Apendicectomía temprana versus diferida para el absceso y el flemón apendicular
Resumen
Antecedentes
El absceso y el flemón apendicular representan del 2% al 10% de las apendicitis agudas. Los pacientes con absceso o flemón apendicular generalmente requieren una apendicectomía para aliviar los síntomas y evitar las complicaciones. El momento de realizar la apendicectomía para el absceso o el flemón apendicular es polémico.
Objetivos
Evaluar los efectos de la apendicectomía temprana versus diferida para el absceso y el flemón apendicular, en cuanto a la morbilidad general y la mortalidad.
Métodos de búsqueda
Se hicieron búsquedas en la Cochrane Library (CENTRAL; 2016, número 7), MEDLINE Ovid (1950 hasta 23 agosto 2016), Embase Ovid (1974 hasta 23 agosto 2016), Science Citation Index Expanded (1900 hasta 23 agosto 2016), y en la Chinese Biomedical Literature Database (CBM) (1978 hasta 23 agosto 2016). También se hicieron búsquedas de ensayos en curso en el World Health Organization (WHO) International Clinical Trials Registry Platform search portal (23 agosto 2016) y en ClinicalTrials.gov (23 agosto 2016).
Criterios de selección
Se incluyeron todos los ensayos controlados aleatorios individuales y grupales independientemente del idioma, el estado de publicación o la edad de los participantes, que compararon apendicectomía temprana versus diferida en pacientes con absceso y flemón apendicular.
Obtención y análisis de los datos
Dos autores de la revisión, de forma independiente, identificaron los ensayos para la inclusión, recopilaron los datos y evaluaron el riesgo de sesgo. Se realizaron metanálisis utilizando Review Manager 5. Se calculó el cociente de riesgos (CR) para los resultados dicotómicos y la diferencia de medias (DM) para los resultados continuos con intervalos de confianza (IC) del 95%.
Resultados principales
Se incluyeron dos ensayos controlados aleatorios con un total de 80 participantes en esta revisión.
1. Apendicectomía abierta temprana versus diferida para el flemón apendicular
Cuarenta participantes (pediátricos y adultos) con flemón apendicular se asignaron al azar a apendicectomía temprana (apendicectomía tan pronto la masa apendicular se detectó en el transcurso del ingreso) (n = 20), o a apendicectomía diferida (tratamiento conservador inicial seguido de apendicectomía en un intervalo de seis semanas después) (n = 20). El ensayo presentaba un alto riesgo de sesgo. No se registraron muertes en ningún grupo. No hay evidencia suficiente para determinar el efecto de utilizar la apendicectomía abierta temprana ni diferida sobre la morbilidad general (CR 13,00; IC del 95%: 0,78 a 216,39; evidencia de muy baja calidad), la proporción de participantes que desarrollaron infección de la herida (CR 9,00; IC del 95%: 0,52 a 156,91; evidencia de muy baja calidad) o fístula fecal (CR 3,00; IC del 95%: 0,13 a 69,52; evidencia de muy baja calidad). En el grupo de apendicectomía temprana la calidad de la evidencia de un aumento en la duración de la estancia hospitalaria y el tiempo que los pacientes estuvieron alejados de las actividades normales (DM 6,70 días; IC del 95%: 2,76 a 10,64 y DM 5,00 días; IC del 95%: 1,52 a 8,48; respectivamente) es de muy baja calidad. El ensayo no informó ni la calidad de vida ni los resultados del dolor.
2. Apendicectomía laparoscópica temprana versus diferida para el absceso apendicular
Cuarenta participantes pediátricos con absceso apendicular se asignaron al azar a apendicectomía temprana (apendicectomía laparoscópica urgente) (n = 20) o a apendicectomía diferida (tratamiento conservador inicial seguido de apendicectomía laparoscópica en un intervalo de diez semanas después) (n = 20). El ensayo presentaba un alto riesgo de sesgo. El ensayo no informó la morbilidad general ni las complicaciones. No se registraron muertes en ningún grupo. No hubo evidencia suficiente para determinar los efectos de la apendicectomía laparoscópica temprana ni diferida en resultados relacionados con la estancia hospitalaria entre los grupos (DM ‐0,20 días; IC del 95%: ‐3,54 a 3,14; evidencia de muy baja calidad). La calidad de vida relacionada con la salud se midió con el cuestionario Pediatric Quality of Life Scale‐Version 4.0 (una escala de 0 a 100 donde los valores mayores indican una mejor calidad de vida). La puntuación de la calidad de vida relacionada con la salud medida a las 12 semanas después de la apendicectomía fue mayor en el grupo de apendicectomía temprana que en el grupo de apendicectomía diferida (DM 12,40 puntos; IC del 95%: 9,78 a 15,02), pero la calidad de la evidencia fue muy baja. Este ensayo no informó el dolor ni el tiempo que los pacientes estuvieron alejados de las actividades normales.
Conclusiones de los autores
No está claro si la apendicectomía temprana evita las complicaciones en comparación con la apendicectomía diferida en los pacientes con absceso y flemón apendicular. La evidencia que indica un aumento en la duración de la estancia hospitalaria y el tiempo que los pacientes estuvieron alejados de las actividades normales en los pacientes con apendicectomía abierta temprana es de muy baja calidad. La evidencia de una mejor calidad de vida relacionada con la salud después de la apendicectomía laparoscópica temprana en comparación con la apendicectomía diferida es de muy baja calidad. En ambas comparaciones analizadas en esta revisión los datos son escasos y no es posible descartar efectos beneficiosos ni perjudiciales significativos de la apendicectomía temprana versus diferida.
En este tema se necesitan urgentemente ensayos adicionales que deben especificar un conjunto de criterios para el uso de los antibióticos, el drenaje percutáneo del absceso apendicular antes de la cirugía y la resolución del absceso y el flemón apendicular. Los ensayos futuros deben incluir resultados como el tiempo que los pacientes están alejados de las actividades normales, la calidad de vida y la duración de la estancia hospitalaria.
PICO
Resumen en términos sencillos
Extracción quirúrgica temprana o diferida del apéndice en pacientes con apendicitis sintomática complicada
Pregunta de la revisión
¿Cuáles son los riesgos y los beneficios de la extracción temprana versus diferida del apéndice en los pacientes con apendicitis sintomática complicada?
Antecedentes
El apéndice humano es un conducto que se encuentra a nivel de la conexión del intestino delgado y grueso. Las posibles funciones del apéndice pueden ser proteger el cuerpo contra la infección y mantener niveles saludables de bacterias en los intestinos cuando se recuperan de la diarrea. La apendicitis incluye diversas afecciones clínicas debidas a la inflamación del apéndice.
La apendicitis complicada se define como un flemón apendicular (masa inflamatoria simple sin pus localizado en el lado inferior derecho del apéndice) o un absceso apendicular (bolsa de pus que rodea un apéndice con inflamación aguda o roto). Los pacientes con esta afección generalmente requieren la extracción quirúrgica del apéndice para aliviar los síntomas y evitar las complicaciones. El momento de la extracción quirúrgica del apéndice es polémico. La cirugía inmediata es técnicamente exigente. Algunos expertos cuestionan lo adecuado de la apendicectomía diferida, ya que los pacientes tienen pocas probabilidades de presentar una recurrencia después de un tratamiento no quirúrgico exitoso. Sin embargo, el diagnóstico verdadero podría no estar claro en algunos casos, y aplazar la apendicectomía puede retrasar el diagnóstico de la enfermedad subyacente.
Características de los estudios
Se buscaron todos los ensayos controlados aleatorios relevantes hasta el 23 de agosto de 2016. Se identificaron dos ensayos con 80 participantes. Uno comparó apendicectomía abierta temprano versus diferida en 40 niños y adultos con flemón apendicular. El otro ensayo comparó apendicectomía por mínimo acceso (laparoscópica) (cuando la cirugía se realiza mediante una incisión muy pequeña) temprana versus diferida en 40 niños con absceso apendicular. Se realizaron estudios en los Estados Unidos e India. La edad de los pacientes de los ensayos varió entre un año y 84 años, y el 27,5% eran mujeres.
Resultados clave
Ambos estudios fueron pequeños y tuvieron varias limitaciones, por lo que no es posible estar seguros acerca de cómo se comparan los efectos de los dos enfoques quirúrgicos. A partir de un ensayo en niños y adultos que comparó apendicectomía abierta con diferida, no hubo evidencia suficiente para mostrar el efecto de utilizar cualquiera de los enfoques sobre la tasa general de complicación o la proporción de participantes que desarrollaron infección de la herida. La confiabilidad con respecto a un aumento en la estancia hospitalaria y en el tiempo de alejamiento de las actividades normales con la apendicectomía abierta es muy baja. No se registraron muertes en el estudio. La calidad de vida y el dolor no se informaron en este ensayo.
El otro ensayo en niños con absceso apendicular que recibieron apendicectomía por mínimo acceso temprana o diferida no informó las tasas generales de complicación. El ensayo no proporcionó evidencia suficiente para mostrar el efecto de utilizar cualquier enfoque sobre la duración de la estancia hospitalaria entre los participantes. Hay una confiabilidad muy baja con respecto a que los niños a los que se les realizó apendicectomía por mínimo acceso temprana tuvieran una mejor calidad de vida en comparación con los niños que recibieron apendicectomía por mínimo acceso diferida. El estudio no informó si hubo alguna muerte y no proporcionó información sobre el dolor ni sobre el tiempo que los pacientes estuvieron alejados de las actividades normales.
Actualmente los efectos beneficiosos y perjudiciales de la apendicectomía temprana versus diferida no se comprenden bien porque la información actual se basa en evidencia de muy baja calidad.
Calidad de la evidencia
Ambos ensayos presentaban un alto riesgo de sesgo. En general, la calidad de la evidencia se consideró muy baja. Por lo tanto, se necesitan urgentemente más ensayos bien diseñados.
Authors' conclusions
Summary of findings
| Early versus delayed open appendicectomy for appendiceal phlegmon | ||||||
| Patient or population: paediatric and adult patients with appendiceal phlegmon | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed appendicectomy | Early appendicectomy | |||||
| Overall morbidity Median follow‐up: 33,5 months | 0 per 1000 | 300 per 1000 | RR 13.00 | 40 | ⊕⊝⊝⊝ | — |
| Wound infection Median follow‐up: 33,5 months | 0 per 1000 | 200 per 1000 | RR 9.00 | 40 | ⊕⊝⊝⊝ | — |
| Faecal fistula Median follow‐up: 33,5 months | 0 per 1000 | 50 per 1000 | RR 3.00 | 40 | ⊕⊝⊝⊝ | — |
| Mortality Median follow‐up: 33,5 months | See comment | See comment | Not estimable | 40 | ⊕⊕⊝⊝ | There was no mortality in either group. |
| Total length of hospital stay (days) Follow‐up: 3 weeks | The mean total length of hospital stay in the delayed appendicectomy group was 14.7 days | The mean total length of hospital stay in the early appendicectomy group was 6.7 days higher | MD 6.70 (2.76 to 10.64) | 40 | ⊕⊝⊝⊝ | — |
| Time away from normal activities (days) Median follow‐up: 33,5 months | The mean time away from normal activities in the delayed appendicectomy group was 20 days | The mean time away from normal activities in the early appendicectomy group was 5 days higher | MD 5.00 (1.52 to 8.48) | 40 | ⊕⊝⊝⊝ | — |
| Quality of life Median follow‐up: 33,5 months | Not reported | |||||
| Pain (days) Follow‐up: 3 weeks | Not reported | |||||
| *The basis for the assumed risk was the control group proportion in the study. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded one level for serious risk of bias. | ||||||
| Early versus delayed laparoscopic appendicectomy for appendiceal abscess | ||||||
| Patient or population: paediatric participants with appendiceal abscess Setting: secondary and tertiary care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed appendicectomy | Early appendicectomy | |||||
| Overall morbidity | Not reported | |||||
| Wound infection | Not reported | |||||
| Faecal fistula | Not reported | |||||
| Mortality Follow‐up: 12 weeks | See comment | See comment | Not estimable | 40 | ⊕⊝⊝⊝ | There was no mortality in either group. |
| Total length of hospital stay (days) Follow‐up: 12 weeks | The mean total length of hospital stay in the delayed appendicectomy group was 6.7 days | The mean total length of hospital stay in the early appendicectomy group was 0.2 days lower | MD −0.20 (−3.54 to 3.14) | 40 | ⊕⊝⊝⊝ | — |
| Time away from normal activities (days) | Not reported | |||||
| Quality of life (Pediatric Quality of Life Scale‐Version 4.0, a scale of 0 to 100 with higher values indicating better quality of life) Follow‐up: 12 weeks | The mean quality of life score in the delayed appendicectomy group was 84.37 points | The mean quality of life score in the early appendicectomy group was 12.40 points higher | MD 12.40 (9.78 to 15.02) | 40 | ⊕⊝⊝⊝ | We considered the observed mean difference in quality of life score to be clinically significant. |
| Pain (days) | Not reported | |||||
| *The basis for the assumed risk was the control group proportion in the study. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded two levels due to very serious imprecision (small sample size). | ||||||
Background
Description of the condition
Appendicitis refers to inflammation of the appendix. Acute appendicitis is the most common cause of acute abdominal pain (Andersen 2005; Cheng 2015a; Rehman 2011; Wilms 2011). The overall incidence of acute appendicitis varies between 76 and 227 cases per 100,000 population per year in different countries (Addiss 1990; Andersson 1994; Andreu‐Ballester 2009; Buckius 2012; Körner 1997; Lee 2010; Pieper 1982; Williams 1998). The overall lifetime risk for acute appendicitis is approximately 7% to 8% in the USA and 16% in South Korea (Addiss 1990; Lee 2010). It affects all age groups, with the highest incidence in the second decade of life (Addiss 1990; Anderson 2012; Wilms 2011).
Acute appendicitis can be broadly divided into two subgroups: simple appendicitis (e.g. early or uncomplicated appendicitis) and complicated appendicitis (e.g. gangrenous appendicitis and appendiceal phlegmon or abscess) (Andersen 2005; Cheng 2015a; Simillis 2010).
The most common type is simple appendicitis, which is the early stage of acute appendicitis (Andersen 2005; Cheng 2015a; Simillis 2010). In case of a missed or delayed diagnosis of simple appendicitis, the appendix may become gangrenous, potentially leading to perforation and localised or generalised peritonitis (inflammation of the peritoneum), resulting in complicated appendicitis (Andersen 2005; Cheng 2015a; Cheng 2015b; Deelder 2014; Simillis 2010).
Appendiceal phlegmon and appendiceal abscess present as a mass, resulting from both inflammation and walled‐off perforation of the appendix (Ahmed 2005; Nitecki 1993). A walled‐off appendiceal perforation differs from a simple inflammatory mass – consisting of the inflamed appendix, its adjacent viscera and the greater omentum (an appendiceal phlegmon) – in that it containspus (an appendiceal abscess) (Ahmed 2005; Nitecki 1993). The proportion of appendiceal mass (phlegmon or abscess) in acute appendicitis ranges from 2% to 10% in different case series studies (Andersson 2007; Cueto 2006; Oliak 2000; Shipsey 1985; Willemsen 2002), with higher risk in children and the elderly whose diagnosis or therapy of acute appendicitis are delayed (Andersson 1994; Boomer 2010; Cirocchi 2008; Livingston 2007; Oliak 2000).
The prognosis for an appendiceal phlegmon or abscess is good (Markides 2010; Santacroce 2012). The overall mortality rate of appendiceal phlegmon or abscess is less than 1% (Cueto 2006; Markides 2010; Santacroce 2012). However, appendiceal phlegmon or abscess is associated with higher morbidity than simple appendicitis (Andersen 2005; Cheng 2015a; Cueto 2006; Simillis 2010). Common postoperative complications include wound infections, intra‐abdominal abscesses, incisional hernias and bowel obstructions (Blakely 2011; Cueto 2006; Frazee 1996; Kang 2000; Kumar 2004; St Peter 2010; Yau 2007).
Description of the intervention
Appendicectomy, or surgical removal of the appendix, is performed primarily as an emergency procedure to treat acute appendicitis (Andersen 2005; Andersen 2015). People with simple appendicitis usually need either an antibiotic treatment or an appendicectomy to relieve their symptoms and avoid complications (Markides 2010; Salminen 2015; Santacroce 2012; Sauerland 2010; Vons 2011; Wilms 2011). Appendicectomy is one of the most common emergency surgical procedures performed (Santacroce 2012); there are approximately 300,000 each year in the USA alone (Hall 2010). There are two types of appendicectomy: open appendicectomy (removal of the appendix by laparotomy) and laparoscopic appendicectomy (removal of the appendix by keyhole surgery) (Cheng 2012; Cheng 2013; Markides 2010; Sauerland 2010).
Surgery for people with complicated appendicitis may be early or delayed (Andersson 2007; Markides 2010; Simillis 2010). While there is no universally accepted definition of early appendicectomy (Andersson 2007; Simillis 2010), we considered that in people with appendiceal phlegmon or abscess, any appendicectomy performed immediately or several days later within the same admission was early appendicectomy. Delayed appendicectomy (also known as interval appendicectomy) is defined as initial conservative (non‐surgical) treatment followed by appendicectomy several weeks later within a later admission. The role of delayed appendicectomy for people with appendiceal phlegmon or abscess is controversial: some authors have suggested that delayed appendicectomy is not necessary unless the person presents with recurrent symptoms (Andersson 2007; Willemsen 2002), whereas others do not agree (Deelder 2014; Gillick 2001). Patients in the delayed appendicectomy group usually need antibiotics to relieve their symptoms and sometimes require percutaneous drainage of appendiceal abscesses (Andersson 2007; Simillis 2010). Overall, studies report surgical morbidity ranging from 2% to 30% in different case series studies (Blakely 2011; Cueto 2006; Frazee 1996; Kang 2000; Kumar 2004; St Peter 2010; Yau 2007).
How the intervention might work
Common management of appendiceal phlegmon or abscess involves initial conservative treatment with antibiotics followed by delayed appendicectomy (Andersson 2007; Kumar 2004; Simillis 2010). In theory, conservative treatment localises the inflammatory process and decreases the risk of surgical complications when compared with early appendicectomy during the acute inflammatory phase (Andersson 2007; Kumar 2004; Simillis 2010). Delayed appendicectomy can prevent the recurrence of appendicitis, which may occur if there is no appendicectomy at all (Andersson 2007; Kumar 2004; Simillis 2010). However, delayed appendicectomy involves waiting several weeks, during which time the appendicitis may worsen, develop complications or recur following the temporary success of the conservative treatment (Andersson 2007; Kumar 2004). Overall, the success rate of conservative treatment is approximately 90% (Andersson 2007), but when it fails, people may experience substantial morbidity (Andersson 2007; Simillis 2010). Moreover, the true diagnosis could be uncertain in some cases, and postponing surgery could delay diagnosis of underlying cancer or Crohn's disease.
With the growing experience of surgeons and the development of surgical instruments, authors have increasingly reported the safety and feasibility of early appendicectomy in appendiceal phlegmon or abscess (Blakely 2011; Frazee 1996; Kang 2000; Markides 2010; St Peter 2010; Yau 2007). Early appendicectomy can address appendiceal phlegmon or abscess in a single admission without the risk of recurrent appendicitis (Andersson 2007; Kumar 2004; Simillis 2010), and it may reduce the time away from normal activities for patients (Blakely 2011). However, there are concerns about the high morbidity associated with an early appendicectomy (i.e. challenging closure, suture of the inflamed appendix stump) (Andersson 2007; Simillis 2010), with the potential for unnecessary ileocaecal (ileum and cecum) resection or right‐sided hemicolectomy (surgical removal of the right side of the colon) due to a technical problem or suspicion of malignancy (Andersson 2007; Simillis 2010).
Why it is important to do this review
Given the pros and cons for both early and delayed appendicectomy, the timing of appendicectomy for appendiceal phlegmon or abscess remains controversial (Ahmed 2005). Until now, there has been no Cochrane Review assessing the roles of early and delayed appendicectomy for appendiceal phlegmon or abscess.
Objectives
To assess the effects of early versus delayed appendicectomy for appendiceal phlegmon or abscess, in terms of overall morbidity and mortality.
Methods
Criteria for considering studies for this review
Types of studies
We included all individual and cluster‐randomised controlled trials (RCTs) comparing early versus delayed appendicectomy in people with appendiceal phlegmon or abscess. We excluded quasi‐randomised trials (in which allocation is based on a pseudo‐random sequence, e.g. odd/even hospital number or date of birth, alternation) and non‐randomised studies because of the high risk of bias in such studies.
Types of participants
We included all people (both children and adults, irrespective of sex or ethnicity) who underwent appendicectomy (elective and emergent) for appendiceal phlegmon or abscess. Preoperative diagnosis of appendiceal phlegmon or abscess could be established using medical history, physical examination, and imaging results (e.g. ultrasonography, computer tomography). Use of antibiotics and percutaneous drainage of appendiceal abscess were allowed for participants in both groups.
Types of interventions
We included trials comparing early appendicectomy with delayed appendicectomy (irrespective of whether the surgical procedure was open or laparoscopic). We defined early appendicectomy as appendicectomy performed immediately or several days later within the same admission. Delayed appendicectomy was performed several weeks after initial diagnosis in a later admission.
Types of outcome measures
Primary outcomes
-
Overall morbidity (overall complication rate defined by study authors and graded by the Clavien‐Dindo complications classification system) (Clavien 2009)
-
Wound infection (time point closest to 14 days)
-
Abdominal abscess (time point closest to 14 days)
-
Bowel obstruction (time point closest to 14 days)
-
Incisional hernia (time point closest to 90 days)
-
Faecal fistula (time point closest to 14 days)
-
-
Mortality (death rate after operation, time point closest to 90 days)
Secondary outcomes
-
Length of hospital stay
-
Duration of first hospitalisation
-
Total hospital stay
-
-
Time away from normal activities
-
Quality of life (time point closest to 90 days, any validated score)
-
Pain (days with pain)
Search methods for identification of studies
We designed the search strategies with the help of the Cochrane Colorectal Cancer Group (CCCG) Information Specialist (Sys Johnsen). We conducted the searches irrespective of language, year or publication status.
Electronic searches
We searched the following electronic databases with no language or date of publication restrictions.
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2016, Issue 7) in the Cochrane Library (Appendix 1).
-
MEDLINE Ovid (1950 to 23 August 2016) (Appendix 2).
-
Embase Ovid (1974 to 23 August 2016) (Appendix 3).
-
Science Citation Index Expanded in the Web of Science (1900 to 23 August 2016) (Appendix 4).
-
Chinese Biomedical Literature Database (CBM) (1978 to 23 August 2016) (Appendix 5).
Searching other resources
We searched the following databases to identify ongoing trials: the World Health Organization (WHO) International Clinical Trials Registry Platform search portal (apps.who.int/trialsearch), ClinicalTrials.gov (www.clinicaltrials.gov), Current Controlled Trials (www.controlled‐trials.com), Chinese Clinical Trial Register (www.chictr.org), and the EU Clinical Trials Register (www.clinicaltrialsregister.eu). We searched the meeting abstracts via the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) (www.sages.org), the Society for Surgery of the Alimentary Tract (SSAT) (ssat.com), and Conference Proceedings Citation Index to explore further relevant clinical trials. We also searched the reference lists in included studies and any relevant systematic reviews identified.
Data collection and analysis
We conducted the systematic review according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011); we also guided our work according to the Cochrane Colorectal Cancer Group module.
Selection of studies
After completing the searches, we merged the search results using Endnote X7 reference management software and removed duplicate records. Two review authors (LJ, WS) independently scanned the title and abstract of every record identified by the search for inclusion. We retrieved the full text for further assessment if the inclusion criteria were unclear from the abstract. We detected duplicate publications by identifying common authors, centres, details of the interventions, numbers of participants and baseline data (Higgins 2011). We excluded papers not meeting the inclusion criteria and listed the reasons for the exclusion. We included all eligible studies irrespective of whether they reported measured outcome data. The two review authors resolved any disagreements by discussion with a third review author (CY).
Data extraction and management
To extract study characteristics and outcome data, we used a standard data collection form that we had piloted on at least one study in the review. Two review authors (XX, ZR) extracted the following study characteristics from included studies.
-
Methods: study design, total duration study and run‐in, number of study centres and location, study setting, withdrawals, date of study.
-
Participants: total number of participants, mean age, age range, sex, severity of condition, diagnostic criteria, inclusion criteria, exclusion criteria.
-
Interventions: intervention, comparison.
-
Outcomes: primary and secondary outcomes specified and collected, time points reported.
-
Notes: funding for trial, notable conflicts of interest of trial authors.
Two review authors (XX, ZR) independently extracted outcome data from included studies. We resolved disagreements by consensus or by involving a third person (CY). One review author (CN) copied across the data from the data collection form into the Review Manager 5 (RevMan 5) file (RevMan 2014). We double checked that the data were entered correctly by comparing the study reports with the presentation of the data in the systematic review. A second review author (CY) spot‐checked study characteristics for accuracy against the trial report.
Assessment of risk of bias in included studies
Two review authors (LJ, WS) independently assessed risk of bias in the included trials based on the following domains: random sequence generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective reporting; and differences in baseline characteristics (Appendix 6). Following evaluation of the above domains, we assigned a 'low risk of bias' judgement to included trials with a low risk of bias in all of the assessed domains. If we judged the risk of bias to be unclearor high, we listed the trial under the group of trials as 'high risk of bias' trials. We resolved any difference in opinion by discussion. In cases of unsettled disagreements, a third review author (CY) adjudicated. We presented the results of the risk of bias assessment in two figures (a 'Risk of bias' graph figure and a 'Risk of bias' summary figure), which we generated using RevMan 2014.
Measures of treatment effect
We performed the meta‐analysis using RevMan 5 software (RevMan 2014). For dichotomous outcomes, we calculated risk ratio (RR) with 95% confidence interval (CI) (Deeks 2011). In case of rare events (e.g. mortality), we planned to calculate the Peto odds ratio (OR) (Deeks 2011). For continuous outcomes, we calculated the mean difference (MD) with 95% confidence interval (Deeks 2011). For continuous outcomes with different measurement scales in different randomised controlled trials, we planned to calculate the standardised mean differences (SMD) with 95% CIs (Deeks 2011).
Unit of analysis issues
The unit of analysis was the individual participant. We did not find any cluster‐randomised trial for this review. In case of a cluster‐randomised trial, we intended to analyse the data adjusted for clustering using the generic inverse‐variance method in RevMan 5 (Higgins 2011).
Dealing with missing data
We contacted the original investigators to request further information in case of missing data. However, there was no reply. Thus, we used only the available data in the analyses.
Assessment of heterogeneity
We planned to describe the heterogeneity in the data using the Chi2 test (Deeks 2011). We considered a P value less than 0.10 to indicate statistically significant heterogeneity (Deeks 2011). We also planned to use the I2 statistic to measure the quantity of heterogeneity. In case of statistical heterogeneity, clinical heterogeneity (variability in the participants, interventions and outcomes studied) or both, we planned to perform the meta‐analysis but interpret the result cautiously and to investigate potential sources of heterogeneity.
Assessment of reporting biases
We planned to use funnel plots to assess reporting biases, using visual asymmetry to determine the presence of reporting biases (Sterne 2011). We also planned to perform linear regression to determine funnel plot asymmetry (Egger 1997). We did not create funnel plots to assess reporting biases, as the number of trials included was fewer than 10 (Sterne 2011).
Data synthesis
We planned to perform the meta‐analysis using RevMan 2014. We would have employed the random‐effects model for the analysis. We considered a P value less than 0.05 to be statistically significant.
However, we did not perform any meta‐analysis because we included only a single trial for each outlined outcome.
Subgroup analysis and investigation of heterogeneity
We would have performed the following subgroup analyses if we had found enough trials.
-
Laparoscopic versus open appendicectomy.
-
Adults versus children.
-
One type of appendix stump closure versus another.
Sensitivity analysis
We would have performed the following sensitivity analyses if we had found enough trials.
-
Excluding trials with a high or unclear risk of bias.
-
Consecutively excluding every study from the meta‐analysis to explore the impact of individual studies on the overall effect.
-
Changing between worst/best‐case scenario analysis and best/worst‐case scenario analysis for the binary outcomes in case of missing data.
Summary of findings table
We evaluated the quality of evidence using the GRADE approach for each outcome, including any subgroup analysis or sensitivity analysis (Schünemann 2009). We presented the quality of evidence in 'Summary of findings' tables for the following comparisons: early versus delayed open appendicectomy for appendiceal phlegmon and early versus delayed laparoscopic appendicectomy for appendiceal abscess. We downgraded the quality of evidence by one (serious concern) or two (very serious concerns) levels for the following reasons: risk of bias, inconsistency (unexplained heterogeneity, inconsistency of results), indirectness (indirect population, intervention, control, outcomes), imprecision (wide confidence intervals) and publication bias. We justified, documented and incorporated our judgements about the quality of the evidence (high, moderate, low or very low) into the reporting of results for each outcome.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
We identified a total of 4696 records through the electronic searches: 691 in the Cochrane Library, 2390 in MEDLINE Ovid, 979 in Embase Ovid, 56 in Science Citation Index Expanded in the Web of Science and 579 in the Chinese Biomedical Literature Database (CBM). We identified one record through scanning reference lists of the identified randomised controlled trials (Handa 1997). We excluded 552 duplicates and 4134 clearly irrelevant records through screening titles and abstracts. We retrieved the remaining 10 records for further assessment. We excluded eight studies for the reasons listed in the Characteristics of excluded studies table. In total, two randomised controlled trials fulfilled the inclusion criteria. We searched trial registers for ongoing trials, but did not identify any additional studies to be considered for future updates of this review. The study flow diagram is shown in Figure 1.
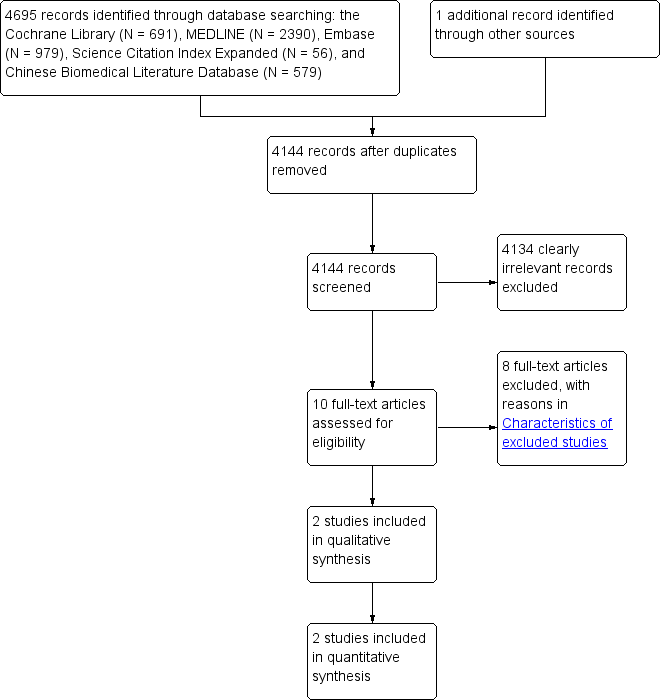
Study flow diagram.
Included studies
Both of the included trials contributed data to the analyses. We provide details of the trials in the Characteristics of included studies table. One trial compared early open appendicectomy with delayed open appendicectomy for paediatric and adult participants with appendiceal phlegmon (Kumar 2004), while the other trial compared early laparoscopic appendicectomy with delayed laparoscopic appendicectomy for paediatric participants with appendiceal abscess (St Peter 2010). Overall, the two trials included 80 participants. Participants' age ranged from 1 year to 84 years. The mean proportion of females was 5% in Kumar 2004 and 47.5% in St Peter 2010. There was no difference in the characteristics of participants in the intervention group or control in either of the trials. Overall, 40 (50%) participants had appendiceal phlegmon (Kumar 2004), and the other 40 (50%) had appendiceal abscess (St Peter 2010). The duration of short term follow‐up in the two trials was 3 weeks and 12 weeks, respectively.
For Kumar 2004, short‐term outcome measures included operative time, operative difficulty, postoperative complications, length of hospital stay, and duration of time away from work. Long‐term outcome measures were: number of hospital visits made, presence of severe incisional pain, scar appearance, and patients with recurrent appendicitis, during a follow‐up period of 24‐52 (median 33.5) months.
Excluded studies
We excluded one randomised controlled trial because it focused on perforated appendicitis without appendiceal abscess (Blakely 2011). None of the other excluded studies were randomised controlled trials (Aranda‐Narváez 2010; Bahram 2011; Erdoğan 2005; Goh 2005; Handa 1997; Senapathi 2002; Weber 2003).
Risk of bias in included studies
The risk of bias of the included studies is shown in Figure 2 and Figure 3. None of the trials were at low risk of bias across all domains.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Both trials were at unclear risk for random sequence generation and allocation concealment.
Blinding
Both trials were at high risk of bias for blinding of participants and personnel because it was impossible to blind the participants or healthcare providers (Kumar 2004; St Peter 2010). It was unclear whether trials blinded outcome assessors.
Incomplete outcome data
There was a low risk of bias for incomplete outcome data in both trials because there were no missing data (Kumar 2004; St Peter 2010).
Selective reporting
The trial protocol was available for one trial (St Peter 2010), which reported all pre‐specified outcomes. Thus, we considered the trial to be free from selective reporting bias. The trial protocol was not available for the other trial (Kumar 2004), and as some outcomes of interest for this review (mortality, quality of life and pain) were not reported, we considered the trial to be high risk of bias for selective reporting.
Other potential sources of bias
With regard to differences in baseline characteristics, we did not observe any baseline imbalances, therefore we considered both trials to be at low risk in this domain (Kumar 2004; St Peter 2010).
Effects of interventions
See: Summary of findings for the main comparison Early versus delayed open appendicectomy for appendiceal phlegmon; Summary of findings 2 Early versus delayed laparoscopic appendicectomy for appendiceal abscess
Early versus delayed open appendicectomy for appendiceal phlegmon
One trial (N = 40) compared early open appendicectomy with delayed open appendicectomy in paediatric and adult participants with appendiceal phlegmon (Kumar 2004). Twenty participants were randomised to the early appendicectomy group (appendicectomy as soon as appendiceal mass resolved within the same admission) and 20 participants to the delayed appendicectomy group (initial conservative treatment followed by interval appendicectomy six weeks later). None of the participants crossed from the delayed appendicectomy group to the early appendicectomy group or underwent percutaneous drainage of the appendiceal phlegmon. There was no clinical or statistical heterogeneity, as the analysis included only one trial. We summarise the results in summary of findings Table for the main comparison.
Kumar 2004 evaluated the following outcomes.
Overall morbidity
The overall complication rate was 30% in the early appendicectomy group and 0% in the delayed appendicectomy group. There was no evidence of difference in the rate of overall morbidity between the groups (risk ratio (RR) 13.00; 95% confidence interval (CI) 0.78 to 216.39; P = 0.07; Analysis 1.1).
The overall wound infection rate was 20.0% in the early appendicectomy group and 0% in the delayed appendicectomy group). There was no evidence of difference between the groups (RR 9.00; 95% CI 0.52 to 156.91; P = 0.13; Analysis 1.2).
The proportion of participants experiencing faecal fistula was 5.0% in the early appendicectomy group and 0% in the delayed appendicectomy group. There was no evidence of difference between the groups (RR 3.00; 95% CI 0.13 to 69.52; P value = 0.49; Analysis 1.3).
The trial did not report the rates of abdominal abscess, bowel obstruction or incisional hernia.
We downgraded the quality of evidence to very low due to risk of bias (lack of blinding, unclear random sequence generation and allocation concealment) and very serious imprecision.
Mortality
There was no mortality in either group. We downgraded the quality of evidence to low due to very serious imprecision.
Length of hospital stay
The mean length of hospital stay was 21.4 days in the early appendicectomy group and 14.7 days in the delayed appendicectomy group. Total hospital stay for participants in the delayed appendicectomy group included a combination of the first and second admissions. The total hospital stay was longer in the early appendicectomy group than in the delayed appendicectomy group (mean difference (MD) 6.70 days; 95% CI 2.76 to 10.64; P < 0.001; Analysis 1.4).
We downgraded the quality of the evidence to very low due to risk of bias (lack of blinding, unclear random sequence generation and allocation concealment) and very serious imprecision.
Time away from normal activities
The mean time away from normal activities was 25.0 days in the early appendicectomy group and 20.0 days in the delayed appendicectomy group. The time away from normal activities was longer in the early appendicectomy group than in the delayed appendicectomy group (MD 5.00 days; 95% CI 1.52 to 8.48; P = 0.005; Analysis 1.5).
We downgraded the quality of the evidence to very low due to risk of bias (lack of blinding, unclear random sequence generation and allocation concealment) and very serious imprecision.
Kumar 2004 did not report on quality of life or pain.
Early versus delayed laparoscopic appendicectomy for appendiceal abscess
One trial (N = 40) compared early laparoscopic appendicectomy with delayed laparoscopic appendicectomy in paediatric participants with appendiceal abscess (St Peter 2010). Twenty participants were randomised to the early appendicectomy group (emergent laparoscopic appendicectomy), and 20 participants to the delayed appendicectomy group (initial conservative treatment followed by interval appendicectomy 10 weeks later). Four participants crossed from the delayed appendicectomy group to the early appendicectomy group. Eleven participants in the delayed appendicectomy group underwent percutaneous drainage of the appendiceal abscess. There was no clinical or statistical heterogeneity, as the analysis included only one trial. We summarise the results in summary of findings Table 2.
Overall morbidity
St Peter 2010 did not report this outcome.
Mortality
There was no mortality in either group. We downgraded the quality of the evidence to low due to very serious imprecision.
Length of hospital stay
The mean length of hospital stay was 6.7 days in the early appendicectomy group versus 6.5 days in the delayed appendicectomy group. Total hospital stay for participants in the delayed appendicectomy group included a combination of the first and second admissions. There was no evidence of difference in the total hospital stay between the groups (MD −0.20 days; 95% CI −3.54 to 3.14; P = 0.91; Analysis 2.1).
We downgraded the quality of the evidence to very low due to risk of bias (lack of blinding, unclear random sequence generation and allocation concealment) and very serious imprecision.
Time away from normal activities
St Peter 2010 did not report this outcome.
Quality of life
St Peter 2010 used the Pediatric Quality of Life Scale‐Version 4.0 to assess quality of life, a scale of 0 to 100 with higher values indicating better quality of life. The mean quality of life score at 12 weeks after appendicectomy was 96.77 points in the early appendicectomy group and 84.37 points in the delayed appendicectomy group. The quality of life score at 12 weeks after appendicectomy was higher in the early appendicectomy group than in the delayed appendicectomy group (MD 12.40 points; 95% CI 9.78 to 15.02; P value < 0.001; Analysis 2.2). We downgraded the quality of the evidence to very low due to risk of bias (lack of blinding, unclear random sequence generation and allocation concealment) and very serious imprecision.
Pain
St Peter 2010 did not report this outcome.
Subgroup analysis
We did not perform any planned subgroup analysis because too few trials were included in this review.
Sensitivity analysis
We did not perform any planned sensitivity analysis because we included only two trials in this review, and both were at high risk of bias but had no missing data.
Reporting biases
We did not create funnel plots to assess reporting biases because the number of trials included was fewer than 10. We identified a study protocol for one trial (St Peter 2010). The trial was free of reporting bias because it reported all of the pre‐specified outcomes. The trial protocol was not available for the Kumar 2004 trial, but it reported both primary and secondary outcomes of this review. Thus we considered both included trials to be free of reporting bias.
Discussion
Summary of main results
This review includes two randomised controlled trials involving 80 paediatric and adult participants undergoing open or laparoscopic appendicectomy for appendiceal phlegmon or abscess. Both trials were at a high risk of bias (Kumar 2004; St Peter 2010). We found no evidence of differences in overall morbidity or mortality between the early appendicectomy group and the delayed appendicectomy group. One very low‐quality trial showed that early open appendicectomy increased total hospital stay and time away from normal activities for paediatric and adult participants with appendiceal phlegmon (Kumar 2004). However, the other very low‐quality trial suggested that early laparoscopic appendicectomy was better than delayed laparoscopic appendicectomy in terms of health‐related quality of life for paediatric participants with appendiceal abscess (St Peter 2010).
There are several possible reasons for the differences in findings between the two studies. First, the types of participants of interest between the two studies were different. One trial included both paediatric and adult participants with appendiceal phlegmon (Kumar 2004), while the other trial only included paediatric participants with appendiceal abscess (St Peter 2010). Additionally, the types of interventions between the two studies were different. Participants in one trial underwent early open appendicectomy as soon as the appendiceal mass resolved (Kumar 2004), while participants in the other trial underwent early (emergent) laparoscopic appendicectomy (St Peter 2010). Laparoscopic appendicectomy appears to be superior to open appendicectomy for suspected appendicitis (Sauerland 2010). Moreover, most participants with appendiceal abscess underwent percutaneous drainage of the abscess (when possible) and delayed appendicectomy in one trial, while participants with appendiceal phlegmon in the other trial did not need percutaneous drainage of the phlegmon.Thus, we did not pool the two studies because of the obvious clinical heterogeneity between them.
There was no mortality in either trial. Although overall morbidity was higher in the early appendicectomy group (30%) than in the delayed appendicectomy group (0%) for participants with appendiceal phlegmon, the difference was not statistically significant. Appendicectomy is one of the most common operations performed in the world, yet there were only 80 participants contributing data to this review, so it lacked the statistical power to detect any clinically meaningful difference between early and delayed appendicectomy for preventing complications, even if such a difference were present. In addition, where we detected differences, our confidence was low, as the small numbers mean results could be spurious, and moreover underpowered analyses can exacerbate the impact of bias. Thus, it is unclear whether early appendicectomy prevents complications compared to delayed appendicectomy for people with appendiceal phlegmon or abscess; the data are sparse, and we cannot rule out significant benefits or harms for either intervention.
Overall completeness and applicability of evidence
The need for an appendicectomy after successful conservative management of complicated appendicitis remains controversial (Simillis 2010). Because of the risk of recurrent appendicitis and missed finding of malignancy, appendicectomy is a common treatment for complicated appendicitis (appendiceal phlegmon or abscess). Both trials included participants undergoing emergent or elective appendicectomy for appendiceal phlegmon or abscess. Most participants with appendiceal abscesses in one trial underwent percutaneous drainage of the abscess before delayed appendicectomy. Thus, the results of this review are applicable to participants who are about to undergo emergent or elective appendicectomy for appendiceal phlegmon or abscess. In addition, participants who are about to undergo delayed appendicectomy require percutaneous drainage of appendiceal abscesses (when possible).
Quality of the evidence
Overall, we considered the quality of the evidence to be very low (summary of findings Table for the main comparison; summary of findings Table 2). The main reason for downgrading was wide confidence intervals for the effect estimates. We also downgraded further for risk of bias. Neither of the trials was at a low risk of bias across all domains; one major source of risk was lack of blinding, which might introduce detection bias and performance bias. Although it was impossible to blind the participants or healthcare providers, blinding of outcome assessors could be achieved with appropriate study design. Likewise, there was an unclear risk of selection bias in both trials, as authors did not report details on random sequence generation or allocation concealment. We could not assess statistical heterogeneity because there was only one trial in each comparison.
Potential biases in the review process
There were several potential biases of note in the review process. First, only two trials with 80 participants were identified, reflecting a lack of data on this topic to date. Second, we were unable to assess the impact of publication bias by visual inspection of the funnel plot.
Agreements and disagreements with other studies or reviews
Another systematic review compared early appendicectomy and conservative treatment (antibiotic treatment without delayed appendicectomy) for appendiceal phlegmon or abscess (Simillis 2010), concluding that conservative treatment was better than early appendicectomy in terms of complication and reoperation rate. However, the data did not justify a general recommendation because of significant heterogeneity between included studies. The present review is the first systematic review comparing early versus delayed appendicectomy for appendiceal phlegmon or abscess that includes only randomised controlled trials. Our findings, that early open appendicectomy increases hospital stay and time away from normal activities compared to appendicectomy in people with appendiceal phlegmon, and that early laparoscopic appendicectomy improves health‐related quality of life for participants with appendiceal abscess, is consistent with the findings of Simillis 2010.

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
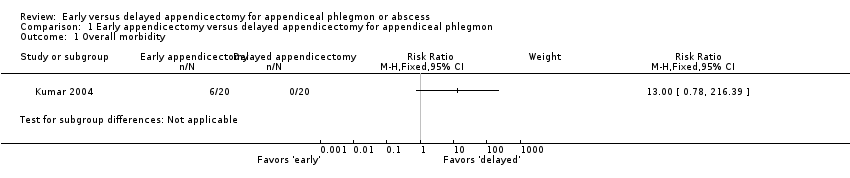
Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 1 Overall morbidity.

Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 2 Wound infection.
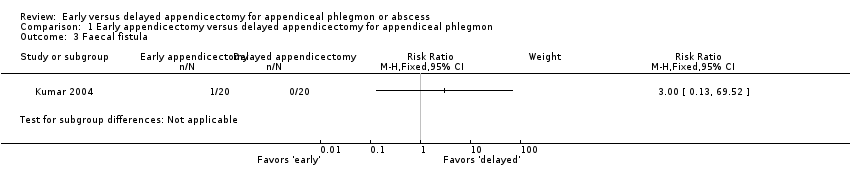
Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 3 Faecal fistula.

Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 4 Total length of hospital stay (days).
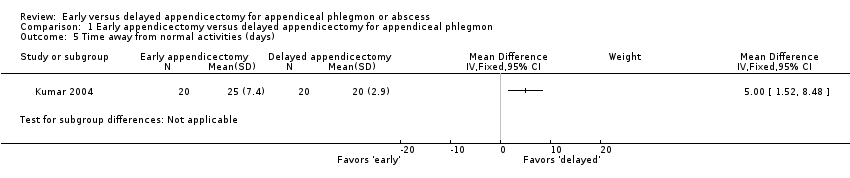
Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 5 Time away from normal activities (days).

Comparison 2 Early appendicectomy versus delayed appendicectomy for appendiceal abscess, Outcome 1 Total length of hospital stay (days).

Comparison 2 Early appendicectomy versus delayed appendicectomy for appendiceal abscess, Outcome 2 Quality of life (score on a scale from 0‐100).
| Early versus delayed open appendicectomy for appendiceal phlegmon | ||||||
| Patient or population: paediatric and adult patients with appendiceal phlegmon | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed appendicectomy | Early appendicectomy | |||||
| Overall morbidity Median follow‐up: 33,5 months | 0 per 1000 | 300 per 1000 | RR 13.00 | 40 | ⊕⊝⊝⊝ | — |
| Wound infection Median follow‐up: 33,5 months | 0 per 1000 | 200 per 1000 | RR 9.00 | 40 | ⊕⊝⊝⊝ | — |
| Faecal fistula Median follow‐up: 33,5 months | 0 per 1000 | 50 per 1000 | RR 3.00 | 40 | ⊕⊝⊝⊝ | — |
| Mortality Median follow‐up: 33,5 months | See comment | See comment | Not estimable | 40 | ⊕⊕⊝⊝ | There was no mortality in either group. |
| Total length of hospital stay (days) Follow‐up: 3 weeks | The mean total length of hospital stay in the delayed appendicectomy group was 14.7 days | The mean total length of hospital stay in the early appendicectomy group was 6.7 days higher | MD 6.70 (2.76 to 10.64) | 40 | ⊕⊝⊝⊝ | — |
| Time away from normal activities (days) Median follow‐up: 33,5 months | The mean time away from normal activities in the delayed appendicectomy group was 20 days | The mean time away from normal activities in the early appendicectomy group was 5 days higher | MD 5.00 (1.52 to 8.48) | 40 | ⊕⊝⊝⊝ | — |
| Quality of life Median follow‐up: 33,5 months | Not reported | |||||
| Pain (days) Follow‐up: 3 weeks | Not reported | |||||
| *The basis for the assumed risk was the control group proportion in the study. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded one level for serious risk of bias. | ||||||
| Early versus delayed laparoscopic appendicectomy for appendiceal abscess | ||||||
| Patient or population: paediatric participants with appendiceal abscess Setting: secondary and tertiary care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed appendicectomy | Early appendicectomy | |||||
| Overall morbidity | Not reported | |||||
| Wound infection | Not reported | |||||
| Faecal fistula | Not reported | |||||
| Mortality Follow‐up: 12 weeks | See comment | See comment | Not estimable | 40 | ⊕⊝⊝⊝ | There was no mortality in either group. |
| Total length of hospital stay (days) Follow‐up: 12 weeks | The mean total length of hospital stay in the delayed appendicectomy group was 6.7 days | The mean total length of hospital stay in the early appendicectomy group was 0.2 days lower | MD −0.20 (−3.54 to 3.14) | 40 | ⊕⊝⊝⊝ | — |
| Time away from normal activities (days) | Not reported | |||||
| Quality of life (Pediatric Quality of Life Scale‐Version 4.0, a scale of 0 to 100 with higher values indicating better quality of life) Follow‐up: 12 weeks | The mean quality of life score in the delayed appendicectomy group was 84.37 points | The mean quality of life score in the early appendicectomy group was 12.40 points higher | MD 12.40 (9.78 to 15.02) | 40 | ⊕⊝⊝⊝ | We considered the observed mean difference in quality of life score to be clinically significant. |
| Pain (days) | Not reported | |||||
| *The basis for the assumed risk was the control group proportion in the study. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded two levels due to very serious imprecision (small sample size). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Overall morbidity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2 Wound infection Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Faecal fistula Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4 Total length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5 Time away from normal activities (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2 Quality of life (score on a scale from 0‐100) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |

