Contenido relacionado
Revisiones y protocolos relacionados
Shihong Zhang, Lichun Wang, Ming Liu, Bo Wu | 17 febrero 2010
Zhou Liu, Lingying Liu, Zhijian Zhang, Zuhui Chen, Bin Zhao | 30 abril 2013
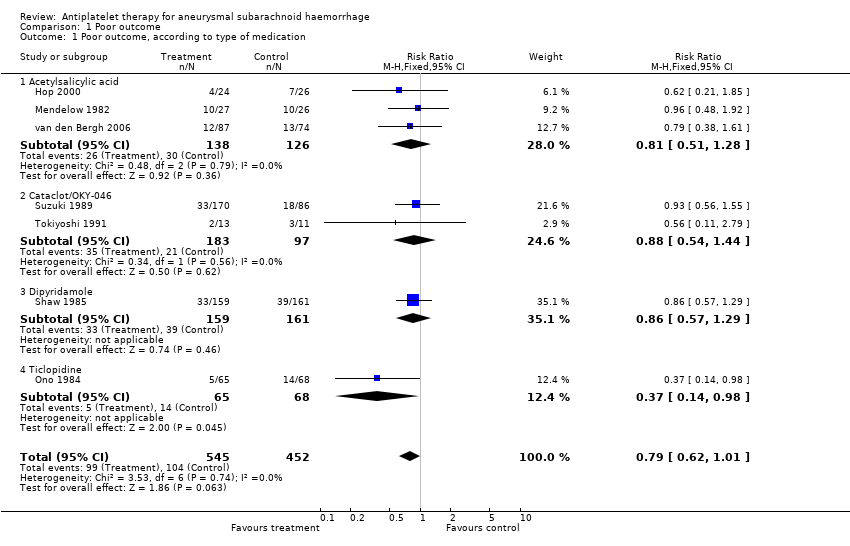
Sanne Dorhout Mees, Gabriel JE Rinkel, Valery L Feigin, Ale Algra, Walter M van den Bergh, Marinus Vermeulen, Jan van Gijn | 18 julio 2007
Antti Lindgren, Mervyn DI Vergouwen, Irene van der Schaaf, Ale Algra, Marieke Wermer, Mike J Clarke, Gabriel JE Rinkel | 15 agosto 2018
Gabriel JE Rinkel, Valery L Feigin, Ale Algra, Jan van Gijn | 18 octubre 2004
Valery L Feigin, Neil Anderson, Gabriel JE Rinkel, Ale Algra, Jan van Gijn, Derrick A Bennett | 20 julio 2005
Jia Guo, Zhenghong Shi, KeHu Yang, Jin Hui Tian, Lei Jiang | 12 septiembre 2012
Peter C Whitfield, Peter Kirkpatrick | 23 abril 2001
Imama A Naqvi, Ayeesha K Kamal, Hasan Rehman | 19 agosto 2020
Ritu Saxena, Peter J Koudstaal | 18 octubre 2004
Respuestas clínicas Cochrane
Jane Burch | 14 septiembre 2018