| 1 Mental state: 1. Clinically important change (PANSS ‐ not improved) short term Show forest plot | 1 | | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
|
| 1.1 overall | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.62, 1.07] |
| 1.2 specific ‐ negative symptoms | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.57, 0.90] |
| 1.3 specific ‐ positive symptoms | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.84, 1.38] |
| 2 Mental state: 2. Average endpoint score (various scales) short term Show forest plot | 4 | | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
|
| 2.1 overall (PANSS) | 3 | 170 | Mean Difference (IV, Fixed, 95% CI) | ‐4.69 [‐8.35, ‐1.03] |
| 2.2 specific ‐ depressive symptoms (CDS) | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐1.01, 1.21] |
| 2.3 specific ‐ depressive symptoms (HDRS) | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐1.41 [‐2.40, ‐0.42] |
| 2.4 specific ‐ negative symptoms (PANSS) | 4 | 214 | Mean Difference (IV, Fixed, 95% CI) | ‐1.15 [‐2.30, 0.01] |
| 2.5 specific ‐ positive symptoms (PANSS) | 4 | 214 | Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐1.35, 0.63] |
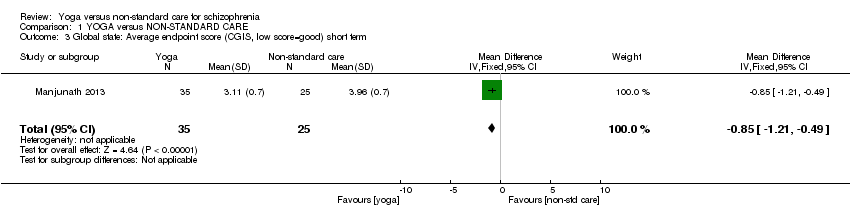
| 3 Global state: Average endpoint score (CGIS, low score=good) short term Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.85 [‐1.21, ‐0.49] |
|
| 4 Social functioning: 1. Clinically important change (SOFS ‐ not improved) short term Show forest plot | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.78, 1.04] |
|
| 5 Social functioning: 2. Average score at endpoint (two scales) Show forest plot | 1 | 88 | Mean Difference (IV, Fixed, 95% CI) | 3.20 [‐0.57, 6.97] |
|
| 5.1 SOFS, high score=good | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 3.70 [‐0.70, 8.10] |
| 5.2 Emotional recognition, TRACS, high score=good | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 1.80 [‐5.54, 9.14] |
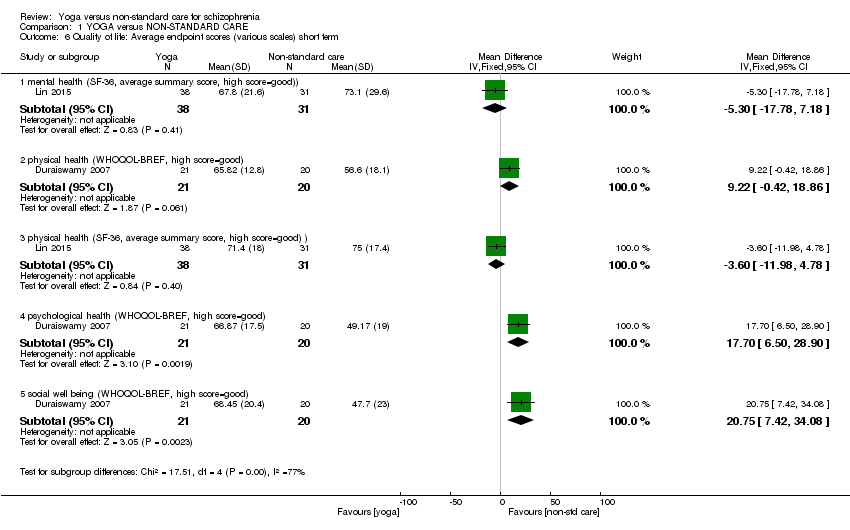
| 6 Quality of life: Average endpoint scores (various scales) short term Show forest plot | 2 | | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
|
| 6.1 mental health (SF‐36, average summary score, high score=good)) | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | ‐5.30 [‐17.78, 7.18] |
| 6.2 physical health (WHOQOL‐BREF, high score=good) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 9.22 [‐0.42, 18.86] |
| 6.3 physical health (SF‐36, average summary score, high score=good) ) | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | ‐3.60 [‐11.98, 4.78] |
| 6.4 psychological health (WHOQOL‐BREF, high score=good) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 17.70 [6.50, 28.90] |
| 6.5 social well being (WHOQOL‐BREF, high score=good) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 20.75 [7.42, 34.08] |
| 7 Adverse effects Show forest plot | 1 | | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only |
|
| 7.1 any serious | 1 | 85 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.05, 0.05] |
| 7.2 others | 1 | 85 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.05, 0.05] |
| 8 Leaving the study early ‐ short term Show forest plot | 6 | 586 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.51, 0.86] |
|