Yoga versus atención no habitual para la esquizofrenia
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (DSM IV). Exclusion criteria: any comorbid psychiatric disorder, medical or neurological illness. | |
| Interventions | 1. Yoga: Yoga training (one month) from a trained yoga instructor developed from a particular school (Swami Vivekananda Yoga Anusandhana Samsthana), followed by two months of self‐practice at home, caregivers were instructed to monitor the yoga therapy at home and keep a log of the yoga sessions practised, the techniques consisted of the following components, (i) shithileekarana vyayama (loosening exercises) for 10 minutes, (ii) asanas (yoga postures) for approximately 20 minutes) (iii) breathing exercises for 18 minutes, (iv) quick relaxation techniques for 3 minutes, meditation was not included .(n=34) 2. Exercise: one‐month exercise training from a trained yoga instructor followed by two months practice of exercises at home, ‘physical exercises’ were adopted from the National Fitness Corps*, with duration of 1 hour in total, consisted of brisk walking (10 minutes), jogging (5 minutes), exercise in standing (20 minutes), and sitting posture exercises (20 minutes), with 2‐minute breaks with a non‐specific instruction of ‘just relax now’ between different exercises, exercise in standing included 8 components consisting of moving arms and/or legs from the ‘’position: attention’’, and sitting posture exercises consisted of exercises in cross‐legged sitting, no details of caregivers instructed to monitor exercise at home, therapist:participant ratio not detailed. (n=31) 3. Wait‐list control group: in which patients did not receive any add‐on intervention. (n=26) Patients in all the three groups continued to receive stable dose of antipsychotic medications until the end of the study. | |
| Outcomes | Leaving the study early. Mental state: PANSS. Social functioning: SOFS, TRACS ‐ emotional functioning. | |
| Notes | Same yoga intervention as Duraiswamy 2007; Manjunath 2013; Varambally 2012. Included only data from intervention groups 1 and 3.Same exercise intervention as Duraiswamy 2007; Manjunath 2013; Varambally 2012. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: ''Using computer‐generated random numbers, 91 patients were allocated to three treatment groups'' Response: Low risk |
| Allocation concealment (selection bias) | High risk | Quote: ''The randomization was performed by one of the authors in the study (Dr JT)''. Response: This could potentially be high risk as the order of allocation could be known, which could influence the allocation of participants to either intervention. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants and personnel delivering the yoga intervention will be aware they are undertaking or delivering the yoga intervention. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: ''The raters were blind to the status, and the raters were not involved in imparting yoga therapy or exercise'' Response: Low risk |
| Incomplete outcome data (attrition bias) | High risk | Quote: ''The number of patients who completed the study and included in the final analysis was 27 in the Yoga group, 17 in the Exercise Group and 22 in the Waitlist group'' Response: Extent of withdrawal broadly similar between yoga and control group, but rated as high risk as not all participants randomised were included in the final analysis (7 in Yoga group, 14 in Exercise group, and 4 in Waitlist group ‐ 27.5% overall). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes were reported. |
| Other bias | High risk | Funding: not stated. One of the authors may be invested in intervention due to affiliation with Swami Vivekananda Yoga Anusandhana. Yoga for this study was developed from this school. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (DSM IV). Exclusion criteria: Prior participation in yoga study in research centre, mental ''retardation'' sufficient to impact trial understanding, presence of comorbid conditions that may worsen with exercise, neurological illnesses that may cause cognitive impairment independent of schizophrenia, presence of physical disability or illness for which yoga or physical exercise are contra‐indicted. | |
| Interventions | 1.Yoga: yoga delivered by a 'qualified instructor', programme was developed by a yoga expert and was approved by the Central Council of Research and Naturopathy, Indian Ministry of Health and Family Welfare. Consisted of chanting and breathing exercises, warming/'loosening exercises', standing postures, supine lying postures, prone lying postures, sitting postures, pranayamas (breathing exercises), jalneti (cleaning of nostrils) and prayer for 1 hour in total (every day for 21 consecutive days) with follow‐up at end training (21 days, with the exception of Sundays and bank holidays), 3 and 6 months (n=104). 2. Exercise: delivered by a trained physical exercise instructor, consisted of 15 minutes of brisk walking and 45 minutes of exercises adapted from the Ministry of Education 1965, details not supplied but was 'based' on programme adapted by Duraiswamy 2007* (n=90). Therapist: participant ratio was 1:5 for yoga and exercise, with a separate yoga and exercise instructors for these sessions. Participants advised to continue with yoga, exercise or treatment as usual ''past the training period''. 3. Control: treatment as usual, (n=92). 119 allocated to yoga group, 79 assessed at 6‐month follow‐up (33.6% dropout from initial randomisation), 104 included in final analysis, 106 allocated to exercise group overall, 71 assessed at 6 month follow‐up (38.7% dropout from initial randomisation), 90 included in final analysis. A yoga training booklet supplied to yoga group after completion of 21‐day programme. Particpants in both groups were required to maintain a compliance chart, which documented self‐practice was collected at 3 and 6 months. No adverse effects were reported for either group. Changes in prescribed doses or types of antipsychotics drugs during the study period did not change between groups. | |
| Outcomes | Leaving the study early Unable to use: Cognitive function (University of Pennsylvania Computerized Neurocognitive Battery): no total scores provided. Independent Living Skills Survey (ILSS): listed as an outcome in protocol, but no follow‐up data provided. Global assessment of function (GAF): listed as an outcome in protocol, but no follow‐up data provided. Schedule for Assessment of Negative Symptoms (SANS): listed as an outcome in protocol, but no follow‐up data provided. Schedule for Assessment of Positive Symptoms (SAPS): listed as an outcome in protocol, but no follow‐up data provided. Assessed at baseline, 3 and 6 months. | |
| Notes | *Exercise group: based on protocol devised by Duraiswamy 2007. Therefore exercise intervention also consisted with Behere 2011a; Manjunath 2013; Varambally 2012. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: ''the principal study investigator (T.B.) randomised participants to the YT, PE or TAU in blocks of 12, using an online randomisation program (http://www.randomization.com)''. Response: Low risk. |
| Allocation concealment (selection bias) | Low risk | Quote: ''the randomisation lists were stored ina password‐protected computer by TB, who did not collect outcome measures, administer any interventions or treat the participants''. Response: Low risk. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants and personnel delivering the yoga intervention will be aware they are undertaking or delivering the yoga intervention. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: ''all recruiters and raters, (who administered the cognitive evaluations) were blinded to participants allocation''. Response: Low risk. |
| Incomplete outcome data (attrition bias) | Low risk | Intention‐to‐treat analysis was employed and reasons given for dropout. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes were reported. |
| Other bias | Unclear risk | A yoga training booklet was supplied 'to participants' after completion of 21 day programme. Presumably booklet was supplied to exercise group also which may have systematically influenced effect of randomisation. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (DSM IV). Exclusion criteria: severe physical ailments such as recent and decompensated myocardial infarction, fracture, seizure disorders, mental retardation or comorbid substance abuse (except nicotine) any comorbid psychiatric disorder, medical or neurological illness. | |
| Interventions | 1.Yoga: Yoga delivered by a certified yoga trainer from a particular school (Swami Vivekananda Yoga Anusandhana Samsthana). Consisted of shithileekarana vyayama (loosening exercises) for 10 minutes, asanas (yoga postures) for approximately 20 minutes, breathing exercises for 18 minutes and a quick relaxation technique for 3 minutes, 15 sessions (5 days a week for 3 weeks) with 3‐month follow‐up, no meditation included, expected adherence to the yoga intervention was > 75%. (n=31) 2. Exercise: 15 sessions (5 days a week for 3 weeks) of ‘physical exercises’ were adopted from the National Fitness Corps*, with duration of 1 hour in total, consisted of brisk walking (10 minutes), jogging (5 minutes), exercise in standing (20 minutes), and sitting posture exercises (20 minutes), with 2‐minute breaks with a non‐specific instruction of ‘just relax now’ between different exercises, exercise in standing included 8 components consisting of moving arms and/or legs from the ‘’position: attention’’, and sitting posture exercises consisted of exercises in cross‐legged sitting, exercise was 5 days a week for 3 weeks. (n=30) A therapist trained to teach both yoga and exercise taught the subjects in their allocated treatment groups. Twenty‐six per cent (n=16) did not complete the training due to disinterest, long distance from the hospital for outpatients. Participants were expected to continue their training for next 3 months at home, reviewed by the therapist once a month and reminder telephone calls and letters about maintaining practice. No adverse effects were reported for either group. No change to medication was made for at least 4 weeks before entry into the study and through the study period. Reported that medication was changed during the study period in two patients (one in each group) as they had exacerbation of symptoms. | |
| Outcomes | Mental state: PANSS Quality of life: WHOQOL‐BREF Unable to use: Extrapyramidal symptoms (SIM): not listed as an outcome Abornal movement (AIMS): not listed as an outcome Assessed at baseline and at 4 months | |
| Notes | Same exercise intervention as Behere 2011; Manjunath 2013; Varambally 2012. Same yoga intervention as Behere 2011; Manjunath 2013; Varambally 2012. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: ''Subjects were randomly assigned, using a computer‐generated Response: Low risk |
| Allocation concealment (selection bias) | Unclear risk | No details of allocation concealment were given. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants and personnel delivering the yoga intervention will be aware they are undertaking or delivering the yoga intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details regarding blinding of outcome assessment were given. |
| Incomplete outcome data (attrition bias) | High risk | Quote: ''All but four subjects who completed 3 weeks of training were available for follow‐up assessment after 4 months''.. .''comparable proportions (33% each) of patients allocated initially to each of the two groups were available for the final Response: Not clear to which groups the 4 participants who did not complete training were randomised, rated as high risk as not all participants randomised were included in the final analysis. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes were reported. |
| Other bias | Unclear risk | Same exercise intervention as Behere 2011; Manjunath 2013; Varambally 2012. Same yoga intervention as Behere 2011; Manjunath 2013; Varambally 2012. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia, diagnosis based on DSM‐IV criteria. Exclusion criteria: severe physical illness (myocardial infarction, hypertension, fracture, spinal problem), seizure disorders, mental retardation or comorbid substance dependence, unstable psychotic symptoms, known pregnancy or other contraindication to MRI, a history of brain trauma or organic brain disease, known history of intellectual disability or special school attendance. | |
| Interventions | 1.Yoga: 12 weeks of Hatha yoga therapy delivered by certified yoga instructor (three sessions per week, each 40/50 minutes per session which included (i) breathing control (10 minutes), (ii) warming up (10 minutes), (iii) asanas (yoga postures) for 30 minutes (iv) relaxation for 10 minutes, 5‐10 participants per class, no meditation included, expected adherence to the yoga intervention was >70%, average yoga class attendance was 47%. (n=48) 2. Aerobic: 12 weeks of treadmill walking(three sessions per week, each 1 hour) carried out by a certified coach, for 15‐20 minutes and stationary cycling for 25‐30 minutes, each participant's heart rate was continuously monitored during the exercise session using a portable recorder, the heart rate was maintained in the range of 45%‐49% of the VO2 max value, expected adherence to the aerobic intervention was >70%, average attendance rate was 58%. (n=46) 3. Wait‐list control group: treatment as usual. (n=46) Patients in both groups continued on an unchanged dosage of medication as much as possible, more than a 25% change in dosage in the first 6 weeks after commencement of the intervention was not permitted. | |
| Outcomes | Mental state: PANSS Mental state: negative symptoms CDS total score Quality of life: SF 36. Leaving the study early. Unable to use ‐ Cognitive functioning (verbal learning‐assessed by Hong Kong List Learning test, working memory‐assessed by the Digid Span test, attention and concentration‐assessed by the Letter Cancellation test Q score, cognitive flexibility‐assessed by the Stroop Color and Word Test) as no reported total end scale measure. MRI: not listed as an outcome. Physical fitness (VO2max test) as < 50% data reported (41/94=43%). Balance (SEBT): not listed as an outcome and < 50% data reported (40/96=41.6%). Flexibility (Sit‐and‐Reach Test): not listed as an outcome and < 50% data reported (40/96=41.6%). Standing balance test: not listed as an outcome and no data reported Body perception and drug adherence measure (Figure rating scale, cognitive attitude towards body size, compliance rating scale, drug attitude inventory): not listed as an outcome and no data reported. DXA: not listed as an outcome and no data reported. Side effects rating scale (UKU rating scale): as no reported total end scale measure. | |
| Notes | '61 (53.5%) were diagnosed with schizophrenia, 13 (11.4%) had schizoaffective disorder, and 39 (34.2%) had schizophreniform, brief psychotic disorders and psychosis not otherwise specified'. Data extracted from two main sources; 1 dissertation and 1 published paper. A dissertation pertaining to this study revealed that unfortunately that at some time point between the 12‐week and 18‐month time point the control group received a 'compensated' 12 week yoga or exercise programme which systematically negated the control group condition, also > 50% attrition, so 18‐month follow‐up data could not be included. *of the 85 randomised, 69 provided data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: ''A randomization list was created using a random number generator. The random list had a block size of 12 (i.e. for every 12 subjects, 4 would be assigned to the yoga group, 4 to the aerobic group and 4 to the control group'' Response: Low risk. |
| Allocation concealment (selection bias) | Low risk | Quote: ''The randomization list was concealed from research staff involved in recruitment, assessment and intervention''. Response: Low risk. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants and personnel delivering the yoga intervention are aware they are undertaking or delivering the yoga intervention. |
| Blinding of outcome assessment (detection bias) | Low risk | Qoute: ''Two research assistants will be well trained and recruited to do the assessment, and remains blind to the treatment allocation''. Response: Low risk. |
| Incomplete outcome data (attrition bias) | High risk | Quote: 48 allocated to yoga group but 45 reported to be included in intention‐to‐treat analysis, 46 allocated to aerobic exercise group but 40 reported to be included in intention‐to‐treat analysis, and data for lesser number of participants reported for all measures, e.g. for PANSS and quality of life scores data reported for 38 participants in yoga group and 31 for the non‐standard care group. Response: High risk, as not all participants randomised were included in the analysis. |
| Selective reporting (reporting bias) | High risk | Balance listed as an outcome but data not supplied in published paper. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (DSM IV and later confirmed using the Mini International Neuropsychiatric Interview by the first author). Exclusion criteria: No exclusion criteria specified. | |
| Interventions | 1.Yoga: Yoga delivered by a certified yoga trainer from a particular school (Swami Vivekananda Yoga Anusandhana Samsthana). Consisted of shithileekarana vyayama (loosening exercises) for 10 minutes, asanas (yoga postures) for approximately 20 minutes, breathing exercises for 18 minutes and a quick relaxation technique for 3 minutes, in total 51‐minute session over 2 weeks in the wards (at least 10 sessions), with 4 months of self‐practice, no meditation included, (n=44) 2. Exercise: ‘physical exercises’ were adopted from the National Fitness Corps, with duration of 1 hour in total, consisted of brisk walking (10 minutes), jogging (5 minutes), exercise in standing (20 minutes), and sitting posture exercises (20 minutes), with 2‐minute breaks with a non‐specific instruction of ‘just relax now’ between different exercises, exercise in standing included 8 components consisting of moving arms and/or legs from the ‘’position: attention’’, and sitting posture exercises consisted of exercises in cross‐legged sitting, in total 45‐minute session over 2 weeks in the wards (at least 10 sessions), with 4 months of self‐practice . (n=44) Yoga and exercise were delivered by the same therapist who was qualified to teach both. For yoga and exercise groups; after 2 weeks, participants were advised to practice the same for the next 4 weeks. Family members, who were observing their training during their inpatient stay, were requested to monitor their performance at home after discharge. Participants came to the 6‐week follow‐up alone or ‘’with different caregivers/kin and hence the report of practice at home was not reliably obtained’’. | |
| Outcomes | Mental State: PANSS (termed clinical state), HDRS, CGIS Leaving the study early Unable to use: Extra‐pyramidal side effects (SAS): not listed as an outcome. | |
| Notes | Participants in both groups were routinely offered "games, exercise and chanting" by nurses between 8am and 9am which was routine practice. Adherence to this was not maintained. The majority (n=83) had a diagnosis of schizophrenia,the major subgroup was paranoid schizophrenia (46.6%), the rest of the patients were diagnosed to have other subtypes of schizophrenia (41.9%) and unspecified psychosis (11.5%). Content of exercise and yoga interventions were the same as Behere 2011, Duraiswamy 2007 and Varambally 2012. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: ''A randomization table was generated for 90 patients to have equal representation of yoga or exercise as an add‐on/complementary treatment''. Response: Likely to be adequate |
| Allocation concealment (selection bias) | Unclear risk | No details of allocation concealment given. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants and personnel delivering the yoga intervention will be aware they are undertaking or delivering the yoga intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details were given regarding blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) | High risk | Quote: ''Among the 88 patients, 82 completed the 2‐week intervention successfully and were assessed at that time point. During follow‐up at 6 the week, more patients dropped out (n=28) and only 60 were available for third assessment (completed sample)''. Response: Rated as high risk as not all participants randomised were included in the final analysis (44 randomised to each group but data provided for 35 in yoga group and 25 in exercise group). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes were reported. |
| Other bias | High risk | Funding: not stated. One of the authors may be invested in intervention due to affiliation with Swami Vivekananda Yoga Anusandhana. Yoga for this study was developed from this school. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia confirmed by a psychiatrist according to DSM‐IV criteria. | |
| Interventions | 1.Yoga: Yoga delivered by a certified yoga trainer from a particular school (Swami Vivekananda Yoga Anusandhana Samsthana). Consisted of shithileekarana vyayama (loosening exercises) for 10 minutes, asanas (yoga postures) for approximately 20 minutes, breathing exercises for 18 minutes and a quick relaxation technique for 3 minutes, in total 45 minutes per session, daily for one month (about 25 sessions), with 3‐month follow‐up of self‐practice at home, no meditation included, expected adherence to the yoga intervention was > 75%. (n=47) 2. Exercise: ‘physical exercises’ were adopted from the National Fitness Corps, with duration of 1 hour in total, consisted of brisk walking (10 minutes), jogging (5 minutes), exercise in standing (20 minutes), and sitting posture exercises (20 minutes), with 2‐minute breaks with a non‐specific instruction of ‘just relax now’ between different exercises, exercise in standing included 8 components consisting of moving arms and/or legs from the ‘’position: attention’’, and sitting posture exercises consisted of exercises in cross‐legged sitting, in total 45 minutes per session, daily for one month (about 25 sessions), with 3‐month follow‐up of self‐practice at home. (n=37) 3. Wait‐list control group: receiving no yoga intervention. (n=36) No changes were made to medication status unless absolutely needed. | |
| Outcomes | Mental state: PANSS. Social functioning: SOFS. Unable to use ‐ Adverse events: extra‐pyramidal symptoms rating scale (no data reported). | |
| Notes | Yoga and exercise content same as Behere 2011, Duraiswamy 2007, Manjunath 2013. Included only data from intervention groups 1 and 3. No incentive was offered for participation in the study but to ''facilitate participation'' the cost of bus travel between their home and the yoga centre was covered for study participants and their relative between their home and the yoga centre. It was not specified if exercise was delivered by the yoga instructor. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: ''one investigator (JT) uninvolved in the treatments or assessment generated random numbers'' Response: Lacking detail if sequence‐generation strategy was adequate |
| Allocation concealment (selection bias) | Unclear risk | Quote: ''subject's allocation to one of these groups was kept concealed and only ascertained after consent and before he/she was to be randomized'' Response: Unclear risk, as concealment strategy was not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: ''only the social worker and the yoga therapist were informed to start the corresponding intervention'' Response: Unclear risk, participants as well as social worker and yoga therapist were aware of group allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: ''the rater was unaware of group allocation'' Response: Low risk |
| Incomplete outcome data (attrition bias) | High risk | Quote: ''some did not turn up at the 4th month follow‐up and therefore final sample was smaller; 39, 22 and 34 in yogasana, exercise and waiting list groups'' Response: High risk, as more participants withdrew from the exercise group (40.5%) than the yoga group (17%) and 26% overall not followed up and not included in analysis. |
| Selective reporting (reporting bias) | High risk | Extrapyramidal symptoms scale (adverse events) listed as an outcome but no data reported. |
| Other bias | High risk | Funding: not stated. One of the authors may be invested in intervention due to affiliation with Swami Vivekananda Yoga Anusandhana. Yoga for this study was developed from this school. |
CDS: Calgary Depression Scale
CGI: Clinical Global Impression Severity
DSM IV: Diagnostic and Statistical Manual of Mental Disorders
HDRS: Hamilton Depression Rating Scale
MRI: magnetic resonance imaging
PANSS: Positive and Negative Syndrome Scale
SOFS: Social Occupational Functioning Scale
TRACS:TRENDS Accuracy Score (TRENDS=Tool for Recognition of Emotions in Neuropsychiatric DisorderS)
WHOQOL‐BREF: World Health Organisation Quality Of Life
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga plus occupational recreational therapy and conventional treatment versus occupational recreational therapy and conventional treatment, not 'non‐standard care'. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga versus standard‐care not non‐standard care. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga versus standard‐care not non‐standard care. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga as a package of care versus standard care, not non‐standard care. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga versus standard‐care not non‐standard care. | |
| Allocation: 'quasi' randomised not randomised as stated in protocol. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga versus standard‐care not non‐standard care. | |
| Allocation: ''double blind''. Participants: people with schizophrenia. Interventions: 'Tagara' (local drug with anti‐psychotic properties) and 'Brahmyadiyoga' (a herbal compound) versus chlorpromazine versus placebo, not yoga. | |
| Allocation: randomised. Participants: people with schizophrenia. Intervention: yoga plus motivational and feedback session versus waiting list, not yoga alone. | |
| Allocation: ''double blind''. Participants: people with schizophrenia. Interventions: 'Tagara' (local drug with anti‐psychotic properties) and 'Brahmyadiyoga' (a herbal compound) versus chlorpromazine versus placebo, not yoga. | |
| Allocation: randomised. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: cross‐over trial of yoga and exercise, not clear which randomised to first, exercise or yoga. | |
| Allocation: randomised. Participants: caregivers of people with schizophrenia, not sufferers of schizophrenia. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga versus standard‐care not non‐standard care. | |
| Allocation: participants randomly selected but not randomly allocated to intervention/control group. | |
| Allocation: randomised. Participants: people with schizophrenia. Intervention: yoga plus counselling versus standard care, not yoga alone. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Effects study of yoga therapy on the association of mental illness with metabolic disorders |
| Methods | Allocation: randomised. Blinding: no details given. Duration: no details given. Design: parallel. Setting: Toyko Metropolitan Matsuzawa Hospital. |
| Participants | Diagnosis: schizophrenia (DSM IV). Exclusion criteria: patients with diabetes, renal failure, pervasive development disorders, mental retardation. |
| Interventions | 1. Yoga therapy: (no further details given). 2. 'A simple exercise': (no further details given). |
| Outcomes | Oxidative‐stress markers (no further outcomes listed). |
| Starting date | 05 December 2014. |
| Contact information | Masanari Itokawa (itokawa‐[email protected]), Hiromi Idozawa (Chiken‐[email protected]) |
| Notes | Contacted for study information 16 February 2016, no reply. |
DSM IV: Diagnostic and Statistical Manual of Mental Disorders
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mental state: 1. Clinically important change (PANSS ‐ not improved) short term Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 1 Mental state: 1. Clinically important change (PANSS ‐ not improved) short term. | ||||
| 1.1 overall | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.62, 1.07] |
| 1.2 specific ‐ negative symptoms | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.57, 0.90] |
| 1.3 specific ‐ positive symptoms | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.84, 1.38] |
| 2 Mental state: 2. Average endpoint score (various scales) short term Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2 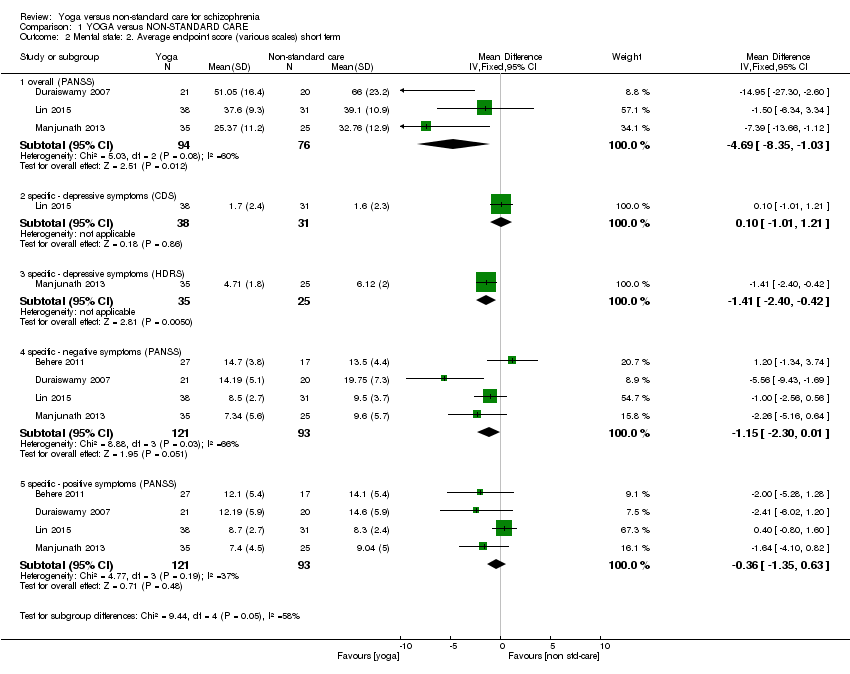 Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 2 Mental state: 2. Average endpoint score (various scales) short term. | ||||
| 2.1 overall (PANSS) | 3 | 170 | Mean Difference (IV, Fixed, 95% CI) | ‐4.69 [‐8.35, ‐1.03] |
| 2.2 specific ‐ depressive symptoms (CDS) | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐1.01, 1.21] |
| 2.3 specific ‐ depressive symptoms (HDRS) | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐1.41 [‐2.40, ‐0.42] |
| 2.4 specific ‐ negative symptoms (PANSS) | 4 | 214 | Mean Difference (IV, Fixed, 95% CI) | ‐1.15 [‐2.30, 0.01] |
| 2.5 specific ‐ positive symptoms (PANSS) | 4 | 214 | Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐1.35, 0.63] |
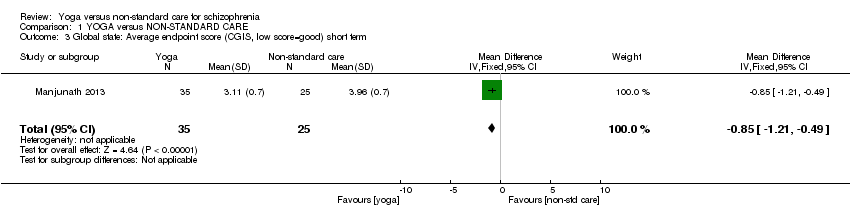
| 3 Global state: Average endpoint score (CGIS, low score=good) short term Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.85 [‐1.21, ‐0.49] |
| Analysis 1.3 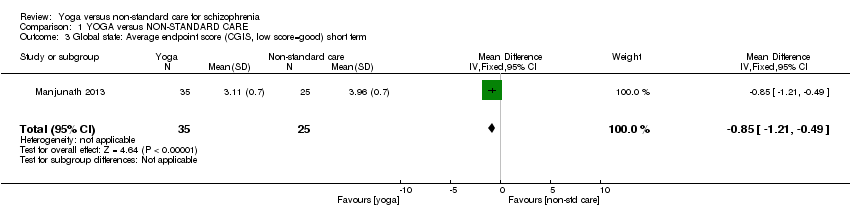 Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 3 Global state: Average endpoint score (CGIS, low score=good) short term. | ||||
| 4 Social functioning: 1. Clinically important change (SOFS ‐ not improved) short term Show forest plot | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.78, 1.04] |
| Analysis 1.4  Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 4 Social functioning: 1. Clinically important change (SOFS ‐ not improved) short term. | ||||
| 5 Social functioning: 2. Average score at endpoint (two scales) Show forest plot | 1 | 88 | Mean Difference (IV, Fixed, 95% CI) | 3.20 [‐0.57, 6.97] |
| Analysis 1.5  Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 5 Social functioning: 2. Average score at endpoint (two scales). | ||||
| 5.1 SOFS, high score=good | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 3.70 [‐0.70, 8.10] |
| 5.2 Emotional recognition, TRACS, high score=good | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 1.80 [‐5.54, 9.14] |
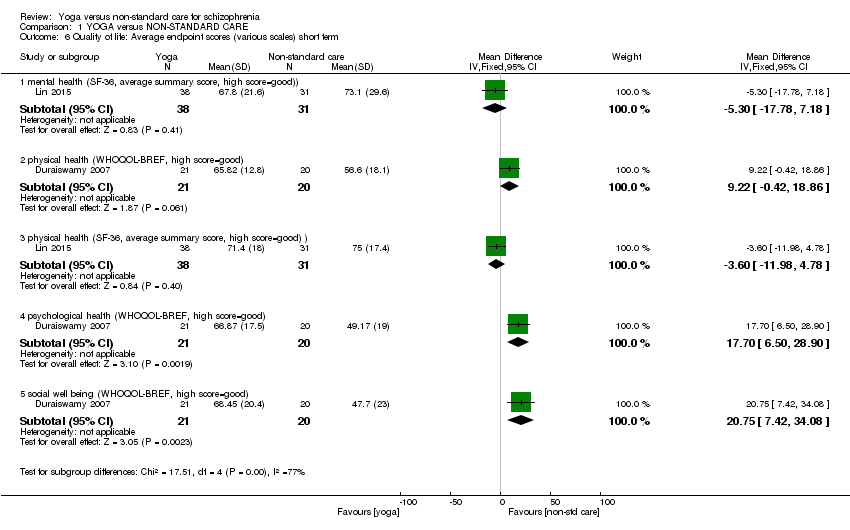
| 6 Quality of life: Average endpoint scores (various scales) short term Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.6  Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 6 Quality of life: Average endpoint scores (various scales) short term. | ||||
| 6.1 mental health (SF‐36, average summary score, high score=good)) | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | ‐5.30 [‐17.78, 7.18] |
| 6.2 physical health (WHOQOL‐BREF, high score=good) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 9.22 [‐0.42, 18.86] |
| 6.3 physical health (SF‐36, average summary score, high score=good) ) | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | ‐3.60 [‐11.98, 4.78] |
| 6.4 psychological health (WHOQOL‐BREF, high score=good) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 17.70 [6.50, 28.90] |
| 6.5 social well being (WHOQOL‐BREF, high score=good) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 20.75 [7.42, 34.08] |
| 7 Adverse effects Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 7 Adverse effects. | ||||
| 7.1 any serious | 1 | 85 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.05, 0.05] |
| 7.2 others | 1 | 85 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.05, 0.05] |
| 8 Leaving the study early ‐ short term Show forest plot | 6 | 586 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.51, 0.86] |
| Analysis 1.8 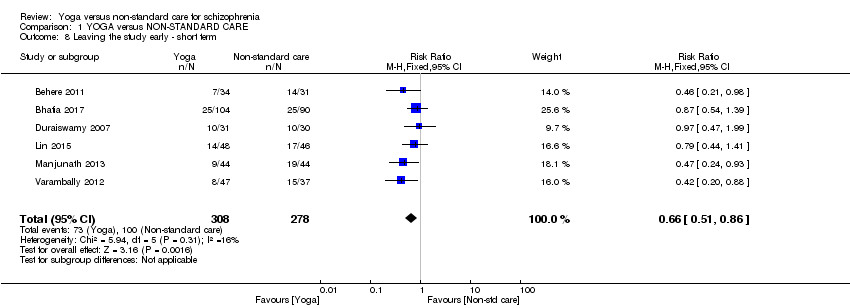 Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 8 Leaving the study early ‐ short term. | ||||

37Study flow diagram for 2015 searches

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 1 Mental state: 1. Clinically important change (PANSS ‐ not improved) short term.

Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 2 Mental state: 2. Average endpoint score (various scales) short term.
Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 3 Global state: Average endpoint score (CGIS, low score=good) short term.

Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 4 Social functioning: 1. Clinically important change (SOFS ‐ not improved) short term.

Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 5 Social functioning: 2. Average score at endpoint (two scales).
Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 6 Quality of life: Average endpoint scores (various scales) short term.

Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 7 Adverse effects.

Comparison 1 YOGA versus NON‐STANDARD CARE, Outcome 8 Leaving the study early ‐ short term.
| Intervention | plus | Control | Participants | Reference tag | Relevant Cochrane review |
| Yoga | nil | standard care | people with schizophrenia | Behere 2011; Ikai 2013; Ikai 2014; Jayaram 2013; Lin 2006;Lin 2015;Varambally 2012a; Visceglia 2011 | Yoga versus standard care for schizophrenia |
| counselling | standard care | ||||
| motivational and feedback session | |||||
| nil | caregivers of people with schizophrenia | ||||
| Yoga | non‐standard care | people with schizophrenia | Yoga as part of a package of care versus non‐standard care | ||
| Chlorpromazine | nil | placebo | Chlorpromazine versus placebo for schizophrenia | ||
| 'Tagara' (local drug with anti‐psychotic properties) and 'Brahmyadiyoga' (a herbal compound) | nil | Chlorpromazine versus herbal compounds for schizophrenia | |||
| chlorpromazine | |||||
| * This particular study used yoga combined with relaxation exercises, breathing exercises, body movement exercises, basic acting exercises, the Alexander technique, theatre games, exercise ''to build self confidence'', creative work using props, use of music to enhance creativity and moods. | |||||
| Methods | Allocation: randomised (clearly described). |
| Participants | Diagnosis: people with a clinical diagnosis of schizophrenia. |
| Interventions | 1. Yoga: the yoga intervention should be clearly described and consist of the following components; (i) shithileekarana vyayama (loosening exercises) for approximately 10 minutes (ii) yoga postures (asanas) for approximately 20 minutes (iii) breathing exercises and relaxation techniques for approximately 20 minutes using a manualised protocol, yoga programme for 12 weeks, 3 times weekly, follow‐up at 6 months and 1 year, yoga delivered by a trained yoga instructor, meditation not included. 2. Standard care control*. All groups stable pharmacotherapy. |
| Outcomes | Mental state (binary outcomes). Relapses (binary outcomes). QOL (binary outcomes). Disability (binary outcomes). Activities of daily living (binary outcomes). Costs: cost of services, cost of care. Adverse events related to yoga (number and type of injuries). Service outcomes: days in hospital, time attending outpatient psychiatric clinic. |
| Notes | Adherence should be logged with patients expected to adhere to 70% to 75% of scheduled sessions. * Regarding design of a future study, readers are directed to the first yoga review in this series (Broderick 2015) ‐ as a comprehensive yoga versus standard care study has not yet been published, this would be the initial priority. When this is conducted, many legitimate active comparators to yoga could be suggested; such as, but not limited to the following; yoga versus talking therapy, yoga versus expressive therapies, yoga versus other forms of exercise such as Tai'chi. |
| Intervention | plus | Active Comparator Broad Group | Specific interventions* |
| Yoga | nil | expressive therapy | art therapy |
| drama therapy | |||
| music therapy | |||
| dance therapy | |||
| writing therapy | |||
| talking therapies | cognitive behavioural therapy | ||
| dialectic behaviour therapy | |||
| humanistic therapies | |||
| exercise | aerobic‐based interventions | ||
| combined aerobic and resistance programme | |||
| resistance‐based interventions | |||
| Tai'chi | |||
| qi'gong | |||
| *This list of specific interventions is not exhaustive and merely provides some examples of legitimate active comparators to yoga which are not currently available. These interventions could also be considered alternatively. For instance, exercise consists of heterogeneous interventions, it is accepted there could be other equally justifiable intervention titles such as 'supervised' exercise, 'non‐supervised exercise', or 'group‐based exercise', 'individual exercise', or exercise could be considered in terms of intensity such as 'high intensity', 'moderate intensity' and 'low intensity'. Note the specific intervention should be delivered by suitably qualified personnel. | |||
| YOGA versus NON‐STANDARD CARE for schizophrenia | ||||||
| Patient or population: people with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | YOGA versus NON‐STANDARD CARE | |||||
| Mental state: clinically important change Follow‐up: 4 months | Low1 | RR 0.81 | 84 | ⊕⊕⊝⊝ | ||
| 800 per 1000 | 648 per 1000 | |||||
| Moderate1 | ||||||
| 900 per 1000 | 729 per 1000 | |||||
| High1 | ||||||
| 1000 per 1000 | 810 per 1000 | |||||
| Global state: relapse | No trial reported this outcome. | |||||
| Social functioning: clinically important change | Low1 | RR 0.90 | 84 | ⊕⊕⊝⊝ | ||
| 700 per 1000 | 630 per 1000 | |||||
| Moderate1 | ||||||
| 900 per 1000 | 810 per 1000 | |||||
| Adverse effects ‐ any | See comment | See comment | Not estimable | 85 | ⊕⊕⊕⊝ | Risks were calculated from pooled risk differences. The study reported no adverse effects. |
| Quality of life: clinically important change SF‐36 average change score mental health * | The mean quality of life: average change ‐ mental health in the intervention (yoga) groups was | 69 | ⊕⊕⊝⊝ | * no trial reported binary data; we chose 1 of 2 QOL measures as proxy measure | ||
| Physical health: clinically important change WHQOL‐BREF ‐ average change score * | The mean physical health: average change in the intervention (yoga) groups was | 41 | ⊕⊕⊝⊝ | * no trial reported binary data; we chose physical health dimension of QOL measure as proxy measure. | ||
| Costs: direct and indirect costs of care | No trial reported this outcome. | |||||
| Leaving the study early: short term | Low1 | RR 0.64 | 586 | ⊕⊕⊕⊝ | ||
| 200 per 1000 | 120 per 1000 | |||||
| Moderate1 | ||||||
| 400 per 1000 | 240 per 1000 | |||||
| High1 | ||||||
| 600 per 1000 | 360 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence CI: confidence interval; RR: risk ratio | ||||||
| 1 Moderate risk approximates to that of non‐standard care in trial(s). 3 Imprecision: Downgraded one level due to small sample size 7 Imprecision: Downgraded one level as based on one study with no reported adverse events. 8 Risk of bias: Downgraded one level as a number of participants withdrew from one trial and it was not clear to which group they were randomised. | ||||||
| Review title | Status |
| Yoga versus standard care for schizophrenia | Full review: Broderick 2015 |
| Yoga versus non‐standard care for schizophrenia | This review. |
| Yoga as part of a package of care versus standard care | Protocol: Broderick 2016b |
| Yoga as part of a package of care versus non‐standard care |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mental state: 1. Clinically important change (PANSS ‐ not improved) short term Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 overall | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.62, 1.07] |
| 1.2 specific ‐ negative symptoms | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.57, 0.90] |
| 1.3 specific ‐ positive symptoms | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.84, 1.38] |
| 2 Mental state: 2. Average endpoint score (various scales) short term Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 overall (PANSS) | 3 | 170 | Mean Difference (IV, Fixed, 95% CI) | ‐4.69 [‐8.35, ‐1.03] |
| 2.2 specific ‐ depressive symptoms (CDS) | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐1.01, 1.21] |
| 2.3 specific ‐ depressive symptoms (HDRS) | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐1.41 [‐2.40, ‐0.42] |
| 2.4 specific ‐ negative symptoms (PANSS) | 4 | 214 | Mean Difference (IV, Fixed, 95% CI) | ‐1.15 [‐2.30, 0.01] |
| 2.5 specific ‐ positive symptoms (PANSS) | 4 | 214 | Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐1.35, 0.63] |
| 3 Global state: Average endpoint score (CGIS, low score=good) short term Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.85 [‐1.21, ‐0.49] |
| 4 Social functioning: 1. Clinically important change (SOFS ‐ not improved) short term Show forest plot | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.78, 1.04] |
| 5 Social functioning: 2. Average score at endpoint (two scales) Show forest plot | 1 | 88 | Mean Difference (IV, Fixed, 95% CI) | 3.20 [‐0.57, 6.97] |
| 5.1 SOFS, high score=good | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 3.70 [‐0.70, 8.10] |
| 5.2 Emotional recognition, TRACS, high score=good | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 1.80 [‐5.54, 9.14] |
| 6 Quality of life: Average endpoint scores (various scales) short term Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 mental health (SF‐36, average summary score, high score=good)) | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | ‐5.30 [‐17.78, 7.18] |
| 6.2 physical health (WHOQOL‐BREF, high score=good) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 9.22 [‐0.42, 18.86] |
| 6.3 physical health (SF‐36, average summary score, high score=good) ) | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | ‐3.60 [‐11.98, 4.78] |
| 6.4 psychological health (WHOQOL‐BREF, high score=good) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 17.70 [6.50, 28.90] |
| 6.5 social well being (WHOQOL‐BREF, high score=good) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 20.75 [7.42, 34.08] |
| 7 Adverse effects Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 any serious | 1 | 85 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.05, 0.05] |
| 7.2 others | 1 | 85 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.05, 0.05] |
| 8 Leaving the study early ‐ short term Show forest plot | 6 | 586 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.51, 0.86] |

