Intervenciones para el tratamiento de la gangrena gaseosa
Resumen
Antecedentes
La gangrena gaseosa es una enfermedad grave y rápidamente progresiva causada por una infección bacteriana, generalmente como resultado de una lesión; tiene una elevada incidencia de amputación y un pronóstico deficiente. Requiere de diagnóstico temprano y tratamientos exhaustivos que pueden incluir desbridamiento inmediato de la herida, tratamiento con antibióticos, oxigenoterapia hiperbárica, hierbas medicinales chinas, apoyo sistémico y otras intervenciones. No se ha confirmado la eficacia y la seguridad de muchos de los tratamientos disponibles.
Objetivos
Evaluar la eficacia y la seguridad de las posibles intervenciones en el tratamiento de la gangrena gaseosa en comparación con intervenciones alternativas o ninguna intervención.
Métodos de búsqueda
En marzo 2015 se hicieron búsquedas de ensayos relevantes en: registro especializado del Grupo Cochrane de Heridas (Cochrane Wounds Group), Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL), (The Cochrane Library), Ovid MEDLINE, Ovid EMBASE, EBSCO CINAHL, Science Citation Index, la China Biological Medicine Database (CBM‐disc), la China National Knowledge Infrastructure (CNKI) y en la Chinese scientific periodical database of VIP INFORMATION (VIP). También se realizaron búsquedas de investigaciones elegibles en las listas de referencias de todos los ensayos identificados y las revisiones relevantes y en cuatro registros de ensayos. No hubo restricciones con respecto al idioma, la fecha de publicación ni el ámbito de estudio.
Criterios de selección
Se seleccionaron los ensayos controlados aleatorios (ECA) y los ensayos controlados cuasialeatorios que compararon un tratamiento para la gangrena gaseosa con otro tratamiento o con ningún tratamiento.
Obtención y análisis de los datos
De forma independiente, dos autores de la revisión seleccionaron los estudios potencialmente elegibles mediante la revisión de sus títulos, resúmenes y textos completos. Los dos autores de la revisión extrajeron los datos mediante un formulario de extracción prediseñado y evaluaron el riesgo de sesgo de cada estudio incluido. Cualquier desacuerdo en este proceso fue resuelto por el tercer autor de la revisión mediante consenso. No fue posible realizar un metanálisis debido al escaso número de estudios incluidos en la revisión y a la heterogeneidad clínica significativa entre los mismos, de manera que en su lugar se realizó una revisión narrativa.
Resultados principales
Se incluyeron dos ECA con un total de 90 participantes. Ambos ECA evaluaron el efecto de las intervenciones en la "tasa de curación" de la gangrena gaseosa; la "tasa de curación" se definió de forma diferente en cada estudio, y de forma diferente a la definida en esta revisión.
Un ensayo comparó el agregado de hierbas chinas al tratamiento estándar (desbridamiento y tratamiento con antibióticos; 26 participantes) versus tratamiento estándar solo (20 participantes). Al final del ensayo el cociente de riesgos (CR) calculado de 3,08 (intervalos de confianza [IC] del 95%: 1,00 a 9,46) favoreció a las hierbas chinas. El otro ensayo comparó el tratamiento estándar (desbridamiento y tratamiento con antibióticos) más oxigenoterapia hiperbárica (OTHB; 21 participantes) tópica con tratamiento estándar más OTHB sistémica (23 participantes). No hubo pruebas de diferencias entre los dos grupos; CR de 1,10 (IC del 95%: 0,25 a 4,84). En ambas comparaciones las pruebas fueron de calidad muy baja según la evaluación GRADE debido al riesgo de sesgo y la imprecisión, por lo que se necesitan ensayos adicionales para confirmar estos resultados.
Ningún ensayo informó los resultados primarios de esta revisión de calidad de vida, y amputación y muerte causadas por la gangrena gaseosa, ni sobre los eventos adversos. No hubo ensayos disponibles que consideraran otros tratamientos como el desbridamiento inmediato, el tratamiento con antibióticos, el apoyo sistémico y otros tratamientos posibles.
Conclusiones de los autores
El reanálisis de la tasa de curación según la definición utilizada en la revisión no mostró efectos beneficiosos del uso adicional de hierbas chinas o de OTHB tópica al tratar la gangrena gaseosa. La falta de pruebas consistentes dio lugar a que no fuese posible determinar qué intervenciones son seguras y efectivas para tratar la gangrena gaseosa. Se necesitan ECA rigurosos adicionales con asignación al azar, ocultación de la asignación y cegamiento apropiados que se centren en los tratamientos principales y los resultados clínicos más importantes, y que aporten pruebas útiles en esta área.
PICOs
Resumen en términos sencillos
Intervenciones para el tratamiento de la gangrena gaseosa
Antecedentes
La gangrena gaseosa es una infección grave e intensa que puede dar lugar a la amputación de un miembro e incluso la muerte; es una emergencia médica. Ocurre generalmente cuando se infecta una lesión causada por un traumatismo o un accidente, o como resultado de una infección posoperatoria, aunque también puede surgir sin una lesión obvia. La gangrena gaseosa es causada por bacterias (especialmente especies Clostridium), que pueden vivir y crecer en las heridas en las que hay una concentración baja de oxígeno. Las bacterias liberan toxinas que causan un daño significativo al tejido alrededor de la herida, y pueden causar un deterioro mortal en el todo cuerpo. El tratamiento exitoso de la infección requiere de un diagnóstico temprano y tratamientos efectivos.
Se utilizan diversos tratamientos para la gangrena gaseosa. Los principales son el desbridamiento (eliminación de materia muerta, sustancias extrañas y colecciones de sangre de la herida) y los antibióticos para eliminar las bacterias. Otros tratamientos que se pueden agregar a estos tratamientos fundamentales incluyen la oxigenoterapia hiperbárica (en la cual se provee oxígeno a alta presión) y las hierbas medicinales chinas, así como otras intervenciones que tratan los síntomas de la gangrena gaseosa.
Pregunta de la revisión
Se investigó qué intervenciones son efectivas y seguras para el tratamiento de la gangrena gaseosa.
Datos encontrados
En marzo 2015, se realizaron búsquedas en una amplia gama de bases de datos médicas y registros de ensayos médicos para identificar los ensayos controlados aleatorios (ECA; que producen los resultados más fiables) que compararon un tratamiento de la gangrena gaseosa con otro tratamiento, o con ningún tratamiento. Se identificaron dos ECA relevantes con 90 participantes con gangrena gaseosa.
Un ECA (46 participantes) comparó tratamiento estándar más tratamiento con hierbas chinas versus tratamiento estándar solo (desbridamiento y antibióticos). Este ECA mostró una tasa de curación mayor en el grupo de participantes tratados con hierbas chinas que en el grupo que recibió tratamiento estándar solo (21/26 versus 9/20 participantes respectivamente). La definición de "curación" utilizada en el ensayo fue la proporción de participantes que se curaron o mejoraron. Cuando se restringió la definición de "curación" a los participantes que se curaron (y se excluyeron los que "mejoraron"), la diferencia en la tasa de curación entre el grupo de hierbas chinas (12/26 participantes) y el grupo de tratamiento estándar (3/20 participantes) fue ligeramente más pequeña.
El otro ECA (44 participantes) comparó tratamiento estándar más oxigenoterapia hiperbárica (OTHB) tópica (aplicada en la superficie de la herida) versus tratamiento estándar más OTHB sistémica que se administró en todo el cuerpo. La tasa de curación fue mayor en el grupo de participantes que recibieron OTHB tópica que en el grupo que recibió OTHB sistémica (19/21 versus 11/23 participantes, respectivamente). La definición de "curación" utilizada en el ensayo fue la proporción de participantes que se curaron o mejoraron significativamente. Cuando se restringió la definición de "curación" a los participantes que se curaron (y se excluyeron los que "mejoraron significativamente"), hubo poca diferencia entre el grupo de OTHB tópica (3/21 participantes) y el grupo de OTHB sistémica (3/23 participantes).
La calidad de las pruebas para ambas comparaciones sobre el resultado de la tasa de curación fue muy baja. Ningún ensayo informó la calidad de vida, la amputación o la muerte atribuible a la gangrena gaseosa, ni los efectos perjudiciales del tratamiento. No se encontraron ensayos que investigaran otros tratamientos para la gangrena gaseosa.
Conclusiones
Aún no se conocen los efectos beneficiosos y perjudiciales de diferentes tratamientos para la gangrena gaseosa porque los ensayos disponibles no proporcionan pruebas de alta calidad, debido a los tamaños pequeños de la muestra y a varios problemas con la forma en la que se realizaron los ensayos, que pueden introducir sesgo en los resultados. Se necesitan ensayos adicionales o estudios observacionales con un diseño de estudio apropiado, que se centren en los tratamientos principales para la gangrena gaseosa y que informen sobre la calidad de vida, la amputación y la muerte causada por la gangrena gaseosa y los efectos perjudiciales que puede causar el tratamiento.
Authors' conclusions
Summary of findings
| Additional Chinese herbs compared with no additional Chinese herbs for treating gas gangrene | ||||||
| Patient or population: patients with gas gangrene | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no Chinese herbs | Risk with Chinese herbs | |||||
| Cure rate | Study population | RR 3.08 | 46 | ⊕⊝⊝⊝ | ||
| 150 per 1000 | 462 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to limitations in design; high risk of performance and reporting bias, and unclear risk of bias in other bias sources. 2 Downgraded two levels due to imprecision; only one trial with small sample size and very wide confidence interval that included the possibility of an effect in either direction (crosses line of no effect). | ||||||
| Additional topical HBOT compared with additional systemic HBOT for treating gas gangrene | ||||||
| Patient or population: patients with gas gangrene | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with systemic HBOT | Risk with Topical HBOT | |||||
| Cure rate | Study population | RR 1.10 | 44 | ⊕⊝⊝⊝ | ||
| 130 per 1000 | 143 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to limitations in design; high risk of performance and reporting bias, and unclear risk of bias in selection and detection bias. 2 Downgraded two levels for imprecision; only one trial with small sample size and very wide confidence interval that included the possibility of an effect in either direction (crosses line of no effect). | ||||||
Background
Description of the condition
Gas gangrene
Gas gangrene is an acute, severe, painful infection in which the muscles and subcutaneous tissues become filled with gas and serosanguineous exudate (i.e. blood serum that appears pink because it contains a small number of red blood cells; see Glossary Appendix 1; Anderson 2007). It is the result of infection by specific bacteria that invade muscle tissue, and produce exotoxins (potent toxins secreted by the micro‐organism; Appendix 1), particularly one called 'alpha toxin' ‐ a membrane‐disrupting toxin with phospholipase C activity ‐ that causes tissue necrosis (death; Appendix 1) and gas production (Stevens 1988). Gas gangrene is also called 'clostridial myonecrosis' because Clostridium species are the most common cause of the infection.
Pathogens and etiology
Gas gangrene can be grouped into clostridial and non‐clostridial forms, depending on the type of bacteria causing the infection.
Clostridium species are Gram‐positive, spore‐forming, anaerobic bacilli commonly found in soil, and dust, that are also found in the gastrointestinal tract, vagina and on the skin of humans (Xiao 2008). The most common subtype of Clostridium that causes clostridial gas gangrene isClostridium perfringens, previously known as C welchii. Other Clostridium species, including C novyi, C septicum, C histolyticum, C bifermentans and C fallax, are also responsible for the infection (De 2003).
Non‐clostridial species of bacteria are able to produce gas and have also been implicated in causing gas gangrene. These non‐clostridial organisms are mainly aerobic and Gram‐negative, and include Escherichia coli, Proteus species, Pseudomonas aeruginosa, Klebsiella pneumoniae, Enterococcus species, and Bacteroides species (Bessman 1975; Hart 1983; De 2003).
In most cases of gas gangrene, pathogens invade the tissues through trauma wounds, while the remainder arise spontaneously or from surgical procedures (Hart 1990). Spontaneous gas gangrene is often caused by the haematogenous spread (i.e. through the blood; Appendix 1) of C septicum, which is relatively aerotolerant (tolerates oxygen), and thus more capable of initiating infection in the absence of obvious damage to tissues. The portal of entry to the blood stream is believed to be mucosal ulceration, or, in patients with colon disease, perforation of the gastrointestinal tract (Leung 1981; Stevens 1990). The usual manifestation is a necrotising infection in an extremity or in the abdominal wall, accompanied by hypotension (low blood pressure) and renal failure (Gerding 2011). When tissue is damaged in people who have undergone trauma or had surgery, the vascular supply may be compromised, which leads to a lowering of the oxygen tension within the tissues, thus providing circumstances in which micro‐organisms multiply readily. Under conditions of low oxygen these organisms produce and release a variety of exotoxins, including lecithinase, collagenase, hyaluronidase, fibrinolysin and haemagglutinin, which can lead to local and systemic (whole body) changes in the affected patients. Alpha‐toxin, a C‐lecithinase, which is a major lethal toxin in gas gangrene, leads to necrosis and haemolysis (breakdown of blood) that can subsequently cause anaemia, jaundice and even renal failure. Other exotoxins also play an important role in destroying and liquefying healthy tissue, and in the rapid spread of infection (Hart 1990).
Epidemiology
Historically, gas gangrene has been a complication of battlefield injuries. The incidence associated with war wounds was 5% in World War I, 0.7% in World War II, 0.2% in the Korean War, and 0.02% in the Vietnam War (Bartlett 2007). These days battlefield gas gangrene is not a major cause for concern (Titball 2005), but in civilian practice, gas gangrene remains a considerable risk due to lack of prevention of the infection, an absence of standard treatment away from the battlefield environment, and an increasing prevalence in elderly people and people with diabetes (Brown 1974; Titball 2005). The estimated number of cases in the USA is about 1000 per year (Gerding 2011). Injuries resulting from earthquake may suddenly increase the number of people suffering from gas gangrene (Pu 2008; Wang 2010). Several cases of gas gangrene have been also reported in injecting drug users in Scotland (McGuigan 2002), and patients undergoing liposuction in Germany (Lehnhardt 2008).
Traumatic injuries account for about 50% of civilian cases of gas gangrene, with vehicular accidents accounting for the majority (about 70%); the remaining cases develop in people after crush injuries, industrial accidents, gunshot wounds, and burns. Postoperative complications account for about 30% of cases, and are most frequently associated with surgery on the appendix, biliary tract, or intestine. Approximately 20% are spontaneous and associated with an occult (apparently symptom‐free, so 'hidden', and not known about) colonic malignancy (Bartlett 2007; Gerding 2011).
Gas gangrene carries a high fatality rate that ranges from 25% in those with trauma, to nearly 100% in those who do not receive treatment (Melville 2006; Gerding 2011). Inadequate treatment, advanced age, location of the infection on the trunk, severe underlying diseases, and shock are factors that increase the risk of a poor prognosis with gas gangrene (Gerding 2011). There is no indication from current studies that gender or race differences have an effect on the prognosis.
Diagnosis
Early diagnosis is the most crucial part of successful management of gas gangrene.
A diagnosis of gas gangrene can be suspected, until proven otherwise, when the following features are present: history of prior trauma or surgery, muscle swelling, severe pain, oedema (swelling due to accumulation of fluid), wound discolouration, watery discharge, haemorrhagic bullae (elevated blisters, usually exceeding 5 mm in diameter, filled with blood; Appendix 1), malodour (unpleasant smell; Appendix 1) and crepitus (a crackling sound; Appendix 1; Altemeier 1971; Hart 1990). A Gram‐stain of wound exudate is considered to be the most rapid means of confirming the suspected diagnosis (Hart 1990). Diagnosis should also involve histopathologic examination of the lesion for myonecrosis (necrotic damage) without polymorphonuclear leukocytes (a type of white blood cell), and imaging methods that find gas in the tissue (Gerding 2011). Anaerobic (oxygen‐free) cultures should be taken when the wound is debrided (trimmed of dead material; Appendix 1) to confirm the identity of the pathogens, but treatment should be initiated before the findings are available, because it usually takes 48 to 72 hours for Clostridium species to grow in culture media and a 24‐hour delay in treatment can be fatal to patients with gas gangrene (Altemeier 1971; Hart 1990). Spontaneous gas gangrene with the culture of C septicum should be carefully investigated, as it may have metastasised from the site of a gastrointestinal malignancy (Hart 1990).
Description of the intervention
Treating gas gangrene involves complex interventions encompassing immediate debridement, antibiotic treatment, hyperbaric oxygen therapy (HBOT) and systemic support treatment (Schwartz 1978; Stevens 2005). A combination of these interventions is necessary (Hart 1990; Brook 2008; Chen 2011). In addition, Chinese herbal medicine is sometimes used as an adjunct treatment (Zhao 2004; Liu 2011).
How the intervention might work
Immediate debridement
Surgical debridement is considered to be the cornerstone of treatment for gas gangrene. Once gas gangrene is suspected, an aggressive debridement of all tissues involved should be carried out immediately for early diagnosis and treatment (Schwartz 1978; Brook 2008; Chen 2011). Early surgical intervention with multiple incisions and fasciotomy (incisions that are left open to relieve underlying pressure in the tissues) involves the removal of all compromised tissue, foreign material and haematoma (collections of blood) to allow decompression and drainage (Brook 2008). Leaving the wounds wide open is necessary for aeration (oxygenation; Hart 1990).
While myositis (inflammation of muscle; Appendix 1) is still relatively localised, radical decompression of the fascial compartments involved (by free longitudinal incisions and excisions of the infected muscle) usually arrests the process, and eliminates the need for amputation in order to conserve a functional limb. Without timely debridement, gas gangrene may progress to the extremities, which may result in amputation (Altemeier 1971; Brook 2008). Though amputation does not apply to gas gangrene of the trunk, which has a much poorer prognosis, the aggressive debridement of compromised skin, muscle and fascia in that area is still necessary (Morgan 1971).
Antibiotic treatment
Antibiotics are as important in the treatment of gas gangrene as surgical debridement (Hart 1983).
Studies in animals have shown that prompt treatment with antibiotics can significantly improve survival rates (Marrie 1981; Stevens 1987a). Several types of antibiotics, including penicillin, clindamycin, rifampin, metronidazole, chloramphenicol, tetracycline, and erythromycin have been shown to be effective in vitro or in animal studies (Stevens 1987a; Stevens 1987b; Oda 2008). These antibiotics provide a diverse array of mechanisms of action, including inhibition of: cell wall synthesis (penicillin), protein synthesis (chloramphenicol, tetracycline, and clindamycin), RNA synthesis (rifampin), electron transport (metronidazole; Stevens 1987b), and release of the induced toxin (erythromycin; Oda 2008).
Historically in humans, penicillin G has been recommended in doses of between 10 and 24 million units per day (Holland 1975; Laflin 1976; Hart 1983). Currently, a combination of penicillin and clindamycin is widely used for treating clostridial gas gangrene (Stevens 2005). The rationale for using penicillin in combination with clindamycin is that some strains of Clostridium are resistant to clindamycin but susceptible to penicillin. Clindamycin is thought to be the superior drug for reducing toxin formation (Gerding 2011). In clinical practice, other antibiotics commonly used with penicillin G for treating gas gangrene include ceftriaxone and erythromycin (Headley 2003).
Other, non‐clostridial bacteria are frequently found in gas gangrene tissue cultures, so treatment that is active against Gram‐positive (e.g. penicillin or cephalosporin), Gram‐negative (e.g. aminoglycoside, cephalosporin, or ciprofloxacin), and anaerobic organisms (e.g. clindamycin or metronidazole) should be combined in the antibiotic therapy until the results of bacteriological culture are known (Folstad 2004; Trott 2005).
Additional therapy
Hyperbaric oxygen therapy (HBOT)
HBOT is the medical use of oxygen at a pressure higher than atmospheric pressure. It produces a significant increase in the partial pressure of oxygen in body tissues, which suppresses the growth of anaerobic bacteria (Hart 1983). Another important role of HBOT is to relieve the hypoxic (oxygen‐poor) environment of surrounding ischaemic tissue, which limits the extent of necrosis (Hart 1990). Evidence derived from in vitro experiments and animal models indicated that HBOT can enhance survival, and exert a direct bactericidal effect on most Clostridium species by inhibiting alpha‐toxin production (Kaye 1967; Demello 1973; Hart 1983; Hirn 1993; Stevens 1993). HBOT has even been recommended before initial debridement on the basis of experimental evidence and the results of favourable clinical experience (Holland 1975).
The recommended pressure used in HBOT ranges from 2 to 3 atmospheres absolute pressure (ATA), and the exposure time ranges from 90 minutes, with 100% oxygen, to between five and 12 hours with periodic air breaks (Hart 1990). Clinical and experimental evidence has suggested that patients treated with 3 ATA for 90 minutes benefit from more conservative surgery and less extensive amputation, and that treatment with this regimen may be preferred (Tibbles 1996). Patients may tolerate exposure to oxygen pressures of up to 3 ATA for a maximum duration of 120 minutes (Tibbles 1996).
The recommendation, however, seems to lack sufficient supporting clinical evidence. A systematic review that evaluated the efficacy of HBOT for treating hypoxic wounds concluded that the therapeutic effect of HBOT is still unclear due to an absence of high‐quality trials (Wang 2003). As well as having questionable efficacy, HBOT may increase the risk of some adverse events including oxygen toxicity, barotrauma (damage caused by pressure differences between air spaces and fluids within the body; Appendix 1), decompression sickness, and pulmonary damage, most of which, however, seem to be reversible and self‐limiting (Hart 1990; Tibbles 1996).
Chinese herbal medicine
Results from case series suggest oral and topical (surface) use of Chinese herbs accompanied with debridement and antibiotic therapy may reduce fatalities caused by gas gangrene (Zhao 2004; Liu 2011). Typically, Chinese herbal medicine consists of complex prescriptions of a combination of several herbal components. The mechanism of action of the herbal medicines is reported to involve haemostasis (prevention of bleeding), detumescence (subsidence of swelling; Appendix 1) and antibacterial activity (Hou 2010).
Systemic support treatment
Supportive measures are an essential part of the treatment for gas gangrene, and include careful medical management and prompt therapy for complications of clostridial bacteraemia (bacteria in the blood; Appendix 1; Schwartz 1978).
Management of gas gangrene frequently involves volume expansion (of the blood) within the patient, with the addition of intravenous fluid, plasma and blood. A high level of calories, protein and vitamins should be also administered (Xiao 2008). Shock is a frequent complication of gas gangrene, and rapid volume expansion may be required to deal with it. Monitoring central venous pressure (Appendix 1) or pulmonary capillary wedge pressure (Appendix 1) may be valuable in severely ill patients. Additionally, careful monitoring of electrolytes and packed cell volume (of blood; Appendix 1) may also be necessary (Schwartz 1978; Hart 1990).
Other treatments
Hydrogen peroxide or potassium permanganate solution (both are antiseptic and oxidizing agents; Appendix 1) can be used to clean the wound site repeatedly, which may help to disinfect and improve the hypoxic condition (Chen 2011; Hu 2015).
Animal studies have shown that ozone (oxygen molecules with three atoms, rather than the normal two), which inactivates most bacterial species, may have some effect on treating gas gangrene (Rotter 1974; Stanek 1976).
Antitoxins, which are antibodies with the ability to neutralise a specific toxin, have been used to alleviate the poisoning symptoms, but the use of these is not recommended because of the risk of increasing hypersensitivity (undesirable reactions caused by the immune system; Appendix 1; Schwartz 1978).
Why it is important to do this review
Gas gangrene is a severe infection with a high fatality rate. Although it occurs less frequently than other wound infections, when it does occur, delay in diagnosis and treatment, or inadequate deployment of interventions may result in amputation, permanent disability or even death. Resolute and effective measures are needed to ensure favourable prognoses in people with gas gangrene. This review is intended to summarize current evidence of the efficacy and safety of possible interventions for treating gas gangrene, and to highlight gaps in the relevant research.
Objectives
To evaluate the efficacy and safety of potential interventions in the treatment of gas gangrene compared with alternative interventions or no interventions.
Methods
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (RCTs) in which people, rather than limbs or wounds, were randomly allocated into different treatments. We also considered quasi‐randomised controlled trials (qRCTs), a study design that is considered secondary to RCTs in terms of the evaluation of efficacy. We excluded any other types of study.
Types of participants
Eligible studies in the review involved patients with gas gangrene irrespective of age, gender, etiology and severity. A diagnosis of gas gangrene depended on a history of serious trauma or surgery, with clinical presentation including wounds with unusual swelling and pain, and symptoms of systemic poisoning. We considered anaerobic bacterial culture and tissue biopsy as the gold standard for diagnosis. We accepted different authors' definitions of gas gangrene, but considered them critically.
Types of interventions
In this review, we considered all types of interventions for the treatment of gas gangrene. Interventions of interest included (but were not limited to) surgical debridement, antibiotic treatment, HBOT, Chinese herbal medicine, systemic support therapy, wound irrigation, ozone and antitoxin therapy. We included studies that compared one regimen or treatment with another regimen, or treatment with no treatment. We did not consider studies in which an individual might receive different comparative treatments to different limbs or wounds simultaneously.
Types of outcome measures
We analyzed end of treatment outcomes.
Primary outcomes
-
Amputation due to gas gangrene.
-
Infection‐related fatality attributed to gas gangrene.
-
Quality of life: measured by a standardised generic questionnaire such as EQ‐5D, SF‐36, or SF‐6, or SF‐12.
Secondary outcomes
-
All‐cause fatality.
-
Cure rate in a specified period of time. Cure was defined as disappearance of both clinical presentations and abnormal laboratory findings. Cure rate was defined as the proportion of patients being cured.
-
Time to complete healing during the trial period (at a patient level).
-
Severe adverse events or complications including, but not limited to: anaphylaxis (allergic reaction that may cause death), liver injury, gastrointestinal symptoms (caused by antibiotics), oxygen toxicity, barotrauma, decompression sickness, pulmonary damage (caused by HBOT), shock, renal failure and multiple organ dysfunction syndrome.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases to identify reports of relevant clinical trials:
-
The Cochrane Wounds Group Specialized Register (searched 25 March 2015);
-
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2015, Issue 2);
-
Ovid MEDLINE (1946 to 24 March 2015);
-
Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations) (24 March 2015);
-
Ovid EMBASE (1974 to 24 March 2015);
-
EBSCO CINAHL (1982 to 25 March 2015);
-
Science Citation Index (1981 to March 2015);
-
China Biological Medicine Database (CBM‐disc; 1979 to March 2015);
-
China National Knowledge Infrastructure (CNKI; 1979 to March 2015);
-
Chinese scientific periodical database of VIP INFORMATION (VIP; 1989 to March 2015).
We used the following search strategy in The Cochrane Central Register of Controlled Trials (CENTRAL):
#1 MeSH descriptor Gas Gangrene explode all trees
#2 gas* NEXT gangrene:ti,ab,kw
#3 clostridi* NEXT myonecrosis:ti,ab,kw
#4 ((nonclostridi* OR non‐clostridi*) NEXT myonecrosis):ti,ab,kw
#5 (#1 OR #2 OR #3 OR #4)
The search strategies for Ovid MEDLINE, Ovid EMBASE and EBSCO CINAHL can be found in Appendix 2. We combined the Ovid MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (2008 revision) (Lefebvre 2011). We combined the EMBASE search with the Ovid EMBASE trial filter terms developed by the UK Cochrane Centre (Lefebvre 2011). We combined the CINAHL search with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN 2015). Search strategies for the three databases of publications in Chinese are listed in Table 1.There were no restrictions with respect to language, date of publication or study setting.
| Search strategies |
| China Biological Medicine Database (CBM‐disc) |
| #1 "气性坏疽"[常用字段:智能] |
| China National Knowledge Infrastructure (CNKI) |
| (主题="气性坏疽") OR ((主题="梭菌"+"梭状") AND (主题="肌坏死"+"肌炎")) |
| Chinese scientific periodical database of VIP INFORMATION (VIP) |
| ((题名或关键词=肌坏死 或 文摘=肌坏死 或 题名或关键词=肌炎 或 文摘=肌炎 与 专业=经济管理+图书情报+教育科学+自然科学+农业科学+医药卫生+工程技术+社会科学 与 范围=全部期刊) 与 (题名或关键词=梭状 或 文摘=梭状 或 题名或关键词=梭菌 或 文摘=梭菌 与 专业=经济管理+图书情报+教育科学+自然科学+农业科学+医药卫生+工程技术+社会科学 与 范围=全部期刊)) 或者 (题名或关键词=气性坏疽 或 文摘=气性坏疽 与 专业=经济管理+图书情报+教育科学+自然科学+农业科学+医药卫生+工程技术+社会科学 与 范围=全部期刊) |
| Science Citation Index |
| Gas gangrene or clostridi* myonecrosis |
| ClinicalTrials.gov (www.clinicaltrials.gov) |
| "Gas Gangrene"(By topics) |
| Current Controlled Trials (www.controlled‐trials.com) |
| "gas gangrene" or "myonecrosis" |
| WHO International Clinical Trials Registry Platform (www.who.int/trialsearch) |
| gas gangrene or clostridi* myonecrosis or non‐clostridi* myonecrosis or nonclostridi* myonecrosis |
| Australian New Zealand Clinical Trials Registry (www.anzctr.org.au) |
| "gas gangrene" or "clostridial myonecrosis" or "non‐clostridial myonecrosis" or "nonclostridial myonecrosis" |
We also searched the following clinical trials registries:
-
ClinicalTrials.gov (www.clinicaltrials.gov);
-
Current Controlled Trials (http://www.controlled‐trials.com/);
-
WHO International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/);
-
Australian New Zealand Clinical Trials Registry (http://www.anzctr.org.au/).
The search strategies for the above registries are listed in Table 1.
Searching other resources
We tried to identify additional studies by searching the reference lists of all relevant trials and reviews we identified.
Data collection and analysis
Selection of studies
Independently, two review authors (ZY, JH) selected trials that met the inclusion criteria from all references retrieved by the search. Any disagreements were resolved by discussion between the authors, with adjudication by the third review author (YQ).
Data extraction and management
Two review authors (ZY, YQ) independently extracted the details of study population (age, gender, setting, severity, pathogen), characteristics of the study, nature of the interventions and outcomes, using a pre designed data extraction form. We tried to contact the authors of the original studies to obtain more information in the case of missing or unclear data. With differences in data extraction identified, we referred back to the original articles and discussed the differences. Any disagreements were resolved by discussion with a third author (JH) and through consensus.
Assessment of risk of bias in included studies
Two review authors (ZY, YQ) performed methodological quality assessments independently, using the Cochrane tool for assessing risk of bias (Higgins 2011). We resolved any disagreement through discussion with a third review author (SZ).
The Cochrane tool for assessing risk of bias includes seven specific domains, namely:
-
random sequence generation;
-
allocation concealment;
-
blinding of participants and personnel;
-
blinding of outcome assessment;
-
incomplete outcome data;
-
selective outcome reporting;
-
other sources of bias, which were divided into two aspects in our review: confirmed diagnosis of gas gangrene, and comparability of baseline characteristics between groups.
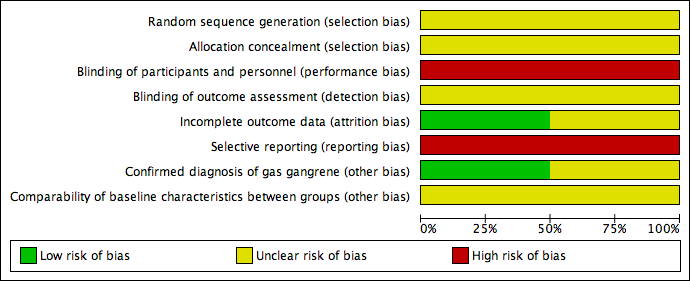
Each criterion was judged as being: 'low' (meaning low risk of bias), 'high' (high risk of bias) or 'unclear' (lack of information or uncertainty about the risk of bias). We present our assessment of risk of bias in a 'Risk of bias' summary figure that displays the quality of all included studies.
Measures of treatment effect
We intended to report quantitative data from individual trials for outcomes listed in the inclusion criteria using risk ratios (RR) for dichotomous outcomes, standardised mean differences (SMD) for continuous outcomes (e.g. quality of life), and hazard ratios (HR) for time‐to‐event outcomes (e.g. time to healing), all with 95% confidence intervals (CI), where appropriate.
Unit of analysis issues
The unit of analysis for all outcomes in our review was the individual rather than a limb or a wound. Where the limb or the wound was used as the unit of analysis in studies, we planned to contact the authors to establish whether an individual received only one treatment. If so, we would have asked for the data at individual level; otherwise, we would have excluded these studies.
Dealing with missing data
We tried to contact the authors of the included trials to obtain missing data, but did not receive a response. For time‐to‐event outcomes, if the authors did not report HR and 95% CI in the primary studies, we planned to ask them to provide the summary results or individual patient data. If missing data could not be obtained from the study authors, our plan was to analyse the data that were available, and then to perform sensitivity analyses where we assumed the worst outcome for participants lost to follow‐up.
Assessment of heterogeneity
We assessed studies for clinical heterogeneity by checking the inclusion criteria, exclusion criteria, differences in the interventions and in the definition and measurement of outcomes. We also assessed methodological heterogeneity by examining the risk of bias of all included trials. In addition, we planned to calculate the Q statistic and I² values to quantify statistical heterogeneity. We planned to interpret I² values of more than 50%, or a P value of less than 0.10, as representing substantial heterogeneity.
Assessment of reporting biases
If sufficient studies had been available, we would have assessed publication bias for primary outcomes by means of a funnel plot. Evidence of asymmetry in funnel plots would have indicated possible publication bias.
Data synthesis
We intended to conduct a head‐to‐head comparison across trials using the statistical package within the Cochrane review‐writing software, Review Manager (RevMan; RevMan 2014). We would have expressed results as RR with 95% CI for dichotomous outcome measures; SMD with 95% CI for continuous outcomes such as quality of life, where different assessment scales may be used in different studies; and HR with 95% CI for time‐to‐event outcomes. We planned to use a fixed‐effect model unless there was evidence of heterogeneity (I² over 25%) that suggested that a random‐effects model would be more appropriate. For time‐to‐event data, we planned to use the inverse variance method on the estimated HR and standard error. If there had been high statistical heterogeneity (I² over 50%), we would not have pooled the results, but presented them in a narrative format.
However, because of the small number of included studies and substantial clinical heterogeneity between them, we did not implement the above plan.
Subgroup analysis and investigation of heterogeneity
In the presence of sufficient studies, we would have conducted analyses separately to study the difference in results for the following groups:
-
etiologies: post‐traumatic, postoperative and spontaneous;
-
location of gas gangrene: extremity versus trunk;
-
patient age: children (aged between 0 and 18 years) compared with adults (over 18 years).
Sensitivity analysis
In the presence of a sufficient number of studies, we would also have performed a sensitivity analysis to investigate whether, and how, results might have been affected by studies with missing data or without adequate allocation concealment, blinding, or a clearly specified definition of gas gangrene, by excluding them from the analyses.
Results
Description of studies
Results of the search
The total of 2481 citations identified through our searches included 1600 unique references from the electronic databases, seven unique records from the trial registries and 874 duplicate records, which we removed. Checking the remaining titles and abstracts allowed us to exclude a further 1599 irrelevant records, leaving us with eight references for full‐text assessment. We excluded five references for the reasons outlined in Characteristics of excluded studies. We included two trials and detailed their characteristics in Characteristics of included studies. There is an ongoing trial (NCT02111161), the full text of which requires further assessment for eligibility. Details of the information available for this trial and the reason for it awaiting classification are listed in Characteristics of ongoing studies. The selection flow is shown in Figure 1.

Study flow diagram
Included studies
Two single‐centre RCTs with parallel design met our inclusion criteria for types of studies, participants, and interventions completely (Hou 2010; Li 2001; Characteristics of included studies). Cure rate, which we had defined as a secondary outcome in our review, was the only primary outcome used in both trials. We included the trials since they provided the most relevant evidence available on the topic.
The first trial started in 1980 and was conducted in a general hospital with 400 beds and 1.6 million outpatients per year (Hou 2010). The trialists randomized 46 patients with crepitus around their wounds and X‐rays indicating gas between the muscles in wounds into two groups. Both groups received identical debridement, antibiotics and symptomatic treatments, but the intervention group also received Chinese herbal medicine for dressing and oral use. The herbal medicine was prepared locally with Cirsium setosum (field thistle/Herba Cirsii), Portulaca oleracea (purslane/verdolaga), and Sedum lineare (carpet sedum/needle stonecrop). Information about who prepared and administered the herbal medicine was not available. Treatment duration ranged from two to eight weeks without blinding. Cure rate was the only outcome analyzed in the trial, and was defined as significant improvement in symptoms, signs and laboratory results after one week of treatment, and disappearance of swelling, pain and other symptoms, normal laboratory results, and no amputation after two to five weeks of treatment. Improvement of participants was defined as improvement in symptoms after one week of treatment and normal signs, normal laboratory results and no amputation after two to eight weeks of treatment. Failure was defined as no improvement, or deterioration in symptoms or signs after one week of treatment, or transfer to another hospital for further treatment. Cure rate was defined as the proportion of patients who were cured or improved.
The second trial was also conducted in a general hospital with 520 beds and 0.2 million outpatients per year (Li 2001). The trial started in 1995. All 44 participants had a confirmed diagnosis of gas gangrene through anaerobic cultures, 47.7% (21/44) of whom were infected with Clostridium perfringens. Participants in the two groups received debridement and antibiotic treatment, as well as topical or systemic HBOT. Participants were followed up for 10 days. Again, cure rate was the only outcome analyzed in the trial. Cure was defined as disappearance of both the symptoms and purulent excreta within a wound, and formation of granulation tissue or healing by secondary intention. Significant improvement was defined as a significant improvement in symptoms of gas gangrene, reduction in the area of the wound, a significant decrease in purulent excreta within the wound, and formation of granulation tissue. Moderate improvement was defined as improvement in symptoms of gas gangrene, with a clear border to the wound, and a decrease in purulent excreta within the wound. Failure was defined as no improvement in symptoms, with an unclear border to the wound, and no reduction in purulent excreta within the wound. Cure rate was defined as the proportion of participants who were cured or significantly improved.
However, both definitions of cure rate used in these trials differed from that specified in our review (Secondary outcomes).
Excluded studies
We excluded two animal studies (Zhang 1988; Rao 1994), three observational studies (Mou 1985; Luo 1987; Ma 2008), and one systematic review (Raman 2006; Characteristics of excluded studies).
Risk of bias in included studies
Summaries of the risk of bias are shown in Figure 2 and Figure 3.
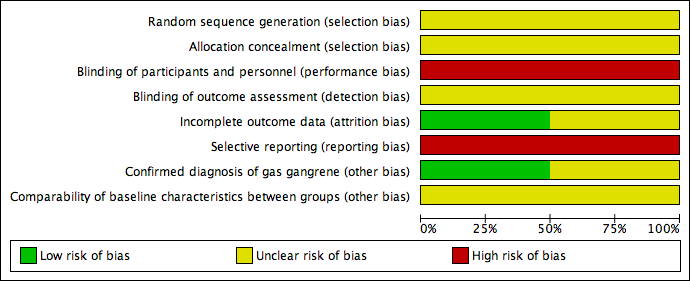
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Both included studies stated that they used a method of randomisation, but neither study detailed the methods of random sequence generation or allocation concealment employed (Li 2001; Hou 2010), so selection bias may exist.
Blinding
Although blinding methods were not specified in either trial (Li 2001; Hou 2010), it seemed impossible to have blinded both the participants and personnel to the allocated treatments. Since placebo was not given to the control group, the participants in Hou 2010 were likely to know whether they received Chinese herbs. As the procedures for delivering topical and systemic HBOT are different, the participants in Li 2001 could also have identified the treatment they received. The personnel in both studies would also be aware of the interventions assigned to the participants. As a result, performance bias seems inevitable.
No information about whether the outcome assessors were aware of grouping information before the measurement of participants' outcomes was available from either trial. Consequently, detection bias may exist.
Incomplete outcome data
Both studies included all randomly allocated participants in their analysis (Li 2001; Hou 2010). The Hou 2010 study may have been subject to attrition bias, because of those participants who transferred to other hospitals, for whom actual outcomes were unavailable other than having been defined by the study authors as failing to improve. There was insufficient information to judge whether the number of transfers were balanced across the two groups. If attrition occurred in different proportions across the groups, this would introduce attrition bias.
Selective reporting
The outcome of cure rate analyzed in both studies was a composite outcome, consisting of several components such as amputation and symptom improvement (Li 2001; Hou 2010). However, the number of amputations or symptom improvements were not specified, which indicates selective reporting bias.
Other potential sources of bias
Two aspects were considered for other sources of bias: misdiagnosis of gas gangrene and imbalance of baseline characteristics between groups. The Hou 2010 study did not provide results of anaerobic cultures or details of comparisons of baseline characteristics between groups. We could not confirm whether the trial was subjected to either bias. The Li 2001 study confirmed diagnosis of gas gangrene for all the participants through anaerobic culture, but did not report results about the comparison of some important between‐group characteristics at baseline.
Effects of interventions
See: Summary of findings for the main comparison Summary of findings. Additional Chinese herbs compared with no additional Chinese herbs for treating gas gangrene; Summary of findings 2 Summary of findings. Additional topical HBOT compared with additional systemic HBOT for treating gas gangrene
We identified two trials that we included in the review. One assessed the efficacy of adjunctive use of Chinese herbs (Hou 2010), and the other the adjunctive use of topical versus systemic HBOT in the treatment of gas gangrene (Li 2001). We did not identify trials that investigated other interventions. See: summary of findings Table for the main comparison and summary of findings Table 2. For both trials the GRADE assessment was very low quality evidence due to risk of bias and imprecision.
Chinese herbal medicine
Primary outcomes
The Hou 2010 study did not assess any of the primary outcomes defined in our review.
Secondary outcomes
Cure rate at the end of the Hou 2010 study was the only outcome reported. In the group treated with Chinese herbs (26 participants), 12 were cured, 9 were improved and 5 were not improved. The cure rate defined in the trial for this group was 80.8% (21/26), but if the rate was recalculated according to that defined in our review the rate was 46.2% (12/26). In comparison, in the group that did not receive treatment with Chinese herbs (20 participants), three were cured, six were improved and 11 were not improved. The cure rate defined in the trial was 45.0% (9/20), but if the rate was recalculated according to the definition used in this review (Secondary outcomes) it was reduced to 15.0% (3/20). According to the calculation in the trial and our review, the RRs were 1.79 (95% CI 1.07 to 3.02) and 3.08 (95% CI 1.00 to 9.46; Figure 4), respectively, and favoured adjunctive Chinese herbal medicine.
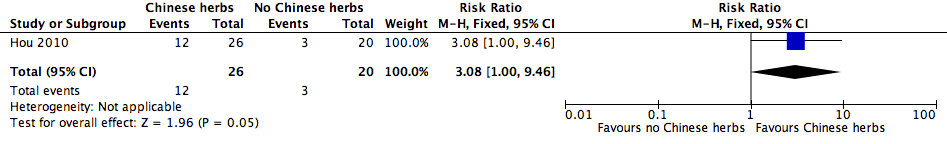
Forest plot of comparison: 1 Additional Chinese herbs versus no additional Chinese herbs, outcome: 1.1 Cure rate.
Topical HBOT
Primary outcomes
The Li 2001 study did not assess any of the primary outcomes defined in our review.
Secondary outcomes
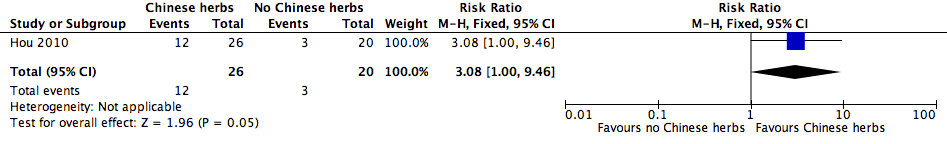
Cure rate after 10 days of treatment was the only outcome reported from the Li 2001 study. In the topical HBOT group (21 participants) 3 participants were cured, 16 were significantly improved and 2 were moderately improved, with a defined cure rate of 90.5% (19/21). By comparison in the systemic HBOT group (23 participants), 3 were cured, 8 were significantly improved, 11 were moderately improved and 1 did not improve, with a defined cure rate of 47.8% (11/23). The RR reported in the study was 1.89 (95% CI 1.21 to 2.96). However, when we used our definition of cure, our calculations provided a cure rate of 14.3% (3/21) in the topical HBOT group and of 13.0% (3/23) in the systemic HBOT group, with an RR of 1.10 (95% CI 0.25 to 4.84; Figure 5; Secondary outcomes).

Forest plot of comparison: 2 Additional topical HBOT versus additional systemic HBOT, outcome: 2.1 Cure rate.
Discussion
Summary of main results
At present, high quality evidence to determine the efficacy and safety of possible interventions for treating gas gangrene is unavailable. Only two RCTs that focused on topical HBOT and adjunctive use of Chinese herbs (Li 2001; Hou 2010) were found and both were at high or unclear risk of bias. Most of the important outcomes were not reported, including all the primary outcomes (Primary outcomes) we had hoped to include in our review; nor were there any reports of adverse events. The only outcome reported was cure rate, which was one of the secondary outcomes we had planned to include in our review, but the measures for this outcome differed between the two trials.The authors' definitions of cure rate, which included patients who were either cured or improved in the calculation (Included studies), differed from our definition. Re‐analysis of the cure rate based on our definition (i.e. only including participants who were cured; Secondary outcomes) showed limited evidence of benefit for the addition of Chinese herbs to standard treatment and no evidence of benefit for topical HBOT over systemic HBOT.
Overall completeness and applicability of evidence
Both studies included all randomized participants in the analysis without reporting the number lost to follow‐up. Participants who transferred to other hospitals may have produced censored data, but in Hou 2010 transfer was considered as an indication of treatment failure, which would tend to generate a misleading estimate, if outcomes were missing in imbalanced proportions across the groups. A higher proportion of transfers in the treatment group probably resulted in a conservative estimate of effect size on cure rate and a higher proportion in the control group probably led to an overestimate of the effect. Durations of follow‐up for each individual that varied from two to eight weeks may also have led to incompleteness in outcome detection in the Hou 2010 study, but specific information about whether and how data were incomplete was not available. Participants in the Li 2001 study were only followed up for 10 days and longer‐term outcomes were not reported.
The applicability of the evidence may have been influenced by the practice settings, patient characteristics, and causative agents. The two trials were conducted in general hospitals in Chinese towns, where healthcare resources and economic levels could not be comparable to those in tertiary hospitals in urban areas. The majority of participants had crepitus around their wounds, and X‐rays indicated gas between muscles in wounds. The duration of gas gangrene at baseline varied from two to 15 days in one study (Hou 2010), and from six hours to two weeks in the other (Li 2001). In the latter study, all the participants were diagnosed with gas gangrene through bacterial culture, but the pathogens varied between participants, with Clostridium perfringens accounting for nearly half of the participants.
Quality of the evidence
The quality of the evidence currently available is extremely low (summary of findings Table for the main comparison; summary of findings Table 2). The trials suffered from a high risk of bias in selective reporting and blinding of the participants and personnel. Some important methodological aspects of the RCTs were unclear, including random sequence generation, allocation concealment, blinding of outcome assessment and comparability of baseline characteristics. Data on the primary outcomes we hoped to include in our review were not available from the included studies. Cure rate, which we had defined as a secondary outcome for our review, was the only outcome the studies reported. This outcome could not reflect practitioners' and patients' main concerns about amputation, fatality and quality of life, and thus it is difficult to generalise the reported effects on cure rate to more relevant clinical outcomes. Small sample sizes within each study also resulted in low precision of the estimates. The small number of included studies made it impossible to assess consistency across studies with regard to publication bias.
Potential biases in the review process
Although we conducted a thorough review of published studies and ongoing trials, it remains possible that some relevant trials completed before the establishment of trial registries may not have released their results. We tried to contact the authors of the two included trials to obtain missing data, but we did not receive any response.
Agreements and disagreements with other studies or reviews
In addition to the one included trial that investigated Chinese herbs, we identified several observational studies (Tang 1982; Yu 1986; Ma 1991; Zhao 2004; Liu 2011). These all supported the adjunctive use of Chinese herbs, but their efficacy remains controversial because the studies were all case series without any control group, the herbs differed from study to study, and the sample sizes were small, varying from four to 20 participants.
Wth regard to the effectiveness of HBOT, other clinical evidence focused more on whether adjunctive use of HBOT can improve the prognosis of gas gangrene, but its benefits and harms remains controversial because of inconsistent results. A systematic review suggested a lack of trials to support the HBOT use for gas gangrene (Wang 2010), while the results of two retrospective multicentre studies did not demonstrate a survival advantage with HBOT for major necrotising infections that included gas gangrene (Brown 1994; George 2009). Furthermore, subgroup analysis for clostridial myonecrosis in retrospective comparative effectiveness research that included nearly 46,000 patients with necrotising soft tissue infections indicated that patients who received HBOT did not have a statistically significantly lower risk of mortality or complications (Soh 2012). Similar results have also been reported in some retrospective studies of HBOT added to surgery and antibiotic treatment for gas gangrene (Hart 1983; Shupak 1984; Korhonen 1999).
However, another systematic review concluded that evidence from some high quality observational studies suggested that HBOT may be an effective way to treat gas gangrene (Saunders 2003), but this review did not provide the list of the included studies or sufficient details about their study characteristics to substantiate this conclusion. Another review (Leach 1998), which was based on experimental research and clinical experience, suggested that additional HBOT for the treatment of gas gangrene was supported by strong scientific evidence, however the authors did not draw their conclusions from RCTs, since no trials were identified.
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Forest plot of comparison: 1 Additional Chinese herbs versus no additional Chinese herbs, outcome: 1.1 Cure rate.

Forest plot of comparison: 2 Additional topical HBOT versus additional systemic HBOT, outcome: 2.1 Cure rate.

Comparison 1 Additional Chinese herbs versus no additional Chinese herbs, Outcome 1 Cure rate.

Comparison 2 Additional topical HBOT versus additional systemic HBOT, Outcome 1 Cure rate.
| Additional Chinese herbs compared with no additional Chinese herbs for treating gas gangrene | ||||||
| Patient or population: patients with gas gangrene | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no Chinese herbs | Risk with Chinese herbs | |||||
| Cure rate | Study population | RR 3.08 | 46 | ⊕⊝⊝⊝ | ||
| 150 per 1000 | 462 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to limitations in design; high risk of performance and reporting bias, and unclear risk of bias in other bias sources. 2 Downgraded two levels due to imprecision; only one trial with small sample size and very wide confidence interval that included the possibility of an effect in either direction (crosses line of no effect). | ||||||
| Additional topical HBOT compared with additional systemic HBOT for treating gas gangrene | ||||||
| Patient or population: patients with gas gangrene | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with systemic HBOT | Risk with Topical HBOT | |||||
| Cure rate | Study population | RR 1.10 | 44 | ⊕⊝⊝⊝ | ||
| 130 per 1000 | 143 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to limitations in design; high risk of performance and reporting bias, and unclear risk of bias in selection and detection bias. 2 Downgraded two levels for imprecision; only one trial with small sample size and very wide confidence interval that included the possibility of an effect in either direction (crosses line of no effect). | ||||||
| Search strategies |
| China Biological Medicine Database (CBM‐disc) |
| #1 "气性坏疽"[常用字段:智能] |
| China National Knowledge Infrastructure (CNKI) |
| (主题="气性坏疽") OR ((主题="梭菌"+"梭状") AND (主题="肌坏死"+"肌炎")) |
| Chinese scientific periodical database of VIP INFORMATION (VIP) |
| ((题名或关键词=肌坏死 或 文摘=肌坏死 或 题名或关键词=肌炎 或 文摘=肌炎 与 专业=经济管理+图书情报+教育科学+自然科学+农业科学+医药卫生+工程技术+社会科学 与 范围=全部期刊) 与 (题名或关键词=梭状 或 文摘=梭状 或 题名或关键词=梭菌 或 文摘=梭菌 与 专业=经济管理+图书情报+教育科学+自然科学+农业科学+医药卫生+工程技术+社会科学 与 范围=全部期刊)) 或者 (题名或关键词=气性坏疽 或 文摘=气性坏疽 与 专业=经济管理+图书情报+教育科学+自然科学+农业科学+医药卫生+工程技术+社会科学 与 范围=全部期刊) |
| Science Citation Index |
| Gas gangrene or clostridi* myonecrosis |
| ClinicalTrials.gov (www.clinicaltrials.gov) |
| "Gas Gangrene"(By topics) |
| Current Controlled Trials (www.controlled‐trials.com) |
| "gas gangrene" or "myonecrosis" |
| WHO International Clinical Trials Registry Platform (www.who.int/trialsearch) |
| gas gangrene or clostridi* myonecrosis or non‐clostridi* myonecrosis or nonclostridi* myonecrosis |
| Australian New Zealand Clinical Trials Registry (www.anzctr.org.au) |
| "gas gangrene" or "clostridial myonecrosis" or "non‐clostridial myonecrosis" or "nonclostridial myonecrosis" |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cure rate Show forest plot | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.08 [1.00, 9.46] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Cure rate Show forest plot | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.25, 4.84] |

