Fentanilo intranasal para el tratamiento del dolor agudo en niños
Información
- DOI:
- https://doi.org/10.1002/14651858.CD009942.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 10 octubre 2014see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Anestesia
- Copyright:
-
- Copyright © 2015 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Conceiving of the review: Ronan O'Sullivan (ROS)
Co‐ordinating the review: Adrian Murphy (AM)
Undertaking manual searches: AM
Screening search results: AM
Organizing retrieval of papers: Siobhan McCoy (SMC)
Screening retrieved papers against inclusion criteria: John Cronin (JC) and Michael J Barrett (MB)
Appraising quality of papers: JC and MB
Abstracting data from papers: Jeffrey Hom (JH) and SMC
Writing to authors of papers for additional information: AM
Providing additional data about papers: AM
Obtaining and screening data on unpublished studies: AM
Managing data for the review: AM
Entering data into Review Manager (RevMan 5.2): JC and Nandini Kandamany (NK)
Analysing RevMan statistical data: Timothy Grant (TG)
Performing other statistical analysis not using RevMan: TG
Interpreting data: ROS and Abel Wakai (AW)
Making statistical inferences: TG
Writing the review: AM
Securing funding for the review: ROS
Performing previous work that served as the foundation of the present study: AM
Serving as guarantor for the review (one review author): ROS
Taking responsibility for reading and checking the review before submission: ROS and AM
Sources of support
Internal sources
-
National Children's Research Centre, Ireland.
External sources
-
No sources of support supplied
Declarations of interest
Adrian Murphy: none known.
Ronan O'Sullivan: none known.
Abel Wakai: none known.
Timothy Grant: I began working at ICON Clinical Research on December 1, 2012. None of my work at ICON involves related areas, and all work is performed independently of the work I had previously completed in preparation of this review. My current work involves primarily oncology and vaccines, and no activities focus on anaesthesia or pain management. Neither I, Tim Grant, nor my employer, ICON Clinical Research, is in a position to benefit financially from this review; I have no conflicts of interest. This work was performed independently of my employment, and this work is related in no way to my employer.
Michael J Barrett: none known.
John Cronin: none known.
Siobhan C McCoy: none known.
Jeffrey Hom: none known.
Nandini Kandamany: none known.
Acknowledgements
We would like to thank Andy Smith (content editor), Cathal Walsh (statistical editor) and David Herd and Meredith Borland (peer reviewers) for help and editorial advice provided during preparation of the protocol for the systematic review and the full systematic review.
Version history
| Published | Title | Stage | Authors | Version |
| 2014 Oct 10 | Intranasal fentanyl for the management of acute pain in children | Review | Adrian Murphy, Ronan O'Sullivan, Abel Wakai, Timothy S Grant, Michael J Barrett, John Cronin, Siobhan C McCoy, Jeffrey Hom, Nandini Kandamany | |
| 2012 Jul 11 | Intranasal fentanyl for the management of acute pain in children | Protocol | Adrian Murphy, Ronan O'Sullivan, Abel Wakai, Timothy Grant, Michael J Barrett, John Cronin, Siobhan C McCoy, Jeffrey Hom | |
Differences between protocol and review
We made the following changes to the published protocol (Murphy 2012).
-
Byline: Nandini Kandamany joined the review team.
-
Searching other resources: We did not contact pharmaceutical companies.
-
In the published protocol for this review, we intended to document the following in the 'Summary of findings' (SoF) table.
-
Pain score reduction (using age‐appropriate validated pain scales) following administration of INF at multiple time points.
-
Occurrence of adverse events post INF administration.
-
Acceptability of INF administration among participants.
-
Use of 'rescue analgesia' post INF administration.
-
Participant and parental satisfaction as defined by study authors.
-
Cost as defined by study authors.
-
Mortality
-
However, the included studies did not document participant/parental satisfaction nor cost; therefore these were not included in the SOF table.
Notes
Feedback incorporated August 2015 (see Feedback)
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Child; Humans;
PICO

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
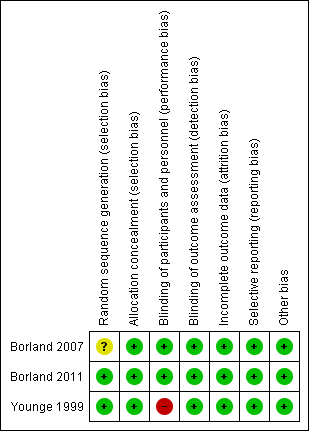
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Intranasal fentanyl compared with intravenous morphine for the management of acute moderate to severe pain in children | ||||||
| Patient or population: children (aged < 18 years) with acute severe pain Settings: emergency department Intervention: intranasal fentanyl Comparison: intravenous morphine | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Intravenous morphine | Intranasal fentanyl | |||||
| Pain reduction (mean VAS) Pain assessed before analgesia (0 min) and at 5, 10, 20 and 30 min after analgesia | 0 min = 67 5 min = 42 10 min = 41 20 min = 35 30 min = 33 | 0 min = 68 5 min = 55 10 min = 46 20 min = 37 30 min = 37 | 67 participants (1 study) | ⊕⊕⊕⊕ | Given no statistically significant difference between treatment arms, VAS scores were combined to form an overall VAS score for each time point. Combined VAS scores produced statistically significant reductions in pain at 5, 10 and 20 min after analgesia | |
| Respiratory depression | No cases were reported in this study | No cases were reported in this study | 67 participants (1 study) | ⊕⊕⊕ | Dosage regimen for this study was calculated for 3 weight intervals. Inclusion of 21 children outside the weight intervals (1 less than 20 kg and 20 greater than | |
| Hypotension | No cases were reported in this study | No cases were reported in this study | 67 participants (1 study) | ⊕⊕⊕ | Dosage regimen for this study was calculated for 3 weight intervals. Inclusion of 21 children outside the weight intervals (1 less than 20 kg and 20 greater than | |
| Decreased level of consciousness | No cases were reported in this study | No cases were reported in this study | 67 participants (1 study) | ⊕⊕⊕ | Dosage regimen for this study was calculated for 3 weight intervals. Inclusion of 21 children outside the weight intervals (1 less than 20 kg and 20 greater than | |
| Intolerance to analgesia | 1 participant complained of a momentary flush at the IV site following administration of morphine | 4 participants; 3 participants reported a "bad taste" following INF administration, 1 participant vomited 20 min following INF administration | 67 participants (1 study) | ⊕⊕⊕⊕ | ||
| Use of ED "rescue" analgesia | 1 participant required 5 additional doses of IV morphine (protocol violation) | 1 participant required 6 additional doses of INF (protocol violation) | 67 participants (1 study) | ⊕⊕⊕ | Protocol violation in control and intervention arms of this trial. As per protocol, participants should receive only 4 additional doses of either agent | |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| ED: Emergency department. IV: Intravenous. INF: Intranasal fentanyl. VAS: Visual analogue scale. | ||||||
| 0 min | 5 min | 10 min | 20 min | 30 min | |
| Intravenous morphine (mm) | 67 | 42 | 41 | 35 | 33 |
| Intranasal fentanyl (mm) | 68 | 55 | 46 | 37 | 37 |
| Difference (mm) (95% CI) | ‐1 (‐12 to 9) | ‐13 (‐23 to ‐3) | ‐5 (‐16 to 7) | ‐2 (‐13 to 10) | ‐4 (‐16 to 8) |
| Borland 2007: Mean visual analogue score (mm) over time. | |||||
| SINF | HINF | P value | |
| Before analgesia | 80.0 (60.0‐95.5) | 77.5 (60.0‐100) | 0.881 |
| 10 min | 49.5 (26.5‐68.5) | 43.0 (15.2‐66.0) | 0.176 |
| 20 min | 27.5 (18.5‐56.5) | 35.0 (9.0‐57.0) | 0.758 |
| 30 min | 20.0 (10.0‐46.0) | 21.5 (4.75‐51.0) | 0.662 |
| Borland 2011: Median visual analogue pain score (mm) over time. | |||
| 0 min | 5 min | 10 min | 20 min | 30 min | |
| Intranasal fentanyl | 4 | 3 | 1 | 1 | 1 |
| Intramuscular morphine | 4 | 3 | 2 | 2 | 1 |
| Younge 1999: Median pain score (Wong Baker Faces, ordinal scoring 0‐5) over time. | |||||

