Intervenciones para el tratamiento de la gangrena gaseosa
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Single‐centre RCT with parallel design | |
| Participants | 46 participants with crepitus around their wounds and X‐rays indicating gas between muscles in wounds were recruited. Recruitment commenced in 1980 Intervention group: 26 participants, 21 male and 5 female. Their ages ranged from 23 to 68 years, with an average age of 41 years. Duration of gas gangrene varied from 2 to 13 days, and body temperature varied from 37.8 ℃ to 40.1 ℃. According to laboratory tests, 16 participants had leukocytosis, 3 had lowered haemoglobin, 1 had high fasting glucose, 2 had an increase in blood urea nitrogen, 2 had elevated transaminase levels, and 4 an electrolyte disorder. X‐rays showed that none had fractures Control group: 20 participants, 18 male and 2 female. Their ages ranged from 16 to 72 years, with an average age of 43 years. Duration of gas gangrene varied from 2 to 15 days, and body temperature varied from 38.1 ℃ to 41.1 ℃. According to laboratory tests, 11 participants had leukocytosis, 4 had lowered haemoglobin, 3 had high fasting glucose, 4 had an increase of blood urea nitrogen, 3 had elevated transaminase levels, and 3 had an electrolyte disorder. It was unclear whether some had fractures, as no related information was explicitly reported | |
| Interventions | Intervention group: debrided with multiple incisions, all compromised tissue removed, washed with hydrogen peroxide; antibiotic treatment consisting of penicillin 2.4 g iv 4 times daily and tinidazole 0.4 g iv twice daily; traditional Chinese medicine dressing with mashed Cirsium setosum (field thistle/Herba Cirsii), Portulaca oleracea (purslane/verdolaga), and Sedum lineare (carpet sedum/needle stonecrop), 30 g of each herb; oral medication with 50ml squeezed juice of the same Chinese herbs, 20 g for each herb, 4 times daily; symptomatic treatment. Control group: the same debridement, antibiotics and symptomatic treatment as those in the intervention group, but without traditional Chinese medicine dressing or oral medication | |
| Outcomes | The only outcome reported from the study was cure rate. 'Cure' was defined as significant improvement in symptoms, signs and laboratory tests after 1 week of treatment, and limb salvage with disappearance of swelling, pain and other symptoms and after 2 to 5 weeks of treatment. 'Improved' was defined as improvement in symptoms after 1 week of treatment and limb salvage with normal signs and laboratory tests after 2 to 8 weeks of treatment. 'No improvement' was defined as no improvement or deterioration in symptoms and signs after 1 week of treatment or being transferred to other hospitals for further treatment. 'Cure rate' was defined as the proportion of patients who were cured or improved | |
| Notes | We defined cure rate as the proportion of patients being cured and re‐calculated it, using this definition, in this review. Both the results of the trial and our review are shown in Effects of interventions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Although the authors stated randomisation was used for allocation, information about the methods of random sequence generation was not available |
| Allocation concealment (selection bias) | Unclear risk | Comment: Information about allocation concealment was not available |
| Blinding of participants and personnel (performance bias) | High risk | Comment: The lack of placebo treatment for the control group probably informed participants of their treatment group |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: Information about blinding was not available |
| Incomplete outcome data (attrition bias) | Unclear risk | Comment: Participants who transferred to other hospitals were regarded as treatment failures, but it was unclear how many were transferred, and whether they were lost to follow‐up as a result of the transfer |
| Selective reporting (reporting bias) | High risk | Comment: Information about important outcomes was not available |
| Confirmed diagnosis of gas gangrene (other bias) | Unclear risk | Comment: Information about anaerobic cultures was not available |
| Comparability of baseline characteristics between groups (other bias) | Unclear risk | Comment: Although the authors stated that there were no significant differences in age and infection severity, the definition of infection severity was unclear, and information that would have permitted comparison in age and infection severity between the 2 treatment groups was not available |
| Methods | Single‐centre RCT with parallel design | |
| Participants | 44 participants with gas gangrene confirmed through anaerobic cultures were recruited. Recruitment started in 1995 Anaerobic bacteria identified included: 21 cases of Clostridium perfringens, 17 cases of Bacillus bellonesis, 8 cases of B septicus, and 7 cases of B histolyticus. Combinations of the above anaerobic bacteria and other purulent bacteria were found in 42 cases Intervention group: 21 participants, 14 male and 7 female. Their ages ranged from 12 to 43 years, and duration of gas gangrene varied from 6 hours to 1 week. Open fracture was found in 10 cases, muscle contusion in 6 cases, foreign bodies in wounds in 4 cases, and amputation in 1 case. X‐rays identified gas between muscles in wounds in 17 cases Control group: 23 participants, with 15 male and 8 female. Their ages varied from 13 to 46 years, and duration of gas gangrene varied from 8 hours to 2 weeks. Open fracture was found in 9 cases, muscle contusion in 6 cases, foreign bodies in wounds in 7 cases, and amputation in 1 case. X‐rays identified gas between muscles in wounds in 18 cases | |
| Interventions | Intervention group: topical use of hyperbaric oxygen therapy (HBOT) in combination with debridement and antibiotic treatment. The wound was placed in a therapy chamber and exposed to a high level of oxygen 3 times daily for 2 hours each time. Oxygen was pumped in at a velocity of 2 to 4 L/min, and pressure of 2.7 to 3.7kPa Control group: systemic use of hyperbaric oxygenation in combination with debridement and antibiotics treatment. A traditional method called "three days seven times" was used for the HBOT. The participants treated with this method inhaled high concentrations of oxygen 3 times on the first day after debridement, twice on the second and the third days, and once daily thereafter | |
| Outcomes | The only outcome reported in the study was cure rate. 'Cure' was defined as the disappearance of the symptoms of gas gangrene, significant decrease in purulent excreta within a wound, and formation of granulation tissue within a wound or the healing of a wound by secondary intention. 'Significant improvement' was defined as a significant improvement in symptoms of gas gangrene, reduction in the area of a wound, significant decrease in purulent excreta within a wound, and formation of granulation tissue. 'Moderate improvement' was defined as an improvement in symptoms of gas gangrene, with a clear border to the wound, and a decrease in purulent excreta within a wound. 'No improvement' was defined as no improvement in symptoms, with an unclear border to a wound, and an increase in purulent excreta within a wound. Cure rate was defined as the proportion of participants who were cured or significantly improved | |
| Notes | It was unclear how systemic HBOT was given to the control group and whether the 2 groups received the same treatments with the exception of HBOT, because further details about interventions, such as the duration and pressure of HBOT in the control group and the types of antibiotics in both groups, were not available We defined cure rate as the proportion of patients who were cured and recalculated it, using this definition, in this review. Both the results of the trial and our review are shown in Effects of interventions | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Although the authors stated that randomisation was used for allocation, information about the methods of random sequence generation was not available |
| Allocation concealment (selection bias) | Unclear risk | Comment: Information about allocation concealment was not available |
| Blinding of participants and personnel (performance bias) | High risk | Comment: Blinding seems to have been impossible because the interventions compared differed in their delivery method |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: Information about blinding was not available |
| Incomplete outcome data (attrition bias) | Low risk | Comment: All the randomized participants were included in the analysis and no information indicated that any participant was lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Comment: Information about important outcomes was not available |
| Confirmed diagnosis of gas gangrene (other bias) | Low risk | Comment: All included participants with clinical presentations of gas gangrene were swabbed and the swabs cultured to confirm infection by anaerobic bacteria. Information about the proportion of each bacterial type was presented |
| Comparability of baseline characteristics between groups (other bias) | Unclear risk | Comment: Information that would have permitted comparison of characteristics between the 2 groups at baseline was not available |
Abbreviations
HBOT: hyperbaric oxygen therapy
iv: intravascular
RCT: randomized controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Observational study | |
| Observational study | |
| Observational study | |
| Systematic review | |
| Animal study | |
| Animal study |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Immunoglobulin for necrotizing soft tissue infections: a randomised controlled trial |
| Methods | Double‐blinded phase 2 RCT with parallel design |
| Participants | Adult patients with NSTI based on surgical findings who were admitted to or planned to be admitted to the ICU at Rigshospitalet. Targeted population includes those with gas gangrene, Fournier gangrene, necrotising fasciitis and other NSTIs. |
| Interventions | Intervention group: IVIG (Privigen) plus basic treatments Control group: saline 0.9% plus basic treatments |
| Outcomes | Primary outcomes: Physical Component Summary Score of Short‐Form 36 in the sixth month after randomisation Secondary outcomes
|
| Starting date | April 2014 |
| Contact information | Principal Investigator: Professor Anders Perner; Email: [email protected] |
| Notes | The trial is ongoing and it is unclear whether or not subgroup analysis for the patients with gas gangrene will be available. |
Abbreviations
AUC: area under the curve
ICU: intensive care unit
IVIG: intravenous immunoglobulin
NSTI: necrotising soft tissue infection
RCT: randomized controlled trial
SOFA: Sequential Organ Failure Assessment
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cure rate Show forest plot | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.08 [1.00, 9.46] |
| Analysis 1.1  Comparison 1 Additional Chinese herbs versus no additional Chinese herbs, Outcome 1 Cure rate. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cure rate Show forest plot | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.25, 4.84] |
| Analysis 2.1  Comparison 2 Additional topical HBOT versus additional systemic HBOT, Outcome 1 Cure rate. | ||||

Study flow diagram
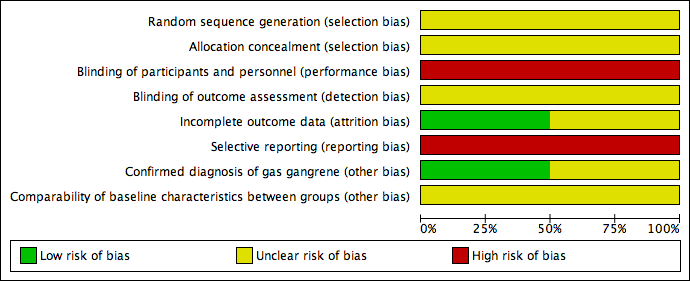
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
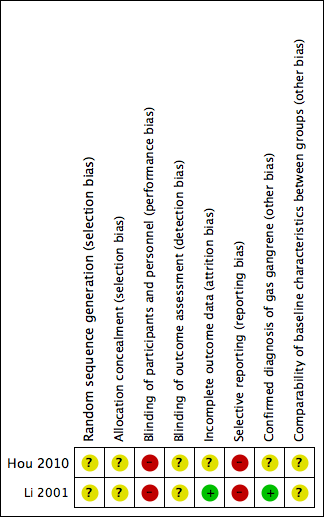
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
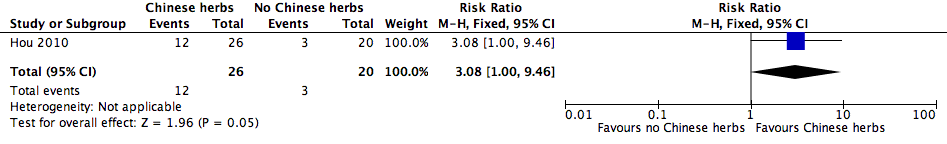
Forest plot of comparison: 1 Additional Chinese herbs versus no additional Chinese herbs, outcome: 1.1 Cure rate.

Forest plot of comparison: 2 Additional topical HBOT versus additional systemic HBOT, outcome: 2.1 Cure rate.
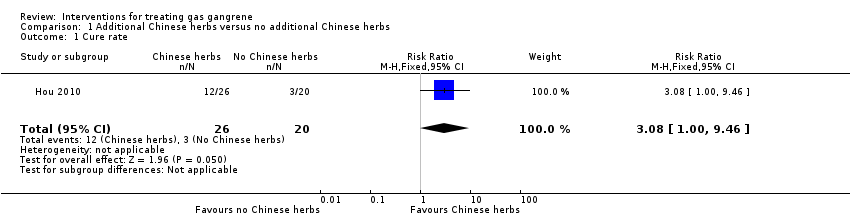
Comparison 1 Additional Chinese herbs versus no additional Chinese herbs, Outcome 1 Cure rate.
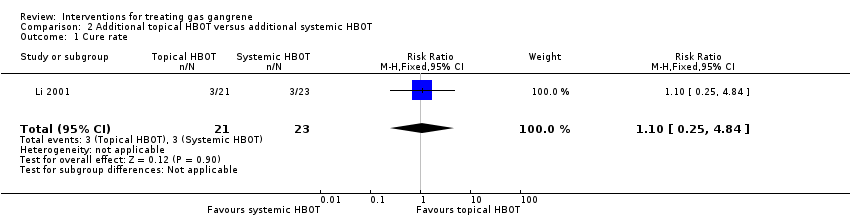
Comparison 2 Additional topical HBOT versus additional systemic HBOT, Outcome 1 Cure rate.
| Additional Chinese herbs compared with no additional Chinese herbs for treating gas gangrene | ||||||
| Patient or population: patients with gas gangrene | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no Chinese herbs | Risk with Chinese herbs | |||||
| Cure rate | Study population | RR 3.08 | 46 | ⊕⊝⊝⊝ | ||
| 150 per 1000 | 462 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to limitations in design; high risk of performance and reporting bias, and unclear risk of bias in other bias sources. 2 Downgraded two levels due to imprecision; only one trial with small sample size and very wide confidence interval that included the possibility of an effect in either direction (crosses line of no effect). | ||||||
| Additional topical HBOT compared with additional systemic HBOT for treating gas gangrene | ||||||
| Patient or population: patients with gas gangrene | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with systemic HBOT | Risk with Topical HBOT | |||||
| Cure rate | Study population | RR 1.10 | 44 | ⊕⊝⊝⊝ | ||
| 130 per 1000 | 143 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to limitations in design; high risk of performance and reporting bias, and unclear risk of bias in selection and detection bias. 2 Downgraded two levels for imprecision; only one trial with small sample size and very wide confidence interval that included the possibility of an effect in either direction (crosses line of no effect). | ||||||
| Search strategies |
| China Biological Medicine Database (CBM‐disc) |
| #1 "气性坏疽"[常用字段:智能] |
| China National Knowledge Infrastructure (CNKI) |
| (主题="气性坏疽") OR ((主题="梭菌"+"梭状") AND (主题="肌坏死"+"肌炎")) |
| Chinese scientific periodical database of VIP INFORMATION (VIP) |
| ((题名或关键词=肌坏死 或 文摘=肌坏死 或 题名或关键词=肌炎 或 文摘=肌炎 与 专业=经济管理+图书情报+教育科学+自然科学+农业科学+医药卫生+工程技术+社会科学 与 范围=全部期刊) 与 (题名或关键词=梭状 或 文摘=梭状 或 题名或关键词=梭菌 或 文摘=梭菌 与 专业=经济管理+图书情报+教育科学+自然科学+农业科学+医药卫生+工程技术+社会科学 与 范围=全部期刊)) 或者 (题名或关键词=气性坏疽 或 文摘=气性坏疽 与 专业=经济管理+图书情报+教育科学+自然科学+农业科学+医药卫生+工程技术+社会科学 与 范围=全部期刊) |
| Science Citation Index |
| Gas gangrene or clostridi* myonecrosis |
| ClinicalTrials.gov (www.clinicaltrials.gov) |
| "Gas Gangrene"(By topics) |
| Current Controlled Trials (www.controlled‐trials.com) |
| "gas gangrene" or "myonecrosis" |
| WHO International Clinical Trials Registry Platform (www.who.int/trialsearch) |
| gas gangrene or clostridi* myonecrosis or non‐clostridi* myonecrosis or nonclostridi* myonecrosis |
| Australian New Zealand Clinical Trials Registry (www.anzctr.org.au) |
| "gas gangrene" or "clostridial myonecrosis" or "non‐clostridial myonecrosis" or "nonclostridial myonecrosis" |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cure rate Show forest plot | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.08 [1.00, 9.46] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cure rate Show forest plot | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.25, 4.84] |

