Organising health care services for persons with an intellectual disability
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Study Design: ITS Types of interventions: Multidisciplinary team + Change to site of service delivery + Change in scope and nature of services | |
| Participants | Clinical Problem: Focus is on persons with ID and any of the following alone or in combination: challenging behaviour, psychiatric needs, offending against the law) Setting: Wales Sample size and demographics not reported | |
| Interventions | No C group. Compares results from three intervention time periods: I1: Baseline (1975 ‐ 1982). Specialty hospital for persons with an ID I2: Community support teams (1983 ‐ 1989). Multiple agencies (health, social services, and volunteer sectors) provide care from broad range of professions (e.g. social work, occupational therapy, physiotherapy, psychology) specific to persons with ID I3: Intervention includes I2 plus additional specialist services specific to with an ID including Intensive Support Services, Emergency Intervention Service and weekly outpatient clinics (1990 ‐ 1995). I3 differs from I2 in three ways: 1) The specialist services focuses on the needs of persons with an intellectual disability and complex behavioural and/or psychiatric needs, 2) with a less broad complement of professions consisting primarily of psychologists and nurses, and 3) the services are more intensive and practical (as opposed to consultative) (Neither caseload nor frequency of intervention reported) | |
| Outcomes | Mean number of annual admissions at hospital for persons with an intellectual disability for short‐term and long term (i.e. > 6 months) stays Quality of life and burden measures NR | |
| Notes | Presence of co‐interventions may bias results Lacks control group for comparison Mann‐Whitney U test used to compare mean results from different time periods: does not account for time trend and auto‐correlation | |
| Methods | Study Design: RCT Types of interventions: Multidisciplinary team + Continuity of care + Change to setting/site of service | |
| Participants | Clinical Problem: Persons with moderate to mild ID with a DSM‐III‐R diagnosis of mental illness or behavioral complications concerning mental illness; residing in community Setting: Michigan, USA Sample Size: N = 23 I; 23 C | |
| Interventions | C: Standard case management specializing in ID. Community mental health agency administers range of multidisciplinary mental health services coordinated by case manager specializing in ID. I: Intensive case management specializing in ID. Intervention provides services described in C as well as greater direct contact services with participants in their natural environment. Team members specialised in ID | |
| Outcomes | Behaviour: Relevant section of American Association of Mental Deficiency Adaptive Behaviour Scale (AAMD‐ABS) Maladaptive behaviour: Relevant section of AAMD‐ABS Quality of life and burden measures NR | |
| Notes | Stratified by level of maladaptive behaviour before randomised ensuring similarity between groups Used repeated measures analysis of variance to identify significant interaction term | |
| Methods | Study Design: RCT Types of interventions: Revision of professional roles | |
| Participants | Clinical Problem: Adults with ID who experienced significant bereavement (death of sibling or parent); excluded persons with dementia or psychosis Setting: United Kingdom Sample Size: N = 11 I; 23 C | |
| Interventions | C: Standard mainstream control group. Trained bereavement counselors with no experience working with persons with ID deliver counseling in fixed setting of client’s choice. I: Bereavement work provided by carers (family or paid worker) who know client well but have no bereavement counseling experience. | |
| Outcomes | Behaviour: Community (ABC‐C) comprising scales for 1) irritability, 2) lethargy, 3) stereotypy, 4) hyperactivity, 5) inappropriate speech Health of the Nation Outcome Scales for People with Learning Disabilities (HoNOS‐LD) Quality of life and burden measures NR | |
| Notes | t‐test used to compare magnitude of change between pre and post intervention scores | |
| Methods | Study Design: RCT Types of interventions: Multidisciplinary team + Continuity of care | |
| Participants | Clinical Problem: Patients with severe psychotic illness with mild intellectual disability (IQ range 51‐70) or borderline IQ (IQ range 71‐85) Setting: London and Manchester, England Sample size: N = 50 I; 54 C Median age: 36.5 | |
| Interventions | C: Standard mainstream case management: Case manager is trained mental health professional responsible for direct care and coordinating health and social inputs outside of hospital; member of multidisciplinary team I: Intensive mainstream case management. Same as C but smaller case load | |
| Outcomes | Mean number of days in hospital for psychiatric reasons Quality of life: Burden measures NR | |
| Notes | Results are from larger study including persons without low IQ score. 95% confidence intervals show effect of intervention in persons with lower IQ | |
| Methods | Study Design: CBA Types of interventions: Multidisciplinary team + Change in setting/site of service | |
| Participants | Clinical Problem: Persons with intellectual disability and challenging behaviour Setting: Wales Sample size: N = 14 I; 12 C Average age: Intervention 29, Control 33 | |
| Interventions | C: Standard community treatment team specializing in ID. Persons with ID exhibit challenging behaviour, but are not referred for specialist input. Persons with ID had very little behavioural support, no written plans, and their carers had no specific training in challenging behaviour (K. Lowe, personal communication, April 16, 2008) I: In addition to C, multidisciplinary specialist support team for persons with ID. Provides intensive, individually tailored support to people with ID and their carers in natural setting over short to medium term. | |
| Outcomes | Problem behaviour: Quality of life: Carer burden: | |
| Notes | Mann‐Whitney U test used to compare distributions of I vs. C | |
| Methods | Study Design: RCT Types of interventions: Multidisciplinary team + continuity of care | |
| Participants | Clinical Problem: Persons with mild to moderate intellectual disability and psychiatric disorder Setting: South‐east London, England Sample size: N = 10 I, 10 C Average age: 45 | |
| Interventions | C: Standard community treatment team specializing in ID. (One member of team has direct contact no more than once per week) I: Assertive community treatment team specializing in ID. Same as C but, with as many contacts as needed from two professionals, one of whom acts as case‐coordinator. Author note: Frequency of contact was main criterion for identifying assertive community treatment | |
| Outcomes | Function and problem behaviour: Quality of Life: Carer burden: | |
| Notes | Differences in baseline measurement between groups adjusted using ANCOVA | |
| Methods | Study Design: RCT Types of interventions: Multidisciplinary team | |
| Participants | Clinical Problem: Persons with mild to moderate intellectual disability and a (1) serious mental health disorder or (2) challenging behaviour, or both (1) and (2) Setting: England Avergae age: N = 15 I; 15 C Average age: 40.53 | |
| Interventions | C: Standard community treatment team specializing in ID. Author note: standard= no more than one visit per week from any one professional I: Assertive community treatment team specializing in ID. Same as C, but more frequent contact. Author note: assertive = more than one visit per week from one or more professionals | |
| Outcomes | Function: Quality of Life: Carer burden: | |
| Notes | Authors used two way ANOVA. Differences in outcome were compared using time x intervention type interaction term in model | |
| Methods | Study Design: RCT Types of interventions: Multidisciplinary team + Changes to the setting/site of service delivery + Continuity of care | |
| Participants | Clinical Problem: Persons with mild or borderline intellectual disability and serious mental illness (i.e. require in‐patient hospitalization) Setting: Netherlands Sample size: N = 25 I; 25 C Average age: Intervention: mean 31.4, SD 12.6 | |
| Interventions | C: Standard hospital treatment: 48‐bed facility specializing in treatment of people with dual diagnosis. Interventions include: psychopharmacological medication, behavioral therapy, social skills training, education, structured daily activities. I: Outreach treatment team: One member of team visits patient in home environment; works with care givers involved in daily life. Other interventions similar to C. | |
| Outcomes | Psychiatric symptoms: Quality of life measure NR Carer burden: | |
| Notes | Differences in baseline measurement between groups adjusted using ANCOVA Authors also conducted equivalence testing | |
Characteristics of findings tables:
C: Control group conditions.
I: Intervention group conditions.
ID: intellectual disability.
ITS: interrupted time series.
RCT: randomised controlled trial.
CBA: controlled before and after study.
NR: not reported.
NS: not significant.
SD: standard deviation.
CI 95% confidence interval.
* primary outcome was either identified by original study author or identified by review authors as best reflecting intervention
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| After only design with a control group | |
| Before and after study with no control group for comparison | |
| Pilot for upcoming RCT study | |
| Study participants are children | |
| After only design with no control group for comparison | |
| After only design with no control group for comparison | |
| Descriptive study | |
| Before and after study with no control group | |
| Persons with intellectual disability not identified in study | |
| Before and after study with no baseline for comparison | |
| Before and after study with no control group | |
| Before and after study with non‐comparable controls (persons without intellectual disability) | |
| Descriptive study of health problems and diagnoses | |
| Before and after study with not control group | |
| Descriptive study | |
| Before and after study with no control group | |
| After only study comparing care coordination to a control group. Adjusted length of stay results using diagnosis‐related standard. Did not compare outcomes at baseline | |
| Describes costs and review of Criscione 1993 | |
| Same methods as Criscione 1993 using updated data | |
| Descriptive study of individuals with dual diagnosis | |
| Interrupted time series with insufficient data points for adults | |
| Descriptive study of physical health needs | |
| Interrupted time series | |
| Before and after study with no control group | |
| Interrupted time series Insufficient number of pre‐admission data points | |
| Impact of intervention not studied | |
| Study of Children with Prader‐Willi syndrome | |
| Does not evaluate effect of intervention on persons with intellectual disability alone | |
| Before and after study with no control group | |
| 'Naturalistic' study (i.e. no attempt to influence interventions) with no baseline comparison | |
| Review article on assertive community treatment | |
| Descriptive study of residential models | |
| Persons with intellectual disability not identified in study | |
| Randomised controlled trial of opportunistic health screening tool | |
| Cross sectional study of oral health needs at Texas state facilities | |
| Before and after study with no control group or | |
| Descriptive study | |
| Descriptive study of specialised hospital psychiatric unit | |
| Descriptive study of educational intervention to improve communication between stakeholders | |
| Before and after study with no control group | |
| Before and after study with no control group | |
| Study of impact of multidimensional service provision | |
| Before and after study with no control group | |
| Study sample does not include persons with intellectual disability | |
| Cross sectional study of impact of Community Mental Health Centre on contact with inpatient psychiatric services | |
| Descriptive study using comprehensive health check in primary care | |
| Descriptive study with no control group | |
| Qualitative description of general practice using annual health review | |
| Before and after study with no control group | |
| Randomised controlled trial of cognitive behavioural programme | |
| Pharmacy intervention in institution based residential setting. Controlled before and after with no control group and interrupted time series | |
| Before and after study with control group | |
| Study participants are children | |
| Descriptive and retrospective evaluation of referrals and referral letters evaluated for appropriateness | |
| Descriptive study of persons with intellectual disability with and without support from community intellectual disability team | |
| Descriptive study of residential setting options | |
| After only study with no control group | |
| Descriptive study of health and health education needs | |
| Before and after study with no control group | |
| Descriptive study of unmet needs in persons with dual diagnosis | |
| Follow up study with no control group | |
| Descriptive retrospective study of out‐patient clinic for persons with intellectual disability | |
| Interrupted time series | |
| Descriptive study of acute specialist inpatient unit for persons with dual diagnosis | |
| Descriptive study of admissions to specialist inpatient unit for persons with dual diagnosis | |
| Descriptive study of general practitioners views on specialist physician support | |
| Case studies of outreach treatment for persons with dual diagnosis | |
| Descriptive study of patients with dual diagnosis in outreach and inpatient setting | |
| Follow up study with no control group | |
| Follow up study using general population as control | |
| Follow up study with no control group | |
| Before and after study with no control group | |
| Evaluation of sheltered workshop |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global assessment of function (symptomatology) Show forest plot | 2 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐0.76 [‐6.07, 4.55] |
| Analysis 1.1  Comparison 1 Assertive community treatment versus standard community treatment, Outcome 1 Global assessment of function (symptomatology). | ||||
| 2 Global assessment of function (Disability) Show forest plot | 2 | 50 | Mean Difference (IV, Fixed, 95% CI) | 1.05 [‐4.05, 6.16] |
| Analysis 1.2  Comparison 1 Assertive community treatment versus standard community treatment, Outcome 2 Global assessment of function (Disability). | ||||
| 3 Carer uplift/burden Show forest plot | 2 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐3.48, 3.54] |
| Analysis 1.3  Comparison 1 Assertive community treatment versus standard community treatment, Outcome 3 Carer uplift/burden. | ||||
| 4 Quality of life Show forest plot | 2 | 50 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.75, 0.36] |
| Analysis 1.4  Comparison 1 Assertive community treatment versus standard community treatment, Outcome 4 Quality of life. | ||||

EMBASE = Excerpta Medica Database
MEDLINE = United States National Library of Medicine's bibliographic database
EBMZ = Evidence Based Medicine Reviews Multifile
Social Sci.= Social sciences database
CINAHL = Cumulative Index to Nursing & Allied Health Literature
EPOC = Effective Practice and Organisation of Care registry
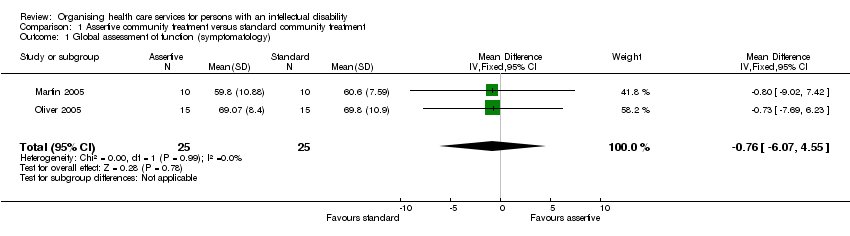
Comparison 1 Assertive community treatment versus standard community treatment, Outcome 1 Global assessment of function (symptomatology).

Comparison 1 Assertive community treatment versus standard community treatment, Outcome 2 Global assessment of function (Disability).
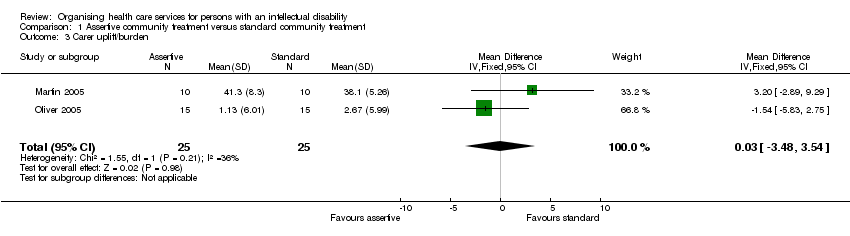
Comparison 1 Assertive community treatment versus standard community treatment, Outcome 3 Carer uplift/burden.

Comparison 1 Assertive community treatment versus standard community treatment, Outcome 4 Quality of life.
| Author, year | Concealment of allocation | Follow up of study participants | Blinded assessment of outcome | Baseline measurement | Reliable primary outcome | Protection against contamination |
| Coelho, 1993 | Not clear | Done | Not done | Done | Not clear | Not clear |
| Dowling, 2006 | Done | Not done | Not done | Done | Done | Not done |
| Hassiotis, 2001 | Not clear | Not clear | Not done | Done | Not Done | Done |
| Martin, 2005 | Done | Done | Not clear | Done | Done | Not done |
| Oliver, 2005 | Done | Done | Done | Done | Done | Not done |
| VanMinnen, 1997 | Not clear | Done | Not clear | Done | Done | Done |
| Not clear: not reported in study Not done: study authors specifically describe item and does not meet EPOC criteria Done: study authors specifically describe item and it meets EPOC criteria Scoring criteria provided by EPOC (Cochrane 2006b; Cochrane 2006a) | ||||||
| Author, Year | Main results | Summary |
| Allen, | I1 vs I2 Short term stays: mean (SD): pre = 142.5 (42.0); post = 124.7 (20.7) change: 17.8 less admission/year for I2 Long term stays: mean (SD): pre = 16 (4.5); post = 9.0 (2.1) change: 7 less admissions/year for I2 I2 vs I3 mean (SD): pre = 124.7 (20.7); post = 30.7 (30.7) change: 94.0 less admissions/year for I3 Long term stays: mean (SD): pre = 9 (2.1); post = 3.5 (2.4) change: 5.5 less admissions/year for I3 | Reanalysis of results showed no evidence that community support teams alone or in combination with specialist services decreases short stay admissions
Reanalysis of results showed no evidence that community support teams alone or in combination with specialist services decreases long term stay admissions.
|
| Coelho, 1993 | Intervention with time shows significantly better results in all behaviour measures: mean (SD) for I: pre = 199.4 (28.5); post = 211.9 (30.9) mean (SD) for C: pre = 206.0 (30.0); post = 201.3 (29.0) AAMD‐ABS: mean (SD) for I: pre = 53.7 (22.5); post = 40.1 (20.3) mean (SD) for C: pre = 53.4 (27.5); post = 53.0 (29.0) Maladaptive behaviour decreases more for I (P = 0.001) MMBS: mean (SD) for I: pre = 12.7 (7.0); post = 6.5 (4.6) mean (SD) for C: pre = 12.0 (7.6); post = 11.5 (6.4) Maladaptive behaviour decreases more for I (P = 0.001) | Supports the use of decreased caseloads by professionals in a team and greater frequency of episodes of direct care with persons with dual diagnosis in their natural environment |
| Dowling, 2006 | Improvements in behaviour for standard practice control group ONLY. Significant difference in change in all measures except speech: 1) ABC irritability: mean change (SD) for I = ‐0.9 (5.8); for C = 6.1 (4.4); Greater improvement for C (P > 0.001) 2) ABC lethargy: mean change (SD) for I = ‐1.8 (4.5); for C = 5.7 (6.4); Greater improvement for C (P = 0.001)
| Supports mainstream bereavement counselling over grief work provided by carers at home and during day activities |
| Hassiotis, 2001 | Persons with IQ of 85 or lower in intervention group were hospitalised for shorter lengths than those in control: mean days in hospital (SD): I = 47.2 (98.0); C = 104.8 (159.5) difference = 57.5 days; CI 110.9 to 4.2 Study reports no significant difference for quality of life scores for persons with IQ of 85 or less (results NR)
| Supports intensive case management to decrease hospital length of stays for persons with a borderline or mild intellectual disability and psychotic illness
|
| Lowe, 1996 | DAS shows I group has significantly more behaviour problems (P < 0.05), but shows no difference in percentage rated severe + frequent (SD and P‐value NR) ABC shows no difference in average score and no difference for number of problem behaviours (SD and P‐values NR) No difference in ICI score (SD and P‐value NR) MBI not used for this comparison
| No evidence that specialist support services team is better than standard community treatment alone for persons with intellectual disability and challenging behaviour |
| Martin, 2005 | No difference in GAF scores: No difference in ABC score (P = 0.447) Difference in QOLQ score favours C (P < 0.023) No difference in Uplift/Burden score (P = 0.151) (See figures 2‐5 for details) | No evidence that assertive community treatment is better than standard community treatment for persons with ID and mental health disorders |
| Oliver, 2005 | No difference in GAF scores: Symptomalogy (P = 0.080), Social function and performance (P = 0.79) No difference in any dimension of WHOQOL‐Bref or of Uplift/Burden Scale (See figures 2‐5 for details) | No evidence that assertive community treatment is better than standard community treatment for persons with ID and mental health disorders |
| VanMinnen, 1997 | No difference in psychiatric symptoms at endpoint: PIMRA‐I mean: I = 15.6 (SD NR); C = 14.4 (SD NR) PIMRA‐SR mean: I = 16.7 (SD NR); C = 16.8 (SD NR); difference = 0.1 (CI ‐3.7 to 3.9) (P = 0.96) Reiss mean: I = 12.7 (SD NR); C = 13.7 (SD NR) Carer burden not measured at endpoint for C group | Home based treatment of patients with dual diagnosis is as effective as hospital based treatment |
| * primary outcome was either identified by original study author or identified by review authors as best reflecting intervention NS: not significant. I: intervention. C: control. ID: intellectual disability. SD: standard deviation. CI 95% confidence interval. | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global assessment of function (symptomatology) Show forest plot | 2 | 50 | Mean Difference (IV, Fixed, 95% CI) | ‐0.76 [‐6.07, 4.55] |
| 2 Global assessment of function (Disability) Show forest plot | 2 | 50 | Mean Difference (IV, Fixed, 95% CI) | 1.05 [‐4.05, 6.16] |
| 3 Carer uplift/burden Show forest plot | 2 | 50 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐3.48, 3.54] |
| 4 Quality of life Show forest plot | 2 | 50 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.75, 0.36] |

