Ortesis de la rodilla para el tratamiento del síndrome de dolor patelofemoral
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Prospective, single‐centre, single‐blinded, randomised controlled trial | |
| Participants | Based in Turkey. No recruitment/study dates documented. 86 participants were recruited (72 female, 14 male; mean age 42 years, range 17 to 80 years) diagnosed with patellofemoral pain syndrome by physicians and an orthopaedic surgeon. Two groups: Knee sleeve group: n = 41 (female 35, male 6; age 42.2 years (SD 15.3, range 17 to 80); mean duration of symptoms 24.2 months (SD 13.6, range 1 to 80)) Control group: n = 45 (female 37, male 8; age 41.0 years (SD 9.3, range 20 to 59); mean duration of symptoms 18.2 months (SD 13.2, range 1 to 72)) Inclusion criteria: Anterior or retropatellar knee pain when walking up and down stairs, squatting, kneeling or prolonged sitting for at least 4 weeks were enrolled in this study. In addition, they should have pain in at least 2 of the following physical tests: patellar compression test, in which pressure is applied over the patella while the knee is fully extended, Clarke’s test (physician places his/her hand over the patient’s patella, presses gently downwards, as the patient contracts the quadriceps muscle and the test is positive if pain occurs, which indicates patellofemoral joint problems), patellar apprehension test (the physician should be aware that patients with a history of subluxation or dislocation of the patella might feel very uncomfortable at this point and try to stop the physician from completing the test) and palpation of the posterior medial‐lateral borders of the patella. Hypermobility, measurement of Q‐angle and patellar tilt test were also applied. All participants underwent weight‐bearing anteroposterior telemetric X‐ray evaluation and tangential knee radiography in 30 and 45 degrees of flexion. Patellar subluxation (which was demonstrated by measuring the lateral PF angle), subchondral sclerosis and presence of degenerative changes were determined from these radiographs. All participants were diagnosed as having PFPS based on history, physical examination, and radiological evaluation Exclusion criteria: People with tibiofemoral compartment osteoarthritis, knee effusion, inflammatory joint pathology, infection, previous knee arthroplasty, lower extremity fracture history and severe cardiovascular diseases were excluded from the study. After the physical examination, full blood count, erythrocyte sedimentation rate (ESR), C‐reactive protein (CRP) and biochemical markers were evaluated in order to determine the presence of other systemic inflammatory diseases. | |
| Interventions | Knee sleeve group: Received the control group's exercise programme in addition to an Altex Patellar Knee support (Altex Patellar knee support AL‐2285C), which is a neoprene sleeve with a patella cut‐out. This was worn whilst performing the exercises as well as during the day for the six‐week study period. The knee support was only removed at night for sleeping Control group: A home‐based exercise therapy including a standardised protocol developed by a physiotherapist. This consisted of isometric and isotonic programmes for quadriceps muscles, performed five times per week. All participants performed 10 repetitions per day for six weeks. All participants provided with an exercise sheet, outlining the programme. All participants were reviewed at 2‐weekly intervals to monitor compliance to allocated treatment. | |
| Outcomes | Outcomes assessed at baseline and at 6 weeks post‐commencement of the sleeve and exercise interventions Outcomes evaluated included:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Consecutive admission to the outpatient clinic. Materials and Methods (Page 101) participants were "randomly allocated to either" group, with "randomisation made according to the consecutive admissions of the patients to the outpatient clinic" This appears to be quasi‐randomised |
| Allocation concealment (selection bias) | High risk | Not documented whether allocation was concealed but this seems unlikely. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding of physiotherapist: Materials and Methods section (page 101): “only the therapist who applied the therapy was aware of the therapy”. Although it would be logistically difficult to blind the participants or study personnel to the intervention, the standardisation of the intervention with the exercise sheet detailing the home‐exercise programme attempted to reduce physiotherapist's potential bias. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The assessor was blinded to group allocation. Methods section (page 101): "the physician was blinded to the treatment program". However, no safeguards were described and subjective outcomes reported by the patients were not blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Results section (page 102): "all patients completed the regular exercise program", therefore none appeared lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. However, all outcomes presented within the Results section (page 103) and Table 2, as previously discussed in the Methods section. |
| Other bias | Low risk | No other potential bias identified |
| Methods | Prospective, single‐centre, non‐blinded, randomised controlled trial | |
| Participants | Based in Israel. Participants recruited in the summer of 1990. All participants were male Israeli army recruits and were diagnosed and reviewed by a team that comprised an army physician and an orthopaedic surgeon. Review took place every two weeks during 14 weeks of basic military training. 59 participants (all males) with 84 affected and eligible knees were recruited. Three groups: Genutrain knee sleeve group: n = 22 knees (all male, age: not reported, duration not stated but was up to 2 weeks) Simple elastic sleeve group: n = 22 knees (all male, age: not reported, duration not stated but was up to 2 weeks) Control group: n = 40 knees (all male, age: not reported, duration not stated but was up to 2 weeks) No further details of the participants' characteristics were included in the text. Eligibility criteria: All participants presented with both subjective and objective findings indicative of patellofemoral pain syndrome, but with no history of knee trauma or symptoms of patellofemoral pain syndrome prior to joining the miliary services. | |
| Interventions | Simple elastic sleeve group: Received same basic military training as the control group in addition to receiving a simple elastic knee sleeve. Genutrain knee sleeve group: Received same basic military training as the control group in addition to receiving an elastic knee sleeve with silicone plastic ring (Genutrain, Bauerfeind GmbH, Kempen, Germany). The paper does not clearly define when and for how long the knee sleeves were worn by participants in the two knee sleeve groups. Control group: received no treatment but standard 14 weeks of basic military training. | |
| Outcomes | Outcomes were evaluated every 2 weeks for a total of 14 weeks during basic military training and then 2 months following the completion of basic military training. The outcomes assessed were: 1. Pain subjectively rated using a 1 to 4 Likert system where: 1 = discomfort, 2 = moderate pain, 3 = significant pain but continue to train, 4 = severe pain and stop training. 2. Participant satisfaction with their brace/treatment was rated on a 1 to 4 Likert system. The definitions of each criterion were not provided. 3. Complications from wearing the interventions were evaluated through questioning participants about their experiences. Complications such as the sleeve rubbing or skin abrasions were recorded. | |
| Notes | The imbalance in the numbers in the treatment groups was not explained. It is possible that random allocation applied to treatment (knee orthosis) versus no treatment groups and not the two knee orthosis groups. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Methods not stated, only that the participants were randomised. Materials and Methods (page 209): "Recruits with overuse patellofemoral pain were divided randomly into treatment (Groups 1 and 2) and nontreatment groups (Group 3)." Note it is not clear whether any randomisation occurred for allocation of the different knee sleeves. |
| Allocation concealment (selection bias) | Unclear risk | No information provided to indicate whether participant allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | No information provided in the paper regarding blinding of participants or study personnel and clinicians to group allocation. However, this would have been logistically difficult to achieve due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) | High risk | No information was provided in the paper indicating whether the assessor was blinded to group allocation during the data collection phases. |
| Incomplete outcome data (attrition bias) | Unclear risk | All participants appear to be accounted for at end of the trial. However, group allocation statistics were available only for knees not participants. See also 'Other bias'. |
| Selective reporting (reporting bias) | High risk | No protocol available. Pain scores were only reported for baseline and at two months after completion of their basic military training. No data presented on participant satisfaction. |
| Other bias | High risk | It was not explicitly stated how many participants in each group presented with bilateral knee symptoms. Results (page 209): “59 recruits were diagnosed as having anterior knee pain in 84 affected knees”. Unresolvable unit of analyses problems. |
| Methods | Prospective, single‐centre, single‐blinded, randomised controlled trial | |
| Participants | Based in Canada. No recruitment/study dates documented. We assume participants are 'mixed civilian' but the details of actual composition of population are not given. The population was drawn from an university sports centre, university campus community and city fitness facilities, and family physician clientele. 152 participants met the inclusion criteria 21 withdrew and 2 crossed over. Data were reported for 129 participants (76 females, 53 males) with 186 affected knees: diagnosed and eligibility determined by two sport medicine physicians Four groups: Knee brace group: n = 32 (gender not specified; mean age 34 years (SD 11); symptom duration 8 months (SD 6 months)); 47 knees Exercise group: n = 34 (gender not specified; mean age 35 years (SD 11); symptom duration 11 months (SD 8 months)); 50 knees Exercise and knee brace group: n = 32 (gender not specified; mean age 35 years (SD 11); symptom duration 10 months (SD 7 months)); 45 knees Exercise and knee sleeve group: n = 31 (gender not specified; mean age 35 years (SD 9); symptom duration 7 months (SD 5 months)); 44 knees Eligibility criteria: listed under 3 categories in the trial report. History
Physical examination
X‐ray examination
| |
| Interventions | Knee brace group: Participants wore a knee brace only. The brace was a Special FX Knee Brace (Generation II Orthotics, Inc, Richmond, BC). It has a Y‐shaped inferior patellar buttress pad and an external stabilisation strap to help control patellar movement Exercise group: Participants received a structured home rehabilitation programme only. This structured home‐rehabilitation programme consisted of a strengthening component, consisting of a 6‐stage progression of 2‐leg eccentric drop squats, then single leg lunges, and finally 1‐leg eccentric drop squats. The stretching component of the rehabilitation programme consisted of seated spinal rotations, supine hip external rotation, standing quadriceps stretch, and sitting hamstring stretch. Stretches were performed daily prior to and after the strengthening component of the programme. Each stretch was performed passively 3 times, with each stretch held for 30 seconds. Exercise and knee brace group: Participants received the exercise group's structured home‐rehabilitation and were prescribed and fitted with the Special FX Knee Brace (Generation II Orthotics, Inc, Richmond, BC) as described above. Exercise and knee sleeve group: Participants received the exercise group's structured home‐rehabilitation programme and were prescribed and fitted with a knee sleeve constructed with same sleeve material as the patella brace. No hole was made in the sleeve over the patella. The knee braces and knee sleeves were fitted by the second research assistant. In those diagnosed with bilateral PFPS, both knees were fitted with a knee brace or knee sleeve. Participants in the brace group, exercise and brace group or exercise and knee sleeve group were encouraged to wear their braces or sleeves at all times except whilst sleeping | |
| Outcomes | The outcome measurements were performed at baseline and at 3, 6 and 12 weeks. Outcomes evaluated were: 1. VAS knee pain rating. This was evaluated in three different situations: during sport activity; 1 hour after sport activity; and following 30 minutes of sitting with knees flexed. 2. Knee Function Scale. For the purpose of this study, the scale was modified. A 'no pain' response was added to the occurrence of pain category, with a corresponding score of 18. The maximum score of the knee function scale was therefore increased to 53, which equated to normal function. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised to interventions. Methods, Study Procedure (page 236): “random number generator with block design” |
| Allocation concealment (selection bias) | Low risk | Randomisation was through concealed allocation through a second researcher. Methods, Study Procedure (Page 236): "a second research assistant used a random number generator with block design to assign subjects to 1 of 4 treatment group." |
| Blinding of participants and personnel (performance bias) | High risk | No information provided regarding the blinding of researchers or clinical personnel. No information provided regarding the blinding of study participants; however, participants or clinician blinding would be logistically difficult due to the nature of the study interventions. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Study was described as 'single‐blinded' in the abstract of the trial report, which also stated "The investigators were blinded to the treatment group of each subject." However, no information was provided in the text of the trial report including measures taken to avoid unblinding of group allocation. Moreover, subjective outcomes reported by the patients were not blinded. |
| Incomplete outcome data (attrition bias) | High risk | Separate participant flow not provided for individual groups. Thus group allocation of the 21 withdrawals and 2 cross‐overs excluded from the analyses. See also 'Other bias'. Data inconsistencies and potential labelling errors between table 3 and figures in the article. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. However, all outcomes reported in the Methods section were reported in the Results section (pages 237 to 239). |
| Other bias | High risk | In the Analysis (p 237) it is stated that "If a subject had bilateral symptoms, each knee was individually included in the analysis." Unresolvable unit of analysis issues. |
| Methods | Prospective, single‐centre, non‐blinded, randomised controlled trial | |
| Participants | Based in USA. No recruitment/study dates documented. 59 participants (data for 51: 13 females, 38 males). All participants were military cadets. Unclear who diagnosed and determined eligibility. Three groups: Palumbo sleeve group: n = 18 (3 female, 15 male; age not reported; duration of symptoms within 3 weeks of starting training) Cho‐Pat knee strap group: n = 13 (2 female, 11 male; age not reported; duration of symptoms within 3 weeks of starting training) Control group: n = 20 (8 female, 12 male; age not reported; duration of symptoms within 3 weeks of starting training) No further information on baseline characteristics available Inclusion criteria: Complaint of anterior knee pain within first three weeks of military training Exclusion criteria: Lack of desire to remain in basic training; previous surgery; history patellar dislocation; previously known knee disorders; abnormalities on physical examination; abnormal radiographs | |
| Interventions | Palumbo sleeve group: Participants received all interventions provided in the control group in addition to the provision, fitting and instruction to wear the Palumbo Brace throughout all military training activities Cho‐Pat knee strap group: Participants received all interventions provided in the control group in addition to the provision, fitting and instruction to wear the Cho‐Pat Knee Strap throughout all military training activities 'Brace wear was monitored throughout the study to ensure compliance." (p11 of article) Control group: Enrolled in physical therapy consisting of an exercise programme of closed‐chain quadriceps strengthening exercises and a lower limb tissue flexibility (stretching) programme; ibuprofen prescribed (800 milligrams) 3 times daily; and completion of basic military physical training. The trainees were allowed to substantially modify their activities at the risk of being 'disenrolled' from their 2 months training. | |
| Outcomes | Participants were evaluated weekly from baseline to 8 weeks post‐randomisation. The main outcome assessed was the Patient Pain Profile Questionnaire, which incorporates a VAS score, a measure of participant's desire to remain in training and a measure of their desire to remain in training if their knee pain resolves. | |
| Notes | The total number of recruits able to complete the training was also documented and the relevant reasons for attrition explained | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation not clearly documented. Materials and Methods (page 11): participants “were then randomised into the groups”. |
| Allocation concealment (selection bias) | Unclear risk | No clear documentation as to whether randomisation was performed through a concealed method. Materials and Methods (page 11): participants “were then randomised into the groups”. |
| Blinding of participants and personnel (performance bias) | High risk | No information was provided regarding whether participants or study personnel/clinicians were blinded to group allocation. Due to the nature of the intervention, it would have been logistically difficult to blind participants to the bracing interventions. |
| Blinding of outcome assessment (detection bias) | High risk | The paper did not detail whether assessors were blinded to group allocation. |
| Incomplete outcome data (attrition bias) | Unclear risk | Participant attrition was documented with all participants accounted for. Materials and methods page 12: "four participants were excluded from the study due to insufficient follow‐up. Four additional patients failed to complete basic training leaving 51 patients in the study cohort". While the % losses were similar in the three groups (13% to 14%), some bias could result from differing reasons for missing data. |
| Selective reporting (reporting bias) | High risk | The Materials and Methods section states a number of outcome measurements were collected (Page 11). These included: "thigh circumference, effusion, popliteal angle, compression test, localised tenderness, apprehension test, Q‐Angle, range of motion, Lachmann test, anterior drawer, varus/valgus instability and McMurray’s tests.” However, these were not reported. The paper also only reported findings from the initial 3‐week follow‐up period, neglecting to provide data from weeks 4 to 8. No explanation was provided for this discrepancy in reporting. |
| Other bias | Unclear risk | Baseline characteristics not provided for all randomised participants. |
| Methods | Prospective, single‐centre, non‐blinded, randomised controlled trial | |
| Participants | Based in Denmark. No recruitment/study dates documented We assume participants are 'mixed civilian' but this is not actually stated. Unclear who diagnosed and determined eligibility 35 participants (35 unilateral knees) (25 female, 10 male; mean age 23 years (range 18 to 35); mean duration of symptoms 21 months (3 to 120 months)) Two groups: Knee brace group: n = 17 (gender, age and duration of symptoms not specified; 10 participants had a history of patellar subluxation and 7 participants had a history of idiopathic chondromalacia patellae) Control group: n = 18 (gender, age and duration of symptoms not specified; 7 participants had a history of patellar subluxation; and 11 participants had a history of idiopathic chondromalacia patellae) Inclusion criteria: Arthroscopy was done on all knees and revealed different stages of diseased articular cartilage. The knees were initially evaluated subjectively and objectively according to the numerical rating system described by Turba 1979, assessing swelling, pain, symptoms of instability, and limitation of activity. Objectively, the evaluation included motion, pain effusion, quadriceps atrophy, and patellar hypermobility. Exclusion criteria: Patients with obvious signs of meniscus tears, joint laxity, radiological osteoarthritis, former surgery of the knee, or recurrent subluxation of the patella | |
| Interventions | Knee brace group: In addition to the exercise programme, participants in this group wore a knee brace made of orthoplast. The brace only allowed a knee range of motion from 0 to 30 degrees of flexion. The brace was worn for a 6‐week period. No details provided with regards to whether the brace was worn at night or not. Control group: An isometric quadriceps and hamstrings exercise programme. This was performed for at least 15 minutes, 4 times daily. Participants were asked to exercise within the limits of their pain. | |
| Outcomes | A follow‐up was performed after 6 weeks and 3 and 12 months Outcome measures included:
| |
| Notes | Five participants subsequently underwent surgery; 4 for correction of patellar malalignment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention of randomisation procedure. No detail provided regarding sequence generation. Patients and Methods section (page 377) “seventeen patients were randomised to a knee brace made of orthoplast”. |
| Allocation concealment (selection bias) | Unclear risk | No mention of randomisation procedure, with the methods of allocation concealment not described. |
| Blinding of participants and personnel (performance bias) | High risk | This was not described in the paper. It was unclear from information presented in the paper which personnel were involved in the trial and whether they were blinded to group allocation. Given the nature of this intervention, it would be logistically difficult to blind participants or personnel to group allocation. |
| Blinding of outcome assessment (detection bias) | High risk | There was insufficient information detailing potential assessor blinding, and data collection of the outcome measures. |
| Incomplete outcome data (attrition bias) | Unclear risk | All participants seem to be accounted in the Results section (page 378) but incomplete reporting of data (see next item). |
| Selective reporting (reporting bias) | High risk | All outcome measures discussed in the Patients and Methods sections were presented in the Results section (page 387). However, no raw data were available and no numerical values were provided for the Turba scale. The paper only presented the frequency of 'excellent' and 'good' results as a combined number. It was therefore difficult to interpret the Results (Page 378 and Table 1). |
| Other bias | High risk | The Patients and Methods section was not clear, particularly in relation to the data collection procedure, which was not described. |
Outcomes in bold are those that are relevant for this review.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| No orthosis examined | |
| No orthosis examined | |
| Examined the use of orthosis as a 'preventative' rather than 'treatment' intervention | |
| The intervention under investigation was a resistance exercise device rather than a brace or orthosis | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| None of the participants presented with patellofemoral pain syndrome; all had pain‐free knees | |
| Randomisation was used to allocate the order of treatment within individual participants but not the allocation of interventions among participants | |
| Randomisation was used to allocate the order of treatment within individual participants but not the allocation of interventions among participants. None of the participants presented with patellofemoral pain syndrome | |
| The intervention under investigation was a resistance exercise device rather than a brace or orthosis | |
| Recruited participants who did not have patellofemoral pain syndrome. Outcome measurement of interest was the 'prevention' not the 'treatment' of patellofemoral pain syndrome | |
| Paper solely reported concentric isokinetic test results. This outcome was not a pre‐specified outcome measure of interest in this review | |
| A comparison of two taping techniques with no investigation of orthosis interventions | |
| Not a randomised controlled trial |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | "Therapy of the patellofemoral pain syndrome: A prospective randomised study with two treatment groups: Physiotherapy and 2. Recentering orthosis plus physiotherapy" |
| Methods | Open, randomised controlled trial |
| Participants | 135 male and females aged between 18 and 50 (target recruitment). Inclusion criteria: patient's suffering longer than 2 months but not longer than 2 years with any 3 of the following symptoms: anterior knee pain while running; anterior knee pain while climbing stairs; anterior knee pain while bicycling; anterior knee pain while sitting with flexed knees; anterior knee pain while squatting. Exclusion criteria: osteoarthritis 3° to 4°; local cartilage damage 3° to 4°; subluxation of the patella; previous knee injuries (ACL ruptures); tendinosis of the patella tendon; Osgood Schlatter; pathological damage of the knee joint (osteochondrosis dissecans); valgus knee with more than 3 fingers between the malleoli; varus knee with more than 2 fingers between the femoral condyles |
| Interventions | Group 1: prescription of physiotherapy: 12 x 30‐minute physiotherapy sessions (to be delivered x 2 weekly sessions over a 6‐week period) Group 2: a Patella Pro Orthosis and a prescription of physiotherapy (12 x physiotherapy for 30 minutes). The patients should wear the Patella Pro Orthosis for 6 hours even during physiotherapy |
| Outcomes | 1. A 'healing' score (7 points Likert scale) Outcomes will be measured at the initial visit, 6 weeks, 3 months and 12 months |
| Starting date | 01.03.2012 |
| Contact information | Wolf Petersen, Caspar Theyys Strasse 27‐31, 14193, Berlin, Germany, w.petersen@mlk‐berlin.de |
| Notes | Commercial source of funding: Otto Bock Health Care GmbH Abt. Medical Affairs, Germany |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during activity (0 to 10; higher score means worse pain) Show forest plot | 3 | 234 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐1.16, 0.24] |
| Analysis 1.1  Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 1 Pain during activity (0 to 10; higher score means worse pain). | ||||
| 1.1 Knee sleeve | 3 | 162 | Mean Difference (IV, Fixed, 95% CI) | ‐0.48 [‐1.31, 0.35] |
| 1.2 Patellar strap | 1 | 23 | Mean Difference (IV, Fixed, 95% CI) | ‐1.09 [‐3.71, 1.53] |
| 1.3 Knee brace | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.68, 1.28] |
| 2 Pain scores (0 to 10; higher score means worse pain) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2 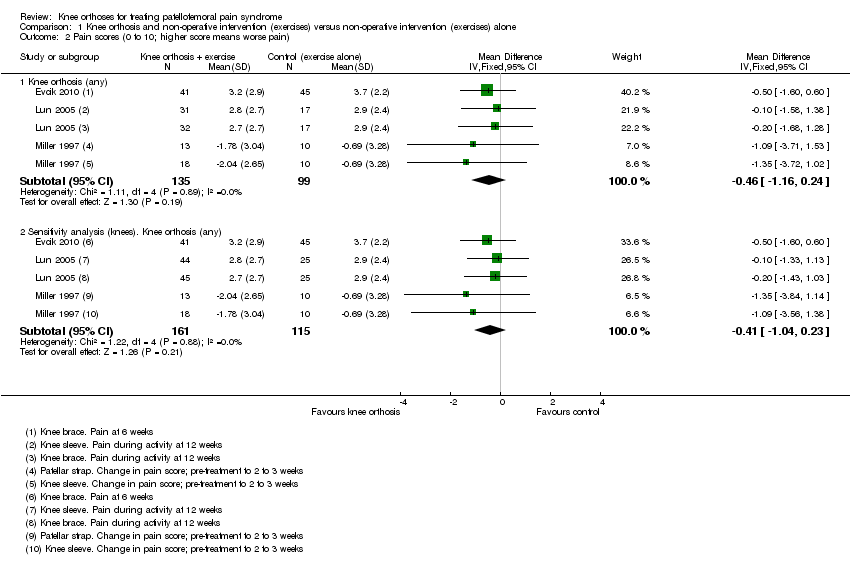 Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 2 Pain scores (0 to 10; higher score means worse pain). | ||||
| 2.1 Knee orthosis (any) | 3 | 234 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐1.16, 0.24] |
| 2.2 Sensitivity analysis (knees). Knee orthosis (any) | 3 | 276 | Mean Difference (IV, Fixed, 95% CI) | ‐0.41 [‐1.04, 0.23] |
| 3 Different pain scores (0 to 10; higher score means worse pain) at 12 weeks Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 3 Different pain scores (0 to 10; higher score means worse pain) at 12 weeks. | ||||
| 3.1 Pain during activity | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐1.20, 0.90] |
| 3.2 Sensitivity analysis (knees). Pain during activity | 1 | 139 | Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐1.02, 0.72] |
| 3.3 Pain 1 hour after sporting activity | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | 0.75 [‐0.19, 1.69] |
| 3.4 Sensitivity analysis (knees). Pain 1 hour after sporting activity | 1 | 139 | Mean Difference (IV, Fixed, 95% CI) | 0.75 [‐0.04, 1.53] |
| 3.5 Pain after 30 minutes sitting with knees flexed | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.82, 1.32] |
| 3.6 Sensitivity analysis (knees). Pain after sitting with knees flexed | 1 | 139 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.64, 1.14] |
| 4 Excellent or good results in terms of reduction in symptoms Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 4 Excellent or good results in terms of reduction in symptoms. | ||||
| 4.1 At 12 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 At 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Functional scores (higher score means higher function) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.5 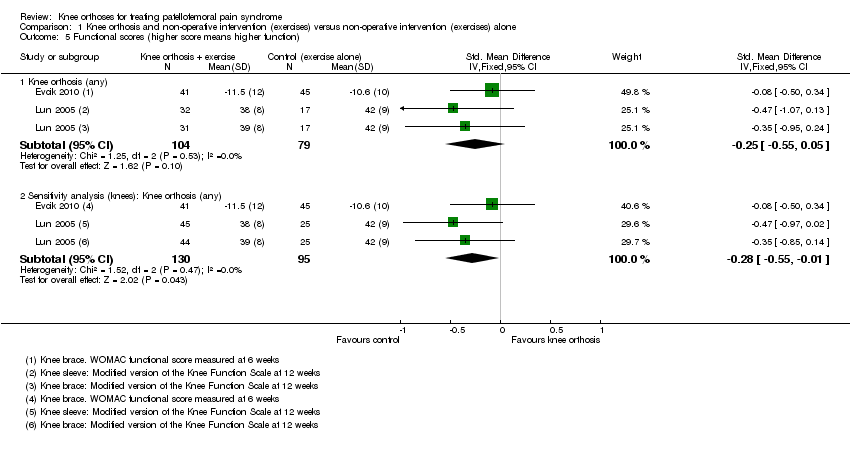 Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 5 Functional scores (higher score means higher function). | ||||
| 5.1 Knee orthosis (any) | 2 | 183 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐0.55, 0.05] |
| 5.2 Sensitivity analysis (knees): Knee orthosis (any) | 2 | 225 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.55, ‐0.01] |
| 6 Discontinuation of a basic military training programme Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.6  Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 6 Discontinuation of a basic military training programme. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain score (0 to 10: higher score means worse pain) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1 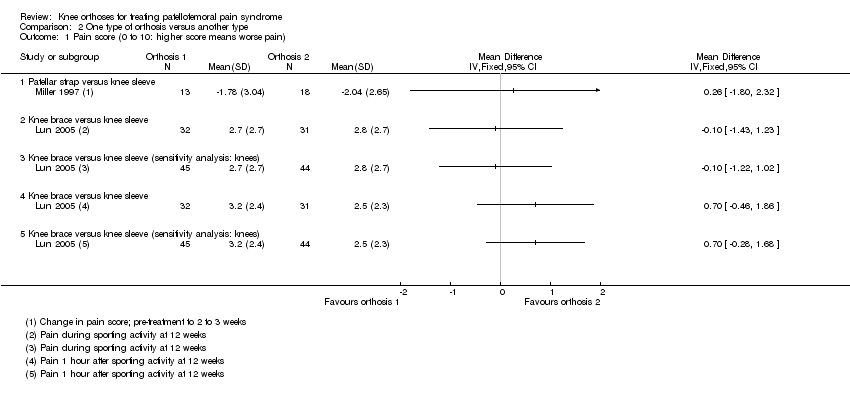 Comparison 2 One type of orthosis versus another type, Outcome 1 Pain score (0 to 10: higher score means worse pain). | ||||
| 1.1 Patellar strap versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Knee brace versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Knee brace versus knee sleeve (sensitivity analysis: knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Knee brace versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Knee brace versus knee sleeve (sensitivity analysis: knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Functional score (0 to 53: higher scores means greater function) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 One type of orthosis versus another type, Outcome 2 Functional score (0 to 53: higher scores means greater function). | ||||
| 2.1 Knee brace versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Knee brace versus knee sleeve (sensitivity analysis: knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Discontinuation of a basic military training programme Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 One type of orthosis versus another type, Outcome 3 Discontinuation of a basic military training programme. | ||||
| 3.1 Patellar strap versus knee sleeve | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Complications Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.4 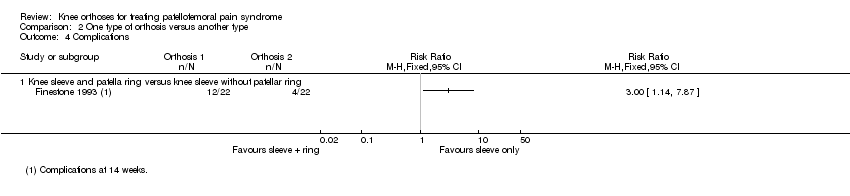 Comparison 2 One type of orthosis versus another type, Outcome 4 Complications. | ||||
| 4.1 Knee sleeve and patella ring versus knee sleeve without patellar ring | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during activity (0 to 10: higher score means worse pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1 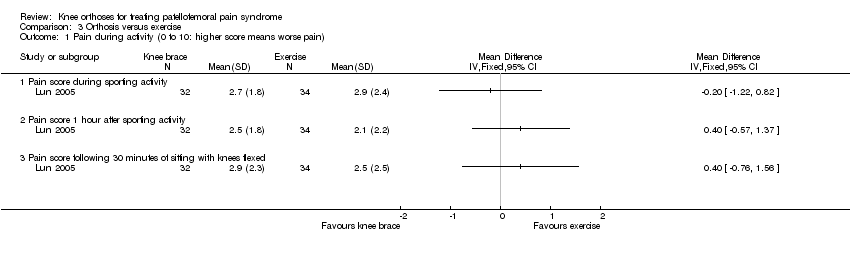 Comparison 3 Orthosis versus exercise, Outcome 1 Pain during activity (0 to 10: higher score means worse pain). | ||||
| 1.1 Pain score during sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Pain score 1 hour after sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Pain score following 30 minutes of sitting with knees flexed | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Sensitivity analyses (knees): Pain during activity (0 to 10: higher score means worse pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.2  Comparison 3 Orthosis versus exercise, Outcome 2 Sensitivity analyses (knees): Pain during activity (0 to 10: higher score means worse pain). | ||||
| 2.1 Pain score during sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Pain score 1 hour after sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Pain score following 30 minutes of sitting with knees flexed | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Functional scores (0 to 53: higher scores means greater function) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.3 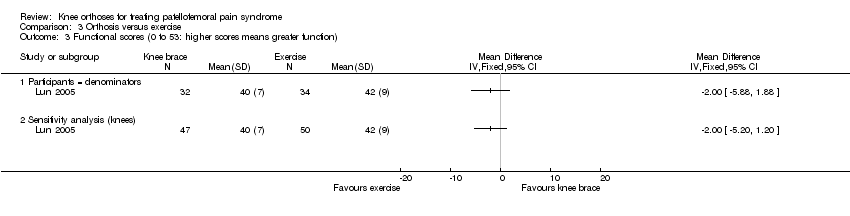 Comparison 3 Orthosis versus exercise, Outcome 3 Functional scores (0 to 53: higher scores means greater function). | ||||
| 3.1 Participants = denominators | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Sensitivity analysis (knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
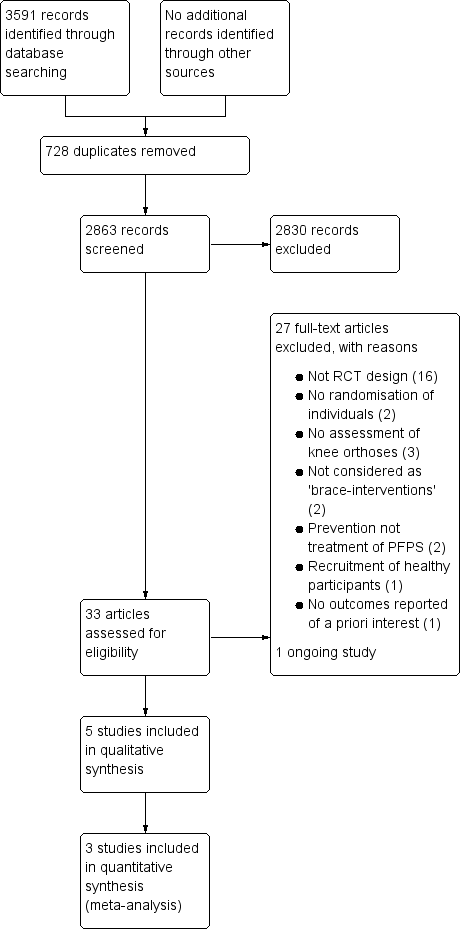
Study flow diagram

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
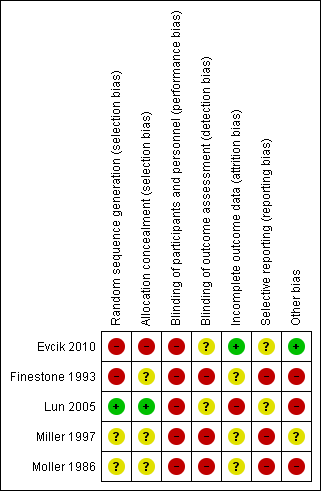
Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Forest plot 1.1. Comparison: knee orthosis and exercises versus exercises alone. Outcome: pain during activity (0 to 10; higher score means worse pain)

Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 1 Pain during activity (0 to 10; higher score means worse pain).
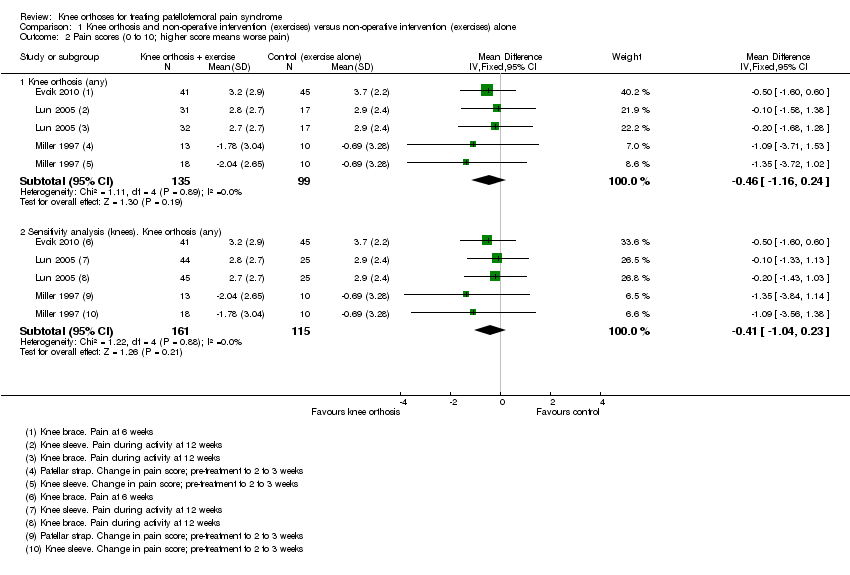
Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 2 Pain scores (0 to 10; higher score means worse pain).

Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 3 Different pain scores (0 to 10; higher score means worse pain) at 12 weeks.
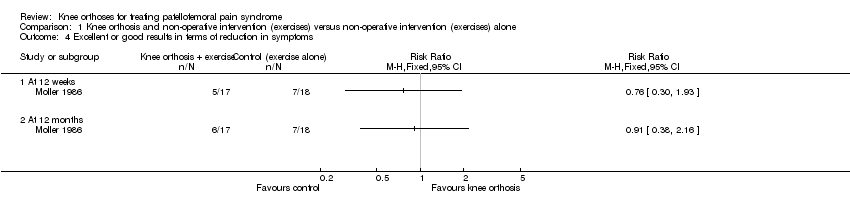
Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 4 Excellent or good results in terms of reduction in symptoms.

Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 5 Functional scores (higher score means higher function).
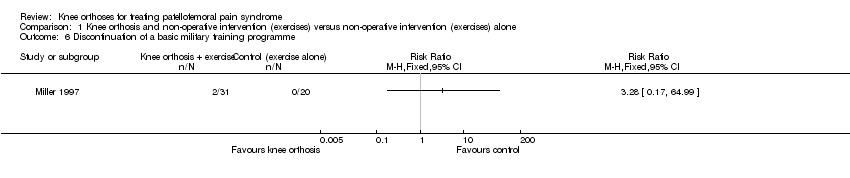
Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 6 Discontinuation of a basic military training programme.

Comparison 2 One type of orthosis versus another type, Outcome 1 Pain score (0 to 10: higher score means worse pain).

Comparison 2 One type of orthosis versus another type, Outcome 2 Functional score (0 to 53: higher scores means greater function).
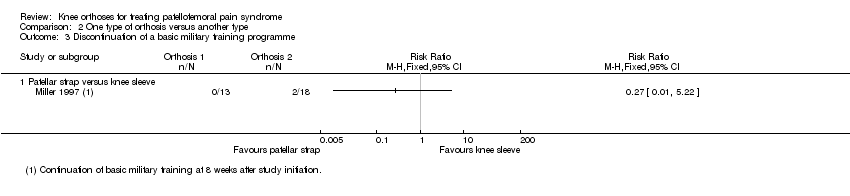
Comparison 2 One type of orthosis versus another type, Outcome 3 Discontinuation of a basic military training programme.

Comparison 2 One type of orthosis versus another type, Outcome 4 Complications.

Comparison 3 Orthosis versus exercise, Outcome 1 Pain during activity (0 to 10: higher score means worse pain).
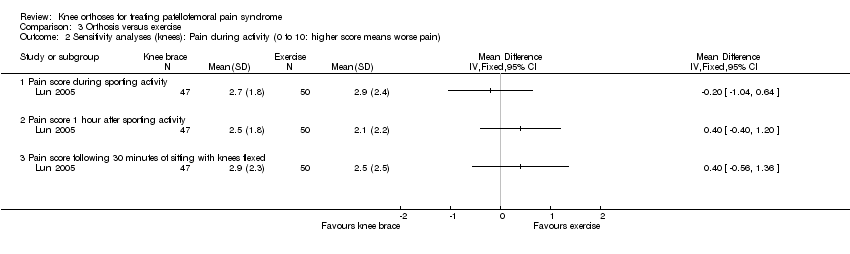
Comparison 3 Orthosis versus exercise, Outcome 2 Sensitivity analyses (knees): Pain during activity (0 to 10: higher score means worse pain).

Comparison 3 Orthosis versus exercise, Outcome 3 Functional scores (0 to 53: higher scores means greater function).
| Knee orthosis and exercise versus exercise alone for patellofemoral pain syndrome (PFPS) | ||||||
| Patient or population: Adults (recruited from health clinics or military recruits) with PFPS (duration of symptoms ranged from acute, under 2 to 3 weeks in two trials, to predominantly chronic in three trials: mean durations 8.3 months, 21 months, 21 months) Settings: Health clinics, home and military training establishments Intervention: Knee orthosis (various types: knee sleeve, knee brace or patellar strap) and exercise (military training, home exercise programme) Comparison: Exercise alone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Exercise alone | Knee orthosis and exercise | |||||
| Pain score (VAS) Scale from: 0 to 10 (higher scores mean worse pain) Follow‐up: 3 to 12 weeks (short‐term) | The mean pain score for the exercise alone group ranged across the control groups from 2.7 to 3.2 points; the mean change score from ‐0.47 to ‐0.96 points | The mean pain score in the knee orthosis and exercise group was 0.46 points lower (1.16 lower to 0.24 higher) | MD ‐0.46 (‐1.16 to 0.24) | 234 (3) | ⊕⊝⊝⊝ | The MD and 95% CIs do not include clinically important treatment effects. MCID: 30 mm on an 100 mm VAS (Lee 2003) |
| Functional outcomes Scale various 2 Follow‐up: 6 and 12 weeks (short‐term) | The mean functional score in the knee orthosis and exercise group was 0.15 points lower (0.69 lower to 0.38 higher) The mean difference in knee function (short‐term) in the knee orthosis group was 0.25 standard deviations lower (0.55 lower to 0.05 higher) | SMD ‐0.25 (‐0.55 to 0.05) | 183 (2) | ⊕⊝⊝⊝ | Lower values equate to higher disability. The SMD result equates to a small difference at most and in absolute terms, the mean differences for each trial were small (e.g. 0.9 for a range 0 to 68) and not clinically important | |
| Quality of Life and General Health Assessments | See comment | See comment | No study reported this outcome | |||
| Impact on sporting and occupational participation | See comment | See comment | 51 (1)4 | ⊕⊝⊝⊝ | One trial reported that 2 out of 31 (6.5%) participants in the knee orthosis groups versus 0 of 20 (0%) in the control group withdrew from their military training programme. | |
| Resource use | See comment | See comment | No study reported this outcome | |||
| Participant satisfaction | See comment | See comment | No study reported this outcome | |||
| Complications Follow‐up: 14 weeks6 | See comment | See comment | 59 with 84 affected knees (1) | ⊕⊝⊝⊝ | Trial reported 16 complications (skin abrasions or discomfort) for 44 knees (36%) of participants in the knee orthosis group. | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including selection bias (1 trial) and performance bias (all 3 trials)), and one level for indirectness (this reflects the clinical heterogeneity such as variation in the interventions and outcome measures and measurement, and the generally inadequate description of these). There was, however, no statistical heterogeneity in the pooled data. 2. One trial reported WOMAC functional scores (0 to 68; higher values mean worse function) at six weeks and the other the results of a modified version of the Knee Function Scale (0 to 53; higher values mean better function) at 12 weeks. 3. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including selection bias (1 trial) and performance bias (both trials)), and one level for imprecision (wide confidence intervals and limited data). 4. Data on resumption of sports activities were not split by treatment group in one trial (35 participants). 5. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including performance and detection biases), and one level for indirectness (abandonment of military training may be for other reasons than serious knee pain). 6. The single study recording this outcome did not record complications for all groups. The follow‐up for complications appeared be during use; i.e. the basic military training programme of 14 weeks.. 7. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including performance and detection biases and serious unit of analyses issues relating to the inclusion of participants with anterior knee pain in both knees), and imprecision (incomplete data from one small trial). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during activity (0 to 10; higher score means worse pain) Show forest plot | 3 | 234 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐1.16, 0.24] |
| 1.1 Knee sleeve | 3 | 162 | Mean Difference (IV, Fixed, 95% CI) | ‐0.48 [‐1.31, 0.35] |
| 1.2 Patellar strap | 1 | 23 | Mean Difference (IV, Fixed, 95% CI) | ‐1.09 [‐3.71, 1.53] |
| 1.3 Knee brace | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.68, 1.28] |
| 2 Pain scores (0 to 10; higher score means worse pain) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Knee orthosis (any) | 3 | 234 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐1.16, 0.24] |
| 2.2 Sensitivity analysis (knees). Knee orthosis (any) | 3 | 276 | Mean Difference (IV, Fixed, 95% CI) | ‐0.41 [‐1.04, 0.23] |
| 3 Different pain scores (0 to 10; higher score means worse pain) at 12 weeks Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Pain during activity | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐1.20, 0.90] |
| 3.2 Sensitivity analysis (knees). Pain during activity | 1 | 139 | Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐1.02, 0.72] |
| 3.3 Pain 1 hour after sporting activity | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | 0.75 [‐0.19, 1.69] |
| 3.4 Sensitivity analysis (knees). Pain 1 hour after sporting activity | 1 | 139 | Mean Difference (IV, Fixed, 95% CI) | 0.75 [‐0.04, 1.53] |
| 3.5 Pain after 30 minutes sitting with knees flexed | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.82, 1.32] |
| 3.6 Sensitivity analysis (knees). Pain after sitting with knees flexed | 1 | 139 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.64, 1.14] |
| 4 Excellent or good results in terms of reduction in symptoms Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 At 12 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 At 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Functional scores (higher score means higher function) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Knee orthosis (any) | 2 | 183 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐0.55, 0.05] |
| 5.2 Sensitivity analysis (knees): Knee orthosis (any) | 2 | 225 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.55, ‐0.01] |
| 6 Discontinuation of a basic military training programme Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain score (0 to 10: higher score means worse pain) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Patellar strap versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Knee brace versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Knee brace versus knee sleeve (sensitivity analysis: knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Knee brace versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Knee brace versus knee sleeve (sensitivity analysis: knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Functional score (0 to 53: higher scores means greater function) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Knee brace versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Knee brace versus knee sleeve (sensitivity analysis: knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Discontinuation of a basic military training programme Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Patellar strap versus knee sleeve | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Complications Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Knee sleeve and patella ring versus knee sleeve without patellar ring | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during activity (0 to 10: higher score means worse pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Pain score during sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Pain score 1 hour after sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Pain score following 30 minutes of sitting with knees flexed | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Sensitivity analyses (knees): Pain during activity (0 to 10: higher score means worse pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Pain score during sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Pain score 1 hour after sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Pain score following 30 minutes of sitting with knees flexed | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Functional scores (0 to 53: higher scores means greater function) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Participants = denominators | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Sensitivity analysis (knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

