Musicoterapia para pacientes con esquizofrenia y trastornos similares a la esquizofrenia
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: people with schizophrenia (ICD‐10). | |
| Interventions | 1. Group music therapy: STAM (one weekly session; total 16 sessions). N = 37. | |
| Outcomes | Cognitive functioning: BCST, CCPT, PASAT, WMS. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised ‐ no further details. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding (performance bias and detection bias) | Low risk | Assessors were masked to treatment. |
| Incomplete outcome data (attrition bias) | Low risk | No drop outs. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes were considered in the analysis. |
| Other bias | Unclear risk | Adequate music therapy method: unclear (highly structured approach, relational aspects unclear). |
| Methods | Allocation: randomised ‐ no further details. | |
| Participants | Diagnosis: schizophrenia type II (CCMD‐3). | |
| Interventions | 1. Receptive and 'participative' group music therapy (music listening, or music listening in combination with reading poems or dancing, music was chosen by the participants after an "induction" given by the therapist), five one‐hour sessions per week (total 30 sessions). N = 30. | |
| Outcomes | Mental state: SANS. | |
| Notes | Music therapy was conducted by musicians. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding (performance bias and detection bias) | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) | Unclear risk | No information about how many participants have completed the study can be found in the results or discussion part of the article. According to the study design (only inpatients) and Chinese reporting standards (drop outs are usually reported if there are any) we assume that all participants have completed the study. |
| Selective reporting (reporting bias) | Low risk | All outcome measures were considered in the analysis. |
| Other bias | High risk | Adequate music therapy method: yes. |
| Methods | Allocation: randomised ‐ no further details. | |
| Participants | Diagnosis: schizophrenia (CCMD‐3). | |
| Interventions | 1. Receptive group music therapy (music listening, music listening in combination with verbal inductions given by the therapist, 'positive hypnosis'/positive imagery, ), 5 weekly 40‐min sessions per week (total 30 sessions). N = 30. | |
| Outcomes | Mental state: depression (SDS). | |
| Notes | Music therapy was conducted by nurses, unclear how much they were trained in music therapy. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding (performance bias and detection bias) | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) | Low risk | All 60 participants completed the trial. |
| Selective reporting (reporting bias) | Low risk | All outcome measures were considered in the analysis. |
| Other bias | Unclear risk | Adequate music therapy method: yes. |
| Methods | Allocation: randomised ‐ block randomisation with ratio of experimental treatment to control treatment 1:2. | |
| Participants | Diagnosis: schizophrenia or related psychoses (ICD‐10: F2). | |
| Interventions | 1. Active individual music therapy (improvisation, songs, dialogue), weekly sessions of 50 min (total 12 sessions). N = 33. | |
| Outcomes | Mental state: PANSS. Unable to use ‐Quality of life: SFQ (unknown reliability and validity). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers. |
| Allocation concealment (selection bias) | Low risk | Randomisation was conducted by a person independent of the researcher, and extensive steps were taken to mask the researcher to the participants' allocation status. |
| Blinding (performance bias and detection bias) | Low risk | Interviews were conducted by a researcher masked to treatment condition; a test of the success of masking was provided: Interviewer attempted to guess the allocation status of each of the participants after three month follow‐up data had been collected (kappa = .31, P <. 01). |
| Incomplete outcome data (attrition bias) | Low risk | Analysis was carried out on an intention‐to‐treat basis. Multiple imputation was used to account for the missing data in outcome measures at follow‐up. This method imputes m > 1 plausible values for each missing value, under the assumption of missing at random. In this review, only the actually observed data were used, not the imputed data. Multiple imputation is not recommended when only dependent variables are missing (Allison 2002, p. 54, p. 70). |
| Selective reporting (reporting bias) | Low risk | All outcome measures were considered in the analysis. |
| Other bias | Low risk | Adequate music therapy method: yes. |
| Methods | Allocation: randomised ‐ no further details. | |
| Participants | Diagnosis: residual schizophrenia (DSM‐III‐R). | |
| Interventions | 1. Active and receptive large‐group music therapy (music listening, singing and playing on instruments, discussion), five one‐hour sessions per week (on average 19 sessions). N = 38. | |
| Outcomes | Mental state: SANS. Unable to use ‐ | |
| Notes | Author unable to provide additional data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding (performance bias and detection bias) | Low risk | Nurses who did the SANS and DAS assessment for participants were blind to treatment status. |
| Incomplete outcome data (attrition bias) | Low risk | All 76 participants completed the trial. |
| Selective reporting (reporting bias) | Low risk | All outcome measures were considered in the analysis. |
| Other bias | Unclear risk | Adequate music therapy method: yes. |
| Methods | Allocation: randomised ‐ no further details. | |
| Participants | Diagnosis: schizophrenia or related psychoses (27 of 37 had F20 in ICD‐10). | |
| Interventions | 1. Active group music therapy (focusing on musical processes and discussion of patients' problems), on average 7.5 sessions of 60 to 105 minutes. N = 21. | |
| Outcomes | Mental state: SANS. Unable to use ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A die was thrown. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding (performance bias and detection bias) | Low risk | Researchers and patients were blinded to the fact that research of music therapy was the study aim. |
| Incomplete outcome data (attrition bias) | Low risk | Drop outs were reported. Intention‐to‐treat analysis was used: Participants whose diagnosis was changed after inclusion in the study were not excluded. |
| Selective reporting (reporting bias) | Low risk | All outcome measures were considered in the analysis. |
| Other bias | Low risk | Adequate music therapy method: yes. |
| Methods | Allocation: randomised; no further details given. | |
| Participants | Diagnosis: schizophrenia (CCMD‐3). | |
| Interventions | 1. Receptive group music therapy (music listening, other music activities: dancing, discussion emphasising the emotional aspects of the music while listening to it), five one‐hour sessions per week (total 30 sessions). N = 16. | |
| Outcomes | Mental state: BPRS; depression (SDS, Ham‐D). | |
| Notes | Music therapy was conducted by the authors (probably psychiatrists) and nurses. No information given if these clinicians were trained in music therapy. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding (performance bias and detection bias) | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the trial. |
| Selective reporting (reporting bias) | Low risk | All outcome measures were considered in the analysis. |
| Other bias | Unclear risk | Adequate music therapy method: yes. |
| Methods | Allocation: randomised ‐ no further details. | |
| Participants | Diagnosis: schizophrenia (CCMD‐2). | |
| Interventions | 1. Active and receptive individual and group music therapy (music listening, improvisation, discussion), six two‐hour sessions per week (total 78 sessions). N = 41. | |
| Outcomes | Global state: No clinically important improvement (as rated by trialists). Unable to use ‐ | |
| Notes | Author unable to provide additional data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding (performance bias and detection bias) | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) | Unclear risk | Two drop outs were reported and the reported data are based on a total number excluding the drop outs. No participants with complete data were excluded. |
| Selective reporting (reporting bias) | Low risk | All outcome measures were considered in the analysis. |
| Other bias | Low risk | Adequate music therapy method: yes. |
BCST ‐ Bergs' Card Sorting Test
BPRS – Brief Psychiatric Rating Scale
CCMD‐2/3 ‐ Chinese Classification of Mental Disorders 2/3
CCPT ‐ Conners Continuous Performance Task 10
CSQ ‐ Client Satisfaction Questionnaire
DAS ‐ Disability Assessment Schedule
DSM‐III‐R ‐ Diagnostic and Statistical Manual of Mental Disorders‐III‐R
ePEX ‐ Protechnic Exeter
F ‐ Female
GAF – General Assessment of Function
Ham‐D – Hamilton Depression Scale
HAS – Hamilton Anxiety Scale
ICD‐10 ‐ ICD‐10: F2 – International Classification of Diseases (version 10); ‘F’ refers to large disease sub‐categories within ICD
M ‐ Male
NOSIE ‐ Nurses' Observation Scale for Inpatient Evaluation
PANSS ‐ The Positive and Negative Syndrome Scale
PASAT ‐ Auditory Serial Addition Paced Test
PSE ‐ Present State Examination Change Rating Scale
SANS ‐ Scale for the Assessment of Negative Symptoms
SAS ‐ Self‐Rating Anxiety Scale
SD – Standard deviation
SDS ‐ Self‐Rating Depression Scale
SDSI ‐ Social Disability Schedule for Inpatients
SFQ ‐ The Social Functioning Questionnaire
SPG ‐ Skalen zur psychischen Gesundheit
STAM ‐ Sound Training Attention and Memory
WMS ‐ Wechsler Memory Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: not randomised (all received the same intervention). | |
| Allocation: randomised. | |
| Allocation: unclear (unable to retrieve full report). | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: not randomised (CCT, matched groups). | |
| Allocation: randomised. | |
| Allocation: not randomised (single case study). | |
| Allocation: not randomised (single group study). | |
| Allocation: randomised. | |
| Allocation: unclear (CCT; author was contacted but we did not get the requested information). | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: not randomised (pre‐post test). | |
| Allocation: randomised. | |
| Allocation: not randomised (CCT/comparison of 2 cohorts). | |
| not able to retrieve information needed. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: not randomised (single group study). | |
| Allocation: not randomised (n‐of‐1‐CCT). | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: not randomised (CCT, quasi‐randomised). | |
| Allocation: not randomised (single case study). | |
| Allocation: not randomised (single group study). | |
| Allocation: not randomised (single case study). | |
| Allocation: not randomised (single group study). | |
| Allocation: not randomised (CCT, allocation by order of intake). | |
| Allocation: not randomised (CCT, cross‐over design) | |
| Allocation: not randomised (CCT). | |
| Allocation: randomised. | |
| Allocation: not randomised (CCT, allocation by order of intake). | |
| Allocation: not randomised (CCT, matched groups). | |
| Allocation: randomised. | |
| Allocation: not randomised (single group study). | |
| Allocation: not randomised (single group study). | |
| Allocation: not randomised (single case study). | |
| Allocation: randomised. | |
| Allocation: not randomised (single group study). | |
| Allocation: not randomised (groups were matched by age, sex, education, and diagnosis). | |
| Allocation: not randomised (single group study). | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: not randomised (single group study). | |
| Allocation: not randomised (single group study). | |
| Allocation: not randomised to music therapy versus placebo or standard care (random allocation of participants to three active treatment conditions including music therapy; a control group (medication only) was not randomised but obtained from a waiting list). | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: not randomised (CCT, quasi‐randomised according to the date of entry). | |
| Allocation: not randomised (CCT, quasi‐randomised according to the date of entry). | |
| Allocation: randomised. | |
| Allocation: not randomised (all received the same stimuli within the same session); not an intervention study. | |
| Allocation: not randomised (pre‐post test design). | |
| Allocation: not randomised (uncontrolled pre‐post design). | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: possibly randomised, unclear. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. | |
| Allocation: randomised. |
CBT – Cognitive Behavioural Therapy
CCT – Controlled Clinical Trial
MTV – Music Television
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Resource‐oriented music therapy for psychiatric patients with low therapy motivation (RCT‐MTPSY, registration no. NCT00137189). |
| Methods | Allocation: randomised, stratified by treatment centre and type of disorder (psychotic versus non‐psychotic). |
| Participants | Diagnosis: people with a non‐organic mental disorder (F1 to F6 according to ICD‐10), presenting with a low therapy motivation and showing a willingness to work with music. |
| Interventions | 1. Individual resource‐oriented music therapy, 2 times a week over a period of 3 months, lasting 45 minutes; in addition to standard care. |
| Outcomes | Mental state: Negative Symptoms (SANS), SANS Subscale Affective Flattening or Blunting. General Functioning: Global Assessment of Functioning Scale (GAF). Interpersonal and social functioning: Inventory of Interpersonal Problems (IIP‐32). Intrapersonal functioning: Motivation for change, URICA. Intrapersonal functioning: Self‐efficacy, General Perceived Sef‐Efficacy Scale. Intrapersonal functioning: Rosenberg Self Esteem Scale (RSES). Quality of life: Quality of Life Enjoyment and Satisfaction Questionnare‐18 (Q‐LES‐Q‐18). Musical engagement: Interest in Music Scale (IiM). |
| Starting date | 2004. |
| Contact information | Christian Gold. |
| Notes |
| Trial name or title | Evaluation of a group music therapy program on quality of life in people living with severe and enduring mental illness (SEMI) in the community. |
| Methods | Allocation: randomised. |
| Participants | Diagnosis: severe and enduring mental disorder (e.g. schizophrenia, bipolar disorders, major depression). |
| Interventions | 1. Group music therapy (including singing, percussive improvisation, writing and recording an original song). |
| Outcomes | Mental state: BSI. Quality of life: Q‐LES‐Q‐18. Social functioning: ESSI. Intrapersonal functioning: Self‐esteem (RSES). |
| Starting date | 2009. |
| Contact information | Denise Grocke. |
| Notes |
BSI / BSI‐18 ‐ Brief Symptom Inventroy‐18
CGI ‐ Clinical Global Impressions Scale
SF‐36 ‐ Short Form‐36 Health Survey
ESSI ‐ ENRICHED Social Support Instrument
GAF ‐ Global Assessment of Functioning Scale
IiM ‐ Interest i Music
IIP‐32 ‐ Inventory of Interpersonal Problems
Q‐LES‐Q‐18 ‐ Quality of Life Enjoyment and Satisfaction Questionnare‐18
RCT randomised controlled trial
RSES ‐ Rosenberg Self Esteem Scale
SANS ‐ Scale for the Assessment of Negative Symptoms
URICA ‐ The University of Rhode Island Change Assessment Scale
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: No clinically important overall improvement (as rated by trialists) Show forest plot | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.03, 0.31] |
| Analysis 1.1  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 1 Global state: No clinically important overall improvement (as rated by trialists). | ||||
| 1.1 20 or more sessions | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.03, 0.31] |
| 2 Mental state: General ‐ 1a. Average endpoint score (PANSS, high score = poor) Show forest plot | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐0.84, 0.12] |
| Analysis 1.2  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 2 Mental state: General ‐ 1a. Average endpoint score (PANSS, high score = poor). | ||||
| 2.1 less than 20 sessions | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐0.84, 0.12] |
| 3 Mental state: General ‐ 1b. Average endpoint score (BPRS, high score = poor) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 3 Mental state: General ‐ 1b. Average endpoint score (BPRS, high score = poor). | ||||
| 3.1 20 or more sessions | 2 | 100 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.73 [‐1.16, ‐0.31] |
| 4 Mental state: Specific ‐ 2. Negative symptoms ‐ average endpoint score (SANS, high score = poor) Show forest plot | 4 | 240 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.74 [‐1.00, ‐0.47] |
| Analysis 1.4  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 4 Mental state: Specific ‐ 2. Negative symptoms ‐ average endpoint score (SANS, high score = poor). | ||||
| 4.1 less than 20 sessions | 2 | 110 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.79 [‐1.19, ‐0.40] |
| 4.2 20 or more sessions | 2 | 130 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.69 [‐1.05, ‐0.33] |
| 5 Mental state: Specific ‐ 3a. Depression ‐ average endpoint score (SDS, high score = poor) Show forest plot | 2 | 90 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.63 [‐1.06, ‐0.21] |
| Analysis 1.5  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 5 Mental state: Specific ‐ 3a. Depression ‐ average endpoint score (SDS, high score = poor). | ||||
| 5.1 20 or more sessions | 2 | 90 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.63 [‐1.06, ‐0.21] |
| 6 Mental state: Specific ‐ 3b. Depression ‐ average endpoint score (Ham‐D, high score = poor) Show forest plot | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐1.25, 0.21] |
| Analysis 1.6  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 6 Mental state: Specific ‐ 3b. Depression ‐ average endpoint score (Ham‐D, high score = poor). | ||||
| 6.1 20 or more sessions | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐1.25, 0.21] |
| 7 Mental state: Specific ‐ 4. Anxiety ‐ average endpoint score (SAS, high score = poor) Show forest plot | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.61 [‐1.13, ‐0.09] |
| Analysis 1.7  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 7 Mental state: Specific ‐ 4. Anxiety ‐ average endpoint score (SAS, high score = poor). | ||||
| 7.1 20 or more sessions | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.61 [‐1.13, ‐0.09] |
| 8 Leaving the study early Show forest plot | 8 | 493 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.38, 2.78] |
| Analysis 1.8  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 8 Leaving the study early. | ||||
| 8.1 less than 20 sessions | 4 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.36, 2.99] |
| 8.2 20 or more sessions | 4 | 232 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.06, 15.45] |
| 9 General functioning: Average endpoint score (GAF, high score = good) Show forest plot | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.53, 0.43] |
| Analysis 1.9  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 9 General functioning: Average endpoint score (GAF, high score = good). | ||||
| 9.1 less than 20 sessions | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.53, 0.43] |
| 10 Social functioning: Average endpoint score (SDSI, high score = poor) Show forest plot | 1 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.78 [‐1.27, ‐0.28] |
| Analysis 1.10  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 10 Social functioning: Average endpoint score (SDSI, high score = poor). | ||||
| 10.1 20 or more sessions | 1 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.78 [‐1.27, ‐0.28] |
| 11 Behaviour: 1. Positive behaviour ‐ average endpoint score (NOSIE, high score = poor) Show forest plot | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.24 [‐1.79, ‐0.68] |
| Analysis 1.11  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 11 Behaviour: 1. Positive behaviour ‐ average endpoint score (NOSIE, high score = poor). | ||||
| 11.1 20 or more sessions | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.24 [‐1.79, ‐0.68] |
| 12 Behaviour: 2. Negative behaviour ‐ average endpoint score (NOSIE, high score = poor) Show forest plot | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐2.22 [‐2.87, ‐1.57] |
| Analysis 1.12  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 12 Behaviour: 2. Negative behaviour ‐ average endpoint score (NOSIE, high score = poor). | ||||
| 12.1 20 or more sessions | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐2.22 [‐2.87, ‐1.57] |
| 13 Cognitive functioning: 1. Attention ‐ average endpoint score (PASAT, high score = good) Show forest plot | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.72 [0.22, 1.21] |
| Analysis 1.13  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 13 Cognitive functioning: 1. Attention ‐ average endpoint score (PASAT, high score = good). | ||||
| 13.1 less than 20 sessions | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.72 [0.22, 1.21] |
| 14 Cognitive functioning: 2. Vigilance and attention ‐ average endpoint score (CCPT, high score = good) Show forest plot | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.23, 0.74] |
| Analysis 1.14  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 14 Cognitive functioning: 2. Vigilance and attention ‐ average endpoint score (CCPT, high score = good). | ||||
| 14.1 less than 20 sessions | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.23, 0.74] |
| 15 Cognitive functioning: 3. Memory ‐ average endpoint score (WMS, high score = good) Show forest plot | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [‐0.06, 0.92] |
| Analysis 1.15  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 15 Cognitive functioning: 3. Memory ‐ average endpoint score (WMS, high score = good). | ||||
| 15.1 less than 20 sessions | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [‐0.06, 0.92] |
| 16 Cognitive functioning: 4. Abstract thinking ‐ average endpoint score (BCST, high score = good) ) Show forest plot | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.39, 0.58] |
| Analysis 1.16  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 16 Cognitive functioning: 4. Abstract thinking ‐ average endpoint score (BCST, high score = good) ). | ||||
| 16.1 less than 20 sessions | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.39, 0.58] |
| 17 Patient satisfaction: Average endpoint score (CSQ, high score = good) Show forest plot | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.16, 0.80] |
| Analysis 1.17  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 17 Patient satisfaction: Average endpoint score (CSQ, high score = good). | ||||
| 17.1 less than 20 sessions | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.16, 0.80] |
| 18 Quality of life: Average endpoint score (SPG, high score = good) Show forest plot | 1 | 31 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.66, 0.75] |
| Analysis 1.18  Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 18 Quality of life: Average endpoint score (SPG, high score = good). | ||||
| 18.1 less than 20 sessions | 1 | 31 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.66, 0.75] |

Study flow diagram (all searches)

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 1 Global state: No clinically important overall improvement (as rated by trialists).

Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 2 Mental state: General ‐ 1a. Average endpoint score (PANSS, high score = poor).
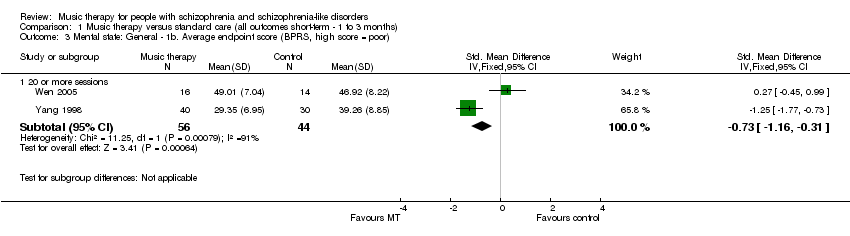
Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 3 Mental state: General ‐ 1b. Average endpoint score (BPRS, high score = poor).

Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 4 Mental state: Specific ‐ 2. Negative symptoms ‐ average endpoint score (SANS, high score = poor).
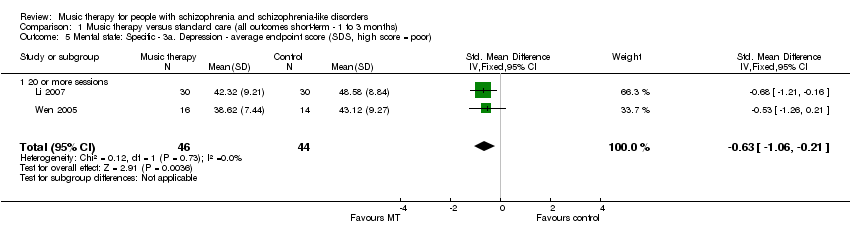
Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 5 Mental state: Specific ‐ 3a. Depression ‐ average endpoint score (SDS, high score = poor).

Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 6 Mental state: Specific ‐ 3b. Depression ‐ average endpoint score (Ham‐D, high score = poor).
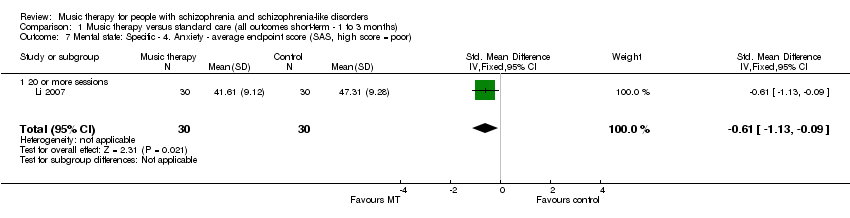
Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 7 Mental state: Specific ‐ 4. Anxiety ‐ average endpoint score (SAS, high score = poor).

Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 8 Leaving the study early.
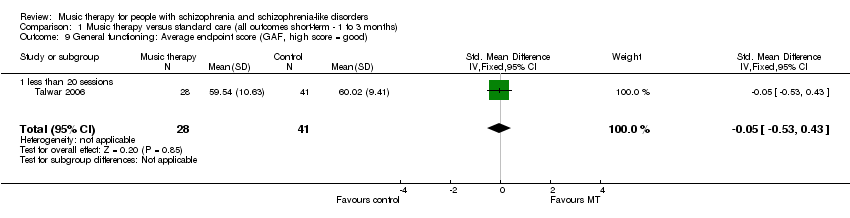
Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 9 General functioning: Average endpoint score (GAF, high score = good).
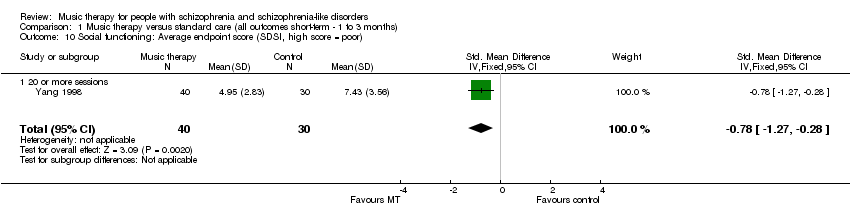
Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 10 Social functioning: Average endpoint score (SDSI, high score = poor).
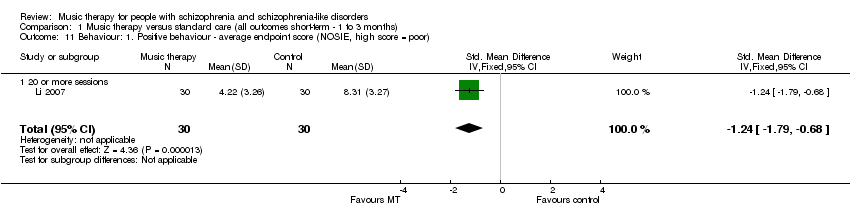
Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 11 Behaviour: 1. Positive behaviour ‐ average endpoint score (NOSIE, high score = poor).

Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 12 Behaviour: 2. Negative behaviour ‐ average endpoint score (NOSIE, high score = poor).
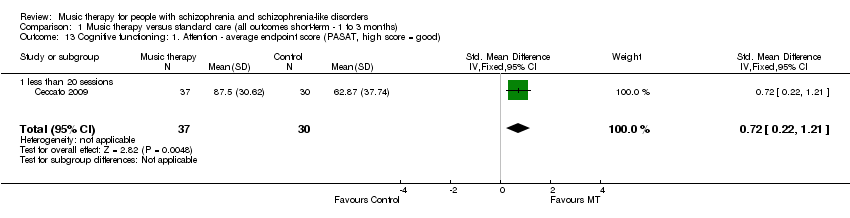
Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 13 Cognitive functioning: 1. Attention ‐ average endpoint score (PASAT, high score = good).

Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 14 Cognitive functioning: 2. Vigilance and attention ‐ average endpoint score (CCPT, high score = good).

Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 15 Cognitive functioning: 3. Memory ‐ average endpoint score (WMS, high score = good).

Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 16 Cognitive functioning: 4. Abstract thinking ‐ average endpoint score (BCST, high score = good) ).
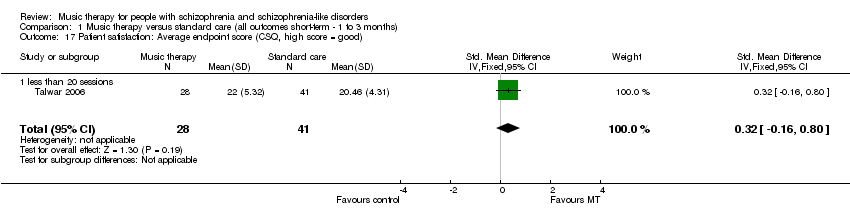
Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 17 Patient satisfaction: Average endpoint score (CSQ, high score = good).

Comparison 1 Music therapy versus standard care (all outcomes short‐term ‐ 1 to 3 months), Outcome 18 Quality of life: Average endpoint score (SPG, high score = good).
| MUSIC THERAPY versus STANDARD CARE for people with schizophrenia and schizophrenia‐like disorders | ||||||
| Patient or population: people with schizophrenia and schizophrenia‐like disorders | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | MUSIC THERAPY versus STANDARD CARE | |||||
| Mental state: Negative symptoms | The mean Mental state: Negative symptoms in the intervention groups was | 240 | ⊕⊕⊕⊕ | SMD ‐0.74 (‐1 to ‐0.47) | ||
| Social functioning | The mean Social functioning in the intervention groups was | 70 | ⊕⊕⊕⊕ | SMD ‐0.78 (‐1.27 to ‐0.28) | ||
| Global state: No clinically important overall improvement | Study population | RR 0.1 | 72 | ⊕⊕⊕⊕ | ||
| 710 per 1000 | 71 per 1000 | |||||
| Medium risk population | ||||||
| 710 per 1000 | 71 per 1000 | |||||
| General mental state | The mean General mental state in the intervention groups was | 69 | ⊕⊕⊕⊕ | SMD ‐0.36 (‐0.84 to 0.12) | ||
| General mental state | The mean General mental state in the intervention groups was | 100 | ⊕⊕⊕⊝ | SMD ‐0.73 (‐1.16 to ‐0.31) | ||
| General functioning | The mean General functioning in the intervention groups was | 69 | ⊕⊕⊕⊝ | SMD ‐0.05 (‐0.53 to 0.43) | ||
| Quality of life | The mean Quality of life in the intervention groups was | 31 | ⊕⊕⊕⊝ | SMD 0.05 (‐0.66 to 0.75) | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Limitations in the designs such as poorly reported randomisation and blinding, as well as less‐well defined music therapy. | ||||||
| No. of | Adequate | Adequate | Modality | Form of therapy | Therapy | ||||||
| Improvisation | Playing and/or singing pre‐ | Songwriting | Listening | Verbal | Others | ||||||
| Max. 16 (1/week over 4 months) | Yes | Yes | Receptive | No | No | No | Central | No | No | Fixed structure | |
| Max. 30 | Yes | Unclear | Receptive | No | No | No | Central | Yes | Dancing, reading poems with music background | Unclear | |
| Max. 30 | Yes | Unclear | Receptive | No | No | No | Central | Yes | No | Unclear | |
| Max. 12 sessions (1/week over 3 months) | Yes | Yes | Active | Central | Yes | No | No | Central | No | Process‐ | |
| 19 sessions received | Yes | Unclear | Both | Yes | Yes | No | Central | Yes | No | Fixed structure | |
| 7.5 sessions received | Yes | Yes | Active | Yes | Yes | No | No | Yes | No | Process‐ | |
| Max. 30 | Yes | Unclear | Receptive | No | No | No | Central | Yes | Dancing | Unclear | |
| Max. 78 (6/week over 3 months) | Yes | Yes | Both | Yes | Yes | No | Yes | Yes | Learning musicology | Unclear | |
| Adequate music therapeutic method: A "yes" indicates that the method applied considered both musical experiences and relational aspects as dynamic forces of change in music therapy. A "no" indicates that relational aspects are missing. | |||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Global state: No clinically important overall improvement (as rated by trialists) Show forest plot | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.03, 0.31] |
| 1.1 20 or more sessions | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.03, 0.31] |
| 2 Mental state: General ‐ 1a. Average endpoint score (PANSS, high score = poor) Show forest plot | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐0.84, 0.12] |
| 2.1 less than 20 sessions | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐0.84, 0.12] |
| 3 Mental state: General ‐ 1b. Average endpoint score (BPRS, high score = poor) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 20 or more sessions | 2 | 100 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.73 [‐1.16, ‐0.31] |
| 4 Mental state: Specific ‐ 2. Negative symptoms ‐ average endpoint score (SANS, high score = poor) Show forest plot | 4 | 240 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.74 [‐1.00, ‐0.47] |
| 4.1 less than 20 sessions | 2 | 110 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.79 [‐1.19, ‐0.40] |
| 4.2 20 or more sessions | 2 | 130 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.69 [‐1.05, ‐0.33] |
| 5 Mental state: Specific ‐ 3a. Depression ‐ average endpoint score (SDS, high score = poor) Show forest plot | 2 | 90 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.63 [‐1.06, ‐0.21] |
| 5.1 20 or more sessions | 2 | 90 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.63 [‐1.06, ‐0.21] |
| 6 Mental state: Specific ‐ 3b. Depression ‐ average endpoint score (Ham‐D, high score = poor) Show forest plot | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐1.25, 0.21] |
| 6.1 20 or more sessions | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐1.25, 0.21] |
| 7 Mental state: Specific ‐ 4. Anxiety ‐ average endpoint score (SAS, high score = poor) Show forest plot | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.61 [‐1.13, ‐0.09] |
| 7.1 20 or more sessions | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.61 [‐1.13, ‐0.09] |
| 8 Leaving the study early Show forest plot | 8 | 493 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.38, 2.78] |
| 8.1 less than 20 sessions | 4 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.36, 2.99] |
| 8.2 20 or more sessions | 4 | 232 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.06, 15.45] |
| 9 General functioning: Average endpoint score (GAF, high score = good) Show forest plot | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.53, 0.43] |
| 9.1 less than 20 sessions | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.53, 0.43] |
| 10 Social functioning: Average endpoint score (SDSI, high score = poor) Show forest plot | 1 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.78 [‐1.27, ‐0.28] |
| 10.1 20 or more sessions | 1 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.78 [‐1.27, ‐0.28] |
| 11 Behaviour: 1. Positive behaviour ‐ average endpoint score (NOSIE, high score = poor) Show forest plot | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.24 [‐1.79, ‐0.68] |
| 11.1 20 or more sessions | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.24 [‐1.79, ‐0.68] |
| 12 Behaviour: 2. Negative behaviour ‐ average endpoint score (NOSIE, high score = poor) Show forest plot | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐2.22 [‐2.87, ‐1.57] |
| 12.1 20 or more sessions | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐2.22 [‐2.87, ‐1.57] |
| 13 Cognitive functioning: 1. Attention ‐ average endpoint score (PASAT, high score = good) Show forest plot | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.72 [0.22, 1.21] |
| 13.1 less than 20 sessions | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.72 [0.22, 1.21] |
| 14 Cognitive functioning: 2. Vigilance and attention ‐ average endpoint score (CCPT, high score = good) Show forest plot | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.23, 0.74] |
| 14.1 less than 20 sessions | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.23, 0.74] |
| 15 Cognitive functioning: 3. Memory ‐ average endpoint score (WMS, high score = good) Show forest plot | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [‐0.06, 0.92] |
| 15.1 less than 20 sessions | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [‐0.06, 0.92] |
| 16 Cognitive functioning: 4. Abstract thinking ‐ average endpoint score (BCST, high score = good) ) Show forest plot | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.39, 0.58] |
| 16.1 less than 20 sessions | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.39, 0.58] |
| 17 Patient satisfaction: Average endpoint score (CSQ, high score = good) Show forest plot | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.16, 0.80] |
| 17.1 less than 20 sessions | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.16, 0.80] |
| 18 Quality of life: Average endpoint score (SPG, high score = good) Show forest plot | 1 | 31 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.66, 0.75] |
| 18.1 less than 20 sessions | 1 | 31 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.66, 0.75] |

