Yoga como parte de un paquete de atención versus la atención habitual para la esquizofrenia
Resumen
Antecedentes
El yoga es una práctica espiritual antigua que se originó en la India y actualmente se acepta en el mundo occidental como una forma de relajación y ejercicio. Ha sido de interés determinar la eficacia del yoga proporcionado a los pacientes con esquizofrenia como parte de un paquete de atención versus la atención habitual.
Objetivos
Examinar los efectos del yoga como parte de un paquete de atención versus la atención habitual.
Métodos de búsqueda
Se hicieron búsquedas en el registro de ensayos del Grupo Cochrane de Esquizofrenia (Cochrane Schizophrenia Group) (fecha más reciente 30 marzo 2017) que se basa en búsquedas regulares en MEDLINE, PubMed, Embase, CINAHL, BIOSS, AMED, PsychINFO y en registros de ensayos clínicos. Se realizaron búsquedas en las referencias de todos los estudios incluidos. No hay limitaciones de idioma, fecha, tipo de documento o estado de publicación para la inclusión de los archivos en el registro.
Criterios de selección
Todos los ensayos controlados aleatorios (ECA) que incluyeron pacientes con esquizofrenia y que compararon el yoga como parte de un paquete de atención versus un control atención habitual.
Obtención y análisis de los datos
Los autores de la revisión, de forma independiente, seleccionaron los estudios, calificaron su calidad y extrajeron los datos. Para los resultados binarios, se calculó la diferencia de riesgos (DR) y su intervalo de confianza (IC) del 95%; el análisis fue de intención de tratar. Para los datos continuos se calculó la diferencia de medias (DM) entre los grupos y su IC. Para los análisis se emplearon los modelos de efectos mixtos y de efectos fijos. Se examinó la heterogeneidad (técnica I2), se evaluó el riesgo de sesgo de los estudios incluidos y se crearon las tablas "Resumen de los hallazgos" mediante GRADE (Grading of Recommendations Assessment, Development and Evaluation).
Resultados principales
Se incluyen tres estudios en esta revisión. Todos los resultados fueron a corto plazo (menos de ocho semanas). Se informaron datos utilizables para dos resultados solamente; abandono temprano del estudio y calidad de vida. Hubo cierta evidencia que favoreció al yoga como parte de un paquete de atención en las puntuaciones finales de calidad de vida (un ECA, n = 80, DM 22,93; IC 19,74 a 26,12; evidencia de baja calidad). Los datos del abandono temprano del estudio fueron ambiguos entre los grupos de tratamiento (tres ECA, n = 193; DR 0,06; IC: ‐0,01 a 0,13; evidencia de calidad moderada, heterogeneidad alta). En general, en esta revisión falta un número excesivo de resultados clave, que incluyen el estado mental y general, el funcionamiento social, la salud física, los efectos adversos y los costos de la atención.
Conclusiones de los autores
En esta revisión se incluyó un escaso número de estudios pequeños que carecían de muchos resultados clave. Los escasos datos impiden establecer con algún grado de confiabilidad que el yoga proporcionado como parte de un paquete de atención tiene efectos beneficiosos en comparación con la atención habitual.
PICO
Resumen en términos sencillos
Yoga como parte de un paquete de atención versus la atención habitual para la esquizofrenia
Pregunta de la revisión
¿El yoga, proporcionado como parte de un paquete más grande de atención, es efectivo para los pacientes con esquizofrenia en comparación con la atención habitual?
Antecedentes
El yoga incluye posturas físicas y ejercicios respiratorios para promover el equilibrio entre la mente y el cuerpo. En la actualidad, el yoga se ha adoptado ampliamente como método de relajación y ejercicio para la reducción del estrés, así como para la promoción de la salud y la sensación de bienestar. La esquizofrenia es una enfermedad mental en que los pacientes presentan síntomas como oír voces que no existen, una respuesta emocional deficiente y retraimiento social. A menudo la esquizofrenia afecta a los pacientes durante períodos prolongados de la vida y se trata principalmente mediante fármacos antipsicóticos. Sin embargo, estos fármacos no siempre son completamente efectivos y algunos estudios de investigación indican que el yoga como un tratamiento complementario podría tener efectos beneficiosos y ayudaría a mejorar la calidad de vida de los pacientes con esquizofrenia. El yoga se puede combinar con otras terapias como el asesoramiento psicológico u otras formas de ejercicios en un "paquete de atención".
Características de los estudios
En esta revisión fue posible incluir solamente tres estudios a corto plazo (con una duración de ocho semanas) que asignaron al azar a pacientes con esquizofrenia a recibir sesiones de yoga como parte de un paquete de atención o a la atención habitual. El yoga se combinó con arte dramático, música y baile en un estudio y con una sesión motivacional y de retroalimentación en otro estudio. El estudio final incluido en esta revisión combinó el yoga con asesoramiento y una sesión interactiva de preguntas y respuestas. La contribución relativa del yoga no se esbozó claramente en estos estudios. Estos estudios se encontraron mediante búsqueda electrónica en el registro del Grupo Cochrane de Esquizofrenia (Cochrane Schizophrenia Group) en marzo de 2017. Durante los ensayos, todos los participantes se mantuvieron con el tratamiento antipsicótico prescrito.
Resultados clave
Los estudios de esta revisión no analizaron muchos resultados importantes como el funcionamiento mental, físico y social, los efectos adversos ni las consideraciones económicas. Se pueden haber producido algunos cambios pequeños en la calidad de vida a favor del yoga como parte de un paquete de atención, pero en general no hubo evidencia suficiente y de buena calidad en esta revisión para afirmar de manera consistente que se debe prescribir el yoga como parte de un paquete de atención de forma complementaria a la atención habitual para la esquizofrenia.
Calidad de las pruebas
La evidencia era limitada y débil. El número de estudios incluidos fue pequeño y sólo se informó el seguimiento a corto plazo para dos resultados. Con frecuencia, la esquizofrenia es una enfermedad a largo plazo y se necesitan ensayos adicionales más grandes y a largo plazo que se centren en resultados importantes.
Authors' conclusions
Summary of findings
| Yoga package versus standard care for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Yoga package versus standard care | |||||
| Mental State: clinically important change | No useable mental state data reported. | |||||
| Social functioning: clinically important change | No study reported on social functioning. | |||||
| Adverse events: clinically important adverse effect | No study reported on adverse effects. | |||||
| Quality of life: clinically important change* Follow‐up: mean 4 weeks | The mean quality of life (GQOLI‐74) in the intervention groups was | 80 | ⊕⊕⊝⊝ | * Clinically important data not available: nearest outcome reported were Average endpoint scores on the GQOLI‐74 | ||
| Leaving the study early: any reason Leaving the study early: participants lost to follow‐up ‐ short term (low=good) | Low1 | 0.06 [‐ 0.01 to 0.13] | 193 (3 studies) | ⊕⊕⊕⊝ | ||
| 800 per 1000 | 1000 per 1000 (640 to 1000) | |||||
| Moderate1 | ||||||
| 900 per 1000 | 1000 per 1000 (720 to 1000) | |||||
| High1 | ||||||
| 1000 per 1000 | 1000 per 1000 (800 to 1000) | |||||
| Costs of care: direct and indirect | No study reported direct or indirect costs of care. | |||||
| Physical health: clinically important change | No study reported on physical health. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Imprecision: Downgraded one level as a number of participants withdrew from two trials, not accounted for in final analysis. 3Imprecision: Downgraded one level due to relatively small number of participants included. | ||||||
Background
Description of the condition
Schizophrenia is a relatively common serious mental disorder with a lifetime prevalence of 0.3% to 0.6% and incidence of 10.2 to 22.0 per 100,000 people (McGrath 2008). Schizophrenia is characterised by a constellation of symptoms that can present in a wide variety of ways depending on the individual. Symptoms can broadly be divided into positive symptoms and negative symptoms. Positive symptoms include delusions, hallucinations, disorganised speech, and disorganised behaviour. Negative symptoms include anhedonia (lack of pleasure), alogia (reduced speech), and affective flattening, or a lack of emotional responsiveness (Tandon 2013). Additionally, while they are not included in the current International Classification of Diseases (ICD‐10) or Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM‐5) diagnostic systems as diagnostic criteria, characteristic cognitive deficits are widely recognised in schizophrenia and are the target of considerable clinical and research attention (Carbon 2014).
Schizophrenia has been identified as a serious public health concern, ranking 11th in the causes of years lived with disability worldwide (Global Burden of Disease 2015).The mainstay of treatment is antipsychotic medication (Owen 2016). A recent review highlighted that antipsychotic medication is associated with an increased risk for several physical diseases, including obesity, dyslipidaemia, diabetes mellitus, thyroid disorders and hyponatraemia, cardiovascular, respiratory tract, gastrointestinal, haematological, musculoskeletal and renal diseases, as well as movement and seizure disorders (Correll 2015). Although antipsychotic medication is effective in reducing positive symptoms, usually within the early stages of treatment (Leucht 2013), it is of less benefit for negative symptoms (Fusar‐Poli 2015) and cognitive deficits (Nielsen 2015). Unfortunately, it is the negative and cognitive symptoms that cause most disability (Vancampfort 2011; Vancampfort 2012). The side‐effect profile and inherent limitations of antipsychotics as well as patient preference to avoid this route where possible, have resulted in additional non‐pharmacological interventions being utilised as either an adjunct or alternative to medication therapy (Kern 2009). Low‐cost treatments that decrease negative symptoms, reduce cognitive deficits and promote mental and physical quality of life and functional recovery are warranted.
Description of the intervention
Yoga originates from India as an ancient Hindu practice incorporating physical postures with breathing exercises seeking to bring about a balance between the mental and physical state (Büssing 2012; Ross 2012; Sherman 2012). The principles behind its practice were first described by Pantajali, and were believed to allow the mind and the body to be prepared for spiritual development (Ross 2012). In the Western world, yoga has now been widely adopted as both a method of relaxation and exercise. Hatha yoga is the most widely adopted practice used in the Western world (Collins 1998). Its use of postures (asanas) improves strength, flexibility, co‐ordination and endurance and its use of breathing exercises (pranayama) improves respiratory control and concentration. Mantra yoga is another well‐known and widely practiced form of Hindu yoga and focuses on the use of chants to achieve mental and spiritual transformation (Sherman 2012).
With its increasing popularity, research into the effect of yoga on both physical and mental health has identified key benefits of yoga. It has been shown to both reduce stress and improve cognitive function in healthy individuals (Bangalore 2012), and also to be useful as a complementary therapy for many health conditions, resulting in better blood pressure control and improvements in mental health conditions including depression and anxiety disorders (Büssing 2012).
Yoga's benefit for other mental health conditions has lead to research into the role of yoga as a potential complementary therapy for the management of schizophrenia. A systematic review of randomised controlled trials (RCTs) indicated that yoga could also be of benefit as an add‐on treatment to standard care by reducing both positive and negative symptoms of schizophrenia and improving the health‐related quality of life of people with schizophrenia (Vancampfort 2012), although the evidence is limited, as only three trials were included. A further review echoed the possible improvements in quality of life, but highlighted that long‐term benefits are not known and the safety of the intervention was not reported (Cramer 2013). Recently, it was demonstrated that yoga also improves the cognitive sub‐domain of long‐term memory (k=2, n=184: Hedges' g=.32, P < .05) in people with schizophrenia (Dauwan 2016).
Exercise is a subset of physical activity that is planned, structured, and repetitive and has, as a final or an intermediate objective, the "improvement or maintenance of physical fitness" (Caspersen 1985). Exercise is intentional and has an aim of increasing one or more of the components of physical fitness (i.e. cardiorespiratory fitness, muscular strength and endurance, body composition, flexibility and neuromotor fitness), or physical activity, or improving a physical indicator such as blood pressure.
Yoga can therefore be considered a form of exercise. While purist yoga‐only programmes are often delivered, yoga also has the potential to be delivered as a part of a multi‐modal intervention or 'package of care'. This could be alongside other exercise, which could consist of any other activity which falls under the umbrella term of exercise, encompassing broad categories of skill‐related fitness, health‐related fitness, body‐mind fitness, as well as physical activities which are not specifically fitness focused. Yoga could also be combined with expressive therapies or talking therapies. Multi‐modal interventions could consist of two components or a diverse mix of more than two elements; for example, yoga combined with other exercise combinations such as Tai‐chi plus art therapy.
Expressive therapies include broad categories of art therapy, dance therapy, drama therapy, music therapy and writing therapy. These represent different approaches, but the uniting principal is that these forms of therapy take place within a patient‐therapist relationship.
In art therapy the patient is directed to use a range of art materials to make images, and the focus is on the relation between the image, the creator, and the therapist (Crawford 2007). Dance therapy is also sometimes referred to as dance‐movement therapy (DMT) (Payne 2006), and has been used as a healing ritual since early human history, although there is no one particular therapeutic dance (Ren 2013). Drama therapists use games, storytelling and role‐play (Crawford 2007). Music therapy is often perceived as a psychotherapeutic method in the sense that it addresses intra‐ and inter‐psychic, as well as social processes by using musical interaction as a means of communication, expression, and transformation (Geretsegger 2017). Writing therapy uses the act of writing and processing the written word as a therapeutic tool.
Talking therapies can be considered to consist of, but are not limited to; talking treatments, counselling, psychological therapies or treatments and psychotherapies. Cognitive behaviour therapy (CBT) is one of the most well‐recognised talking therapies. In CBT, links are made between the person’s feelings and patterns of thinking which underpin their distress. The participant is encouraged to take an active part in their therapy by using the following techniques (Jones 2012).
-
Challenging their habitual patterns of thinking.
-
Examining the evidence for and against their distressing beliefs.
-
Using reasoning abilities and personal experience to develop rational and personally acceptable alternative explanations and interpretations (Alford 1994) and to test these alternative explanations in real world situations(Tarrier 1993).
As CBT has latterly developed into a 'catch all' term for a variety of similar interventions, the criteria developed by Jones 2012 will be incorporated in this review.
How the intervention might work
Yoga has been identified as having a role in regulating the autonomic nervous system (Varambally 2012), decreasing sympathetic tone, and creating a reaction the opposite to 'fight or flight' reaction. There is a subsequent effect on the limbic system and hypothalamic pituitary axis leading to a reduction in blood cortisol levels. This leads to a regulation of heart rate and blood pressure, which has obvious cardiovascular benefits (Damodaran 2002). Yoga also focuses on relaxed breathing and this internal concentration is thought to reduce stress by minimising mental focus on external stressors or threats (Bangalore 2012). The decrease in cortisol levels is also thought to have an effect on the better control of blood glucose, cholesterol and total lipids. Since antipsychotic medication for the treatment of schizophrenia is associated with dyslipidaemia, diabetes and obesity (Correll 2015; Vancampfort 2015), yoga may be a useful adjuvant to therapy to minimise these effects (Bangalore 2012). The improvement in the physical health of these patients could have a direct benefit to their mental health. Yoga is also identified to have a role in improving sleep (Collins 1998). There is also thought to be a role of oxytocin, a hormone related to improved mood, analogues of which have been suggested as a possible treatment for schizophrenia (Bangalore 2012; Feifel 2011). It has been identified that plasma levels of oxytocin are higher in people after the practice of yoga (Varambally 2012).
Mechanisms explaining the beneficial effects of exercise in people with schizophrenia are not fully elucidated at this time. At present, the plausible mechanisms for change in positive and negative symptoms through exercise fall into one of two broad testable hypotheses: (1) biochemical changes such as increased levels of neurotransmitters (e.g. endorphins, dopamine or serotonin), which could be tested in schizophrenia‐like animal models, and (2) psychological changes such as social support, sense of autonomy, improved perceptions of competence, enhanced body image, self‐efficacy and distraction. Cardio‐metabolic and neurochemical pathways between skeletal muscle, the spinal cord, and the brain offer plausible, testable mechanisms that might help explain the effects of exercise on brain health in people with schizophrenia. Previous research demonstrated that changes in hippocampal volume and cortical thickening (or less thinning) following aerobic exercise were correlated with improvements in aerobic fitness measured by change in maximum oxygen consumption (Vancampfort 2014). The underlying mechanisms of brain volume increases resulting from improved aerobic fitness are still unknown, but it was shown recently (Kimhy 2015) that increased production of brain‐derived neurotrophic growth factors (BDNF) probably plays a role. More interventional and longitudinal exploration is needed of the underlying mechanisms for brain health improvements in patients with schizophrenia following exercise. Future research could investigate whether exercise, for example, reduces the inflammatory status of the brain by increasing levels of the anti‐inflammatory cytokine interleukin‐10.
As expressive therapy consists of broad categories of art therapy, dance therapy, drama therapy, music therapy and writing therapy, the effects of these treatments are diverse, and are not completely known. It is not fully understood whether the healing aspect of therapy is the process of the actual expressive therapy, the relationship that develops between the therapist and the patient, or most likely, a complex fusion of the two. Generally, research into the physiological and biochemical effects of these therapies in schizophrenia is in its infancy. From a social and emotional perspective, music therapy for example can have particular motivating, relationship‐building, and emotionally expressive qualities that may help those who do not respond to verbal therapy (Rolvsjord 2001; Solli 2008), while dance therapy is associated with other therapeutic benefits. Body movement dance can stimulate and release feelings, enable communication and enhance non‐verbal contact. In addition, the non‐critical therapeutic setting can decrease anxiety (Ren 2013).
Talking therapies are a diverse set of treatments which can be considered under the following broad categories; Cognitive‐Behavioural, Humanistic, Insight‐Oriented, Postmodernist, Systemic and Others. They are therefore associated with diverse effects, some of which are not fully understood. Cognitive behavioural therapy (CBT), for instance, aims to remediate distressing emotional experiences or dysfunctional behaviour by changing the way in which the individual interprets and evaluates the experience or cognates on its consequence and meaning (Jones 2012). CBT uses normalisation techniques as well as behavioural techniques to reduce distress and improve functioning. It has also been proposed (Birchwood 2006) that CBT might focus upon the following.
-
Distress reduction or the reduction of depression and problem behaviour associated with beliefs about psychotic symptomatology.
-
The emotional and interpersonal difficulty in individuals at high risk of developing psychosis.
-
Relapse prodromes to prevent relapse in psychosis.
-
‘Comorbid’ depression and social anxiety, including the patient’s appraisal of the diagnosis and its stigmatising consequences.
-
General stress reactivity, thereby increasing resilience to life stress and preventing psychotic relapse.
-
Increasing self‐esteem and social confidence in people with psychosis.
Little research has been conducted on the effect of multi‐modal interventions which encompass yoga. When delivered as part of a package of care, it is not known whether the multi‐modal intervention dilutes, has an additive effect, or makes no difference to the effect of yoga. If yoga is combined with another form of exercise, the results may be different to yoga combined with expressive or talking therapies. Even combining yoga with another exercise, the effect could depend on frequency, intensity, time and type of exercise, and whether the focus is on skill‐related fitness, health‐related fitness, body‐mind fitness, or physical activities which are not specifically fitness focused. Expressive and talking therapies are so diverse, that if combined with yoga, their combined effect could not be generalised.
Why it is important to do this review
It was originally envisaged that one Cochrane review entitled 'Yoga for schizophrenia' would adequately map this area, but on closer evaluation it became apparent that the yoga comparison includes several distinct strands. A pragmatic decision was therefore taken to logically group comparisons into a series of independent reviews, outlined in Table 1, conducted by the same core group of authors, and to synthesise these into a future overview entitled 'Yoga for schizophrenia, an overview of Cochrane systematic reviews'.
| Review number | Review Title | Status |
| 1 | Yoga versus standard care for schizophrenia | |
| 2 | Yoga versus non‐standard care for schizophrenia | |
| 3 | Yoga as part of a package of care versus standard care | Current review |
| 4 | Yoga as part of a package of care versus non‐standard care |
Due to a growing demand from patients to use alternative or adjunct treatment to their medication (Elkins 2005) and a prevalence of poor antipsychotic compliance (van Os 2009), adjunctive non‐pharmacological options are increasingly important. Yoga as a package of care is one such non‐pharmacologically‐based add‐on treatment in the management of people with schizophrenia. In resource‐constrained times the question arises ‐ is yoga delivered as a package of care more effective than standard care for people with schizophrenia? This review will provide the most comprehensive answer possible to this question and may expedite the integration of yoga as a package of care into clinical practice.
Objectives
To examine the effects of yoga as part of a package of care versus standard care for schizophrenia.
Methods
Criteria for considering studies for this review
Types of studies
All relevant randomised controlled trials (RCTs). If a trial was described as 'double‐blind' but implied randomisation, we would have included such trials in a sensitivity analysis (see Sensitivity analysis). We excluded quasi‐randomised studies, such as those allocating by alternate days of the week. Where people were given additional treatments to exercise or yoga, we only included data if the adjunct treatment was evenly distributed between groups and only the group allocation was randomised.
Types of participants
We included people with a diagnosis of schizophrenia or related disorders, including schizophreniform disorder, schizoaffective disorder and delusional disorder, regardless of their gender, age or severity of their illness. This included diagnoses made by any means. We were interested in making sure that information was as relevant to the current care of people with schizophrenia as possible. We therefore proposed, if information was available, to clearly highlight the current clinical state (acute, early post‐acute, partial remission, remission) as well as the stage (prodromal, first episode, early illness, persistent) and as to whether the studies primarily focused on people with particular problems (for example, negative symptoms, treatment‐resistant illnesses).
Types of interventions
1. Yoga as part of a package of care
We included packages of care that combined yoga with another therapy, however defined by the study. Yoga can incorporate any of the major subtypes such as Mantra, Laya, Hatha and Raja and also include any of the combination of definitions including breathing exercises, meditation and body postures. We recognise that a package of care could include many diverse approaches that could be considered inappropriate to synthesise together. We proposed the following combinations of interventions, but recognise that this may not be entirely inclusive.
1.1 Yoga plus other exercise (not including yoga)
Yoga is combined with another type of exercise. We have used the term 'other exercise' as yoga is also a type of exercise. 'Other exercise' can include broad categories of exercise focused on health‐related fitness (such as aerobic programme), mind and body fitness (such as Tai'chi) and other physical activity not necessarily focused on fitness. We recognise that these categories may not fully map this area and proposed to keep each of the above categories separate as they represent quite different approaches.
1.2 Yoga plus talking therapy
Yoga is combined with a talking therapy to form a package of care. Talking therapy can include broad categories of Cognitive‐Behavioral, Humanistic, Insight‐oriented, Postmodernist, Systemic and Other. We proposed to keep each of the above categories separate as they represent quite different approaches.
1.3 Yoga plus expressive therapies
Yoga is combined with expressive therapies. This can include broad categories of art therapy, dance therapy, drama therapy, music therapy and writing therapy. We proposed to keep each of the above categories separate as they represent quite different approaches.
1.4 Yoga plus combination of above
2. Standard care
We defined standard care as the care participants would normally receive or have previously received for the management of their schizophrenia, without yoga intervention. This could also have included waiting‐list control.
Types of outcome measures
We aimed to divide all outcomes into short term (less than six months), medium term (seven to 12 months) and long term (over one year).
Primary outcomes
1. Mental state
1.1 Clinically important change in mental state (as defined by individual studies)
1.2 Any change in mental state (as defined by individual studies)
1.3 Average endpoint/change scores on mental state scales
2. Global state
2.1 Relapse
2.2 Clinically important change in global state (as defined by each study)
2.3 Any change in global state
2.4 Average endpoint/change scores from global state scales
3. Social functioning
3.1 Clinically important change in social functioning (as defined by individual studies)
3.2 Any change in social functioning (as defined by individual studies)
3.3 Average endpoint/change scores on social functioning scales
4. Adverse effects
4.1 Clinically important adverse effects
Secondary outcomes
5. Quality of life
5.1 Clinically important change in quality of life functioning (as defined by individual studies)
5.2 Any change in quality of life (as defined by individual studies)
5.3 Average endpoint/change scores on quality of life scales
6. Cognitive functioning
6.1 Clinically important change in cognitive functioning (as defined by individual studies)
6.2 Any change in cognitive functioning (as defined by individual studies)
6.3 Average endpoint/change scores on cognitive functioning scales
7. Leaving the study early
7.1 Any reason
7.2 Due to adverse effects of intervention
7.3 Due to lack of engagement with intervention
7.4 Due to death (suicide, natural causes, other)
8. Costs of care
8.1 Direct costs of care
8.2 Indirect costs of care
9. Effect on standard care
9.1 Reduction in reported adverse effects of standard care
9.2 Change in the level of standard care required to manage condition
10. Physical health
10.1 Clinically important change in physical health (as defined by individual studies)
10.2 Any change in physical health
11. Service use
11.1 Acute hospital admissions
11.2 Length of stay in hospital
12. Disability
12.1 Important change in disability (as defined by individual studies)
13. Daily living
13.1 Clinically important change in daily living skills (as defined by individual studies)
13.2 Any change in daily living skills (as defined by individual studies)
13.3 Average endpoint/change scores on daily living scales
'Summary of findings' table
We used the GRADE approach to interpret findings (Schünemann 2011) and used GRADE profile to export data from this review to create a 'Summary of findings' table. This table provides outcome‐specific information concerning the overall quality of evidence from each included study in the comparison, the magnitude of effect of the interventions examined, and the sum of available data on all outcomes we rated as important to patient care and decision making. We aimed to select the following main outcomes for inclusion in the 'Summary of findings' table.
-
Mental state: clinically important change (as defined by studies)
-
Social functioning: clinically important change (as defined by studies)
-
Adverse effects: clinically important adverse effect
-
Quality of life: clinically important change (as defined by studies)
-
Leaving the study early
-
Costs of care ‐ direct and indirect
-
Physical health: clinically important change (as defined by studies)
If data were not available for these pre‐specified outcomes but were available for ones that were similar, we presented the closest outcome to the pre‐specified one in the table but took this into account when grading the finding (see Differences between protocol and review).
Search methods for identification of studies
Electronic searches
Cochrane Schizophrenia Group Trials Register
As this review is part of a series of yoga reviews and an umbrella overview, the Cochrane Schizophrenia's Information Specialist had already searched the Group's trials register (latest search 30 March 2017) using the following search strategy:
*Yoga* in Title, Abstract and Index Terms of REFERENCE or in Interventions of STUDY
The Cochrane Schizophrenia Group maintains a register of trials. This is compiled by systematic searches of major resources (including AMED, BIOSIS, CINAHL, Embase, MEDLINE, PsycINFO, PubMed, and registries of clinical trials) and their monthly updates, handsearches, grey literature, and conference proceedings (see Group Module). There is no language, date, document type, or publication status limitations for inclusion of records into the register. A number of studies were identified as potentially suitable for inclusion in this review and the Information Specialist re‐ran this search in April 2017 to ensure no new studies were missed for this review.
Searching other resources
1. Reference searching
We inspected references of all included studies for further relevant studies.
2. Personal contact
We contacted the first author of each included study for information regarding unpublished trials. We noted the outcome of this contact in the included or awaiting assessment studies tables.
Data collection and analysis
Selection of studies
The lead review author JB and a post‐doctoral researcher (JM see ‐ Acknowledgements) independently inspected citations from the searches and identified relevant abstracts. Findings were compared to ensure reliability. If disputes arose, we acquired the full‐text report for more detailed scrutiny. JB and JM obtained and inspected the full‐text reports of the abstracts meeting the review criteria. If necessary, review author DV re‐inspected a sample of identified reports in order to ensure reliable selection. Where it was not possible to resolve disagreement by discussion, we attempted to contact the authors of the study for clarification.
Data extraction and management
1. Extraction
JB and JM extracted data from all included studies independently and compared results of extracted data from all of the studies. We fully discussed any disagreement and documented decisions. If necessary, we contacted authors of studies for clarification. With remaining problems CEA (see Acknowledgements) clarified issues and we documented these final decisions. We attempted to extract data presented only in graphs and figures whenever possible, but we only included such data if JB and JM independently had the same result. We attempted to contact authors through an open‐ended request in order to obtain missing information or for clarification whenever necessary. If studies had been multi‐centre we planned to extract data relevant to each component centre separately. We attempted to report total end‐scale measures, as opposed to sub‐scale measures where possible. There were two exceptions; if available we would have reported Positive and Negative Syndrome Scale (PANSS) positive syndrome scores and negative syndrome scores as well as total scores. We reported Quality of Life (QOL) sub‐scale measures if total end‐score values for this scale were not reported.
2. Management
2.1 Forms
We extracted data onto standard, simple forms.
2.2 Scale‐derived data
We included continuous data from rating scales only if:
a) the psychometric properties of the measuring instrument had been described in a peer‐reviewed journal (Marshall 2000);
b) the measuring instrument had not been written or modified by one of the trialists for that particular trial; and
c) the instrument should be a global assessment of an area of functioning and not sub‐scores which are not, in themselves, validated or shown to be reliable. However there are exceptions, we included sub‐scores from mental state scales measuring positive and negative symptoms of schizophrenia.
Ideally, the measuring instrument should either have been: i. a self‐report or ii. completed by an independent rater or relative (not the therapist). We realise that this is not often reported clearly; in Description of studies we noted if this was the case or not.
2.3 Endpoint versus change data
There are advantages of both endpoint and change data. Change data can remove a component of between‐person variability from the analysis. On the other hand, calculation of change needs two assessments (baseline and endpoint), which can be difficult in unstable and difficult to measure conditions such as schizophrenia. We decided primarily to use endpoint data, and only use change data if the former were not available. We preferred to combine endpoint and change data in the analysis as we aimed to use mean differences (MD) rather than standardised mean differences (SMD) throughout (Deeks 2011).
2.4 Skewed data
Continuous data on clinical and social outcomes are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data, we aimed to apply the following standards.
For all change data, and endpoint data from studies > 200 participants
We planned to enter all change data, as when continuous data were presented on a scale that included a possibility of negative values (such as change data), it is difficult to tell whether data are skewed or not.
We also planned to enter endpoint data from studies of at least 200 participants, for example, in the analysis irrespective of the following rules, because skewed data posed less of a problem in large studies.
For endpoint data from studies < 200 participants
(a) When a scale started from the finite number zero, we subtracted the lowest possible value from the mean, and divided this by the standard deviation. If this value was lower than one, it strongly suggested a skew and we presented these data as 'other data'. If this ratio was higher than one but below two, there would have been suggestion of skew. We entered these data and tested whether their inclusion or exclusion changed the results substantially. Finally, if the ratio was larger than two, we included these data, because skew was less likely (Altman 1996; Higgins 2011).
(b) If a scale started from a positive value (such as the PANSS, Kay 1986 which can have values from 30 to 210), we modified the calculation described above to take into account the scale starting point. In these cases, skew was present if 2 SD > (S ‐ S min), where S is the mean score and 'S min' is the minimum score.
2.5 Common measure
To facilitate comparison between trials, we intended, where possible, to convert variables that can be reported in different metrics, such as days in hospital (mean days per year, per week or per month) to a common metric (e.g. mean days per month).
2.6 Conversion of continuous to binary
Where possible, we tried to convert outcome measures to dichotomous data. This can be done by identifying cut‐off points on rating scales and dividing participants accordingly into 'clinically improved' or 'not clinically improved'. It is generally assumed that if there is a 50% reduction in a scale‐derived score such as the Brief Psychiatric Rating Scale (BPRS, Overall 1962) or the PANSS (Kay 1986), this could be considered to be a clinically‐significant response (Leucht 2005) HMaxwell: Only Leucht 2005 reference in Additional refererences; usually Leucht 2005 and Leucht 005a are listed. If data based on these thresholds were not available, we used the primary cut‐off presented by the original authors.
2.7 Direction of graphs
Where possible, we entered data in such a way that the area to the left of the line of no effect indicated a favourable outcome for yoga as a package of care. Where keeping to this makes it impossible to avoid outcome titles with clumsy double‐negatives (e.g. 'Not un‐improved') we reported data where the left of the line indicates an unfavourable outcome and noted this in the relevant graphs.
Assessment of risk of bias in included studies
JB and JM worked independently to assess risk of bias using criteria described in the Cochrane Handbook for Systematic reviews of Interventions (Higgins 2011a) to assess trial quality. This set of criteria, such as sequence generation, allocation concealment, blinding, incomplete outcome data and selective reporting, is based on evidence of associations between overestimate of effect and high risk of bias of the article.
If the raters disagreed, we made the final rating by consensus, with the involvement of review author DV. Where inadequate details of randomisation and other characteristics of trials were provided, we contacted authors of the studies in order to obtain further information. We reported non‐concurrence in quality assessment, but if disputes arose as to which category a trial was to be allocated, again, we resolved this by discussion.
We noted the level of risk of bias in Risk of bias in included studies, Characteristics of included studies and summary of findings Table for the main comparison.
Measures of treatment effect
1. Binary data
For binary outcomes we planned to calculate a standard estimation of the risk ratio (RR) and its confidence interval (CI). It has been shown that RR is more intuitive (Boissel 1999) than odds ratios and that odds ratios tend to be interpreted as RRs by clinicians (Deeks 2000). As one of the outcomes contained a trial with no events we used RD (risk difference) to illustrate the findings in the graph. Using this measure made no material difference to the finding except for its graphical presentation. The number needed to treat for an additional beneficial outcome (NNTB) and the number needed to treat for an additional harmful outcome (NNTH), with their CIs are intuitively attractive to clinicians, but are problematic both in their accurate calculation in meta‐analyses and interpretation (Hutton 2009). For binary data presented in the summary of findings Table for the main comparison, where possible, we calculated illustrative comparative risks.
2. Continuous data
For continuous outcomes we estimated mean difference (MD) between groups. We preferred not to calculate effect size measures (standardised mean difference (SMD)). However, if scales of very considerable similarity were used, we presumed there was a small difference in measurement, and we calculated effect size, and transformed the effect back to the units of one or more of the specific instruments.
Unit of analysis issues
1. Cluster trials
Studies increasingly employ 'cluster randomisation' (such as randomisation by clinician or practice) but analysis and pooling of clustered data poses problems. Firstly, authors often fail to account for intra‐class correlation in clustered studies, leading to a 'unit of analysis' error (Divine 1992), whereby P values are spuriously low, CIs unduly narrow and statistical significance overestimated. This causes type I errors (Bland 1997; Gulliford 1999).
If we had included cluster‐randomised trials and clustering had not been accounted for in primary studies, we would have presented data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. In subsequent versions of this review, if such studies are included, we will seek to contact authors of such studies to obtain intra‐class correlation coefficients (ICCs) for their clustered data and to adjust for this by using accepted methods (Gulliford 1999).
Had clustering been incorporated into the analysis of primary studies, we would have presented these data as if from a non‐cluster randomised study, but adjusted for the clustering effect.
We have been advised by a statistical expert that the binary data as presented in a report should be divided by a 'design effect'. This is calculated using the mean number of participants per cluster (m) and the ICC [Design effect=1+(m‐1)*ICC] (Donner 2002). If the ICC was not reported we will assume it to be 0.1 (Ukoumunne 1999).
If cluster studies were appropriately analysed taking into account ICCs and relevant data documented in the report, synthesis with other studies would be possible using the generic inverse variance technique.
2. Cross‐over trials
A major concern of cross‐over trials is the carry‐over effect. It occurs if an effect (e.g. pharmacological, physiological or psychological) of the treatment in the first phase is carried over to the second phase. As a consequence, on entry to the second phase the participants can differ systematically from their initial state, despite a wash‐out phase. For the same reason, cross‐over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both effects are very likely in severe mental illness, we had planned to only use data from the first phase of cross‐over studies.
3. Studies with multiple treatment groups
Had a study involved more than two treatment arms, if relevant, we would have presented the additional treatment arms in comparisons. If data were binary we would simply have added these and combined them within the two‐by‐two table. If data were continuous we would have combined data following the formula in section 7.7.3.8 of the Cochrane Handbook for Systematic reviews of Interventions (Higgins 2011). If the additional treatment arms were not relevant, we would not have used these data.
Dealing with missing data
1. Overall loss of credibility
At some degree of loss of follow‐up, data must lose credibility (Xia 2009). We decided that, for any particular outcome, should more than 50% of data be unaccounted for, we would not use such data within the analyses. If, however, more than 50% of those in one arm of a study were lost, but the total loss was less than 50%, we would have addressed this loss within the 'Summary of findings' table by downgrading quality. We would also have downgraded quality within the 'Summary of findings' table if losses were 25% to 50% in total.
2. Binary
In the case where attrition for a binary outcome was between 0% and 50% and where these data were not clearly described, we would have present these data on a 'once‐randomised‐always‐analyse' basis (an intention‐to‐treat (ITT) analysis). Those leaving the study early were all assumed to have the same rates of negative outcome as those who completed, with the exception of the outcome of death and adverse effects (for these outcomes we planned to use the rate of those who stayed in the study ‐ in that particular arm of the trial ‐ for those who did not). We undertook a sensitivity analysis to test how prone the primary outcomes were to change when data only from people who complete the study to that point were compared to the ITT analysis using the above assumptions.
3. Continuous
3.1 Attrition
In the case where attrition for a continuous outcome was between 0% and 50%, and data only from people who completed the study to that point were reported, we used these data.
3.2 Standard deviations
If standard deviations (SDs) were not reported, firstly we would have tried to obtain the missing values from the authors. If not available, where there were missing measures of variance for continuous data, but an exact standard error (SE) and CIs available for group means, and either a P value or t value available for differences in mean, we would have calculated them according to the rules described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). When only the SE was reported, SDs were calculated by the formula SD=SE * square root (n). Chapters 7.7.3 and 16.1.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) present detailed formulae for estimating SDs from P values, t or F values, CIs, ranges or other statistics. If these formulae did not apply, we would have calculated the SDs according to a validated imputation method, which is based on the SDs of the other included studies (Furukawa 2006). Although some of these imputation strategies can introduce error, the alternative would have been to exclude a given study’s outcome and thus to lose information. We would nevertheless have examined the validity of the imputations in a sensitivity analysis excluding imputed values.
3.3 Assumptions about participants who left the trials early or were lost to follow‐up
Various methods are available to account for participants who left the trials early or are lost to follow‐up. Some trials just present the results of study completers, others use the method of last observation carried forward (LOCF), while more recently methods such as multiple imputation or mixed‐effects models for repeated measurements (MMRM) have become more standard. While the latter methods seem to be somewhat better than LOCF (Leon 2006), we feel that the high percentage of participants leaving the studies early and differences in the reasons for leaving the studies early between groups is often the core problem in randomised schizophrenia trials. We therefore did not exclude studies based on the statistical approach used. However, we would preferably have used more sophisticated approaches such as MMRM or multiple imputation to LOCF, and only presented completer analyses if some kind of ITT data were not available at all. Moreover, we would have addressed this issue in the item 'incomplete outcome data' of the 'Risk of bias' tool.
Assessment of heterogeneity
1. Clinical heterogeneity
We considered all included studies initially, without seeing comparison data, to judge clinical heterogeneity. We simply inspected all studies for clearly outlying people or situations which we had not predicted would arise.
2. Methodological heterogeneity
We considered all included studies initially, without seeing comparison data, to judge methodological heterogeneity. We simply inspected all studies for clearly outlying methods which we had not predicted would arise.
3. Statistical heterogeneity
3.1 Visual inspection
We visually inspected graphs to investigate the possibility of statistical heterogeneity.
3.2 Employing the I2 statistic
We investigated heterogeneity between studies by considering the I2 method alongside the Chi2 P value. The I2 provides an estimate of the percentage of inconsistency thought to be due to chance (Higgins 2003). The importance of the observed value of I2 depends on: i. magnitude and direction of effects and ii. strength of evidence for heterogeneity (e.g. 'P' value from Chi2 test, or a CI for I2). We interpreted an I2 estimate greater than or equal to around 50% accompanied by a statistically significant Chi2 statistic as evidence of substantial levels of heterogeneity (Section 9.5.2, Cochrane Handbook for Systematic Reviews of Interventions) (Deeks 2011). If substantial levels of heterogeneity had been found in the primary outcome, we planned to explore reasons for heterogeneity (Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results (Egger 1997). These are described in section 10.1 of the Cochrane Handbook for Systematic reviews of Interventions (Sterne 2011).
1. Protocol versus full study
We tried to locate protocols of included randomised trials. If the protocol was available, we compared outcomes in the protocol and in the published report. If the protocol was not available, we compared outcomes listed in the methods section of the trial report with actually reported results.
2. Funnel plot
We are aware that funnel plots may be useful in investigating reporting biases but are of limited power to detect small‐study effects. We did not intend to use funnel plots for outcomes where there were 10 or fewer studies, or where all studies were of similar size. Only three studies were included. In future updates of this review, where funnel plots are possible, we will seek statistical advice in their interpretation.
Data synthesis
We understand that there is no closed argument for preference for use of fixed‐effect or random‐effects models. The random‐effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This often seems to be true to us, and the random‐effects model takes into account differences between studies, even if there is no statistically significant heterogeneity. There is, however, a disadvantage to the random‐effects model. It puts added weight onto small studies which often are the most biased. Depending on the direction of effect, these studies can either inflate or deflate the effect size. We chose the fixed‐effect model for all analyses.
Subgroup analysis and investigation of heterogeneity
1. Subgroup analyses
1.1 Primary outcomes
We did not anticipate a need for any subgroup analysis.
1.2 Clinical state, stage or problem
We proposed to undertake this review and provide an overview of the effects of yoga as part of a package of care for people with schizophrenia in general. In addition, however, we planned to report data on subgroups of people in the same clinical state, stage and with similar problems.
2. Investigation of heterogeneity
If inconsistency was high we would have reported it. First, we would have investigated whether data had been entered correctly. Second, if data were correct, the graph would have been visually inspected and we would have removed outlying studies to see if homogeneity was restored. For this review we decided that should this occur with data contributing to the summary finding of no more than around 10% of the total weighting, data would be presented. If not, data would not be pooled and these issues would be discussed. We know of no supporting research for this 10% cut‐off but we used prediction intervals as an alternative to this unsatisfactory state.
If, in future updates of this review, unanticipated clinical or methodological heterogeneity are obvious, we will simply state hypotheses regarding these. We do not anticipate undertaking analyses relating to these.
Sensitivity analysis
1. Implication of randomisation
We planned to include trials in a sensitivity analysis if they were described in some way as to imply randomisation. For the primary outcomes we would have included these studies and if there was no substantive difference when data from implied randomised studies were added to those with a better description of randomisation, then all data would have been employed from these studies.
2. Assumptions for lost binary data
Where assumptions had to be made regarding people lost to follow‐up (see Dealing with missing data), we planned to compare the findings of the primary outcomes when we used our assumption/s and when we compared with completer data only. If there was a substantial difference, we would have reported results and discussed them but continued to employ our assumption.
If assumptions had to be made regarding missing SDs data (see Dealing with missing data), we would have compared the findings of the primary outcomes when we use our assumption/s and when we used data only from people who completed the study to that point. A sensitivity analysis would have been undertaken testing how prone results were to change when completer data only were compared to the imputed data using the above assumption. If there was a substantial difference, we would have reported results and discussed them but continued to employ our assumption.
3. Risk of bias
For the primary outcome, we analysed the effects of excluding trials that we judged to be at high risk of bias across relevant domains (see Assessment of reporting biases) for the meta‐analysis of the primary outcome. If excluding trials at high risk of bias had substantially altered the direction of effect or the precision of the effect estimates, then we would have included relevant data from these trials in the analysis.
4. Imputed values
We intended to undertake a sensitivity analysis to assess, if necessary, the effects of including data from trials where, if necessary, we use imputed values for ICC in calculating the design effect in cluster‐randomised trials.
5. Fixed‐effect and random‐effects
All data were synthesised using a fixed‐effect model, however we also aimed to synthesise data for the primary outcome using a random‐effects model to evaluate whether this altered the significance of the results. If the significance of results had changed, we would have noted this in the text.
Results
Description of studies
Please see Characteristics of included studies, Characteristics of excluded studies, and Characteristics of ongoing studies.
Results of the search
In the searches we undertook for this review, we found 1034 papers that were potentially relevant. We identified no duplicates. After removing 727 articles that were clearly irrelevant, we inspected 307 abstracts. From these, we selected 42 reports for further assessment for inclusion. We then grouped these into 'studies' where several of the reports referred to the same trial. We excluded 19 studies (36 reports), and one study was categorised as an 'ongoing study'. There are no studies awaiting assessment. Thus, the searches generated five reports of three trials, which were included in the meta‐analysis. The PRISMA table shows results of our searches (see Figure 1).

Study flow diagram.
Included studies
1. Methods
No details of blinding of were described in the Paikkatt 2012 and Xie 2006 studies. The Isuru 2015 study provided detail relating to the blinding of the outcome assessor. All studies were parallel studies and were described as randomised. Outcomes were reported immediately after the intervention in all studies. Maintenance was not assessed as no study included a follow‐up period.
2. Length of trials
The overall duration of all included trials was short term, which consisted of three weeks Isuru 2015, one month (Paikkatt 2012) and eight weeks in duration (Xie 2006). No medium‐ or long‐term data were therefore presented by the included trials.
3. Participants
A total of 193 people (n=30 Paikkatt 2012, n=73 Isuru 2015, n=90 Xie 2006) participated in the three studies. Males were included exclusively in one study (Paikkatt 2012), while both men and women were included in the other two (Isuru 2015; Xie 2006).
All studies included people with schizophrenia. Two different diagnostic criteria were employed in this review. Isuru 2015 and Paikkatt 2012 used the ICD‐10 classification while Xie 2006 employed the CCMD‐3 criteria. Xie 2006 stated the cohort included "30 biased schizophrenia and 12 un‐differentiated schizophrenic" participants. No report referred to the current clinical state of participants (acute, early postacute, partial remission, remission), and similarly no report focused on people with particular problems, for example negative symptoms or treatment illnesses. All studies included ''chronic'' hospitalised patients with a minimum duration of illness of two years in one study (Paikkatt 2012) and a mean of almost seven years in the Xie 2006 study. The remaining study (Isuru 2015) did not report the duration, but stated that participants had "long standing" schizophrenia. In this study, 20 participants were admitted for treatment "under court orders to the forensic unit" of the hospital, likely reflecting a complex cohort with multifactorial elements such as unremitting or poorly managed disease manifesting in anti‐social behaviour.
4. Setting
All studies took place in an inpatient setting; in India (Paikkatt 2012), in Sri Lanka Isuru 2015, and in China (Xie 2006).
5. Interventions
5.1 Yoga
The yoga intervention was delivered by a trained yoga instructors in Paikkatt 2012 and by two senior nurses who had training in ''basic yoga theory'' in Xie 2006. Both studies employed supervised group yoga sessions with a yoga instructor:participant ratios of ''less than'' 1:10 in Xie 2006 and the ratio was not specified in Paikkatt 2012.
In the Isuru 2015 study, it was stated that instructors were trained and were from an Academy of Performing Arts. It was reported they had experience of successfully completing rehabilitation programmes for refugees, war victims and ex‐combatants. No instructor:participant ratio was specified in this study.
The yoga programmes described varied between studies. The frequency of yoga sessions provided was every day (except holidays) for ''about'' 1.5 hours for ''about'' one month in Paikkatt 2012. The frequency of yoga sessions was not specified in Xie 2006, but the programme duration was eight weeks in total. Both studies assessed follow‐up after completion of the yoga intervention. In the Isuru 2015 study, the therapy sessions lasted six hours per day and were conducted on eight days over a three‐week period.
The yoga discipline (e.g. Hatha yoga) was not listed in any study included in this review. The yoga intervention consisted of the postures/asanas in the following positions standing, supine, prone lying, sitting and also consisted of breathing (pranayama) exercises in Paikkatt 2012. The inclusion of meditation was not specified in this study. The yoga intervention in Xie 2006 appeared more passive, consisting of ''attention concentrating, breathe adjusting and simple meditation''. No asanas/postures were described, although it did specify that the training was progressed in intensity and complexity once the basics were mastered. No details of the yoga element of the programme was listed in Isuru 2015.
The add‐on element included a motivational and feedback session in Paikkatt 2012. In this study, patients ''were motivated'' by explaining the rationale and positive effects of the yoga practice. The add‐on element in Xie 2006 was a session whereby patients communicated their experiences, and nurses provided counselling and conducted a question and answers session with patients. In Isuru 2015, the add‐on element consisted of 'breathing control training, identification and correct interpretation of basic emotions, observation of others behaviour and mimicking, attention enhancing procedures, maintaining correct body posture'. in this study, the package of care also consisted of basic acting exercises, the Alexander technique, theatre games, exercises "to build self confidence", creative work and music.
The relative time spent conducting different elements, asanas/postures, or the add‐on element was not specified although the total time spent was ''about'' 1.5 hours in Paikkatt 2012 and one hour in Xie 2006. The Isuru 2015 study comprised the longest duration of six hours per day.
No feasibility outcomes were referred to in any study such as satisfaction, compliance or adherence. Self‐practice of yoga was not referred to in any of the included studies.
5.2 Standard‐care control
All studies compared the yoga package against standard care. No other comparator arm was included. In Paikkatt 2012, it was specified that both groups continued on pharmacotherapy. Xie 2006 referred to both groups continuing with ''normal treatment''. In Isuru 2015, it was specified the comparison group received standard care which included medication and occupation therapy. It did not explicitly state in this study whether the experimental arm received medication and occupational therapy, but presumably 'in‐ward treatment' was inclusive of these treatments.
6. Outcomes
The following outcomes for which we could obtain data are listed below, followed by a summary of data that we could not use in this review as well as missing outcomes.
6.1 Outcome scales
6.1.1 Mental state
i. Positive and Negative Syndrome Scale (PANSS) (Kay 1986)
This 30‐item scale assesses severity of psychotic symptomology in general. It consists of three sub‐scales; positive symptoms, negative symptoms general psychopathology, and a total score. Scoring ranges from one to seven, with a low score indicating a lesser severity of symptoms (1=absent, 2=minimal, 3=mild, 4=moderate, 5=moderate severe, 6=severe, 7=extreme). As only median and interquartile ranges were provided for this measure in one study (Isuru 2015), this was included under 'other data'. One further study (Paikkatt 2012) also reported the PANSS, but we were unable to include this data as only the mean (SD) of individual PANSS variables was reported.
6.1.2 Quality of life
i. General Quality of Life Unventory‐74 (GQOLI‐74) (Li 1995)
This questionnaire was created specifically for use in the Chinese population and was based on the WHO Quality of Life Assessment Instrument. The inventory comprises 74 items that can be classified into 20 facets that are then categorised into a global health status/QOL assessment and the following four domains: (1) physical well‐being (sleep and energy, pain and physical discomfort, eating functioning, sexual functioning, sensory functioning, and capability of daily living), (2) psychological well‐being (psychological distress, negative feelings, positive feelings, cognitive functioning, and body/self‐image), (3) social well‐being (social support, interpersonal relationships, work and study capacity, recreational and leisure activities, and marriage and family), and (4) material well‐being (housing situation, community services, living environment, and financial situation) and a total score. Satisfactory levels of reliability and validity have been demonstrated by this instrument (Li 1995; Li 1998).
6.1.3 Activities of daily living
i. Checklist for basic living skills
This checklist consisted of questions related to personal hygiene which consisted of the following seven categories; toileting, brushing teeth, bathing, hair care, nail care, eating habit and house keeping. Paikkatt 2012 reported that rating was done on the basis of a four‐point scale, which ranged from zero to three, where the score of zero suggests that the patient can perform the skill independently and the score three suggests the skill cannot be performed without any help. Presumably, the scale was dichotomised by the study authors as only the absence or presence of the skill was reported. Data for this scale were tabulated under 'other data' as individual variables in sub‐scales of toileting, brushing teeth, bathing, hair care, nail care, eating habit and house keeping were provided, with the absence of a total score. Due to the lengthy nature of the checklist, data for subscales of 'toileting' and 'eating habit' were provided in this review.
6.1.4 General well‐being
i. Post Graduate Institute (PGI) general well‐being measure (Verma 1989)
In 1970, Dr. H Dubey developed a general well‐being schedule, which was a 25‐item, six‐point scale with 33 scores. The Hindi version was used in this study which consists of 20 items (such as feeling happiness, life satisfaction, adequate sleep and feeling good). Participants are required to indicate which questions they agree or disagree with and the number of agreements constitute the well‐being of the individual. Verma 1989 cited that the reliability estimated by the Kuder and Richardson formula‐20 was 0.98 and the coefficient for the test–retest reliability was 0.91. As no total score was supplied, data from this scale were tabulated as 'other data'.
6.2 Missing outcomes
Notably, this review was subject to a large number of missing outcomes. No studies reported data on key outcomes of global state, social functioning or adverse effects. The only outcomes for which we could report data were; leaving the study early and quality of life. Data for the outcomes of mental state, activities of daily living and general well‐being was provided in trials, but was tabulated as 'other data' as no total scores were provided.
Excluded studies
We generated over 1,000 potential studies from this search as detailed in Figure 1. The Trial Search Co‐ordinator excluded 727 studies, and the review authors excluded a further 265 reports as they did not meet study criteria. We examined a further 42 reports in detail. Twenty studies (37 reports) were excluded. One was an ongoing trial (JPRN‐UMIN000013746). The majority of studies were excluded as they included yoga interventions only ‐ as opposed to yoga delivered as part of a package of care. One study investigated the effects of yoga on caregivers, rather than on people with a diagnosis of schizophrenia themselves (Varambally 2013). Two studies (Ramu 1999, Mahal 1976) compared types of drugs rather than yoga interventions. We have provided details of excluded studies in the Characteristics of excluded studies table. Table 2 details comparisons relevant to other reviews suggested by excluded and included studies.
| Intervention | Plus | Control | Participants | Reference tag | Proposed relevant Cochrane review |
| Yoga | Nil | Exercise | People with schizophrenia | Bhatia 2017; Duraiswamy 2007; Lin 2015; Manjunath 2013; Varambally 2012; JPRN‐UMIN000013746 | Yoga versus non‐standard care for schizophrenia |
| Counselling | Standard care | ||||
| Motivational and feedback session | |||||
| Nil | Caregivers of people with schizophrenia | ‐ | |||
| Yoga | Non‐standard care | People with schizophrenia | Yoga as part of a package of care versus non‐standard care | ||
| Chlorpromazine | Nil | Placebo | Chlorpromazine versus placebo for schizophrenia | ||
| 'Tagara' (local drug with antipsychotic properties) and 'Brahmyadiyoga' (an herbal compound) | Nil | Chlorpromazine | Chlorpromazine versus herbal compounds for schizophrenia |
Risk of bias in included studies
See also 'Risk of bias' tables in Characteristics of included studies and Figure 2 and Figure 3.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
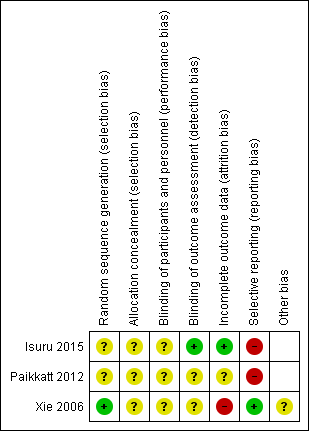
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
All studies included in this review were randomised controlled trials (RCTs). Details of sequence generation were not provided in the Paikkatt 2012 or Isuru 2015 studies, and therefore rated as unclear risk of bias. A coin tossing method was used to generate the sequence Xie 2006 and rated as low risk of bias. No study provided details of the concealment strategy so we judged an unclear risk of bias for allocation concealment in all three trials.
Blinding
Due to the nature of the intervention, none of the studies were able to use a double‐blind technique, since it would not be possible for yoga/control participants or practitioners delivering the yoga package to be blind to group allocation. The risk of performance bias was therefore rated as unclear in all studies. No details were provided on blinding of the outcome assessor two studies which were therefore rated as unclear risk of detection bias (Paikkatt 2012; Xie 2006). Isuru 2015 did state that investigators assessing the outcome measures were blind to the treatment and therefore was rated low risk of detection bias.
Incomplete outcome data
In one study, Paikkatt 2012, even though attrition was low and balanced (n=1 per group), participants who left early were not included in the final analysis, which we therefore rated as an unclear risk of bias. In Xie 2006 attrition bias was rated as high risk as eight participants left early from the yoga group and two from the normal control group which were not included in the final analysis.
Selective reporting
In Paikkatt 2012, reporting bias was rated as high risk of bias as the PGI general well‐being measure is a 20‐item scale, but results for only seven items were reported. Isuru 2015 was also rated as high risk as data were not reported for two outcomes listed. The remaining study in this review Xie 2006 was rated as low risk as all stated outcomes appeared to be reported.
Other potential sources of bias
A possible further source of bias was that data extraction from Xie 2006 study relied on translation from an outside source. No other potential sources of bias were apparent.
Effects of interventions
See: Summary of findings for the main comparison Yoga package versus standard care for schizophrenia
1. COMPARISON 1: Yoga package versus standard care
1.1 Mental state: median and interquartile range (PANSS, low=good)
Unuseable data were reported for mental state and are presented as 'other data'.
1.2 Global state: general well‐being (PGI not improved)
Unuseable data were reported for global state and are presented as 'other data'.
1.3 Quality of life: average endpoint score (GQOLI‐74, high=good, short term)
For quality of life we found a single study (n=80) that measured endpoint scores on the GQOLI‐74. There was a difference, favouring yoga, between the yoga package and standard care (mean difference (MD) 22.93 confidence interval (CI) 19.74 to 26.12, low‐quality evidence).
1.4 Leaving the study early: any reason (short term)
All three included studies reported data relevant to this outcome involving 193 participants. There was no clear difference between treatment groups in numbers leaving the study early (risk difference (RD) 0.06 CI ‐0.01 to 0.13; moderate‐quality evidence; Analysis 1.4, ). This outcome had high levels of heterogeneity (Chi2 = 6.59; df=2.0; P=0.04; I2 = 70%). When Xie 2006 was removed, the I2 decreased to 0%; the result also remained equivocal.
1.5 Activities of daily living (Checklist for basic living skills, low=good)
One trial (n = 28) reported data for daily living activities.
1.5.1 Bathing ‐ does not clean all parts of the body
For this outcome there was a favourable effect for yoga package (RD ‐0.57 CI ‐0.84, ‐0.30).
1.5.2 Eating habit ‐ does not eat sufficient amount
There was no clear difference between treatment groups for this outcome (RD 0.00 CI ‐0.13, 0.13).
1.5.3 Hair care ‐ does not dry hair after washing
There was no clear difference between treatment groups for this outcome (RD 0.00 CI ‐0.13, 0.13).
1.5.4 House keeping ‐ does not keep bed/clothes neat and tidy
For this outcome there was a favourable effect for yoga package (RD ‐0.57 CI ‐0.88, ‐0.27).
1.5.5 Nail care ‐ does not keep nails short and clean
For this outcome there was a favourable effect for yoga package (RD ‐0.36 CI ‐0.70, ‐0.01).
1.5.6 Teeth brushing ‐ does not brush teeth daily
For the outcome of brushing teeth, there was a favourable effect for yoga pakage (RD ‐0.43 CI ‐0.70, ‐0.16).
1.5.7 Toiletting ‐ does not use appropriate place
There was no clear difference between treatment groups for this outcome (RD 0.00, CI ‐0.13 to 0.13)
Discussion
Summary of main results
1. YOGA AS A PACKAGE OF CARE versus STANDARD CARE for schizophrenia
Overall, there was a lack of good‐quality evidence for this comparison with few data available; only three studies could be included in the review. The small number of studies included and significant number of missing outcomes was problematic. For instance, data were only available for 2/7 (leaving the study early, and quality of life) of the predetermined outcomes for the 'Summary of findings' table. Data for important outcomes of mental state, social functioning, general well‐being, activities of daily living, change in physical health, adverse effects and costs of care were either unavailable or unusable. The paucity of data significantly weakens the impact of results.
There was a difference in favour of the yoga package for the outcome of quality of life, but this was based on one study with low‐quality evidence (Xie 2006). Included studies were mostly ranked unclear or high risk of bias.
Data were too scarce to pool results and overall, based on these findings, we can not confidently encourage or dissuade the practice of yoga as a package of care as an adjunct therapy to standard care for people with schizophrenia.
Overall completeness and applicability of evidence
1. Completeness
Evidence was relevant, but overall data were far too sparse to extensively address the objectives of this review. The search strategy identified three trials involving 193 participants comparing yoga as a package of care versus standard‐care control.
A further notable limitation of this review was the absence of medium‐ or long‐term outcomes. It is therefore unknown whether small positive changes seen in the outcome of quality of life deteriorated, maintained, or even continued along the same trends, so further studies reporting medium‐ and particularly long‐term follow‐up are necessary. Indeed, the short‐term follow‐up may influence the directness of evidence given the chronic nature of schizophrenia. Even within short‐term outcomes, no useable data were provided for the majority of outcomes (mental state, general well‐being, activities of daily living, social functioning, physical functioning, adverse effects and costs of care), which weakens the impact of this review.
Even within the limited number of outcomes available, the lack of binary data for the outcome of quality of life, loss to follow‐up and lack of intention‐to‐treat (ITT) analysis means that the central question underlying the review, whether yoga as a package confers any advantage over standard care, cannot be answered with any degree of confidence.
2. Applicability
This review appeared to include relatively homogeneous chronic schizophrenia populations, but diagnostic criteria varied between studies. All studies included hospitalised patients. One study (Isuru 2015) included a significant proportion of participants (20/73) who were admitted for treatment to the forensic psychiatry unit of the hospital. Given the chronicity of this population and inpatient as well as forensic setting, presumably these studies evaluated the effect of a yoga package of care in individuals with more intractable disease, so the wider applicability of results in out‐patient or more newly diagnosed populations is unknown.
All studies took place in non 'Western' settings with one study based in China, one in India and one in Sri Lanka. Yoga in general, may be a more accepted mainstream practice in these countries, perhaps particularly in India, where this practice originated, so the broader implication of these studies is therefore unknown. As resources to obtain yoga training may be more available in some low‐ and middle‐income countries, the implication of these, albeit weak, results may find greater resonance in some non‐'Western' settings.
The first review, within this series of reviews, yoga versus standard care (Broderick 2015) excluded any combinations of yoga and other adjunctive practices such as counselling in an attempt to generate the 'purest' comparison of yoga versus standard care. The inception of the present review was data‐driven, but is also cognisant of the trend to 'fuse' yoga with another practice to form a package of care. Yoga could be combined with another form of exercise or other adjunctive non‐exercise endeavour such as talking therapy, arts therapy or a combination of the above. This review revealed the paucity of studies that have investigated yoga as a package of care. One study combined yoga with a ''motivational and feedback session'' (Paikkatt 2012), while an other study combined yoga with relaxation exercises and a group counselling and question and answers session delivered by two nurses (Xie 2006). The remaining study combined yoga with music, dance and drama therapies (Isuru 2015).
The yoga practice was not consistent between studies, one study included the following yoga postures (asanas); standing postures, lying postures (supine), sitting postures and pranayama‐breathing exercises. The remaining two studies were lacking details on dosage, exposure and nature of progression, with one study reporting the yoga practice consisted of ''attention concentrating'', ''breathe adjusting'' and ''simple meditation'' and seemingly a low proportion of more physical content such as asanas or postures. The other study did not divulge any details about the yoga intervention, and given the list of specific interventions employed, it would seem that yoga formed a very small element of the overall package of care. It is likely that the difference in yoga content and exposure between the studies means the limited results reported in this review cannot be interpreted with any degree of certainty. Yoga is a nuanced heterogeneous practice which has evolved over many years since its inception, based on the training of the instructor and intuitively guided by the energy of the group and a myriad of other factors which are difficult to quantity. The challenges of comparing yoga studies was highlighted in the first review within this series Broderick 2015. It much be acknowledged that comparing yoga as a package of care studies is an even more difficult endeavour due to the diversity of yoga practices and other therapeutic components. Also, the relative effect of each one of these therapies within the package of care is not known, whether it is the synergy of the combined treatments or individual components which dilutes or accelerates benefits.
The three studies included in this review were relatively small, with 193 participants in total. The small size of these studies significantly weakens the quality of evidence presented, therefore any demonstrated difference between the yoga package and control outcomes should be considered in this context. Further studies with a larger sample size should be considered.
Quality of the evidence
See also Risk of bias in included studies and summary of findings Table for the main comparison.
The quality of available data limits our confidence in any changes shown in this review. There was a limited number of outcome measures used in these trials. Data on leaving the study early were available from all three trials. For two trials, leaving the study early were the only useable data (Isuru 2015; Paikkatt 2012). One trial reported a quality of life measure in addition which we included in this review, but the implication of significant change in total mean scores is not known, which limits the utility of this measure. The other trial in this review included the following additional outcome measures; general well‐being, activities of daily living and disability ‐ but data were not useable for these outcomes and none corresponded to the predetermined list of outcomes in the 'Summary of findings' table. Notably, the PANSS which measures mental state‐a critical outcome in this population, was included in two studies but unfortunately was not reported in a useable format.
The quality of the current evidence was low to moderate based on GRADE. Generally, studies were noted to be sparse in terms of methodological detail with a rating of unclear or high risk of bias commonly attributed to studies included in this review. One of the fundamental prerequisites of an RCT methodology is random sequence generation, however this was unclear in two studies, raising concern about selection bias. It was accepted due to the nature of the intervention that study participants and yoga practitioners could not be blind to the intervention. Performance bias may have been problematic in all studies, as blinding of the outcome assessor was unclear. We rated one study as high risk of attrition bias due to incomplete outcome data (Xie 2006), and in the other two studies it was unclear. Selective reporting was rated as at a high risk of bias for two of the studies included in this review (Isuru 2015; Paikkatt 2012). Collectively, these biases should be borne in mind when interpreting the results of this study.
Studies were data extracted from full‐text journal publications, with one study relaying on translation from Chinese from an outside source.
Potential biases in the review process
We aimed the search for studies to be as extensive as possible, and we made every attempt to include global studies and not just those published in the English language. There remains the possibility that there may be other unpublished trials of interventions that the review authors do not currently have access to. This means that the review authors may unwittingly have perpetuated a publication bias.
Agreements and disagreements with other studies or reviews
Cramer 2013 published a review of yoga in schizophrenia but excluded studies containing multimodal interventions, such as mindfulness‐based stress reduction and mindfulness‐based cognitive therapy that included yoga, although the Xie 2006 study which combined yoga with relaxation exercises and a group counselling and question and answers session was included, which overlapped with this review. Multimodal yoga interventions or yoga as a package of care as described within the present review was not specifically listed as an exclusion criterion in the systematic review by Vancampfort 2012 and in the meta‐analysis of Dauwan 2016, but no studies included in the present review were included in the Vancampfort review nor the Dauwan meta‐analysis.

Study flow diagram.
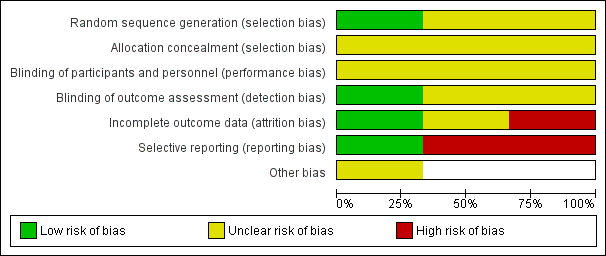
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
| Study | Variable | Yoga package, median (interquartile range) (n = 33) | Control (median, interquartile range) (n = 40) |
| Isuru 2015 | PANSS positive | 15.0 (10.0 to 17.5) | 16.0 (14.0 to 18.0) |
| Isuru 2015 | PANSS negative | 17.0 (11.0 to 22.5) | 18.0 (15.0 to 22.0) |
| Isuru 2015 | PANSS total | 61.0 (49.5 to 72.0) | 63.5 (54.5 to 72.8) |
Comparison 1 Yoga package versus standard care, Outcome 1 Mental state: 1. Average score (PANSS, low = good).
| Study | Sub‐sections | Yoga Package (n = 14) | Control (n = 14) |
| Paikkatt 2012 | Not feeling happiness | 0 | 9 |
| Paikkatt 2012 | Not feeling satisfied | 4 | 4 |
| Paikkatt 2012 | Inadequate sleep | 2 | 2 |
| Paikkatt 2012 | Feeling good | 1 | 7 |
| Paikkatt 2012 | Not in control of anger | 1 | 3 |
| Paikkatt 2012 | Not feeling worthy | 1 | 7 |
| Paikkatt 2012 | Not feeling healthy | 0 | 4 |
Comparison 1 Yoga package versus standard care, Outcome 2 Global state: General well‐being: not improved (PGI general well‐being measure, low = good).

Comparison 1 Yoga package versus standard care, Outcome 3 Quality of life: Average end‐point score (GQOLI‐74, high = good) short term.
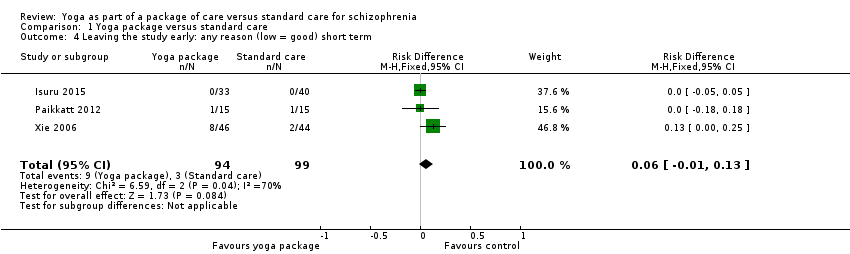
Comparison 1 Yoga package versus standard care, Outcome 4 Leaving the study early: any reason (low = good) short term.
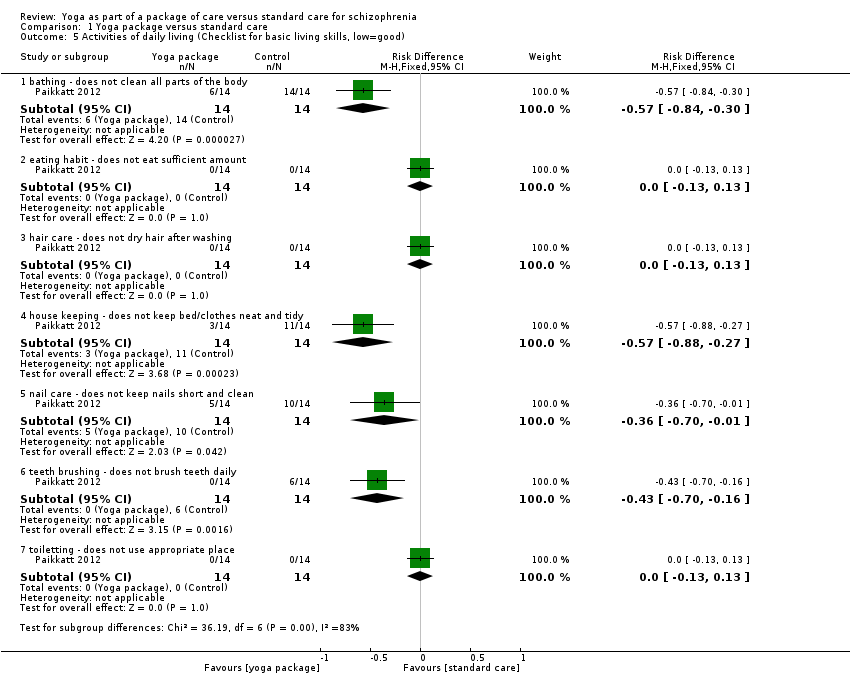
Comparison 1 Yoga package versus standard care, Outcome 5 Activities of daily living (Checklist for basic living skills, low=good).
| Methods | Allocation: randomised (clearly described). |
| Participants | Diagnosis: people with a clinical diagnosis of schizophrenia using DSM‐IV criteria. |
| Interventions | 1. Yoga: the yoga intervention should be clearly described and consist of the following components: (i) shithileekarana vyayama (loosening exercises) for approximately 10 minutes, (ii) yoga postures (asanas) for approximately 20 minutes, (iii) breathing exercises and relaxation techniques for approximately 20 minutes using a manualised protocol, yoga programme for 12 weeks, 3 times weekly, follow‐up at 6 months and 1 year, yoga delivered by a trained yoga instructor, meditation not included. 2. Standard‐care control. All groups stable pharmacotherapy. |
| Outcomes | Mental state (binary outcomes). Relapses (binary outcomes). Quality of life (binary outcomes). Disability (binary outcomes). Activities of daily living (binary outcomes). Costs: cost of services, cost of care. Adverse events related to yoga (number and type of injuries). Service outcomes: days in hospital, time attending outpatient psychiatric clinic. |
| Notes | Adherence should be logged with participants expected to adhere to 70% to 75% of scheduled sessions. |
| DSM‐IV:Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition | |
| Yoga package versus standard care for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Yoga package versus standard care | |||||
| Mental State: clinically important change | No useable mental state data reported. | |||||
| Social functioning: clinically important change | No study reported on social functioning. | |||||
| Adverse events: clinically important adverse effect | No study reported on adverse effects. | |||||
| Quality of life: clinically important change* Follow‐up: mean 4 weeks | The mean quality of life (GQOLI‐74) in the intervention groups was | 80 | ⊕⊕⊝⊝ | * Clinically important data not available: nearest outcome reported were Average endpoint scores on the GQOLI‐74 | ||
| Leaving the study early: any reason Leaving the study early: participants lost to follow‐up ‐ short term (low=good) | Low1 | 0.06 [‐ 0.01 to 0.13] | 193 (3 studies) | ⊕⊕⊕⊝ | ||
| 800 per 1000 | 1000 per 1000 (640 to 1000) | |||||
| Moderate1 | ||||||
| 900 per 1000 | 1000 per 1000 (720 to 1000) | |||||
| High1 | ||||||
| 1000 per 1000 | 1000 per 1000 (800 to 1000) | |||||
| Costs of care: direct and indirect | No study reported direct or indirect costs of care. | |||||
| Physical health: clinically important change | No study reported on physical health. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Imprecision: Downgraded one level as a number of participants withdrew from two trials, not accounted for in final analysis. 3Imprecision: Downgraded one level due to relatively small number of participants included. | ||||||
| Review number | Review Title | Status |
| 1 | Yoga versus standard care for schizophrenia | |
| 2 | Yoga versus non‐standard care for schizophrenia | |
| 3 | Yoga as part of a package of care versus standard care | Current review |
| 4 | Yoga as part of a package of care versus non‐standard care |
| Intervention | Plus | Control | Participants | Reference tag | Proposed relevant Cochrane review |
| Yoga | Nil | Exercise | People with schizophrenia | Bhatia 2017; Duraiswamy 2007; Lin 2015; Manjunath 2013; Varambally 2012; JPRN‐UMIN000013746 | Yoga versus non‐standard care for schizophrenia |
| Counselling | Standard care | ||||
| Motivational and feedback session | |||||
| Nil | Caregivers of people with schizophrenia | ‐ | |||
| Yoga | Non‐standard care | People with schizophrenia | Yoga as part of a package of care versus non‐standard care | ||
| Chlorpromazine | Nil | Placebo | Chlorpromazine versus placebo for schizophrenia | ||
| 'Tagara' (local drug with antipsychotic properties) and 'Brahmyadiyoga' (an herbal compound) | Nil | Chlorpromazine | Chlorpromazine versus herbal compounds for schizophrenia |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mental state: 1. Average score (PANSS, low = good) Show forest plot | Other data | No numeric data | ||
| 2 Global state: General well‐being: not improved (PGI general well‐being measure, low = good) Show forest plot | Other data | No numeric data | ||
| 3 Quality of life: Average end‐point score (GQOLI‐74, high = good) short term Show forest plot | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 22.93 [19.74, 26.12] |
| 4 Leaving the study early: any reason (low = good) short term Show forest plot | 3 | 193 | Risk Difference (M‐H, Fixed, 95% CI) | 0.06 [‐0.01, 0.13] |
| 5 Activities of daily living (Checklist for basic living skills, low=good) Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 bathing ‐ does not clean all parts of the body | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.57 [‐0.84, ‐0.30] |
| 5.2 eating habit ‐ does not eat sufficient amount | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] |
| 5.3 hair care ‐ does not dry hair after washing | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] |
| 5.4 house keeping ‐ does not keep bed/clothes neat and tidy | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.57 [‐0.88, ‐0.27] |
| 5.5 nail care ‐ does not keep nails short and clean | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.36 [‐0.70, ‐0.01] |
| 5.6 teeth brushing ‐ does not brush teeth daily | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.43 [‐0.70, ‐0.16] |
| 5.7 toiletting ‐ does not use appropriate place | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] |

