Apendicectomía temprana versus diferida para el absceso y el flemón apendicular
Información
- DOI:
- https://doi.org/10.1002/14651858.CD011670.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 02 junio 2017see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Colorrectal
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Cheng Y and Xiong X: drafted the protocol and drafted the final review.
Lu J: selected which trials to include and assessed the risk of bias of the trials.
Wu S: selected which trials to include and assessed the risk of bias of the trials.
Xiong X: extracted data from the trials.
Zhou R: extracted data from the trials.
Cheng N: revised the protocol, entered data into RevMan, and carried out the analysis.
Cheng Y and Xiong X: contributed equally to developing the review.
Sources of support
Internal sources
-
The Second Affiliated Hospital, Chongqing Medical University, China.
-
West China Hospital, Sichuan University, China.
External sources
-
No sources of support supplied
Declarations of interest
Cheng Y: none known.
Xiong X: none known.
Lu J: none known.
Wu S: none known.
Zhou R: none known.
Cheng N: none known.
Acknowledgements
We would like to thank the Cochrane Colorectal Cancer Group (CCCG), including Henning Keinke Andersen and Sara Hallum, both assisting in the development of the review, and Sys Johnsen and Marija Barbateskovic, who developed the search strategies. Furthermore, Dr Jianping Gong for careful revision of the final review. We also want to thank the involved editors, peer reviewers, sign off editor and the CEU screening editor for valuable input and comments to this review. And finally, the Copy Edit Support for careful revision of the final manuscript.
Version history
| Published | Title | Stage | Authors | Version |
| 2024 May 02 | Early versus delayed appendicectomy for appendiceal phlegmon or abscess | Review | Shiyi Zhou, Yao Cheng, Nansheng Cheng, Jianping Gong, Bing Tu | |
| 2017 Jun 02 | Early versus delayed appendicectomy for appendiceal phlegmon or abscess | Review | Yao Cheng, Xianze Xiong, Jiong Lu, Sijia Wu, Rongxing Zhou, Nansheng Cheng | |
| 2015 Apr 21 | Early versus delayed appendicectomy for appendiceal phlegmon or abscess | Protocol | Yao Cheng, Xianze Xiong, Jiong Lu, Sijia Wu, Rongxing Zhou, Yixin Lin, Nansheng Cheng | |
Differences between protocol and review
We made clarifications to the types of participants according to the reviewer's suggestion. Hospital costs are neither comparable nor reliable among included studies due to inflation and inter‐country economic differences. Thus, we did not include hospital costs as an outcome in the review stage.
We applied the GRADE approach for evaluating the quality of evidence for each outcome, which we had not stated in the protocol.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Time‐to‐Treatment;
- Abscess [complications, mortality, *surgery];
- Appendectomy [*methods, mortality];
- Appendicitis [complications, mortality, *surgery];
- Cellulitis [complications, mortality, *surgery];
- Conservative Treatment;
- Emergencies;
- Length of Stay;
- Quality of Life;
- Randomized Controlled Trials as Topic;
Medical Subject Headings Check Words
Adult; Child; Humans;
PICO

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
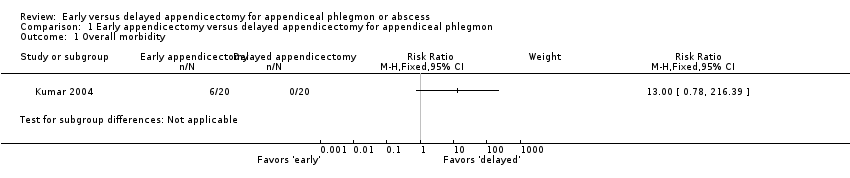
Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 1 Overall morbidity.

Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 2 Wound infection.
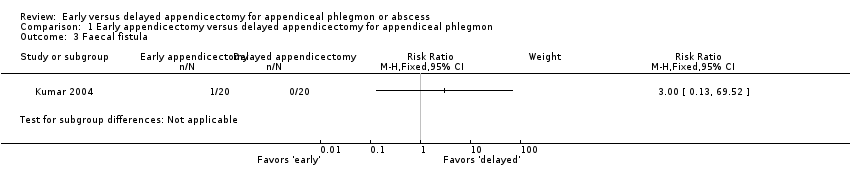
Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 3 Faecal fistula.

Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 4 Total length of hospital stay (days).
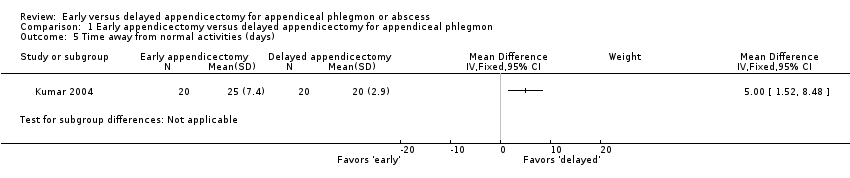
Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 5 Time away from normal activities (days).

Comparison 2 Early appendicectomy versus delayed appendicectomy for appendiceal abscess, Outcome 1 Total length of hospital stay (days).

Comparison 2 Early appendicectomy versus delayed appendicectomy for appendiceal abscess, Outcome 2 Quality of life (score on a scale from 0‐100).
| Early versus delayed open appendicectomy for appendiceal phlegmon | ||||||
| Patient or population: paediatric and adult patients with appendiceal phlegmon | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed appendicectomy | Early appendicectomy | |||||
| Overall morbidity Median follow‐up: 33,5 months | 0 per 1000 | 300 per 1000 | RR 13.00 | 40 | ⊕⊝⊝⊝ | — |
| Wound infection Median follow‐up: 33,5 months | 0 per 1000 | 200 per 1000 | RR 9.00 | 40 | ⊕⊝⊝⊝ | — |
| Faecal fistula Median follow‐up: 33,5 months | 0 per 1000 | 50 per 1000 | RR 3.00 | 40 | ⊕⊝⊝⊝ | — |
| Mortality Median follow‐up: 33,5 months | See comment | See comment | Not estimable | 40 | ⊕⊕⊝⊝ | There was no mortality in either group. |
| Total length of hospital stay (days) Follow‐up: 3 weeks | The mean total length of hospital stay in the delayed appendicectomy group was 14.7 days | The mean total length of hospital stay in the early appendicectomy group was 6.7 days higher | MD 6.70 (2.76 to 10.64) | 40 | ⊕⊝⊝⊝ | — |
| Time away from normal activities (days) Median follow‐up: 33,5 months | The mean time away from normal activities in the delayed appendicectomy group was 20 days | The mean time away from normal activities in the early appendicectomy group was 5 days higher | MD 5.00 (1.52 to 8.48) | 40 | ⊕⊝⊝⊝ | — |
| Quality of life Median follow‐up: 33,5 months | Not reported | |||||
| Pain (days) Follow‐up: 3 weeks | Not reported | |||||
| *The basis for the assumed risk was the control group proportion in the study. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded one level for serious risk of bias. | ||||||
| Early versus delayed laparoscopic appendicectomy for appendiceal abscess | ||||||
| Patient or population: paediatric participants with appendiceal abscess Setting: secondary and tertiary care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed appendicectomy | Early appendicectomy | |||||
| Overall morbidity | Not reported | |||||
| Wound infection | Not reported | |||||
| Faecal fistula | Not reported | |||||
| Mortality Follow‐up: 12 weeks | See comment | See comment | Not estimable | 40 | ⊕⊝⊝⊝ | There was no mortality in either group. |
| Total length of hospital stay (days) Follow‐up: 12 weeks | The mean total length of hospital stay in the delayed appendicectomy group was 6.7 days | The mean total length of hospital stay in the early appendicectomy group was 0.2 days lower | MD −0.20 (−3.54 to 3.14) | 40 | ⊕⊝⊝⊝ | — |
| Time away from normal activities (days) | Not reported | |||||
| Quality of life (Pediatric Quality of Life Scale‐Version 4.0, a scale of 0 to 100 with higher values indicating better quality of life) Follow‐up: 12 weeks | The mean quality of life score in the delayed appendicectomy group was 84.37 points | The mean quality of life score in the early appendicectomy group was 12.40 points higher | MD 12.40 (9.78 to 15.02) | 40 | ⊕⊝⊝⊝ | We considered the observed mean difference in quality of life score to be clinically significant. |
| Pain (days) | Not reported | |||||
| *The basis for the assumed risk was the control group proportion in the study. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded two levels due to very serious imprecision (small sample size). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Overall morbidity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2 Wound infection Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Faecal fistula Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4 Total length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5 Time away from normal activities (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2 Quality of life (score on a scale from 0‐100) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |

