Pronóstico global de los diagnósticos de trastorno del espectro autista en edad preescolar
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 192 (84) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: retrospective | |
| Population | Sample size (% male): 152 (82) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 147 (80) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 70 (83) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 18 (72) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 35 (89) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: retrospective, with whole cohort considered | |
| Population | Sample size (% male): 12 (75) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 13 (77) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 14 (66). Note, data were only provided for the full sample (n = 39), which includes children without ASD. | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 43 (80) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 23 (78) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 67 (82) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: retrospective | |
| Population | Sample size (% male): 59 (81) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 17 (71) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 25 (68) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 60 (87) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 30 (73) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 27 (81.5) | |
| Notes | Conflict of interest: the author(s) declared no potential COI with respect to the research, authorship, and/or publication of the article. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 219 (81) | |
| Notes | Conflict of interest: Deborah Fein is part owner of M‐CHAT‐R, LLC, which receives royalties from companies that incorporate the M‐CHAT‐R into commercial products and charge for its use. Data reported in the current paper are from the freely available paper versions of the M‐CHAT and M‐CHAT‐R. Alexander Hinnebusch and Lauren Miller declared that they had no COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 100 (84) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 70 (89) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 24 (79) ASD poor and 36 (78) ASD good | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 77 (83) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: retrospective with whole cohort considered | |
| Population | Sample size (% male): 52 (82‐85) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: retrospective | |
| Population | Sample size (% male): 19 (80) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 35 (91) | |
| Notes | Conflict of interest: not reported. This was a publication of a PhD thesis. There was no information included in the paper about COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 15 (100) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 26 (88) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 79 (ND) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 37 (ND) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: retrospective | |
| Population | Sample size (% male): 37 (86) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 32 (66) | |
| Notes | Conflict of interest: the author(s) declared the following potential COI with respect to the research, authorship, and/or publication of this article: Amélie Terroux declared to be an employee of the Centre de réadaptation en déficience intellectuelle et troubles envahissant du développement de la Montérégie‐Est. Marjorie Morin and Céline Mercier were also under contract for the same agency for the duration of the study. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 60 (100) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: not described | |
| Population | Sample size (% male): 98 (‐) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 11 (ND) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 19 (84) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 28 (79) | |
| Notes | Conflict of interest: not reported (Masters thesis) | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 55 (84) | |
| Notes | Conflict of interest: Small Business Innovation Research (SBIR) grants, sponsored by the NIMH, are administered through business entities to support research in technological innovation and dissemination. Therefore, all SBIR principle investigators if they are directly involved in the grant have a financial conflict of interest. R Solomon, the principle investigator of the study, was involved in the design of the study, wrote the first draft of the manuscript and was involved in the decision to submit the article. To limit his bias, R Solomon was assiduously excluded from evaluation of outcomes, data collection, or data analysis, all of which were done independently at MichiganState University under the auspices of LA Van Egeren, a senior level researcher and director of the Community Evaluation and Research Collaborative. The only involvement with data occurred when the data collected at Easter Seals sites were identified at the “central office” in Ann Arbor and sent on to Michigan State University for analysis. R Solomon received no other funds outside of the grant (such as honoraria, consultant fees, etc.) before or during the grant. G Mahoney received a fee for consulting as an original part of the grant protocol. The remaining authors declared no COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 102 (80) | |
| Notes | Conflict of interest: Drs Solomon, Iosif, Reinhardt, Libero, Nordahl, Ozon‐off, and Rogers reported no biomedical financial interests or conflicts of interest. Dr Amaral is on the Scientific Advisory Board of Stemina Biomaker Discovery and Axial Biotherapeutics. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 71 (79) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 75 (83) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 272 (86) | |
| Notes | Conflict of interest: Dr Szatmari reported receiving grants from Canadian Institutes of Health Research (CIHR) during the conduct of this study. Dr Cost reported receiving grants from the CIHR during the conduct of the study. Dr Bennett reported receiving grants from CIHR and grants from Hamilton Health Sciences Foundation during the conduct of the study; and grants from Hamilton Health Sciences and Brain Canada outside the submitted work. Dr Smith reported receiving grants from the Centre for Addiction and Mental Health/CIHR as 1 of 5 study site principle investigators during the conduct of the study. Dr Zwaigenbaum reported receiving personal fees from Roche as a data monitoring board member outside the submitted work. No other disclosures were reported. | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 126 (81) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: retrospective | |
| Population | Sample size (% male): 69 (79) | |
| Notes | Conflict of interest: not reported (thesis) | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 129 (87) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: retrospective | |
| Population | Sample size (% male): 8564 (83) | |
| Notes | Conflict of interest: the authors declared they have no COI. | |
| Study characteristics | ||
| Methods | Design: retrospective, with whole cohort considered | |
| Population | Sample size (% male): 15 (87) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: retrospective | |
| Population | Sample size (% male): 534 (84) | |
| Notes | Conflict of interest: not reported | |
| Study characteristics | ||
| Methods | Design: prospective | |
| Population | Sample size (% male): 23 (69) | |
| Notes | Conflict of interest: Dr Zwaigenbaum was supported by the Stollery Children’s Hospital Foundation Chair in Autism Research. Drs Bryson and Smith were supported by the Jack and Joan Craig Chair in Autism Research, Dr Szatmari was supported by the Chedoke Health Chair in Child Psychiatry, and Dr Vaillancourt was supported by a Canada Research Chair in Children’s Mental Health and Violence Protection. | |
Mean scores (IQ, adaptive behaviour or language) for the cohort is < 70 or more than 70% are less than 70. If cohort evenly spread this is signified 'both'.
AD: autistic disorder; ADOS: Autism Diagnostic Observation Schedule; ADI: Autism Diagnostic Interview;ASD: autism spectrum disorder; CARS: Childhood Autism Rating Scale; COI: conflict of interest; DSM: Diagnostic Statistical Manual of Mental Disorders;ICD: International Classification of Diseases; IQ: intelligence quotient ;N: no, not multidisciplinary; NIH: National Institutes of Health; PDD‐NOS: pervasive developmental disorder; PI: principal investigator; RCT: randomised controlled trial; U: unclear; Y: yes, multidisciplinary; ‐: not reported by study
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Study only followed up those children who had consistent diagnosis at two time points and excluded those who moved off spectrum. Unable to obtain information on numbers that moved off spectrum from study authors. | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up. | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| No baseline diagnostic assessment | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Sample only included those diagnosed at baseline and follow‐up therefore unable to determine how many may have lost diagnosis at follow‐up. | |
| Did not use same diagnostic methods/tools at baseline and follow‐up | |
| Did not use same diagnostic methods/tools at baseline and follow‐up |
Characteristics of studies awaiting classification [ordered by study ID]
| Notes | Conference abstract. May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | Conference abstract. May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | Conference abstract. Appears to meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | Appears to meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | Conference abstract. Appears to meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | Conference abstract. May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. Appears to have overlapping participants with Millikovsky‐Ayalon 2012 which is also awaiting classification. |
| Notes | Conference abstract. May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | Conference abstract. May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | Dissertation. We requested a copy of the paper from numerous libraries, but given the date of the thesis, which is in hard copy (no digital copy), we were unable to access the full thesis. |
| Notes | Study is in Hebrew. We contacted the authors for further information (an email was written to the authors in Hebrew) but we did not receive any response. |
| Notes | Conference abstract. May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | Insufficient data to accurately classify as included or excluded. Contacted study authors for further data but did not receive a response |
| Notes | Study is in Italian. We had this article translated from Italian but require further information from the study authors to determine whether the study is eligible for inclusion. We emailed the authors and are awaiting a response. |
| Notes | May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | Study is in Italian. Article was translated in Italian but further information was required from the authors to determine whether the study was eligible for inclusion. We emailed the authors and are awaiting a response. Participants may overlap with Muratori 2002 |
| Notes | Study meets eligibility criteria, however it may include the same participants as another included study by the same authorship group (Malhi 2011). We contacted the study authors several times to confirm whether the participants were the same/overlapping but did not receive a response. |
| Notes | May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |
| Notes | Conference abstract. May meet eligibility criteria. We attempted to obtain the full text through multiple sources and contacted the study authors but were unable to confirm eligibility for inclusion or obtain data. |

Study flow diagram.
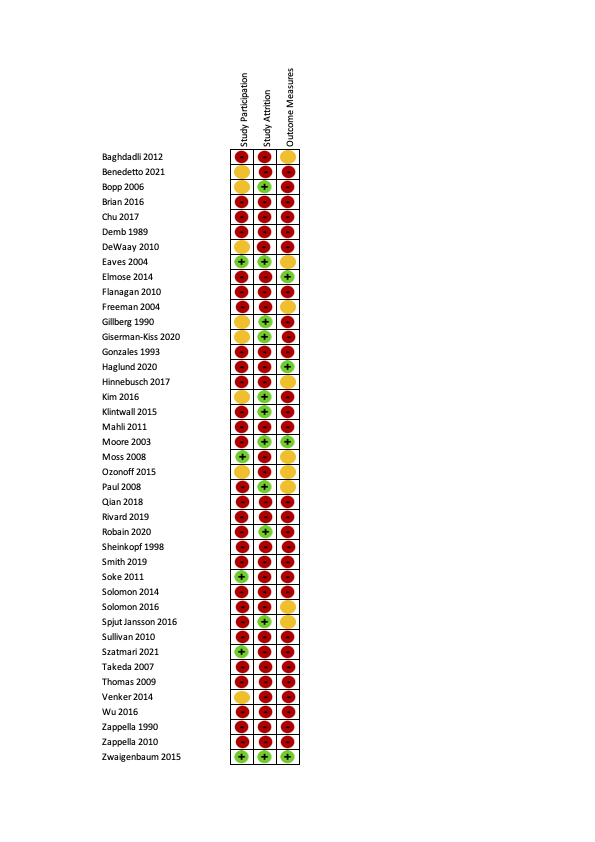
Risk of bias ratings on the QUIPS tool (40 studies). Green is low risk of bias, orange is moderate risk of bias and red is high risk of bias.
Summary risk of bias ratings for provided for each QUIPS domain (i.e.study participation, study attrition, outcome measurement). See Appendix 9 for a figure showing all criteria that were rated for each domain. Studies were rated to have an overall low risk of bias if all three summary domains were rated low or moderate risk of bias. Studies were rated to have an overall high risk of bias if all three summary domains were rated low or moderate risk of bias.

Risk of bias graph: review authors' judgements about each risk of bias item for each included study presented as percentages across all included studies (41 studies).

Risk of bias ratings for each included study for each of the 18 criteria. Red indicates high, orange indicates moderate, green indicates low and yellow indicates unclear risk of bias.

Forest plot of proportion of children that retained their autism diagnosis
Footnote
CI: confidence interval; ES: effect size; N: number in sample

Age at baseline: < 2 years; 2 to 3 years; 4 to 6 years; 7 to 12; years; 13 to 17 years
Footnote
CI: confidence interval; ES: effect size; N: number in sample
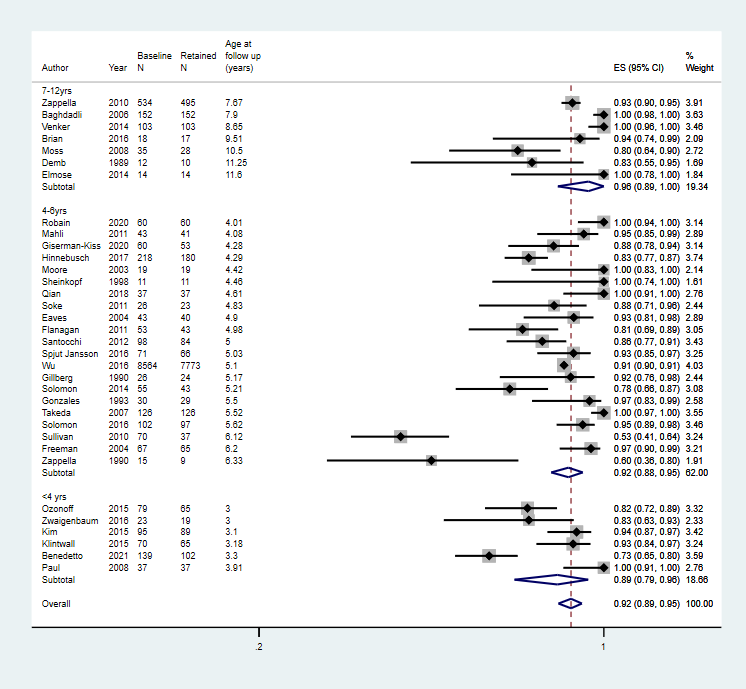
Age at follow up: 2 to 3 years; 4 to 6 years; 7 to 12 years; 13 to 18 years
Footnote
CI: confidence interval; ES: effect size; N: number in sample

Duration of follow‐up: short‐term (up to 2 years), medium‐term (2 to 5 years), and long‐term (6 to 17 years) follow‐up
Footnote
CI: confidence interval; ES: effect size; N: number in sample
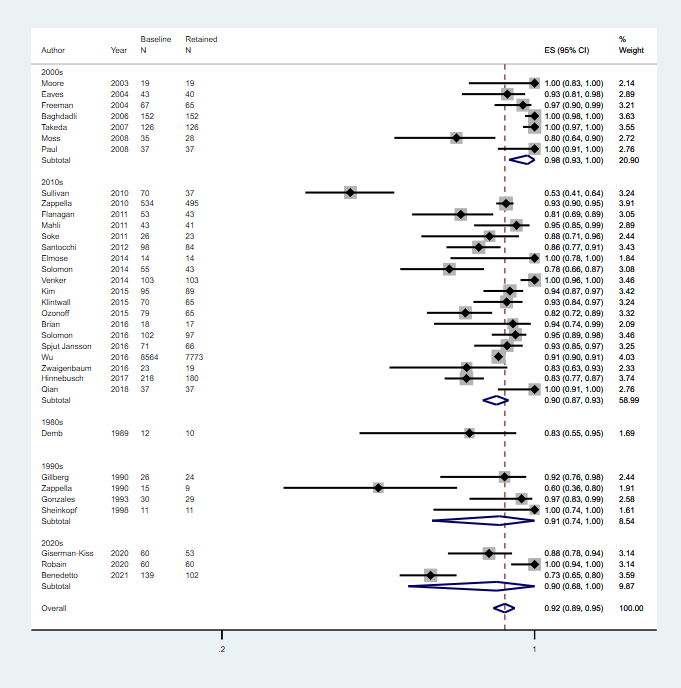
Decade of publication: 1960 to 1969; 1970 to 1979; 1980 to 1989; 1990 to 1999; 2000 to 2009; 2010 to 2019
Footnote
CI: confidence interval; ES: effect size; N: number in sample
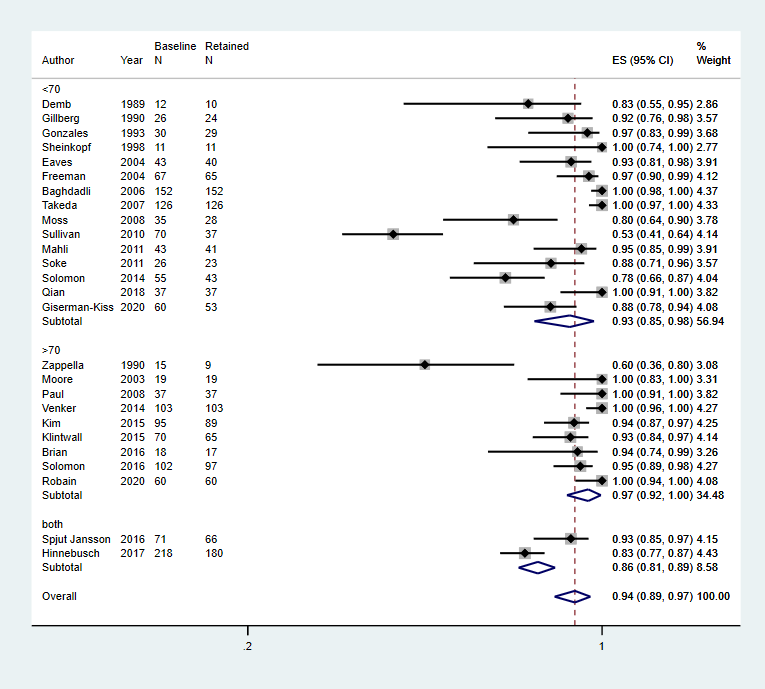
Intelligence: mean IQ 70; mean IQ > 70; or more than 70% of the cohort has IQ 70
Footnote
CI: confidence interval; ES: effect size; IQ: intelligence quotient; N: number in sample

Language: > 70% verbal; > 70% non‐verbal (i.e. use < 15 words); mean standardised language score < 70; mean standardised language score 70; or > 70% of the cohort has mean language score < 70
Footnote
CI: confidence interval; ES: effect size; N: number in sample

Adaptive behaviour: mean standard score 70; mean standard score > 70; or > 70% of the cohort has mean standard score 70
Footnote
CI: confidence interval; ES: effect size; N: number in sample
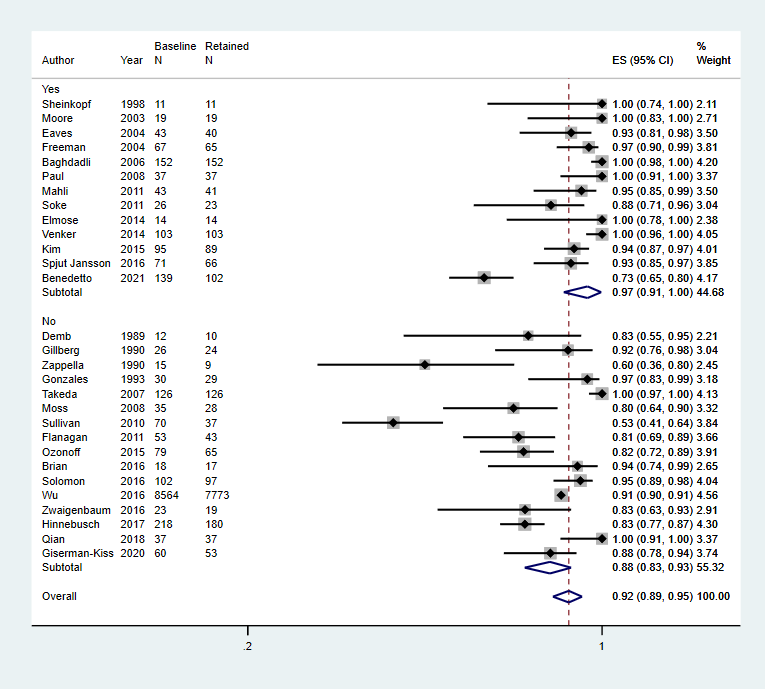
Multidisciplinary team used for diagnosis, Yes or No
Footnote
CI: confidence interval; ES: effect size; N: number in sample
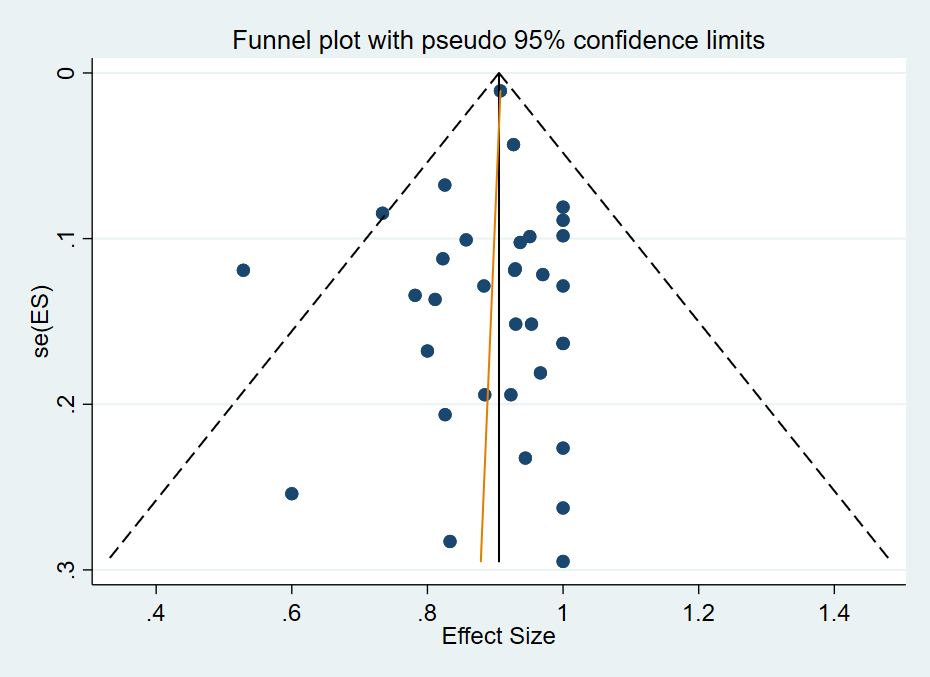
Funnel Plot of included studies
| Proportion of individuals who have a diagnosis of autism spectrum disorder at baseline and continue not meet diagnostic criteria at follow‐up one or more years later | ||||
| Patient or population: children diagnosed with autism spectrum disorder Settings: range of settings | ||||
| Outcomes | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence | Comments |
|---|---|---|---|---|
| Proportion with an autism spectrum disorder diagnosis at baseline and follow‐up Follow‐up: > 12 months | 0.92 (0.89 to 0.95) | 11,105 (34 studies: 1 intervention trial with 1 arm; 1 RCTa; 2 non‐RCTsa; 30 TAU or in the community) | ⊕⊕⊝⊝ Lowb,c | Limitations (ROB): seriousb Inconsistency: seriousc Indirectness: not serious Imprecision: not serious Publication/reporting bias: not serious Effect size: N/A Dose response gradient: N/A Confirmatory evidence: N/A See footnotes below. |
| Social communication at baseline and follow‐up (mean score) Follow‐up: > 12 months | See comments | None of the included studies provided separate domain scores at baseline and follow‐up | ||
| Restricted and repetitive behaviours and interests at baseline and follow‐up (mean score) Follow‐up: > 12 months | See comments | None of the included studies provided separate domain scores at baseline and follow‐up | ||
| Defnitions of levels of evidence High: We are very confident that the true prognosis (probability of future events) lies close to that of the estimate Moderate: We are moderately confident that the true prognosis (probability of future events) is likely to be close to the estimate, but there is a possibility that it is substantially different Low: Our confidence in the estimate is limited: the true prognosis (probability of future events) may be substantially different from the estimate Very low: We have very little confidence in the estimate: the true prognosis (probability of future events) is likely to be substantially different from the estimate
CI: Confidence intervals;N/A: Not applicable;RCT(s): Randomised controlled trial(s);ROB: Risk of bias; TAU: Treatment as usual. | ||||
| aData were taken from the control arm of the study | ||||
| Year published | Classification system | Subgroups (as specified in the classification system) |
|---|---|---|
| 1975 | International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM) | Autistic disorder |
| 1980 | Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM‐III) | PDD: infantile autism, childhood onset PDD and atypical PDD |
| 1987 | Diagnostic and Statistical Manual of Mental Disorders, Third Edition, Revised (DSM‐III‐R) | PDD: autistic disorder, PDD‐not otherwise specified (PDD‐NOS) |
| 1994 to 2000 | Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM‐IV) | Asperger’s disorder, autistic disorder, PDD‐NOS |
| 1996 | International Classification of Diseases, Tenth Revision (ICD‐10) | Childhood autism, Asperger's syndrome, atypical autism, pervasive developmental disorder (PDD) ‐ unspecified |
| 2000 to 2013 | Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM‐IV‐TR) | Asperger’s disorder, autistic disorder, PDD‐NOS |
| 2013 to current | Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5) | Autism spectrum disorder |
| 2018 | International Classification of Diseases, Eleventh Revision (ICD‐11) | Autism spectrum disorder |
| PDD‐NOS: pervasive developmental disorder | ||
| Primary publication | Additional publications from the same study |
|---|---|
| Anderson 2007, Bedford 2016, Gotham 2012, Gotham 2011, Hus 2011, Lord 1995, Lord 2004, Lord 2012, Luyster 2007, Pickles 2014, Richler 2010, Thurm 2007 | |
| Baghdadli 2018, Baghdadli 2008, Baghdadli 2007, Darrou 2010, Pry 2011, Pry 2012 | |
| Bopp 2009; Smith 2007 | |
| Flanagan 2012 | |
| Giserman‐Kiss 2018 | |
| Magiati 2007, Magiati 2011a, Magiati 2011b | |
| Ke 2017, Li 2019 | |
| Mello 2018 | |
| Mahoney 2016 | |
| Solomon 2018, Waizbard‐Bartov 2021 | |
| Baribeau 2020, Baribeau 2021, Courchesne 2021, Bennett 2014, Bennett 2015, Georgiades 2014, Georgiades 2021, Szatmari 2015 | |
| Ellis‐Weismer 2015, Davidson 2017, Ray‐Subramanian 2012, Venker 2016 | |
| aMet inclusion criteria but unable to extract data for synthesis as children without a diagnosis of autism spectrum disorder were also included in the cohort. Authors were contacted but we were unable to obtain required data. | |
| Study | Diagnosis type | N at baseline (% male) | IQ (mean standard score)a | Adaptive behavior (mean standard score)a | Language (mean standard score)a | Age at baseline (years) | Follow‐up duration (years) | Diagnostic tool used at baseline (multidisciplinary or not) | Proportion who met diagnostic criteria at follow‐up |
|---|---|---|---|---|---|---|---|---|---|
| ASD | 152 (82) | < 70 | < 70 | NR | 4.90 | 3.00 | ICD‐10 & CARS (Y) | 1.0 | |
| ASD | 147 (80) | NR | NR | NR | 2.3 | 1 | DSM‐5 and ADOS (Y) | 0.73 | |
| ASD | 18 (72) | > 70 | NR | > 70 | 3.15 | 6.36 | DSM‐IV‐TR & ADOS (N) | 0.94 | |
| ASD | 12 (75) | < 70 | NR | NR | 4.50 | 5.00 | DSM‐III & DSM‐III R (N) | 0.83 | |
| ASD | 43 (80) | < 70 | < 70 | NR | 2.75 | 2.25 | DSM‐IV, CARS, MDT (Y) | 0.93 | |
| ASD | 23 (78) | NR | NR | NR | 3.10 | 8.30 | ICD‐10, ADOS (Y) | 1.00 | |
| ASD | 67 (82) | NR | < 70 | NR | 3.59 | 1.38 | CARS (N) | 0.81 | |
| ASD | 59 (81) | < 70 | NR | NR | 4.00 | 2.2 | DSM IV, CARS (N) | 0.97 | |
| ASD | 25 (68) | < 70 | NR | NR | 1.13 | 4.04 | DSM‐III‐R (N) | 0.92 | |
| ASD | 60 (87) | <70 | NR | <70 | 2.31 | 1.98 | ADOS | 0.883 | |
| ASD | 30 (73) | < 70 | NR | NR | 4.50 | 1.00 | DSM‐III, DSM‐III‐R, DSM‐IV and ICD 10 (N) | 0.97 | |
| ASD | 219 (81) | Both | NR | < 70 | 2.13 | 2.16 | DSM‐IV, ADOS, CARS (N) | 0.83 | |
| ASD | 100 (84) | > 70 | Both | NR | 1.80 | 1.30 | ADOS (Y) | 0.93 | |
| ASD | 70 (89) | > 70 | > 70 | < 70 | 1.83 | 1.36 | ADOS G, ADOS T (U) | 0.93 | |
| ASD | 77 (83) | < 70 | NR | NR | 2.48 | 1.65 | CARS (Y) | 0.95 | |
| ASD | 19 (80) | > 70 | NR | < 70 | 2.83 | 1.59 | ADI‐R (Y) | 1.00 | |
| ASD | 35 (91) | < 70 | < 70 | < 70 | 3.5 | 7.00 | ADI‐R (N) | 0.80 | |
| ASD | 79 (NR) | NR | NR | NR | 2 | 1 | ADI‐R, DSM IV, best clinical estimate (N) | 0.82 | |
| ASD | 37 (NR) | > 70 | > 70 | < 70 | 1.82 | 1.09 | ADOS (Y) | 1.00 | |
| ASD | 37 (86) | <70 | NR | NR | 2.57 | 2 | DSM IV TR; CARS ADI‐R (N) | 1.00 | |
| ASD | 60 (100) | >70 | NR | NR | 3 | 1 | DSM 5 ADOS (N) | 1.00 | |
| ASD | 98 (NR) | NR | NR | NR | 3.25 | 1.75 | ADOS, CARS | 0.86 | |
| ASD | 11 (NR) | < 70 | NR | NR | 2.94 | 1.51 | DSM‐III (Y) | 1.00 | |
| AD | 28 (79) | < 70 | NR | NR | 2.75 | 2.08 | ADI‐R (Y) | 0.89 | |
| ASD | 55 (84) | < 70 | NR | NR | 4.21 | 1.00 | ADOS (U) | 0.78 | |
| ASD | 102 (80) | > 70 | Both | Both | 2.86 | 2.76 | ADOS (N) | 0.95 | |
| ASD | 71 (79) | Both | Both | NR | 3.03 | 2.00 | ADOS, DISCO, ADI‐R (Y) | 0.93 | |
| ASD | 75 (83) | < 70 | < 70 | NR | 3.94 | 2.18 | CARS (N) | 0.53 | |
| ASD | 126 (81) | < 70 | NR | NR | 2.62 | 2.90 | ICD‐10, CARS (N) | 1.00 | |
| ASD | 129 (87) | > 70 | > 70 | Both | 2.80 | 5.85 | DSM‐IV, ADOS (Y) | 1.00 | |
| ASD | 8564 (83) | NR | NR | NR | 3.67 | 1.43 | DSM‐IV‐TR file record review (N) | 0.91 | |
| AD | 15 (87) | > 70 | Both | NR | 4.50 | 1.83 | DSM‐III (N) | 0.60 | |
| ASD | 534 (84) | NR | NR | NR | 5.00 | 2.67 | DSM‐IV‐TR (U) | 0.93 | |
| ASD | 23 (69) | NR | > 70 | NR | 1.50 | 1.50 | DSM‐IV‐TR (N) | 0.83 | |
| aMean score (IQ, adaptive behaviour or language) for the cohort is < 70 or more than 70% are less than 70. If cohort evenly spread this is signified 'both'. AD: autistic disorder; ADI: Autism Diagnostic Interview;ADOS: Autism Diagnostic Observation Schedule; ASD: autism spectrum disorder; CARS: Childhood Autism Rating Scale; DISCO: Diagnostic Interview for Social and Communication Disorders; DSM: Diagnostic Statistical Manual of Mental Disorders; ICD: International Classification of Diseases; IQ: intelligence quotient; N: no; NR: not reported; PDD‐NOS: pervasive developmental disorder‐ not otherwise specified; U: unclear; Y: yes. | |||||||||
| Domain | Relative effect (95% CIs) | No. of participants (studies) | I2 | |
|---|---|---|---|---|
| Age at baseline | 0 to 2 years | 0.94 (0.88 to 0.98) | 251 (5 studies) | 52.64%, P = 0.08 |
| 2 to 3 years | 0.92 (0.88 to 0.95) | 9989 (22 studies) | 90.17%, P < 0.01 | |
| 4 to 5 years | 0.91 (0.76 to 0.99) | 152 (5 studies) | 90.48%, P < 0.01 | |
| 5 to 6 years | 0.93 (0.90 to 0.95) | 534 (1 study) | ‐ | |
| Age at follow‐up | < 4 years | 0.89 (0.79 to 0.96) | 443 (6 studies) | 86.80%, P < 0.01 |
| 4 to 6 years | 0.92 (0.88 to 0.95) | 9794 (21 studies) | 87.88%, P < 0.01 | |
| 7 to 12 years | 0.96 (0.89 to 1.00) | 868 (7 studies) | 88.18%, P < 0.01 | |
| Duration of follow‐up | 1 to 2 years | 0.91 (0.88 to 0.94) | 10,745 (27 studies) | 87.86%, P < 0.01 |
| 2 to 5 years | 0.99 (0.92 to 1.00) | 293 (4 studies) | 78.16%, P < 0.01 | |
| 6 to 17 years | 0.92 (0.77 to 1.00) | 67 (3 studies) | ‐ | |
| Decade of publication | 1980 to 1989 | 0.83 (0.55 to 0.95) | 12 (1 studies) | ‐ |
| 1990 to 1999 | 0.91 (0.74 to 1.00) | 82 (4 studies) | 73.16% P = 0.01 | |
| 2000 to 2009 | 0.98 (0.93 to 1.00) | 479 (7 studies) | 80.57% P < 0.01 | |
| 2010 to 2019 | 0.90 (0.87 to 0.93) | 10,273 (19 studies) | 86.84% P < 0.01 | |
| 2020 to 2029 | 0.90 (0.68 to 1.00) | 259 (3 studies) | ‐ | |
| Intelligencea | < 70 | 0.93 (0.85 to 0.98) | 793 (15 studies) | 90.88%, P < 0.01 |
| > 70 | 0.97 (0.92 to 1.00) | 502 (9 studies) | 77.54%, P < 0.01 | |
| Both < 70 and > 70 | 0.86 (0.81, 0.89) | 289 (2 studies) | ‐ | |
| Languagea | < 70 | 0.92 (0.84 to 0.98) | 382 (6 studies) | 79.65%, P < 0.01 |
| > 70 | 0.94 (0.74 to 0.99) | 18 (1 study) | ‐ | |
| Both | 0.98 (0.96 to 1.00) | 205 (2 studies) | ‐ | |
| Adaptive behavioura | < 70 | 0.85 (0.60 to 0.99) | 300 (5 studies) | 96.33%, P < 0.01 |
| > 70 | 0.97 (0.8 to 1.00) | 233 (4 studies) | 83.28%, P < 0.01 | |
| Both | 0.91 (0.82, 0.97) | 283 (4 studies) | 73.88%, P = 0.01 | |
| Multidisciplinary assessment | Yes | 0.97 (0.91 to 1.00) | 767 (13 studies) | 87.97%, P < 0.01 |
| No | 0.88 (0.83 to 0.93) | 9468 (16 studies) | 89.46%, P < 0.01 | |
| aMean score (IQ, adaptive behaviour or language) for the cohort is < 70 or more than 70% are less than 70. If cohort was evenly spread this is signified 'both'. CI: confidence interval;I2: a statistic that describes the percentage of variation across studies; No.: number. | ||||

