Autocuidado para la bronquiectasia
Información
- DOI:
- https://doi.org/10.1002/14651858.CD012528.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 07 febrero 2018see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Vías respiratorias
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
SS, CK, DL and S Grundy drafted the protocol. For the review, CK and S Grundy selected studies for inclusion; DJWE and SS extracted data from the studies and assessed the risk of bias; SS and DJWE entered data into Review Manager 5 and performed the analyses; SS, CK, DL, SJM S Grundy and S Gudur drafted the final review. SS had overall responsibility for the review.
Sources of support
Internal sources
-
Postgraduate Medical Institute, Edge Hill University, UK.
Employer of Sally Spencer, Dave Lynes and Carol Kelly
-
Aintree University Hospitals NHS Foundation Trust, UK.
Employer of Seamus Grundy
-
Lancaster University, UK.
Employer of David JW Evans and Steve Milan
External sources
-
The authors declare that no such funding was received for this systematic review, Other.
Declarations of interest
Sally Spencer – none known
Carol Kelly – none known
Dave Lynes – none known
Seamus Grundy – none known
David Evans – none known
Stephen Milan – none known
Sharada Gudur‐ none know
Acknowledgements
We would like to the thank Cochrane Airways for their support during preparation of the review. Julia Walters was the Editor for this review and commented critically on the protocol and review. The Background and Methods sections of this review are based on a standard template used by Cochrane Airways. This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to Cochrane Airways. The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
We would like to thank Mrs Alison Clark and Mr Ian Kenworthy for their very valuable patient and parent career comments.
We also like to thank Dr Greening for providing additional information about one of the included studies.
Version history
| Published | Title | Stage | Authors | Version |
| 2018 Feb 07 | Self‐management for bronchiectasis | Review | Carol Kelly, Seamus Grundy, Dave Lynes, David JW Evans, Sharada Gudur, Stephen J Milan, Sally Spencer | |
| 2017 Jan 31 | Self‐management for non‐cystic fibrosis bronchiectasis | Protocol | Carol Kelly, Sally Spencer, Seamus Grundy, Dave Lynes, David JW Evans | |
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Aged; Humans; Middle Aged;
PICO
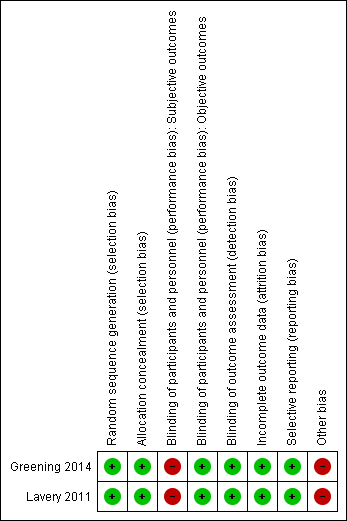
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
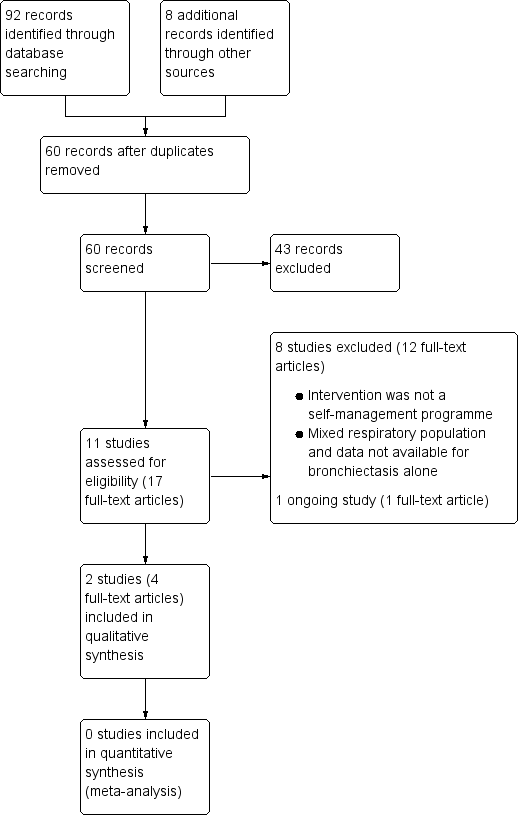
Study flow diagram

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
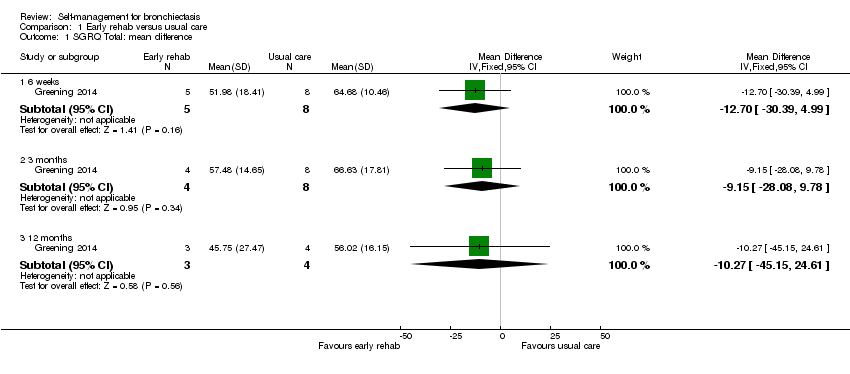
Comparison 1 Early rehab versus usual care, Outcome 1 SGRQ Total: mean difference.

Comparison 1 Early rehab versus usual care, Outcome 2 FEV1 L: mean difference.
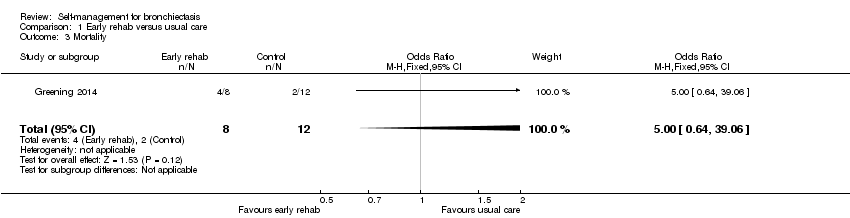
Comparison 1 Early rehab versus usual care, Outcome 3 Mortality.
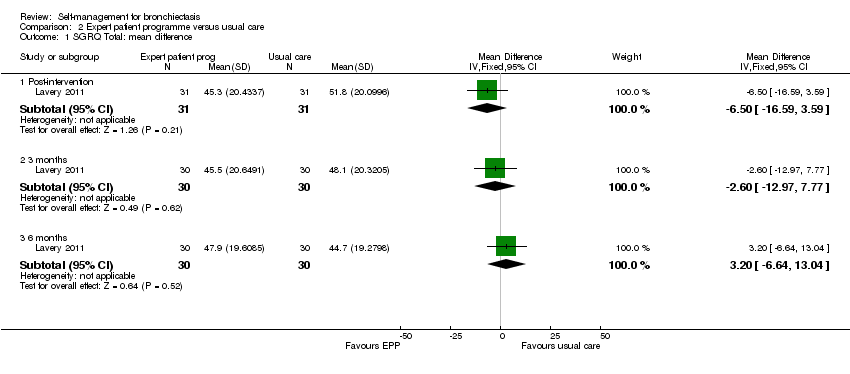
Comparison 2 Expert patient programme versus usual care, Outcome 1 SGRQ Total: mean difference.

Comparison 2 Expert patient programme versus usual care, Outcome 2 Self‐efficacy: Exercise.
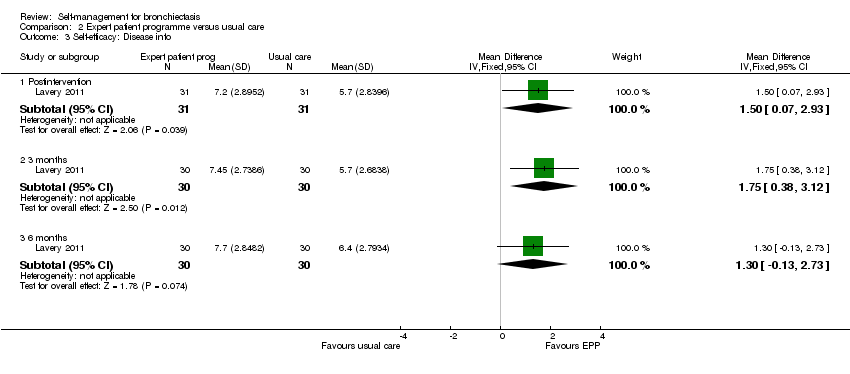
Comparison 2 Expert patient programme versus usual care, Outcome 3 Self‐efficacy: Disease info.

Comparison 2 Expert patient programme versus usual care, Outcome 4 Self‐efficacy: Obtain help.
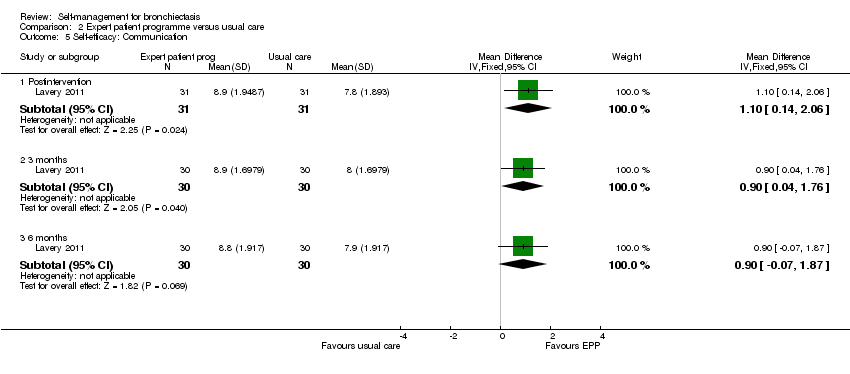
Comparison 2 Expert patient programme versus usual care, Outcome 5 Self‐efficacy: Communication.

Comparison 2 Expert patient programme versus usual care, Outcome 6 Self‐efficacy: Manage disease.

Comparison 2 Expert patient programme versus usual care, Outcome 7 Self‐efficacy: Do chores.
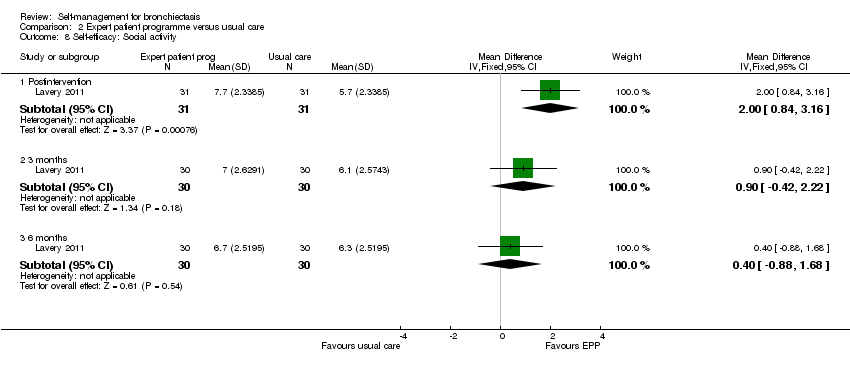
Comparison 2 Expert patient programme versus usual care, Outcome 8 Self‐efficacy: Social activity.

Comparison 2 Expert patient programme versus usual care, Outcome 9 Self‐efficacy: Manage symptoms.
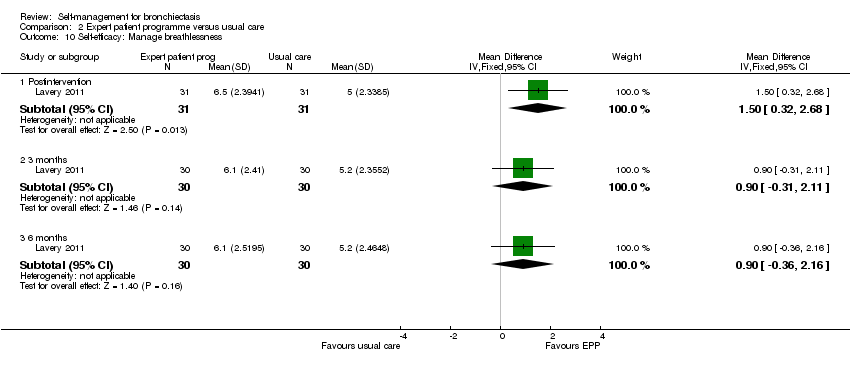
Comparison 2 Expert patient programme versus usual care, Outcome 10 Self‐efficacy: Manage breathlessness.

Comparison 2 Expert patient programme versus usual care, Outcome 11 Self‐efficacy: Manage depression.
| Self‐management compared to usual care for bronchiectasis | ||||||
| Patient or population: people with non‐cystic fibrosis bronchiectasis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with self‐management | |||||
| Health‐related quality of life | The mean health‐related quality of life was 56.02 points | MD 10.27 lower | ‐ | 20 | ⊕⊝⊝⊝ | No clear benefit or harm from self‐management (very low‐quality evidence) |
| Health‐related quality of life Follow up: range post‐intervention to 6 months | The mean health‐related quality of life was 44.7 points | MD 3.2 higher | ‐ | 60 | ⊕⊕⊝⊝ | No clear benefit or harm from self‐management |
| Exacerbations requiring antibiotics | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| Serious adverse events: mortality | ‐ | ‐ | not estimable | 20 | ||
| Hospital admissions (number admitted at least once) | ‐ | ‐ | not estimable | 20 | ‐ | |
| Lung function assessed with: FEV1 L | The mean FEV1 was 1.03 L | MD 0.3 higher | ‐ | 20 | ⊕⊝⊝⊝ | No clear benefit or harm from self‐management |
| Self‐efficacy assessed with: CDSS Follow‐up: postintervention to 6 months | ‐ | ‐ | not estimable | 60 | ⊕⊕⊝⊝ | Six out of ten scales showed significant improvements over time with the intervention. We elected not to include all 10 scales in the table but graded the evidence based on overall quality of the study |
| Economic costs | ‐ | ‐ | ‐ | ‐ | ‐ | Not reported |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1One point deducted for the unblinded nature of the comparison. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 SGRQ Total: mean difference Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 weeks | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | ‐12.70 [‐30.39, 4.99] |
| 1.2 3 months | 1 | 12 | Mean Difference (IV, Fixed, 95% CI) | ‐9.15 [‐28.08, 9.78] |
| 1.3 12 months | 1 | 7 | Mean Difference (IV, Fixed, 95% CI) | ‐10.27 [‐45.15, 24.61] |
| 2 FEV1 L: mean difference Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Discharge | 1 | 17 | Mean Difference (IV, Fixed, 95% CI) | ‐0.13 [‐0.60, 0.34] |
| 2.2 6 weeks | 1 | 14 | Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.55, 0.69] |
| 2.3 3 months | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.55, 0.85] |
| 2.4 12 months | 1 | 8 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐1.11, 1.71] |
| 3 Mortality Show forest plot | 1 | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.64, 39.06] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 SGRQ Total: mean difference Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Post‐intervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐6.5 [‐16.59, 3.59] |
| 1.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.60 [‐12.97, 7.77] |
| 1.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 3.20 [‐6.64, 13.04] |
| 2 Self‐efficacy: Exercise Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 2.10 [0.89, 3.31] |
| 2.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [0.14, 2.66] |
| 2.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [‐0.46, 2.06] |
| 3 Self‐efficacy: Disease info Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.5 [0.07, 2.93] |
| 3.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.75 [0.38, 3.12] |
| 3.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [‐0.13, 2.73] |
| 4 Self‐efficacy: Obtain help Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.10 [0.05, 2.15] |
| 4.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [‐0.34, 1.94] |
| 4.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐0.19, 2.19] |
| 5 Self‐efficacy: Communication Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.10 [0.14, 2.06] |
| 5.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [0.04, 1.76] |
| 5.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐0.07, 1.87] |
| 6 Self‐efficacy: Manage disease Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.10 [0.17, 2.03] |
| 6.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.10 [0.27, 1.93] |
| 6.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐0.27, 1.67] |
| 7 Self‐efficacy: Do chores Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 2.0 [0.78, 3.22] |
| 7.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐0.14, 2.54] |
| 7.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐0.01, 2.41] |
| 8 Self‐efficacy: Social activity Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 2.0 [0.84, 3.16] |
| 8.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐0.42, 2.22] |
| 8.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.40 [‐0.88, 1.68] |
| 9 Self‐efficacy: Manage symptoms Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.90 [0.78, 3.02] |
| 9.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [0.13, 2.27] |
| 9.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐0.41, 1.81] |
| 10 Self‐efficacy: Manage breathlessness Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 1.5 [0.32, 2.68] |
| 10.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐0.31, 2.11] |
| 10.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐0.36, 2.16] |
| 11 Self‐efficacy: Manage depression Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 Postintervention | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | 2.0 [0.91, 3.09] |
| 11.2 3 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [0.19, 2.61] |
| 11.3 6 months | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [0.09, 2.51] |

