeneity across included trials sufficient to cause concerns about the appropriateness of pooling results, we did not report pooled results from the meta‐analysis but instead planned to use a narrative approach to data synthesis. We planned to create a forest plot for each treatment effect, in accord with Cochrane Vascular guidelines (Higgins 2011).
We did not conduct a data synthesis in the form of a meta‐analysis or a narrative approach, since we did not identify published studies that met the inclusion criteria.
Subgroup analysis and investigation of heterogeneity
If we had found considerable heterogeneity within the included studies, we planned to carry out subgroup analyses to investigate possible reasons for this heterogeneity. We also planned to perform the following subgroup analyses, which were guided by DISSECT, a mnemonic‐based approach to the categorisation of aortic dissection (Dake 2013).
-
Duration of disease (i.e. acute dissection (less than 14 days) versus chronic dissection (14 days or more))
-
Intimal tear location (i.e. ascending aorta versus aortic arch)
-
Segmental extent of the disease (i.e. DeBakey Type I versus DeBakey Type II)
-
Size of the dissected aorta (i.e. maximum diameter less than 5.5 cm versus 5.5 cm or more (Pape 2007))
-
Presence or absence of complication
-
Thrombosis of aortic false lumen
-
Presence or absence of connective tissue disorder
-
Gender (Nienaber 2004)
-
Age (i.e. less than 70 years versus 70 years or older (Trimarchi 2010))
We did not undertake subgroup analysis or investigate heterogeneity because we did not conduct a data synthesis.
Sensitivity analysis
We aimed to perform sensitivity analyses on the following:
-
High‐quality trials, defined as studies with a low risk of bias for sequence generation and allocation concealment; and
-
RCTs compared with CCTs.
However, we did not perform a sensitivity analysis because we did not conduct a meta‐analysis of data.
Summary of findings and assessment of the certainty of the evidence
We planned to prepare a summary of findings table according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We intended to use GRADE profiler software to create the tables (GRADEproGDT 2015). For each comparator, we planned to include all primary and secondary outcomes as described in the Types of outcome measures section. Using the GRADE approach, we planned to assess the certainty of the body of evidence for the primary and secondary outcomes prespecified in our Cochrane protocol (Kavanagh 2018), as high, moderate, low or very low, based on the criteria of risk of bias, inconsistency, indirectness, imprecision and publication bias (GRADE Working Group 2004; Guyatt 2008a; Guyatt 2008b; Schünemann 2006). A draft version of the summary of findings table is included in this review (see Table 2).
| Summary of findings for the main comparison: Hybrid repair versus conventional open repair for aortic arch dissection | ||||||
| Patient or population: patients with a diagnosis of aortic arch dissection Settings: hospital Intervention: hybrid repair Comparison: open repair | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with open repair | Risk with hybrid repair | |||||
| Mortality, Follow‐up: median N (months) | Study population | HR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| Neurological deficit, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| Cardiac injury, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| Respiratory compromise, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| Renal ischaemia, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| False lumen thrombosis, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| Mesenteric ischaemia, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
Results
Description of studies
See Figure 1.

Study flow diagram.
Results of the search
We identified three studies that met the inclusion criteria. One study is ongoing (ChiCTR‐IPR‐16009372), while the remaining two studies are unpublished, with study data not available (ChiCTR‐TRC‐11001828; ChiCTR‐TRC‐13003857). The study investigators have been contacted, but with no response. These studies will be assessed further during subsequent review updates. See Characteristics of ongoing studies.
Ongoing studies
The study ChiCTR‐IPR‐16009372 is a randomised parallel controlled trial, which compared and evaluated different therapeutic procedures of the aortic arch for acute Stanford type A aortic dissection, with the aim of elucidating the optimal therapeutic strategy for the aortic arch. The target sample size was 280 participants, over four groups:
-
Total arch replacement (TAR group);
-
Arch reserved procedure (ARP group);
-
Hybrid procedure (Hybrid group); and
-
Triple‐branched stent graft (TBSG group).
The populations included participants diagnosed with Stanford type A aortic dissection by computed tomography angiography (CTA) imaging, with an onset time of less than two weeks. The primary source of funding was Renji Hospital, School of Medicine, Shanghai Jiao Tong University (China). The study describes its recruitment status as pending/not yet recruiting. This study is a registered clinical trial but no trial results are available. The study investigators have been contacted for clarification, and possible results, but we have received no response.
ChiCTR‐TRC‐11001828 is a randomised parallel controlled trial comparing the outcome of the two different operational methods to treat the aortic dissection: replacing ascending aorta plus reconstructing aortic arch with triple‐branched stent graft, and replacing ascending aorta plus replacing half aortic arch to treat the aortic dissection. The target sample size was 100 participants. The population included aortic dissection: type A with an onset time of less than two weeks. Primary outcomes were operation time, length of stay and aortic angiography computed tomography (CT). There were no secondary outcomes. The primary source of funding was the Scientific Research Department of The Affiliated Union Hospital, Fujian Medical University (China). This study is a registered clinical trial but no trial results are available. The study investigators have been contacted for clarification, and possible results, but we have received no response.
ChiCTR‐TRC‐13003857 is a prospective, multicentre, randomised parallel controlled trial, which evaluated the safety and efficacy of Xuper Open Surgery Stent Graft System (Lifetech Scientific, Shenzhen, China) for the surgical treatment of Stanford type A aortic dissection. The intervention was the Xuper Open Surgery Stent Graft System, while the comparator was open surgical repair using the Intergard graft (Getinge AB, Stockholm, Sweden). The population included those diagnosed with Stanford type A aortic dissection. The target sample sizes were 60 and 30, respectively. Primary outcomes included the duration of circulatory arrest. Secondary outcomes included: the incidence of major adverse events (death, paraplegia, brain complications); stent implantation successful (stent in place and successfully released); operation time; cardiopulmonary bypass time; arterial anastomosis time; aortic occlusion time; intraoperative blood loss and blood transfusion volume; and treatment success (12 months after operation). The primary source of funding was Lifetech Scientific (Shenzhen) Co. Ltd. This study is a registered clinical trial but no trial results are available. The study investigators have been contacted for clarification, and possible results, but we have received no response.
We will assess these studies further during subsequent review updates. See Characteristics of ongoing studies.
Included studies
There are no studies with sufficient available information to include
Excluded studies
We excluded 12 studies, upon inspection of the full text, for the following reasons.
-
2 studies were excluded because they did not meet the review study design
-
1 single arm (NCT02724072)
-
1 registry (NCT01500395)
-
-
3 studies were excluded because they did not meet the review intervention
-
3 endovascular (NCT00583817; NCT02201589; NCT03322033)
-
-
5 were excluded because they did not meet the review indication
-
4 Stanford type B dissection (NCT00526487; NCT01568320; NCT02094300; NCT02464943)
-
1 abdominal aortic aneurysm (NCT01704391)
-
-
1 study was excluded because the specific population could not be extracted, due to the type and extent of the lesion (Tsukui 2002)
-
1 study was excluded because it was withdrawn (NCT01107366)
We identified duplicate publications for two excluded studies (NCT02201589; NCT03322033) and three ongoing studies (ChiCTR‐IPR‐16009372; ChiCTR‐TRC‐11001828; ChiCTR‐TRC‐13003857).
A list of excluded studies and the reasons for exclusion are detailed in the Characteristics of excluded studies table.
Risk of bias in included studies
It was not possible to assess the risks of bias due to lack of included studies.
Effects of interventions
It was not possible to study the effect of hybrid repair versus conventional open repair for aortic arch dissection due to lack of included studies.
Discussion
Summary of main results
Patients with acute type A aortic dissection who are left untreated have a mortality rate of approximately 1% per hour, which increases dramatically to 90% within 30 days (Hagan 2000). Surgery of the ascending aorta and aortic arch is particularly complex in nature, owing to the need for patients to undergo either cardiopulmonary bypass, hypothermic circulatory arrest or selective perfusion in order to maintain blood flow to the brain and body during the procedure. These patients may also have significant progression of their disease into the thoracic aorta, meaning a return for secondary operation. The advent of stented grafts to replace conventional fabric grafts has allowed hybrid procedures to now be performed in one single operation, which treats not only the ascending/aortic arch dissection, but also treats further extensive thoracic dissection or potential for further dissection in the form of re‐entry tears. Hybrid surgery also gives an option for patients who were previously deemed unfit to undergo conventional open surgery.
This review demonstrates that while we found three RCTs meeting the inclusion criteria, there was a lack of study data as one RCT is ongoing and two RCTs are unpublished. We therefore could not assess the comparison between hybrid and conventional open repair for aortic arch dissection, for dissection‐related and all‐cause mortality, or for adverse complications. A review of the literature revealed a general lack of RCTs and CCTs, often in favour of prospective single‐arm or observational studies. Aortic arch dissection is relatively new in nature. This further reduces the ability of investigators to perform RCTs and CCTs without compromising overall treatment of the patient. Patients can be randomised to a specific treatment arm that may be otherwise clinically unsuitable. However, although RCTs will be challenging in this area, they are not unrealistic and there is precedent for RCTs in the setting of aortic rupture, such as the UK Improve trial (IMPROVE 2015). They will need to be confined to high‐volume centres that have both open and endovascular expertise to hand. There are well‐established aortic teams at many centres of excellence around the world, and in Europe these teams are encouraged to work together on aortic arch disease as specified in the consensus statement jointly published by the European Association for Cardio‐Thoracic Surgery (EACTS) and the European Society for Vascular Surgery (ESVS) (Czerny 2019).
Overall completeness and applicability of evidence
Overall completeness and applicability of the evidence comparing hybrid and conventional open repair for aortic arch dissection, with relation to dissection‐related and all‐cause mortality, and adverse complications could not be assessed, as we identified no studies for inclusion.
Quality of the evidence
It was not possible to review methodological quality or the certainty of the evidence in the absence of study data for those eligible for inclusion in the review.
Potential biases in the review process
The Cochrane Vascular Information Specialised performed a comprehensive search of the literature and we selected studies according to the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2011). Two review authors (EPK and AE) independently assessed studies for potential inclusion (Figure 1). We resolved any disagreements by discussion, and included the third review author (NH) where necessary.
Agreements and disagreements with other studies or reviews
Data could not be gathered from the three studies identified according to the inclusion criteria (ChiCTR‐TRC‐11001828; ChiCTR‐TRC‐13003857; ChiCTR‐IPR‐16009372). One of these studies, ChiCTR‐TRC‐13003857, describes a Xuper Open Surgery Stent Graft System (Lifetech Scientific, Shenzhen, China), which is a hybrid graft consisting of three parts: a proximal polyester surgical graft, a primary stent graft with two super branches set 3 mm apart, and a delivery system. The Xuper Open Surgery Stent Graft system is used for hybrid arch repair, whereby it is anastomosed to an ascending aortic graft. The side branches from the stent graft are deployed in the left carotid and left subclavian arteries, and the innominate artery is transected and anastomosed to the ascending aortic graft. Although the results of the trial were not available, we did identify a case series of 21 patients in whom the device was used (Yu 2019). Yu 2019 reported that the system was found to be safe and effective for total arch repair in acute aortic dissection with an in‐hospital mortality rate of 4.8% and no need for a re‐intervention at an average follow‐up time of 35.2 ± 2.1 months (range 15 to 42 months).
We found two systematic reviews, which illustrate the current trends for treatment of aortic arch dissection (Mussa 2016; Smith 2017). These are not pertinent to our conclusions, but provide additional information to the reader.
A systematic review which included 82 studies (2 RCTs and 80 observational) (Mussa 2016), reviewed the current evidence relating to diagnosis and treatment of acute aortic syndromes. It should be noted that the two RCTs included in this systematic review evaluated acute and chronic uncomplicated descending aortic dissection. Available data suggested that open surgical repair is optimal for treating Stanford type A (ascending aorta). Thirty‐day mortality for people treated with open surgery was 13% to 17%. The authors also concluded that there is a significant lack of RCTs relating to acute aortic syndromes. While evidence shows there have not been any RCTs or CCTs carried out that compare hybrid repair to conventional open surgical repair for aortic arch dissection, the overall clinical status of the patient, as well as the presence of preoperative complications, often dictates the decision to intervene surgically or to use medical management.
Similarly, a systematic review and meta‐analysis of 'extended' or hybrid arch repair for acute Stanford type A dissection carried out on literature between 1946 and August 2015 found no RCTs have been conducted on this topic (Smith 2017). The study compiled demographics and outcomes on a number of hybrid surgeries, including:
-
total arch replacement ± standard elephant trunk without descending thoracic aortic stent grafting;
-
total arch replacement and descending thoracic aortic stent grafting with frozen stent graft placed under circulatory arrest;
-
hemi‐arch replacement and descending thoracic aortic stent grafting with the stent graft placed under circulatory arrest; and
-
total arch replacement with stent graft placed after coming off cardiopulmonary bypass and with the use of fluoroscopy to identify landing zones.
This review of the literature by Smith and colleagues revealed 38 studies, which included 2140 participants who had an extended/hybrid arch repair as defined above. Overall hospital mortality was 8.6% (95% CI 7.2 to 10.0), stroke rate was 5.7% (95% CI 3.6 to 8.2) and spinal cord ischaemia rate was 2.0% (95% CI 1.2 to 3.0) (Smith 2017). Although the purpose of the review by Smith 2017 was not to compare the hybrid surgical techniques, it is still interesting to note the breakdown between groups. Hospital mortality was 11.9 % (95% CI 7.0 to 17.8), 8.6% (95% CI 7.0 to 10.2), 6.3% (95% CI 4.5 to 8.3 and 5.5% (95% CI 3.3 to 8.3), respectively. Stroke rate was 7.7% (95% CI 4.9 to 10.8), 3.7% (95% CI 2.1 to 5.7), 3.0% (95% CI 1.5 to 5.0) and 1% (95% CI 0.0 to 0.1), respectively, and spinal cord ischaemia rate was 1.6% (95% CI 0.1 to 4.3), 1.95% (95% CI 1.04 to 3.12), 2.9% (95% CI 0.8 to 6.4) and 1% (95% CI 0.0 to 0.1), respectively. It is interesting to consider that the highest death and stroke rates occurred with conventional repair, and that using stent grafts in the descending thoracic aorta reduced these complications without an increase in spinal cord ischaemia rates. Of note, the procedure which theoretically should reduce spinal cord ischaemia by reducing manipulation and coverage of the subclavian arteries, was actually associated with a higher spinal cord ischaemia rate. There are of course many confounding factors, such as stent graft length or patient haemodynamic stability which are not taken into account.
Given the lack of RCTs or CCTs comparing open to hybrid repair for aortic arch dissection, the International Registry of Acute Aortic Dissections (IRAD) was established in 1996 to assess the aetiological factors, modes of presentation, clinical features, treatment, and hospital outcomes of people with acute aortic dissection from around the world. IRAD is a consortium of research centres and currently has 30 large referral centres in 11 countries participating in the registry. Information such as dates and times of symptom onset, presentation, diagnosis, haemodynamic signs of aortic dissection, initial and chronic medical therapy, diagnostic imaging chosen, and surgical and medical management is being studied. IRAD investigators echo other studies and conclude that extensive versus conservative (i.e. open versus hybrid) surgical management of aortic arch dissection should be determined case‐by‐case, and on the basis of the clinical status of the patient, their specific aortic anatomy, i.e. anatomy of great vessels and location of entry and re‐entry tears, and the specific experience of the operator (Di Eusanio 2014). A review of the IRAD data demonstrated a mortality of 25.1%, with a higher mortality in those classified as unstable (Trimarchi 2005). The authors concluded that risk factors associated with Stanford type A aortic dissection will considerably alter the treatment outcome, rather than the choice of treatment alone.
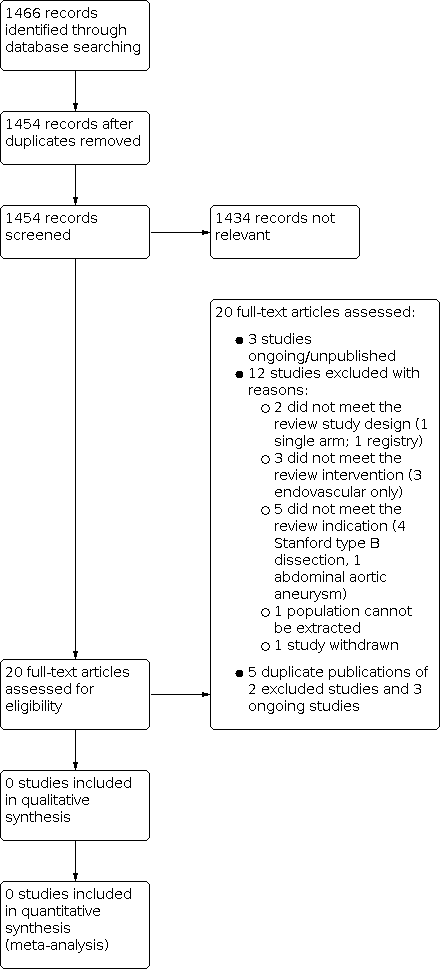
Study flow diagram.
| Types of outcome measures | Defined by | Including |
|---|---|---|
| Primary outcomes | ||
| Mortality | Dissection related and all causes | (Grade V) All deaths at 30 days and 12 months |
| Neurological deficit | Global events | (Grade I ‐ IV) Postoperative agitation, delirium, obtundation, or myoclonic movements, without localised cerebral neurological signs |
| Focal events | (Grade I ‐ IV) Lateralising sensory or motor deficit or focal seizure activity | |
| Spinal neurological events | (Grade I ‐ IV) Paraplegia, paraparesis | |
| Cardiac injury | Myocardial ischaemia | (Grade I ‐ IV) |
| Low cardiac output syndrome | (Grade I ‐ IV) | |
| Arrhythmia | (Grade I ‐ IV) | |
| Pericardial effusion | (Grade I ‐ IV) | |
| Respiratory compromise | Parenchymal complications | (Grade I ‐ IV) Atelectasis, pneumonia, pulmonary oedema, and acute respiratory distress syndrome |
| Pleural complications | (Grade I ‐ IV) Pneumothorax, pleural effusion | |
| Renal ischaemia | Modified RIFLE classification (Bellomo 2004): Risk (I), Injury (II), Failure (III), Loss/End‐Stage Kidney Dysfunction (IV) | (Grade I ‐ IV) Serum creatinine increase, glomerular filtration rate (GFR) decrease, anuria, haemodialysis |
| Secondary outcomes | ||
| False lumen thrombosis | Partial or complete thrombosis | ‐ |
| Mesenteric ischaemia | Gut complications | (Grade I ‐ IV) Ileus or gastric paresis, gut ischaemia manifested as metabolic acidosis or increased lactate |
| Grades as defined by Yan 2014: Grade I: any deviation from the normal postoperative course but self‐limiting or requiring simple therapeutic regimens (including antiemetics, antipyretics, analgesics, electrolytes, and physiotherapy); Grade II: complications requiring pharmacological treatment for resolution; Grade III: complications requiring surgical, endoscopic, or radiological intervention but not requiring regional or general anaesthesia or requiring interdisciplinary intervention; Grade IV: complications requiring surgical, endoscopic, or radiological intervention under regional or general anaesthesia, or requiring new intensive care unit (ICU) admission or ongoing ICU management for > 7 days or hospitalisation for > 30 days, or causing secondary organ failure; Grade V: death caused by a complication. | ||
| Summary of findings for the main comparison: Hybrid repair versus conventional open repair for aortic arch dissection | ||||||
| Patient or population: patients with a diagnosis of aortic arch dissection Settings: hospital Intervention: hybrid repair Comparison: open repair | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with open repair | Risk with hybrid repair | |||||
| Mortality, Follow‐up: median N (months) | Study population | HR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| Neurological deficit, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| Cardiac injury, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| Respiratory compromise, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| Renal ischaemia, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| False lumen thrombosis, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| Mesenteric ischaemia, Follow‐up: median N (months) | Study population | RR N (N to N) | N | ⊕⊝⊝⊝ ⊕⊕⊝⊝ ⊕⊕⊕⊝ ⊕⊕⊕⊕ | ||
| N per 1000 | N per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||

