Intervención conductual intensiva temprana para niños pequeños con trastornos del espectro autista
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (CENTRAL), in the Cochrane Library
#1MeSH descriptor Early Intervention (Education), this term only
#2MeSH descriptor Behavior Therapy, this term only
#3Lovaas*
#4(intens* NEAR/3 ( intervent* or therap* or treat* or program*))
#5(IBI or EIBI)
#6applied NEXT behavio* NEXT analy* or ABA
#7(#1 OR #2 OR #3 OR #4 OR #5 OR #6)
#8MeSH descriptor Child Development Disorders, Pervasive explode all trees
#9(pervasive development* disorder* or PDD or PDDs)
#10Rett*
#11Asperger*
#12autis* or ASD or ASDs
#13Kanner*
#14childhood schizophren*
#15MeSH descriptor Communication Disorders, this term only
#16MeSH descriptor Speech Disorders, this term only
#17MeSH descriptor Language Development Disorders, this term only
#18MeSH descriptor Child Behavior Disorders, this term only
#19communicat* NEAR/3 disorder*
#20speech NEAR/3 (delay* or disorder*)
#21(child* NEAR/3 behavio* NEAR/3 disorder*)
#22(language NEAR/3 (delay* or disorder*))
#23(#8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22)
#24(baby or babies or infant* or toddler* or child* or pre‐school* or preschool* or boy* or girl*)
#25MeSH descriptor Child explode all trees
#26MeSH descriptor Infant, this term only
#27(#24 OR #25 OR #26)
#28(#7 AND #23 AND #27)
Ovid MEDLINE
1 "Early Intervention (Education)"/
2 behavior therapy/
3 Lovaas$.tw.
4 (intens$ adj3 (interven$ or therap$ or treat$ or program$)).tw.
5 (IBI or EIBI).tw. (
6 (applied behavio$ analy$ or ABA).tw.
7 or/1‐6
8 exp Child Development Disorders, Pervasive/
9 (pervasive development$ disorder$ or PDD or PDDs).tw.
10 (autis$ or ASD or ASDs).tw.
11 Asperger$.tw.
12 Kanner$.tw.
13 Rett$.tw.
14 childhood schizophrenia.tw.
15 communication disorders/
16 (communicat$ adj3 disorder$).tw.
17 Speech Disorders/
18 language development disorders/
19 (speech adj3 (delay$ or disorder$)).tw.
20 (language adj3 (delay$ or disorder$)).tw.
21 child behavior disorders/
22 (child$ adj3 behavio$ adj3 disorder$).tw.
23 or/8‐22
24 infant/
25 exp child/
26 (baby or babies or infant$ or toddler$ or child$ or pre‐school$ or preschool$ or boy$ or girl$).tw.
27 or/24‐26
28 7 and 23 and 27)
MEDLINE In‐Process & Other Non‐Indexed Citations Ovid
1 Lovaas$.tw.
2 (intens$ adj3 (interven$ or therap$ or treat$ or program$)).tw.
3 (IBI or EIBI).tw.
4 (applied behavio$ analy$ or ABA).tw.
5 or/1‐4
6 (pervasive development$ disorder$ or PDD or PDDs).tw.
7 (autis$ or ASD or ASDs).tw.
8 Asperger$.tw.
9 Kanner$.tw.
10 Rett$.tw.
11 childhood schizophrenia.tw.
12 (communicat$ adj3 disorder$).tw.
13 (speech adj3 (delay$ or disorder$)).tw.
14 (language adj3 (delay$ or disorder$)).tw.
15 (child$ adj3 behavio$ adj3 disorder$).tw.
16 or/6‐15
17 (baby or babies or infant$ or toddler$ or child$ or pre‐school$ or preschool$ or boy$ or girl$).tw.
18 5 and 16 and 17
MEDLINE Epub Ahead of Print Ovid
1 Lovaas$.tw.
2 (intens$ adj3 (interven$ or therap$ or treat$ or program$)).tw.
3 (IBI or EIBI).tw.
4 (applied behavio$ analy$ or ABA).tw.
5 or/1‐4
6 (pervasive development$ disorder$ or PDD or PDDs).tw.
7 (autis$ or ASD or ASDs).tw.
8 Asperger$.tw.
9 Kanner$.tw.
10 Rett$.tw.
11 childhood schizophrenia.tw.
12 (communicat$ adj3 disorder$).tw.
13 (speech adj3 (delay$ or disorder$)).tw.
14 (language adj3 (delay$ or disorder$)).tw.
15 (child$ adj3 behavio$ adj3 disorder$).tw.
16 or/6‐15
17 (baby or babies or infant$ or toddler$ or child$ or pre‐school$ or preschool$ or boy$ or girl$).tw.
18 5 and 16 and 17
Embase OVID
1 early childhood intervention/
2 behavior therapy/
3 Lovaas$.tw.
4 (intens$ adj3 (interven$ or therap$ or treat$ or program$)).tw.
5 (IBI or EIBI).tw.
6 (applied behavio$ analy$ or ABA).tw.
7 or/1‐6
8 exp autism/
9 (pervasive development$ disorder$ or PDD or PDDs).tw.
10 Rett$.tw.
11 Asperger$.tw.
12 (autis$ or ASD or ASDs).tw.
13 Kanner$.tw.
14 childhood schizophrenia.tw.
15 (communicat$ adj3 disorder$).tw.
16 speech disorder/ (16
17 communication disorder/
18 (speech adj3 (delay$ or disorder$)).tw.
19 language disability/
20 (language adj3 (delay$ or disorder$)).tw.
21 child behavior disorders/
22 (child$ adj3 behavio$ adj3 disorder$).tw.
23 or/8‐22
24 7 and 23
25 (baby or babies or infant$ or toddler$ or child$ or pre‐school$ or preschool$ or boy$ or girl$).tw.
26 exp child/
27 25 or 26
28 24 and 27
CINAHL Plus EBSCOhost (Cumulative Index to Nursing and Allied Health Literature)
S24 S7 and S20 and S23
S23 S21 or S22
S22 BABY OR BABIES OR INFANT* OR toddler* or child* or pre‐school* or preschool* or boy* or girl*
S21 AG infant or AG CHILD OR AG CHILD,PRESCHOOL
S20 S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19
S19 (MH "Child Behavior Disorders")
S18 language N3 delay or language N3 disorder*
S17 speech N3 delay* or speech N3 disorder*
S16 COMMUNICAT* N3 DISORDER*
S15 (MH "Communicative Disorders") OR (MH "Language Disorders") OR (MH "Speech Disorders")
S14 childhood schizophren*
S13 Kanner*
S12 (autis* or ASD or ASDs)
S11 Asperger*
S10 Rett*
S9 (pervasive development* disorder* or PDD or PDDs)
S8 (MH "Child Development Disorders, Pervasive+")
S7 S1 or S2 or S3 or S4 or S5 or S6
S6 (applied behavio* analy*) or (ABA)
S5 (IBI or EIBI)
S4 (intens* N3 interven*) or (intens* N3 therap*) or (intens* N3 treat*) or (intens* N3 program*)
S3 lovaas*
S2 (MH "Behavior Therapy") or (MH "Behavior Modification")
S1 (MH "Early Intervention") OR (MH "Early Childhood Intervention")
PsycINFO OVID
1 early intervention/
2 behavior therapy/
3 behavior modification/
4 Lovaas.tw.
5 (intens$ adj3 (interven$ or therap$ or treat$ or program$)).tw.
6 (IBI or EIBI).tw.
7 (applied behavio$ analy$ or ABA).tw.
8 or/1‐7
9 exp pervasive developmental disorders/
10 (pervasive development$ disorder$ or PDD or PDDs).tw.
11 Rett$.tw.
12 Asperger$.tw.
13 (autis$ or ASD or ASDs).tw.
14 Kanner$.tw.
15 childhood schizophrenia.tw.
16 communication disorders/
17 (communicat$ adj3 disorder$).tw.
18 (speech adj3 (delay$ or disorder$)).tw.
19 (language adj3 (delay$ or disorder$)).tw.
20 language disorders/ or language delay/
21 speech disorders/ or retarded speech development/
22 behavior disorders/
23 or/9‐22
24 ("140" or "160" or "180").ag.
25 (baby or babies or infant$ or toddler$ or child$ or pre‐school$ or preschool$ or boy$ or girl$).tw.
26 24 or 25
27 8 and 23 and 26
ERIC EBSCOhost (Education Resources Information Center; searched after 2011)
S1 (DE "Early Intervention")
S2 (DE "Behavior Modification")
S3 IBI OR EIBI
S4 INTENSIVE N3 ( INTERVENTION* OR THERAP* OR TREATMENT* OR PROGRAM*)
S5 ( APPLIED N1 BEHAVIO*R* N1 ANALY*) OR ABA
S6 Lovaas
S7 S1 OR S2 OR S3 OR S4 OR S5 OR S6
S8 DE "Pervasive Developmental Disorders" OR DE "Asperger Syndrome" OR DE "Autism"
S9 autis*
S10 asperger*
S11 Rett*
S12 Kanner*
S13 ASD or ASDs OR PDD or PDDs
S14 CHILDHOOD SCHIZOPHREN*
S15 S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14
S16 S7 AND S15
S17 DE "Children" OR DE "Infants" OR DE "Preschool Children" OR DE "Toddlers"
S18 infant* or child* or toddler* or preschool* or pre‐school*
S19 S17 OR S18
S20 S16 AND S19
ERIC Datastar Dialog (searched up until 2011)
"((EARLY‐INTERVENTION.DE.) OR (BEHAVIOR‐MODIFICATION.DE.) OR (( INTENSIVE NEAR ( INTERVENTION$1 OR THERAP$3 OR TREATMENT$1 OR PROGRAM$3 ) ) .TI,AB.) OR (( IBI OR EIBI ) .TI,AB.) OR (( APPLIED ADJ BEHAVIOR$2 ADJ ANALY$4 OR ABA ) .TI,AB.) OR (LOVAAS.TI,AB.)) AND ((AUTISM.W..DE. OR PERVASIVE‐DEVELOPMENTAL‐DISORDERS.DE.) OR (ASPERGER‐SYNDROME.DE.) OR (( AUTIS$3 OR ASPERGER$1 OR KANNER$1 OR RETT$1 OR ASD OR ASDS OR PDD OR PDDS ) .TI,AB.) OR (( CHILDHOOD ADJ SCHIZOPHRENI$2 ) .TI,AB.)) AND ((YOUNG‐CHILDREN.DE. OR PRESCHOOL‐CHILDREN.DE. OR TODDLERS.W..DE.) OR (( CHILD$3 OR INFAN$1 OR TODDLER$1 OR PRESCHOOL$3 OR PRE ADJ SCHOOL$3 ) .TI,AB.))"
Sociological Abstracts Proquest
(SU.EXACT("Behavior Modification") OR TI("EIBI" OR "ABA" OR "IBI" OR Lovaas) OR AB("EIBI" OR "ABA" OR "IBI" OR lovaas) OR TI("applied behav* analysis") OR AB("applied behav* analysis") OR TI((intensive) NEAR/3 (interven* OR therapy* OR treat* OR program*))) AND (TI(child* OR baby OR babies OR toddler* OR pre‐school* OR preschool*) OR AB(child* OR baby OR babies OR toddler* OR pre‐school* OR preschool*) OR SU.EXACT("Children" OR "Infants")) AND (SU.EXACT("Behavior Modification") OR TI("EIBI" OR "ABA" OR Lovaas) OR AB("EIBI" OR "ABA" OR lovaas) OR TI("applied behav* analysis") OR AB("applied behav* analysis") OR TI((intensive) NEAR/3 (interven* OR therapy* OR treat* OR program*))) AND (SU.EXACT(("Autism")) OR TI(autis* OR asperg* OR "PDD" OR "PDDs" OR "ASD" OR "ASDs" OR kanner* OR childhood schizophren* OR pervasive development* disorder*) OR AB(autis* OR asperg* OR "PDD" OR "PDDs" OR "ASD" OR "ASDs" OR kanner* OR childhood schizophren* OR pervasive development* disorder*) OR TI((communicat* OR behav*) NEAR/3 disorder*) OR AB((communicat* OR behav*) NEAR/3 disorder*) OR TI ((speech OR language) NEAR/3 (delay* OR disorder*)) OR AB((speech OR language) NEAR/3 (delay* OR disorder*)))
Social Science Citation Index Web of Science
#7 AND #6
DocType=All document types; Language=All languages;
#7 TS=(baby or babies or infant* or toddler* or child* or pre‐school* or preschool* or boy* or girl*)
DocType=All document types; Language=All languages;
#6 #5 AND #4
DocType=All document types; Language=All languages;
#5 TS=(autis* or asperger* or ASD or ASDs or Pervasive development* disorder* or PDD or PDDs or REtt* or Kanner* or childhood schizophren*)
DocType=All document types; Language=All languages;
#4 #3 OR #2 OR #1
DocType=All document types; Language=All languages;
#3 TS=("applied behav* analy*" or ABA)
DocType=All document types; Language=All languages;
#2 TS=(lovaas OR IBI or EIBI)
DocType=All document types; Language=All languages;
#1 TS=(intens* NEAR/3 (interven* or therap* or treat* or program*))
DocType=All document types; Language=All languages;
Conference Proceedings Citation Index ‐ Social Sciences & Humanities Web of Science
#7 AND #6
DocType=All document types; Language=All languages;
#7 TS=(baby or babies or infant* or toddler* or child* or pre‐school* or preschool* or boy* or girl*)
DocType=All document types; Language=All languages;
#6 #5 AND #4
DocType=All document types; Language=All languages;
#5 TS=(autis* or asperger* or ASD or ASDs or Pervasive development* disorder* or PDD or PDDs or REtt* or Kanner* or childhood schizophren*)
DocType=All document types; Language=All languages;
#4 #3 OR #2 OR #1
DocType=All document types; Language=All languages;
#3 TS=("applied behav* analy*" or ABA)
DocType=All document types; Language=All languages;
#2 TS=(lovaas OR IBI or EIBI)
DocType=All document types; Language=All languages;
#1 TS=(intens* NEAR/3 (interven* or therap* or treat* or program*))
DocType=All document types; Language=All languages;
Cochrane Database of Systematic Reviews (CDSR) part ofthe Cochrane Library
#1MeSH descriptor: [Early Intervention (Education)]
#2MeSH descriptor: [Behavior Therapy]
#3Lovaas*:ti,ab
#4(intens* near/3 (intervent* or therap* or treat* or program*)):ti,ab
#5(IBI or EIBI):ti,ab
#6(applied next behavio$ next analy$ or ABA):ti,ab
#7#1 or #2 or #3 or #4 or #5 or #6
#8MeSH descriptor: [Child Development Disorders, Pervasive] explode all trees
#9(pervasive development* disorder* or PDD or PDDs):ti,ab
#10Rett*:ti,ab
#11Asperger*:ti,ab
#12(autis* or ASD or ASDs):ti,ab
#13Kanner*:ti,ab
#14(childhood next schizophren*):ti,ab
#15MeSH descriptor: [Communication Disorders] this term only
#16MeSH descriptor: [Speech Disorders] this term only
#17MeSH descriptor: [Language Development Disorders] this term only
#18MeSH descriptor: [Child Behavior Disorders] this term only
#19communicat* near/3 disorder*:ti,ab
#20speech near/3 (delay* or disorder*):ti,ab
#21(child* near/3 behavio* near/3 disorder*):ti,ab
#22(language near/3 (delay* or disorder*)):ti,ab
#23#8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22
#24(baby or babies or infant* or toddler* or child* or pre‐school* or preschool* or boy* or girl*):ti,ab
#25MeSH descriptor: [Child] explode all trees
#26MeSH descriptor: [Infant] this term only
#27#24 or #25 or #26 #28#7 and #23 and #27 in Cochrane Reviews (Reviews and Protocols)
Database of Abstracts of Reviews of Effectiveness (DARE), part of the Cochrane Library (searched until 2015)
#1MeSH descriptor: [Early Intervention (Education)]
#2MeSH descriptor: [Behavior Therapy]
#3Lovaas*:ti,ab
#4(intens* near/3 (intervent* or therap* or treat* or program*)):ti,ab
#5(IBI or EIBI):ti,ab
#6(applied next behavio$ next analy$ or ABA):ti,ab
#7#1 or #2 or #3 or #4 or #5 or #6
#8MeSH descriptor: [Child Development Disorders, Pervasive] explode all trees
#9(pervasive development* disorder* or PDD or PDDs):ti,ab
#10Rett*:ti,ab
#11Asperger*:ti,ab
#12(autis* or ASD or ASDs):ti,ab
#13Kanner*:ti,ab
#14(childhood next schizophren*):ti,ab
#15MeSH descriptor: [Communication Disorders] this term only
#16MeSH descriptor: [Speech Disorders] this term only
#17MeSH descriptor: [Language Development Disorders] this term only
#18MeSH descriptor: [Child Behavior Disorders] this term only
#19communicat* near/3 disorder*:ti,ab
#20speech near/3 (delay* or disorder*):ti,ab
#21(child* near/3 behavio* near/3 disorder*):ti,ab
#22(language near/3 (delay* or disorder*)):ti,ab
#23#8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22
#24(baby or babies or infant* or toddler* or child* or pre‐school* or preschool* or boy* or girl*):ti,ab
#25MeSH descriptor: [Child] explode all trees
#26MeSH descriptor: [Infant] this term only
#27#24 or #25 or #26
#28#7 and #23 and #27 in Other Reviews
Epistemonikos
(title:(title:(asd OR autis* OR asperger* OR pervasive OR rett) AND (title:(early intervention* OR intensive behav* OR applied behav*) OR abstract:(early intervention* OR intensive behav* OR applied behav*))) OR abstract:(title:(asd OR autis* OR asperger* OR pervasive OR rett) AND (title:(early intervention* OR intensive behav* OR applied behav*) OR abstract:(early intervention* OR intensive behav* OR applied behav*))))
ClinicalTrials.gov
Autism OR ASD OR Asperger OR PDD OR " pervasive developmental " | EIBI OR IBI OR ABA OR "early behavioural" OR "early behavioral" OR "applied behavioral" OR "applied behavioural" OR "Intensive behavioral" OR "Intensive behavioural" | Child
WorldCat OCLC
'kw:("intens* behav*" OR EIBI OR IBI OR ABA OR "applied behav*") AND kw:(autis* OR asd* OR asperg* OR PDD* OR "pervasive development* disorder*")) AND kw:(child* OR infant* OR baby OR babies OR toddler* OR preschool* OR pre‐school*)' > 'Thesis/dissertation'
WHO ICTRP (World Health Organization International Clinical Trials Registry Platform)
(apps.who.int/trialsearch/Default.aspx)
Basic search: autism AND early intensive OR autism AND early intervention OR autism AND intensive behavioral OR autism AND intense behavioral OR autism AND applied behavioral OR autism AND EIBI OR autism AND ABA OR autism AND IBI
Appendix 2. Summary of searches for this update (2011 onwards)
| Database name | Date of search | Database date range or issue | Limits applied to top‐up searches | Number of records |
| Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library | 24 August 2015 | 2015, Issue 7 | 2011‐2015 | 83 |
| 26 April 2016 | 2016, Issue 3 | 2015‐2016 | 13 | |
| 10 August 2017 | 2017, Issue 7 July | 2016‐2017 | 14 | |
| MEDLINE Ovid | 25 August 2015 | 1948 to August Week 2 2015 | ed=20111101‐20150813 | 475 |
| 26 April 2016 | 1946 to April Week 2 201 | ed=20150813‐20160414 | 89 | |
| 10 August 2017 | 1946 to July Week 4 2017 | Deduplicated with previous records | 145 | |
| MEDLINE In‐Process & Other Non‐Indexed Citations Ovid | 10 August 2017 | 08 August 2017 | No limits | 70 |
| MEDLINE EPub Ahead of Print Ovid | 10 August 2017 | 08 August 2017 | No limits | 19 |
| Embase OVID | 25 August 2015 | 1980 to 2015 Week 34 | 2011 to current | 737 |
| 26 April 2016 | 1980 to 2016 Week 17 | 2015 to current | 117 | |
| 10 August 2017 | 1980 to 2017 Week 32 | Deduplicated with previous records | 144 | |
| CINAHL Plus EBSCOhost (Cumulative Index to Nursing and Allied Health Literature) | 24 August 2015 | 1937 to 24 August 2015 | EM 20111101‐ | 740 |
| 26 April 2016 | 1937 to 26 April 2016 | EM 20150801‐ | 95 | |
| 10 August 2017 | 1937 to 10 August 2017 | Deduplicated with previous records | 181 | |
| PsycINFO OVID | 24 August 2015 | 1806 to August Week 3 2015 | up=20111107‐20150817 | 716 |
| 26 April 2016 | 1806 to April Week 3 2016 | up=20150817‐20160418 | 121 | |
| 10 August 2017 | 1806 to July Week 5 2017 | up=20160418‐2017073 | 217 | |
| ERIC EBSCOhost (Education Resources Information Center) | 24 August 2015 | 1966 to 24 August 2015 | 2011 onwards | 513 |
| 26 April 2016 | 1966 to 26 April 2016 | 2015 onwards | 107 | |
| 10 August 2017 | 1966 to 10 August 2017 | Deduplicated with previous records | 87 | |
| Sociological Abstracts Proquest | 25 August 2015 | 1952 to 25 August 2015 | 2011‐2015 | 11 |
| 28 April 2016 | 1952 to 28 April 2016 | 2015‐2016 | 4 | |
| 10 August 2017 | 1952 to 10 August 2017 | 2016‐2017 | 23 | |
| Social Science Citation Index Web of Science | 24 August 2015 | 1970 to 21 August 2015 | 2011‐2015 | 291 |
| 28 April 2016 | 1970 to 25 April 2016 | 2015‐2016 | 84 | |
| 10 August 2017 | 1970 to 09 August 2017 | Deduplicated with previous records | 99 | |
| Conference Proceedings Citation Index ‐ Social Sciences & Humanities Web of Science | 25 August 2015 | 1990 to 21 August 2015 | No limits | 2 |
| 28 April 2016 | 1990 to 21 August 2015 | 2015‐2016 | 0 | |
| 10 August 2017 | 1990 to 09 August 2017 | 2016‐2017 | 1 | |
| Cochrane Database of Systematic Reviews (CDSR) | 24 August 2015 | 2015, Issue 8 | no limits | 3 |
| 26 April 2016 | 2016, Issue 12 | 2015 to 2016 | 2 | |
| 10 August 2017 | 2017, Issue 8 | 2016 to 2017 | 0 | |
| Database of Abstracts of Reviews of Effects (DARE) | 24 August 2015 | 2015, Issue 2 | no limits | 23 |
| Epistemonikos (www.epistemonikos.org) | 10 August 2017 | All content up to 10 August 2017 | no limits | 7 |
| ClinicalTrials.gov (clinicaltrials.gov) | 26 August 2015 | All content up to 26 August 2015 | no limits | 10 |
| 28 April 2016 | All content up to 28 April 2016 | Deduplicated with previous records | 3 | |
| 11 August 2017 | All content up to 11 August 2017 | Deduplicated with previous records | 3 | |
| WorldCat OCLC (theses only; www.worldcat.org) | 25 August 2015 | All content up to 25 August 2015 | 2011 to 2015 | 13 |
| 28 April 2016 | All content up to 28 April 2016 | 2015‐2016 | 6 | |
| 10 August 2017 | All content up to 10 August 2017 | 2016 to 2017 | 2 | |
| WHO International Clinical Trials Registry Platform (ICTRP; apps.who.int/trialsearch/default.aspx) | 26 August 2015 | All content up to 26 August 2015 | no limits | 16 |
| 28 April 2016 | All content up to 28 April 2016 | Deduplicated with previous records | 4 | |
| 11 August 2017 | All content up to 11 August 2017 | Deduplicated with previous records | 5 | |
| Total database and trials register records 2011‐2017 | 5295 | |||

Study flow diagram.
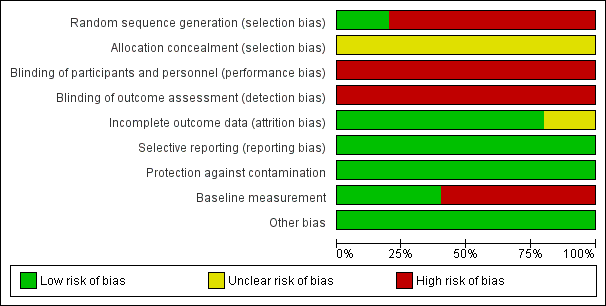
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
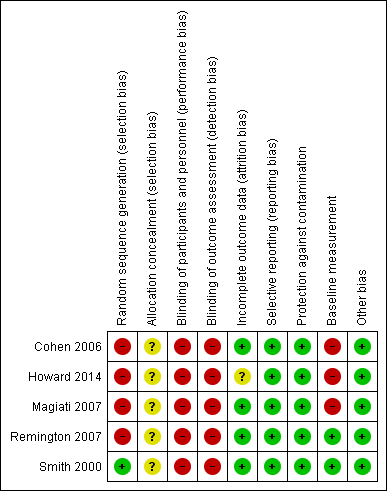
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Adaptive behavior, outcome: 1.1 Vineland Adaptive Behavior Scales Composite

Comparison 1 Early intensive behavioral intervention (EIBI) compared to for young children with autism spectrum disorders (ASD), Outcome 1 Adaptive behavior.

Comparison 1 Early intensive behavioral intervention (EIBI) compared to for young children with autism spectrum disorders (ASD), Outcome 2 Autism symptom severity.

Comparison 1 Early intensive behavioral intervention (EIBI) compared to for young children with autism spectrum disorders (ASD), Outcome 3 Intelligence.
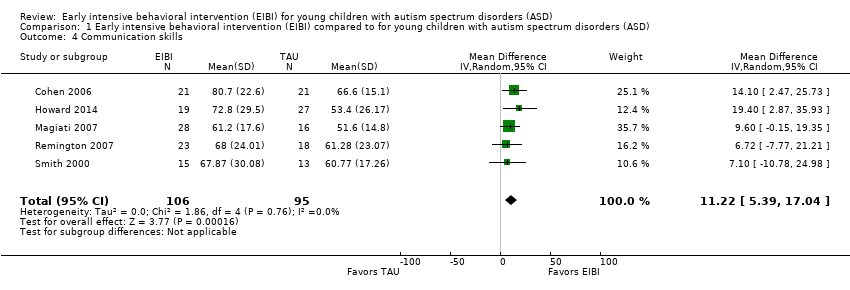
Comparison 1 Early intensive behavioral intervention (EIBI) compared to for young children with autism spectrum disorders (ASD), Outcome 4 Communication skills.

Comparison 1 Early intensive behavioral intervention (EIBI) compared to for young children with autism spectrum disorders (ASD), Outcome 5 Language skills.

Comparison 1 Early intensive behavioral intervention (EIBI) compared to for young children with autism spectrum disorders (ASD), Outcome 6 Social competence.

Comparison 1 Early intensive behavioral intervention (EIBI) compared to for young children with autism spectrum disorders (ASD), Outcome 7 Daily living skills.

Comparison 1 Early intensive behavioral intervention (EIBI) compared to for young children with autism spectrum disorders (ASD), Outcome 8 Problem behavior.
| Study | EIBI N | EIBI N for general education with no extra support | EIBI N for general education with support | TAU N | TAU N for general education with no extra support | TAU N for general education with support |
| Cohen 2006 | 21 | 6 | 11 | 21 | 0 | 1 |
| Smith 2000 | 15 | 4 | 2 | 13 | 0 | 3 |
Comparison 1 Early intensive behavioral intervention (EIBI) compared to for young children with autism spectrum disorders (ASD), Outcome 9 Academic placement.
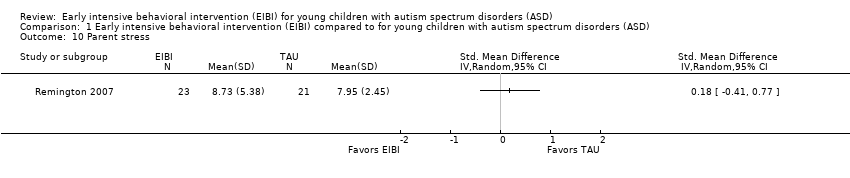
Comparison 1 Early intensive behavioral intervention (EIBI) compared to for young children with autism spectrum disorders (ASD), Outcome 10 Parent stress.
| Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD) | ||||||
| Patient or population: patients with young children (less than six years old) with autism spectrum disorders (ASD) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| TAU | EIBI | |||||
| Adaptive behavior | The mean adaptive behavior score ranged across control groups from 48.60 points to 67.10 points | The mean adaptive behavior score in the intervention groups was, on average, 9.58 points higher (5.57 points higher to 13.6 points higher) | ‐ | 202 | ⊕⊕⊝⊝ | ‐ |
| Autism symptom severity | ‐ | The mean autism symptom severity score in the intervention groups was 0.34 standard deviations lower | ‐ | 81 | ⊕⊝⊝⊝ | General guidelines for the magnitude of an effect suggest that effect sizes of 0.20 to 0.50 are considered to have a small effect, effect sizes of 0.50 to 0.80 are considered to have a medium effect, and effect sizes greater than 0.80 are considered to have a large effect (Cohen 1988) |
| Adverse effects Measured by: worsening of adaptive behavior or autism symptom severity Follow‐up: 2 to 3 years | No adverse events were reported in any study | |||||
| Intelligence | The mean IQ score ranged across control groups from 49.67 points to 73.20 points | The mean IQ score in the intervention groups was, on average, 15.44 higher (9.29 points higher to 21.59 points higher) | ‐ | 202 | ⊕⊕⊝⊝ | ‐ |
| Communication and language skills: expressive language | ‐ | The mean expressive language score in the intervention groups was 0.51 standard deviations higher | ‐ | 165 | ⊕⊕⊝⊝ | General guidelines for the magnitude of an effect suggest that effect sizes of 0.20 to 0.50 are considered to have a small effect, effect sizes of 0.50 to 0.80 are considered to have a medium effect, and effect sizes greater than 0.80 are considered to have a large effect (Cohen 1988) |
| Communication and language skills: receptive language | ‐ | The mean receptive language score in the intervention groups was 0.55 standard deviations higher (0.23 standard deviations higher to 0.87 standard deviations higher) | ‐ | 164 | ⊕⊕⊝⊝ | General guidelines for the magnitude of an effect suggest that effect sizes of 0.20 to 0.50 are considered to have a small effect, effect sizes of 0.50 to 0.80 are considered to have a medium effect, and effect sizes greater than 0.80 are considered to have a large effect (Cohen 1988) |
| Problem behavior | ‐ | The mean problem behavior score in the intervention groups was 0.58 standard deviations lower (1.24 standard deviations lower to 0.07 standard deviations higher) | ‐ | 67 | ⊕⊝⊝⊝ | General guidelines for the magnitude of an effect suggest that effect sizes of 0.20 to 0.50 are considered to have a small effect, effect sizes of 0.50 to 0.80 are considered to have a medium effect, and effect sizes greater than 0.80 are considered to have a large effect (Cohen 1988) |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ASD: autism spectrum disorders; CCT: clinical controlled trial; CI: Confidence interval; EIBI: early intensive behavioral intervention; IQ: intelligence quotient; RCT: randomized controlled trial | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1One study was conducted using an RCT design (Smith 2000) and four studies were conducted using a CCT design (Cohen 2006; Howard 2014; Magiati 2007; Remington 2007). Quality of evidence rating downgraded two levels due to inclusion of non‐randomized studies and associated risks of bias. | ||||||
|
| Treatment Groups | Comparison Groups | ||||
| Study | Outcomes | Pre‐Treatment | Post‐Treatment | Pre‐Treatment | Post‐Treatment | |
| Primary | Adaptive behavior | VABS composite | VABS composite | VABS composite | VABS composite | |
| Autism severity | NA | NA | NA | NA | ||
| Secondary | IQ | BSID‐II; WPPSI‐R | BSID‐II; WPPSI‐R | BSID; WPPSI‐R | BSID‐II; WPPSI‐R | |
| Non‐verbal IQ | MPS | MPS | MPS | MPS | ||
| Non‐verbal social communication | NA | NA | NA | NA | ||
| Expressive communication | RDLS | RDLS | RDLS | RDLS | ||
| Receptive communication | RDLS | RDLS | RDLS | RDLS | ||
| Play | NA | NA | NA | NA | ||
| Social competence | VABS socialization domain | VABS socialization domain | VABS socialization domain | VABS socialization domain | ||
| Daily living skills | VABS daily living skills domain | VABS daily living skills domain | VABS daily living skills domain | VABS daily living skills domain | ||
| Academic achievement | NA | NA | NA | NA | ||
| Problem behavior | NA | NA | NA | NA | ||
| Parent stress | NA | NA | NA | NA | ||
| Academic placement | NA | Class placement | NA | Class placement | ||
| Quality of life | NA | NA | NA | NA | ||
| Primary | Adaptive behavior | VABS composite; Denver; DP‐II; RIDES | VABS composite; Denver; DP‐II; RIDES | VABS composite | VABS composite | |
| Autism severity | # of DSM‐IV criteria (APA 1994) | NA | # of DSM‐IV criteria | NA | ||
| Secondary | IQ | WPPSI‐R; BSID‐II; S‐B; DAYC; PEP‐R; DAS; DP‐II | WPPSI‐R, BSID‐II, S‐B; DAYC, PEP‐R, DAS | WPPSI‐R, BSID‐II, S‐B; DAS | WPPSI‐R, BSID‐II, S‐B; DAS | |
| Non‐verbal IQ | MPS; S‐B | MPS; S‐B; Leiter‐R | MPS; S‐B | MPS; S‐B; Leiter‐R | ||
| Non‐verbal social communication | NA | NA | NA | NA | ||
| Expressive communication | RDLS; ITLS; REEL‐R; PLS‐3; ITDA; EVT; DP‐II | RDLS; ITLS; REEL‐R; PLS‐3; ITDA; EVT; EOWPVT | RDLS; ITLS; REEL‐R; PLS‐3; ITDA; EVT; DP‐II | RDLS; ITLS; REEL‐R; PLS‐3; ITDA; EVT; EOWPVT | ||
| Receptive communication | RDLS; ITLS; REEL‐R; PLS‐3; ITDA; PPVT‐III; DP‐II | RDLS; ITLS; REEL‐R; PLS‐3; PPVT‐III; ROWPVT; ITDA‐1 | RDLS; ITLS; REEL‐R; PLS‐3; PPVT‐III; DP‐II; ITDA‐1 | RDLS; ITLS; REEL‐R; PLS‐3; PPVT‐III, ROWPVT; ITDA‐1 | ||
| Play | NA | NA | NA | NA | ||
| Social competence | VABS socialization domain | VABS socialization domain | VABS socialization domain | VABS socialization domain | ||
| Daily living skills | VABS daily living skills domain | VABS daily living skills domain | VABS daily living skills domain | VABS daily living skills domain | ||
| Academic achievement | NA | NA | NA | NA | ||
| Problem behavior | NA | NA | NA | NA | ||
| Parent stress | NA | NA | NA | NA | ||
| Academic placement | NA | NA | NA | NA | ||
| Quality of life | NA | NA | NA | NA | ||
| Primary | Adaptive behavior | VABS composite | VABS composite | VABS composite | VABS composite | |
| Autism severity | ADI‐R | ADI‐R | ADI‐R | ADI‐R | ||
| Secondary | IQ | WPPSI‐R; BSID‐R; MPS | WPPSI‐R; BSID‐R; MPS | WPPSI‐R; BSID‐R; MPS | WPPSI‐R; BSID‐R; MPS | |
| Non‐verbal IQ | NA | NA | NA | NA | ||
| Non‐verbal social communication | NA | NA | NA | NA | ||
| Expressive communication | EOWPVT‐R | EOWPVT‐R | EOWPVT‐R | EOWPVT‐R | ||
| Receptive communication | BPVS‐II | BPVS‐II | BPVS‐II | BPVS‐II | ||
| Play | SPT‐II | SPT‐II | SPT‐II | SPT‐II | ||
| Social competence | VABS socialization domain | VABS socialization domain | VABS socialization domain | VABS socialization domain | ||
| Daily living skills | VABS daily living skills domain | VABS daily living skills domain | VABS daily living skills domain | VABS daily living skills domain | ||
| Academic achievement | NA | NA | NA | NA | ||
| Problem behavior | NA | NA | NA | NA | ||
| Parent stress | NA | NA | NA | NA | ||
| Academic placement | NA | NA | NA | NA | ||
| Quality of life | NA | NA | NA | NA | ||
| Primary | Adaptive behavior | VABS composite | VABS composite | VABS composite | VABS composite | |
| Autism severity | ASQ | ASQ | ASQ | ASQ | ||
| Secondary | IQ | BSID‐R; S‐B | BSID‐R; S‐B | BSID‐R; S‐B | BSID‐R; S‐B | |
| Non‐verbal IQ | NA | NA | NA | NA | ||
| Non‐verbal social communication | ESCS | ESCS | ESCS | ESCS | ||
| Expressive communication | RDLS | RDLS | RDLS | RDLS | ||
| Receptive communication | RDLS | RDLS | RDLS | RDLS | ||
| Play | NA | NA | NA | NA | ||
| Social competence | VABS socialization domain | VABS socialization domain | VABS socialization domain | VABS socialization domain | ||
| Daily living skills | VABS daily living skills domain | VABS daily living skills domain | VABS daily living skills domain | VABS daily living skills domain | ||
| Academic achievement | NA | NA | NA | NA | ||
| Problem behavior | DCBC | DCBC | DCBD | DCBD | ||
| Parent stress | QRS‐F parent and family problems subscale | QRS‐F parent and family problems subscale | QRS‐F parent and family problems subscale | QRS‐F parent and family problems subscale | ||
| Academic placement | NA | NA | NA | NA | ||
| Quality of life | NA | NA | NA | NA | ||
| Primary | Adaptive behavior | VABS composite | VABS composite | VABS composite | VABS composite | |
| Autism severity | NA | NA | NA | NA | ||
| Secondary | IQ | BSID‐R; S‐B | BSID‐R; S‐B | BSID‐R; S‐B | BSID‐R; S‐B | |
| Non‐verbal IQ | MPS | MPS | MPS | MPS | ||
| Non‐verbal social communication | NA | NA | NA | NA | ||
| Expressive communication | RDLS | RDLS | RDLS | RDLS | ||
| Receptive communication | RDLS | RDLS | RDLS | RDLS | ||
| Play | NA | NA | NA | NA | ||
| Social competence | VABS socialization domain | VABS socialization domain | VABS socialization domain | VABS socialization domain | ||
| Daily living skills | VABS daily living skills domain | VABS daily living skills domain | VABS daily living skills domain | VABS daily living skills domain | ||
| Academic achievement | WIAT; ELM | WIAT | WIAT | WIAT | ||
| Problem behavior | CBCL | CBCL | CBCL | CBCL | ||
| Parent stress | NA | NA | NA | NA | ||
| Academic placement | Class placement | Class placement | Class placement | Class placement | ||
| Quality of life | NA | NA | NA | NA | ||
| ADI‐R: Autism Diagnostic Interview ‐ Revised (Lord 1994) | ||||||
| 'Risk of bias' item | Question | How risk of bias was assessed |
| Sequence generation | Was the sequence generation method used adequate? | We judged the risk of bias as follows:
|
| Allocation concealment | Was allocation adequately concealed? | We judged the risk of bias as follows:
|
| Blinding of participants and personnel | Were participants and personnel blind to which participants were in the treatment group? | We judged the risk of bias as follows:
|
| Blinding of outcome assessment | Were outcome assessors blind to which participants were in the treatment group? | We judged the risk of bias as follows:
|
| Incomplete outcome data | Did the trial authors deal adequately with missing data? | We judged the risk of bias as follows:
|
| Selective outcome reporting | Did the authors of the trial omit to report on any of their outcomes? | We judged the risk of bias as follows:
|
| Protection against contamination | Could the control group also have received the intervention? | We judged the risk of bias as follows:
|
| Baseline measurements | Were the intervention and control groups similar at baseline for chronological age, IQ, adaptive behavior skills, and communication skills? | We judged the risk of bias as follows:
|
| Other potential sources of bias | Through assessment, we determined whether any other source of bias was present in the trial, such as changing methods during the trial, or other anomalies. | We judged the risk of bias as follows:
|
| IQ: intelligence quotient | ||
| Analysis | Description of method | Reason not used |
| Measurement of treatment effect | Continuous data If outcomes are measured on a consistent scale across studies, we will calculate the effect of each study using the mean difference effect size. | As we needed to use the standardized mean difference (SMD) across most outcomes, we decided to report all effect sizes using the SMD effect size. |
| Dichotomous data If we locate dichotomous data, we will calculate a risk ratio with a 95% confidence interval for each outcome in each trial (Deeks 2017). | We did not locate dichotomous data. | |
| Unit of analysis issues | Cluster‐randomized trials If we locate cluster‐randomized trials, we will analyze them in accordance with the methods outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011, 16.3). | We did not find cluster‐randomized trials. |
| Multiple treatment groups If we locate data from studies with multiple treatment groups, we will analyze each intervention group separately by dividing the sample size for the common comparator groups proportionately across each comparison (Higgins 2011, 16.5.5). | ||
| Assessment of reporting bias | If we identify 10 or more studies, we will draw funnel plots (estimated differences in treatment effects against their standard error). Asymmetry could be due to publication bias, but could also be due to a real relation between trial and effect size, such as when larger trials have lower compliance and compliance is positively related to effect size (Sterne 2011). If we find such a relation, we will examine clinical variation between the studies (Sterne 2011, 10.4). As a direct test for publication bias, we will conduct sensitivity analyses to compare the results from published data with data from other sources. We will do a funnel plot in an update of the review if enough additional trials are located. | We did not locate enough studies to assess reporting bias. |
| Subgroup analyses | If we locate enough trials, we will examine possible clinical and methodological heterogeneity using subgroup analyses. The possible subgroups that we will examine, if present, are: intervention density (intensity) and duration; type of comparison group (for example, home‐based TAU, school‐based TAU, no treatment control), and pre‐treatment participant characteristics (for example, chronological age, symptom severity, IQ, communicative ability, and level of adaptive behavior). | We did not conduct subgroup analyses due to the small number of included trials. |
| Sensitivity analyses | If we locate enough trials, we will explore the impact of studies with high risk of bias on the robustness of the results of the review in sensitivity analyses by removing studies with a high risk of bias on baseline measurements and blinding of outcome assessment, and reanalyzing the remaining studies to determine whether these factors affected the results. | We did not conduct sensitivity analyses due to the small number of included trials. |
| CCTs: controlled clinical trials | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adaptive behavior Show forest plot | 5 | 202 | Mean Difference (IV, Random, 95% CI) | 9.58 [5.57, 13.60] |
| 2 Autism symptom severity Show forest plot | 2 | 81 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.79, 0.11] |
| 3 Intelligence Show forest plot | 5 | 202 | Mean Difference (IV, Random, 95% CI) | 15.44 [9.29, 21.59] |
| 4 Communication skills Show forest plot | 5 | 201 | Mean Difference (IV, Random, 95% CI) | 11.22 [5.39, 17.04] |
| 5 Language skills Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Expressive language | 4 | 165 | Std. Mean Difference (IV, Random, 95% CI) | 0.51 [0.12, 0.90] |
| 5.2 Receptive language | 4 | 164 | Std. Mean Difference (IV, Random, 95% CI) | 0.55 [0.23, 0.87] |
| 6 Social competence Show forest plot | 5 | 201 | Mean Difference (IV, Random, 95% CI) | 6.56 [1.52, 11.61] |
| 7 Daily living skills Show forest plot | 5 | 201 | Mean Difference (IV, Random, 95% CI) | 7.77 [3.75, 11.79] |
| 8 Problem behavior Show forest plot | 2 | 67 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.24, 0.07] |
| 9 Academic placement Show forest plot | Other data | No numeric data | ||
| 10 Parent stress Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |

