Fentanilo intranasal para el tratamiento del dolor agudo en niños
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by year of study]
| Methods | Prospective, randomized, open‐label, 2‐arm study at a single site (paediatric emergency department) in Australia | |
| Participants | 47 patients (3‐10 years of age) with clinically suspected fracture of the upper and/or lower limbs | |
| Interventions | Intervention 1: single dose of INF (50 mcg/mL) at a dose of 1 mcg/kg Intervention 2: single dose of IMM (10 mg/mL) at a dose of 0.2 mg/kg | |
| Outcomes | Primary outcome measure: reduction in pain using Wong Baker Faces (ordinal scale 0‐5). Pain intensity was measured at 0, 5, 10, 20 and 30 minutes Secondary outcome measures: occurrence of opiate toxicity (sedation, respiratory or cardiovascular depression) and participant tolerance of analgesia (nausea/vomiting and reported discomfort) | |
| Notes | Both interventions produced a reduction in pain score. "Rescue analgesia" was administered to 1 participant in the INF group and to no participants in the IMM group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Included in the study were children aged between 3 and 10 years who were otherwise healthy and who presented to the ED with clinical fracture of the upper or lower limbs" |
| Allocation concealment (selection bias) | Low risk | Quote: "Once parents had given informed consent, patients were randomized via a sealed envelope system" |
| Blinding of participants and personnel (performance bias) | High risk | Comment/Quote: Participants were randomly assigned "to receive a single dose of either 1.0 μg/kg INF or 0.2 mg/kg IMM" |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Pain was assessed by the children at 0, 5, 10, 20 and 30 min after treatment administration using Wong Baker Faces (ordinal scoring 0–5) and also by their parents using a visual analogue score (continuous 0–10)" |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Forty‐seven children were recruited into the study, 24 into the INF arm and 23 into the IMM arm, with no parents refusing consent" Comment: No participant was withdrawn from this study following enrolment |
| Selective reporting (reporting bias) | Low risk | Comment: All of the study's prespecified outcomes of interest in the review have been reported in the prespecified way |
| Other bias | Low risk | Comment: The study appears to be free of other sources of bias |
| Methods | Prospective, double‐blind, randomized, placebo‐controlled clinical trial at a single site (tertiary paediatric emergency department) in Australia | |
| Participants | 67 patients (7‐15 years of age) with clinically deformed closed long bone fractures were enrolled | |
| Interventions | Intervention 1: active INF (150 mcg/mL) at a dose of 1.4 mcg/kg AND intravenous placebo Intervention 2: active IVM (10 mg/mL) at a dose of 0.1 mg/kg AND intranasal placebo | |
| Outcomes | Primary outcome measure: reduction in pain using a 100‐mm unmarked visual analogue scale. Pain intensity was measured at 0, 5, 10, 20 and 30 minutes Secondary outcome measures: occurrence of opiate toxicity (sedation, respiratory or cardiovascular depression) and participant tolerance of analgesia (nausea/vomiting and reported discomfort) | |
| Notes | Both interventions produced a reduction in pain score. "Rescue analgesia" was administered to no participants in the group who received active INF and to 2 participants in the group who received active IVM | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A convenience sample of children aged 7 to 15 years, presenting with clinically deformed closed long‐bone fractures, was identified at triage and invited to join the study" |
| Allocation concealment (selection bias) | Low risk | Quote: "The study packs were randomly allocated in the pharmacy and supplied to the department in blocks of 10, and the next available pack was taken on enrolment of the patient" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Study packs contained either the concentrated fentanyl solution or normal saline solution in identical containers plus a 1‐mL ampoule of morphine (10 mg/mL) or normal saline solution also in identical containers" |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The patient provided a pain score with the visual analogue scale at 0, 5, 10, 20, and 30 minutes after the administration of analgesia. They also completed a second assessment to compare their current pain with the previous rating verbally as 'much better,' 'little better,' 'the same,' 'little worse,' or 'much worse.' The child was blinded to previous scores" |
| Incomplete outcome data (attrition bias) | Low risk | Comment: Of the 67 participants enrolled in the study, 2 were withdrawn (1 participant in each study arm) Quote: "1 child was withdrawn when IV access failed and intramuscular analgesia was administered; 1 child received 1 dose of intranasal fentanyl and withdrew at 5 minutes" |
| Selective reporting (reporting bias) | Low risk | Comment: All of the study's prespecified outcomes of interest in the review have been reported in the prespecified way |
| Other bias | Low risk | Comment: The study appears to be free of other sources of bias |
| Methods | Prospective, double‐blind, randomized, controlled trial at a single site (tertiary paediatric emergency department) in Australia | |
| Participants | 189 patients (3‐15 years of age) with clinically deformed closed long bone fractures were enrolled | |
| Interventions | Intervention 1: SINF (50 mcg/mL) at a dose of 1.5 mcg/kg Intervention 2: HINF (300 mcg/mL) at a dose of 1.5 mcg/kg | |
| Outcomes | Primary outcome measure: reduction in pain using a 100‐mm VAS for participants >7 years or Faces Pain Scale for those participants incapable of using the VAS. Pain intensity was measured at 0, 10, 20 and 30 minutes Secondary outcome measures: occurrence of opiate toxicity (sedation, respiratory or cardiovascular depression) and participant tolerance of analgesia (nausea/vomiting and reported discomfort) | |
| Notes | Both interventions produced a reduction in pain score. "Rescue analgesia" was administered to 42 participants in the SINF group and to 25 participants in the HINF group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Children aged 3–15 years inclusive presenting to the ED with clinically deformed closed long bone fractures were included. The patients were identified by the triage nurse as requiring urgent analgesia" |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomized using a computer‐generated programme in blocks of 10 stratified with age brackets of 3–5 years, 6–10 years and 11–15 years with allocation made by a sealed envelope in the study pack" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "All patients received an initial standard dose of 1.5 mcg/kg (either SINF or HINF) administered with the MAD device (Wolfe Tory Medical, Salt Lake City, UT, USA) with volumes >0.2 mL alternated between nostrils. A nurse, blinded to the solution of fentanyl administered, undertook observations including pain scores at 0, 10, 20 and 30 min post initial INF dose" |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Outcome measures included pain scores using either a 100 mm visual analogue pain scale (VAS) for patients >7 years of age if the patient was deemed capable by the observation nurse, or Faces Pain Scale–Revised (FPS‐R) for those patients incapable of using VAS" |
| Incomplete outcome data (attrition bias) | Low risk | Comment: 199 participants were enrolled in this study. 10 were withdrawn during the study (HINF, N = 6; SINF, N = 4) for the following reasons: no written consent, no pain score documented, prehospital administration of opiates, INF not required |
| Selective reporting (reporting bias) | Low risk | Comment: All of the study's prespecified outcomes of interest in the review have been reported in the prespecified way |
| Other bias | Low risk | Comment: The study appears to be free of other sources of bias |
ED: Emergency department.
HINF: High concentration intranasal fentanyl.
IMM: Intramuscular morphine.
INF: Intranasal fentanyl.
IVM: Intravenous morphine.
SINF: Standard concentration intranasal fentanyl.
VAS: Visual analogue scale.
Characteristics of excluded studies [ordered by year of study]
| Study | Reason for exclusion |
| Preemptive treatment of children in pain in advance of lumbar puncture or bone marrow aspiration | |
| Preemptive treatment of children in pain requiring a change in burn dressing | |
| Preemptive treatment of children in pain during catheterization for voiding cystourethrography |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Intranasal fentanyl versus intravenous morphine in the emergency department treatment of severe painful sickle cell crises in children: study protocol for a randomized controlled trial |
| Methods | Randomized, double‐blind, double‐dummy, active control trial |
| Participants | Children (weighing more than 10 kg) between 1 year and 21 years of age with severe painful sickle cell crisis |
| Interventions | Each participant will receive a single active agent and a single placebo via intravenous and intranasal routes |
| Outcomes | The primary endpoint is severity of pain scored at 10 minutes from administration of study medications. Secondary endpoints include pain severity measured at 0, 5, 15, 20, 30, 60 and 120 minutes after administration of analgesia, proportion of participants requiring rescue analgesia and incidence of adverse events |
| Starting date | March 2012 |
| Contact information | Michael Joseph Barrett: [email protected] |
| Notes | Trial Registration: Current Controlled Trials ISRCTN67469672 and EudraCT no. 2011‐005161‐20 |

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
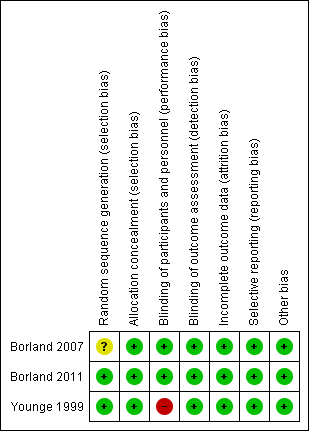
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Intranasal fentanyl compared with intravenous morphine for the management of acute moderate to severe pain in children | ||||||
| Patient or population: children (aged < 18 years) with acute severe pain Settings: emergency department Intervention: intranasal fentanyl Comparison: intravenous morphine | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Intravenous morphine | Intranasal fentanyl | |||||
| Pain reduction (mean VAS) Pain assessed before analgesia (0 min) and at 5, 10, 20 and 30 min after analgesia | 0 min = 67 5 min = 42 10 min = 41 20 min = 35 30 min = 33 | 0 min = 68 5 min = 55 10 min = 46 20 min = 37 30 min = 37 | 67 participants (1 study) | ⊕⊕⊕⊕ | Given no statistically significant difference between treatment arms, VAS scores were combined to form an overall VAS score for each time point. Combined VAS scores produced statistically significant reductions in pain at 5, 10 and 20 min after analgesia | |
| Respiratory depression | No cases were reported in this study | No cases were reported in this study | 67 participants (1 study) | ⊕⊕⊕ | Dosage regimen for this study was calculated for 3 weight intervals. Inclusion of 21 children outside the weight intervals (1 less than 20 kg and 20 greater than | |
| Hypotension | No cases were reported in this study | No cases were reported in this study | 67 participants (1 study) | ⊕⊕⊕ | Dosage regimen for this study was calculated for 3 weight intervals. Inclusion of 21 children outside the weight intervals (1 less than 20 kg and 20 greater than | |
| Decreased level of consciousness | No cases were reported in this study | No cases were reported in this study | 67 participants (1 study) | ⊕⊕⊕ | Dosage regimen for this study was calculated for 3 weight intervals. Inclusion of 21 children outside the weight intervals (1 less than 20 kg and 20 greater than | |
| Intolerance to analgesia | 1 participant complained of a momentary flush at the IV site following administration of morphine | 4 participants; 3 participants reported a "bad taste" following INF administration, 1 participant vomited 20 min following INF administration | 67 participants (1 study) | ⊕⊕⊕⊕ | ||
| Use of ED "rescue" analgesia | 1 participant required 5 additional doses of IV morphine (protocol violation) | 1 participant required 6 additional doses of INF (protocol violation) | 67 participants (1 study) | ⊕⊕⊕ | Protocol violation in control and intervention arms of this trial. As per protocol, participants should receive only 4 additional doses of either agent | |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| ED: Emergency department. IV: Intravenous. INF: Intranasal fentanyl. VAS: Visual analogue scale. | ||||||
| 0 min | 5 min | 10 min | 20 min | 30 min | |
| Intravenous morphine (mm) | 67 | 42 | 41 | 35 | 33 |
| Intranasal fentanyl (mm) | 68 | 55 | 46 | 37 | 37 |
| Difference (mm) (95% CI) | ‐1 (‐12 to 9) | ‐13 (‐23 to ‐3) | ‐5 (‐16 to 7) | ‐2 (‐13 to 10) | ‐4 (‐16 to 8) |
| Borland 2007: Mean visual analogue score (mm) over time. | |||||
| SINF | HINF | P value | |
| Before analgesia | 80.0 (60.0‐95.5) | 77.5 (60.0‐100) | 0.881 |
| 10 min | 49.5 (26.5‐68.5) | 43.0 (15.2‐66.0) | 0.176 |
| 20 min | 27.5 (18.5‐56.5) | 35.0 (9.0‐57.0) | 0.758 |
| 30 min | 20.0 (10.0‐46.0) | 21.5 (4.75‐51.0) | 0.662 |
| Borland 2011: Median visual analogue pain score (mm) over time. | |||
| 0 min | 5 min | 10 min | 20 min | 30 min | |
| Intranasal fentanyl | 4 | 3 | 1 | 1 | 1 |
| Intramuscular morphine | 4 | 3 | 2 | 2 | 1 |
| Younge 1999: Median pain score (Wong Baker Faces, ordinal scoring 0‐5) over time. | |||||

