Protease activity as a prognostic factor for wound healing in venous leg ulcers
Referencias
Additional references
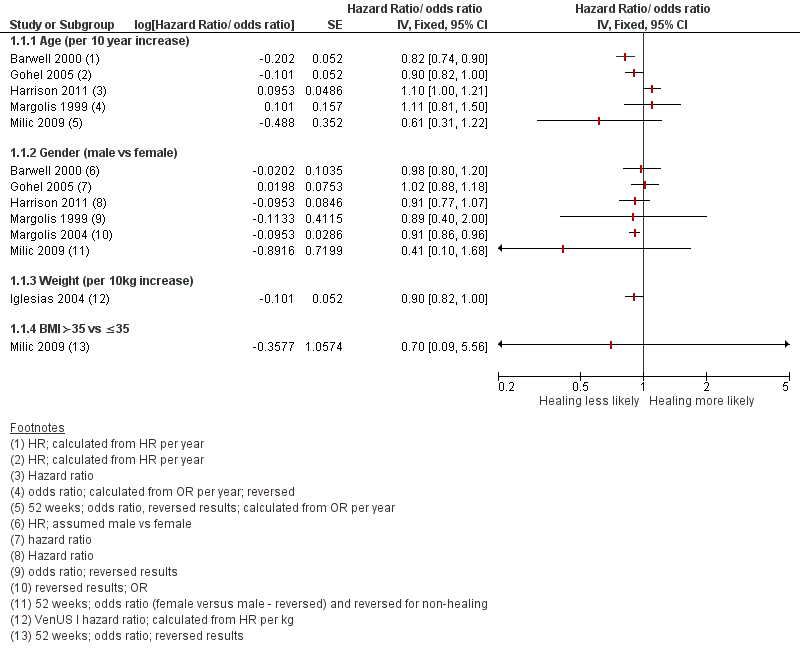
Prognostic factors for healing VLUs: person characteristics

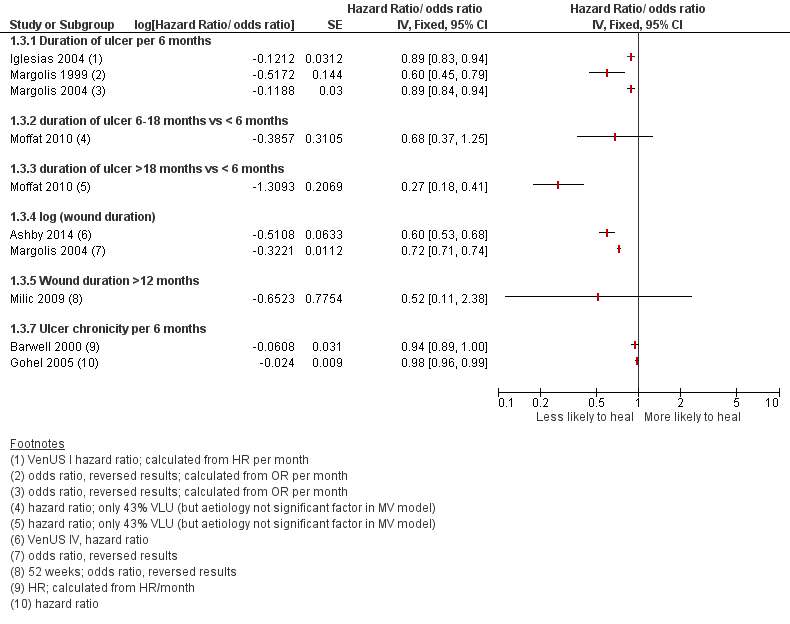
Prognostic factors for VLU healing: wound characteristics 1
Prognostic factors for VLU healing: wound characteristics 2

Prognostic factors for VLU healing: number of ulcers
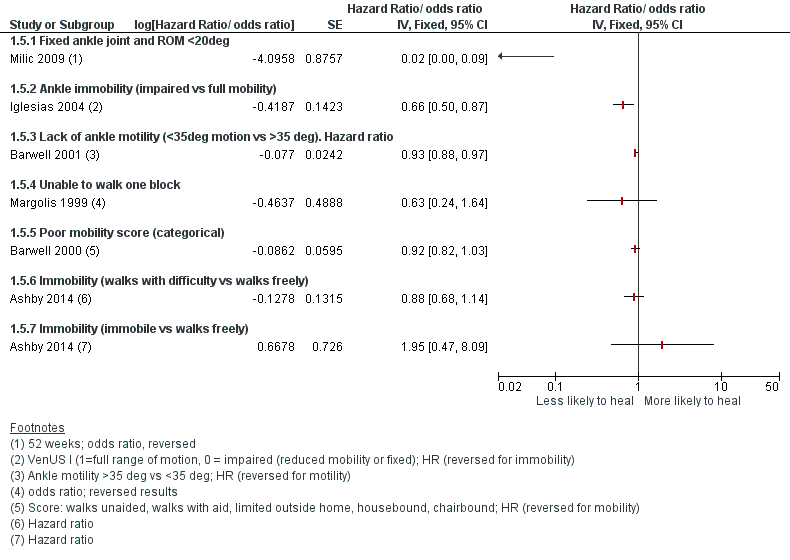
Prognostic factors for VLU healing: mobility and ankle flexion

Prognostic factors for VLU healing: bacteria and infection

