Incentivos para la prevención del hábito de fumar en niños y adolescentes
Resumen
Antecedentes
El hábito de fumar en adultos generalmente tiene sus raíces en la adolescencia. Si los individuos no empiezan a fumar durante este período es poco probable que alguna vez lo hagan. Además, una vez que se establece el hábito de fumar, el abandono implica un desafío; la probabilidad de abandonar posteriormente el hábito es inversamente proporcional a la edad de la iniciación. Un enfoque nuevo para reducir la prevalencia del hábito de fumar en la juventud es el uso de incentivos.
Objetivos
Evaluar el efecto de los incentivos sobre la prevención del inicio del hábito de fumar en niños y adolescentes (de 5 a 18 años de edad). También se intentó evaluar, cuando fue posible, la dosis‐respuesta de los incentivos, los costos de los programas de incentivos, si los incentivos son más o menos efectivos en combinación con otras intervenciones para prevenir la iniciación del hábito de fumar y cualquier consecuencia no intencional que surja del uso de incentivos.
Métodos de búsqueda
Para la revisión original (publicada en 2012) se realizaron búsquedas en el Registro Especializado del Grupo Cochrane de Adicción al Tabaco (Cochrane Tobacco Addiction Group Specialized Register), con búsquedas adicionales en las bases de datos de MEDLINE, Embase, CINAHL, CSA y PsycINFO para obtener términos en relación con los incentivos, en combinación con términos relacionados con el hábito de fumar y el consumo de tabaco, y los niños y adolescentes. Las búsquedas más recientes se realizaron en el registro especializado del Grupo Cochrane de Adicción al Tabaco (Cochrane Tobacco Addiction Group) en diciembre de 2016.
Criterios de selección
Se consideraron los ensayos controlados aleatorios (ECA) que asignaron al azar a niños y adolescentes (de 5 a 18 años de edad) como individuos, grupos o comunidades a las condiciones de intervención o de control, en los que la intervención incluyó un incentivo dirigido a la prevención del consumo de tabaco. También se consideraron los ensayos controlados (EC) con medidas iniciales y resultados posintervención.
Obtención y análisis de los datos
Dos autores de la revisión extrajeron y evaluaron de forma independiente los datos. El resultado primario fue la situación con respecto al hábito de fumar de los niños o adolescentes en el momento del seguimiento que informaron que no fumaban al inicio. Se requirió un seguimiento mínimo de seis meses desde el inicio y se evaluó los riesgos de sesgo de cada estudio incluido. Se utilizó la definición más rigurosa de abstinencia en cada ensayo; no se exigió la validación bioquímica del consumo de tabaco autoinformado para la inclusión de estudios. Cuando fue posible se combinaron los estudios aptos para calcular las estimaciones agrupadas en el seguimiento más largo, con el método de efectos fijos de Mantel‐Haenszel, mediante el agrupamiento de los estudios por diseño de estudio.
Resultados principales
Se identificaron tres ECA elegibles y cinco TC, que incluyeron los participantes de 11 a 14 años de edad, que no eran fumadores al inicio del estudio. De los ocho ensayos identificados, sólo seis tuvieron datos analizables relevantes para esta revisión que contribuyeron a los metanálisis (7275 participantes en total: 4003 intervención; 3272 control; 2484 participantes después de ajustar por agrupación). Todos los estudios excepto uno evaluaron el Smokefree Class Competition (SFC), que se ha ejecutado ampliamente en toda Europa. En este concurso, grupos de jóvenes generalmente de entre 11 y 14 años de edad se comprometen a no fumar durante un período de seis meses e informan su estado regularmente. Si un 90% o más del grupo no fuma al final de los seis meses, el grupo entra en un concurso para ganar premios. El único estudio que no fue un ensayo del SFC fue un ensayo controlado en el cual las escuelas de dos comunidades fueron asignadas a la intervención y las escuelas de una tercera comunidad actuaron como controles. Los estudiantes de la comunidad de intervención con tasas inferiores en cuanto al hábito de fumar al final del proyecto (un año escolar) recibieron recompensas.
La mayoría de los estudios dio lugar a resultados estadísticamente no significativos. Sólo un estudio del SFC informó un efecto significativo del concurso sobre la prevención del hábito de fumar en el seguimiento más largo. Sin embargo, este estudio tuvo un riesgo de sesgos múltiples, y cuando se calculó el cociente de riesgos (CR) ajustado ya no se detectó una diferencia estadísticamente significativa. El CR agrupado para los ECA más consistentes (3 estudios, n = 3056 participantes/1107 ajustado por agrupamiento) sugiere que no existe un efecto estadísticamente significativo de los incentivos, en forma del SFC, para prevenir la iniciación del hábito de fumar entre los niños y adolescentes a largo plazo (CR 1,00; intervalo de Confianza (IC) del 95%: 0,84 a 1,19). Los resultados agrupados de los ensayos no aleatorios tampoco detectaron un efecto significativo del SFC, y no fue posible extraer los datos sobre el resultado de interés del único ensayo que no estudió el SFC. Hay pocas pruebas consistentes para sugerir que las consecuencias no intencionales (como las afirmaciones falsas acerca de su situación con respecto al hábito de fumar y el acoso a los estudiantes que fuman) se asocian consistentemente con dichas intervenciones, aunque no ha habido mucha investigación sobre este tema. No hubo información suficiente para evaluar la relación dosis‐respuesta ni para informar los costos de los incentivos para prevenir el consumo de tabaco.
Se consideró que los ECA incluidos tenían un riesgo de sesgo poco claro, y que los que no eran ECA tenían un alto riesgo de sesgo. Con el uso de GRADE, se consideró que la calidad general de la evidencia del resultado primario fue baja (para los ECA) y muy baja (para los que no eran ECA), debido a la imprecisión (todos los estudios tuvieron intervalos de confianza amplios), y por los riesgos de sesgo identificados. Además, se redujeron las pruebas de estudios que no eran ECA, debido a problemas con el diseño de estos estudios, lo que probablemente introdujo sesgo adicional.
Conclusiones de los autores
Las pruebas muy limitadas actualmente disponibles indican que los programas de incentivos no previenen el inicio del hábito de fumar entre los jóvenes. No obstante hay relativamente pocos estudios publicados y los mismos son de calidad variable. Además, los ensayos incluidos en los metanálisis fueron estudios del SFC, que repartieron premios de tamaño pequeño a moderado a todos los grupos, generalmente mediante un sistema de lotería. Por lo tanto, es posible que otros programas de incentivos puedan tener más éxito en la prevención del consumo de tabaco entre los jóvenes.
Los estudios futuros podrían investigar la eficacia de un abanico más amplio de incentivos. incluyendo aquellos proporcionados a los participantes individuales para prevenir el consumo de tabaco, al mismo tiempo que consideran los efectos de los incentivos en el comienzo del hábito de fumar y en la progresión de este hábito. Resultaría útil si los incentivos se evaluaran en diversas poblaciones de diferentes procedencias étnicas y socioeconómicas y si se describieran los componentes de la intervención de forma detallada.
PICO
Resumen en términos sencillos
¿Los incentivos ayudan a evitar que los jóvenes comiencen a fumar en el plazo medio a largo?
Antecedentes
La mayoría de fumadores empiezan a fumar antes de los 18 años. El inicio del hábito de fumar en una etapa temprana de la vida significa que la persona fumará durante más años que alguien que comienza a fumar en una etapa posterior, lo cual aumenta los riesgos del hábito de fumar para la salud. Debido al gran consumo de tabaco entre los jóvenes y los posibles resultados de salud deficientes en el futuro, encontrar maneras de prevenir el hábito de fumar es una prioridad de la salud pública. Un nuevo enfoque a la prevención del inicio del hábito de fumar en los jóvenes es el uso de incentivos, mediante los cuales los jóvenes o grupos de jóvenes son premiados al no fumar. El objetivo de esta revisión fue evaluar el efecto de los incentivos sobre la prevención del inicio del hábito de fumar en niños y adolescentes (de 5 a 18 años de edad).
Características de los estudios
Ésta es una actualización de una revisión anterior. La primera versión fue publicada en 2012 e incluyó siete estudios. Para esta actualización, se buscaron nuevos estudios en diciembre de 2016 y se encontró uno. Esta revisión incluye ahora ocho ensayos. Siete de los cuales fueron ensayos del Smokefree Class Competition (SFC), que se ha utilizado ampliamente en toda Europa. En este concurso, varias clases (generalmente de entre 11 a 14 años de edad) prometen no fumar durante un período de seis meses. Informan regularmente sobre su situación con respecto al hábito de fumar y si un 90% o más del grupo no fuma al final de los seis meses, el grupo entra en un concurso para ganar premios. En el único ensayo que no analizó el SFC, las clases con el porcentaje más pequeño de estudiantes que fumaban al final del año escolar recibieron recompensas.
Resultados clave
Se evaluaron los resultados de siete ensayos del SFC y se encontró que el concurso no tuvo un impacto significativo sobre si los jóvenes comenzaron a fumar. Puesto que solo hubo un ensayo que no fue del SFC, se concluyó que no hubo suficiente información para evaluar si este programa fue efectivo para evitar que los jóvenes comiencen a fumar. Los posibles efectos negativos del SFC no se han investigado ampliamente, pero los datos disponibles indican que el programa SFC no tiene ningún efecto negativo significativo.
Calidad de las pruebas
La calidad general de la evidencia se consideró baja o muy baja debido a que está sesgada por un bajo número de estudios, con efectos imprecisos y un riesgo de sesgo alto o incierto.
Authors' conclusions
Summary of findings
| Smokefree Class Competitions (SFC) for preventing smoking uptake | |||||
| Patient or population: Children and adolescents aged 5 ‐ 18 years who were non‐smokers at baseline Settings: Schools in Germany, the Netherlands, Finland, Switzerland, Canada and the United States Intervention: Participation in SFC Comparison: No participation in SFC | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants Actual number/ effective number2 | Quality of the evidence | |
| Assumed risk1 | Corresponding risk | ||||
| Smoking uptake at longest follow‐up (RCTS) | 317 per 1000 | 320 per 1000 | RR 1.00 (0.84 to 1.19) | 3056/1108 (3) | Low3, 4 |
| Smoking uptake at longest follow‐up (Non‐RCTs) | 158 per 1000 | 132 per 1000 | RR 0.82 (0.63 to 1.08) | 4219/1377 (3) | Very low3, 5, 6 |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1'Assumed risk' calculated as risk in control groups. | |||||
Background
Description of the condition
In 2015, smoking was the second leading risk factor globally for early death and disability. It is estimated that 6.4 million deaths, 11.5% of all deaths worldwide, were attributable to smoking (Reitsma 2017). Global projections of mortality data estimate that unless urgent action is taken on tobacco control, total tobacco‐attributable deaths will increase to over 8 million by 2030 (Mathers 2006).
Data from the Global Youth Tobacco Survey (2000 to 2007) revealed that approximately 10% of students aged 13 to 15 years smoked cigarettes, with prevalence ranging from 5% in the Eastern Mediterrranean to 19% in the European Region (Warren 2008). In the United States, surveillance data from 2015 found that 9.3% of high school students (grades 9 to 12) had smoked cigarettes, 8.6% had smoked cigars and 7.2% had smoked hookah in the 30 days before the survey. Although use of cigarettes and cigars declined in the period 2011 to 2015, use of hookah increased. Prevalence was higher among male than female students for cigarettes (10.7% versus 7.7%), cigars (11.5% versus 5.6%) and hookah (7.4% versus 6.9%) (Singh 2016).
Adult smoking usually has its roots in adolescence (USDHHS 2012). If individuals do not take up smoking during this period it is unlikely that they ever will (Mayhew 2000). Moreover, once smoking becomes established, cessation is challenging; the probability of subsequently quitting is inversely proportional to the age of initiation (Breslau 1996). Unfortunately, most smokers initiate the behaviour before 18 years of age; indeed, among those who smoke cigarettes, nearly 25% of young people have reported smoking their first cigarette before the age of 10 (GYTS 2002).
Earlier onset of smoking provides for more life‐years of tobacco use, thereby increasing the associated health risks, including respiratory conditions, cardiovascular disease and cancers (USDHHS 2012). Earlier onset is also associated with heavier use, with heavier tobacco users less likely to quit smoking and therefore more likely to experience tobacco‐related health problems (Breslau 1996).
Given the prevalence of tobacco use among young people and the corresponding health burden into the future, strategies to prevent smoking in adolescence are a public health priority. Currently, public health policies and programmes aimed at reducing tobacco use among adolescents have demonstrated varying levels of success. Tax increases on tobacco products have been found to be successful in reducing smoking among this target group (USDHHS 2012), and there is evidence for the effectiveness of mass media campaigns (Brinn 2010; USDHHS 2012). The evidence for the long‐term effectiveness of community and school‐based programmes reported in the literature has been inconsistent over the years. However, the 2012 US Surgeon General's report on preventing tobacco use among youth and young adults (USDHHS 2012) suggests that co‐ordinated, multicomponent community programmes may be able to reduce smoking among young people; the mix of strategies and the reach of the programme are likely to affect results. Similarly, selected school‐based smoking prevention programmes have demonstrated successful long‐term outcomes. Successful programmes are generally intensive, comprehensive, interactive, start early and are sustained, and are integrated into a community‐level approach (USDHHS 2012).
One novel approach to reducing the prevalence of smoking is the use of incentives. An incentive may be defined as "any tangible benefit externally provided with the explicit intention of promoting positive health, educational or social behavioural change" (Kavanagh 2011, p. 193). There is growing interest in the use of incentives schemes to encourage young people to adopt healthy and pro‐social behaviours (Kavanagh 2011). A review of incentives programmes to improve health, education and other social behaviours in youth aged 11 to 19 years identified nine studies which focused on healthy behaviours (Kavanagh 2011). A meta‐analysis of these studies found a statistically significant positive impact, although the number of studies was small, as were some of the sample sizes. Three studies in this review were anti‐smoking interventions; a meta‐analysis of two of the three studies showed a statistically significant effect of anti‐smoking competitions on daily smoking rates at one‐year follow‐up (risk ratio (RR) 1.05, 95% confidence interval (CI) 1.02 to 1.08). The efficacy of anti‐smoking competitions for preventing smoking initiation was not reported.
Description of the intervention
Incentives may take the form of contests, competitions, incentive schemes, lotteries, raffles, and contingent payments. This range of incentives has been more extensively reviewed for its effectiveness for encouraging cessation and continued abstinence in smoking cessation programmes.
A Cochrane Review of incentives and contingency management programmes for smoking cessation found that they appear to boost cessation rates while they are in place (Cahill 2015). Sustained success rates beyond the reward schedule were achieved in work site‐based trials, with substantial cash payments for abstinence. Incentive schemes conducted among pregnant smokers were also found to improve cessation rates. This review reflected a shift in the debate about incentives, from feasibility to the relative success or limitations of the mechanisms deployed, and contributed to a growing evidence base which defines the rationale for incentive‐based programmes. The findings contrast with earlier Cochrane Reviews of ‘Quit and Win’ contests (Cahill 2008) and the use of competitions and incentives for smoking cessation (Cahill 2011), which both noted a lack of high‐quality trials, limiting their conclusions. Additionally, in the case of Cahill 2011, most incentives in the included studies were small.
Incentive schemes have also been used for managing chronic conditions, avoiding sexually transmitted infections and for weight loss, and have been used in education (Marteau 2009) and exercise adherence (Mitchell 2013). Systematic reviews of the wider literature relating to incentives for encouraging healthy behaviours have found that incentives are effective in stimulating ‘simple,’ discrete behavioural changes (e.g. clinic attendance) (Jochelson 2007; Kane 2004). Incentives aimed at more complex lifestyle behaviours (e.g. smoking and sexual behaviour) have been found to be successful in increasing participation in health promotion programmes, but once the incentive is withdrawn participants tend to revert to former behaviours (Jochelson 2007). It has also been argued that the size of the incentive is important, with higher‐value incentives more powerful in encouraging behaviour change and participation in lifestyle programmes (Jochelson 2007), and incentive effects increasing among recipients with high deprivation levels (Mantzari 2015).
How the intervention might work
Incentives operate on learning theory principles by giving an immediate reward for behaviours that will provide health gains in the future. In the field of behavioural economics, research has found that people are motivated by the experience of past rewards and the prospect of future awards (Carmerer 1999). Moreover, the desire to avoid regret (i.e. not being rewarded) can be a strong force in decision‐making under risk (Connolly 2006). Incentive schemes are also framed around what is termed “present bias,” a tendency of humans to pursue immediate rewards ahead of rewards that are distant but more highly valued (Volpp 2008). Marteau 2009 highlighted some unintended consequences of incentives, including the undermining of a participant’s intrinsic motivation (Kane 2004) and informed consent, as well as the potential for damaging the trust between health professionals and their patients.
Why it is important to do this review
There is considerable interest in the use of incentives to encourage cessation or prevent smoking. It is conceivable that incentives may be more successful with a young target group, who may be more sensitive to monetary rewards, and who might find it easier to not start smoking compared to the more complex task of quitting once dependent on nicotine. The Smokefree Class Competition Programme, which started in 1989, continues to operate in several European countries (European Commission 2016).
In the last 10 years, there has been considerable evolution of the debate around incentives, and the most recent review of incentives for smoking cessation (Cahill 2015) has contributed to the evidence base for incentive‐based programmes and identified further areas for investigation. Given the magnitude of the problem globally of youth smoking uptake, this is an area worthy of further investigation.
Objectives
To assess the effect of incentives on preventing children and adolescents (aged 5 to 18 years) from starting to smoke. Our review aimed to address the following questions:
-
Do incentives prevent children and adolescents from starting to smoke tobacco?
-
Does the amount and type of incentive affect prevention of smoking initiation?
-
What are the cost implications of incentives to the community?
-
Are incentives more or less effective in combination with other interventions to prevent smoking initiation?
-
What are the unintended consequences arising from the use of incentives (e.g. false claims, ineligible applicants)?
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials allocating individuals, groups or communities to intervention or control conditions.
Controlled trials with baseline measures and post‐intervention outcomes. We included non‐randomized controlled trials in this review, to widen the evidence base in an area where literature is currently sparse. We recognise that potential biases are likely to be greater for non‐randomized studies compared with randomized trials (Higgins 2011). We therefore conducted separate meta‐analyses for randomized and non‐randomized studies.
We excluded cross‐sectional studies where observations of random groups of participants were made before and after the intervention, as these did not necessarily provide data on the smoking status of the same individual participants who reported no smoking at baseline.
Types of participants
Children (aged 5 to 12 years) and adolescents (aged 13 to 18) in any setting. Our population of interest were baseline non‐smokers, as we were interested in the efficacy of incentives in preventing smoking initiation. We used the definition of non‐smoker as provided in each study.
Types of interventions
We adapted the definition of 'incentive' provided by Kavanagh 2011. Our definition of an incentive was any tangible benefit externally provided with the explicit intention of preventing smoking. This includes contests, competitions, incentive schemes, lotteries, raffles, and contingent payments to reward not starting to smoke, thereby remaining a non‐smoker. We included rewards to third parties (e.g. to schools, healthcare providers or family members), as well as interventions that directly rewarded children and adolescents.
For each study, we attempted to determine whether the participants received any other smoking interventions such as smoking education in school, and whether the control group received any interventions. Any comparator groups were deemed eligible.
Types of outcome measures
Primary outcomes
The primary outcome was smoking status at longest follow‐up of children or adolescents who reported no smoking at baseline. While the gold standard for this review was biochemically‐verified sustained abstinence from smoking, we used the outcomes defined by the included trials and have included trials that did not use biochemically‐verified outcomes. We have reported smoking status defined by the strictest criteria (i.e. where pupils who had ever smoked within the designated follow‐up period were defined as current smokers) at the longest follow‐up for each study, with a minimum follow‐up of six months from baseline (the start of the intervention).
Secondary outcomes
We aimed to assess the dose‐response of the amount of incentive, but there were insufficient data with which to do so. Where possible, we report narratively on the costs and any unintended harms from the use of incentives.
Search methods for identification of studies
Electronic searches
For the original version of the review (published 2012), we undertook searches of the Cochrane Tobacco Addiction Group Specialized Register (Appendix 1), alongside the following databases: MEDLINE (Appendix 2, 1947 to 24th May 2012); Embase (Appendix 3, 1980 to 2012 week 20); CINAHL (Appendix 4, 1937 to 24th May 2012); PsycINFO (Appendix 5, 1806 to 24th May 2012); CSA (Appendix 6, search date 24th May 2012, ASSIA from 1987, ERIC from 1986, PAIS from 1972, Sociological Abstract from 1952).
We conducted updated searches in December 2016. We searched the Cochrane Tobacco Addiction Group Specialized Register (Appendix 1), which includes studies identified by systematic electronic searches of multiple databases, and handsearching of specialist journals and the 'grey' literature (conference proceedings and unpublished reports not normally covered by most electronic databases). At the time of the search the Register included the results of searches of the Cochrane Central Register of Controlled trials (CENTRAL), issue 11, 2016; MEDLINE (via OVID) to update 20161202; Embase (via OVID) to week 201650; PsycINFO (via OVID) to update 20160926. See the Tobacco Addiction Group Module in the Cochrane Library for full search strategies and a list of other resources searched.
Searching other resources
We checked cited studies while reviewing trial reports, and attempted to contact trial authors for any required unpublished data. We also searched across multiple registers in Current Controlled Trials (www.controlled‐trials.com/) and in the Australian and New Zealand Trials Registry (www.anzctr.org.au/trialSearch.aspx), using all keyword combinations for study protocols of completed and ongoing trials. We did not apply any language restrictions.
Data collection and analysis
There were three stages in the data collection and analysis process, outlined below.
Stage 1: Selection of studies
The Information Specialist of the Cochrane Tobacco Addiction Group prescreened all studies identified in the electronic search for possible inclusion in this update. We rejected articles at this stage if the title or abstract or both did not focus on the impact of incentives on preventing youth smoking. If we could not categorically reject the article on the basis of title and abstract, two review authors (MH and DT) obtained and screened the full text.
Two review authors (MH and DT) independently assessed the relevant studies for inclusion, resolving discrepancies by consensus and reporting reasons for the non‐inclusion of studies (these appear in the Characteristics of excluded studies tables). While we planned for the Cochrane Tobacco Addiction Group editorial team to resolve any ongoing disagreements between the two review authors, this proved to be unnecessary.
Stage 2: Data extraction and assessment of risk of bias
Two review authors (MH and DT) independently extracted the following data into a data extraction form:
-
Study design, including inclusion and exclusion criteria, method of randomization (if used)
-
Setting (e.g. country, multicentre or single centre, inpatient or outpatient, etc.)
-
Demographics of participants, including average age, sex, socioeconomic status, smoking status
-
Intervention and control description
-
Primary outcome measure, including definition of abstinence and length of follow‐up, measurements used including any biochemical verification
The two review authors also assessed the risks of bias by including their judgement in the data extraction table of the following:
-
Was the sequence generation adequate?
-
Was allocation concealed?
-
Who was blinded?
-
Were incomplete data addressed? (e.g. was there an intention‐to‐treat analysis? What was the attrition rate? Was there differential attrition by group assignment or by baseline smoking status?)
-
Was the study free of selective reporting? (e.g. were all of the study's prespecified outcomes reported?)
-
Was the study free of detection bias? (e.g. was there biochemical verification of self‐reported smoking status? In cases of self‐report, did participants believe their answer would affect their receipt of incentives?)
The two review authors compared their data extraction forms and resolved discrepancies by consensus.
Stage 3: Analysis
Where possible, we contacted the trial authors to request missing data. We excluded participants for whom no outcome data were available, rather than conducting an intention‐to‐treat analysis of all randomized participants with imputed values for the missing data. In smoking cessation trials it is generally accepted that missing data should be imputed as ‘failures’ (i.e. smoking), as this is a conservative approach and is a plausible outcome in such trials. In most other instances an imputation approach is generally not recommended, because studies with imputed data may be given more weight than they deserve if entered as dichotomous data and none of the assumptions made when imputing data are likely to reflect the truth (Higgins 2011). Proceeding with an available‐case analysis is a more conservative approach than imputing that those lost to follow‐up have not started smoking. This approach produces a less conservative result compared with imputing that those lost to follow‐up all started smoking, but we do not think this is particularly plausible in this context.
We calculated a risk ratio (RR) for the outcome for each trial, defined as (number of smokers in the intervention group who were non‐smokers at baseline/total number of baseline non‐smokers randomized to the intervention group) / (number of smokers in the control group who were baseline non‐smokers/total number of baseline non‐smokers randomized to the control group). We obtained adjusted RRs from cluster‐randomized trials, using schools as the unit of analysis, by adjusting the original (non‐adjusted) RRs using an intraclass correlation coefficient (ICC) of 0.097 (ICC for current smoking status averaged among all ethnicities), as reported by Siddiqui 1996. An RR less than 1 favoured the intervention, indicating that more participants refrained from smoking in the intervention group compared to the control group.
We used the Chi2 test and the I2 statistic to assess heterogeneity among studies and found no evidence of significant heterogeneity, reflecting the fact that the included trials were sufficiently homogeneous in terms of participants, interventions and outcomes assessed. We therefore combined eligible studies to calculate an estimated pooled weighted average of RRs using the Mantel‐Haenszel fixed‐effect method, with a 95% confidence interval. We performed separate meta‐analyses for randomized and non‐randomized controlled trials.
Assessment of reporting biases
We had planned on preparing a funnel plot to investigate for the possibility of reporting biases (if there were at least 10 included studies). There were too few studies to carry this out.
Subgroup analyses
In the event of significant heterogeneity, we had planned for possible subgroup analyses including: type of intervention (solely financial rewards versus financial rewards plus other smoking cessation intervention; staged versus one‐off incentive); type of incentive (individual versus rewards to third parties; lottery versus definite payment of a specified reward amount); and size of the incentive (low, high). Owing to the fact that we found no significant heterogeneity among studies and because there were insufficient data, we did not carry out these analyses.
Sensitivity analysis
While we performed separate meta‐analyses for randomized and non‐randomized controlled trials, there were too few studies to undertake a sensitivity analysis by first including, then excluding less rigorous trials (as originally planned).
Summary of findings table
Following standard Cochrane methodology, we created a 'Summary of findings' table for the primary outcome. We assessed the evidence from the randomized and non‐randomized controlled trials separately. Also following standard Cochrane methodology, we used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for the primary outcome.
Results
Description of studies
We identified 182 potentially relevant new records in our updated search conducted in December 2016 (Figure 1). The Information Specialist of the Cochrane Tobacco Addiction Group reviewed the titles and abstracts, and excluded records that clearly did not relate to the research question. Full text records were retrieved from databases for evaluation. The review authors found one additional record, which had been listed in the original (2012) review as an ongoing study. Two review authors (MH and DT) checked the four relevant studies and evaluated them against the prespecified inclusion criteria. We identified one controlled study that met our inclusion criteria, which we added to the seven studies included in the previous review. We list 32 excluded studies in the Characteristics of excluded studies table, with reasons for their exclusion.

PRISMA study flow diagram of search results
Included studies
All of the eight included studies rewarded smoking abstinence with a minimum follow‐up period of six months after the start of the intervention. We give full details of the included studies in the Characteristics of included studies table. Where there were multiple reports of the same study, these appear in the reference list of 'included studies', with the primary report indicated by an asterisk.
All included studies took place in a school setting. Three studies were undertaken in Germany (Isensee 2012a; Schulze 2006; Wiborg 2002), and one each in the Netherlands (Crone 2003), Finland (Vartiainen 1996), Switzerland (Stucki 2014), Canada (Kairouz 2009) and the USA (Burke 1992). All studies were cluster‐controlled trials, with allocation by school. Three studies were randomized controlled trials (Crone 2003; Isensee 2012a; Schulze 2006), and the rest were controlled trials, without randomization.
Target group of intervention
All of the studies targeted school students. Kairouz 2009 enrolled primary school students (sixth grade classes, typically aged 11 to 12). The remaining studies targeted junior high school students (seventh and eighth grades, typically 12 to 14 years old).
Types of incentives
All but one (Burke 1992) of the included studies were trials of the 'Smokefree Class Competition' (SFC) intervention, or a closely related variant. The SFC originated in Finland in 1989 and since then has grown into one of the largest smoking prevention programmes in Europe (Hanewinkel 2010), with funding from the European Commission. The general requirements for the competition are as follows: (i) at least 90% of the class must agree to participate (i.e. participation is voluntary); (ii) classes sign a contract and commit to remain smoke‐free for six months (usually defined as greater than or equal to 90% of the class is non‐smoking); (iii) classes and teachers monitor the smoking status of students and report regularly to the competition organisers as to whether at least 90% of the class remains non‐smoking (usually monthly) (IFT‐NORD 2009). If classes report that less than 90% of the class are smoke‐free, they are dropped from the competition. At the end of the six months, the classes in the competition that have remained smoke‐free have the chance of winning a prize, usually through a prize draw or lottery.
There is some flexibility in the implementation of the SFC to allow different countries to adapt the programme to suit their context. This is evident in the studies included in this review. In addition to the main competition prize, classes may be awarded other incentives for participating (Kairouz 2009). The final prize draw may also be contingent on additional factors. For example, in Crone 2003 competition prizes were available to six classes with less than 10% smoking and a "photo best expressing a non‐smoking class" (p. 676), decided by a jury panel. In other studies, it is clear that smoke‐free classes went into a lottery to win a prize (Schulze 2006; Vartiainen 1996). In Kairouz 2009, Stucki 2014 and Wiborg 2002, it is less clear exactly how the prizes were awarded to smoke‐free classes. Definitions of 'smoke‐free' also differed. Vartiainen 1996 defined smoke‐free classes as classes who reported 100% non‐smoking; the other studies in this review set a tolerance level of 90% or more smoke‐free.
The prizes in the included SFC trials ranged from special activities (e.g. hip‐hop classes, Kairouz 2009) to monetary prizes (Crone 2003; Vartiainen 1996) and class trips (Isensee 2012a; Schulze 2006; Vartiainen 1996; Wiborg 2002). Several studies did not provide detailed accounts of the type and amount of incentives. Kairouz 2009 reported that teachers and students received participation incentives but did not detail what these were. They also reported that "participating classes were eligible for a half‐day surprise activity (e.g. a hip‐hop dance with a DJ) (p. 475), but did not report whether this was specifically the competition prize or how eligible classes were selected to receive these activities, and we were unable to obtain further details from the authors. We have assumed in the absence of further information that the half‐day surprise activities were awarded to smoke‐free classes. Isensee 2012a, Schulze 2006 and Wiborg 2002 all reported that the grand prize was a class trip. They reported awarding other prizes to smoke‐free classes, but did not elaborate on these.
Monetary prizes were distributed in the trials conducted by Crone 2003 and Vartiainen 1996. In Crone 2003, prizes of EUR 220 to EUR 450 were given to six classes with less than 10% smoking and "a photo best expressing a non‐smoking class" (p. 676). In Vartiainen 1996, smoke‐free classes entered a lottery to win four main prizes of USD 2000 and 10 second prizes of USD 200; the grand prize was a class trip. In this study, prize money could be used in any way the winning classes chose.
The one study that was not a trial of the SFC (Burke 1992) was a controlled trial in which schools in two communities were assigned to the intervention, with schools in a third community acting as controls. In the first competition, intervention communities competed against each other and students in the community with lower smoking rates at the end of the project were rewarded with a movie pass and a voucher for free ice‐cream. In a second competition, students in the intervention classes with most improved knowledge about smoking were rewarded with a T‐shirt with the project logo on it.
Incentives as part of a larger programme, or stand‐alone
Five studies reported combining the competition with some education about the health effects of smoking (Burke 1992; Crone 2003; Kairouz 2009; Schulze 2006; Vartiainen 1996). In Burke 1992, both intervention and control classes received an education programme (six sessions) about the health and social effects of smoking which included skills training for resisting peer and media pressures to smoke.
In the trials of SFC competitions, Vartiainen 1996 reported that contact teachers in the classes organized health education sessions about smoking, but it was not clear whether these sessions were delivered to both intervention and control groups. Crone 2003 reported that intervention classes received three lessons on knowledge, attitudes and social influence before classes signed the contract not to smoke for five months. Additionally, two video lessons on smoking and social influence were available as an optional extra during the intervention period. In Schulze 2006, the intervention included weekly curricula consisting of health information about smoking and strategies for how to quit smoking and resist peer pressure to smoke. Kairouz 2009 reported that the intervention arm received a six‐month programme consisting of didactic material, a teacher's guide and resources to improve knowledge about health and social effects of smoking. The dose and frequency of this programme was not clear.
Theoretical basis of the intervention
The best practice guide for the SFC competition (IFT‐NORD 2009) reports that the SFC relies on four theoretical models for behaviour modification. The first is learning theory, which asserts that positive reinforcement increases the probability of producing a given desirable behaviour, such as not smoking. The SFC also incorporates a 'social contract' to remain smoke‐free. The second is social learning theory, which states that people learn from one another through observation, imitation, and modelling. In the SFC, students serve as models for non‐smoking behaviour for their peers. Thirdly, the theory of planned behaviour states that personal attitude, subjective norms, and perceived behavioural control together shape an individual's behaviours. Finally, SFC relies on developmental psychology, in that the developmental orientation of adolescents is towards short‐term goals, and hence the competition's emphasis is on positive short‐term consequences of non‐smoking behaviour. The studies that trialled the SFC variously reported an underpinning theoretical framework.
Crone 2003 based their intervention on a 'social influence' model, relying on peer pressure directed at young people to both resist smoking and to promote not starting to smoke. Kairouz 2009 reported that the premise for their intervention rested on positive reinforcement for not smoking to stimulate a desired behaviour, but did not reference a specific social theory. Isensee 2012a reported that the intervention was based on principles of correcting social norms (i.e. correcting the common overestimation of smoking by adolescents) and fostering commitment to a social contract; Stucki 2014 referenced Isensee 2012a to provide the theoretical basis for their intervention. Wiborg 2002 cited learning theory as the theory underpinning the SFC competition trialled in Germany, reported in this paper. Schulze 2006 and Vartiainen 1996 did not report an underlying theoretical framework for the intervention, but both were trials of the SFC.
Burke 1992 referenced Fishein and Ajzen's (Ajzen 1977) theory of reasoned action as the theoretical framework for their intervention. This theory posits that preventing the initiation of a voluntary behaviour, such as smoking, is dependent on changing smoking‐relevant beliefs or subjective norms, or both. Burke 1992 used group competitions with rewards as persuasive interventions designed to change beliefs and norms.
Risk of bias in included studies
Summary assessments of the risk of bias for key areas in each of the included studies are shown in Figure 2 and Figure 3. Full details of 'Risk of bias' assessments for each study can be found in the Characteristics of included studies table.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Randomization, sequence generation and allocation concealment
Three studies were randomized controlled cluster trials (Crone 2003; Isensee 2012a; Schulze 2006). Isensee 2012a and Schulze 2006 stratified schools according to school type (‘Gymnasium’ and ‘Sekundarschule’ schools; gymnasium schools enrol high academic‐achieving students). In the remaining five studies randomization was not used (Burke 1992; Kairouz 2009; Stucki 2014; Vartiainen 1996; Wiborg 2002).
In two of the five quasi‐experimental studies, the control group was matched to the intervention group (Kairouz 2009; Wiborg 2002). In Kairouz 2009, two control schools were matched to each intervention school according to location and a social deprivation index. In Wiborg 2002, the same proportion of classes from different grades and school types as in the intervention group was randomly selected from classes in a city in Germany that had not been invited to participate in the competition. Burke 1992, Stucki 2014 and Vartiainen 1996 did not match intervention and control groups.
Two of the three RCTs (Crone 2003; Isensee 2012a) reported adequate randomization procedures (sequence generation and allocation concealment). The other RCT (Schulze 2006) did not report their process for sequence generation or allocation concealment.
Several studies reported significant differences between intervention and control groups at baseline, which is not uncommon in cluster‐randomized trials where groups and not individuals are the unit of randomization. Burke 1992 and Kairouz 2009 did not provide data on demographics (age, sex, socioeconomic status (SES)) or smoking status for either intervention or control groups at baseline. Stucki 2014 reported differences in age, class atmosphere and number of smoking peers. Kairouz 2009 did report a comparison of baseline characteristics for those who completed follow‐up, with significant differences by age, school location and social deprivation index (adjusted for in their analyses). Vartiainen 1996 only provided a baseline comparison on smoking status. A higher proportion of the control group reported daily smoking at baseline compared with the intervention group, which was adjusted for in the final reported analysis. Wiborg 2002 did not report baseline group differences in SES or ethnicity. Smoking prevalence at baseline was higher in the control group than in the experimental group, although the difference was not statistically significant. There were no baseline differences in age or sex.
Overall, we judged the three RCTs (Crone 2003; Isensee 2012a; Schulze 2006) to be at low or unclear risk of selection bias. However the three non‐RCTs (Kairouz 2009; Stucki 2014; Wiborg 2002) were all at high risk of selection bias.
Blinding (performance bias and detection bias)
None of the included studies adequately described whether participants or personnel were blinded during the study, but it is unlikely, given the nature of this type of intervention. We considered that despite this, the outcome was unlikely to have been significantly influenced by lack of blinding.
In most of the studies that evaluated the SFC (Crone 2003; Isensee 2012a; Schulze 2006; Vartiainen 1996; Wiborg 2002) we judged the risk of detection bias as low, as efforts were made by study investigators to dissociate the collection of results from the SFC itself, and we therefore judged differential misreport between the two groups to be unlikely. None of the included studies reported on whether the research investigators were blinded when it came to analyzing study outcomes. Kairouz 2009 reported that there were significantly more students in the intervention group who reported ever smoking at baseline but subsequently denied ever smoking at follow‐up, compared with control (24% versus 16%). We therefore judged this study to be at high risk of detection bias.
None of the studies trialling the SFC used biochemical verification of self‐reported smoking status. Some authors argue that interpretation of cotinine results in a population who are likely to be smoking sporadically, rather than daily, would not be meaningful (Crone 2003; Kairouz 2009).
Burke 1992 (the only study that was not a trial of the SFC competition) did not report whether the research investigators were blinded to participants' group allocation when analyzing the data. Saliva samples were collected when the surveys were administered, to measure salivary thiocyanate (TCN). They used the TCN results to justify reliance on self‐report, except at baseline, when 39 self‐reported ‘never smokers’ were reclassified as ‘occasional smokers.’ As a result we rated the study at high risk of detection bias.
Incomplete outcome data
With the exception of Stucki 2014 and Burke 1992, all studies struggled with significant attrition at longest follow‐up. Burke 1992, Isensee 2012a and Stucki 2014 were the only studies assigned a low risk for attrition bias: Stucki 2014 and Burke 1992 had only small numbers lost to follow‐up, and Isensee 2012a conducted attrition analyses and found interaction effects only for age and school type.
We rated three studies which found differential attrition by smoking status or group assignment, or in which over half of the participants were lost to follow‐up, at high risk of attrition bias (Crone 2003; Schulze 2006; Wiborg 2002). We judged the remaining studies to be at unclear risk as, although over 50% of participants were followed up, it was unclear if differential attrition was present.
Differential attrition between the two groups of baseline non‐smokers could put the results at risk of bias. For example, if more baseline non‐smokers were lost to follow‐up at in the control group, this might bias the results towards overestimating the effect of the intervention in preventing smoking. As two of the three RCTs were at high risk of attrition bias, (Crone 2003; Schulze 2006) these were downgraded one level according to the GRADE assessment.
Selective reporting
For all included studies there was insufficient information for us to make an assessment of risk of reporting bias, and we therefore rated all studies as 'unclear'. None of the records clearly identified our prespecified primary outcomes. Only one study referred to a published study protocol (Isensee 2012a). While the study publication reported on smoking status (the only primary outcome relating to behaviour), it did not report on other study outcomes, such as knowledge, attitudes and intention to use tobacco (Hanewinkel 2007b).
Effects of interventions
See: Summary of findings for the main comparison
Outcomes
Only one study (Burke 1992) included a biochemical assessment of smoking status. The rest relied on self‐report. Definitions of smoking at follow‐up differed between the studies. Crone 2003 defined smoking at follow‐up as current smoking (including daily, weekly and experimental smokers). The definition of current smoking used by Schulze 2006 also included irregular (less than weekly) smoking. Wiborg 2002 measured four‐week prevalence of smoking, and Vartiainen 1996 measured daily smoking as the outcome variable. Stucki 2014 measured six‐month and one‐month smoking prevalence. In Kairouz 2009 and Isensee 2012a, the outcome was defined as 'ever smoking' (even just a puff). Only one study used a different definition of smoking at baseline than at follow‐up. Schulze 2006 defined 'current smokers' at baseline as regular smokers whereas at follow‐up 'current smokers' included both regular and irregular (at least one a week) smokers.
Where possible we have used the most conservative definition (i.e. ever smoking) in assessing the effects of the intervention. This measure is thought to be most representative of smoking initiation among baseline non‐smokers. Raw outcome data, especially in the earlier studies, were often difficult to extract and we needed to contact the authors of seven of the eight included studies for more data. Four of the seven authors provided additional data for the 2012 review (Crone 2003; Isensee 2012a; Wiborg 2002), and this update (Stucki 2014) .
All studies reported a follow‐up period from the start of the intervention of more than six months. The shortest long‐term follow‐up was reported by Stucki 2014 (approximately seven months) and the longest was 24 months (Schulze 2006).
Results
Primary outcome
Of the eight trials identified, only six had analyzable data relevant for this review and contributed to meta‐analyses (7275 participants who were non‐smokers at baseline; 4003 in intervention and 3272 in control). After adjusting for clustering the effective sample size was 2484 participants; 1320 intervention and 1164 control. Due to different reporting methods used, and participants included, we were unable to quantify the total number of participants in the included studies. The pooled risk ratio (RR) for the more robust randomized controlled trials (RCTs) (3 studies, n = 3056, 1108 after adjusting for clustering) suggests that, from the available data, there is no statistically significant effect of incentives on preventing smoking initiation among children and adolescents in the long term (RR 1.00, 95% confidence interval (CI) 0.84 to 1.19, Analysis 1.1). The confidence interval indicated that participants in the SFC may be anywhere between 16% less likely and 19% more likely to initiate smoking, compared with those who do not take part in an SFC. The pooled result from the three controlled trials (CTs) also did not detect a significant effect (RR 0.85, 95% CI 0.65 to 1.11) (3 studies, n = 4219 participants, 1377 after clustering adjustment). Details of the results of the eight included studies in this review are tabulated in Analysis 2.1 and Analysis 2.2. In these tables, we have reported smoking status at the longest follow‐up, including both the summary statistics provided in the original trial reports (if available) and our adjusted RRs.
Burke 1992 and Vartiainen 1996 did not provide data at follow‐up for the outcome of interest for this review (smoking status of participants who reported no smoking at baseline). Burke 1992 analyzed mean salivary thiocyanate (TCN) levels between groups at 18 months follow‐up and found a non‐significantly higher mean TCN level among baseline never‐smokers in intervention (560 mcg/mL, standard deviation (SD) 403) versus control participants (514 mcg/mL, SD 424). Vartiainen 1996 reported on the increase in daily smoking prevalence at follow‐up. There was a short‐term effect of the intervention, with a lower daily smoking prevalence in the intervention (11.1%) versus the control group (16.4%) at one month after the competition, but this was not sustained in the long term. From baseline to longest follow‐up (18 months), daily smoking increased by 10.8% in the intervention group and 11.2% in the control group.
Of the remaining six studies (all trials of the SFC intervention), four (Crone 2003; Isensee 2012a; Kairouz 2009; Stucki 2014) appropriately accounted for the clustered design in the analyses of their data. For consistency, we reanalyzed the data from all six studies to account for clustering and to enable us to conduct a meta‐analysis as planned using the Mantel‐Haenszel fixed‐effect method. In order to run these analyses, we needed to know the number of clusters (schools) at follow‐up for each study. We were able to extract these data from the paper or obtain them directly from authors for all of the studies, expect for one (Wiborg 2002). In the case of Wiborg 2002, we knew the number of classes in both groups at follow‐up and used these data to estimate a plausible number of schools. The authors reported that five classes did not participate in the study due to organizational and structural changes in their schools, indicating that these classes were from more than one school. Assuming that these classes were from at least two schools, we estimated a number of classes per school ratio (5/2 = 2.5). We then estimated the number of schools in the intervention and control groups, based on this ratio. The classes/school ratio (2.5) estimated for Wiborg 2002 is similar to that of two other studies (Isensee 2012a; Schulze 2006) for which we had data but less than in Crone 2003 (7.5). While we did not adjust for any baseline differences between the groups in these five trials, our results are similar to authors' adjusted analyses where these have been reported.
Only one study, a non‐randomized controlled trial (Wiborg 2002), reported a significant effect of the intervention on the prevention of smoking at the longest follow‐up. At the post‐test (six months after the start of the intervention and one month after the intervention ceased), Wiborg 2002 reported a significant difference in four‐week smoking prevalence in the intervention versus the comparison group. Of the intervention students, 7.8% reported having smoked during the past four weeks compared to 13.9% of the control students. A significant difference persisted 12 months after the start of the intervention. At this time, four‐week smoking prevalence of baseline non‐smokers was reported as 17% in the intervention group versus 21.3% in the comparison group. The results reported in the paper were statistically significant (odds ratio (OR) 1.36, 95% CI 1.04 to 1.76). For consistency, we have applied the inverse of the odds ratio reported by Wiborg 2002, so that an OR less than 1 favours the intervention, indicating that more participants refrained from smoking in the intervention group compared to the control group; the inverse OR at 12 months is 0.74, 95% CI 0.96 to 0.57. However, our reanalysis to adjust for clustering found that the risk of initiating smoking at follow‐up was non‐significantly less in the intervention compared with the control group (adjusted RR 0.81, 95% CI 0.53 to 1.23).
Of the other non‐randomized controlled trials for which we had appropriate outcome data, Kairouz 2009 reported that 14% of the intervention group initiated smoking during follow‐up, compared with 16% in the control group. Stucki 2014 reported no significant difference in smoking uptake between the intervention and control groups. Our reanalysis of Kairouz 2009 produced a similar result to that of Wiborg 2002 (RR 0.81, 95% CI 0.55 to 1.20). Our reanalysis of Stucki 2014 produced a RR of 1.12 (95% CI 0.52 to 2.40).
None of the three RCTs (Crone 2003; Isensee 2012a; Schulze 2006) demonstrated a significant long‐term effect of the intervention on smoking initiation, although Crone 2003 reported a significant impact at the short‐term follow‐up. At the first post‐test in Crone 2003 (eight months after the start of the intervention and two months after the intervention ceased), 9.6% of baseline non‐smokers reported current smoking in the intervention group, compared with 14.2% in the control group. The effect of the intervention on initiation at 19 months was not reported in the paper, owing to the large number of non‐responders at the second follow‐up point. Our reanalysis with outcome data provided from the authors found that the risk of initiating smoking at follow‐up was non‐significantly less in the intervention, compared with the control group (adjusted RR 0.92, 95% CI 0.53 to 1.61).
Schulze 2006 reported that a similar proportion of the intervention (62.1%) and control groups (61.5%) remained never‐smokers at longest follow‐up. When we reanalyzed the data for current smoking prevalence among baseline non‐smokers at follow‐up we found a result similar to that reported in the paper (RR 0.98, 95% CI 0.77 to 1.24).
Isensee 2012a reported that there was no intervention effect on smoking initiation among baseline never‐smokers during the study period, but did report an effect among baseline experimental smokers. The probability among baseline experimental smokers of progressing to established use was higher for those who did not participate in the intervention; that is, students in the control group combined with students from classes who were randomized to the intervention group but opted not to participate in the trial (adjusted hazard ratio as reported in the paper = 1.45, 95% CI 1.00 to 2.10). In our reanalysis to assess the impact of the competition on smoking initiation, we compared data for the group that were randomized and participated in the intervention versus the control group. The classes that were randomized to the intervention group but opted not to participate in the trial were excluded, instead of being combined with the control group. We thought this was a more conservative comparison than including them as control participants, because classes who were randomized to the intervention but did not participate had a higher smoking prevalence at baseline. We found that the risk of initiating smoking was 5% more likely in the intervention group, compared with the control group; however the confidence interval was wide and encompassed possible positive and negative effects (RR 1.05, 95% CI 0.80 to 1.38). It is notable that Isensee 2012a was the most robust study in this review, judged to be at the lowest risk of bias.
Secondary outcomes
Amount and type of incentive
We were not able to assess whether the amount or type of incentive affected prevention of smoking. This is because data on incentives were incomplete and because the small number of studies makes these comparisons difficult.
Incentives as part of a more complex intervention
We were also unable to assess whether incentives were more or less effective in combination with other interventions to prevent starting smoking, owing to the fact that of those studies that clearly provided an additional educational component to their incentive programmes (Crone 2003; Kairouz 2009; Schulze 2006), none measured the "incentive effect" of the intervention (i.e. they did not include an arm that received additional education but no incentive). The effect sizes were small across all studies with analyzable data and did not suggest that programmes that combined incentives and education (Crone 2003; Kairouz 2009; Schulze 2006) were more effective than those using incentives alone (Isensee 2012a; Wiborg 2002).
Cost implications
Only one study rigorously assessed the costs associated with the incentive programmes. Hoeflymayr 2008 analyzed the cost effectiveness of the SFC intervention reported on by Wiborg 2002, using economic modelling, based on estimates of reduced smoking prevalence in the intervention group and models of assumed future smoking behaviour and cessation. The estimate from the study was that the SFC intervention prevented 3076 students from becoming established smokers in the 2001/2 school year. The estimated direct benefits were EUR 5.59 million (benefit/cost ratio 8.2), and total net benefits EUR 15 million (3.6 benefit/cost ratio).
Unintended consequences
One study specifically examined whether participants in the intervention group might have made false claims about their smoking status. Kairouz 2009 reported that their social contract prevention programme may have encouraged student smokers to misrepresent their smoking status at follow‐up in order to increase their class chances of winning a prize. This study found large numbers of ever‐smokers at baseline subsequently denying ever smoking at follow‐up. In total, 16% of baseline ever‐smokers in the control group denied smoking at follow‐up, compared to 24% in the intervention group. In both groups, denial was more frequent among participants who had smoked the lowest number of cigarettes at baseline, perhaps suggesting an element of recall bias. Isensee 2012a also considered under‐reporting of smoking status among intervention participants and reported that inconsistent response patterns over time did not differ by intervention status (data not presented).
Finally, one study assessed whether the SFC trialled by Isensee 2012a increased bullying or a perception of isolation among students (Hanewinkel 2002). When compared with control classrooms on three dependent variables – being victimised, active bullying or being isolated – adjusted ORs indicated no significant differences at post‐test for the intervention groups. Kairouz 2009 reported that after exposure to the SFC, intervention participants were more likely than control participants to report that people “should not hang out with smokers” (14% versus 11%) and that they themselves would “not want to be friends with a classmate who smokes” (28% versus 25%). However, it should be noted that the prevalence of these attitudes fell in both groups at the follow‐up measurement and that the authors did not report on the proportion of participants in both groups who perceived themselves as marginalized at baseline and follow‐up (arguably a more sensitive indicator of whether the competition resulted in the perception of isolation among students). Theoretically, a negative outcome of young people being told not to smoke for an incentive may be that youth smoke in reaction against directives from authority figures (i.e. the concept of "forbidden fruit," Sussman 2010) but we found no evidence of this in the studies included in this review.
No other studies reported on secondary outcomes for this review (dose‐response of the amount of incentive, costs or any adverse effects).
Discussion
Most of the studies in this review were trials of the so‐called 'Smokefree Class Competition' (SFC). At the core of this competition is the commitment of classes not to smoke for a six‐month period (the social contract) and rewarding smoke‐free classes with prizes. While this competition has been widely implemented in schools in more than 20 European countries (Isensee 2012a), there has been considerable controversy about its effectiveness in preventing smoking among young school students in the long term. A lively debate has taken place in academic journals between those who argue for the effectiveness of this competition and those who argue that the effectiveness has been overstated (Etter 2006; Hanewinkel 2007a; Hanewinkel 2006; Potschke‐Langer 2006). While one study of the SFC competition in this review reported a long‐term significant effect of incentives, we judged the study to be at high risk of selection bias and results were not adjusted to take account of its cluster design. When we reanalyzed the data, the effect was non‐significant. The pooled risk ratio (RR) for the more robust RCTs (3 studies, n = 3056 participants) suggests that, from the available data, there is no statistically significant effect of incentives to prevent smoking initiation among children and adolescents in the long term. Pooled adjusted results from the three less robust trials also failed to detect a significant effect.
All of the studies in this review were cluster trials which, compared with individually randomized trials, are more complex to design, require a larger number of participants to obtain equivalent statistical power, and require more complex analysis (Campbell 2004). They are also prone to several risks of bias (Giraudeau 2009), as can be seen in the trials included in this review. For example, of the three cluster RCTs in this review, one (Schulze 2006) may have been susceptible to selection bias as recruitment occurred after randomization and three classes assigned to control refused to forego the intervention and were subsequently included in the intervention group. In the five non‐randomized cluster trials there were baseline imbalances between groups. In two of these (Vartiainen 1996; Wiborg 2002), the intervention group comprised schools that had already registered to participate in the competition, so there may have been intrinsic differences in the level of motivation between intervention and control groups. Attrition was a significant issue for these studies. Only two studies managed to retain 80% of the sample at the longest follow‐up (Burke 1992; Stucki 2014) and only one study (Crone 2003) appropriately reported on the number of clusters (schools) and the number of participants at each time point. Some studies failed to adequately report reasons for attrition or to adequately assess the effects of attrition on the distribution of confounding variables across groups at final follow‐up (Crone 2003; Kairouz 2009; Schulze 2006; Vartiainen 1996). None of the studies reported an intention‐to‐treat analysis for smoking initiation. While this may not be appropriate for studies assessing smoking initiation, it does mean that in these studies there were significant amounts of missing data in the final analyses. In addition to risks of bias, there were other limitations to the conduct of the trials. Only two studies reported a sample size calculation. These were appropriately adjusted to account for clustering effects but because of loss to follow‐up both studies were underpowered to demonstrate a significant effect. Finally, only three studies appropriately adjusted their analyses to account for clustering. Overall, these studies were of variable quality and we would recommend that future cluster RCTs of incentives adhere to the extension to the CONSORT statement for cluster‐randomized trials to improve the quality of the evidence in this area (Campbell 2004). The quality of the evidence contributing to the primary outcome was assessed according to GRADE standards. We rated the quality of the evidence as 'low' for the RCT and 'very low' for the non‐RCT evidence. The risks of bias outlined above meant that the proportion of information from studies at high risk of bias was sufficient to affect the interpretation of results, and we therefore downgraded the quality of the evidence on this basis. When the more robust RCTs were assessed alone, information was still from studies with an unclear risk of bias. We judged two of the three RCTs to be at a high risk of attrition bias. The imprecision of results also resulted in the evidence being downgraded across study type, as all studies had wide confidence intervals.
The other limitation of the studies in this review is the variability in the reported detail of the interventions, both in terms of the dose and any additional components delivered, such as education. Where detail was provided, the incentives described were small (e.g. hip hop classes, a movie pass or a voucher for ice‐cream) to moderate in size (the most recent study distributed six prizes between EUR 220 and EUR 450 to classes). In the SFC interventions, smoke‐free classes were not guaranteed an incentive, but instead went into the draw for prizes or had to satisfy additional criteria to win a prize (e.g. in the study by Crone 2003, classes were awarded a prize if they were smoke‐free and produced a photo judged as best expressing a non‐smoking class). Only one study (Crone 2003) reported on how many prizes were awarded. Additionally, all the included studies distributed the incentive to whole classes, rather than giving it directly to individuals who reported or were confirmed to have refrained from smoking. This is in contrast to studies that have tested the efficacy of competitions and incentives on smoking cessation, which generally have rewarded individual quitters (Cahill 2011), with higher incentives demonstrating promise for longer‐term abstinence (Cahill 2015).
This begs the question about whether small to moderately‐sized incentives that successful participants are not necessarily guaranteed to receive are sufficient motivation for children and adolescents to refrain from smoking. In the Cochrane Review of the effectiveness of competitions and incentives for smoking cessation, only one included study offered evidence that incentives may improve long‐term smoking cessation. The authors of this trial suggested that they had an adequate sample size to detect an effect, in addition to a substantial reward to sustain the target behaviour (abstinence) (Volpp 2008). In this study a total of USD 750 was given to individuals incrementally for completion of a smoking cessation programme and sustained abstinence at nine or 12 months. It may not be financially, logistically or ethically feasible to distribute incentives to individuals who do not take up smoking. Certainly, the issue of confirming non‐smoking status needs consideration, as most biological indicators of smoking only measure recent tobacco use (Dolcini 2003). It may also not be financially feasible to distribute incentives to all classes who remain smoke‐free, especially when considering scaling up competitions to regional or national levels. Nevertheless, future trials should consider the size of the incentive and describe this in detail, as well as the final number of prizes distributed relative to the number of smoke‐free classes. An important question that remains unanswered is whether the efficacy of incentives for smoking prevention might be different depending on whether the reward for behaviour change was certain or only probable (i.e. determined by a prize lottery); behavioural psychology suggests that outcomes may differ under these conditions (Tversky 1981). The final limitation of the included studies is that in the three studies that provided an additional educational component to their intervention, they did not assess the "incentive effect" of the intervention, over and above the additional education.
A 2012 meta‐analysis assessing the effects of the SFC intervention on current smoking among adolescents (Isensee 2012b), reported rates of current smoking at baseline and longest follow‐up between intervention and control groups in five of the SFC studies included in this review (Crone 2003; Isensee 2012a; Schulze 2006; Vartiainen 1996; Wiborg 2002), and pooled the RRs of smoking at follow‐up. This yielded a RR of 0.86 (95% CI 0.79 to 0.94). The authors concluded that there is "some evidence that SFC contributes to smoking prevention in adolescents" (Isensee 2012b, p. 114) We would argue that this review suggests some evidence for a reduction in smoking among intervention participants, but that measuring the effect of the competition on smoking prevention required an assessment of the smoking status of baseline non‐smokers at follow‐up. Further, as the authors noted, there were several limitations to their review; they combined RCTs and non‐RCTs in their meta‐analysis, did not assess the risks of bias in the studies, and did not make any adjustment to the data for the cluster design of trials where this had not been undertaken in the original studies.
Potschke‐Langer 2006 argues that if smoking prevention (or delay of smoking onset) is the primary aim of the SFC intervention, studies should be comparing proportions of never‐smokers at follow‐up, as a comparison of smoking prevalence only tells us about the respective groups at one point in time and not about smoking dynamics over time (i.e. a young person may change their smoking status during the intervention period). This is an issue raised by Isensee 2012a in the most robust study of the SFC intervention. In this study, there were reportedly no group differences in the frequency of initiation of smoking among baseline never‐smokes. However, the probability among baseline experimental smokers of progressing to established use over the study period of 19 months was higher for non‐participants in the competition. The authors conclude that the "salient effect of the intervention is that it reduces the risk of a progression into higher stages of use among experimental smokers" and suggest that perhaps early experimental smokers are the group most amenable to intervention effects (p. 339). This is a question that is worthy of further investigation and future trials should assess intervention impact on both smoking initiation and progression.
Although the interventions covered in this review run the risk of deception by smokers regarding their smoking status in order to increase their chances of winning a prize, there is not a lot of evidence to support this. While one study reported that inconsistent response patterns were higher in the intervention than in the control group, this may have been affected by recall bias (Kairouz 2009). Several studies went to some lengths to disguise the fact that outcome assessments were linked to the competition to reduce misreporting of smoking status (reporting on smoking status for the competition was a separate process). By purposely de‐linking the evaluation of the SFC from the competition itself (reporting of smoking status of participating classes for the competition was separate from the survey that measured smoking outcomes for evaluative purposes), students may have been less likely to under‐report their smoking status, although this cannot be completely ruled out. Only one study (Hanewinkel 2010) has been conducted to investigate other possible unintended consequence of these competitions; namely, bullying or perceptions of isolation among students who cause their class to drop out of the competition because they smoke. This study found that there was no significant effect of the competition on bullying or perceptions of isolation. Kairouz 2009 found that intervention participants were more likely to report that people "should not hang out with smokers" and that they themselves "would not want to be friends with a classmate who smokes", but the prevalence of attitudes in both groups fell at follow‐up and the authors did not report on the proportion of participants in either group who perceived themselves as marginalized. A further limitation of the studies is that tobacco use other than cigarettes was not assessed. In the USA, the prevalence of hookah use increased in the period 2011 to 2015, while cigarette use decreased (Singh 2016).
One final point relates to the transferability of this evidence to other contexts. All studies included in this review were conducted in high‐income countries. There was variability across studies in the reporting of the proportion of participants who were from minority ethnic or lower socioeconomic backgrounds. Where this was reported and could be interpreted, the studies included a smaller proportion of participants representative of minority groups (Burke 1992; Crone 2003; Isensee 2012a) and low socioeconomic backgrounds (Crone 2003). Mercken 2012 reanalyzed data from the study reported by Crone 2003; a multilevel model was tested separately for adolescents in each of the categories of the two included SES indicators in this study (educational level and employment status of parents). These stratified analyses found that the overall significant short‐term effect of the intervention was only present for high SES adolescents (Mercken 2012). Further, when these additional analyses were stratified by gender, the intervention appeared only to be effective among boys with higher parental educational levels (OR 0.24, 95% CI 0.07 to 0.79), although these results should be interpreted cautiously, as sample size calculations were not based on these subgroup analyses. Future studies should report details about the sociodemographic characteristics of participants at baseline and follow‐up, and if possible analyze their results by ethnic and socioeconomic group to be able to assess whether incentives differentially affect participants from these backgrounds.
Limitations of this review include our focusing our analysis solely on the effectiveness of incentives to prevent smoking initiation (as in our protocol) and did not examine the impact of incentives on progression of smoking. Findings from the most recent study of the SFC intervention suggest that the effect of the competition might be greater for occasional smokers compared with non‐smokers at baseline. Another limitation that may have biased our results is that our outcome data were incomplete. We could not extract appropriate data for this review from two studies (Burke 1992; Vartiainen 1996) or directly from the authors, and we had to estimate the number of clusters for another study (Wiborg 2002). We concentrated on getting outcome data from authors, rather than further detailed process information (e.g. programme implementation), which is also a limitation of this review.

PRISMA study flow diagram of search results
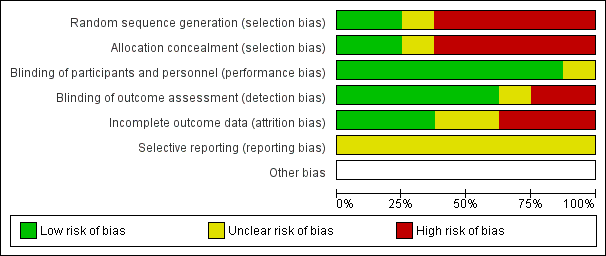
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
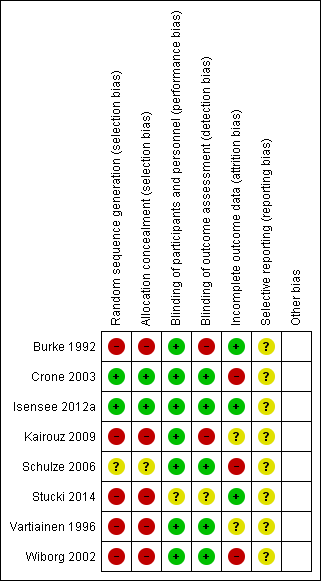
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
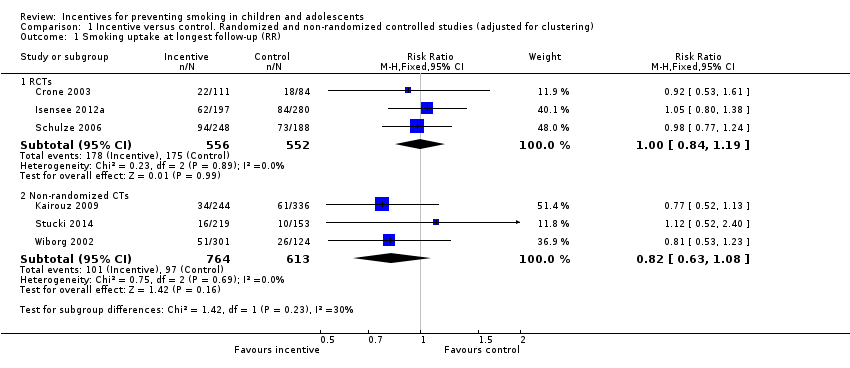
Comparison 1 Incentive versus control. Randomized and non‐randomized controlled studies (adjusted for clustering), Outcome 1 Smoking uptake at longest follow‐up (RR).
| Study | Number of non‐smokers at baseline | Number of smokers at endpoint who reported not smoking at baseline | Time point | Outcome | Biological criterion | Results | Secondary outcomes (dose response, cost, harms) |
| Crone 2003 | 556 intervention; 420 control (data from authors) | 112 intervention; 88 control
| 19 months | Smoking = current smoking, including daily/weekly/experimental | Not biochemically verified | Not reported at 19 months in published paper. Our reanalysis: RR 0.92 (95% CI 0.53 to 1.61) | Not reported |
| Isensee 2012a | 430 never‐ smokers in intervention; 610 never‐smokers in control (data from authors) | 136 intervention; 184 control | 19 months | Smoking = ever smoking, even just a puff | Not biochemically verified | From published paper: Authors reported that no group differences were found in the frequency of smoking initiation but data not presented in paper. Our reanalysis: RR 1.05 (95% CI 0.80 to 1.38) | Bullying (Hanewinkel 2010): "When compared with control classrooms on all three dependent variables – being victimised, active bullying or being isolated – the adjusted ORs indicated no significant differences at post‐test for any of the IGs [Intervention Groups]". |
| Schulze 2006 | 591 never‐smokers in intervention; 449 never‐smokers in control | 224 intervention; 173 control | 24 months | Smoking = current smoking, including irregular (less than weekly) smoking | Not biochemically verified | From published paper: 62.1% remained ‘never smoker’ in intervention group at follow‐up versus 61.4% in control group: OR 1.02 (0.83 to 1.24) adjusted for age, sex and school type.
Our reanalysis: RR 0.98 (95% CI 0.77 to 1.24) | Not reported |
Comparison 2 Results of included studies, Outcome 1 Results table: RCTs.
| Study | Number of non‐smokers at baseline | Number of smokers at endpoint who reported not smoking at baseline | Time point | Outcome | Biological criterion | Results | Secondary outcomes (dose response, cost, harms) | Comment |
| Burke 1992 | Not reported | Not reported | 18 months | Mean (SD) score of 5‐category self‐definition of smoking and 10‐category self‐reported frequency | Salivary thiocyanate (TCN) | From published paper: Mean TCN at follow‐up of pre‐intervention never‐smokers higher (560 mcg/mL, SD 403) versus control (514 mcg/mL, SD 424). Primary outcome for this review not available. | Not reported | |
| Kairouz 2009 | 664 intervention; 915 control | 93 intervention; 165 control | 10 ‐ 18 months | Smoking = ever smoking, even just a puff | Not biochemically verified | From published paper: OR 0.8 (0.5 to 1.1), adjusted for age, gender, school location, social deprivation index. Our reanalysis: RR 0.81 (95% CI 0.55 to1.20) | Intervention participants more likely than control participants to report that people “should not hang out with smokers” (14% versus 11%) and that they, themselves would “not want to be friends with a classmate who smokes” (28% versus 25%) | Concerns about misreporting of smoking status. Note large numbers of ever‐smokers at baseline then denying ever smoking at follow‐up. Stat sig more in intervention vs control (24% vs 16%) |
| Stucki 2014 | 544 intervention, 378 control | 39 intervention, 24 control | About 7 months | Smoking = any smoking in last 6 months, even just a puff and smoking during the previous month | Not biochemically verified | From published and additional data from authors. OR for decreased smoking prevalence 0.7, CI 0.5 to 1.0 | Increased smoking‐related knowledge b ‐1.0, P < 0.01 | |
| Vartiainen 1996 | Not reported and not available from authors | Not reported and not available from authors | 18 months | Smoking = daily smoking | Not biochemically verified | Reports only on the increase in prevalence of smoking from baseline to follow‐up. From baseline to longest follow‐up, increase by 10.8% points in Intervention group vs 11.2% points in control group: OR 1.25 (P = 0.15). Primary outcome for this review not available. | Not reported. Except in discussion – authors report "The social pressure created by the competition process was not greatly criticised in the pupils’ answers." | |
| Wiborg 2002 | 1215 intervention group; 502 control (data from authors) | 207 intervention; 107 control | 12 months | Smoking = 4 week prevalence of smoking | Not biochemically verified | From published paper: OR 1.36 (1.04 to 1.76), adjusted for age, sex, smoking status at baseline Our reanalysis: RR 0.81 (95% CI 0.53 to 1.23) | Cost benefit (Hoeflymayr 2008). Cost benefit ratio: economic modelling based on estimates of reduced smoking prevalence in Intervention group and models of assumed future smoking behaviour and cessation. Not based on prevention of initiation | |
Comparison 2 Results of included studies, Outcome 2 Results table: non‐randomized CTs.
| Smokefree Class Competitions (SFC) for preventing smoking uptake | |||||
| Patient or population: Children and adolescents aged 5 ‐ 18 years who were non‐smokers at baseline Settings: Schools in Germany, the Netherlands, Finland, Switzerland, Canada and the United States Intervention: Participation in SFC Comparison: No participation in SFC | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants Actual number/ effective number2 | Quality of the evidence | |
| Assumed risk1 | Corresponding risk | ||||
| Smoking uptake at longest follow‐up (RCTS) | 317 per 1000 | 320 per 1000 | RR 1.00 (0.84 to 1.19) | 3056/1108 (3) | Low3, 4 |
| Smoking uptake at longest follow‐up (Non‐RCTs) | 158 per 1000 | 132 per 1000 | RR 0.82 (0.63 to 1.08) | 4219/1377 (3) | Very low3, 5, 6 |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1'Assumed risk' calculated as risk in control groups. | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking uptake at longest follow‐up (RR) Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 RCTs | 3 | 1108 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.84, 1.19] |
| 1.2 Non‐randomized CTs | 3 | 1377 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.63, 1.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Results table: RCTs Show forest plot | Other data | No numeric data | ||
| 2 Results table: non‐randomized CTs Show forest plot | Other data | No numeric data | ||

