Profilaxis antibiótica para el desgarro perineal de tercer y cuarto grado durante el parto vaginal
Appendices
Appendix 1. Search strategy
For the initial version of the review, authors searched CENTRAL (The Cochrane Library 2005, Issue 2), MEDLINE (1966 to 15 July 2005) using the strategy below:
#1 PERINEUM single term (MeSH)
#2 perine*
#3 (tear* or injur* or lacerat* or trauma or damage*)
#4 (#2 and #3)
#5 (anal near sphincter) or (rectal mucosa) or rectum or (anal epithelium) or anus or (recto‐vaginal fistulae) or (anorectal mucosa) or (anal skin)
#6 (tear* or injur* or damage* or lacerat* or rupture* or trauma)
#7 (#5 and #6)
#8 (obstetric* near tear*) or (obstetric near lacerat*)
#9 EPISIOTOMY single term (MeSH)
#10 episiotom* or postepisiotom*
#11 EXTRACTION OBSTETRICAL explode tree 1 (MeSH)
#12 vacuum or ventouse or forcep*
#13 deliver*
#14 (birth or childbirth or child‐birth or (child next birth))
#15 antibio*
#16 ANTIBIOTICS explode all trees (MeSH)
#17 (#1 or #4 or #7 or #8)
#18 (#9 or #10 or #11 or #12 or #13 or #14)
#19 (#15 or #16)
#20 (#17 and #18 and #19)
Appendix 2. Methods to be used in future updates
Data collection and analysis
Selection of studies
Two review authors will independently assess for inclusion all the potential studies we identify as a result of the search strategy. We will resolve any disagreement through discussion or, if required, we will consult a third person.
We will create a study flow diagram to map out the number of records identified, included and excluded.
Data extraction and management
We will design a form to extract data. For eligible studies, at least two review authors will extract the data using the agreed form. We will resolve discrepancies through discussion or, if required, we will consult a third person. We will enter data into Review Manager software (RevMan 2014) and check for accuracy.
When information regarding any of the above is unclear, we will attempt to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors will independently assess risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We will resolve any disagreement by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
We will describe for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We will assess the method as:
-
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
-
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
-
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We will describe for each included study the method used to conceal allocation to interventions prior to assignment and will assess whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We will assess the methods as:
-
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
-
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
-
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We will describe for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We will consider that studies are at low risk of bias if they were blinded, or if we judge that the lack of blinding would be unlikely to affect results. We will assess blinding separately for different outcomes or classes of outcomes.
We will assess the methods as:
-
low, high or unclear risk of bias for participants;
-
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We will describe for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We will assess blinding separately for different outcomes or classes of outcomes.
We will assess methods used to blind outcome assessment as:
-
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We will describe for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We will state whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information is reported, or can be supplied by the trial authors, we will re‐include missing data in the analyses which we undertake.
We will assess methods as:
-
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
-
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
-
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We will describe for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We will assess the methods as:
-
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
-
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
-
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We will describe for each included study any important concerns we have about other possible sources of bias.
We will assess whether each study was free of other problems that could put it at risk of bias:
-
low risk of other bias;
-
high risk of other bias;
-
unclear whether there is risk of other bias.
(7) Overall risk of bias
We will make explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we will assess the likely magnitude and direction of the bias and whether we consider it is likely to impact on the findings. We will explore the impact of the level of bias through undertaking sensitivity analyses ‐ see Sensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, we will present results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, we will use the mean difference if outcomes are measured in the same way between trials. We will use the standardised mean difference to combine trials that measure the same outcome, but use different methods.
Unit of analysis issues
Cluster‐randomised trials
We will include cluster‐randomised trials in the analyses along with individually randomised‐trials. We will adjust their sample sizes using the methods described in the Handbook using an estimate of the intracluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation unit.
Cross‐over trials
Cross‐over trials are not eligible for inclusion.
Dealing with missing data
For included studies, we will note levels of attrition. We will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we will carry out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we will attempt to include all participants randomised to each group in the analyses, and all participants will be analysed in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial will be the number randomised minus any participants whose outcomes are known to be missing.
Assessment of heterogeneity
We will assess statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We will regard heterogeneity as substantial if the I² is greater than 30% and either the Tau² is greater than zero, or there is a low P value (less than 0.10) in the Chi² test for heterogeneity.
Assessment of reporting biases
If there are 10 or more studies in the meta‐analysis, we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We will carry out statistical analysis using the Review Manager software (RevMan 2014). We will use fixed‐effect meta‐analysis for combining data where it is reasonable to assume that studies are estimating the same underlying treatment effect: i.e. where trials are examining the same intervention, and the trials’ populations and methods are judged sufficiently similar. If there is clinical heterogeneity sufficient to expect that the underlying treatment effects differ between trials, or if substantial statistical heterogeneity is detected, we will use random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials is considered clinically meaningful. The random‐effects summary will be treated as the average of the range of possible treatment effects and we will discuss the clinical implications of treatment effects differing between trials. If the average treatment effect is not clinically meaningful, we will not combine trials.
If we use random‐effects analyses, the results will be presented as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
If we identify substantial heterogeneity, we plan to investigate it using subgroup analyses and sensitivity analyses. We plan to consider whether an overall summary is meaningful, and if it is, use random‐effects analysis to produce it.
We plan to carry out the following subgroup analyses.
-
Immunocompromised versus not immunocompromised pregnant women, such as HIV infection, chronic steroid use.
-
Women with prolonged prelabour rupture membranes versus women without prolonged prelabour rupture membranes.
-
Women with preterm prelabour rupture membranes (PPROM) versus women without PPROM.
-
Third‐degree tears compared with fourth‐degree tears.
We will restrict subgroup analysis to the following outcomes.
-
Fever or puerperal febrile morbidity.
-
Perineal wound infection.
Sensitivity analysis
We will perform sensitivity analyses for aspects of the review that might affect primary outcomes (fever or puerperal febrile morbidity and perineal wound infection), such as where there was risk of bias associated with the quality of some of the included trials. We plan to carry out sensitivity analysis to explore the effects of fixed‐effect or random‐effects analyses for primary outcomes with statistical heterogeneity.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
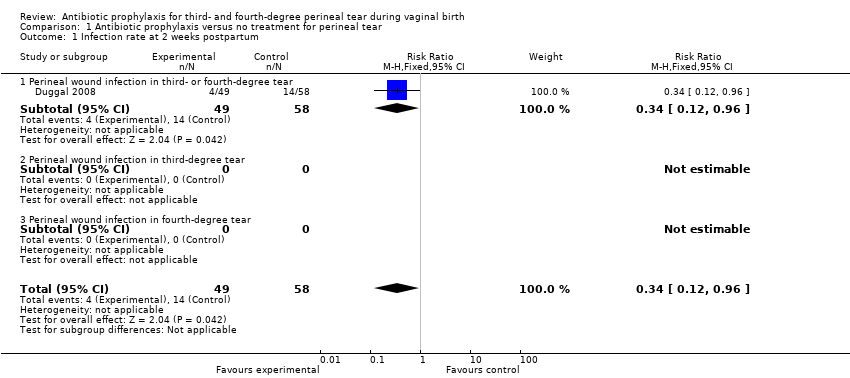
Comparison 1 Antibiotic prophylaxis versus no treatment for perineal tear, Outcome 1 Infection rate at 2 weeks postpartum.

Comparison 1 Antibiotic prophylaxis versus no treatment for perineal tear, Outcome 2 Infection rate at 6 weeks postpartum.
| Antibiotic prophylaxis versus no treatment for perineal tear for third‐ and fourth‐degree perineal tear during vaginal birth | ||||||
| Patient or population: Women with third‐ and fourth‐degree perineal tear during vaginal birth | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Antibiotic prophylaxis versus no treatment for perineal tear | |||||
| Infection rate at 2 weeks postpartum ‐ perineal wound infection in third‐ or fourth‐degree tear | Study population | RR 0.34 | 107 | ⊕⊕⊕⊝ | ||
| 241 per 1000 | 82 per 1000 | |||||
| Moderate | ||||||
| 241 per 1000 | 82 per 1000 | |||||
| Infection rate at 6 weeks postpartum ‐ perineal wound infection in third‐ or fourth‐degree tear | Study population | RR 0.38 | 128 | ⊕⊕⊝⊝ | ||
| 192 per 1000 | 73 per 1000 | |||||
| Moderate | ||||||
| 192 per 1000 | 73 per 1000 | |||||
| Fever or puerperal febrile morbidity | Not estimable | 0 study | See comment | This outcome was not reported in the one included study. | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Small sample size and not met optimal information size (OIS) criteria. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Infection rate at 2 weeks postpartum Show forest plot | 1 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.12, 0.96] |
| 1.1 Perineal wound infection in third‐ or fourth‐degree tear | 1 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.12, 0.96] |
| 1.2 Perineal wound infection in third‐degree tear | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 Perineal wound infection in fourth‐degree tear | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Infection rate at 6 weeks postpartum Show forest plot | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.13, 1.09] |
| 2.1 Perineal wound infection in third‐ or fourth‐degree tear | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.13, 1.09] |
| 2.2 Perineal wound infection in third‐degree tear | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 Perineal wound infection in fourth‐degree tear | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

