Intervenciones no farmacológicas para los trastornos somatoformes y los síntomas físicos sin explicación médica (SFSEM) en adultos
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: DSM‐IV diagnosis of somatisation disorder Method of diagnosis: participants (18‐70 years) with English fluency and literacy, a DSM‐IV diagnosis for somatoform disorder and a CGI‐SD score ≥ 4 were included Exclusion criteria: unstable major medical condition, medication regimen that has not been stable for at least 2 months prior to baseline, active suicidal ideation, history of psychosis, current psychoactive substance dependence, pregnant women or attempting to conceive, participants in psychotherapy concurrent with the period between baseline and 3 months appointments Total number randomised: 84 Age: for intervention group, M = 45.5 (SD = 8.5); for control group, M = 47.9 (SD = 11) Sex: 89% women; 11% men for intervention group 84% women (n = 36), for control group 95% (n = 39) Severity of symptoms at baseline: not reported Duration of symptoms at baseline: for intervention group M = 24.95 (SD = 11.54) years, for control group M = 25 (SD = 15.12) years Setting: participants were recruited through medical clinics and through advertisements in the community (70% referred by physician), after informed consent they received a telephone screening interview. Treatment: department of Psychiatry of medical school Location: New Jersey, USA Number of treatment centres: 1 Co‐morbidities: 65% current co‐morbid DSM‐IV axis I disorder; 70% (n = 30) for intervention group, 59% (n = 24) for control group Adjunctive therapy: not mentioned Adjunctive medication: not mentioned | |
| Interventions | Participants were randomly assigned to either 1. CBT + PCI (n = 43) Duration: 10 sessions during a period of 3 months Treatment protocol: CBT: manualised intervention for people with somatoform disorder, with detailed guidelines for each session, focused on stress management, activity regulation, emotional awareness, cognitive restructuring, and interpersonal communication (Allen 2006, refs 5 and 6 for details) PCI: standard consultation letter sent to the treating physician including recommendations for the ongoing treatment (Allen 2006, Table 1 for details) Therapist: 4 therapists, master‐ or doctoral‐level psychologists with at least 3 years of supervised training in CBT. All received a special training in CBT for SD before the trial 2. PCI alone (n = 41) Duration: NA Treatment protocol: standard consultation letter sent to the treating physician including recommendations for the ongoing treatment (Allen 2006, Table 1 for details). Therapist/face‐to‐face contact: none | |
| Outcomes | Time points for assessment: baseline and 3 months, 9 months, 15 months after baseline Primary outcome: 1. severity of somatisation (CGI‐SD) 2. improvement (CGI‐SD) Secondary outcome: 1. participants' rating of physical functioning (MOS‐36) 2. severity of somatic symptoms (SSS) 3. healthcare utilisation (medical records) Potential mediator 1. participant expectations of improvement | |
| Notes | Date of study: September 1999 ‐ April 2003 Funding source: National Institute of Mental Health Declarations of interest among the primary researchers: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence was used |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) | High risk | Participants and therapists were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Study personnel were masked to participants treatment condition (independent evaluators), but participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | Low risk | < 20% missing per follow‐up moment |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Low risk | The treatment was described in a manual containing detailed guidelines for the conduct of each session (Allen 2006, page 1513) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: medically unexplained symptoms (according to a PHQ‐14 score > 10 and a GP check) Method of diagnosis: adults aged 18‐65 years and registered with participating practices were eligible if they met all 3 criteria: 1. they had been referred at least twice to specialists in the preceding 3 years; 2. they currently reported multiple physical symptoms (PHQ > 10); and 3. their GP believed that their symptoms were unlikely to be adequately explained by physical disease Exclusion criteria: participants who were unable to leave the house independently, other health or social problems precluded an invitation to take part in a study, thoughts of self harm more than a few times in a week (PHQ‐9), current self reported alcohol or drug problems, and current or planned engagement in psychological therapy Total number randomised: 32 Age: for intervention group, M = 45.9 (SD = 12.7); for control group, M = 49.2 (SD = 10.1) Sex: for intervention group 56.3% women (n = 9), 43.7% men (n = 7); for control group 75% women (n = 12), 25% men (n = 4) Severity of symptoms at baseline: PHQ‐14 score for intervention group M = 13.9 (SD = 3.3), for control group M = 14.7 (SD = 2.6) Duration of symptoms at baseline: not reported Setting: selection in 7 participating practices in primary care (selection based on database search, postal questionnaire, and check for exclusion criteria by GP), treatment in a secondary care outpatient symptoms clinic Location: North‐east Edinburgh, Scotland Number of treatment centres: 1 Co‐morbidities: Participants with PHQ‐9 score > 10 (indicating major depressive disorder: for intervention group 31% (n = 5); for control group 56% (n = 9) Participants with GAD‐7 score > 10 (indicating generalised anxiety disorder): for intervention group 19% (n = 3); for control group 31% (n = 5) Adjunctive therapy: participants in both arms continued to receive usual care from their registered general practice. This included referral for investigation or treatment of symptoms as the GP deemed appropriate Adjunctive medication: none reported | |
| Interventions | Participants were randomly assigned to either 1. Treatment in the symptoms clinic (n = 16) Duration: 4 sessions, the first session of 1 hour and further sessions of 20 minutes, during a period of 3 months Treatment protocol: the consultations were structured to first hear the participant's experience of illness then to propose and negotiate constructive explanations of physical symptoms. These explanations were used as the basis for simple cognitive and behavioural actions to modify symptoms and their impact. No specific attempt was made to screen for common mental disorders; however, participants were encouraged to describe their emotional responses to symptoms and other events, and diagnostic labels such as depression were discussed collaboratively with the participant rather than imposed by the doctor (see Burton 2012, ref 14 for theoretical basis). Therapist: an experienced GP with special interest in MUS 2. Usual care (n = 16) Duration: NA Treatment protocol: NA Therapist: NA | |
| Outcomes | Time points for assessment: baseline and 3 months after baseline Primary outcome: (systematic identification of participants, trial recruitment and retention, acceptability to participants (Client Satisfaction Questionnaire)) 1. number and severity of physical symptoms (PHQ‐14) 2. subjective physical and mental health (SF‐12) 3. depressive symptoms (PHQ‐9) 4. generalised anxiety (GAD‐7) | |
| Notes | Date of study: August 2009 ‐ May 2010 Funding source: Chief Scientist Office Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was carried out by automated telephone system using blocked allocation with variable block size |
| Allocation concealment (selection bias) | Low risk | Participants were randomised to either usual care or intervention by the researcher (WN). Treatments were performed by a doctor (CB) |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could not be blinded |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | High risk | In the intervention group, outcome data were analysed for 11 out of 16 participants. Missing: 31.25% (> 20%) |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | High risk | The consultations were structured, but no protocol or manual has been used (Burton 2012, page 3) |
| Researcher allegiance | Unclear risk | The author was also the therapist performing the intervention in the intervention group |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: MUS (abridged somatisation disorder) Method of diagnosis: clinicians referred participants when they thought symptoms were a source of distress OR suspected they had a psychiatric origin. Participants were then interviewed using PHQ and PRIME‐MD, participants were eligible if they had ≥ 4 unexplained symptoms for men and ≥ 6 for women Exclusion criteria: severe psychiatric diagnosis, requiring more intensive intervention of major physical disorder that explains any of the symptoms Total number randomised: 172 Age: for intervention group, M = 41.0 (SD = 12.7); for control group, M = 39.6 (SD = 13.4) Sex: 88% women; 12% men; 86.2% women in intervention group (n = 75); 89.4% women in control group (n = 76). Severity of symptoms at baseline:baseline PHQ‐15 score for intervention group M = 14.17 (95% CI = 13.03 to 15.32), for control group M = 13.98 (95% CI = 12.82 to 15.13) Duration of symptoms at baseline: not reported Setting: recruited from 2 university based primary care clinics, intervention at Psychiatry department Location: New Brunswick, New Jersey, USA Number of treatment centres: 1 Co‐morbidities: 92% had a current co‐morbid DSM‐IV axis I disorder; 92.0% of intervention group (n = 80), 91.8% of control group (n = 78) Adjunctive therapy: not mentioned Adjunctive medication: not mentioned | |
| Interventions | Participants were randomly assigned to either 1. CBT + psychiatric consultation letter (n = 87) Duration: 10 sessions of 50 minutes (first session 90 minutes) during 10‐20 weeks (mean of 3 months) Treatment protocol: standardised CBT intervention according to manual, focusing on reduction of reduction of physical distress and somatic pre‐occupation, through training in relaxation techniques, activity regulation, facilitation of emotional awareness, cognitive restructuring and interpersonal communication. Details in book Woolfolk et al. (Woolfolk 2007, ref 18). Consultation letter: a standard consultation letter was sent to the treating primary care physician, originally developed by Smith et al. (Escobar 2007, ref 13), including recommendations about taking care of people with MUPS Therapist: therapists received training on the intervention protocol from 2 of the authors. Therapists' treatment adherence to the study protocol was rated routinely during the study from evaluations of taped sessions 2. Usual clinical care + psychiatric consultation intervention (n = 85) Duration: NA Treatment protocol: a standard consultation letter was sent to the treating primary care physician (see above) Therapist/face‐to‐face contact: none (other than usual care) | |
| Outcomes | Time points for assessment: baseline and 3 months, 9 months, after baseline Primary outcome: 1. severity of somatisation (CGI + PHQ‐15) 2. improvement of physical symptoms (CGI ‐ improvement) Secondary outcome: 1. participants' rating of physical functioning (physical subscale of MOS‐10) 2. severity of somatic symptoms (VAS) 3. anxiety and depression (HAM‐A and HAM‐D) | |
| Notes | Date of study: recruitment took place from January 2001 through to February 2005, follow‐up until the end of 2006 Funding source: National Institute of Mental Health Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcome assessors were blinded (but had to ask participants…) |
| Incomplete outcome data (attrition bias) | High risk | 21‐24% loss to follow‐up directly after treatment; 41‐48% loss to follow‐up 6 months later |
| Selective reporting (reporting bias) | Low risk | CGI scores not reported (but provided later by first author) |
| Treatment fidelity | Low risk | Treatment sessions followed a manual with step‐by‐step guidelines for each session (Escobar 2007, ref 18) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: chronic multi‐organ BDS Method of diagnosis: participants received a 5‐7 hour bio‐psycho‐social assessment, including a laboratory screening battery, schedules for clinical assessment in neuropsychiatry (SCAN)‐diagnostic interview, as well as a physical and neurological examination. Participants (aged 20‐50 years) with chronic (≥ 2 years) multi‐organ type BDS and moderate‐to‐severe impairment in daily living were eligible for inclusion Exclusion criteria: severe psychiatric morbidity, current alcohol or drug abuse, pregnancy, non‐Scandinavian origin, no informed consent Total number randomised: 120 Age: for intervention group, M = 38 (SD = 9); for control group, M = 40 (SD = 8) Sex: 80% women; 20% men in both study groups, 47 women in intervention group, 48 in control group Severity of symptoms at baseline: all participants in both study groups had a somatisation disorder according to ICD‐10 codes. In the intervention group, 95% had a somatisation disorder according to the DSM‐IV codes (n = 56), in the control group 95% (n = 57). 5% of intervention group (n = 3) and 5% of control group (n = 3) had an undifferentiated somatoform disorder (DSM‐IV codes) Duration of symptoms at baseline: for intervention group M = 12 (SD = 10.6), for control group M = 15 (SD = 12.6) years Setting: primary care physicians and hospital wards referred participants both from rural and urban areas. Intervention took place at the Research Clinic for Funcional Disorders and Psychosomatics in Aarhus University Hospital Location: Arhus region, Denmark Number of treatment centres: 1 Co‐morbidities: 71% of intervention group (n = 42) and 62 % (n = 37) of control group had lifetime psychiatric co‐morbidity. 22% of intervention group (n = 13) and 20% of control group (n =12) had a current major depressive disorder (DSM‐IV codes). 24% of intervention group (n = 14) and 23% of control group (n = 14) had a current anxiety disorder (DSM‐IV codes) Adjunctive therapy/medication: consultation letter; letter to social authorities, when needed; advise to taper off morphine derivatives and benzodiazepines (all also in comparison group) | |
| Interventions | Participants were randomly assigned to either 1. Mindfulness therapy (n = 59) Duration: 8 weekly session and 1 in week 12 (3.5 hours each) during a period of 12 weeks Treatment protocol: participants received information about the nature, course, and treatment of BDS, a treatment manual, 9 group treatment modules based on a mindfulness‐based stress reduction and a cognitive‐behavioural approach (closely following the manual by Jon Kabat Zinn (Fjorback 2013, ref 22, 36, 36). A consultation letter was sent to participants' primary care physicians, and letters to social authorities were sent when needed (see Fjorback 2013 Table 1 for details) Therapist: 2 psychiatrists with experience in BDS and CBT and in psychotherapy of meditation 2. Enhanced TAU (n = 60) (see Fjorback 2013 Figure 1 for details) Duration: 1 x 2‐hour session Treatment protocol: participants received information about the nature, course, and treatment of BDS, a consultation letter to participants' primary care physicians, letters to social authorities when needed, an individual CBT treatment plan according to a manual and an individual psychiatric consultation within the first month after clinical assessment (see Fjorback 2013 Figure 1 for details) Therapist: psychiatrist | |
| Outcomes | Time points for assessment: baseline and 3 months, 9 months, 15 months after baseline Primary outcome: 1. mean change in SF‐36 PCS between baseline and 15 months Secondary outcome: 1. change in other health‐related quality of life measures of the SF‐36 2. illness worry (WI‐8) 3. physical symptoms (SCL‐90‐R Somatisation Subscale) 4. severity of depression and anxiety (SCL‐8) 5. participants reporting improvement (greater than half a SD) | |
| Notes | Date of study: recruitment took place between April 2007 and September 2008, follow‐up until the end of 2009 Funding source: Danish Agency for Science Technology and Innovation, Aase and Ejnar Danielsens Fund, Trygfonden Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was prepared by a statistician |
| Allocation concealment (selection bias) | Low risk | They used pre‐defined concealed random numbers tied to consecutive assessments of participants resulting in opaque envelopes numbered in succession containing assigned treatment |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded, given difference in treatment content, intensity, and duration |
| Blinding of outcome assessment (detection bias) | High risk | All outcomes were participant reported, and these were not blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | > 20% no data at follow up, but multiple imputation may have solved this problem |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. Secondary outcome probability of change > 0.5 SD predefined? |
| Treatment fidelity | Low risk | Treatment followed a model based on a manual (Fjorback 2013, table 1 and ref 39) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: somatisation disorder Method of diagnosis: inclusion criteria were diagnosis of somatisation disorder, history of ≥ 13 unexplained symptoms, the first beginning < 30 years of age, severe enough to seek treatment, take medication, or reduce functioning. This was determined by a research psychiatrist, using a checklist of 37 items that made up diagnostic criteria of somatisation disorder, according to DSM‐III‐R criteria Exclusion criteria: the absence of a primary care provider who agreed to allow the research team to see the participant, lack of transportation to the medical centre, indication of moving out of town during study Total number randomised: 70 Age: mean age 44.2 years (no SD provided) Sex: 84% women (n = 59); 16% men (n = 11) Severity of symptoms at baseline: inclusion criterion: ≥ 13 unexplained symptoms Duration of symptoms at baseline: inclusion criterion: 1 symptom starting before age 30 years Setting: recruitment: internists, GPs, and general population (through advertisements in local media). Treatment: at medical centre Location: Central Arkansas, USA Number of treatment centres: 1 Co‐morbidities: unknown Adjunctive therapy: not mentioned Adjunctive medication: not mentioned Co‐intervention: none reported | |
| Interventions | Participants were randomly assigned to either 1. Group therapy intervention + consultation letter (n = 44) Duration: 8 small group sessions of 2 hours every other week, during a 4‐month period Treatment protocol: the overall goals were to develop a source of peer support, share methods of coping with physical problems, enable participants to increase their ability to perceive and express emotion, and enjoy the experience of participating in the group. Treatment in groups of 4‐6, according to a structured protocol, with a class atmosphere, including didactic presentations, small group discussions, therapy exercises, and group discussions. See Kashner 1995 p.464‐5 for details Co‐intervention (both groups): a standard psychiatric consultation letter was sent to the primary care physician, diagnosing the participant with somatisation disorder and including recommendations for its management Therapist: master's level clinicians 2. Consultation letter only (n = 26) Co‐intervention (both groups): standard psychiatric consultation letter sent to primary care physician, diagnosing the participant with somatisation disorder and including recommendations for its management Duration: NA Treatment protocol: NA Therapist: NA | |
| Outcomes | Time points for assessment: baseline and 4 months, 8 months and 12 months after baseline Outcomes: (unclear what is primary and what is secondary) 1. RAND Health Status (4 domains) 2. days in bed (count) 3. healthcare utilisation (costs) | |
| Notes | Date of study: started in 1987, end unclear (healthcare costs were adjusted for inflation using 1990 dollar rates) Funding sources: Robert Wood Johnson Foundation, National Institute of Mental Health, VA Health Services Research and Development Program for Mental Health Declarations of interest among the primary researchers: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel not blinded to intervention |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors did not know whether participant was in experimental or control group, but most outcomes were participant reported and these were not blinded |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed study |
| Selective reporting (reporting bias) | High risk | Days in bed described as assessed but no results reported |
| Treatment fidelity | Low risk | Treatment was based on a structured protocol developed before the study (available from the authors) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: subthreshold somatisation disorder (abridged somatisation) Method of diagnosis: participants (18‐70 years old) were eligible if no major medical illness explained symptoms after detailed physical and laboratory assessment; individuals must have met criteria for ≥ 4 MUPS out of the 42 somatic symptoms listed in the CIDI rated as currently present if males and at least 6 if female, according to a diagnostic interview Exclusion criteria: history of alcohol/drug abuse (within last 12 months), bipolar or psychotic, unstable medical condition, pregnancy, active suicidal ideation Total number randomised: 48 (10 dropped out, baseline data reported for only 38) Age: intervention group 83% < 40 years (n = 15); control group 40% < 40 years (n = 8) Sex: 79% women; 21% men; for intervention group 83.3% women (n = 15), for control group 75.0% (n = 15) Severity of symptoms at baseline: unclear, participants in both groups met a CGI rating of 4, which equals moderate somatisation Duration of symptoms at baseline: not described Setting: participants were recruited from primary medical clinics and community (advertisements). Treatment: department of psychiatry of a medical school Location: New Jersey, USA Number of treatment centres: 1 Co‐morbidities: 55% met criteria for severe depression (n = 21, HAM‐D 17 criteria), 40% for mild‐to‐moderate depression (n = 15, HAM‐D 17 criteria) and 85% for significant anxiety (n = 23, HAM‐A criteria) Adjunctive therapy: not mentioned Adjunctive medication: psychotropic medication were allowed (Katsamanis 2011, table 3) | |
| Interventions | Participants were randomly assigned to either 1. Psychophysiological treatment + psychiatric consultation intervention (PCI) (n = 24) Duration: 10 weekly sessions during a period of 10 weeks Treatment protocol: psychophysiological treatment: treatment consisted of a manualised intervention, described to participants as an intervention which comprises of a set 'self regulation' techniques that are specifically targeted at particular symptoms of body systems, aiming to assist in coping with physical discomfort and stress (Katsamanis 2011, page 221 for details) Therapist: 4 therapists, either master or doctoral level psychologists, 3 of them certified as biofeedback clinicians with at least 3 years of supervised training in psychophysiological treatment 2. PCI alone (n = 24) Duration: NA Treatment protocol: standard consultation letter sent to the treating physician including recommendations for the ongoing treatment (Katsamanis 2011, table 1 for details). Therapist: NA | |
| Outcomes | Time points for assessment: baseline, halfway the intervention (5 weeks) and at the end of treatment (10 weeks) Primary outcome: 1. severity of somatisation (CGI‐SD, clinician rated) Secondary outcome: 1. level of depression and anxiety (HAM‐D and HAM‐A) 2. participants' rating of physical functioning (MOS, SF‐36) 3. participants' rating of mental functioning (MOS, SF‐36) | |
| Notes | Date of study: the study took place between June 2006 and August 2008 Funding source: National Institue of Mental Health Declarations of interest among the primary researchers: design based on Allen. Cross‐over group (receiving treatment after wait condition) not used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors were masked but almost all outcomes were participant reported |
| Incomplete outcome data (attrition bias) | High risk | 10/48 dropped out and for several outcomes even more (> 20%) |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Low risk | Treatment was based on a manual, containing guidelines, developed before the study (available from the authors) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Unclear risk | Large difference in age between groups suggests randomisation failed |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: multiple medically unexplained symptoms Method of diagnosis: participants with relatively recent onset (3‐12 months) of symptoms were tested for eligibility was assessed with a standardised interview and had to fit to 3 additional criteria: 1. the GP confirmed the medically unexplained nature of their symptoms presented at enrolment, 2. between 18‐60 years of age, 3. sufficient understanding of the Dutch language Exclusion criteria: current psychotherapy or a primary diagnosis of mood, anxiety or psychotic disorder requiring treatment Total number randomised: 106 (4:1) Age: for intervention group, M = 35.5 (SD = 9.4); for control group, M = 35.0 (SD = 8.9) Sex: 69% women; 31% men; for intervention group 67% women (n = 54), for control group 78% women, (n = 14) Severity of symptoms at baseline: not described Duration of symptoms at baseline: not described Setting: recruited in general practices and via advertisements in open population (about 50/50 from each source). Treatment: department of Clinical Psychology of a university Location: Amsterdam, the Netherlands Number of treatment centres: 1 Co‐morbidities: in intervention group, participants had M = 2.34 (SD = 1.9) chronic diseases, in control group, M = 1.89 (SD = 1.7) Adjunctive therapy: not mentioned Adjunctive medication: not mentioned | |
| Interventions | Participants were randomly assigned to either 1. Psychological intervention (n = 83) Duration: maximum 12 x 1‐hour sessions once a week or every 2 weeks during a maximum period of 6 months Treatment protocol: depending on therapist (1 of 15 qualified therapists): cognitive behavioural, client‐centred or eclectic therapy, reflecting usual treatment practice Therapist/face‐to‐face contact: 1 out of 15 trained therapists 2. Usual care (n = 23) Duration: NA Treatment protocol: after the intake, participants were referred back to the GP for care as usual, intake reports were also sent to GP Therapist: 1 of 15 trained therapists | |
| Outcomes | Time points for assessment: baseline and 6 and 12 months after baseline Primary outcome: 1. severity of somatisation (somatisation scale of the SCL‐90) Secondary outcome: 1. self reported psychological symptoms (anxiety and depression: SCL‐90) 2. registered unexplained and explained symptoms in general practice (database) 3. GP consultations (database) | |
| Notes | Date of study: unclear Funding source: Nationaal Fonds Geestelijke Volksgezondheid / ZAO Zorgverzekeringen Declarations of interest among the primary researchers: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes, opened after pretest |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could not be blinded |
| Blinding of outcome assessment (detection bias) | High risk | Self report questionnaires mostly |
| Incomplete outcome data (attrition bias) | High risk | > 20% drop‐outs |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | High risk | Treatment depended on therapist, no manual or protocol was used |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: somatisation disorder Method of diagnosis: participants received an interview and a physical examination. Participants (30‐60 years old) were eligible in case of presence of somatisation disorder in accordance with the definition of functional somatic symptoms and ≥ 1 symptoms fulfilling the criteria of specific functional disorders as outlined in the International Classification of Health Problems for Primary Care‐2. Exclusion criteria: major mental disorder, current psychological of psychiatric treatment, acute or transient functional symptoms, drug abuse, chronic pain disorder, inability to speak Swedish fluently Total number randomised: 50 Age: for intervention group, M = 43.8 (SD = 9.3); for control group, M = 44.6 (SD = 7.4) Sex: 84% women; 16% men; for intervention group 84.8% (n = 28) female, for control group 82.4% female (n = 14) Severity of symptoms at baseline: in intervention group 14/33 participants had ≥ 4 symptoms (42.4%), in the control group 9/17 participants had ≥ 4 symptoms (52.9%). Duration of symptoms at baseline: in the intervention group the mean duration of illness was 9.2 years, in the control group 6.6 years. Setting: recruitment: GPs and hospital doctors; treatment: outpatient clinic of Preventive Medicine Unit at Helsingborg County Hospital Location: Helsingborg, Sweden Number of treatment centres: 1 Co‐morbidities: 19/50 (38%) of all participants were previously treated by psychologist/psychiatrist Adjunctive therapy: not mentioned Adjunctive medication: allowed and recorded | |
| Interventions | Participants were randomly (2 : 1) assigned to either 1. Group therapy using a short cognitive‐behavioural treatment model (n = 43) Duration: 8 weekly sessions of 3 hours, and 1 final session after 3 months Treatment protocol: group sessions of CBT focused on reducing dread of somatic diseases and included the following items: 1. thorough physical examination, 2. education to explain stress symptoms in order to enable cognitive restructuring, 3. relaxation training (Lidbeck 1997, table 2 for details) Therapist: a physician (the author), who was specialised in internal, family, and social medicine and who had received training in stress relaxation 2. Waiting list control group (n = 17) Duration: NA Treatment protocol: NA Therapist: NA | |
| Outcomes | Time points for assessment: baseline and 3 months, 9 months after baseline Outcomes: 1. social problems (SPQ) 2. illness behaviour (IBQ) 3. anxiety and depression (HADS) 4. sleep disturbance (SDI) 5. medication usage (questionnaire) | |
| Notes | Date of study: unclear (probably early 1990s) Funding source: not mentioned Declarations of interest among the primary researchers: not mentioned Lidbeck 2003 provides 1.5‐year follow‐up data, but only for intervention group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "using pair‐wise grouping, i.e. subjects with similar symptoms, duration of symptoms, age etc, were randomly allotted to either the treatment or the control group" (personal communication with Lidbeck) |
| Allocation concealment (selection bias) | Low risk | "randomization was carried out independently by a nurse who was not participating in the study"(Lidbeck 1997, p.17) |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Participants filled in questionnaires and were not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Only 1 drop‐out, no missing data |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Unclear risk | Treatment was structured, but no information provided about a manual |
| Researcher allegiance | Unclear risk | The author was also the therapist performing the intervention in the intervention group |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: multiple somatoform symptoms Method of diagnosis: participants were selected after presentation of ≥ 2 MUPS in the last 6 months, leading to significant clinical distress, according to their GP or to a screening questionnaire. A diagnostic interview (IDCL and Mini‐DIPS) was used to assess study criteria and DSM‐5 psychiatric diagnoses Exclusion criteria: severe current medical condition, chronic medical disease explaining the symptoms, psychotic symptoms, substance dependence Total number randomised: 140 Age: for intervention group, M = 45.7 (SD = 13.6); for control group, M = 51.7 (SD = 15,9) (significant difference at P value < 0.05) Sex: for intervention group 68.6% female (n = 48); for control group, 81.4% female (n = 57) Severity of symptoms at baseline: number of somatoform symptoms, lifetime: for intervention group M = 7.6 (SD = 3.9), for control group M = 6.6 (SD = 3.6); DSM‐IV Somatoform Disorder: for intervention group 91.4% (n = 64), for control group 87.1% (n = 61) Duration of symptoms at baseline:years from onset of somatoform symptoms: for intervention group M = 9.2 (SD = 11.2), for control group M = 11.8 (SD = 12.8) Setting: participants were recruited in primary care practices, general population (news reports), or via 'other ways', treatment took place at an outpatient treatment centre in the university hospital (secondary care) Location: Marburg, Germany Number of treatment centres: 1 Co‐morbidities: affective disorder: for intervention group 66.7% (n = 46); for control group 52.2% (n = 36) DSM‐IV anxiety disorder: for intervention group 41.4% (n = 29); for control group 32.9% (n = 22) Adjunctive therapy: none reported Adjunctive medication: none reported | |
| Interventions | Participants were randomly assigned to either 1. CBT (n = 70) Duration: 1 session of 3‐4 hours, 2 weeks after baseline Treatment protocol: treatment consisted of 1 session in groups of 2‐4 participants. Treatment followed a structured manual with 5 central modules: psychophysiological explanation of symptoms, relaxation, importance of cognition, activity instead of avoidance behaviour, and treatment options and healthcare utilisation (Martin 2007, page 296 for details). Therapist: clinical psychologist or medical specialist for psychotherapeutic medicine, both licences CBT specialists 2. Standard medical care (n = 70) Duration: NA Treatment protocol: NA Therapist: NA | |
| Outcomes | Time points for assessment: baseline, 4 weeks, and 6 months after baseline Primary outcome: 1. healthcare utilisation (structured interview, not at 4 weeks) 2. number and severity of somatoform symptoms (BSI and SOMS‐7) Secondary outcome: 1. health anxiety (WI) 2. general psychopathological symptoms (GSI) 3. Depressive symptoms (BDI) 4. health‐related internal control (KKG) | |
| Notes | Date of study: trial conducted between August 2001 ‐ December 2002 Funding source: German Ministry of Research, Education and Science Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was based on a predefined list of binary variables, using blocking procedures to ensure comparable sample sizes (page 295) |
| Allocation concealment (selection bias) | Low risk | Study assistants enrolled and assigned participants to the groups according to the randomisation list |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could not be blinded |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up at 6 months 15.7% in both groups (< 20%) |
| Selective reporting (reporting bias) | Low risk | All intended outcomes are reported |
| Treatment fidelity | Low risk | The treatment followed a structured manual with 5 central modules (in German), available on request (Martin 2007, page 296) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: DSM‐IV diagnosis of abridged somatisation disorder Method of diagnosis: participants (aged 18‐65 years) were eligible if they were able to understand and read Spanish and fulfilled the criteria for ASD (somatic symptom indexes 4 (men) and 6 (women)). In addition, they had to be stable on pharmacotherapy in the previous month and needed to sign informed consent. The Othmer‐DeSouza test was used as a screening tool Exclusion criteria: any primary psychiatric diagnosis other than somatoform disorders, severe personality disorder, non‐white (not mentioned in design paper), inability to attend intervention sessions Total number randomised: 168 Age: for individual CBT group, M = 43.1 (SD = 11.4); for group CBT group, M = 49.2 (SD 8.6); TAU control group, M = 44.1 (SD = 11.7) Sex: 86% women; 14% men; for TAU group 87.5% women (n = 42), for individual CBT group 82.14% women (n = 46), for group CBT group 89.06% women, n = 57. Severity of symptoms at baseline: not described Duration of symptoms at baseline: most participants had symptoms for > 2 years: for TAU group 79.16% (n = 38), for individual CBT group 87.5% (n = 49), for group CBT group 87.5% (n = 56) Setting: recruitment in primary healthcare centres. Treatment setting not mentioned, but carried out by 2 psychologists Location: provinces of Zaragoza, Mallorca, Huesca in Spain Number of treatment centres: unknown Co‐morbidities: approximately 10% had a co‐morbid depressive disorder, 40% had a co‐morbid anxiety disorder, and 30% had a depressive and anxiety co‐morbid disorder Adjunctive therapy: not mentioned Adjunctive medication: not mentioned | |
| Interventions | Participants were randomly assigned to either 1. Individual CBT + standardised letter to family doctor (n = 56) Duration: 10 weekly sessions of 1 hour, during a period of 10 weeks Treatment protocol: CBT: muscle relaxation training, behaviour modification, emotional mindfulness, cognitive restructuring, social skills, based on Escobar 1998; standardised letter with treatment advice for GP based on Smith 1991 Therapist: psychologists 2. Group CBT + standardised letter to family doctor (n = 64) Duration: 10 weekly sessions of 2 hours, during a period of 10 weeks Treatment protocol: CBT: muscle relaxation training, behaviour modification, emotional mindfulness, cognitive restructuring, social skills, based on Escobar 1998; standardised letter with treatment advice for GP based on Smith 1991 Therapist: psychologists 3. TAU: standardised letter to family doctor only (n = 48) Duration: NA Treatment protocol: standardised letter with treatment advice for GP based on Smith 1991 Therapist: NA | |
| Outcomes | Time points for assessment: baseline, after 10 weeks (immediately after treatment) and 6 and 12 months after treatment (i.e. about 9 and 15 months after baseline) Primary outcome: 1. severity of somatisation (Screening for Somatic Disorders and SSS scale) 2. anxiety and depression (HADS) Secondary outcome: 1. quality of life (SF‐36: reported in Gili 2014) 2. self declared health services (according to design paper (Magallon 2008), but not reported) 3. global improvement (CGI) (according to design paper (Magallon 2008), but not reported) | |
| Notes | Date of study: data collection began in March 2008 and ended in June 2010 Funding source: Red de Investigacion en Actividades de Prvencion y Promocion de la Salud Declarations of interest among the primary researchers: authors declared that they had no competing interests | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence (Maggalon 2008, p. 4) |
| Allocation concealment (selection bias) | Low risk | Allocation was carried out by an independent person who was not involved in the study (p.602) Using central telephone. Sequence will be concealed until interventions are assigned (Moreno 2013, Magallon 2008, p. 4) |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants could not be blinded |
| Blinding of outcome assessment (detection bias) | Unclear risk | Study personnel that carried our the measurements were unaware of which treatment the participant was given. GPs were also kept blind to intervention, as participants were asked not to reveal their treatment condition. However, some outcomes were participant rated and participants could not be blinded (Moreno 2013, p. 602) |
| Incomplete outcome data (attrition bias) | Low risk | < 20% drop‐out, and intention‐to‐treat analysis with last observation carried forward |
| Selective reporting (reporting bias) | High risk | Healthcare use and CGI were mentioned in protocol but not reported |
| Treatment fidelity | Low risk | There were 2 different treatment conditions following the same protocol: individual and group formats (Moreno 2013, ref 23) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: DSM‐IV diagnosis of multisomatoform disorder Method of diagnosis: participants were screened with the PHQ‐15 and SF‐36, then SCID, modified to check for presence of multisomatoform disorder (at least 3 current somatoform symptoms that are functionally disabling and that an organic disease or another mental disorder cannot sufficiently explain, and a history of somatoform symptoms over at least 2 years, resulting in healthcare use Exclusion criteria: insufficient cognitive abilities, severe, chronic and disabling somatic disease or severe co‐morbid mental disorder that caused major impairment in social functioning (e.g. schizophrenia, severe forms of bipolar disorder or substance misuse), risk of suicide, people undergoing psychotherapy at the time of the screening or inability to speak German. In addition, a small number of people with a DSM‐IV diagnosis of hypochondriasis were excluded Total number randomised: 211 Age: for intervention group, M = 47.9 (SD = 10.8); for control group, M = 48.0 (SD = 12.4) Sex: 66% women; 34% men; for intervention group 63% women (n = 67), for control group 69% women (n = 72) Severity of symptoms at baseline:number of SCID somatoform symptoms: for intervention group M = 10.0 (SD = 3.9), for control group M = 10.6 (SD = 4.0) Duration of symptoms at baseline: for intervention group M = 10.4 years (SD = 5.5), for control group M = 10.8 (SD = 5.5) Setting: recruited from outpatients departments of neurology and internal medicine as well as from pain treatment centres and an orthopaedics private clinic. Treatment setting: outpatient departments of psychosomatic medicine Location: southern Germany (Munich, Düsseldorf, Hannover, Heidelberg, Münster and Regensburg) Number of treatment centres: 6 Co‐morbidities: unknown Adjunctive therapy: not mentioned Adjunctive medication: not mentioned | |
| Interventions | Participants were randomly assigned to either 1. Psychodynamic interpersonal psychotherapy (n = 107) Duration: 12 weekly sessions, 1st session 90 minutes, other sessions 45 minutes, during a period of 12 weeks Treatment protocol: manualised treatment consisted of 3 phases: 1. emphasis lay on building a therapeutic relationship with underscoring the legitimacy of bodily complaints and relaxation was introduced, 2. clarifying the participant's emotions, 3. concentrates on termination issues (Sattel 2012, ref 20) Therapist: 4 psychologists and 4 physicians with at least 3 years of training in psychotherapy, who were trained in the use of the manual 2. Enhanced medical care (n = 104) Duration: 3 approximately 30‐minute sessions at 6‐week intervals Treatment protocol: participants received education and counselling regarding therapeutic alternatives based on evidence‐based guidelines for the treatment of somatoform disorders/functional somatic syndromes in primary and somatic specialist care Therapist: physicians specifically trained in EMC | |
| Outcomes | Time points for assessment: baseline, 3 months (end of treatment), and 9 months after end of treatment Primary outcome: 1. SF‐36 ‐ PCS at 9 months' follow‐up Secondary outcome: 1. SF‐36 ‐ MCS 2. PHQ‐15 somatisation module 3. PHQ‐9 depression module 4. Health anxiety: WI 5. doctor visits, use of antidepressants, and use of psychotherapy | |
| Notes | Date of study: between June 2006 and December 2007 participants were selected, follow‐up continued until the beginning of 2009 Funding source: German Research Foundation Declarations of interest among the primary researchers: the authors report no conflicting interests | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was computer generated |
| Allocation concealment (selection bias) | Low risk | After receiving informed consent, the authors submitted a randomisation request, which was received within 24 hours |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Participant administered questionnaires: blinding impossible Healthcare use: blinding unclear |
| Incomplete outcome data (attrition bias) | Low risk | < 20% drop‐outs, multiple imputation, and intention to treat |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Low risk | The used treatment manual was developed jointly and pilot‐tested over the course of 3 years (Sattel 2012, page 61) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: cluster‐randomised controlled trial | |
| Participants | Diagnosis: MUS Method of diagnosis: participants were eligible in case of: 1. persistent (> 6 months) bodily complaints without sufficient explanatory peripheral organ pathology (according to GP), 2. MUS as the main treatment issue, 3. PHQ‐15 score of ≥ 5, 4. relevant health anxiety on the WI‐7 (score ≥ 4), or a combination of these Exclusion criteria: age < 18 or > 70 years, living further than 20 miles away from the respective practice; ongoing psychotherapy; substance abuse; severe psychiatric disorder (e.g. major depression, psychosis, dementia); severe organic disease; inability to complete the questionnaire, or ongoing litigation due to disability, pension or compensation for personal suffering Total number randomised: 328 Age: for intervention group, M = 50.8 (SD = 12.0); for control group, M = 46.6 (SD = 12.9) Sex: for intervention group 75.3% women (n = 128), 24.7% men (n = 42); for control group 74.6% women (n = 100), 25.6% men (n = 34) Severity of symptoms at baseline: somatic symptom severity according to PHQ‐15‐score: LOW (0‐9): for intervention group 28.2% (n = 48) for control group 30.6% (n = 41) MEDIUM (10‐14): for intervention group 38.2% (n = 65) for control group 35.8% (n = 48) HIGH (15‐30): for intervention group 33.5% (n = 57) for control group 33.6% (n = 45) Duration of symptoms at baseline: for intervention group M = 6.74 years (SD = 5.4), for control group M = 5.00 years (SD = 4.6) Setting: participants were recruited and treated by GPs in primary care Location: Heidelberg area, Germany Number of treatment centres: 35 GPs (from 34 practices) Co‐morbidities: Depressive symptoms: for intervention group 33.5% (n = 57); for control group 43.3% (n = 58) Generalised anxiety: for intervention group 16.6% (n = 28); for control group 21.8% (n = 29) Panic disorder: for intervention group 21.8% (n = 29); for control group 17.3% (n = 23) Musculoskeletal system disorders: for intervention group 45%; for control group 51% Hypertension: for intervention group 39%; for control group 39% Endocrine/alimentary/metabolic disorders: for intervention group 34%; for control group 34% Gastrointestinal system disorders: for intervention group 25%; for control group 29% Adjunctive therapy: none reported Adjunctive medication: none reported | |
| Interventions | Participants were randomly assigned to either 1. GP training in diagnosis and management of MUPS and group leading (GP level) + an interpersonal approach of psychodynamically based therapy (participant level) (n = 183) Duration: GP level: 4 training sessions, in total 15.5 hours (diagnosis + management of MUPS) + 3 sessions, in total 12 hours (group leading) participant level: 10 weekly sessions of 90 minutes + 2 booster sessions 3 and 9 months later Treatment protocol: GP level: guideline based curriculum for training of GPs in diagnosis and management of MUPS, consisting of lectures, discussions and role plays (Schaefert 2013, ref 42 for details) + GP training in group leading (methodology not described) Participant level: manualised group intervention consisting of an interpersonal approach of psychodynamically based therapy, with embedded cognitive behavioural elements (Schaefert 2013, table 1 and ref 43 for details) Therapist: GP level: the investigators; participant level: GP + 1‐3 psychosomatic specialists (with ≥ 3 years of training in psychosomatic therapy) 2.GP training in diagnosis and management of MUPS (n = 145) Duration: GP level: 4 training sessions, in total 15.5 hours (diagnosis + management of MUPS) Treatment protocol: guideline based curriculum for training of GPs in diagnosis and management of MUPS, consisting of lectures, discussions and role plays (Schaefert 2013, ref 42 for details) Therapist: GP level: the investigators | |
| Outcomes | Time points for assessment: baseline and 6 months, 12 months after baseline Primary outcome: Quality of life (SF‐36, PCS and MCS) Secondary outcome: Somatic symptom severity (PHQ‐15) Depression (PHQ‐9) Anxiety and panic (PHQ anxiety and panic, only at baseline) Stress (PHQ stress) Health anxiety (WI) Healthcare utilisation (GP documentation and self report) | |
| Notes | Date of study: participant recruitment started in November 2007 in both groups and ended in September 2008 in the intervention group and in December 2009 in the control group, follow‐up continued until the end of 2010 Funding source: German Federal Ministry of Education and Research Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | GPs were unit of randomisation, randomisation was performed in a data and co‐ordinating centre |
| Allocation concealment (selection bias) | Low risk | Blinded randomisation was performed by a statistician under independent management. The GPs were informed by a research assistant |
| Blinding of participants and personnel (performance bias) | High risk | No blinding of participants and personnel possible |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | High risk | Incomplete data in intervention group at 6 months 20.8%, at 12 months 21.9% Incomplete data in control group at 6 months 31.8%, at 12 months 25.6% |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Low risk | The participating GPs were trained with a guideline‐based curriculum in the diagnosis and management of MUS (Schaefert 2013, ref 41, 42) |
| Researcher allegiance | Unclear risk | Some of the authors were also providing the intervention |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: somatisation Method of diagnosis: participants of 20‐45 years who had ≥ 15 contacts in the past 3 years and who had ≥ 5 somatisation symptoms according to a somatisation scale (based on all symptoms listed in DSM‐IIIR) Exclusion criteria: cancer, AIDS, rheumatoid arthritis, multiple sclerosis, dementia, schizophrenia, mental disorder, and psychosis. Included people with other chronic diseases, such as asthma, osteoarthritis, or cardiovascular diseases Total number randomised: 161 Age: for intervention group M = 38 (IQR = 33‐41), for control group M = 39 (IQR = 36‐41) Sex: for intervention group 80% female (n = 61), for control group 78% female (n = 59) Severity of symptoms at baseline: mean somatisation score (scale 0‐48): for intervention group M = 20 (IQR = 16‐25), for control group M = 22 (IQR = 17‐22) Duration of symptoms at baseline: unknown Setting: participants were recruited in the registration network of primary physicians (primary care). the intervention took place at participants' homes Location: Maastricht area, the Netherlands Number of treatment centres: 77 participants' homes Co‐morbidities: of the 77 participants who actually received the intervention, 34 had an active depressive or anxiety disorder (16 depressive, 30 anxiety) according to the DSM‐IV screening. 2 participants fulfilled criteria of DSM‐IV hypochondriasis and 18 of a DSM‐IV chronic benign pain syndrome Adjunctive therapy: none reported Adjunctive medication: none reported | |
| Interventions | Participants were randomly assigned to either 1.Disclosure intervention (n = 81): Duration: unknown Treatment protocol: treatment consisted of 2 meetings with a disclosure doctor + an optional meeting with the doctor and the GP. They were invited to disclose emotionally important events in their life. If not mentioned spontaneously, the doctor asked questions about family life, health, work situation, and childhood Therapist: a trained disclosure doctor and in the third session also the GP 2.Usual care (n = 80): Duration: NA Treatment protocol: NA Therapist: NA (care as usual by own GP) | |
| Outcomes | Time points for assessment: baseline, 6, 12 and 24 months after baseline Primary outcome: 1. Healthcare use (number of visits to all health care) Secondary outcome: 1. Subjective health (scale) 2. Severity of symptoms (SCL‐90 subscore) 3. Depressive symptoms (SCL‐90 subscore) 4. Anxiety (SCL‐90 subscore) 5. Sick leave (number of weeks of sick leave over the preceding 6 months) | |
| Notes | Date of study: unknown, published in 2001 Funding source: Netherlands Organisation for Scientific research Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation was stratified (1 stratum per practice), using a sequence of labelled cards in opaque, sealed, numbered envelopes |
| Allocation concealment (selection bias) | Low risk | An independent person produced the randomisation envelopes, and the research assistant, who did not apply the intervention, executed the randomisation procedure |
| Blinding of participants and personnel (performance bias) | High risk | Although the general practitioners knew which participant received the intervention, they were not told which participants participated as controls. Participants could not be blinded for the intervention |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | Low risk | In the intervention group 70/81 (86.4%) participants completed the trial (and questionnaire at 2 years follow‐up) In the control group 67/80 (83.7%) participants completed the trial (and questionnaire at 2 years' follow‐up) (Schilte 2001, page 87) (loss to follow‐up < 20%) |
| Selective reporting (reporting bias) | High risk | Only results at 24 months of follow‐up are reported |
| Treatment fidelity | High risk | No protocol or manual for treatment (Schilte 2001, page 323) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Unclear risk | Results were not corrected for baseline imbalances |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: BDS Method of diagnosis: participants received a thorough biopsychosocial assessment including a review of all clinical records, a SCAN interview, a physical and neurological examination, and a laboratory screening battery were performed. Participants aged 20‐45 years with chronic (i.e. ≥ 2 years' duration) BDS of the severe multi‐organ type, which requires functional somatic symptoms from at least 3 of 4 bodily systems, and moderate to severe impairment in daily living (Schröder 2012, ref 18 and 19 for details) Exclusion criteria: severe psychiatric morbidity (psychotic and bipolar disorders, alcohol or drug misuse), people involved in litigation, those who were pregnant and those who were not fluent in the Danish language (operationalised as non‐Scandinavian origin) Total number randomised: 120 Age: for intervention group, M = 35.4 (SD = 6.3); for control group, M = 36.2 (SD = 6.5) Sex: for intervention group 74% women (n = 40), 26% men (n = 14); for control group 83% women (n = 55), 17% men (n = 11) Severity of symptoms at baseline: number of functional somatic symptoms: for intervention group M = 32.3 (SD = 7.5), for control group M = 32.6 (SD = 10.0). Duration of symptoms at baseline: for intervention group M = 6.7 (IQR = 3‐14), for control group M = 9.5 (IQR = 4‐15) Setting: the intervention took place in cooperation with the university general hospital in Aarhus, Denmark. Participants were referred from all primary care physicians and hospital wards in the western part of Denmark.(primary and secondary care) Location: Western part of Denmark (Jutland), which covers a population of approximately 2 million persons living in both urban and rural areas. Number of treatment centres: unclear Co‐morbidities: Major depressive disorder: for intervention group 17% (n = 9); for control group 21% (n = 14) Dysthymia: for intervention group 4% (n = 2); for control group 5% (n = 3) Anxiety disorder: for intervention group 19% (n = 10); for control group 18% (n = 12) At least 1 of the above diagnoses: for intervention group 30% (n = 16); for control group 36 (n = 24) Lifetime psychiatric co‐morbidity: for intervention group 57% (n = 31); for control group 61% (n = 40) Adjunctive therapy: none reported Adjunctive medication: none reported | |
| Interventions | Participants were randomly assigned to either 1.STreSS intervention (n = 54) Duration: 9 x 3.5 hour sessions during a period of 4 months Treatment protocol: 1. Comprehensive lifetime review of case notes and clinical records; 2. Comprehensive biopsychosocial assessment and individualised information about the nature,course and treatment options for the symptoms; 3. Letter to participant's primary care physician and referring doctor (if not the primary care physician) regarding diagnosis and illness history as well as treatment recommendations in case of co‐morbid depression or anxiety; 4. 'Usual care' delivered by primary care physician and specialists; 5. 9 modules of manualised psychotherapy, based on a cognitive‐behavioural approach. Each participant was allowed to receive 2 supplemental individual consultations in case of new important physical symptoms or major psychiatric problems; 6. Letter with management recommendations for functional somatic symptoms sent to primary care physician; 7. Treatment manual, including schedule, symptom diary, educational material, worksheets and homework assignment for the 9 treatment modules; 8. Consultancy service by telephone for primary care physicians and specialists; 9. Close cooperation with social authorities or the participant's employer, when needed (see Schröder 2012a, figure 1 for details) Therapist: consultants or senior residents in psychiatry with at least 2 years of training in cognitive‐behavioural treatment, experience with group treatment and expertise in the field of functional somatic syndromes. The senior residents were supervised. 2.Enhanced usual care (n = 66) Duration: 4 months Treatment protocol: 1. Comprehensive lifetime review of case notes and clinical records; 2. Comprehensive biopsychosocial assessment and individualised information about the nature,course and treatment options for the symptoms; 3. Letter to participant's primary care physician and referring doctor (if not the primary care physician) regarding diagnosis and illness history as well as treatment recommendations in case of co‐morbid depression or anxiety; 4. 'Usual care' delivered by primary care physician and specialists (see Schröder 2012a, figure 1 for details) Therapist/face‐to‐face contact: GP, occasionally assisted by a mental care specialist | |
| Outcomes | Time points for assessment: baseline, 4 months, 10 months, 16 months after baseline Primary outcome: 1. treatment response (improvement in the SF‐36 aggregate score 'physical functioning', 'bodily pain' and 'vitality') 2. PCS (subscore SF‐36) Secondary outcome: 1. health anxiety (WI) 2. subjective physical symptoms (physical subscale SCL‐90) 3. mental well‐being (SCL‐8, severity of depression and anxiety) | |
| Notes | Date of study: between March 2005 and December 2006 the case notes of all participants referred were screened for eligibility, follow‐up continued until 16 months after Funding source: Central Denmark Region, the Aarhus University Hospital Research Initiative, the A.P. Møller Foundation for the Advancement of Medical Science and the Medical Association for the County of Aarhus Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | In a block randomisation protocol participants were randomised by means of a computer algorithm that used predefined concealed random numbers and stratified for gender and psychiatric lifetime co‐morbidity status. We used the ratio 9 : 11 (STreSS vs. enhanced usual care) because we expected a higher attrition rate in those allocated to enhanced usual care |
| Allocation concealment (selection bias) | Unclear risk | It was not described who performed the allocation |
| Blinding of participants and personnel (performance bias) | High risk | Referring doctors and therapists were aware of the assignment, as were the participants |
| Blinding of outcome assessment (detection bias) | High risk | Questionnaires were sent by post and administered by independent research assistants who were unaware of the allocation of participants. However, participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | High risk | Incomplete data in intervention group at total of all time points 20.3% (11 out of 54 participants) Incomplete data in control group at total of all time points 36.4% (24 out of 66 participants) (see Schröder 2012, figure 2 for details) |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Low risk | Treatment was based on manualised modules (Schröder 2012, appendix) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: multiple somatoform symptoms Method of diagnosis: participants ≥ 18 years of age with at least 2 somatoform symptoms according to IDCL (for DSM‐IV). For each recorded symptom, the researchers checked whether there was substantial suffering or impairment. A medical evaluation was performed by a physician to exclude medically explained symptoms Exclusion criteria: medically explained symptoms, serious concentration or language problems, suicidal tendencies, psychotic symptoms Total number randomised: 173 (134 actually started treatment, lower numbers in Zaby 2008) Age: for intention‐to‐treat sample (n = 134) M = 48.02 years (SD = 12.34) (no baseline imbalances between study groups) Sex: for intention‐to‐treat sample (n = 134) 76.9% women (n = 103), 23.1% men (n = 31) (no baseline imbalances between study groups) Severity of symptoms at baseline: number of symptoms M = 9.9 (SD = 5.5) Duration of symptoms at baseline: ≥ 6 months Setting: participants were consecutively recruited in co‐operation with primary care physicians, psychotherapists, and by advertisements in local newspapers in the southwest of Germany Treatments were conducted in the outpatient treatment centre for psychological intervention at the University of Landau and the University of Mannheim, Germany Location: Landau and Mannheim region, Germany Number of treatment centres: 2 Co‐morbidities: Panic disorder: for intention‐to‐treat sample 20.1% (n = 27) Social phobia: for intention‐to‐treat sample 9.0% (n = 12) Specific phobia: for intention‐to‐treat sample 6.0% (n = 8) Generalised anxiety: for intention‐to‐treat sample 10.4% (n = 14) Major depressive disorder: for intention‐to‐treat sample 18.7% (n = 25) Adjunctive therapy: participants were free to seek further care Adjunctive medication: participants were free to seek further care | |
| Interventions | Participants were randomly assigned to either 1. CBT (n = 49) Duration: manualised group training with 8 weekly sessions of 90 minutes in 8 groups of 4‐11 members Treatment protocol: the CBT used in this study was developed on the basis of theoretical considerations (Deary et al. 2007) and standardised guidelines for psychological therapy of somatoform disorders, as published elsewhere (Rief 1999; Rief 2002; Sharpe 1992). The manual contained detailed guidelines for conducting each session. Aim of treatment was to create a model to understand bodily discomfort, with integrated biological, psychological and social factors (see Zaby 2008, table 1 for extended information about the group sessions). Therapist: psychological psychotherapists who were supervised regularly 2. Progressive muscle relaxation (n = 41) Duration: manualised group training with 8 weekly sessions of 90 minutes in 11 groups of 4‐11 members Treatment protocol: the progressive muscle relaxation treatment was based on modifications of Jacobson's original program by Bernstein and Borkovec, following a manual (Zaby 2008). It involved learning to tense and relax groups of muscles beginning with a large number of small groups (in this case 16) and then proceeding in steps to a smaller number of large groups (first 7, then 4 groups) (for details, see Schröder 2013, page 299) Therapist/face‐to‐face contact: psychological psychotherapists who were supervised regularly 3. Waiting list control (excluded from analysis, as participants in waiting list group were not randomly assigned) Duration: NA Treatment protocol: participants with a waiting time for the intervention longer than 4 weeks, less than 3 months were included in the waiting list group Therapist/face‐to‐face contact: NA | |
| Outcomes | Time points for assessment: baseline, directly post‐treatment (8 weeks) and 6 months after baseline Primary outcome: 1. Intensity and number of symptoms (SOMS‐7) Secondary outcome: 1. Depression (HADS‐D) 2. Anxiety (HADS‐A) 3. Physical and mental health (SF‐12, PWB, and MWB subscale) 4. Medical care utilisation in previous 6 months (interview at baseline and 6 months) | |
| Notes | Date of study: participants were recruited from April 2005 until May 2006. Treatments were conducted between April 2005 and October 2008 Funding source: the study was supported by a grant awarded to Annette Schröder by the German Research Foundation (DFG) Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised for CBT or PMR using random sequences, exact method not described. When both groups were full, newly included participants were included in the waiting list group. As this group was not randomly assigned we excluded data from this group from analysis |
| Allocation concealment (selection bias) | Low risk | The randomisation was performed by a person who was not involved in assessment or treatment delivery |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants could not be blinded. Blinding of personnel not described |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | High risk | In both intervention groups 23% of participants dropped out before the first treatment (> 20%) |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Low risk | CBT and PMR were conducted as a manualised group training (Schröder 2013, treatment conditions) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Unclear risk | Participants were randomised for CBT or PMR. When both groups were full, newly included participants were included in the waiting list group. In a later stage, these participants were included in both intervention groups. (source: email contact with author) As participants are their own control participant due to this method, we decided to exclude data from the waiting list group from analysis |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: somatisation Method of diagnosis: participants (18‐65 years old) were included if they screened positive for the SOMS‐2 and the GHQ‐12 and if the attending hospital physician was not able to provide a clear physical explanation for the complaints. The screening criteria for SOMS were 4 somatoform symptoms for men and 6 for women, and the cut‐off for the GHQ was ≥ 2. Other inclusion criteria were: persistent symptoms for at least 3 months, ≥ 5 annual doctor's visits or 2 hospitalisations during the past year as a result of the respective symptoms and availability for ≥ 6 months Exclusion criteria: severe mental disorders, e.g. major depression with suicidal ideation, eating disorders, alcohol or substance abuse, an organic disease deemed responsible for most of the symptoms, psychotherapy ‐ ongoing or completed during the past 3 years, pregnancy and low intellectual capacity Total number randomised: 91 Age: for intervention group, M = 44.43 (SD = 13.329); for control group, M = 49.22 (SD = 11.084) Sex: for intervention group 69.4% women (n = 34), for control group 71.4% women (n = 30) Severity of symptoms at baseline: 55 of the participants (92%) had a somatoform disorder Duration of symptoms at baseline: unknown Setting: general hospital (inpatients). Data were collected in the Departments of Neurology, Internal Medicine, General Medicine and Orthopedics of the University Hospital. A research assistant visited the participating units 3 times per week and systematically examined all new participants Location: Freiburg, Germany Number of treatment centres: 1 (although 4 different departments) Co‐morbidities: diagnostic interviews were conducted with 60 participants (66%). 24 (40%) were had depression and 18 (32%) had an anxiety disorder Adjunctive therapy: none reported Adjunctive medication: none reported | |
| Interventions | Participants were randomly assigned to either 1. Short‐term psychotherapeutic intervention (n = 49) Duration: 5 sessions of approximately 50 minutes, during a period of 2 weeks Treatment protocol: treatment consisted of a program predominantly based on the reattribution model, the World Health Organization training package for primary care physicians, cognitive behavioural techniques and a psychodynamic approach (see Schweickhardt 2007, table 1 for the session topics and ref 29 for the treatment manual) Therapist: licensed psychotherapists (3 physicians and 2 psychologists), who have been working with somatising participants for several years 2. Psychoeducational reading material (n = 42) Duration: NA Treatment protocol: psychoeducational reading material consisting of 9 pages describing the aetiology, course, and treatment recommendation of somatoform symptoms Therapist/face‐to‐face contact: NA | |
| Outcomes | Time points for assessment: baseline, 2 weeks, 3 months and 6 months after baseline Primary outcome: 1. Changes regarding motivation for psychotherapy (FPTM) 2. Contact with a psychotherapist Secondary outcome: 1. number and intensity of somatoform symptoms (SOMS‐7) 2. changes regarding emotional distress (HADS, GHQ) 3. quality of life (SF‐12) | |
| Notes | Date of study: participants were recruited between June 2002 and May 2004. The last follow‐up assessments were performed in November 2004 Funding source: this clinical trial was supported by grants from the German Research Association (Deutsche Forschungsgemeinschaft) Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Envelopes containing the allocation information were created in a random order. Participants who had fulfilled all inclusion criteria were assigned to the 2 different groups |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed by an independent statistician. He was not aware of the therapy allocation or the details of the study design |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blinded due to the study conditions. Data were collected by independent research assistants, it is unknown if they were blinded |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | High risk | Missing data at 6‐month follow‐up for psychotherapy motivation and the secondary outcomes were up to 28.5% in the intervention group and 23.8% in the control group (> 20%) |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Low risk | Treatment was based on a manual regarding therapy goals, basic concepts and operationalisation of the individual therapy steps (Schweickhardt 2007, ref 29) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Unclear risk | A high percentage (29%) of the participants from the control group became involved in psychotherapy. This might have influenced the results |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: MUS Method of diagnosis: participants (aged 18‐64, Dutch natives) with no explanation for their symptoms according to their internist were interviewed by the researchers. Those with a mean intensity of symptoms score of ≥ 5 (88%) or a HADS anxiety/depression score of ≥ 10 and ≥ 5 points on functional impairment score (12%) were eligible Exclusion criteria: organic psychiatric disorders (e.g. dementia) or with chronic alcoholism, psychosis, or suicidal ideas and those currently having psychological or psychiatric treatment Total number randomised: 79 Age: for intervention group, M = 36.4 (SD = 12.4); for control group, M = 37.8 (SD = 12.8) Sex: for intervention group 46% women (n = 18), 54% men (n = 21); for control group 53% women (n = 21), 47% men (n = 19) Severity of symptoms at baseline: number of symptoms for intervention group M = 12.9 (SD = 6.7), for control group M = 13.0 (SD = 7.5) Duration of symptoms at baseline: unknown Setting: general medical outpatient clinic of Leiden university hospital (recruitment and treatment) Location: Leiden, the Netherlands Number of treatment centres: 1 Co‐morbidities: psychiatric disorders (based on caseness in the present state examination at baseline): 46% (n = 18) in intervention group; 28% (n = 11) in control group Adjunctive therapy: none reported Adjunctive medication: none reported | |
| Interventions | Participants were randomly assigned to either 1. CBT (n = 39) Duration: 6‐16 x 1‐hour sessions during a maximum period of 6 months Treatment protocol: a broad CBT approach was used in view of the heterogeneous nature of the participants' problems. The main therapeutic techniques included identification and modification of dysfunctional automatic thoughts and behavioural experiments aimed at breaking the vicious cycle of the symptoms and their consequences. The methods used were similar to those described by Salkovskis and Sharpe et al. (for details: Speckens 1995, ref 2 and 12) Therapist: a physician trained in CBT and a behavioural therapist 2. Control group (n = 40) Duration: 1 x 90‐minute session every 3 months (for doctors) Treatment protocol: treatment consisted of optimised medical care. The quality of care was enhanced by basic training by 3 researchers in the detection and management of psychiatric disorders Therapist: the researchers | |
| Outcomes | Time points for assessment: baseline 6 months and 12 months after baseline Outcomes: 1. change in physical symptoms (perceived change, frequency and intensity according to non‐standardised questionnaire) 2. psychological distress (GHQ and HADS anxiety and depression subscale) 3. functional impairment (SIP subscales and numerical analogue scales on functional impairment) 4. hypochondriacal beliefs (IAS subscales health anxiety and illness behaviour and WI) 5. healthcare use (frequency of visits to GP, based on visit counts by participant and doctor, only at 12 months) | |
| Notes | Date of study: from March 1992 to March 1993 participants were recruited, follow‐up continued until 1 year after Funding source: Dutch Ministry of Education and Sciences and the Ministry of Welfare, Public Health Care and Culture Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed using computerised randomisation in blocks of 4 (confirmed by email) |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed by an independent person (confirmed by email) |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | Low risk | Drop‐out rates were low at all follow‐ups (< 20%) |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Unclear risk | A certain structure in methodology, but no manual or protocol was used (Speckens 1995, p. 1329) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: medically unexplained complaints Method of diagnosis: participants (16‐65 years old) with ≥ 5 medically unexplained symptoms and repeated consultations during the last 6 months underwent a physical examination by a GP and a research psychiatrist plus a re‐assessment through 2 questions by the research psychiatrist: 1. What are your symptoms/problems, why are you here today? and, 2. Are there any other symptoms/problems? Finally 1 question was asked about how many visits participants had in last 6 months according to current symptoms, to make sure that they fitted inclusion criteria. After inclusion the standardised BSI questionnaire was filled out by all participants. Exclusion criteria: dementia, psychosis, active suicidal thoughts, alcohol dependence or current treatment for a psychiatric disorder Total number randomised: 68 Age: for intervention group, M = 38.1 (SD = 13); for control group, M = 38.7 (SD = 14) Sex: for intervention group 64.7% women (n = 22), 35.3% men (n = 12); for control group 76.5% women (n = 26), 23.5% men (n = 8) Severity of symptoms at baseline: number of symptoms: for intervention group M = 7.8 (SD = 1.7), for control group M = 8.2 (SD = 1.9) Duration of symptoms at baseline: 57% was > 2 years ill, in the intervention group 20.6% (n = 7) had < 6 months symptoms, in the control group 14.7% (n = 5) Setting: participants were selected by GPs and treated in general outpatient clinic of a general hospital where participants initiate their own visits without prior appointments (primary care) Location: Colombo, Sri Lanka Number of treatment centres: 1 Co‐morbidities: not described Adjunctive therapy: none described Adjunctive medication: none described | |
| Interventions | Participants were randomly assigned to either 1. CBT (n = 34) Duration: 6 x 30‐minute structured sessions over a period of 3 months Treatment protocol: treatment consisted of structured regular visits to 1 professional carer thereby hoping to reduce unstructured visits to different practitioners and co‐ordinating care. Treatment was based on the principles of CBT, using modifications of that described by Salkovskis and Sharpe et al. and Goldberg et al.'s reattribution technique for details Sumathipala 2000, ref Salkovskis, Sharpe and Goldberg). Through structured sessions, participants were made aware of the psychological component of their condition, and helped to reduce unnecessary medical consultations and investigations. When possible, 1 non‐professional carer, usually the spouse, was involved. The intervention group was managed by a research psychiatrist using the above specified intervention strategy. A treatment manual was prepared to keep the therapeutic sessions uniform Therapist: research psychiatrist 2. Control group (n = 34) Duration: NA Treatment protocol: the controls received assessments but no intervention in terms of a structured therapy. They continued to receive care from their usual carers and could visit the doctors of their choice. The controlled group received appointments for a follow‐up assessment after 3 months Therapist/face‐to‐face contact: NA | |
| Outcomes | Time points for assessment: baseline and 3 months after baseline Outcomes: 1. level of distress/psychiatric morbidity (GHQ‐30) 2. number and severity of symptoms (BSI + 2 open‐ended questions) 3. number of participant initiated doctor visits (diary) 4. participants perceived satisfaction with previous treatment (VAS scale) | |
| Notes | Date of study: participant recruitment took place from consecutive participants attending the clinic from 15 December 1997 to the end of March 1998, the treatment and re‐assessments continued until the end of June 1998 Funding source: The Wellcome Trust (international programme) provided a project grant Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A list of treatment assignments was prepared in advance using simple randomisation by random numbers generated from a calculator. These were available in 68 sealed opaque envelops bearing sequential registration numbers on the outside of the envelope |
| Allocation concealment (selection bias) | Low risk | An epidemiologist who did not take part in the data collection was responsible for randomisation |
| Blinding of participants and personnel (performance bias) | Unclear risk | The first research psychiatrist opened the envelope to reveal the random treatment allocation. The non‐clinical research assistant and the second psychiatrist remained blind to the group status throughout the study. Participants could not be blinded |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | High risk | At 3 months, loss to follow‐up was 30% in the intervention group and 38% in control group (> 20%) |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Low risk | Treatments were structured. A treatment manual was prepared to keep the therapeutic sessions uniform. (Sumathipala 2000, p. 750) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: MUS Method of diagnosis: participants (16‐65 years old) with ≥ 5 MOS and repeated consultations during the last 6 months were selected by the primary care doctors. They underwent an extensive physical examination by trial co‐ordinator and trial physician plus an independent reassessment through 2 questions: 1. What are your symptoms/problems, why are you here today? and, 2. Are there any other symptoms/problems? to elicit the number of symptoms and visits in the previous 6 months. After inclusion the standardised BSI questionnaire was filled out by all participants Exclusion criteria: dementia, psychosis or alcohol dependence current treatment for a psychiatric disorder Total number randomised: 150 Age: aged 16‐58 years, M 35 years Sex: for intervention group 79% women (n = 59), 21% men (n = 16); for control group 77% women (n = 58), 23% men (n = 17) Severity of symptoms at baseline: number of symptoms M = 8.6 (SD = 2.2) Duration of symptoms at baseline: M = 42.0 months (SD = 40) Setting: a general outpatient clinic of a general hospital where participants initiate their own visits without prior appointments (primary care) Location: Colombo, Sri Lanka Number of treatment centres: 1 Co‐morbidities: not described Adjunctive therapy: none described Adjunctive medication: none described | |
| Interventions | Participants were randomly assigned to either 1. CBT (n = 75) Duration: 6 x 30‐minute structured sessions over a period of 3 months (of which 3 mandatory) Treatment protocol: treatment consisted of structured regular visits to 1 professional carer thereby aiming to reduce unstructured visits to different practitioners and co‐ordinating care. Treatment was based on the principles of CBT, using modifications of that described by Salkovskis and Sharpe et al. and Goldberg et al.'s reattribution technique for details Sumathipala 2000, ref Salkovskis, Sharpe and Goldberg) Treatment started with a SEMI interview by 1 of the authors: results, summary, and formulation based on findings were passed on to primary care physician, they were also trained to use this information to inform the strategy for their CBT intervention. Participants in the intervention group completed a diary, which was used during training. The CBT training was a short course consisting of 5 sessions covering the basis of MUS; the relevance of the explanatory model, elicited by the SEMI, to the CBT model of such symptoms; and the CBT treatment approach. Training was accomplished through lectures, supplemented by case vignettes and role‐play of therapeutic sessions by simulated participants based on case scenarios from the pilot trial, all with reference to the intervention manual (for details: Sumathipala 2008, ref 30) Therapist: trained primary care physicians 2. Structured care (n = 75) Duration: 6 x 30‐minute structured sessions over a period of 3 months (of which 3 mandatory) Treatment protocol: treatment started with a SEMI interview by 1 of the authors: only results were passed on to primary care physician, they were not trained to use this information to inform the strategy for their CBT intervention No CBT was given, but during the 6 sessions the physicians were free to manage the participants as they wished within the sessions. No training or supervision was provided for these doctors, and the intervention was not manualised Therapist: untrained primary care physicians | |
| Outcomes | Time points for assessment: baseline, 3 months, 6 months, 9 months and 12 months after baseline Outcomes: 1. number of symptoms (as counted by researcher) 2. level of distress/psychiatric morbidity (GHQ‐30) 3. number and severity of symptoms (BSI + 2 open‐ended questions) 4. number of participant initiated doctor visits (diary) | |
| Notes | Date of study: not described Funding source: The Wellcome Trust (international programme) provided a project grant Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Trial participants were first randomised to the 2 intervention groups using a random permuted block design, with a block size of 4. Next, participants were randomly allocated to 1 of the 3 doctors selected to deliver the intervention to which they had been allocated |
| Allocation concealment (selection bias) | Low risk | Randomisation codes were generated by a statistician in the UK and passed on to the independent epidemiologist (M.R.N.A.) in Sri Lanka, who executed the random allocation of treatment condition |
| Blinding of participants and personnel (performance bias) | High risk | Neither the primary care doctors who delivered the interventions nor the participants who received them could be masked to their allocation because of the nature of the interventions |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded, and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | High risk | Loss to follow‐up was highest after 6 and 12 months: 20% at both time points in the intervention group and 28% (6 months) and 30% (12 months) in the structured care group (> 20%) |
| Selective reporting (reporting bias) | Low risk | All intended outcomes are reported |
| Treatment fidelity | Low risk | Treatments were structured. A treatment manual was prepared to keep the therapeutic sessions uniform (Sumathipala 2000, p. 750) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: MUS Method of diagnosis: men and women (aged 18‐70 years) belonging to the 10% most frequently attending in the past year, who had physical symptoms for at least 6 months that were not (fully) explained by a physical disease or by substance abuse (according to the GP) were selected. They had to experience functional impairment due to these physical symptoms and they had to be eligible according to a MINI SCID interview Exclusion criteria: frequent attendance for other reasons than physical symptoms, physical symptoms fully explained by somatic diseases, no significant distress or functional impairment due to the symptoms, psychosis or bipolar disorder in medical history, current alcohol or drug abuse, cognitive impairment, problems with the Dutch language, and previous mindfullness‐based cognitive therapy Total number randomised: 125 Age: for intervention group, M = 47.6 (SD = 11); for control group, M = 46.5 (SD = 12) Sex: for intervention group 80% women (n = 49), 20% men (n = 12); for control group 68% women (n = 38), 32% men (n = 18) Severity of symptoms at baseline:somatisation disorder 13% in intervention group (n = 8), 13% in control group (n =7); pain disorder 18% (n =11) in intervention group, 21% (n = 12) in control group Duration of symptoms at baseline: not described Setting:primary care, potential participants were selected from the digital databases, screened for exclusion criteria by the GP, invited by letter and interviewed by telephone Location: area of Nijmegen, a medium‐sized city in the Netherlands, general practices were located in neighbourhoods with both low and higher socioeconomic standards Number of treatment centres: unknown Co‐morbidities: hypochondriasis 3% (n = 2) in intervention group, 2% (n = 1) in control group; depressive disorder 15% in intervention group (n = 9), 23% in control group (n = 13); anxiety disorder 25% in intervention group (n = 15), 25% in control group (n = 14); hypertension 30% in intervention group (n = 18), 20% in control group (n = 11), arthrosis 18% in intervention group (n = 11), 14% in control group (n = 8), asthma/bronchitis 18% in intervention group (n = 11), 11% in control group (n = 6); diabetes mellitus type II 10% in intervention group (n = 6), 9% in control group (n = 5) Adjunctive therapy: none reported Adjunctive medication: none reported | |
| Interventions | Participants were randomly assigned to either 1. Mindfullness‐based cognitive therapy (n = 64) Duration: 8 weekly group sessions of 2.5 hours + 1 silent day (6 hours) during a period of 8 weeks Treatment protocol: the programme protocol was based on the mindfullness‐based cognitive therapy format for people with recurrent depression (see Van Ravesteijn 2013, ref 11) consisted of formal meditation exercises such as body scan, sitting meditation, walking meditation, and mindful movement. Participants were also encouraged to cultivate awareness of everyday activities, such as eating or taking a shower. In addition, the programme included cognitive techniques such as psychoeducation, monitoring and scheduling of activities, identification of negative automatic thoughts, and devising a relapse prevention plan. In the section on psychoeducation, information about respecting physical and mental boundaries and dealing with impairments was included. The silent day was included to give participants the opportunity to deepen their mindfulness practice. To support home practice, participants received a folder with information about the individual sessions, homework assignments, and forms to keep a record of their practice, together with CDs with guided meditations and movement exercises Therapist: 2 experienced mindfulness trainers who had both participated in a 2‐year mindfulness training programme and who had many years of practice experience and experience with courses (both over 30 courses) 2. Enhanced usual care (n = 61) Duration: NA Treatment protocol: participants in the enhanced usual care condition received usual care provided by their GP and other healthcare professionals. The term 'enhanced usual care' was considered appropriate as all participants received a psychiatric interview. The GP was explicitly informed about the psychiatric diagnoses resulting from the interview Therapist: NA | |
| Outcomes | Time points for assessment: baseline, end of treatment and 9 months after baseline Primary outcome: 1. general health status (VAS of EuroQoL 5D) Secondary outcome: 1. mental and physical function (SF‐36, MCS and PCS subscales) 2. physical and mental symptoms (PHQ‐15 and PHQ‐9) 3. health anxiety (WI) 4. healthcare utilisation (contact count by participant) | |
| Notes | Date of study: participants were recruited from December 2009 to August 2010, follow‐up continued until 9 months after Funding source: the study was funded by research grants from The Netherlands Organization for Health Research and Development (ZonMW) Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated permuted‐block randomisation table was used, with block size 20. The participant identification number was matched with the corresponding name to inform each participant about the allocation |
| Allocation concealment (selection bias) | Low risk | The assistant performing allocation was blinded (participants had unique identification numbers) |
| Blinding of participants and personnel (performance bias) | Unclear risk | The research assistant was blinded for interview data. However, other personnel and participants could not be blinded due to the nature of the intervention |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up was < 20% in both research groups, at all follow‐up times |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported |
| Treatment fidelity | Low risk | Treatment followed a structured training protocol (Van Ravesteijn 2013, p. 198) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
| Methods | Study design: randomised controlled trial | |
| Participants | Diagnosis: UPS (according to SCID interview) Method of diagnosis: participants (aged 18‐65 years old, who were able to speak, read, and write Dutch) were eligible if their UPS persisted ≥ 6 months and if their UPS was classified as undifferentiated somatoform disorder or chronic pain disorder according to the criteria of the Structured Clinical Interview for DSM‐IV Axis I Disorders/ Patient edition (SCID‐I/P) Exclusion criteria: UPS not being the principal somatic disease; undifferentiated somatoform disorder or chronic pain disorder not being the principal DSM‐IV‐TR classification; handicaps like cognitive mental impairment with or without blindness impending the participant to participate in the training Total number randomised: 162 Age: for intervention group, M = 46 (IQR = 38‐53); for control group, M = 44 (SD = 35‐52) Sex: for intervention group 79.8% women (n = 67), 20.2% men (n = 17); for control group 82.1% women (n = 64), 17.9% men (n = 14) Severity of symptoms at baseline: undifferentiated somatoform disorder 38.1% for intervention group (n = 32) 39.7% for control group (n = 31); chronic pain disorder 61.9% for intervention group (n = 52), 60.3% for control group (n = 47) Duration of symptoms at baseline: for intervention group M = 8 years, for control group M = 9.5 years Setting: primary care, outpatient clinic and secondary community mental‐health service physicians' received periodical postcards informing them when and how to refer patients. Participants were also recruited via announcements in local newspapers and on websites of patients' associations. Treatment setting unclear Location: Rotterdam area, the Netherlands Number of treatment centres: unknown Co‐morbidities: for intervention group 45.2% had ≥ 1 DSM‐IV axis I disorders (n = 38), for control group this was 37.2% (n = 29) (for details about specific axis I and axis II disorders, see Zonneveld 2012, table 2) Adjunctive therapy: not mentioned Adjunctive medication: not mentioned | |
| Interventions | Participants were randomly assigned to either 1. Group training (n = 84) Duration: 13 weekly 2‐hour sessions in groups of 5‐9 participants (mean 6), in a period of 13 weeks Treatment protocol: treatment consisted of cognitive‐behavioural therapy based on the consequences model. In this model, psychological and social factors, are labelled as consequences of UPS. In the long term, these consequences might produce self perpetuating vicious circles that maintain or aggravate UPS. By changing and reducing the consequences, beliefs are addressed indirectly, after which the beliefs can still be addressed directly. Focus is on improvement of quality of life. Based on this tailored cognitive‐behavioural model, a manual was developed for a group training called 'Coping with the consequences of unexplained physical symptoms' (for details Zonneveld 2012, ref 38). Sessions concern psychoeducation on arousal, habits, activity, emotions, beliefs, physical fitness, information processing, breathing and relaxation, and relapse prevention Therapist: 6 psychologists with a Master's degree, 4 of whom had had at least 3 years' post‐Master's experience with group therapy or CBT, or both and who familiarised themselves with this method 2. Waiting list (n = 78) Duration: 13 weeks Treatment protocol: NA Therapist/face‐to‐face contact: NA | |
| Outcomes | Time points for assessment: baseline and directly post‐treatment (further follow‐ups are without a control group) Primary outcome: 1. improvement in quality of life (SF‐36, PCS and MCS) Secondary outcome: 1. improvement in quality of life (SF‐36, 8 individual subscales) 2. intensity of psychological problems (SCL‐90‐R, 8 subscales including depression and anxiety) | |
| Notes | Date of study: participants were recruited between February 2005 and September 2008. The follow‐up ended in December 2009; 1 year after the intervention group of the last randomisation had completed the training Funding source: the study was funded by RIAGG Rijnmond Declarations of interest among the primary researchers: none reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were assigned to the training or to the waiting list according to a computer generated randomisation list |
| Allocation concealment (selection bias) | Low risk | The randomisation was performed by an investigator who had no clinical involvement in the trial and was working in a different building that the building were assessment and enrolment were done |
| Blinding of participants and personnel (performance bias) | High risk | Participants and trainers could not be blinded for group assignment, as the control condition was a simple waiting list. The data were imported and analysed after participants had completed the trial |
| Blinding of outcome assessment (detection bias) | High risk | Participants were not blinded and most outcomes were participant reported |
| Incomplete outcome data (attrition bias) | High risk | Of the 84 participants in the intervention group, 23 dropped out (27.4%), of the 78 participants in the control group, 6 dropped out (7.7%) (intervention group loss to follow‐up > 20%) |
| Selective reporting (reporting bias) | Low risk | All intended outcomes reported, no means/SDs reported, but on our request these were provided for the meta‐analysis |
| Treatment fidelity | Low risk | The training was manual‐based (Zonneveld 2012, ref 24, 28) |
| Researcher allegiance | Low risk | No indication that researchers had a preference for 1 of the treatment modalities |
| Other bias | Low risk | No other sources of bias |
AIDS: acquired immune deficiency syndrome; BDS: bodily distress syndrome; BSI: Brief Symptom Inventory; CBT: cognitive behavioural therapy; CGI‐SD: Clinical Global Impession Scale for Somatoform Disorders; CIDI: Composite International Diagnostic Interview; DSM: Diagnostic and Statistical Manual of Mental Disorders; GAD: Generalised Anxiety Disorder Scale; GHQ: General Health Questionnaire; GP: general practitioner; GSI: General Symptom Index; HADS: Hospital Anxiety and Depression Scale; HAM‐A: Hamilton Anxiety Rating Scale; HAM‐D: Hamilton Depression Rating Scale; IAS: Illness Attitude Scales; IBQ: Illness Behaviour Questionnaire; ICD: International Classification of Diseases; IDCL: International Diagnostic Checklists; IQR: interquartile range; KKG: Krankheit und Gesundheit; M: mean; MCS: Mental Component Scale; Mini‐DIPS: mini‐Diagnostische Interview bei psychischen Störungen; MOS: Medical Outcomes Study; MUS: medically unexplained symptoms; MWB: Mental Well‐Being; n: number; NA: not available; PCI: psychiatric consultation intervention; PCS: Physical Component Score; PHQ: Patient Health Questionnaire; PRIME‐MD: Primary Care Evaluation of Mental Disorders; PWB: Psychological Well‐Being; ref: reference; SCAN: Schedules for Clinical Assessment in Neuropsychiatry; SCID: Structured Clinical Interview for Mental Disorders; SCL: Symptom Checklist; SD: standard deviation; SDI: Sleep Debt Index; SF‐12: 12‐item Short Form; SIP: Session Initiation Protocol; SPQ: Social Problem Questionnaire; SSS: Severity of Somatic Symptoms; TAU: treatment as usual; UPS: unexplained physical symptoms; VAS: visual analogue scale; WI: Whitely Index.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Compared 2 forms of CBT | |
| This study was not randomised | |
| No separate analysis for participants with somatisation (only for total group, including people with hypochondriacal health anxiety as their main problem) | |
| A non‐pharmacological intervention (relaxation therapy) was combined with a pharmacological one (antidepressants) | |
| GP training study | |
| Compared CBT with CBT+ BT | |
| Treatment as usual in the control group included pharmacological treatment | |
| Not MUPS or somatoform disorder | |
| This (pilot) study was not randomised | |
| The study did not concern people with MUPS of somatoform disorders explicitly | |
| No separate analysis for people with somatisation/MUPS | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders | |
| This study was not randomised | |
| This study was not randomised | |
| The study had a prospective study design (no randomised controlled study) | |
| Participants were not required to have medically unexplained symptoms or somatoform disorders | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders | |
| GP training study | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders | |
| The study was not randomised | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders | |
| Compared 2 forms of BT | |
| The study was not randomised | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders | |
| Treatment was focused on depressive symptoms, not on MUPS | |
| Participants include high healthcare utilisers, the participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders | |
| The study was not randomised | |
| No separate analysis for people with somatisation/MUPS | |
| The intervention consisted of a consultation letter | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders | |
| The study was not randomised | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders and the intervention included pharmacological treatment | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders and for a certain percentage of the participants intervention included pharmacological treatment | |
| GP training study | |
| The study was not randomised | |
| The study was not randomised | |
| Intervention aimed at psychiatric consultation model, combined with GP training | |
| Only people with chronic fatigue syndrome | |
| Participant selection procedure did not include a diagnostic interview or questionnaire to establish MUPS or somatoform disorders |
BT: behavioural therapy; CBT: cognitive behavioural therapy; GP: general practitioner; MUPS: medically unexplained physical symptoms.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomised controlled trial (cross‐over?) |
| Participants | Couples in which 1 of the partners met criteria for somatoform disorder or undifferentiated somatoform disorder as determined by the SOMS and who scored ≤ 101 on the Dyadic Adjustment Scale participated in this study |
| Interventions | Emotion focused couples therapy versus waiting list controls |
| Outcomes | Unclear. Abstract only reports on reported symptoms |
| Notes | Study included in Kleinstäuber 2011 |
| Methods | Phase 1 ‐ the development of a client manual that will be used as an adjunct to therapy Phase 2 ‐ randomised trial in primary care |
| Participants | People with MUPS |
| Interventions | Reattribution therapy |
| Outcomes | Modified Social Adjustment Scale (primary outcome measure) Illness Perception Questionnaire (IPQ), Hospital Anxiety and Depression Scale (HADS), Ecomomis Questionnaire (EQ), SCL‐90‐R (Measures psychological and somatic symptoms) and number of contacts with primary and secondary health care services (derived from participant questionnaire and case notes) |
| Notes | Registration in research register, article untraceable |
| Methods | Randomised clinical trial in primary health care |
| Participants | People with medically unexplained problems |
| Interventions | Intervention group: CBT by F‐grade community mental health nurses (advice) Control group: CBT by F‐grade community mental health nurses (treatment) |
| Outcomes | Unknown |
| Notes | Registration in research register, article untraceable |
| Methods | Cluster‐randomised controlled trial in primary care |
| Participants | People with symptoms of somatisation |
| Interventions | Intervention group: cognitive behavioural group therapy Control group: care as usual |
| Outcomes | Primary outcome measures: ‐ Perceived quality of life (SF‐12) ‐ Number of examinations (number of requested and programmed doctor's examinations during the period of study) |
| Notes | Registration in research register, article untraceable |
| Methods | Randomised controlled trial in inpatients |
| Participants | Inpatients with anxiety and somatisation disorders |
| Interventions | Intervention group: standard treatment + additional exercise training regimen Control group: standard treatment |
| Outcomes | ‐ Respiration, weight, and body fat ‐ Anxiety and depression (Hospital and Depression Scale, HADS), general state of health (SF‐36), and complaints (Symptom Check List, SCL‐90‐R, and the Giessener Beschwerdebogen, GBB), amount of everyday activity and sport activity (Freiburger Fragebogen fuer Koerperliche Aktivitaet, FFKA), and a Screening for Somatoform Disorders instrument (SOMS). ‐an ergometric test was used to establish individual aerobic fitness (aerob/anaerob threshold based on lactate measurement) and training heart rate |
| Notes | Article untraceable |
| Methods | Randomised trial |
| Participants | Turkish immigrants in a tertiary care German hospital |
| Interventions | Bioenergetic training, gymnastics, gestalt therapy, behavioural therapy, social therapy |
| Outcomes | Symptom severity, depression, anxiety, somatisation, aggressiveness and others |
| Notes |
| Methods | Clinical trial |
| Participants | People with somatisation |
| Interventions | Affective cognitive behavioural therapy versus treatment as usual |
| Outcomes | Unknown |
| Notes | Article (book chapter) ‐ untraceable |
CBT: cognitive behavioural; therapy; CGI: Clinical Global Impression Scale; MUPS: medically unexplained physical symptoms.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Treatment of Multi‐organ Bodily Distress Syndrome. A Randomized Controlled Trial of the Effects of Acceptance and Commitment Therapy Given as Group Therapy or Workshop Compared to Standard Treatment (Stress‐4) |
| Methods | Randomised controlled trial, 3‐arm parallel study |
| Participants | First‐time referred participants fulfilling diagnostic criteria for BDS multi‐organ type with symptoms for more than 3 of 4 symptom categories; moderate or severe impact on daily life; symptoms lasting for at least 2 years Aged 20‐50 years; born in Denmark or have Danish parents. The participant understands, speaks, writes and read Danish |
| Interventions | 1. Experimental: Group Therapy: ACT given as conventional group therapy in groups of 7‐8 participants 3,5 hours each session, 9 sessions during 3 month |
| Outcomes | Primary Outcome Measures:Global Clinical Improvement Scale [Time Frame: 14 month after randomisation ] [ Designated as safety issue: No ]Questionnaire, participant‐rated improvement of health since the beginning of the study |
| Starting date | January 2012, planned end date March 2015 |
| Contact information | [email protected] (Johanne Agger) |
| Notes | ClinicalTrials.gov Identifier: NCT01518647 |
| Trial name or title | A Computer‐Based Intervention for Medically Unexplained Physical Symptoms |
| Methods | Randomised controlled trial |
| Participants | Participants aged 18‐75 seeking medical care for physical symptoms (i.e., persistent fatigue, pain complaints, and gastrointestinal, cardiovascular or musculoskeletal symptoms). No major medical illness to explain symptom(s) is found after detailed physical and laboratory assessment. Participants with common disorders such as hypertension, asthma, diabetes, low back strain, etc., will be included if in the opinion of the physician the presenting physical symptoms are not due to the underlying disorder. In order to enter the study, participants must meet criteria for at least 4 medically unexplained symptoms out of the 42 somatic symptoms listed in the Composite International Diagnostic Interview (CIDI) rated as currently present if males and at least 6 symptoms if females (Escobar's abridged criteria). Participants without ready access to a computer and the Internet will be excluded from participating. Also excluded will be individuals with life threatening medical illness, communicative disorder, lack of fluency in English, illiteracy, and major psychiatric conditions including psychoses, bipolar disorder, and alcohol or drug abuse. Participants will be required to add no medications to their regimen during the study period (approximately 6 weeks) |
| Interventions | Intervention: Computer‐based exercises to be executed at home |
| Outcomes | Quick Inventory of Depressive Symptoms Positive and Negative Affect Scale Satisfaction with Life Scale |
| Starting date | 2007 |
| Contact information | |
| Notes | ClinicalTrials.gov identifier: NCT00468013 According to trial register completed in 2009. Contacted investigator (17 July 2014) |
| Trial name or title | Psychosomatic Therapy, Feasibility and Cost Analysis (PsySom) |
| Methods | Randomised pilot study consisting of participants with MUS in primary care. Participants will be followed for 1 year |
| Participants | People with MUS |
| Interventions | Participants will be randomised to intervention (usual care and additional psychosomatic therapy) or control condition (usual care alone) |
| Outcomes | Primary outcome measures are: the number of participants identified and recruited, perceived symptom severity, measured on a Visual Analogue Scale (VAS) and participants' self rated symptoms of distress, depression, anxiety and somatisation (4DSQ: The Four Dimensional Symptom Questionnaire). Other primary outcome measures are the time needed to include the eligible participants, the number of withdrawals in the intervention and control group, compliance in the therapy group and the number of participants who complete the questionnaires Secondary outcome measures are: symptoms of hyperventilation (NHL: Nijmegen Hyperventilation List), physical and mental health status and quality of life (SF‐36), and level of functioning (MAF: measure of general functioning). Participant satisfaction with the received therapy is rated on a 5‐point Likert‐type scale. Medical consumption will be measured by the Cost Diary for medical consumption |
| Starting date | April 2013 |
| Contact information | Dr T.C. olde Hartman, Radboud University, email: [email protected] |
| Notes | ClinicalTrials.gov Identifier: NCT01935258. Results expected Octiver 2014 |
| Trial name or title | Enriching Cognitive‐Behavioral Therapy With Emotion Regulation Training in Patients With Chronic Multiple Somatoform Symptoms (ENCERT): A Randomized Controlled Trial |
| Methods | Randomised controlled trial |
| Participants | Participants 18‐69 years with inclusion Criteria based on DSM‐V diagnosis "somatic symptom disorder [SSD] 300.82" |
| Interventions | ENCERT contains 1. psychoeducation (session 1), 2. relaxation techniques for coping with stress (sessions 2‐4), 3. non‐judgmental awareness of body perceptions, (sessions 5‐7), 4. modifying illness behaviour and accepting unpleasant body perceptions (sessions 8‐13), 5. attention defocusing on positive perceptions plus emotional self support (sessions 14‐15), 6. analysing interpretation processes to understand situational cues (sessions 16‐17), and 7. change of behaviour and interpretations (sessions 18‐20). The innovative elements of ENCERT are: improving the awareness for the association of somatic symptoms with emotions, learning non‐judgmental awareness and acceptance of unpleasant body perceptions, achieving high‐frequent skill exercising with the emotion regulation audio training. Comparator: CBT. This arm is based on traditional cognitive‐behavioural therapy that can be considered the current "treatment of choice", being the only intervention with an evidence grade 1a (Kroenke 2007). As such, it presents the reference of efficacy and safety for new regimen. The strictly manualised program includes the following components focusing on the special needs of people with chronic somatoform disorders: psychoeducation providing a framework for psychotherapy, attention defocusing, reduction of over‐interpretation of symptoms, increase of physical activity, stress reduction |
| Outcomes | Primary Outcome Measures:Change in somatic symptom severity (Screening for Somatoform Disorders, SOMS‐7T) from pre‐assessment to four in‐between assessments to post‐assessment to follow‐up [Time Frame: From pre‐assessment (admission) to four in‐between assessments (9, 13, 17, 21 weeks after admission) to post‐assessment (25 weeks after admission) to follow‐up (12 months after admission) ] [ Designated as safety issue: No ]Assessment of somatic symptom severity during the last 7 days (self rating) |
| Starting date | October 2013 |
| Contact information | Winfried Rief, Ph.D. riefw@uni‐marburg.de Maria Kleinstäuber [email protected]‐Marburg.de |
| Notes | ClinicalTrials.gov identifier: NCT01908855. Results expected 2016 |
| Trial name or title | How effective is a walking training for somatoform disorders? A randomized controlled study |
| Methods | Randomised controlled study |
| Participants | Participants fulfilling as primary diagnosis the criteria of 1 of the 5 somatoform disorders in the DSM‐IV focusing on multiple somatoform symptoms; participants with co‐morbid disorders are eligible; attestation on exclusion of medical causes and physical fitness by a physician; participants with acute suicidality, psychotic symptoms, and who already exercising sufficiently at the beginning of the study (due to expected ceiling effects) will be excluded |
| Interventions | Intervention: walking training based on a walking program by Bös 2006 (see Notes). Participants will be instructed by a qualified coach. The walking training comprises a weekly session of 90 minutes over 12 weeks. The program manual includes a detailed description of each training session. Every session builds on 7 sequences: 1. Introduction, 2. warming‐up, 3. walking, 4. weight and strength training/stretching, 5. relaxation, 6. exchange of experiences, 7. movement‐/health‐related information Comparator: waiting list |
| Outcomes | All of the following primary and secondary outcomes are assessed at baseline and week 12. Primary outcomes: Screening for Somatoform Disorders (SOMS‐7T; baseline, week 12); Short Form 36 Questionnaire (SF‐36) ‐ subscale Physical Health; physiological parameters (physical constitution, heart rate variability; Freiburg Questionnaire of Physical Activity Secondary outcomes: Hospital Anxiety and Depression Scale (HADS‐D); Cognitions About Body and Health (CABAH); Whiteley Index (WI); Short Form 36 Questionnaire (SF‐36) ‐ subscale Mental Health; items healthcare use developed by study authors; body mass index Weekly assessment in the walking group: Symptom Diary of the SOMS‐7T; Short Form 12 Questionnaire (SF‐12) ‐ subscales Physical and Mental Health; protocol on training frequency |
| Starting date | June 2011 |
| Contact information | Prof. Dr. Annette Schröder, University Koblenz‐Landau, Germany: Schroede@uni‐landau.de; Dr. Jens Heider, University Koblenz‐Landau, Germany: heider@uni‐landau.de |
| Notes | Provided by Maria Kleinstäuber (design paper in German) Literature: Bös K, Tiemann M, Brehm W, Mommert‐Jauch P. Walking and more ‐ reaching fitness step by step [Walking und mehr ‐ Schritt für Schritt zur Fitness] (2nd ed.). Aachen, Germany: Meyer & Meyer. 2006 |
| Trial name or title | CIPRUS ‐ Cognitive‐behavioural intervention in primary care for undifferentiated somatoform disorder |
| Methods | Randomised controlled study in general practice |
| Participants | Inclusion criteria: 2) Meeting the criteria for undifferentiated somatoform disorder according to DSM IV: a) The presence of ≥ 1 medically unexplained physical symptoms b) The symptoms last at least 6 months c) The symptoms significantly impair functioning/quality of life 1) Having a medical disorder that explains the symptoms 2) Having a severe psychiatric disorder (i.e. psychosis‐related disorders, dementia and bipolar disorder) 3) Having a handicap such as cognitive mental impairment and/or blindness 4) Being unable to speak or read Dutch |
| Interventions | Mental health nurse practitioners (MHNP) will offer intervention participants a short structured intervention based on cognitive‐behavioural (CB) principles, in addition to usual GP care, to teach participants how to cope with the consequences of their symptoms. In up to 6 sessions participants will be provided with psycho‐education, problem solving techniques, relaxation techniques, and activity scheduling. The consequences model of somatoform complaints has successfully been used in previous Dutch intervention studies and focuses on the consequences or problems that arise due to somatoform complaints and on their aggravating effects, rather than on causes of somatoform complaints. This model will be used as the treatment rationale. The focus is not so much on treating the symptoms, but rather on producing beneficial changes in (physical) functional outcome and quality of life. The MHNPs provide the CB approach of problem solving treatment (PST) as a means to learn to tackle and cope with the identified consequences. PST teaches problem‐solving styles and skills. Several steps to problem solving have been described which will be practised during the sessions: 1. explanation of treatment rationale and 'contracting', 2. identification and clarification of problems, 3. the setting of clear goals, 4. formulation of alternative solutions, 5. selection of preferred solutions, 6. clarification of the necessary steps to implement solutions, and 7. evaluation of progress. In addition, activity scheduling and progressive relaxation techniques will be provided as these are important general features of CBT for somatoform complaints. Participants in the control group will not be offered a specific additional intervention other than the care they would usually receive from the GP |
| Outcomes | The primary clinical outcome is the development in physical functioning along the total follow‐up period as measured by the physical component summary (PCS) of the RAND‐36 The primary outcome measure for the economic evaluation is quality of life as measured by the EuroQol/EQ‐5D. Direct and indirect costs will be assessed with the TIC‐P 20 and data on healthcare use extracted from the electronic medical records of the GPs. Direct costs will be based on the Dutch standard cost prices and the indirect costs will be estimated based on the average of the population Secondary outcome measures are the severity of somatisation (PHQ‐15) and depressive/anxiety symptoms (HADS) |
| Starting date | 2014 |
| Contact information | Kate Sitnikova, VUmc Amsterdam, Netherlands, email [email protected], phone +31204448032 |
| Notes | Dutch Trial Register, identifier NTR4686 |
| Trial name or title | The management of medically unexplained symptoms in primary care settings in Viet Nam: A clinical trial of cognitive behavior therapy |
| Methods | Randomised controlled trial, 3 parallel arms |
| Participants | Primary care participants 18‐65 yrs presenting with ≥ 5 or medically unexplained symptoms; participants with co‐morbid medically unexplained symptoms and depression and/or anxiety |
| Interventions | Arm 1: mood enhanced Cognitive Behaviour Therapy for medically unexplained symptoms. Arm 2: Structured Care. Both interventions are administered using once‐weekly 30‐minute sessions of one‐on‐one therapy with a primary care physician over 4 consultations with an option for 2 additional consultations. Arm 1, Cognitive Behaviour Therapy includes an initial ethnographic illness interview and then metaphor based cognitive restructuring to reduce abnormal illness behaviour, breathing retraining for anxiety symptoms, and activity scheduling for depression symptoms, with sleep hygiene instruction. Arm 2, Structured Care involves an initial ethnographic illness interview followed by time matched clinical sessions with a primary care physician without the CBT content Arm 3: Treatment as Usual will involve short primary care consultations consistent with current practice within Vietnam |
| Outcomes | Primary Outcome 1: number of reported MUS as recorded by non‐treating Primary Care Physician Primary Outcome 2: Phan Vietnamese Psychiatric Rating Scale: Somatisation Score Secondary Outcome 1: Vietnamese Psychiatric Rating Scale: Depression Score Secondary Outcome 2: Phan Vietnamese Psychiatric Rating Scale: Anxiety Score Secondary Outcome 3: Medical Outcomes Survey Short Form 12 WHO‐QOL BREF |
| Starting date | Not yet recruiting (July 2014) |
| Contact information | [email protected] (Zachary Steel) |
| Notes | Australian Trial Register Identifier ACTRN12611000946910 |
| Trial name or title | Effectiveness of a primary care based complex intervention to promote self‐management in patients presenting psychiatric symptoms: study protocol of a cluster‐randomized controlled trial |
| Methods | Cluster‐randomised controlled trial in primary care |
| Participants | 340 participants will be enrolled in the study, 170 in either arm. Inclusion criteria are: a PHQ ≥ 5 on the anxiety, depression or somatoform scale, an age of 18‐65 years old, German literacy, fully able to give consent, sufficient auditory and visual capabilities and no current psychotherapeutic treatment |
| Interventions | Intervention group: a complex, low‐threshold intervention by an Advanced Practice Nurse (APN) using a mixture of case management and counselling techniques to promote self management Control group: usual care |
| Outcomes | Primary outcome: self efficacy, measured by the General Self‐Efficacy Scale (GSE), here used as a proxy for self management Secondary outcomes: PHQ‐D symptom load and questionnaires regarding coping with illness and health related quality of life. Outcome assessments will be applied 8 weeks and 12 months after the baseline assessment |
| Starting date | 2014 |
| Contact information | [email protected]‐hamburg.de |
| Notes | Design paper: Zimmermann T, Puschmann E, Ebersbach M, Daubmann A, Steinmann S, Scherer M. Effectiveness of a primary care based complex intervention to promote self management in participants presenting psychiatric symptoms: study protocol of a cluster‐randomised controlled trial. BMC Psychiatry 2014;14:2. doi: 10.1186/1471‐244X‐14‐2 Trial registration: Clinicaltrials.gov Identifier: NCT01726387. Results expected: 2015 |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of somatic symptoms at end of treatment Show forest plot | 10 | 1081 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.53, ‐0.16] |
| Analysis 1.1  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 1 Severity of somatic symptoms at end of treatment. | ||||
| 1.1 Cognitive behavioural therapy versus usual care or waiting list | 6 | 593 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.69, ‐0.05] |
| 1.2 Behavioural therapy versus usual care or waiting list | 1 | 37 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.87, 0.43] |
| 1.3 Third‐wave cognitive behavioural therapy versus usual care or waiting list | 1 | 114 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.68, 0.06] |
| 1.4 Psychodynamic therapy versus usual care or waiting list | 1 | 252 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.64, ‐0.13] |
| 1.5 Integrative therapies versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.69, 0.40] |
| 2 Severity of somatic symptoms within 1 year after treatment Show forest plot | 7 | 950 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.37, ‐0.11] |
| Analysis 1.2  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 2 Severity of somatic symptoms within 1 year after treatment. | ||||
| 2.1 Cognitive behavioural therapy versus usual care or waiting list | 4 | 496 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.49, ‐0.09] |
| 2.2 Third‐wave cognitive behavioural therapy versus usual care or waiting list | 1 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.53, 0.23] |
| 2.3 Psychodynamic therapy versus usual care or waiting list | 1 | 262 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.44, 0.05] |
| 2.4 Integrative therapies versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.69, 0.40] |
| 3 Severity of somatic symptoms > 1 year after treatment Show forest plot | 2 | 228 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.80, ‐0.24] |
| Analysis 1.3  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 3 Severity of somatic symptoms > 1 year after treatment. | ||||
| 3.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 228 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.80, ‐0.24] |
| 4 Acceptability Show forest plot | 14 | 1644 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.99] |
| Analysis 1.4  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 4 Acceptability. | ||||
| 4.1 Cognitive behavioural therapy versus usual care or waiting list | 10 | 1037 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.85, 1.01] |
| 4.2 Behavioural therapy versus usual care or waiting list | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 0.9 [0.67, 1.21] |
| 4.3 Third‐wave cognitive behavioural therapy versus usual care or waiting list | 1 | 125 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.72, 1.00] |
| 4.4 Psychodynamic therapy versus usual care or waiting list | 1 | 328 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.88, 0.96] |
| 4.5 Integrative therapies versus usual care or waiting list | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.81, 1.39] |
| 5 Severity of anxiety symptoms at end of treatment ‐ participant rated Show forest plot | 4 | 270 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.20, 0.32] |
| Analysis 1.5  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 5 Severity of anxiety symptoms at end of treatment ‐ participant rated. | ||||
| 5.1 Cognitive behavioural therapy versus usual care or waiting list | 3 | 185 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.22, 0.37] |
| 5.2 Integrative therapies versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.53, 0.56] |
| 6 Severity of anxiety symptoms at end of treatment ‐ clinician rated Show forest plot | 3 | 320 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.63, ‐0.17] |
| Analysis 1.6  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 6 Severity of anxiety symptoms at end of treatment ‐ clinician rated. | ||||
| 6.1 Cognitive behavioural therapy versus usual care | 2 | 284 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.63, ‐0.14] |
| 6.2 Behavioural therapy versus usual care | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐1.24, 0.10] |
| 7 Severity of anxiety symptoms within 1 year after treatment ‐ participant rated Show forest plot | 2 | 134 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.22, 0.58] |
| Analysis 1.7  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 7 Severity of anxiety symptoms within 1 year after treatment ‐ participant rated. | ||||
| 7.1 Cognitive behavioural therapy versus usual care or waiting list | 1 | 49 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.59, 0.59] |
| 7.2 Integrative therapies versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [‐0.21, 0.88] |
| 8 Severity of anxiety symptoms within 1 year after treatment ‐ clinician rated Show forest plot | 2 | 251 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.15, ‐0.18] |
| Analysis 1.8  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 8 Severity of anxiety symptoms within 1 year after treatment ‐ clinician rated. | ||||
| 9 Severity of anxiety symptoms > 1 year after treatment ‐ clinician rated Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.9 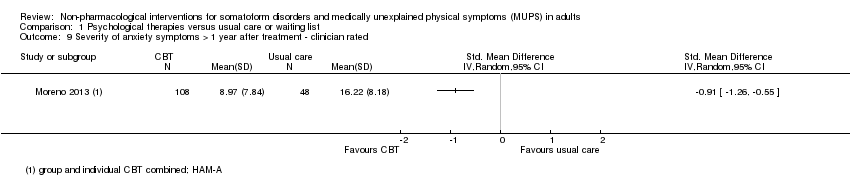 Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 9 Severity of anxiety symptoms > 1 year after treatment ‐ clinician rated. | ||||
| 10 Severity of depressive symptoms at end of treatment ‐ participant rated Show forest plot | 6 | 661 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.22, 0.16] |
| Analysis 1.10  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 10 Severity of depressive symptoms at end of treatment ‐ participant rated. | ||||
| 10.1 Cognitive behavioural therapy versus usual care or waiting list | 4 | 325 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.13, 0.31] |
| 10.2 Psychodynamic therapy versus usual care or waiting list | 1 | 251 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.55, ‐0.04] |
| 10.3 Integrative therapy versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.45, 0.64] |
| 11 Severity of depressive symptoms at end of treatment ‐ clinician rated Show forest plot | 3 | 316 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.48, ‐0.02] |
| Analysis 1.11 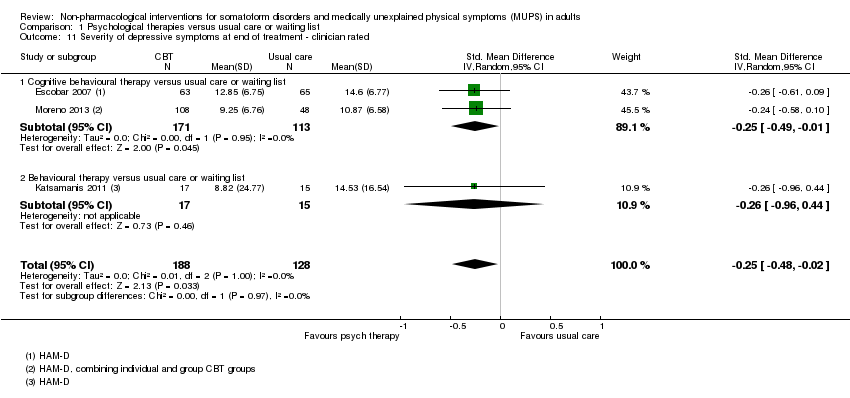 Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 11 Severity of depressive symptoms at end of treatment ‐ clinician rated. | ||||
| 11.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 284 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.49, ‐0.01] |
| 11.2 Behavioural therapy versus usual care or waiting list | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.96, 0.44] |
| 12 Severity of depressive symptoms within 1 year after treatment ‐ participant rated Show forest plot | 4 | 535 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.34, 0.42] |
| Analysis 1.12 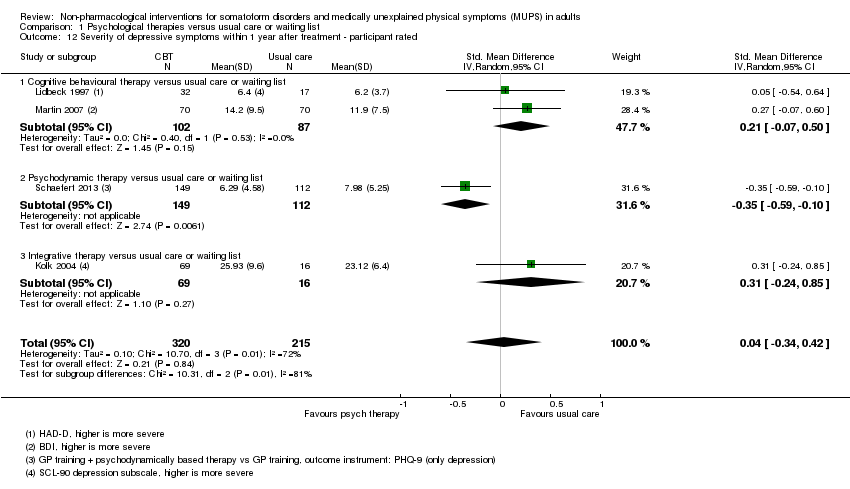 Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 12 Severity of depressive symptoms within 1 year after treatment ‐ participant rated. | ||||
| 12.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 189 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.07, 0.50] |
| 12.2 Psychodynamic therapy versus usual care or waiting list | 1 | 261 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.59, ‐0.10] |
| 12.3 Integrative therapy versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.24, 0.85] |
| 13 Severity of depressive symptoms within 1 year after treatment ‐ clinician rated Show forest plot | 2 | 251 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐1.17, 0.07] |
| Analysis 1.13  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 13 Severity of depressive symptoms within 1 year after treatment ‐ clinician rated. | ||||
| 14 Severity of depressive symptoms > 1 year after treatment ‐ clinician rated Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.14  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 14 Severity of depressive symptoms > 1 year after treatment ‐ clinician rated. | ||||
| 15 Dysfunctional cognitions, emotions and behaviours at end of treatment Show forest plot | 3 | 440 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.37, 0.16] |
| Analysis 1.15  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 15 Dysfunctional cognitions, emotions and behaviours at end of treatment. | ||||
| 15.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 189 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.73, 0.44] |
| 15.2 Psychodynamic therapy versus usual care or waiting list | 1 | 251 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.39, 0.12] |
| 16 Dysfunctional cognitions, emotions, and behaviours within 1 year after treatment Show forest plot | 3 | 451 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.38, 0.07] |
| Analysis 1.16  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 16 Dysfunctional cognitions, emotions, and behaviours within 1 year after treatment. | ||||
| 16.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 189 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.79, 0.30] |
| 16.2 Psychodynamic therapy versus usual care or waiting list | 1 | 262 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.38, 0.11] |
| 17 Adverse events Show forest plot | 3 | 445 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.47, 3.66] |
| Analysis 1.17  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 17 Adverse events. | ||||
| 18 Treatment response at end of treatment Show forest plot | 4 | 391 | Risk Ratio (M‐H, Random, 95% CI) | 3.30 [2.08, 5.21] |
| Analysis 1.18 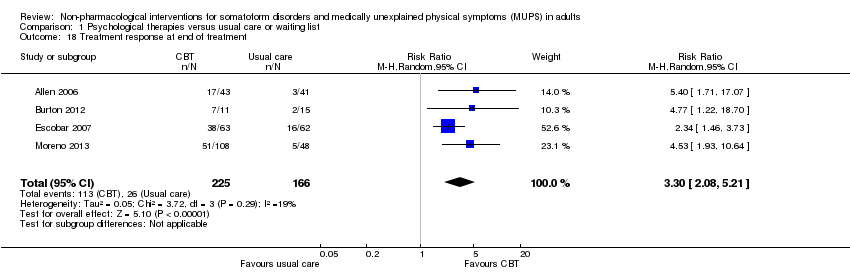 Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 18 Treatment response at end of treatment. | ||||
| 19 Treatment response within 1 year after treatment Show forest plot | 3 | 332 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.25, 5.10] |
| Analysis 1.19  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 19 Treatment response within 1 year after treatment. | ||||
| 20 Treatment response > 1 year after treatment Show forest plot | 2 | 240 | Risk Ratio (M‐H, Random, 95% CI) | 10.31 [2.95, 36.02] |
| Analysis 1.20 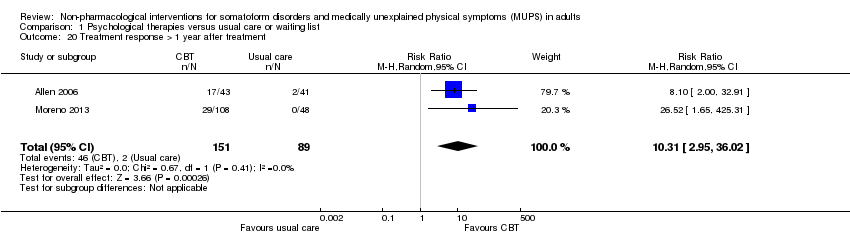 Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 20 Treatment response > 1 year after treatment. | ||||
| 21 Functional disability and quality of life at end of treatment Show forest plot | 7 | 730 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [0.03, 0.32] |
| Analysis 1.21 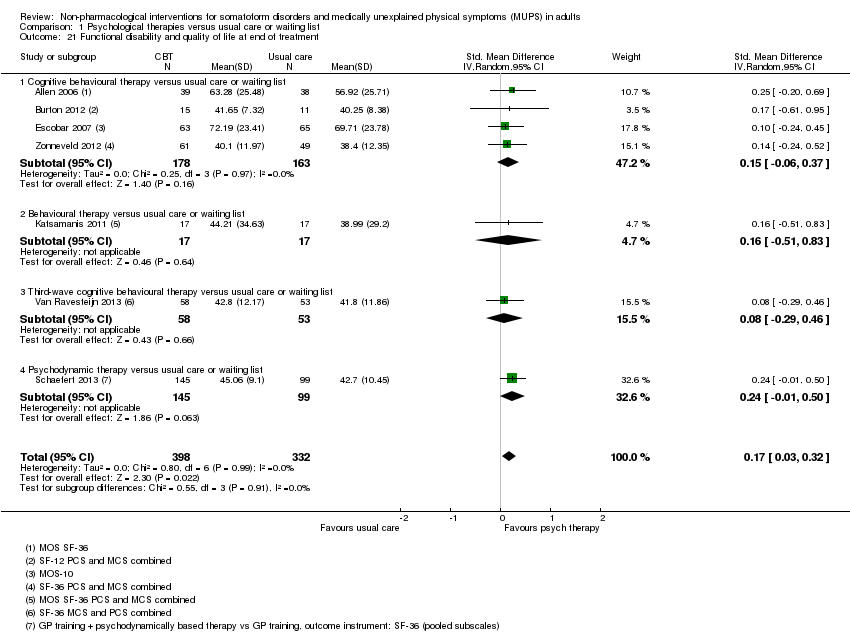 Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 21 Functional disability and quality of life at end of treatment. | ||||
| 21.1 Cognitive behavioural therapy versus usual care or waiting list | 4 | 341 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.06, 0.37] |
| 21.2 Behavioural therapy versus usual care or waiting list | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.51, 0.83] |
| 21.3 Third‐wave cognitive behavioural therapy versus usual care or waiting list | 1 | 111 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.29, 0.46] |
| 21.4 Psychodynamic therapy versus usual care or waiting list | 1 | 244 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.01, 0.50] |
| 22 Functional disability and quality of life within 1 year after treatment Show forest plot | 4 | 526 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.01, 0.33] |
| Analysis 1.22 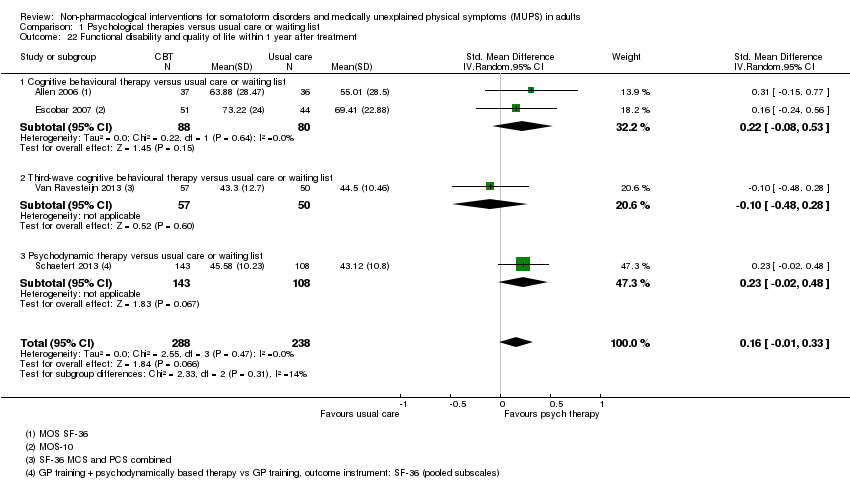 Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 22 Functional disability and quality of life within 1 year after treatment. | ||||
| 22.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 168 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.08, 0.53] |
| 22.2 Third‐wave cognitive behavioural therapy versus usual care or waiting list | 1 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.48, 0.28] |
| 22.3 Psychodynamic therapy versus usual care or waiting list | 1 | 251 | Std. Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.02, 0.48] |
| 23 Functional disability and quality of life > 1 year of treatment Show forest plot | 1 | 72 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.11, 0.82] |
| Analysis 1.23 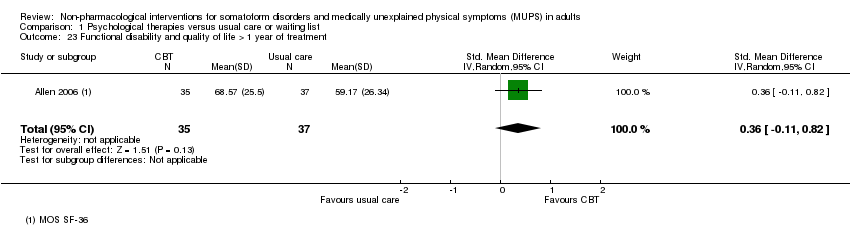 Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 23 Functional disability and quality of life > 1 year of treatment. | ||||
| 24 Healthcare use at end of treatment Show forest plot | 2 | 117 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐1.06, ‐0.30] |
| Analysis 1.24  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 24 Healthcare use at end of treatment. | ||||
| 25 Healthcare use within 1 year after treatment Show forest plot | 4 | 532 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.31, 0.12] |
| Analysis 1.25  Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 25 Healthcare use within 1 year after treatment. | ||||
| 25.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 189 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.56, 0.02] |
| 25.2 Integrative therapies versus usual care or waiting list | 1 | 81 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.44, 0.69] |
| 25.3 Psychodynamic therapy versus usual care or waiting list | 1 | 262 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.23, 0.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of somatic symptoms at end of treatment Show forest plot | 5 | 624 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.43, 0.04] |
| Analysis 2.1 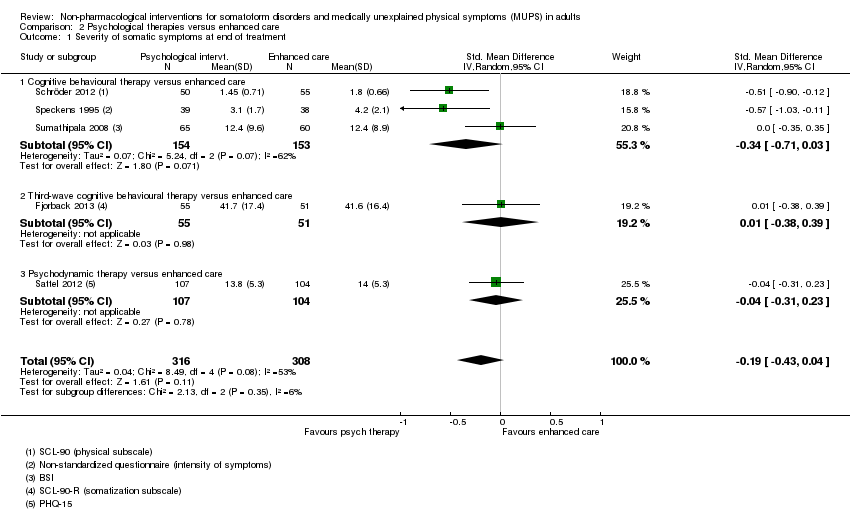 Comparison 2 Psychological therapies versus enhanced care, Outcome 1 Severity of somatic symptoms at end of treatment. | ||||
| 1.1 Cognitive behavioural therapy versus enhanced care | 3 | 307 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.71, 0.03] |
| 1.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 106 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.38, 0.39] |
| 1.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.31, 0.23] |
| 2 Severity of somatic symptoms within 1 year after treatment Show forest plot | 5 | 593 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.40, ‐0.02] |
| Analysis 2.2  Comparison 2 Psychological therapies versus enhanced care, Outcome 2 Severity of somatic symptoms within 1 year after treatment. | ||||
| 2.1 Cognitive behavioural therapy versus enhanced care | 3 | 289 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.60, ‐0.00] |
| 2.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 93 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.36, 0.46] |
| 2.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.47, 0.07] |
| 3 Severity of somatic symptoms > 1 year after treatment Show forest plot | 2 | 172 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.73, 0.10] |
| Analysis 2.3  Comparison 2 Psychological therapies versus enhanced care, Outcome 3 Severity of somatic symptoms > 1 year after treatment. | ||||
| 3.1 Cognitive behavioural therapy versus enhanced care | 1 | 82 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.98, ‐0.09] |
| 3.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.53, 0.30] |
| 4 Acceptability Show forest plot | 5 | 679 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.87, 1.00] |
| Analysis 2.4  Comparison 2 Psychological therapies versus enhanced care, Outcome 4 Acceptability. | ||||
| 4.1 Cognitive behavioural therapy versus enhanced care | 3 | 349 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.82, 1.02] |
| 4.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.82, 1.01] |
| 4.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.89, 1.14] |
| 5 Severity of anxiety or depressive symptoms (or both) at end of treatment Show forest plot | 5 | 624 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.30, 0.02] |
| Analysis 2.5 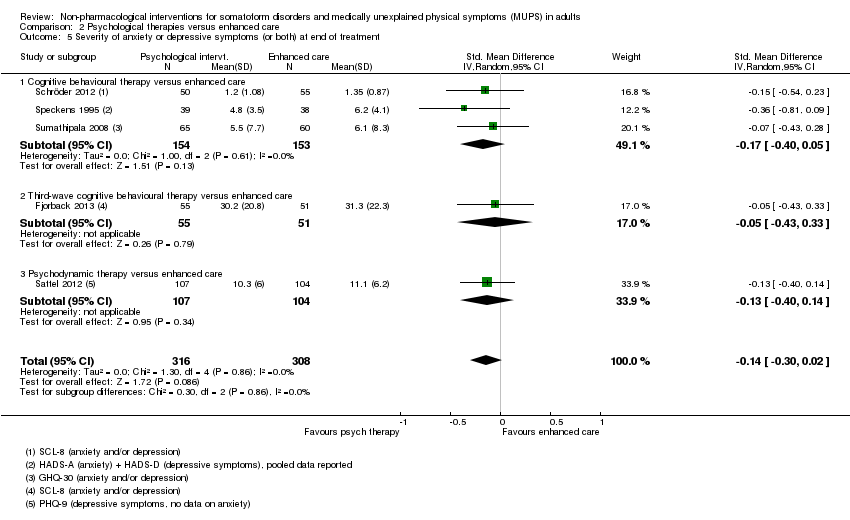 Comparison 2 Psychological therapies versus enhanced care, Outcome 5 Severity of anxiety or depressive symptoms (or both) at end of treatment. | ||||
| 5.1 Cognitive behavioural therapy versus enhanced care | 3 | 307 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.40, 0.05] |
| 5.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.43, 0.33] |
| 5.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.40, 0.14] |
| 6 Severity of anxiety or depressive symptoms (or both) within 1 year after treatment Show forest plot | 5 | 593 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.29, 0.03] |
| Analysis 2.6 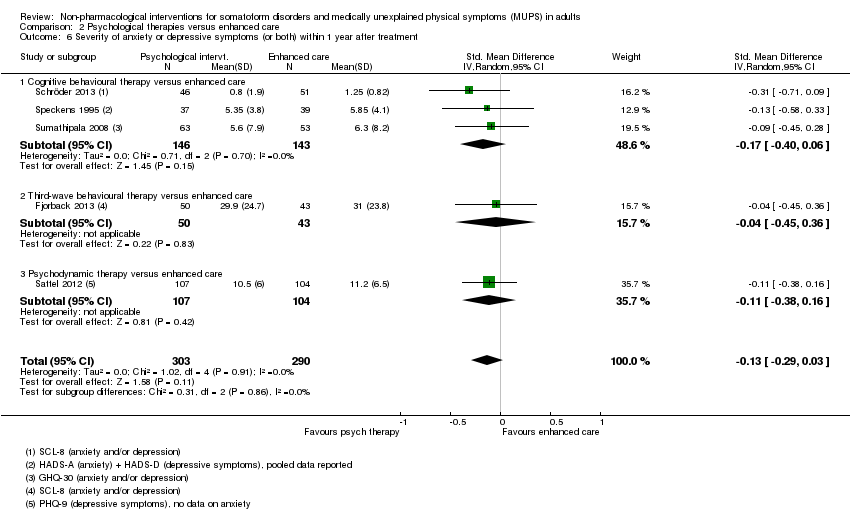 Comparison 2 Psychological therapies versus enhanced care, Outcome 6 Severity of anxiety or depressive symptoms (or both) within 1 year after treatment. | ||||
| 6.1 Cognitive behavioural therapy versus enhanced care | 3 | 289 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.40, 0.06] |
| 6.2 Third‐wave behavioural therapy versus enhanced care | 1 | 93 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.45, 0.36] |
| 6.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.38, 0.16] |
| 7 Severity of anxiety or depressive symptoms (or both) > 1 year after treatment Show forest plot | 2 | 184 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.55, 0.03] |
| Analysis 2.7  Comparison 2 Psychological therapies versus enhanced care, Outcome 7 Severity of anxiety or depressive symptoms (or both) > 1 year after treatment. | ||||
| 7.1 Cognitive behavioural therapy versus enhanced care | 1 | 94 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.77, 0.04] |
| 7.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.56, 0.26] |
| 8 Dysfunctional cognitions, emotions, and behaviours at end of treatment Show forest plot | 4 | 499 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.29, 0.10] |
| Analysis 2.8 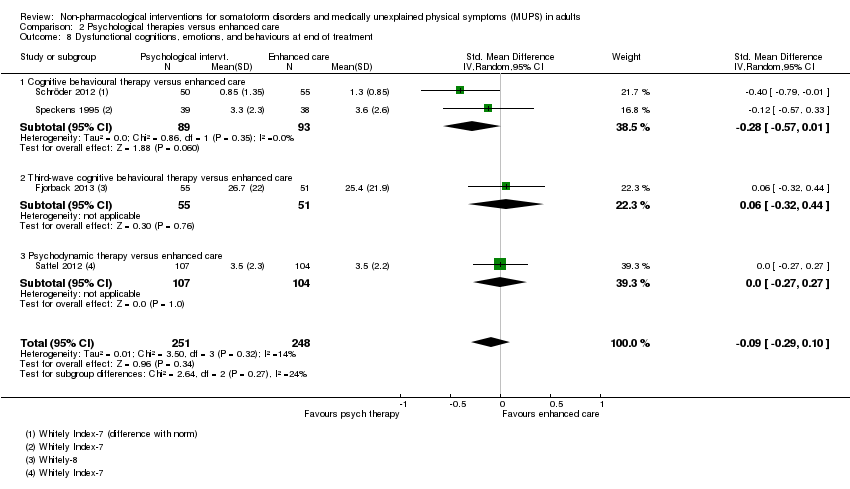 Comparison 2 Psychological therapies versus enhanced care, Outcome 8 Dysfunctional cognitions, emotions, and behaviours at end of treatment. | ||||
| 8.1 Cognitive behavioural therapy versus enhanced care | 2 | 182 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.57, 0.01] |
| 8.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 106 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.32, 0.44] |
| 8.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.27, 0.27] |
| 9 Dysfunctional cognitions, emotions, and behaviours within 1 year after treatment Show forest plot | 4 | 477 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.49, 0.00] |
| Analysis 2.9  Comparison 2 Psychological therapies versus enhanced care, Outcome 9 Dysfunctional cognitions, emotions, and behaviours within 1 year after treatment. | ||||
| 9.1 Cognitive behavioural therapy versus enhanced care | 2 | 173 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐0.83, ‐0.07] |
| 9.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 93 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.44, 0.38] |
| 9.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.40, 0.14] |
| 10 Dysfunctional cognitions, emotions, and behaviours > 1 year after treatment Show forest plot | 2 | 184 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.27, 0.11] |
| Analysis 2.10  Comparison 2 Psychological therapies versus enhanced care, Outcome 10 Dysfunctional cognitions, emotions, and behaviours > 1 year after treatment. | ||||
| 10.1 Cognitive behavioural therapy versus enhanced care | 1 | 94 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.36, ‐0.51] |
| 10.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.64, 0.19] |
| 11 Functional disability and quality of life at end of treatment Show forest plot | 4 | 497 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.05, 0.30] |
| Analysis 2.11  Comparison 2 Psychological therapies versus enhanced care, Outcome 11 Functional disability and quality of life at end of treatment. | ||||
| 11.1 Cognitive behavioural therapy versus enhanced care | 2 | 182 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.08, 0.51] |
| 11.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.31, 0.46] |
| 11.3 Psychodynamic therapy at end of treatment | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.19, 0.35] |
| 12 Functional disability and quality of life within 1 year after treatment Show forest plot | 4 | 476 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [0.02, 0.38] |
| Analysis 2.12  Comparison 2 Psychological therapies versus enhanced care, Outcome 12 Functional disability and quality of life within 1 year after treatment. | ||||
| 12.1 Cognitive behavioural therapy versus enhanced care | 2 | 173 | Std. Mean Difference (IV, Random, 95% CI) | 0.30 [0.00, 0.60] |
| 12.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 92 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.31, 0.51] |
| 12.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.11, 0.43] |
| 13 Functional disability and quality of life > 1 year of treatment Show forest plot | 2 | 184 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.16, 0.60] |
| Analysis 2.13  Comparison 2 Psychological therapies versus enhanced care, Outcome 13 Functional disability and quality of life > 1 year of treatment. | ||||
| 13.1 Cognitive behavioural therapy versus enhanced care | 1 | 94 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.01, 0.83] |
| 13.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.39, 0.44] |
| 14 Healthcare use at end of treatment Show forest plot | 2 | 334 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.33, 0.28] |
| Analysis 2.14  Comparison 2 Psychological therapies versus enhanced care, Outcome 14 Healthcare use at end of treatment. | ||||
| 14.1 Cognitive behavioural therapy versus enhanced care | 1 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.56, 0.15] |
| 14.2 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.16, 0.38] |
| 15 Healthcare use within 1 year after treatment Show forest plot | 2 | 319 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.46, ‐0.01] |
| Analysis 2.15  Comparison 2 Psychological therapies versus enhanced care, Outcome 15 Healthcare use within 1 year after treatment. | ||||
| 15.1 Cognitive behavioural therapy versus enhanced care | 1 | 108 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.46, 0.30] |
| 15.2 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.59, ‐0.05] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of somatic symptoms at end of treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 3.1 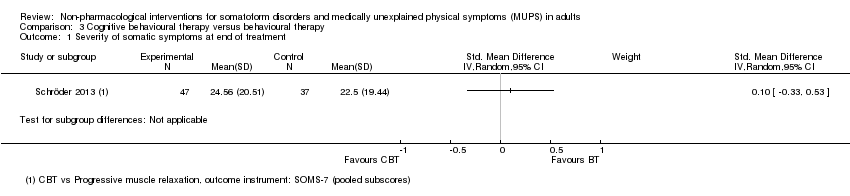 Comparison 3 Cognitive behavioural therapy versus behavioural therapy, Outcome 1 Severity of somatic symptoms at end of treatment. | ||||
| 2 Acceptability Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 3.2  Comparison 3 Cognitive behavioural therapy versus behavioural therapy, Outcome 2 Acceptability. | ||||
| 3 Severity of anxiety or depressive symptoms (or both) at end of treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 3.3  Comparison 3 Cognitive behavioural therapy versus behavioural therapy, Outcome 3 Severity of anxiety or depressive symptoms (or both) at end of treatment. | ||||
| 4 Functional disability and quality of life at end of treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 3.4  Comparison 3 Cognitive behavioural therapy versus behavioural therapy, Outcome 4 Functional disability and quality of life at end of treatment. | ||||
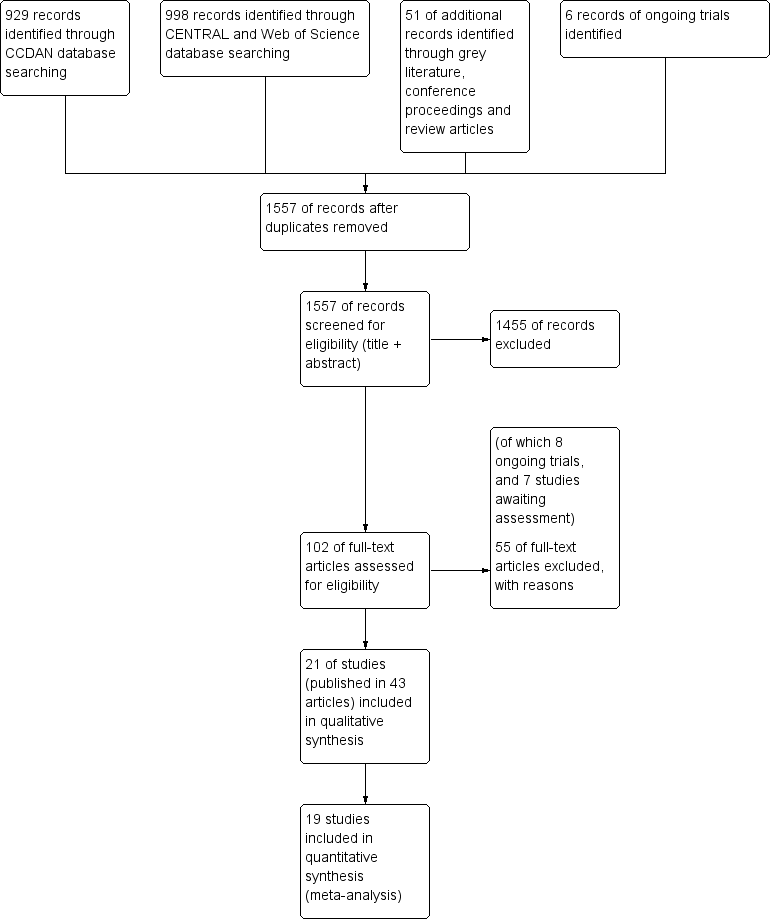
6 Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Funnel plot of comparison: 1 Psychological therapies versus usual care or waiting list, outcome: 1.4 Acceptability.
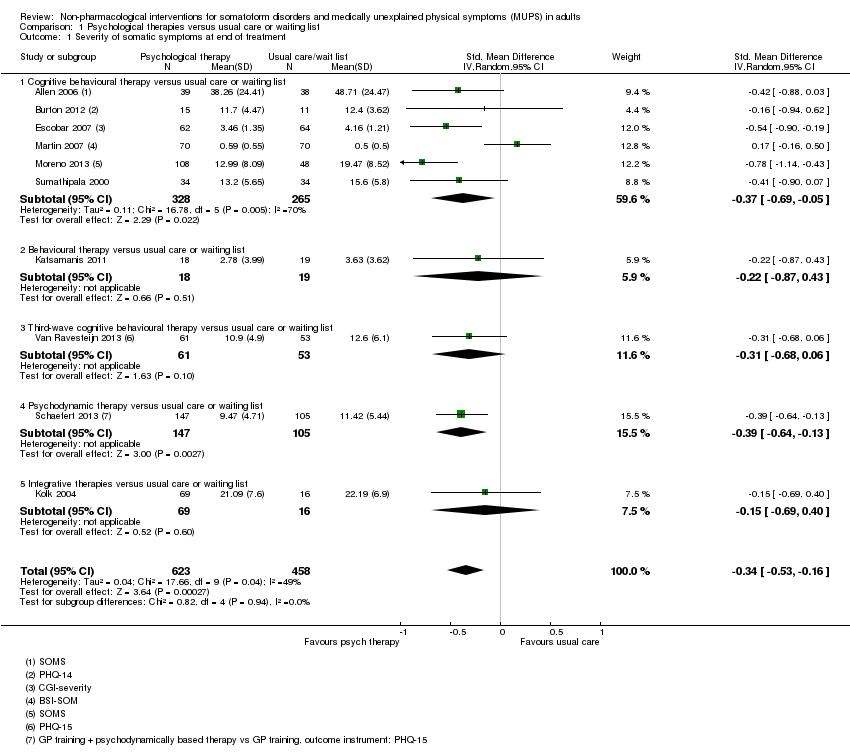
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 1 Severity of somatic symptoms at end of treatment.
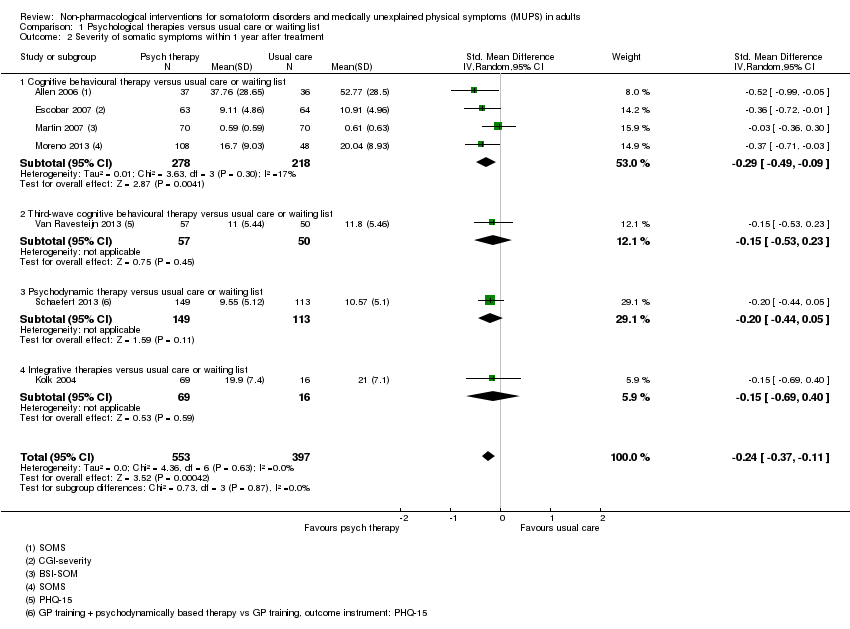
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 2 Severity of somatic symptoms within 1 year after treatment.
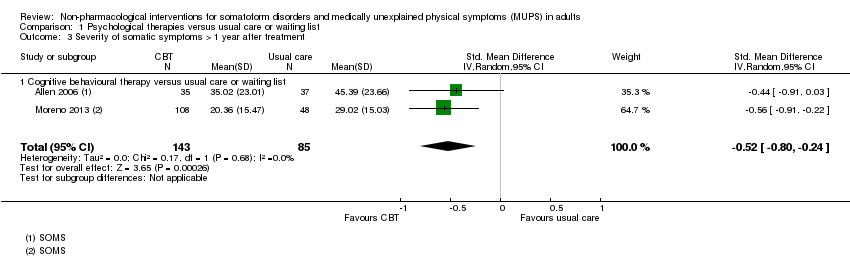
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 3 Severity of somatic symptoms > 1 year after treatment.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 4 Acceptability.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 5 Severity of anxiety symptoms at end of treatment ‐ participant rated.
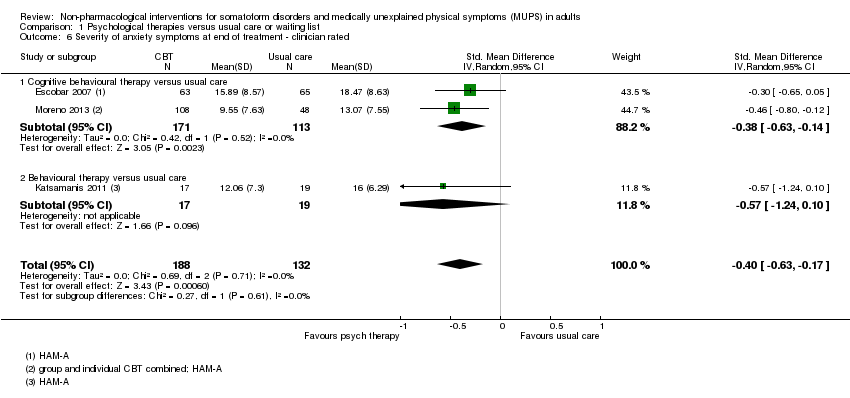
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 6 Severity of anxiety symptoms at end of treatment ‐ clinician rated.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 7 Severity of anxiety symptoms within 1 year after treatment ‐ participant rated.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 8 Severity of anxiety symptoms within 1 year after treatment ‐ clinician rated.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 9 Severity of anxiety symptoms > 1 year after treatment ‐ clinician rated.
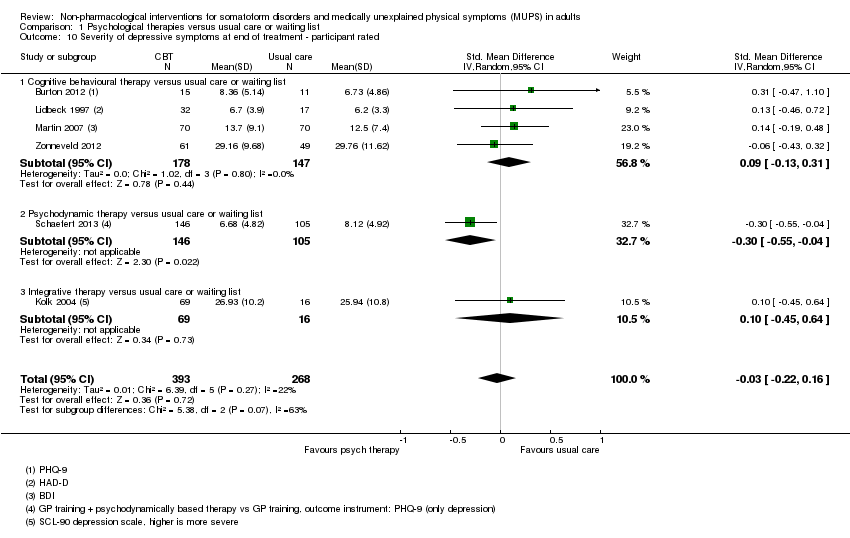
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 10 Severity of depressive symptoms at end of treatment ‐ participant rated.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 11 Severity of depressive symptoms at end of treatment ‐ clinician rated.
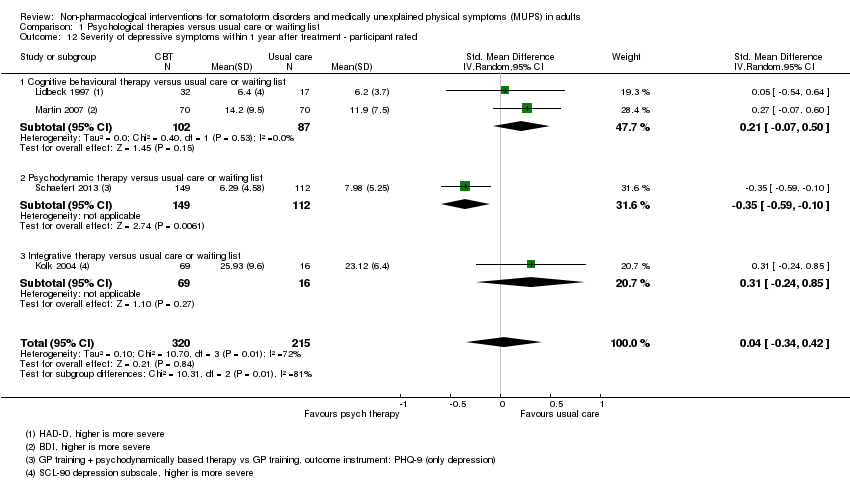
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 12 Severity of depressive symptoms within 1 year after treatment ‐ participant rated.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 13 Severity of depressive symptoms within 1 year after treatment ‐ clinician rated.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 14 Severity of depressive symptoms > 1 year after treatment ‐ clinician rated.
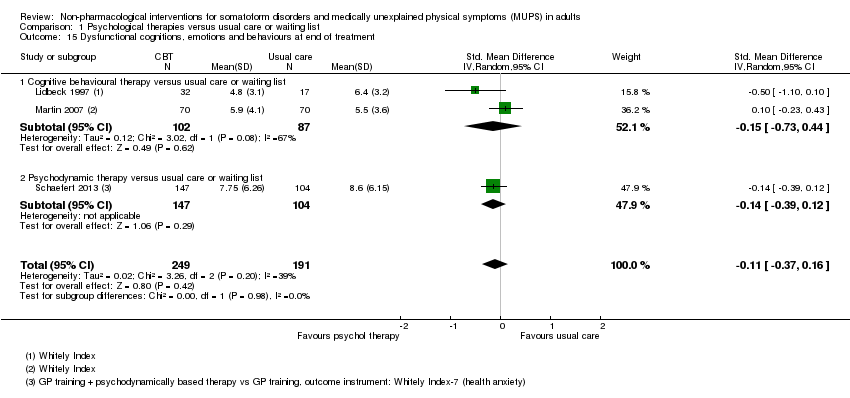
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 15 Dysfunctional cognitions, emotions and behaviours at end of treatment.
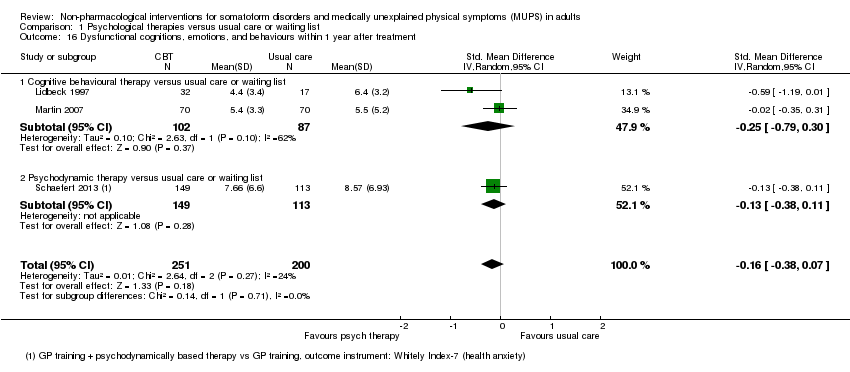
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 16 Dysfunctional cognitions, emotions, and behaviours within 1 year after treatment.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 17 Adverse events.
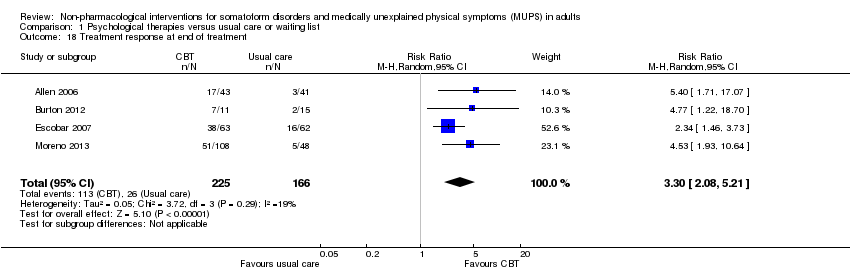
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 18 Treatment response at end of treatment.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 19 Treatment response within 1 year after treatment.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 20 Treatment response > 1 year after treatment.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 21 Functional disability and quality of life at end of treatment.
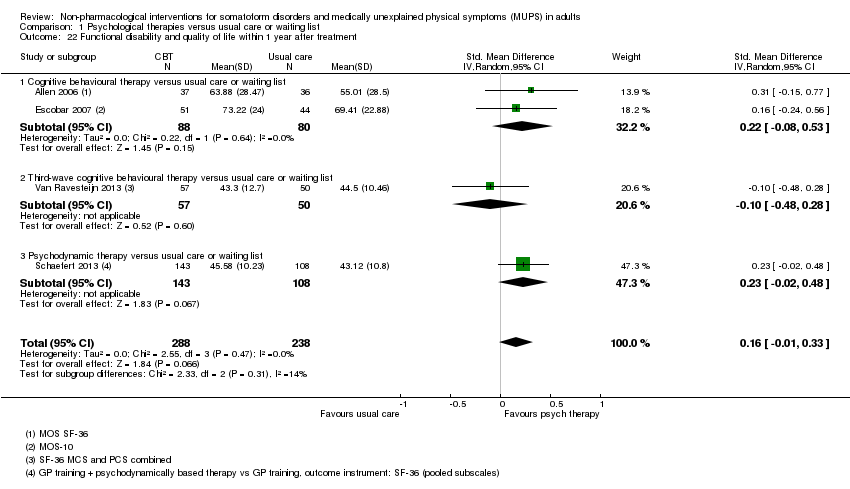
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 22 Functional disability and quality of life within 1 year after treatment.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 23 Functional disability and quality of life > 1 year of treatment.

Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 24 Healthcare use at end of treatment.
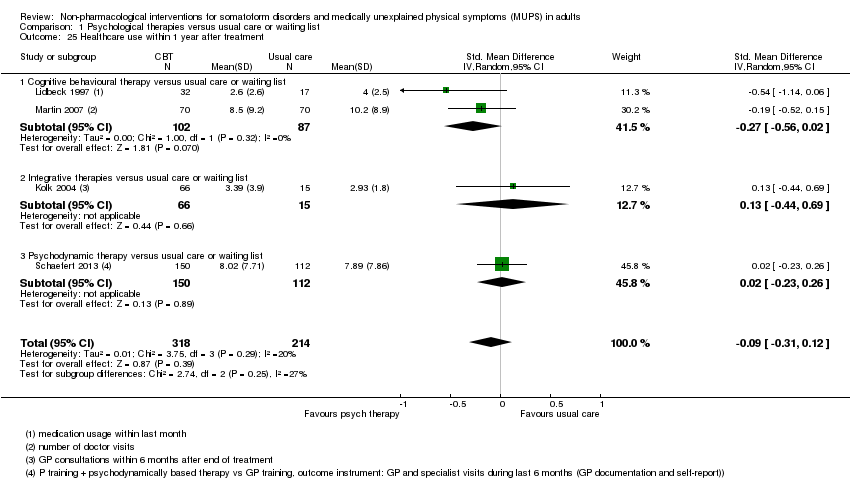
Comparison 1 Psychological therapies versus usual care or waiting list, Outcome 25 Healthcare use within 1 year after treatment.

Comparison 2 Psychological therapies versus enhanced care, Outcome 1 Severity of somatic symptoms at end of treatment.

Comparison 2 Psychological therapies versus enhanced care, Outcome 2 Severity of somatic symptoms within 1 year after treatment.

Comparison 2 Psychological therapies versus enhanced care, Outcome 3 Severity of somatic symptoms > 1 year after treatment.

Comparison 2 Psychological therapies versus enhanced care, Outcome 4 Acceptability.
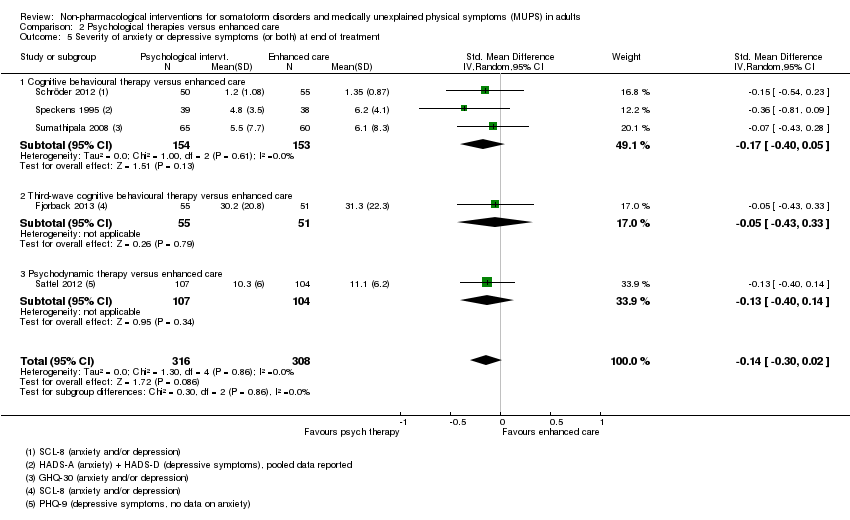
Comparison 2 Psychological therapies versus enhanced care, Outcome 5 Severity of anxiety or depressive symptoms (or both) at end of treatment.

Comparison 2 Psychological therapies versus enhanced care, Outcome 6 Severity of anxiety or depressive symptoms (or both) within 1 year after treatment.

Comparison 2 Psychological therapies versus enhanced care, Outcome 7 Severity of anxiety or depressive symptoms (or both) > 1 year after treatment.

Comparison 2 Psychological therapies versus enhanced care, Outcome 8 Dysfunctional cognitions, emotions, and behaviours at end of treatment.

Comparison 2 Psychological therapies versus enhanced care, Outcome 9 Dysfunctional cognitions, emotions, and behaviours within 1 year after treatment.

Comparison 2 Psychological therapies versus enhanced care, Outcome 10 Dysfunctional cognitions, emotions, and behaviours > 1 year after treatment.
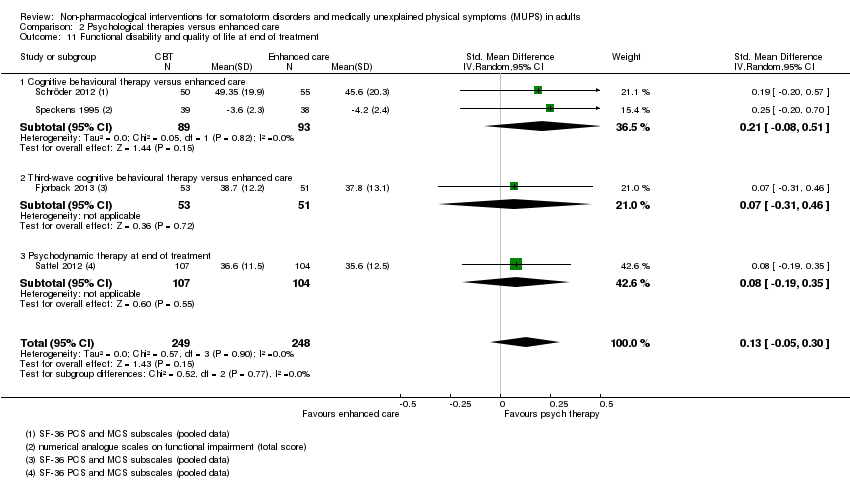
Comparison 2 Psychological therapies versus enhanced care, Outcome 11 Functional disability and quality of life at end of treatment.
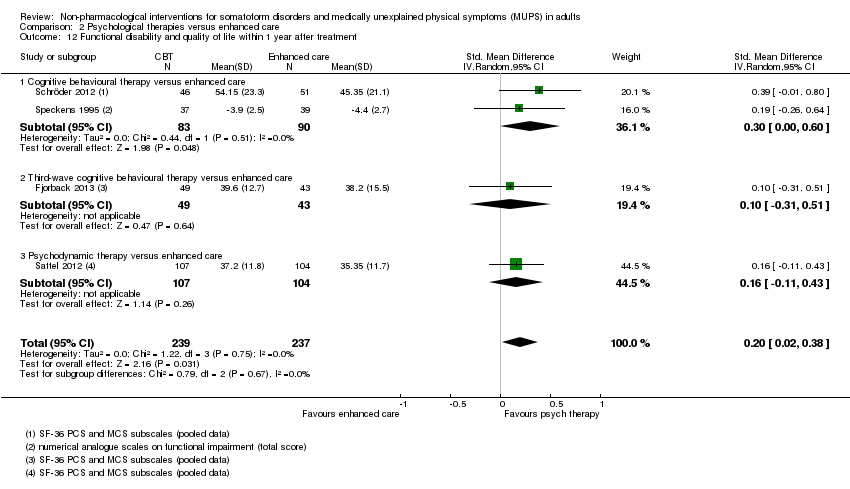
Comparison 2 Psychological therapies versus enhanced care, Outcome 12 Functional disability and quality of life within 1 year after treatment.
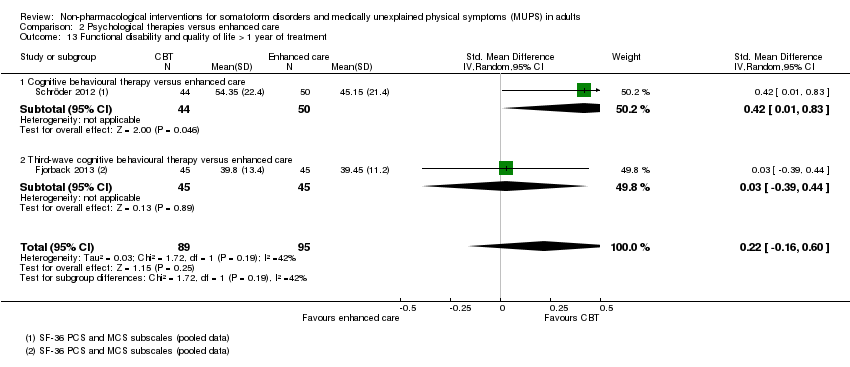
Comparison 2 Psychological therapies versus enhanced care, Outcome 13 Functional disability and quality of life > 1 year of treatment.
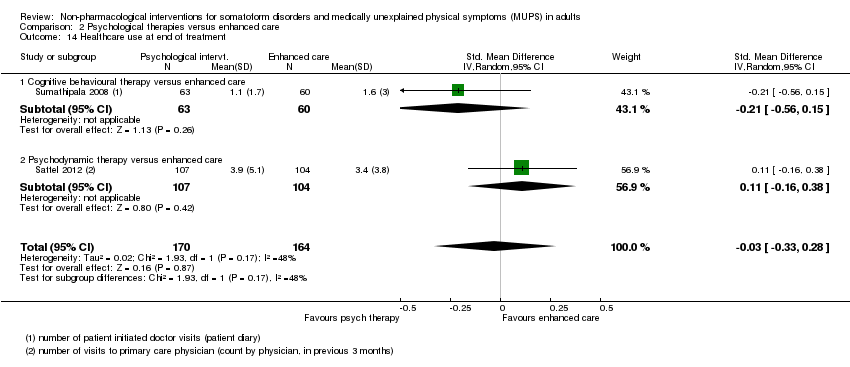
Comparison 2 Psychological therapies versus enhanced care, Outcome 14 Healthcare use at end of treatment.

Comparison 2 Psychological therapies versus enhanced care, Outcome 15 Healthcare use within 1 year after treatment.

Comparison 3 Cognitive behavioural therapy versus behavioural therapy, Outcome 1 Severity of somatic symptoms at end of treatment.
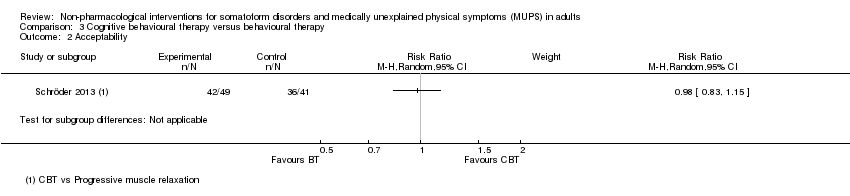
Comparison 3 Cognitive behavioural therapy versus behavioural therapy, Outcome 2 Acceptability.
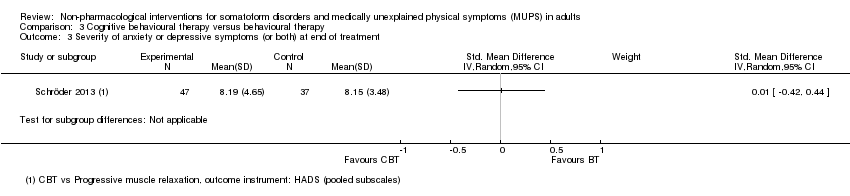
Comparison 3 Cognitive behavioural therapy versus behavioural therapy, Outcome 3 Severity of anxiety or depressive symptoms (or both) at end of treatment.

Comparison 3 Cognitive behavioural therapy versus behavioural therapy, Outcome 4 Functional disability and quality of life at end of treatment.
| Psychological therapy compared with usual care for somatoform disorders and medically unexplained physical symptoms | ||||||
| Patient or population: people with somatoform disorders and medically unexplained physical symptoms | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Usual care | Psychological therapy | |||||
| Severity of somatic symptoms at end of treatment | The mean severity of somatic symptoms at end of treatment ranged across control groups from | The mean severity of somatic symptoms at end of treatment in the intervention groups was | ‐ | 1081 | ⊕⊕⊝⊝ | A difference of 0.34 SMD was considered to be 'small to medium' |
| Acceptability | 896 per 1000 | 833 per 1000 | RR 0.93 | 1644 | ⊕⊕⊕⊝ | Excluding the outlier (see footnote) (70 participants) reduced I2 statistic from 70% to 33% |
| Dysfunctional cognitions, emotions, or behaviours (participant rated) at end of treatment | The mean dysfunctional cognitions, emotions, or behaviours (participant rated) at end of treatment in the control groups was | The mean dysfunctional cognitions, emotions, or behaviours (participant rated) at end of treatment in the intervention groups was | ‐ | 440 | ⊕⊕⊕⊝ | A difference of 0.11 SMD was considered to be 'small' |
| Treatment response at end of treatment | 157 per 1000 | 517 per 1000 | RR 3.30 | 391 | ⊕⊕⊝⊝ | ‐ |
| Functional disability/quality of life at end of treatment | ‐ | The mean functional disability/quality of life at end of treatment in the intervention groups was | ‐ | 730 | ⊕⊕⊝⊝ | A difference of 0.17 SMD was considered to be small |
| Healthcare use | ‐ | The mean healthcare use in the intervention groups was | ‐ | 532 | ⊕⊕⊕⊝ | Difference small and not statistically significant |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Measured with different instruments using different scales. | ||||||
| Patient or population: somatoform disorders and medically unexplained physical symptoms | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Enhanced or structured care | Psychological therapies | |||||
| Severity of somatic symptoms at end of treatment | ‐ | The mean severity of somatic symptoms at end of treatment in the intervention groups was | ‐ | 624 | ⊕⊕⊕⊝ | 95% CI excluded large effect (> 0.5 SMD) |
| Acceptability | 904 per 1000 | 841 per 1000 | RR 0.93 | 679 | ⊕⊕⊕⊝ | ‐ |
| Dysfunctional cognitions, emotions, or behaviours at end of treatment | ‐ | The mean dysfunctional cognitions, emotions, or behaviours at end of treatment in the intervention groups was | ‐ | 499 | ⊕⊕⊕⊝ | 95% CI excluded clinically relevant effect |
| Treatment response at end of treatment | Study population | Not estimable | 0 | See comment | No studies reported on this outcome (see text) | |
| See comment | See comment | |||||
| Moderate | ||||||
| ‐ | ‐ | |||||
| Functional disability/quality of life at end of treatment | ‐ | The mean functional disability/quality of life at end of treatment in the intervention groups was | ‐ | 497 | ⊕⊕⊕⊝ | 95% CI excluded clinically relevant effect |
| Healthcare use within 1 year after treatment | ‐ | The mean healthcare use within 1 year after treatment in the intervention groups was | ‐ | 319 | ⊕⊕⊝⊝ | ‐ |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Analysis 2.1. 11 No blinding (all studies) and >20% loss to follow up (2 studies) | ||||||
| Eligible for this review? | |||
| DSM‐IV | ICD‐10 | YES | NO |
| Somatisation disorder | Somatisation disorder | x | ‐ |
| Undifferentiated somatoform disorder (duration > 6 months) | Undifferentiated somatoform disorder (duration > 6 months) | x | ‐ |
| ‐ | Somatoform autonomic dysfunction | x | ‐ |
| Pain disorder | Persistent somatoform pain disorder | x | ‐ |
| Somatoform disorders, unspecified | Somatoform disorders unspecified | x | ‐ |
| Hypochondriasis | Hypochondriacal disorder | ‐ | x |
| ‐ | Other somatoform disorders | ‐ | x |
| Body dysmorphic disorder | Body dysmorphic disorder | ‐ | x |
| Conversion disorder | Dissociative and conversion disorders | ‐ | x |
| YES | NO | ||
| Alternative somatoform diagnoses (such as abridged somatisation disorder or multisomatoform disorder) | x | ‐ | |
| Chronic MUPS (duration ≥ 6 months) | x | ‐ | |
| Functional somatic syndromes | ‐ | x | |
| Specific functional somatic symptoms | ‐ | x | |
| DSM: Diagnostic and Statistical Manual of Mental Disorders; ICD: International Classification of Diseases. | |||
| Intervention | Group/alone | Duration | Number of sessions | Therapist | Comparison | duration of follow‐up | |
| Martin 2007 | CBT | group | once | 1 | psychologist and psychotherapeutic specialist | usual care | 6 months |
| Burton 2012 | psychological therapy in symptoms clinic | alone | 3 months | 4 | experienced specialised GP | usual care | 3 months |
| Schweickhardt 2007 | psychotherapy | alone | 2 weeks | 5 | psychotherapists | psychoeducational reading material | 6 months |
| Sumathipala 2000 | CBT | alone | 3 months | 6 | research psychiatrist | usual care | 3 months |
| Sumathipala 2008 | CBT | alone | 3 months | 6 | trained primary care physician | enhanced treatment as usual | 12 months |
| Schröder 2013 | CBT | group | 2 months | 8 | psychotherapist | progressive muscle relaxation | 6 months |
| Van Ravensteijn 2013 | mindfullness‐based cognitive therapy | group | 2 months | 8 | experienced mindfullness trainer | enhanced treatment as usual | 9 months |
| Fjorback 2013 | mindfullness | group | 3 months | 8 | experienced psychiatrist | enhanced treatment as usual | 15 months |
| Kashner 1995 | group psychological intervention + CL | group | 4 months | 8 | master level clinician | consultation letter | 12 months |
| Lidbeck 1997 | CBT | group | 3 months | 9 | trained physician | waiting list | 9 months |
| Schroder 2012 | stress intervention (psychotherapy + letter etc) | group + alone | 4 months | 9 | consultant or senior resident psychiatry | enhanced treatment as usual | 16 months |
| Katsamanis 2011 | psychophysiologic treatment + psychiatric consultation | alone | 10 weeks | 10 | psychologist or biofeedback clinician | psychiatric consultation | 10 weeks |
| Moreno 2013 | CBT + Letter (1) CBT + Letter (2) | alone (1) group (2) | 10 weeks | 10 | psychologist | usual care + letter | 12 months |
| Allen 2006 | CBT + psychiatric consultation | alone | 3 months | 10 | trained and experienced psychologist | psychiatric consultation | 15 months |
| Escobar 2007 | CBT + psychiatric consultation letter | alone | 3 months | 10 | therapist | usual care + PCL | 9 moths |
| Sattel 2012 | psychodynamic interpersonal psychotherapy | alone | 3 months | 12 | psychologist or physician with psychotherapy experience | enhanced treatment as usual | 9 months |
| Schaefert 2013 | GP training in MUPS + interpersonal psychodynamically based therapy | group | 9 months | 12 | psychosomatic specialist | GP training in MUPS | 12 months |
| Zonneveld 2012 | CBT | group | 13 weeks | 13 | psychologist | waiting list | 13 weeks |
| Schilte 2001 | disclosure intervention | alone | unclear | unclear | trained disclosure doctor | usual care | 24 months |
| Speckens 1995 | CBT | alone | 6 months | 6‐16 | trained physician and behavioural therapist | enhanced treatment as usual | 12 months |
| Kolk 2004 | psychological intervention (varied) | alone | max 6 months | max 12 | trained therapist | usual care | 12 months |
| CBT: cognitive behavioural therapy; GP: general practitioner; max: maximum; MUPS: medically unexplained physical symptoms. | |||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of somatic symptoms at end of treatment Show forest plot | 10 | 1081 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.53, ‐0.16] |
| 1.1 Cognitive behavioural therapy versus usual care or waiting list | 6 | 593 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.69, ‐0.05] |
| 1.2 Behavioural therapy versus usual care or waiting list | 1 | 37 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.87, 0.43] |
| 1.3 Third‐wave cognitive behavioural therapy versus usual care or waiting list | 1 | 114 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.68, 0.06] |
| 1.4 Psychodynamic therapy versus usual care or waiting list | 1 | 252 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.64, ‐0.13] |
| 1.5 Integrative therapies versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.69, 0.40] |
| 2 Severity of somatic symptoms within 1 year after treatment Show forest plot | 7 | 950 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.37, ‐0.11] |
| 2.1 Cognitive behavioural therapy versus usual care or waiting list | 4 | 496 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.49, ‐0.09] |
| 2.2 Third‐wave cognitive behavioural therapy versus usual care or waiting list | 1 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.53, 0.23] |
| 2.3 Psychodynamic therapy versus usual care or waiting list | 1 | 262 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.44, 0.05] |
| 2.4 Integrative therapies versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.69, 0.40] |
| 3 Severity of somatic symptoms > 1 year after treatment Show forest plot | 2 | 228 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.80, ‐0.24] |
| 3.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 228 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.80, ‐0.24] |
| 4 Acceptability Show forest plot | 14 | 1644 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.88, 0.99] |
| 4.1 Cognitive behavioural therapy versus usual care or waiting list | 10 | 1037 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.85, 1.01] |
| 4.2 Behavioural therapy versus usual care or waiting list | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 0.9 [0.67, 1.21] |
| 4.3 Third‐wave cognitive behavioural therapy versus usual care or waiting list | 1 | 125 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.72, 1.00] |
| 4.4 Psychodynamic therapy versus usual care or waiting list | 1 | 328 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.88, 0.96] |
| 4.5 Integrative therapies versus usual care or waiting list | 1 | 106 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.81, 1.39] |
| 5 Severity of anxiety symptoms at end of treatment ‐ participant rated Show forest plot | 4 | 270 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.20, 0.32] |
| 5.1 Cognitive behavioural therapy versus usual care or waiting list | 3 | 185 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.22, 0.37] |
| 5.2 Integrative therapies versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.53, 0.56] |
| 6 Severity of anxiety symptoms at end of treatment ‐ clinician rated Show forest plot | 3 | 320 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.63, ‐0.17] |
| 6.1 Cognitive behavioural therapy versus usual care | 2 | 284 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.63, ‐0.14] |
| 6.2 Behavioural therapy versus usual care | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐1.24, 0.10] |
| 7 Severity of anxiety symptoms within 1 year after treatment ‐ participant rated Show forest plot | 2 | 134 | Std. Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.22, 0.58] |
| 7.1 Cognitive behavioural therapy versus usual care or waiting list | 1 | 49 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.59, 0.59] |
| 7.2 Integrative therapies versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [‐0.21, 0.88] |
| 8 Severity of anxiety symptoms within 1 year after treatment ‐ clinician rated Show forest plot | 2 | 251 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.15, ‐0.18] |
| 9 Severity of anxiety symptoms > 1 year after treatment ‐ clinician rated Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10 Severity of depressive symptoms at end of treatment ‐ participant rated Show forest plot | 6 | 661 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.22, 0.16] |
| 10.1 Cognitive behavioural therapy versus usual care or waiting list | 4 | 325 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.13, 0.31] |
| 10.2 Psychodynamic therapy versus usual care or waiting list | 1 | 251 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.55, ‐0.04] |
| 10.3 Integrative therapy versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.45, 0.64] |
| 11 Severity of depressive symptoms at end of treatment ‐ clinician rated Show forest plot | 3 | 316 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.48, ‐0.02] |
| 11.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 284 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.49, ‐0.01] |
| 11.2 Behavioural therapy versus usual care or waiting list | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.96, 0.44] |
| 12 Severity of depressive symptoms within 1 year after treatment ‐ participant rated Show forest plot | 4 | 535 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.34, 0.42] |
| 12.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 189 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.07, 0.50] |
| 12.2 Psychodynamic therapy versus usual care or waiting list | 1 | 261 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.59, ‐0.10] |
| 12.3 Integrative therapy versus usual care or waiting list | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.24, 0.85] |
| 13 Severity of depressive symptoms within 1 year after treatment ‐ clinician rated Show forest plot | 2 | 251 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐1.17, 0.07] |
| 14 Severity of depressive symptoms > 1 year after treatment ‐ clinician rated Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15 Dysfunctional cognitions, emotions and behaviours at end of treatment Show forest plot | 3 | 440 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.37, 0.16] |
| 15.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 189 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.73, 0.44] |
| 15.2 Psychodynamic therapy versus usual care or waiting list | 1 | 251 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.39, 0.12] |
| 16 Dysfunctional cognitions, emotions, and behaviours within 1 year after treatment Show forest plot | 3 | 451 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.38, 0.07] |
| 16.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 189 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.79, 0.30] |
| 16.2 Psychodynamic therapy versus usual care or waiting list | 1 | 262 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.38, 0.11] |
| 17 Adverse events Show forest plot | 3 | 445 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.47, 3.66] |
| 18 Treatment response at end of treatment Show forest plot | 4 | 391 | Risk Ratio (M‐H, Random, 95% CI) | 3.30 [2.08, 5.21] |
| 19 Treatment response within 1 year after treatment Show forest plot | 3 | 332 | Risk Ratio (M‐H, Random, 95% CI) | 2.53 [1.25, 5.10] |
| 20 Treatment response > 1 year after treatment Show forest plot | 2 | 240 | Risk Ratio (M‐H, Random, 95% CI) | 10.31 [2.95, 36.02] |
| 21 Functional disability and quality of life at end of treatment Show forest plot | 7 | 730 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [0.03, 0.32] |
| 21.1 Cognitive behavioural therapy versus usual care or waiting list | 4 | 341 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.06, 0.37] |
| 21.2 Behavioural therapy versus usual care or waiting list | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.51, 0.83] |
| 21.3 Third‐wave cognitive behavioural therapy versus usual care or waiting list | 1 | 111 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.29, 0.46] |
| 21.4 Psychodynamic therapy versus usual care or waiting list | 1 | 244 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.01, 0.50] |
| 22 Functional disability and quality of life within 1 year after treatment Show forest plot | 4 | 526 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.01, 0.33] |
| 22.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 168 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.08, 0.53] |
| 22.2 Third‐wave cognitive behavioural therapy versus usual care or waiting list | 1 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.48, 0.28] |
| 22.3 Psychodynamic therapy versus usual care or waiting list | 1 | 251 | Std. Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.02, 0.48] |
| 23 Functional disability and quality of life > 1 year of treatment Show forest plot | 1 | 72 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [‐0.11, 0.82] |
| 24 Healthcare use at end of treatment Show forest plot | 2 | 117 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐1.06, ‐0.30] |
| 25 Healthcare use within 1 year after treatment Show forest plot | 4 | 532 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.31, 0.12] |
| 25.1 Cognitive behavioural therapy versus usual care or waiting list | 2 | 189 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.56, 0.02] |
| 25.2 Integrative therapies versus usual care or waiting list | 1 | 81 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.44, 0.69] |
| 25.3 Psychodynamic therapy versus usual care or waiting list | 1 | 262 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.23, 0.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of somatic symptoms at end of treatment Show forest plot | 5 | 624 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.43, 0.04] |
| 1.1 Cognitive behavioural therapy versus enhanced care | 3 | 307 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.71, 0.03] |
| 1.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 106 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.38, 0.39] |
| 1.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.31, 0.23] |
| 2 Severity of somatic symptoms within 1 year after treatment Show forest plot | 5 | 593 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.40, ‐0.02] |
| 2.1 Cognitive behavioural therapy versus enhanced care | 3 | 289 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.60, ‐0.00] |
| 2.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 93 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.36, 0.46] |
| 2.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.47, 0.07] |
| 3 Severity of somatic symptoms > 1 year after treatment Show forest plot | 2 | 172 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.73, 0.10] |
| 3.1 Cognitive behavioural therapy versus enhanced care | 1 | 82 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.98, ‐0.09] |
| 3.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.53, 0.30] |
| 4 Acceptability Show forest plot | 5 | 679 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.87, 1.00] |
| 4.1 Cognitive behavioural therapy versus enhanced care | 3 | 349 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.82, 1.02] |
| 4.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.82, 1.01] |
| 4.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.89, 1.14] |
| 5 Severity of anxiety or depressive symptoms (or both) at end of treatment Show forest plot | 5 | 624 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.30, 0.02] |
| 5.1 Cognitive behavioural therapy versus enhanced care | 3 | 307 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.40, 0.05] |
| 5.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.43, 0.33] |
| 5.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.40, 0.14] |
| 6 Severity of anxiety or depressive symptoms (or both) within 1 year after treatment Show forest plot | 5 | 593 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.29, 0.03] |
| 6.1 Cognitive behavioural therapy versus enhanced care | 3 | 289 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.40, 0.06] |
| 6.2 Third‐wave behavioural therapy versus enhanced care | 1 | 93 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.45, 0.36] |
| 6.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.38, 0.16] |
| 7 Severity of anxiety or depressive symptoms (or both) > 1 year after treatment Show forest plot | 2 | 184 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.55, 0.03] |
| 7.1 Cognitive behavioural therapy versus enhanced care | 1 | 94 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.77, 0.04] |
| 7.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.56, 0.26] |
| 8 Dysfunctional cognitions, emotions, and behaviours at end of treatment Show forest plot | 4 | 499 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.29, 0.10] |
| 8.1 Cognitive behavioural therapy versus enhanced care | 2 | 182 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.57, 0.01] |
| 8.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 106 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.32, 0.44] |
| 8.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.27, 0.27] |
| 9 Dysfunctional cognitions, emotions, and behaviours within 1 year after treatment Show forest plot | 4 | 477 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.49, 0.00] |
| 9.1 Cognitive behavioural therapy versus enhanced care | 2 | 173 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐0.83, ‐0.07] |
| 9.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 93 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.44, 0.38] |
| 9.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.40, 0.14] |
| 10 Dysfunctional cognitions, emotions, and behaviours > 1 year after treatment Show forest plot | 2 | 184 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.27, 0.11] |
| 10.1 Cognitive behavioural therapy versus enhanced care | 1 | 94 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.36, ‐0.51] |
| 10.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.64, 0.19] |
| 11 Functional disability and quality of life at end of treatment Show forest plot | 4 | 497 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.05, 0.30] |
| 11.1 Cognitive behavioural therapy versus enhanced care | 2 | 182 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.08, 0.51] |
| 11.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.31, 0.46] |
| 11.3 Psychodynamic therapy at end of treatment | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.19, 0.35] |
| 12 Functional disability and quality of life within 1 year after treatment Show forest plot | 4 | 476 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [0.02, 0.38] |
| 12.1 Cognitive behavioural therapy versus enhanced care | 2 | 173 | Std. Mean Difference (IV, Random, 95% CI) | 0.30 [0.00, 0.60] |
| 12.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 92 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.31, 0.51] |
| 12.3 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.11, 0.43] |
| 13 Functional disability and quality of life > 1 year of treatment Show forest plot | 2 | 184 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.16, 0.60] |
| 13.1 Cognitive behavioural therapy versus enhanced care | 1 | 94 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [0.01, 0.83] |
| 13.2 Third‐wave cognitive behavioural therapy versus enhanced care | 1 | 90 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.39, 0.44] |
| 14 Healthcare use at end of treatment Show forest plot | 2 | 334 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.33, 0.28] |
| 14.1 Cognitive behavioural therapy versus enhanced care | 1 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.56, 0.15] |
| 14.2 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.16, 0.38] |
| 15 Healthcare use within 1 year after treatment Show forest plot | 2 | 319 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.46, ‐0.01] |
| 15.1 Cognitive behavioural therapy versus enhanced care | 1 | 108 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.46, 0.30] |
| 15.2 Psychodynamic therapy versus enhanced care | 1 | 211 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.59, ‐0.05] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Severity of somatic symptoms at end of treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2 Acceptability Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3 Severity of anxiety or depressive symptoms (or both) at end of treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4 Functional disability and quality of life at end of treatment Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |

