Cirugía ovárica para el alivio de síntomas en las pacientes con síndrome de ovario poliquístico
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | A randomised controlled trial | |
| Participants | 60 women attending the outpatient infertility clinic with a diagnosis of CC‐resistant PCOS at Ain Shams University Maternity Hospital, Cairo, Egypt between February 2010 and September 2010 | |
| Interventions | 30 women underwent unilateral ovarian drilling and 30 underwent bilateral ovarian drilling | |
| Outcomes | The primary outcome was documented ovulation through a midluteal serum progesterone > 3 ng/ml 3 months after laparoscopy No harms reported. | |
| Notes | Funding source: Not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible due to study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 126 women with PCOS were randomised from March 2006 until February 2008, between the ages of 15 and 45 years, with a history of infertility for at least 1 year and 3 treatment cycles with no response to CC (CC‐resistant), conducted in Tehran, Iran | |
| Interventions | Participants received metformin treatment (n = 63) or underwent LOD (n = 63) | |
| Outcomes | The primary outcome measure was menstrual regularity. The levels of FSH, LH, free testosterone and the level of hirsutism assessed using the Ferriman Gallwey score were included. No harms reported. | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Low risk | The groups were allocated using serially‐numbered opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible with study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | All randomised women were analyzed |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | The study comprised 163 women (aged 18 – 32 years) with CC‐resistant PCOS among those attending the Outpatient Clinic at the Mansoura University Hospitals, Mansoura, Egypt, and a private practice setting in the period from January 2005 to January 2007 | |
| Interventions | Participants were randomly allocated to either treatment with ultrasound‐guided transvaginal needle ovarian drilling (UTND; n = 82) or laparoscopic electrosurgery ovarian drilling (n = 81) | |
| Outcomes | Normal menstruation, hirsutism and acne, testosterone. No harms reported. | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "computer‐generated random table" |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible with study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 146 CC‐resistant PCOS women who were attending the infertility clinic were recruited from Zagazig University Hospital, Zagazig, Egypt. Time‐frame not stated | |
| Interventions | Metformin (850 mg (1 tablet daily) + letrozole (n = 73)) versus LOD (n = 73). Metformin dosage was increased after 1 week up to 1700 mg/day (2 tablets daily) and only stopped once pregnancy was confirmed. Letrozole was added from day 3 each month of spontaneous or induced bleeding, and continued for 5 days. LOD was 4 drills to each ovary | |
| Outcomes | Hormonal profile including testosterone, fasting glucose, glu/insulin ratio, regularity of periods, BMI No harms reported. | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "computer‐generated random numeric table" |
| Allocation concealment (selection bias) | Low risk | "concealed in sealed dark envelopes" |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible with study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 50 women were recruited from fertility clinics in New Zealand between mid‐1996 and late 1999 with the following inclusion criteria: 1) 20 ‐ 38 years; 2) infertility > 12 months; 3) Clomiphene resistance; 4) BMI < 33; 5) PCOS | |
| Interventions | Women were randomised into LOD (n = 29) (10 holes per ovary) versus ovulation induction with gonadotrophin (metrodin HP (Serono) or FSH (Puregon)) (n = 21) | |
| Outcomes | Hirsutism, acne. Testosterone pre‐ and post‐LOD, not compared to medical arm. BMI stated as no difference but not quantified Participants were given questionnaires regarding acceptability and convenience of both procedures. No harms reported. | |
| Notes | Funding source: "Supported in part by Auckland Medical Research Foundation, grant 81310" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Computer generated sequences" |
| Allocation concealment (selection bias) | Unclear risk | Randomisation in "sealed opaque envelopes" |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible with study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | 3 withdrawals out of 50 |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 286 women with CC‐resistant PCOS attending Department of Obstetrics and Gynecology of the University of Naples ‘‘Federico II’’, Italy. Age 18 ‐ 40 years | |
| Interventions | Women were randomised to either conventional LOD (123 women)or Transvaginal Hydrolaparoscopy (123 women). | |
| Outcomes | Ovarian adhesion formation. | |
| Notes | Study funding: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Two hundred and forty‐six patients were randomized into two groups in a 1:1 ratio by use of a randomization list generated by a computer with blocks of 4". |
| Allocation concealment (selection bias) | Low risk | The allocation sequence was concealed from the researchers, who enrolled and assessed the participants and attached a sequentially‐numbered, opaque, sealed, and stapled envelope containing the allocated treatment |
| Blinding of participants and personnel (performance bias) | High risk | Participants and surgeon were not blinded to the procedure performed because concealment was not possible due to the differences in the procedures |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | Minimal attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | The study was conducted in the Women's Health Center in Cairo, Egypt from May 2007 to September 2008. 200 women were assessed for eligibility, 110 included in the study | |
| Interventions | Participants were randomly allocated to diagnostic laparoscopy plus metformin therapy (group 1, n = 55) or laparoscopic ovarian drilling (group 2, n = 55) | |
| Outcomes | Menstrual cycle regularity, testosterone levels, fasting glucose to insulin ratio, BMI. No harms reported. | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed using a "computer‐generated random numbers table" |
| Allocation concealment (selection bias) | Low risk | Allocation concealment was done using "serially numbered opaque envelopes. The patient's allocation was not changed after opening the envelope" |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible with study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | The study population comprised 282 women with CC‐resistant PCOS attending the Outpatient Clinic in Mansoura University Hospital, Mansoura, Egypt, and a private practice setting from September 2005 to February 2009. Participants in Group A (n = 138) received combined metformin–CC for up to 6 cycles and participants in group B underwent LOD (n = 144) with 6 months follow‐up | |
| Interventions | In group A, all participants received metformin for 5 days starting from day 3 of spontaneous or induced menstruation. In the LOD group (group B), laparoscopy was performed using the 3‐puncture technique. Each ovary was cauterised at 4 points, each for 4 seconds at 40 W for a depth of 4 mm with a mixed current, using a monopolar electrosurgical needle | |
| Outcomes | Resumption of regular menstruation, ovulation rate, mid‐cycle endometrial thickness, pregnancy and miscarriage rates. No intra‐operative or post‐operative complications in either group. | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The random sequence was by "computer‐generated random numeric table" |
| Allocation concealment (selection bias) | Low risk | "Opaque envelopes were numbered and sealed containing the allocation information given to a nurse who assigned the patients to study arms of treatment" |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible with study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | The study comprised 260 women with CC‐resistant PCOS among those attending the Outpatient Clinic in Mansoura University Hospitals, Mansoura, Egypt, and a private practice setting from August 2006 to March 2009 | |
| Interventions | Group A (n = 128) received 2.5 mg letrozole daily for 5 days for up to 6 cycles. Group B (n = 132) underwent LOD with 6 months follow‐up. In letrozole group (group A), treatment continued for up to 6 cycles. In LOD group (group B), laparoscopy was performed using 3‐puncture technique. Each ovary was cauterised at 4 points, each for 4 seconds at 40 W for a depth of 4 mm with a mixed current, using a monopolar electrosurgical needle. Follow‐up continued for 6 months after the procedure | |
| Outcomes | Resumption of regular menstruation, ovulation rate, pregnancy, miscarriage, live birth rates and midcycle endometrial thickness. No operative complications developed, No multiple pregnancies or OHSS in either group. | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Women were randomized according to a computer‐generated random numeric table prepared by an independent statistician" |
| Allocation concealment (selection bias) | Low risk | "concealment of treatment allocation by use of sealed opaque envelopes that were given to a third party (nurse) who assigned patients to study arms; group A (letrozole) or B (LOD)". |
| Blinding of participants and personnel (performance bias) | High risk | "the treatment was revealed to both the investigator and the patient" |
| Blinding of outcome assessment (detection bias) | Low risk | "the radiologist who performed transvaginal ultrasound follow up assessment was blinded to the treatment groups" |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 35 infertile CC‐resistant women with PCOS were prospectively randomised in 2 groups and evaluated from January 2000 through January 2004. Conducted in Suleyman Demireal University Hospital, Isparta, Turkey | |
| Interventions | 17 women underwent laparoscopic ovarian drilling with a multi‐needle intervention( LOMNI) and 18 women received step‐up ovulation induction treatment with recombinant FSH for ovulation induction in addition to intrauterine insemination | |
| Outcomes | Cycle regularity, pregnancy rate, OHSS and cost | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Computer generated random sequence" |
| Allocation concealment (selection bias) | Low risk | Allocated using "sealed opaque envelopes" prior to their surgery |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible with study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | Although 1 woman in the LOMNI group and 2 women in the ovulation induction group were lost to follow‐up, their pregnancy results were available and they all received telephone interviews at the end of the follow‐up period |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 50 women who were CC‐resistant were recruited between February 2003 and May 2004, conducted in 2 university hospitals in Naples, Italy | |
| Interventions | The participants were randomised to clomiphene + metformin (6 cycles) (n = 25) versus LOD alone (n = 25) and followed up for 6 months. LOD was by 3 ‐ 6 punctures of 3 mm diameter and 4 ‐ 5 mm depth, for 2 ‐ 3 seconds at 40 W) | |
| Outcomes | Amenorrhoea at cycle day 35. No operative complications were identified, no drug‐related adverse effects resulting in treatment discontinuation. | |
| Notes | Funding source: "Authorship and contribution to the article is limited to the 8 authors indicated. There was no outside funding or technical assistance with the production of this article" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization |
| Allocation concealment (selection bias) | Low risk | "concealed in sealed dark envelopes until intervention was assigned" |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible with study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | 3 were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 44 women with PCOS were recruited between June 2005 and June 2007 from an Obstetrics and Gynaecology clinic in New Dehli, India | |
| Interventions | 22 participants underwent unilateral ovarian drilling and 22 underwent bilateral ovarian drilling. The number of drilling sites in each ovary was limited to 5 | |
| Outcomes | The clinical and biochemical response, ovulation and menstrual regularity over a follow‐up period of 1 year were compared. Tubo‐ovarian adhesion rate was compared during caesarean section or during repeat laparoscopy | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Mentioned as randomly allocated but not stated how |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible with study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 43 women were recruited from a gynaecology clinic in New Delhi, India, between January 2006 to 2009, all with CC‐resistant PCOS and subfertility | |
| Interventions | Recruits were randomised into LOD (unilateral, 5 holes) (n = 21) vs rosiglitazone (n = 23) at a dose of 4 mg twice daily and CC at a dose of 100 mg daily from the 3rd day of the period for 5 days | |
| Outcomes | Hormonal profile including testosterone, glucose insulin ratio, ovulation, pregnancy rate. No OHSS in either group. | |
| Notes | Funding source: Not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization |
| Allocation concealment (selection bias) | Low risk | "sealed envelope containing numbers from the computer generated random table" |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible with study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 121 women with PCOS attending the infertility clinic of Al‐Zahra Hospital in Rasht, Guilan Province, Iran | |
| Interventions | Comparison between bilateral and unilateral ovarian drilling | |
| Outcomes | FSH, LH and free testosterone levels before and after surgery, responses on ovulation and pregnancy rates. Testosterone levels included No harms reported. | |
| Notes | Study Funding: "The authors thank the Vice Chancellor for Research of Guilan University of Medical Sciences for funding this project" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A randomization list was generated using blocked sample randomizations |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible due to study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | The study was conducted from January 2004 through September 2007 in the infertility unit of Al‐Hammadi Specialized Hospital, Riyadh, Saudi Arabia. 82 women with anovulatory infertility associated with PCOS, who had been CC‐resistant, underwent LOD to assess the optimal number of punctures to be applied to ovarian tissue | |
| Interventions | Women who met inclusion criteria (and had no exclusions) were randomly assigned to 1 of the 5 treatment groups (1:1:1:1:1 ratio). Each randomization number corresponded with 1 of the 5 possible interventions (Gp1: 2 punctures & 300 J; Gp 2: 3 punctures & 450 J; Gp 3: 4 punctures & 600 J; Gp 4: 5 punctures & 750 J; and Gp 5: 6 ‐ 8 punctures & > 900 J). There were 17 cases in groups 3 and 4, and 16 cases in groups 1, 2, and 5 | |
| Outcomes | Menstrual regularity, testosterone, FAI at 6 months follow‐up. No harms reported. | |
| Notes | Due to the multiple group comparisons, for analysis purposes, the outcomes of those with 2 punctures were compared to those with 4 punctures (considered dose for LOD) ‐ i.e., Gp 3 (LOD with 4 punctures) vs Gp 1 (2 punctures) Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Low risk | Labelling of the randomization number was done by a person not involved with the trial |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible due to study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | 6 were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 20 women with CC‐resistant PCOS were recruited in the Department of Obstetrics and Gynaecology of the All India Institute of Medical Sciences, New Delhi, India | |
| Interventions | Group I (n = 10) had unipolar ovarian drilling done by unipolar diathermy needle at power settings of 30 ‐ 40 watts. Group II (n = 10) had bipolar ovarian drilling done by bipolar diathermy needle at power settings of 40 ‐ 50 watts | |
| Outcomes | Menstrual regularity at 3 months, hormonal profile including testosterone, Glucose insulin ratio, pregnancy rate, ovulation rate. No harms reported. | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "computerised random table" |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible due to study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | High risk | Baseline values of glucose insulin ratio were significantly different between groups despite randomization |
| Methods | A randomised controlled trial | |
| Participants | 34 women diagnosed with PCOS with infertility for more than 2 years in Department of Obstetrics and Gynaecology, Mie University School of Medicine, Mie, Japan. Time frame not stated | |
| Interventions | In Group A (n = 17) laparoscopic ovarian drilling was performed using Harmonic scalpel. | |
| Outcomes | Hormonal profile including testosterone levels, menstrual regularity. No harms reported. | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly allocated". |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible due to study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 17 women with CC‐resistant PCOS were recruited from the Division of Endocrinology and Infertility, Inonu University of Medicine, Malatya, Turkey. Time frame not stated | |
| Interventions | 17 women were randomly assigned to either Group A (ovarian electrocautery; n = 8) or group B (GnRHa + low‐dose OCP (desogestrel 0.15 mg + ethinyl estradiol = 35 mcg); n = 9). 10 ‐ 12 cautery points were applied to each ovary | |
| Outcomes | Hormonal profile including testosterone. No harms from either modality. | |
| Notes | Low‐dose OCP was given from the beginning of 1st day of induced menstruation and continued for 3 months Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Sequential assignment based on table of random numbers". |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible due to study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | The study was performed in the Department of Obstetrics and Gynaecology and Fertility care unit, Faculty of Medicine, Mansoura University Hospital, Egypt, from January 2003 to December 2006. 87 women were recruited | |
| Interventions | Participants were allocated to either unilateral (Group A: n = 43) or bilateral (Group B: n = 44) laparoscopic ovarian drilling | |
| Outcomes | Testosterone concentrations, FSH, LH, post‐operative nausea, vomiting and pain; ovulation, pregnancy, and miscarriage rates | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated by an independent investigator blinded to treatment groups |
| Allocation concealment (selection bias) | Low risk | "using the closed envelope method" |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible due to study design |
| Blinding of outcome assessment (detection bias) | Low risk | "An independent assessor blinded to the treatment groups obtained the scores". |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 120 women with polycystic ovary syndrome and clomiphene citrate resistance between January 2007 and December 2009 in the Women's Health Centre and Physiology Department, Assiut University, Egypt. | |
| Interventions | Patients were assigned randomly to 2 groups of 60 women each. Group A received an adjusted thermal dose based on ovarian volume with use of a new model for dose calculation (60 J/cm3 of ovarian tissue), and group B received 600 J per ovary through 4 ovarian holes regardless of size (traditional form of LOD). 1 month afterward, the hormonal profile was re‐evaluated, and second‐look laparoscopy was performed in women who had not conceived by 6 months to evaluate adnexal adhesions | |
| Outcomes | Menstrual cycle regularity, hormonal profile including testosterone, BMI and adhesions | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was done using a computer generated random table" |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible due to study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | 5 lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 80 women with PCOS and CC–resistant infertility between January 2006 and June 2008 in Shen‐Zen City Materninty and Child Healthcare Hospital, Shen‐Zhen, China. Participants underwent ultrasound‐guided transvaginal ovarian interstitial yttrium aluminium garnet laser treatment. Participants were divided randomly into 4 groups (A, B, C, and D) | |
| Interventions | Group A (n = 20), 1 coagulation point per ovary; group B (n = 20), 2 points; group C (n = 20), 3 points; group D (n = 20), 4 to 5 points | |
| Outcomes | Hormonal profile including testosterone and regularity of menstrual pattern. Follow‐up period was 6 months post‐operation. No complications occurred. | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "80 random numbers generated by computer were divided randomly into 4 groups: A, B, C, and D". |
| Allocation concealment (selection bias) | Low risk | The random allocation sequence was concealed in a closed, dark‐coloured envelope until the surgeries were assigned, and specifically just before entering the operating room. Randomisation occurred after participants agreed to join the study |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible due to study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
| Methods | A randomised controlled trial | |
| Participants | 62 infertile women with PCOS from University hospitals and a private day surgery unit in Naples, Italy. Time frame not stated | |
| Interventions | In group A (n = 32), ovarian drilling was performed by mini‐laparoscopy under local anaesthesia plus conscious sedation. In group B (n = 30), the control group underwent ovarian drilling by the traditional laparoscopic approach under general anaesthesia | |
| Outcomes | Hormonal profile including testosterone levels, pain scores post‐surgery (follow‐up period of 1 year) | |
| Notes | Funding source: Not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly allocated". |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) | High risk | Not stated but not possible due to study design |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) | Low risk | No attrition |
| Selective reporting (reporting bias) | Low risk | None detected |
| Other bias | Low risk | None detected |
BMI: body mass index
CC: clomiphene citrate
FAI: free androgen index
FSH: follicle stimulating hormone
GnRHa: gonadotrophin‐releasing hormone
J: joule(s)
LH: luteinising hormone
OCP: oral contraceptive pill
OHSS: ovarian hyperstimulation syndrome
W: watt(s)
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Fertility outcomes only | |
| Testosterone outcomes not reported | |
| Fertility outcomes only. Compared LOD versus continuing with clomiphene | |
| Reproductive outcomes only. | |
| Not an RCT | |
| Not an RCT | |
| Not a true randomised trial as randomization was by 'alternating' treatment protocol | |
| Ovarian reserves only | |
| Ovarian reserves only | |
| Ovarian reserves only | |
| Study retracted |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Comparison between laproscopic ovarian diathermy and urinary purified fsh in women with clomiphene citrate‐resistant polycystic ovarian syndrome: a randomized controlled trial |
| Methods | 210 women with clomiphene‐resistant PCOS will be randomly divided into 3 equal groups using computer‐generated random numbers. Group 1 will receive combined metformin and FSH, group 2 will have LOD and group 3 will act as the control group with no intervention. |
| Participants | 210 women with clomiphene‐resistant PCOS |
| Interventions | Metforimn and FSH, LOD, no intervention |
| Outcomes | Ovulation, pregnancy |
| Starting date | November 2014 |
| Contact information | |
| Notes |
| Trial name or title | Comparison between letrozole and laparoscopic ovarian drilling in women with clomiphene‐resistant polycystic ovarian syndrome (PCOS) |
| Methods | 140 women with clomiphene‐resistant PCOS will be randomly divided into 2 equal groups using computer‐generated random numbers. Group 1 will receive letrozole, group 2 will have laparoscopic ovarian drilling (LOD) |
| Participants | 140 women with clomiphene‐resistant PCOS |
| Interventions | Letrozole, LOD |
| Outcomes | Ovulation, pregnancy |
| Starting date | November 2014 |
| Contact information | |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Menstrual regularity Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 LOD vs medical interventions, Outcome 1 Menstrual regularity. | ||||
| 1.1 LOD vs Metformin alone | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Menstrual regularity Show forest plot | 5 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2 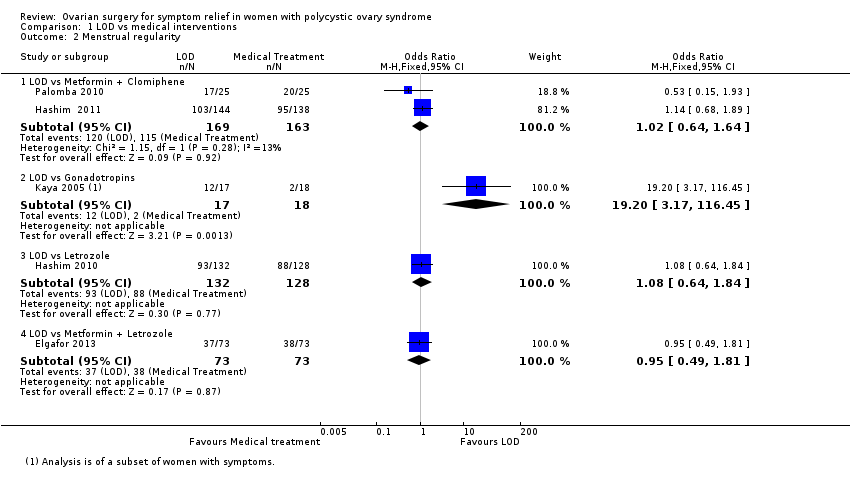 Comparison 1 LOD vs medical interventions, Outcome 2 Menstrual regularity. | ||||
| 2.1 LOD vs Metformin + Clomiphene | 2 | 332 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.64, 1.64] |
| 2.2 LOD vs Gonadotropins | 1 | 35 | Odds Ratio (M‐H, Fixed, 95% CI) | 19.2 [3.17, 116.45] |
| 2.3 LOD vs Letrozole | 1 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.64, 1.84] |
| 2.4 LOD vs Metformin + Letrozole | 1 | 146 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.49, 1.81] |
| 3 Improvement in androgenic symptoms (hirsutism/acne) Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3 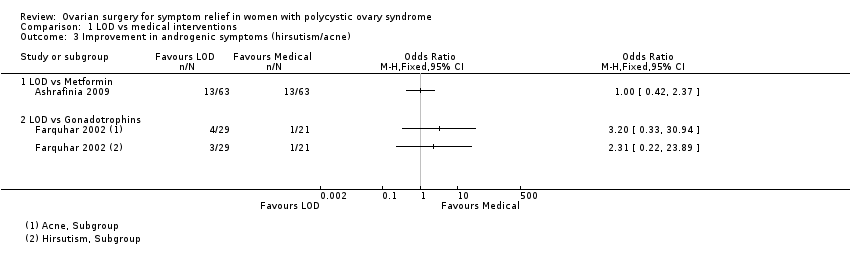 Comparison 1 LOD vs medical interventions, Outcome 3 Improvement in androgenic symptoms (hirsutism/acne). | ||||
| 3.1 LOD vs Metformin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 LOD vs Gonadotrophins | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Harms Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 LOD vs medical interventions, Outcome 4 Harms. | ||||
| 4.1 LOD vs Metformin + Clomiphen | 2 | 332 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.36] |
| 4.2 LOD vs Gonadotrophins | 1 | 33 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.00, 1.61] |
| 5 BMI Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 LOD vs medical interventions, Outcome 5 BMI. | ||||
| 5.1 LOD vs Metformin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 LOD vs Metformin + Letrozole | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Testosterone and free androgen index Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.6  Comparison 1 LOD vs medical interventions, Outcome 6 Testosterone and free androgen index. | ||||
| 6.1 LOD vs Metformin | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 LOD vs GnRHa + OCP | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 LOD vs Metformin + Letrozole | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 LOD versus Rosiglitazone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Fasting Glucose:Insulin Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.7 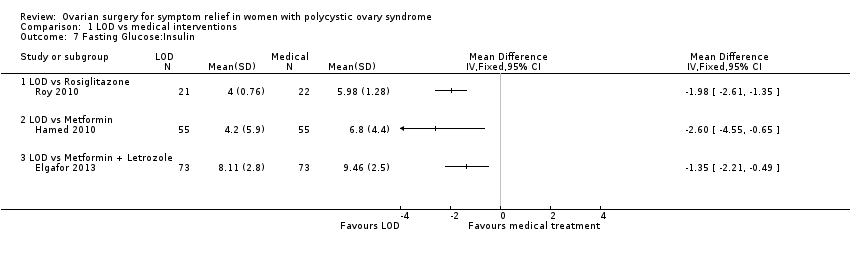 Comparison 1 LOD vs medical interventions, Outcome 7 Fasting Glucose:Insulin. | ||||
| 7.1 LOD vs Rosiglitazone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 LOD vs Metformin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 LOD vs Metformin + Letrozole | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Menstrual regularity Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 LOD vs other surgical interventions, Outcome 1 Menstrual regularity. | ||||
| 1.1 LOD vs Unilateral LOD | 2 | 104 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.62, 3.71] |
| 1.2 LOD vs Ultrasound guided transvaginal ovarian drilling | 1 | 147 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.64, 2.37] |
| 1.3 Laser LOD vs Harmonic Scalpel | 1 | 34 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.13 [0.17, 26.03] |
| 2 Improvement in androgenic symptoms (hirsutism/acne) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2 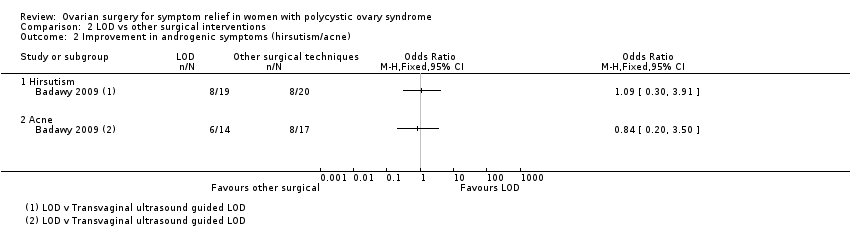 Comparison 2 LOD vs other surgical interventions, Outcome 2 Improvement in androgenic symptoms (hirsutism/acne). | ||||
| 2.1 Hirsutism | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Acne | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Harms: Adhesions Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3 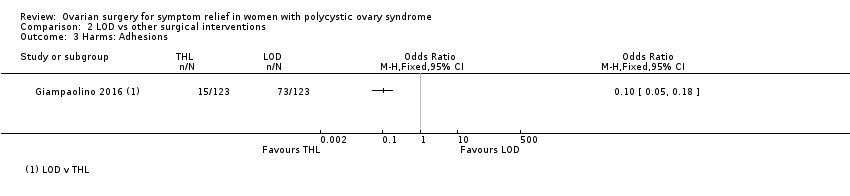 Comparison 2 LOD vs other surgical interventions, Outcome 3 Harms: Adhesions. | ||||
| 4 Testosterone and free androgen index Show forest plot | 6 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.4  Comparison 2 LOD vs other surgical interventions, Outcome 4 Testosterone and free androgen index. | ||||
| 4.1 LOD vs Ultrasound guided transvaginal ovarian drilling | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 LOD versus mini laparoscopy with sedation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 LOD vs unilateral LOD | 3 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Laser LOD vs Harmonic Scalpel | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Menstrual regularity Show forest plot | 2 | 73 | Odds Ratio (M‐H, Fixed, 95% CI) | 16.04 [4.19, 61.34] |
| Analysis 3.1 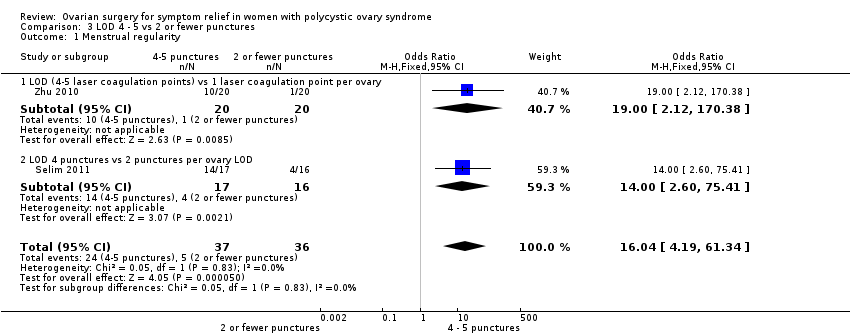 Comparison 3 LOD 4 ‐ 5 vs 2 or fewer punctures, Outcome 1 Menstrual regularity. | ||||
| 1.1 LOD (4‐5 laser coagulation points) vs 1 laser coagulation point per ovary | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 19.0 [2.12, 170.38] |
| 1.2 LOD 4 punctures vs 2 punctures per ovary LOD | 1 | 33 | Odds Ratio (M‐H, Fixed, 95% CI) | 14.0 [2.60, 75.41] |
| 2 Testosterone and free androgen index Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.2  Comparison 3 LOD 4 ‐ 5 vs 2 or fewer punctures, Outcome 2 Testosterone and free androgen index. | ||||
| 2.1 LOD 4‐5 punctures vs 2 or fewer punctures (Testosterone) | 2 | 73 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.12, ‐0.68] |
| 2.2 LOD 4 punctures vs 2 punctures (FAI) | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | ‐1.5 [‐3.21, 0.21] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Menstrual regularity Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.1 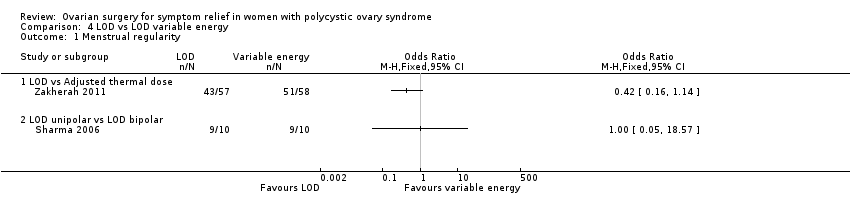 Comparison 4 LOD vs LOD variable energy, Outcome 1 Menstrual regularity. | ||||
| 1.1 LOD vs Adjusted thermal dose | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 LOD unipolar vs LOD bipolar | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Harms Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.2 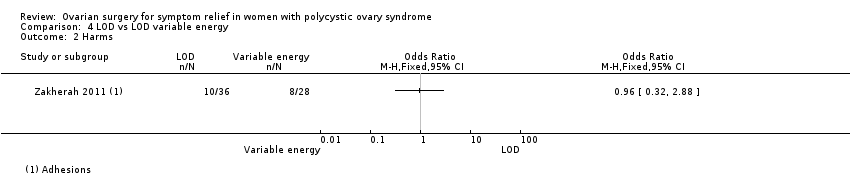 Comparison 4 LOD vs LOD variable energy, Outcome 2 Harms. | ||||
| 3 BMI Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.3  Comparison 4 LOD vs LOD variable energy, Outcome 3 BMI. | ||||
| 4 Testosterone and free androgen index Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.4  Comparison 4 LOD vs LOD variable energy, Outcome 4 Testosterone and free androgen index. | ||||
| 4.1 LOD vs Adjusted thermal dose | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 LOD unipolar vs LOD bipolar | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Metabolic measures Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.5  Comparison 4 LOD vs LOD variable energy, Outcome 5 Metabolic measures. | ||||
| 5.1 LOD (unipolar) vs bipolar | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
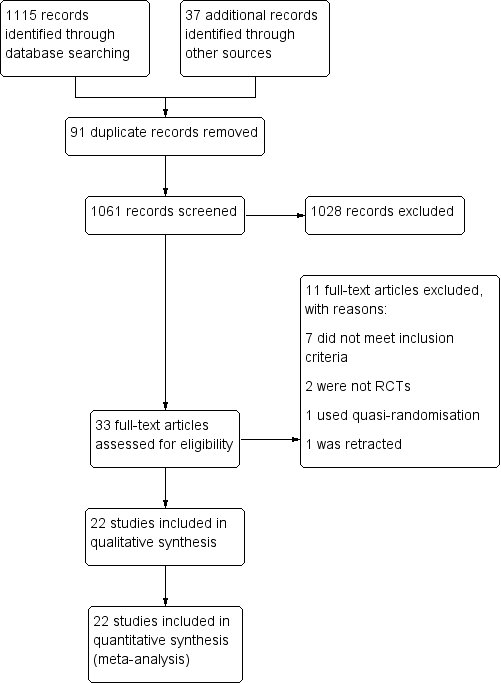
Study flow diagram
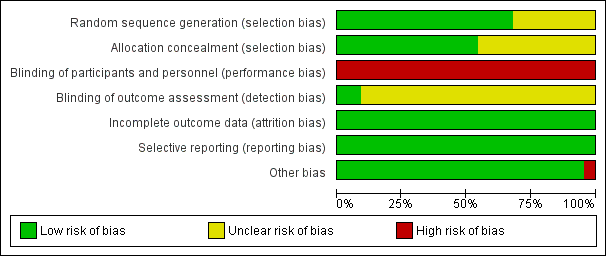
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
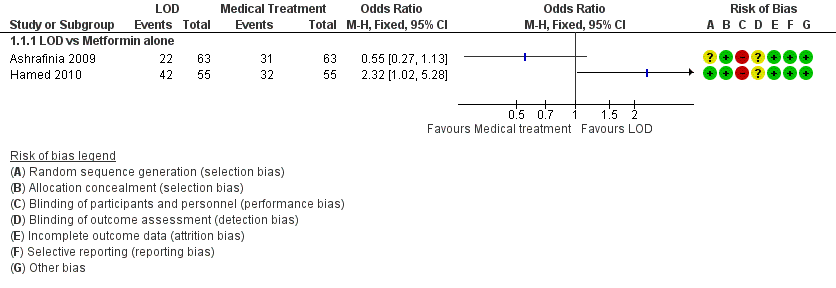
Forest plot of comparison: 1 LOD vs medical interventions, outcome: 1.1 Menstrual regularity.
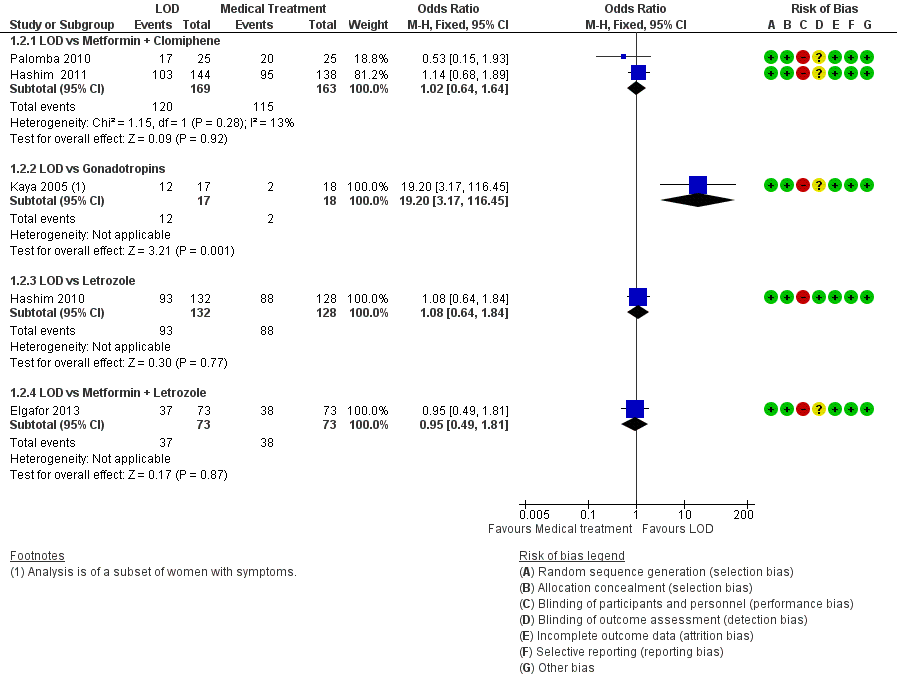
Forest plot of comparison: 1 LOD vs medical interventions, outcome: 1.2 Menstrual regularity.
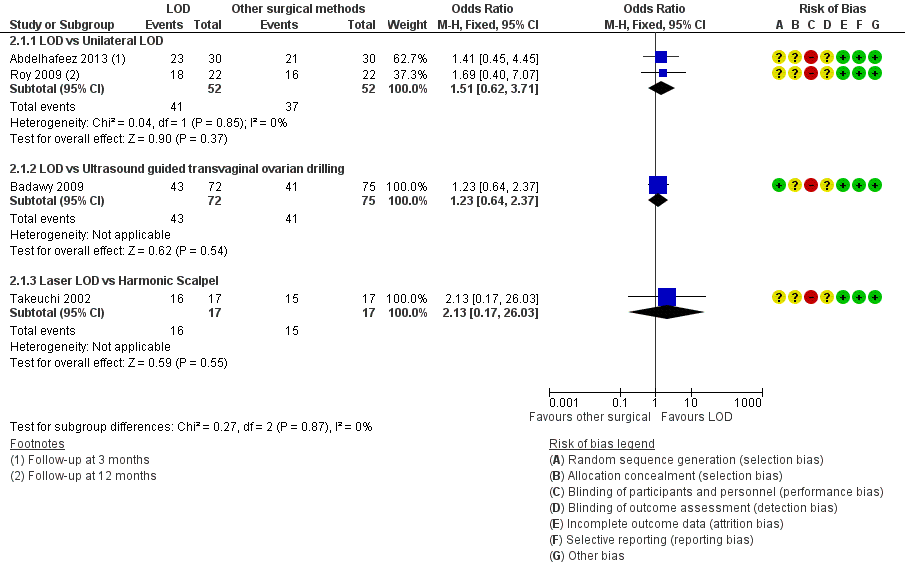
Forest plot of comparison: 2 LOD vs other surgical interventions, outcome: 2.1 Menstrual regularity.
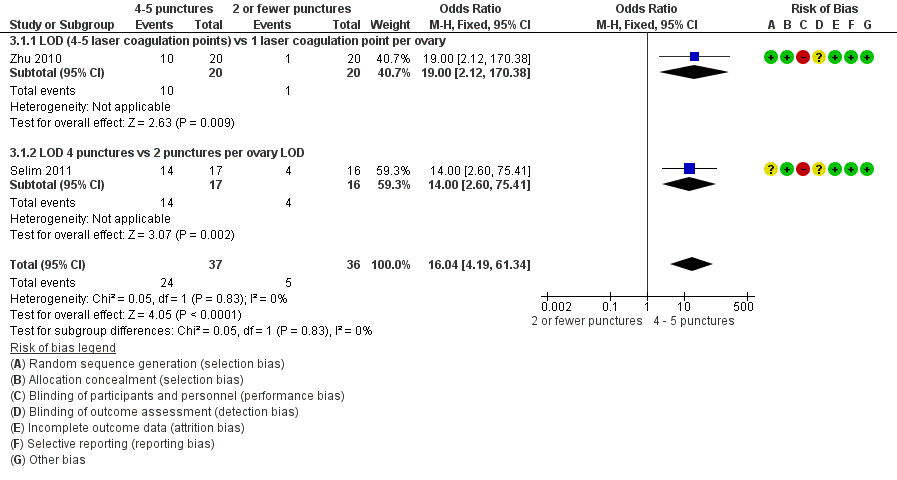
Forest plot of comparison: 3 LOD 4 ‐ 5 vs 2 or fewer punctures, outcome: 3.1 Menstrual regularity.

Forest plot of comparison: 4 LOD vs LOD variable energy, outcome: 4.1 Menstrual regularity.
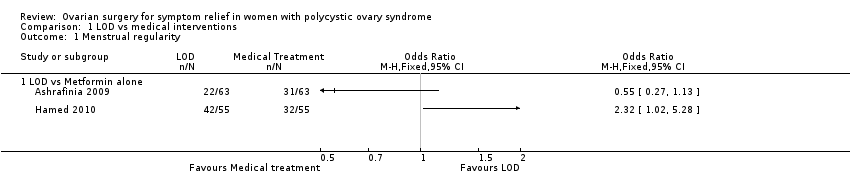
Comparison 1 LOD vs medical interventions, Outcome 1 Menstrual regularity.

Comparison 1 LOD vs medical interventions, Outcome 2 Menstrual regularity.
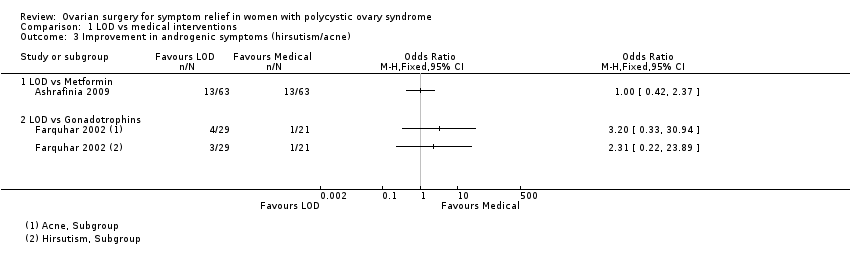
Comparison 1 LOD vs medical interventions, Outcome 3 Improvement in androgenic symptoms (hirsutism/acne).
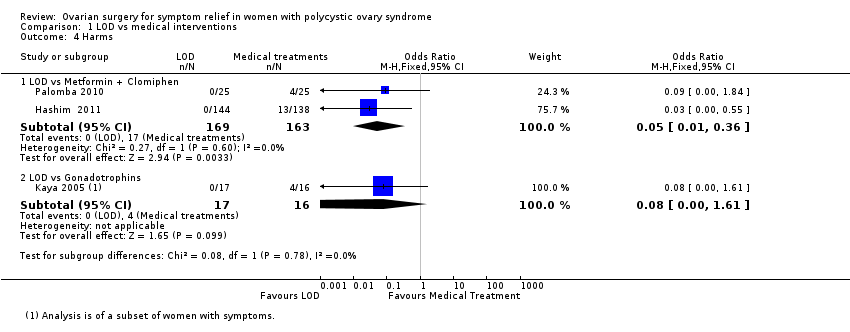
Comparison 1 LOD vs medical interventions, Outcome 4 Harms.
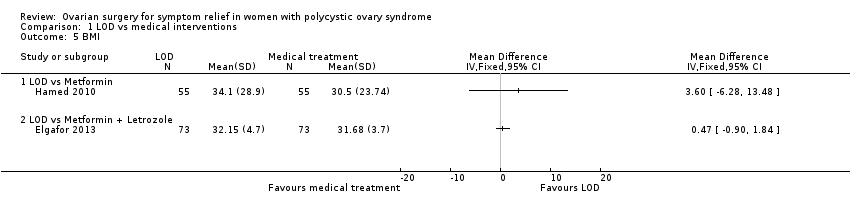
Comparison 1 LOD vs medical interventions, Outcome 5 BMI.

Comparison 1 LOD vs medical interventions, Outcome 6 Testosterone and free androgen index.
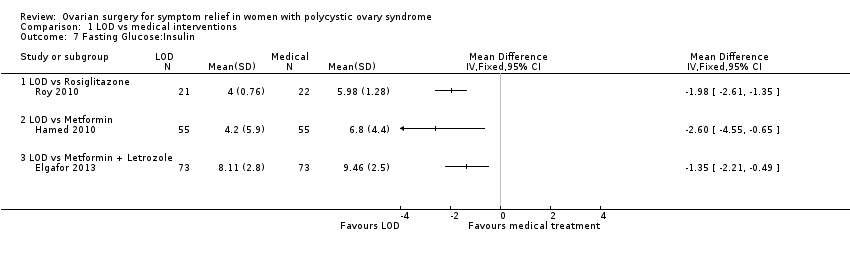
Comparison 1 LOD vs medical interventions, Outcome 7 Fasting Glucose:Insulin.

Comparison 2 LOD vs other surgical interventions, Outcome 1 Menstrual regularity.

Comparison 2 LOD vs other surgical interventions, Outcome 2 Improvement in androgenic symptoms (hirsutism/acne).
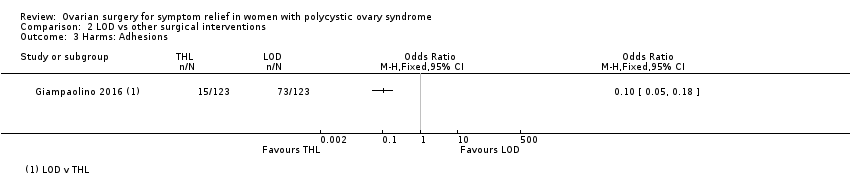
Comparison 2 LOD vs other surgical interventions, Outcome 3 Harms: Adhesions.

Comparison 2 LOD vs other surgical interventions, Outcome 4 Testosterone and free androgen index.
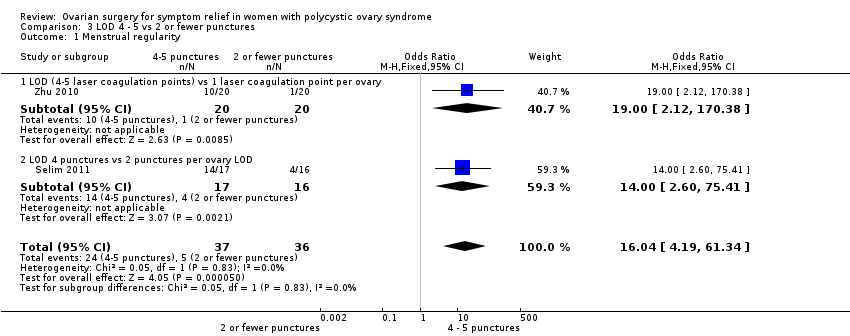
Comparison 3 LOD 4 ‐ 5 vs 2 or fewer punctures, Outcome 1 Menstrual regularity.

Comparison 3 LOD 4 ‐ 5 vs 2 or fewer punctures, Outcome 2 Testosterone and free androgen index.
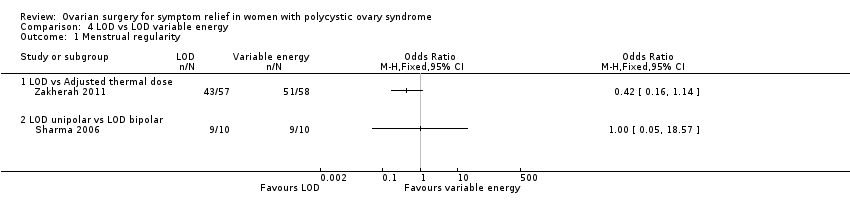
Comparison 4 LOD vs LOD variable energy, Outcome 1 Menstrual regularity.

Comparison 4 LOD vs LOD variable energy, Outcome 2 Harms.

Comparison 4 LOD vs LOD variable energy, Outcome 3 BMI.

Comparison 4 LOD vs LOD variable energy, Outcome 4 Testosterone and free androgen index.
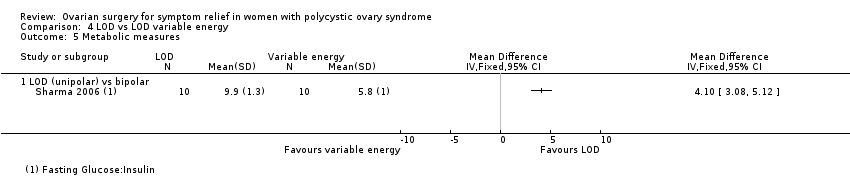
Comparison 4 LOD vs LOD variable energy, Outcome 5 Metabolic measures.
| LOD compared to medical interventions for symptom relief in women with polycystic ovary syndrome | ||||||
| Patient or population: Women with symptoms of PCOS | ||||||
| Outcomes | Relative effect | Anticipated absolute effects* (95% CI) | Quality of the evidence | What happens | ||
| Without LOD | With LOD | Difference | ||||
| Menstrual regularity at 6 months LOD vs metformin LOD vs metformin + clomiphene LOD vs gonadotropins LOD vs letrozole LOD vs metformin + letrozole | Findings inconsistent and data unsuitable for pooling | Not calculable | ⊕⊝⊝⊝ | |||
| OR 1.02 | 70.6% | 71.0% | 0.4% more | ⊕⊕⊝⊝ | ||
| OR 19.20 | 11.1% | 70.6% | 59.5% more | ⊕⊕⊝⊝ | ||
| OR 1.08 | 68.8% | 70.4% | 1.6% more | ⊕⊕⊝⊝ | ||
| OR 0.95 | 52.1% | 50.8% | 1.3% fewer | ⊕⊕⊝⊝ | ||
| Improvement in androgenic symptoms at 6 months (hirsutism/acne) ‐ LOD vs metformin | OR 1.00 | 79.4% | 79.4% | 0.0% fewer | ⊕⊕⊝⊝ | |
| Improvement in androgenic symptoms at 6 months (hirsutism/acne) ‐ LOD vs gonadotrophins | Acne: OR 3.20 (0.33 to 30.94) Hirsutism: OR 2.31, (0.22 to 23.89) | See comments | ⊕⊝⊝⊝VERY LOW 1, 4 | Acne: 4/29 without LOD, 1/21 with LOD Hirsutism: 3/29 without LOD, 1/21 with LOD | ||
| Harms: GI Upset at 6 months ‐ LOD vs metformin + clomiphene Harms: OHSS rates at 6 months ‐ LOD vs gonadotrophins | OR 0.05 | 10.4% | 0.6% | 9.9% fewer | ⊕⊕⊕⊝ | |
| OR 0.08 | 25.0% | 2.6% | 22.4% fewer | ⊕⊕⊝⊝ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level for serious risk of bias: Included studies not double‐blinded, and in some cases methods of randomization unclear. | ||||||
| LOD compared to other surgical interventions for symptom relief in women with polycystic ovary syndrome | ||||||
| Patient or population: Women with symptoms of PCOS | ||||||
| Outcomes | Relative effect | Anticipated absolute effects* (95% CI) | Quality of the evidence | What happens | ||
| Without LOD | With LOD | Difference | ||||
| Menstrual regularity ‐ LOD vs unilateral LOD | OR 1.51 | 71.2% | 78.8% | 7.7% more | ⊕⊕⊕⊝ | 1 study follow‐up at 3 months. 1 study follow‐up at 12 months |
| Menstrual regularity at 6 months ‐ LOD vs ultrasound‐guided transvaginal ovarian drilling | OR 1.23 | 54.7% | 59.7% | 5.1% more | ⊕⊕⊝⊝ | |
| Menstrual regularity at 12 months | OR 2.13 | 88.2% | 94.1% | 5.9% more | ⊕⊕⊝⊝ | Note control group is NdYAG Laser |
| Improvement in androgenic symptoms at 6 months (Acne) ‐ LOD vs USS guided | OR 0.84 (0.20 to 3.5) | 47.1% | 42.7% | 4.3% fewer | ⊕⊕⊝⊝ | |
| Improvement in androgenic symptoms at 6 months (Hirsutism) ‐ LOD vs USS‐guided | OR 1.09 | 40.0% | 42.1% (16.7 to 72.3) | 2.1% more (23.3 fewer to 32.3 more) | ⊕⊕⊝⊝ | |
| Harms: Adhesions at 6 months ‐ LOD vs THL | OR 0.10 | 59.3% | 12.7% | 46.6% fewer | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level for serious risk of bias: Included studies not double‐blinded or unclear allocation concealment or unclear randomization method. | ||||||
| LOD 4 ‐ 5 punctures compared to 2 or fewer punctures for symptom relief in women with polycystic ovary syndrome | ||||||
| Patient or population: Women with symptoms of PCOS | ||||||
| Outcomes | Relative effect | Anticipated absolute effects* (95% CI) | Quality of the evidence | What happens | ||
| Without LOD 4‐5 | With LOD 4‐5 | Difference | ||||
| Menstrual regularity at 6 months ‐ LOD 4 ‐ 5 coagulation points compared to 2 or fewer | OR 16.04 | 13.9% | 72.1% | 58.2% more | ⊕⊕⊝⊝ | |
| Menstrual regularity at 6 months ‐ LOD (4 ‐ 5 laser coagulation points) vs 1 laser coagulation point per ovary | OR 19.00 | 5.0% | 50.0% | 45.0% more | ⊕⊕⊝⊝ | |
| Menstrual regularity at 6 months ‐ LOD 4 punctures vs 2 punctures per ovary | OR 14.00 | 25.0% | 82.4% | 57.4% more | ⊕⊕⊝⊝ | |
| Improvement in androgenic symptoms | No data available | |||||
| Harms LOD 4 ‐ 5 versus fewer punctures | No data available | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level for serious risk of bias: Included studies not double‐blinded or methods of randomization unclear. | ||||||
| LOD compared to LOD variable energy for symptom relief in women with polycystic ovary syndrome | ||||||
| Patient or population: Women with symptoms of PCOS | ||||||
| Outcomes | Relative effect | Anticipated absolute effects* (95% CI) | Quality of the evidence | What happens | ||
| Without LOD | With LOD | Difference | ||||
| Menstrual regularity at 6 months ‐ LOD vs adjusted thermal dose | OR 0.42 | 87.9% | 75.4% | 12.6% fewer | ⊕⊝⊝⊝ | |
| Menstrual regularity at 3 months ‐ LOD unipolar vs LOD bipolar | OR 1.00 | 90.0% | 90.0% | 0.0% fewer | ⊕⊝⊝⊝ | Groups had different metabolic characteristics at baseline |
| Improvement in androgenic symptoms | No data available | |||||
| Harms: Adhesions at 6 months | OR 0.96 | 28.6% | 27.7% | 0.8% fewer | ⊕⊝⊝⊝ VERY LOW1, 2 | Women that remained enrolled for second‐look laparoscopy |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level for serious risk of bias: Included studies not double‐blinded or unclear allocation concealment. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Menstrual regularity Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 LOD vs Metformin alone | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Menstrual regularity Show forest plot | 5 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 LOD vs Metformin + Clomiphene | 2 | 332 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.64, 1.64] |
| 2.2 LOD vs Gonadotropins | 1 | 35 | Odds Ratio (M‐H, Fixed, 95% CI) | 19.2 [3.17, 116.45] |
| 2.3 LOD vs Letrozole | 1 | 260 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.64, 1.84] |
| 2.4 LOD vs Metformin + Letrozole | 1 | 146 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.49, 1.81] |
| 3 Improvement in androgenic symptoms (hirsutism/acne) Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 LOD vs Metformin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 LOD vs Gonadotrophins | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Harms Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 LOD vs Metformin + Clomiphen | 2 | 332 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.36] |
| 4.2 LOD vs Gonadotrophins | 1 | 33 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.00, 1.61] |
| 5 BMI Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 LOD vs Metformin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 LOD vs Metformin + Letrozole | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Testosterone and free androgen index Show forest plot | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 LOD vs Metformin | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 LOD vs GnRHa + OCP | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 LOD vs Metformin + Letrozole | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 LOD versus Rosiglitazone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Fasting Glucose:Insulin Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 LOD vs Rosiglitazone | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 LOD vs Metformin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 LOD vs Metformin + Letrozole | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Menstrual regularity Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 LOD vs Unilateral LOD | 2 | 104 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.51 [0.62, 3.71] |
| 1.2 LOD vs Ultrasound guided transvaginal ovarian drilling | 1 | 147 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.64, 2.37] |
| 1.3 Laser LOD vs Harmonic Scalpel | 1 | 34 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.13 [0.17, 26.03] |
| 2 Improvement in androgenic symptoms (hirsutism/acne) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Hirsutism | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Acne | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Harms: Adhesions Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Testosterone and free androgen index Show forest plot | 6 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 LOD vs Ultrasound guided transvaginal ovarian drilling | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 LOD versus mini laparoscopy with sedation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 LOD vs unilateral LOD | 3 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Laser LOD vs Harmonic Scalpel | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Menstrual regularity Show forest plot | 2 | 73 | Odds Ratio (M‐H, Fixed, 95% CI) | 16.04 [4.19, 61.34] |
| 1.1 LOD (4‐5 laser coagulation points) vs 1 laser coagulation point per ovary | 1 | 40 | Odds Ratio (M‐H, Fixed, 95% CI) | 19.0 [2.12, 170.38] |
| 1.2 LOD 4 punctures vs 2 punctures per ovary LOD | 1 | 33 | Odds Ratio (M‐H, Fixed, 95% CI) | 14.0 [2.60, 75.41] |
| 2 Testosterone and free androgen index Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 LOD 4‐5 punctures vs 2 or fewer punctures (Testosterone) | 2 | 73 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.12, ‐0.68] |
| 2.2 LOD 4 punctures vs 2 punctures (FAI) | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | ‐1.5 [‐3.21, 0.21] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Menstrual regularity Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 LOD vs Adjusted thermal dose | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 LOD unipolar vs LOD bipolar | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Harms Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 BMI Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Testosterone and free androgen index Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 LOD vs Adjusted thermal dose | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 LOD unipolar vs LOD bipolar | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Metabolic measures Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 LOD (unipolar) vs bipolar | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

