Ejercicios para pacientes de edad avanzada hospitalizados por enfermedades agudas
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | ‐ RCT comparing an acute geriatric ward (AGW) with 2 usual care general medical wards (MW). | |
| Participants | ‐ 444 older medical patients (190 AGW and 223 MW). 25 were excluded due to protocol violations. | |
| Interventions | ‐ Acute geriatric based ward differed from the standard ward in that it provided a geriatrician, physiotherapist, occupational therapist. Interdisciplinary team work focussed on early and intensive rehabilitation and intense discharge planning. | |
| Outcomes | ‐ Functional status (Barthel Index), cognitive status (MMSE), psychological well being, mortality, place of residence, length and cost of hospital stay, hospital readmission, healthcare costs, events after discharge, outpatient visits and personal assistance requirements. | |
| Notes | ‐ Language: English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | ‐ RCT of a geriatric special care unit compared to a traditional medical or surgical ward. | |
| Participants | ‐ 271 medical/surgical patients (95 treatment, 176 control). | |
| Interventions | ‐ Geriatric special care unit. Registered nurses/assistants trained for project. Emphasis on maximising patient independence. Multidisciplinary team meeting twice weekly. Early discharge planning and home visit 3 weeks after discharge. | |
| Outcomes | ‐ Discharge destination, mortality, complications during hospitalisation, length and cost of hospital stay, use of physical or chemical restraints. | |
| Notes | ‐ Language: English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
| Methods | ‐ RCT of a geriatric special care unit compared to a traditional medical or surgical ward. | |
| Participants | ‐ 424 medical/surgical patients (123 treatment, 301 control). | |
| Interventions | ‐ Geriatric special care unit. Registered nurses/assistants trained for project. Emphasis on maximising patient independence. Multidisciplinary team meeting twice weekly. Early discharge planning and home visit 3 weeks after discharge. | |
| Outcomes | ‐ Discharge destination, mortality, complications during hospitalisation, length and cost of hospital stay, use of physical or chemical restraints. | |
| Notes | ‐ Language: English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
| Methods | ‐ RCT of an acute care elders unit (ACE) compared to usual care units. | |
| Participants | ‐ 1531 of 6609 eligible patients. | |
| Interventions | ‐ Multidisciplinary ACE unit. Specially designed environment, patient centred care, nursing care plans for prevention of functional decline, rehabilitation, patient discharge to home and review of medical care to prevent iatrogenic illness. Daily team rounds. | |
| Outcomes | ‐ Function (ADL and IADL), mobility, mortality, discharge destination, hospital costs and LOS, satisfaction and use of at‐risk medications. | |
| Notes | ‐ Language: English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | ‐ see Landefeld 1995 | |
| Participants | ‐ see Landefeld 1995 | |
| Interventions | ‐ see Landefeld 1995 | |
| Outcomes | ‐hospital length of stay and costs | |
| Notes | ‐ see Landefeld 1995 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
| Methods | ‐ CCT of additional exercise intervention compared to usual care. | |
| Participants | ‐ 236 of 251 eligible patients (110 intervention, 126 usual care). | |
| Interventions | ‐ Exercise only intervention | |
| Outcomes | ‐ Functional status (Barthel Index, Timed Up and Go and Functional Ambulation Classification), adverse events in hospital (mortality, falls, admission to the intensive care unit), discharge destination from hospital, hospital length of stay and readmission within 28 days of discharge. | |
| Notes | ‐ Language: English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
| Methods | ‐ RCT of additional exercise intervention compared to usual care. | |
| Participants | ‐ 160 of 186 eligible patients (80 in each group). | |
| Interventions | ‐ Exercise only intervention | |
| Outcomes | ‐ Functional status (Barthel Index and TUG), adverse events (mortality, admission to ICU and falls), discharge destination from hospital, hospital length of stay and readmission within 28 days of discharge. | |
| Notes | ‐ Language: English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | ‐ RCT of an acute care elders (ACE) unit compared to usual care | |
| Participants | ‐ 651 of 1794 eligible patients (327 intervention, 324 usual care). | |
| Interventions | ‐ Multidisciplinary ACE unit. Specially designed environment, patient centred care, nursing care plans for prevention of functional decline, rehabilitation, patient discharge to home and review of medical care to prevent iatrogenic illness. Daily team rounds. | |
| Outcomes | ‐ Function (ADL, IADL and ability to walk), mental status (subscore of MMSE), depression (Geriatric Depression Scale), overall health status, discharge destination from hospital, place or residence 3 months after discharge, acute hospital length and cost of hospital stay. | |
| Notes | ‐ Language: English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
| Methods | ‐ RCT of an exercise program that included a hospital component and a self‐administered 1 month home component. | |
| Participants | ‐ 300 subjects of 2198 eligible patients (151 control, 149 intervention) | |
| Interventions | ‐ Exercise only intervention | |
| Outcomes | ‐ Function (Functional Independence Measure, Locomotion Scale, frequency of leaving the neighbourhood, IADLs, National Health Interview Survey Physical Activity Scale), hospital length of stay, RAND General Health Scale, mortality. | |
| Notes | ‐ Language: English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | ‐ A CCT examining the effect of a psychogeriatric intervention group in addition to usual care compared to usual care. | |
| Participants | ‐ 237 patients enrolled (140 treatment group, 97 usual care). | |
| Interventions | ‐ Multidisciplinary joint treatment by a psychogeriatric team leader in addition to usual care. Full time physiotherapist and additional 3 nurses on intervention ward. Aim to optimise patient function. Weekly team meetings. | |
| Outcomes | ‐ Length of stay, SIVIS dependency scales (Help index, Mobility, ADL+ continence), discharge destination, residence in a long‐term care facility | |
| Notes | ‐ Language: English. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Participants too young | |
| No control group | |
| Patients not randomly allocated to group. Prospectively matched intervention and control pairs. | |
| Physical exercise intervention not prescribed for all patients in the intervention group | |
| Patients not randomised during acute medical exacerbation | |
| Not a physical exercise intervention program. Encouragement with self care and other personal activities provided | |
| Participants too young | |
| Exercise intervention prescribed only if felt appropriate. Exercise not prescribed for all patients in the intervention group. | |
| Participants too young. Patients were required to be 60 years of age or older. Mean age of approximately 80 years but standard deviation not reported. | |
| Exercise not prescribed for all patients in the intervention group. | |
| Physical exercise intervention not prescribed for all patients in the intervention group | |
| Physical exercise intervention not prescribed for all patients in the intervention group | |
| No control group | |
| Patients not randomly allocated to group | |
| Patients not randomly allocated to group. Prospective individual matching of patients. | |
| Published abstract only. Unclear if patients randomised within 48 hours of hospital admission. Correspondence with authors has occurred and further information to be obtained. | |
| Historical control group | |
| Physical exercise intervention not prescribed for all patients in the intervention group | |
| Participants too young | |
| Patients not randomly allocated to group | |
| Patients not randomised within 3 days of hospital admission | |
| Physical exercise intervention not prescribed for all patients in the intervention group | |
| Patients not randomly allocated to group. Prospective patient matching. | |
| Patients not randomised within 3 days of hospital admission | |
| Patients not randomised within 3 days of hospital admission | |
| Patients not randomised within 3 days of hospital admission | |
| Patients not randomised within 3 days of hospital admission | |
| Patients not randomly allocated to group | |
| Participants too young |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Maintained or improved ADL scores between hospital admission and discharge ‐ MDI versus usual care Show forest plot | 3 | 2271 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.97, 1.15] |
| Analysis 1.1  Comparison 1 Function ‐ multidisciplinary intervention versus usual care, Outcome 1 Maintained or improved ADL scores between hospital admission and discharge ‐ MDI versus usual care. | ||||
| 2 Maintained or improved mobility scores between hospital admission and discharge ‐ MDI versus usual care Show forest plot | 3 | 2119 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.99, 1.06] |
| Analysis 1.2  Comparison 1 Function ‐ multidisciplinary intervention versus usual care, Outcome 2 Maintained or improved mobility scores between hospital admission and discharge ‐ MDI versus usual care. | ||||
| 3 Maintained or improved ADL scores between 2 weeks prior to hospital admission and discharge‐ MDI v usual care Show forest plot | 2 | 2001 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.00, 1.13] |
| Analysis 1.3  Comparison 1 Function ‐ multidisciplinary intervention versus usual care, Outcome 3 Maintained or improved ADL scores between 2 weeks prior to hospital admission and discharge‐ MDI v usual care. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in Barthel Index between hospital admission and discharge ‐ additional exercise versus usual care Show forest plot | 2 | 293 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.06, 0.40] |
| Analysis 2.1  Comparison 2 Function ‐ additional exercise only versus usual care, Outcome 1 Change in Barthel Index between hospital admission and discharge ‐ additional exercise versus usual care. | ||||
| 2 Change in TUG scores between hospital admission and discharge ‐ additional exercise versus usual care Show forest plot | 2 | 188 | Mean Difference (IV, Random, 95% CI) | ‐2.52 [‐5.75, 0.71] |
| Analysis 2.2  Comparison 2 Function ‐ additional exercise only versus usual care, Outcome 2 Change in TUG scores between hospital admission and discharge ‐ additional exercise versus usual care. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Patient mortality during hospitalisation ‐ MDI versus usual care Show forest plot | 6 | 3552 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.59, 1.64] |
| Analysis 3.1  Comparison 3 Adverse events ‐ multidisciplinary intervention versus usual care, Outcome 1 Patient mortality during hospitalisation ‐ MDI versus usual care. | ||||
| 2 Patient mortality 3 months after hospital discharge ‐ MDI versus usual care Show forest plot | 3 | 2595 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.83, 1.17] |
| Analysis 3.2  Comparison 3 Adverse events ‐ multidisciplinary intervention versus usual care, Outcome 2 Patient mortality 3 months after hospital discharge ‐ MDI versus usual care. | ||||
| 3 Patient complications during hospitalisation ‐ MDI versus usual care Show forest plot | 2 | 550 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.68, 1.29] |
| Analysis 3.3  Comparison 3 Adverse events ‐ multidisciplinary intervention versus usual care, Outcome 3 Patient complications during hospitalisation ‐ MDI versus usual care. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Patient mortality during hospitalisation ‐ additional exercise versus usual care Show forest plot | 3 | 696 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.98 [0.64, 6.18] |
| Analysis 4.1  Comparison 4 Adverse events ‐ additional exercise versus usual care, Outcome 1 Patient mortality during hospitalisation ‐ additional exercise versus usual care. | ||||
| 2 Admission to the Intensive Care Unit (ICU) ‐ additional exercise versus usual care Show forest plot | 2 | 396 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.04, 30.44] |
| Analysis 4.2  Comparison 4 Adverse events ‐ additional exercise versus usual care, Outcome 2 Admission to the Intensive Care Unit (ICU) ‐ additional exercise versus usual care. | ||||
| 3 Falls during hospitalisation ‐ additional exercise versus usual care Show forest plot | 2 | 384 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.40, 3.15] |
| Analysis 4.3  Comparison 4 Adverse events ‐ additional exercise versus usual care, Outcome 3 Falls during hospitalisation ‐ additional exercise versus usual care. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Discharge to preadmission residence/home from hospital ‐ MDI versus usual care Show forest plot | 4 | 1675 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [1.03, 1.14] |
| Analysis 5.1  Comparison 5 Hospital outcomes ‐ multidisciplinary intervention versus usual care, Outcome 1 Discharge to preadmission residence/home from hospital ‐ MDI versus usual care. | ||||
| 2 Acute hospital length of stay ‐ MDI versus usual care Show forest plot | 6 | 3478 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.93, ‐0.22] |
| Analysis 5.2  Comparison 5 Hospital outcomes ‐ multidisciplinary intervention versus usual care, Outcome 2 Acute hospital length of stay ‐ MDI versus usual care. | ||||
| 3 Cost of acute hospital stay ‐ MDI versus usual care Show forest plot | 5 | 3241 | Mean Difference (IV, Fixed, 95% CI) | ‐278.65 [‐491.85, ‐65.44] |
| Analysis 5.3  Comparison 5 Hospital outcomes ‐ multidisciplinary intervention versus usual care, Outcome 3 Cost of acute hospital stay ‐ MDI versus usual care. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Discharge to preadmission residence/home from hospital ‐ additional exercise versus usual care Show forest plot | 2 | 380 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.80, 1.66] |
| Analysis 6.1  Comparison 6 Hospital outcomes ‐ additional exercise versus usual care, Outcome 1 Discharge to preadmission residence/home from hospital ‐ additional exercise versus usual care. | ||||
| 2 Acute hospital length of stay ‐ additional exercise versus usual care Show forest plot | 3 | 680 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐1.23, 1.26] |
| Analysis 6.2  Comparison 6 Hospital outcomes ‐ additional exercise versus usual care, Outcome 2 Acute hospital length of stay ‐ additional exercise versus usual care. | ||||
| 3 Total (acute plus subacute) hospital length of stay‐ additional exercise versus usual care Show forest plot | 2 | 380 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐2.58, 1.17] |
| Analysis 6.3  Comparison 6 Hospital outcomes ‐ additional exercise versus usual care, Outcome 3 Total (acute plus subacute) hospital length of stay‐ additional exercise versus usual care. | ||||
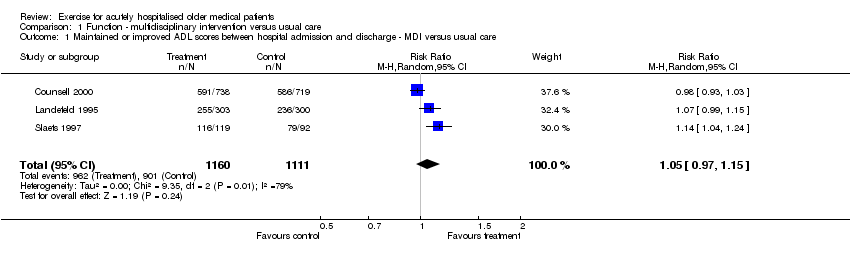
Comparison 1 Function ‐ multidisciplinary intervention versus usual care, Outcome 1 Maintained or improved ADL scores between hospital admission and discharge ‐ MDI versus usual care.
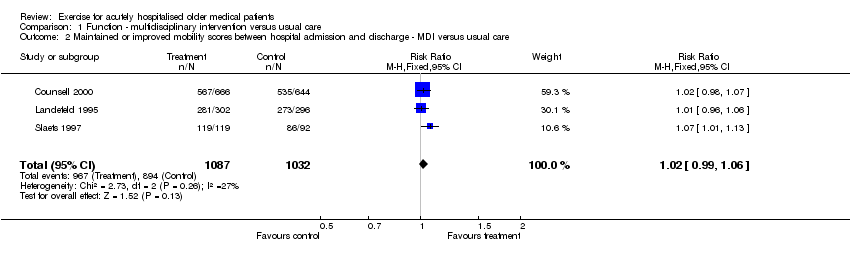
Comparison 1 Function ‐ multidisciplinary intervention versus usual care, Outcome 2 Maintained or improved mobility scores between hospital admission and discharge ‐ MDI versus usual care.

Comparison 1 Function ‐ multidisciplinary intervention versus usual care, Outcome 3 Maintained or improved ADL scores between 2 weeks prior to hospital admission and discharge‐ MDI v usual care.

Comparison 2 Function ‐ additional exercise only versus usual care, Outcome 1 Change in Barthel Index between hospital admission and discharge ‐ additional exercise versus usual care.

Comparison 2 Function ‐ additional exercise only versus usual care, Outcome 2 Change in TUG scores between hospital admission and discharge ‐ additional exercise versus usual care.

Comparison 3 Adverse events ‐ multidisciplinary intervention versus usual care, Outcome 1 Patient mortality during hospitalisation ‐ MDI versus usual care.

Comparison 3 Adverse events ‐ multidisciplinary intervention versus usual care, Outcome 2 Patient mortality 3 months after hospital discharge ‐ MDI versus usual care.

Comparison 3 Adverse events ‐ multidisciplinary intervention versus usual care, Outcome 3 Patient complications during hospitalisation ‐ MDI versus usual care.

Comparison 4 Adverse events ‐ additional exercise versus usual care, Outcome 1 Patient mortality during hospitalisation ‐ additional exercise versus usual care.

Comparison 4 Adverse events ‐ additional exercise versus usual care, Outcome 2 Admission to the Intensive Care Unit (ICU) ‐ additional exercise versus usual care.

Comparison 4 Adverse events ‐ additional exercise versus usual care, Outcome 3 Falls during hospitalisation ‐ additional exercise versus usual care.

Comparison 5 Hospital outcomes ‐ multidisciplinary intervention versus usual care, Outcome 1 Discharge to preadmission residence/home from hospital ‐ MDI versus usual care.
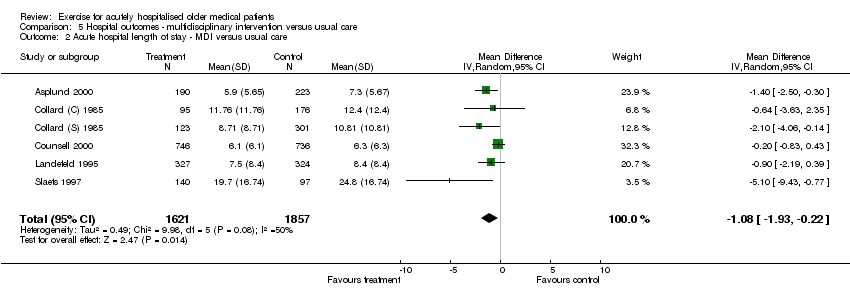
Comparison 5 Hospital outcomes ‐ multidisciplinary intervention versus usual care, Outcome 2 Acute hospital length of stay ‐ MDI versus usual care.

Comparison 5 Hospital outcomes ‐ multidisciplinary intervention versus usual care, Outcome 3 Cost of acute hospital stay ‐ MDI versus usual care.
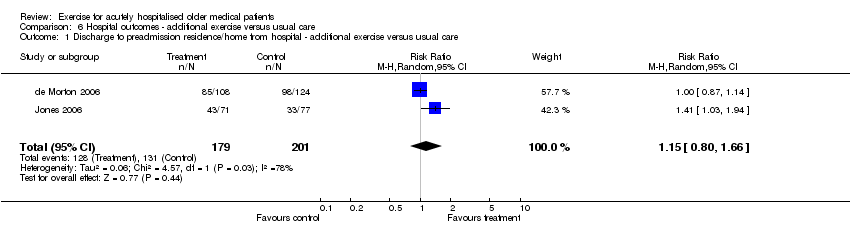
Comparison 6 Hospital outcomes ‐ additional exercise versus usual care, Outcome 1 Discharge to preadmission residence/home from hospital ‐ additional exercise versus usual care.

Comparison 6 Hospital outcomes ‐ additional exercise versus usual care, Outcome 2 Acute hospital length of stay ‐ additional exercise versus usual care.
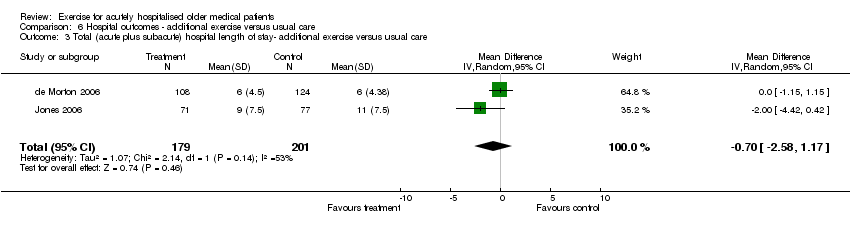
Comparison 6 Hospital outcomes ‐ additional exercise versus usual care, Outcome 3 Total (acute plus subacute) hospital length of stay‐ additional exercise versus usual care.
| Outcome | Comparison | #patients (#trials) | Control event rate | ARD (95%CI), % | Wt Rel % change | NNT (95% CI) | Statistically sig | Quality of evidence |
| Maintain or improve ADL scores between admission and discharge | MDI v UC ‐ function | 2271 (3) | 901/1111 (82.0%) | 0.05 (‐0.03, 0.12) , 5% | 5% (I) | NA | Not statistically significant | Silver |
| Maintain or improve mobility scores between admission and discharge | MDI v UC ‐ function | 2119 (3) | 894/1032 (86.6%) | 0.03 (0.00, 0.06), 3% | 3% (I) | NA | Not statistically significant | Silver |
| Maintain or improve ADL scores between 2 weeks prior to hospital admission and discharge | MDI v UC ‐ function | 2001 (2) | 648/990 (65.5%) | 0.04 (0.00, 0.04), 4% | 7% (I) | NA | Not statistically significant | Silver |
| Mortality during hospitalisation | MDI v UC ‐ adverse events | 3552 (6) | 102/1910 (5.3%) | 0.00 (‐0.03, 0.03), 0% | 1% (I) | NA | Not statistically significant | Silver |
| Mortality 3 months after hospital discharge | MDI v UC ‐ adverse events | 2595 (3) | 214/1311 (16.3%) | 0.00 (‐0.03, 0.03), 0% | 1% (I) | NA | Not statistically significant | Silver |
| Complications during hospitalisation | MDI v UC ‐ adverse events | 550 (2) | 88/372 (23.7%) | ‐0.01 (‐0.09, 0.06), ‐1% | 6% (I) | NA | Not statistically significant | Silver |
| Mortality during hospitalisation | Exercise only versus UC ‐ adverse events | 696 (3) | 4/357 (1.1%) | 0.01 (‐0.01, 0.03), 1% | 98% (W) | NA | Not statistically significant | Silver |
| Admission to ICU during hospitalisation | Exercise only versus UC ‐ adverse events | 396 (2) | 4/206 (1.9%) | 0.01 (‐0.07, 0.09), 1% | 6% (W) | NA | Not statistically significant | Silver |
| Falls during hospitalisation | Exercise only versus UC ‐ adverse events | 384 (2) | 7/203 (3.5%) | 0.00 (‐0.04, 0.04), 0% | 12% (W) | NA | Not statistically significant | Silver |
| Discharge to preadmission residence/home | MDI v UC ‐ hospital outcomes | 1675 (4) | 739/980 (75.4%) | 0.06 (0.02, 0.10), 6%, 6 more patients out of 100 | 8% (I) | 16 (11, 43) | Statistically significant | Silver |
| Discharge to preadmisison residence/home | Exercise only versus UC ‐ hospital outcomes | 380 (2) | 131/201 (65.2%) | 0.08 (‐0.10, 0.26), 8% | 15% (I) | NA | Not statistically significant | Silver |
| Legend: ADL=activities of daily living; ICU=intensive care unit | MDI=multidisciplinary intervention; UC=usual care | ARD=absolute risk difference | Wt Rel=weighted relative change | NNT=number needed to treat | sig=significant |
| Outcome (scale) | #patients (#trials) | Control baseline m | Wt absolute change | Relative % change | NNT | Statistical sig | Quality of evidence |
| Change in TUG score (seconds)‐ additional exercise versus usual care | 188 (2) | 20.59 (de Morton et al.) | ‐2.52 seconds | 2.52/20.59 = 0.12 = 12% | NA | Not statistically significant | Silver |
| Acute hospital LOS ‐ MDI versus usual care | 3478 (6) | 6.3 days (Counsell et al.) | ‐1.08 days | 1.08/6.3 = 0.17 = 17% | 16 | Significant | Silver |
| Cost of acute hospital stay ‐ MDI versus usual care | 3241 (5) | 0 | ‐$278.65 | NA | 26 | Significant | Silver |
| Acute hospital LOS ‐ additional exercise versus usual care | 680 (3) | 6.0 (de Morton et al.) | 0.01 | 0.01/6.0 = 0.002 =0.2% | NA | Not statistically significant | Silver |
| Total LOS (acute plus subacute)‐ additional exercise versus usual care | 380 (2) | 6.0 (de Morton et al.) | ‐0.70 days | 0.70/6.0 = 0.12 = 12% | NA | Not statistically significant | Silver |
| Legend: TUG=timed up and go test; LOS=length of stay; MDI=multidisciplinary intervention | m=mean | Wt=weighted | NNT=number needed to treat | sig=signficant |
| Outcome (scale) | # patients (#trials) | Control baseline m | Wt absolute change | Relative % change | NNT | Statistical sig | Quality of evidence |
| Barthel Index (original and modified versions, scale range 0‐100) ‐ additional exercise versus usual care | 293 (2) | 68.09 (de Morton et al.) | 0.17 x 26.08 = 4.43. This represents 4.45 more points on a 100 point Barthel Index scale. | 4.43/68.09 = 0.06 = 6% | NA | Not statistically significant | Silver |
| Legend: | m=mean | wt=weighted | NNT=number needed to treat | sig=significant |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Maintained or improved ADL scores between hospital admission and discharge ‐ MDI versus usual care Show forest plot | 3 | 2271 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.97, 1.15] |
| 2 Maintained or improved mobility scores between hospital admission and discharge ‐ MDI versus usual care Show forest plot | 3 | 2119 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.99, 1.06] |
| 3 Maintained or improved ADL scores between 2 weeks prior to hospital admission and discharge‐ MDI v usual care Show forest plot | 2 | 2001 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.00, 1.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in Barthel Index between hospital admission and discharge ‐ additional exercise versus usual care Show forest plot | 2 | 293 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.06, 0.40] |
| 2 Change in TUG scores between hospital admission and discharge ‐ additional exercise versus usual care Show forest plot | 2 | 188 | Mean Difference (IV, Random, 95% CI) | ‐2.52 [‐5.75, 0.71] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Patient mortality during hospitalisation ‐ MDI versus usual care Show forest plot | 6 | 3552 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.59, 1.64] |
| 2 Patient mortality 3 months after hospital discharge ‐ MDI versus usual care Show forest plot | 3 | 2595 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.83, 1.17] |
| 3 Patient complications during hospitalisation ‐ MDI versus usual care Show forest plot | 2 | 550 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.68, 1.29] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Patient mortality during hospitalisation ‐ additional exercise versus usual care Show forest plot | 3 | 696 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.98 [0.64, 6.18] |
| 2 Admission to the Intensive Care Unit (ICU) ‐ additional exercise versus usual care Show forest plot | 2 | 396 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.04, 30.44] |
| 3 Falls during hospitalisation ‐ additional exercise versus usual care Show forest plot | 2 | 384 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.40, 3.15] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Discharge to preadmission residence/home from hospital ‐ MDI versus usual care Show forest plot | 4 | 1675 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [1.03, 1.14] |
| 2 Acute hospital length of stay ‐ MDI versus usual care Show forest plot | 6 | 3478 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.93, ‐0.22] |
| 3 Cost of acute hospital stay ‐ MDI versus usual care Show forest plot | 5 | 3241 | Mean Difference (IV, Fixed, 95% CI) | ‐278.65 [‐491.85, ‐65.44] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Discharge to preadmission residence/home from hospital ‐ additional exercise versus usual care Show forest plot | 2 | 380 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.80, 1.66] |
| 2 Acute hospital length of stay ‐ additional exercise versus usual care Show forest plot | 3 | 680 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐1.23, 1.26] |
| 3 Total (acute plus subacute) hospital length of stay‐ additional exercise versus usual care Show forest plot | 2 | 380 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐2.58, 1.17] |


