Antibiotic prophylaxis for hernia repair.
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Study: prospective, randomized | |
| Participants | 287 patients: | |
| Interventions | ATB= ampicillin 1 g subfascial | |
| Outcomes | IP= 5 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | D ‐ Not used |
| Methods | Study: prospective, randomized. | |
| Participants | 97 patients: | |
| Interventions | ATB= cefaloridine 1 g IM | |
| Outcomes | IP= 1 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Methods | Study: prospective, randomized. | |
| Participants | 308 patients: | |
| Interventions | ATB= cefamandol 750 mg subcutaneous. | |
| Outcomes | IP= 0 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | Study: multicenter, prospective, randomized. | |
| Participants | 524 patients: | |
| Interventions | ATB= cefazolin 2 g IV. | |
| Outcomes | IP= 4 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Study: | |
| Participants | 247 patients: | |
| Interventions | ATB= amoxicillin‐clavulanic 2 g IV | |
| Outcomes | IP= 1 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Study: multicenter, prospective, randomized. | |
| Participants | 612 patients: | |
| Interventions | ATB= cefonicid 1 g IV | |
| Outcomes | IP= 4 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Study: multicenter, prospective, randomized. | |
| Participants | 269 patients:136 P / 133 C | |
| Interventions | ATB= Amoxicillin‐clavulanic 1,2 g IV. | |
| Outcomes | IP= 1IC= 12 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Study: prospective, randomized. | |
| Participants | 269 patients: | |
| Interventions | ATB= Ampicilln‐sulbactam 1,5 g IV. | |
| Outcomes | IP= 1 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
P = prophylaxis group, C = control group, IP = infected with prophylaxis, IC = infected without prophylaxis, NM = not mencioned, ATB = antibiotic, MA = timing of prophylaxis administration
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| NOT RANDOMIZED. A total of 1524 consecutive hernia patients, dividided in 3 groups: A) 606 with ceftriaxone, B) 408 with pefloxacine, C) 510 with several cefalosporins or quinolons differents to the A and B groups. One single patient with infection was observed (0,06%). | |
| UNCONTROLLED TRIAL. Single arm with antibiotic prophylaxis. 112 patients submitted to prosthetic herniplasty by anterior approach (94 cases) and by transabdominal preperitoneal laparoscopy (18 cases), received levofloxacin 500 mg IV 30 minutes before the surgical operation and 500 mg os in seven days following. Infection rate was zero. | |
| RETROSPECTIVE. Study developed in two hospitals, one arm by hospital. Administers cefotaxime 2 gr IV 30' before surgery. A total of 147 patients, 63 with prophylaxis and 84 without; 87% with hernioplasty . Both hospitals show an infection rate of zero. | |
| DOES NOT INCLUDE HERNIA PATHOLOGY. | |
| UNCONTROLLED TRIAL. Single arm with antibiotic prophylaxis. Patients with several pathologies; can be identified 189 hernia patients (100 herniorraphy, 89 hernioplasty), prophylaxis with teicoplanine. Infection rate: zero. | |
| RETROSPECTIVE. Study with 475 patients. In 277 prosthetic material is used: 144 with antibiotic prophylaxis (3 infected) and 133 with placebo (10 infected). In 198 patients no prosthetic material was used: 14 with antibiotic prophylaxis (0 infected) and 184 with placebo (13 infected). They recommend prophylaxis when using prosthetic material. | |
| DOES NOT INCLUDE HERNIA PATHOLOGY. | |
| UNCONTROLLED TRIAL. Single arm with antibiotic prophylaxis. 1254 patients intervened with prosthetic material, received ceftriaxone IV 2 g before surgery. Infection rate assessed retrospectively: zero . | |
| RETROSPECTIVE. Large serie that presents methodologic handicaps. Infection rate: a)primary herniorraphy: 1.1% without prophylaxis and 1.3% with prophylaxis; b) primary hernioplasty: 0.34% without prophylaxis and 0.98% with prophylaxis; c) herniorraphy for recurrent hernia: 0% in both groups; d) hernioplasty for recurrent hernia: 2.2% without prophylaxis and 0.43% with prophylaxis. They do not recommend antibiotic prophylaxis on surgery for hernia repair. | |
| PROPHYLAXIS WITH ANTISEPTIC TREATMENT. | |
| RETROSPECTIVE. Multicentric trial where 71% of 5.506 patients received antibiotic prophylaxis. Global infection rate: 8%, without significative differences between patients with and without antibiotic prophylaxis (RR 0.9, IC95% 0.7 ‐ 1.1). Individualized infection rate is not provided for each group. They recommend not to administer antibiotic prophylaxis. | |
| REVIEW. In a study of clean surgical techniques, 134 hydroceles and hernias are included, without antibiotic prophylaxis. Infection rate 3,6%. | |
| INCOMPLETE DATA. The objective of the study is prophylaxis in incisional hernia and patients with inguinal hernia constitute the control group. Data for these patients is not provided. | |
| INCOMPLETE STUDY. No results provided. | |
| INCOMPLETE DATA. Prospective, randomized, well‐designed study on clean surgical techniques. A total of 165 patients had hernia repair (86 receiving cefotaxime 2 gr IV prior to surgery and 79 receiving placebo), but there's no information on the number of infections on these patients. INCOMPLETE DATA. Prospective, randomized, well‐designed study on clean surgical techniques. A total of 165 patients had hernia repair (86 receiving cefotaxime 2 gr IV prior to surgery and 79 receiving placebo), but there's no information on the number of infections on these patients. | |
| DOES NOT INCLUDE HERNIA PATHOLOGY. | |
| DOES NOT INCLUDE HERNIA PATHOLOGY. | |
| DOES NOT INCLUDE HERNIA PATHOLOGY. | |
| UNCONTROLLED TRIAL. Single arm of antibiotic prophylaxis with vancomicine on patients with incisional hernia or inguinal hernia repair with prosthesic material. Infection rate: 1/40 patients (2,5%). | |
| DOES NOT INCLUDE HERNIA PATHOLOGY. | |
| BOTH STUDY ARMS RECEIVED PROPHYLAXIS. Both groups received prophylaxis with a systemic antibiotic. Intervention group, additionally, is administered a colagen sponge impregned with gentamicine. Infection rate: 6/284 patients on control group and 1/293 patients on prophylaxis group | |
| INCOMPLETE DATA. Study on clean surgical techniques, not possible to obtain data of patients with hernia repair. Prophylaxis is penicilline 2 to 12 hours prior to the surgery. | |
| NOT RANDOMISED. Study developed with the patients not included on the published 1990 trial. A total of 1221 patients with herniorraphy. Infection rate: 2/239 patients on prophylaxis, and 15/982 patients without prophylaxis (OR 0.54; IC95% 0,06‐2,07; p= 0.4). They recomment prophylaxis only for high risk patients. | |
| BOTH STUDY ARMS RECEIVED PROPHYLAXIS. Prospective randomised trial, well designed, administering a single dose of ampiciline 2 g IV at induction of anaesthesia in one arm and fortified procaine 1,2 megaunits/24 h IM daily for seven days starting about 3 h after surgery on the other arm. Infection rate: 0/123 patients on ampiciline and 8/106 patients on peniciline (OR = 0,05; IC 95% 0,0 ‐ 0,82). | |
| NOT RANDOMISED. Non homogeneous groups: control group with majority of patients on local anaesthesia, prophylaxis group with majority of patients on general anaesthesia. Children are included on the trial. Control group is sequential in time to the intervention group. Each group is intervened in a different hospital. Infection rate: 82/5335 patients in control grop, 2/1183 patients in peniciline gropu. (OR 0.11; IC95% 0.03‐0.44) | |
| BOTH STUDY ARMS RECEIVED PROPHYLAXIS. Study of several surgical techniques to evaluate the efficacy of a new antibiotic in front of an already stablished one. A total of 128 patients, 5 of whom had hernia repair. | |
| UNCONTROLLED TRIAL. Single arm of 100 patients receiving antibiotic prophylaxis and prosthetic material. | |
| BOTH STUDY ARMS RECEIVED PROPHYLAXIS. | |
| NOT RANDOMISED. Technical review using different types of antibiotics, both intravenous and topical. | |
| MISBALANCES IN TREATMENT BETWEEN GROUPS: Patients with hernioplasty received prophylaxis while patients with herniorraphy received placebo . Patients infected: 2/141 patients on prophylaxis and 9 /137 patients on placebo. They recommend antibiotic prophylaxis to all patients. | |
| RETROSPECTIVE SERIE. Serie of 1076 patients followed for 6 years. Administers local anaesthesia and prosthetic material (Lichtentein and Gilbert), without antibiotic prophylaxis. One single patient with infection (0,09%). | |
| DOES NOT INCLUDE HERNIA PATHOLOGY. |
Data and analyses
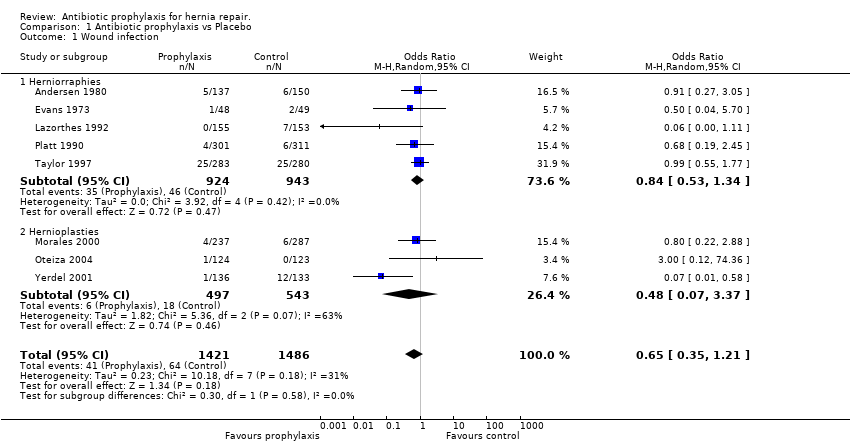
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Wound infection Show forest plot | 8 | 2907 | Odds Ratio (M‐H, Random, 95% CI) | 0.65 [0.35, 1.21] |
| Analysis 1.1  Comparison 1 Antibiotic prophylaxis vs Placebo, Outcome 1 Wound infection. | ||||
| 1.1 Herniorraphies | 5 | 1867 | Odds Ratio (M‐H, Random, 95% CI) | 0.84 [0.53, 1.34] |
| 1.2 Hernioplasties | 3 | 1040 | Odds Ratio (M‐H, Random, 95% CI) | 0.48 [0.07, 3.37] |
Comparison 1 Antibiotic prophylaxis vs Placebo, Outcome 1 Wound infection.
| Parameter | Score | ANDERSEN | EVANS | LAZORTHES | PLATT | TAYLOR | MORALES | YERDEL | OTEIZA |
| (A) Random allocation | 1 = explained 0 = not explained | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| (B) Blinded study | 1 = yes 0 = no | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 |
| (C) Groups of patients are homogeneous | 1 = comparable in technique used, age, sex and comorbid factors 0,5 = one factor differs significantly 0 = more than one factor differs significantly or comparability not specified | 0.5 | 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| (D) Statistical method adequate | 1 = yes 0 = no | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 |
| (E) Incisional surgical site infection was definied | 1 = yes 0 = no | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| (F) Number of antibiotics | 1 = uses only one antibiotic 0,5 = uses more than one antibiotic | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| (G) Outcome assesment | 1 = by personel no related to study 0,5 = by study personel 0 = not specified | 0 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 1 | 0.5 |
| (H) Route of administration | 1 = especified 0 = not especified | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| (I) Number of doses | 1 = especified 0= not especified | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| (J) Timing of administration | 1 = especified 0 = not especified | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| SCORE (%) | 7,5 (75%) | 6,5 (65%) | 5,5 (55%) | 9,5 (95%) | 10 (100%) | 9,5 (95%) | 10 (100%) | 8,5 (85%) |
| AUTHOR/YEAR | PROPHYLAXIS n/N (%) | CONTROL n/N (%) | OR (95% CI Random) |
| Andersen 1980 | 5/137 (3,6%) | 6/150 (4%) | 0.91 (0.27,3.05) |
| Escartín 1999 | 0/14 (0%) | 13/184 (7%) | 0.44 (0.02,7.75) |
| Evans 1973 | 1/48 (2%) | 2/49 (4%) | 0.50 (0.04,5.70) |
| Lazorthes 1992 | 0/155 (0%) | 7/153 (4,5%) | 0.06 (0.00,1.11) |
| Platt 1990 | 4/301 (1,3%) | 6/311 (1,9%) | 0.68 (0.19,2.45) |
| Platt 1992 | 2/239 (0,8%) | 15/982 (1,5%) | 0.54 (0.12,2.40) |
| Reggiori 1996 | 0/123 (0%) | 8/106 (7,5%) | 0.05 (0.00,0.82) |
| Ryan 1967 | 2/1183 (0,1%) | 82/5335 (1,5%) | 0.11(0.03,0.44) |
| Taylor 1997 | 25/283 (8,8%) | 25/280 (8,9%) | 0.99 (0.55,1.77) |
| SUBTOTAL HERNIORRAPHIES (heterogeneity chi‐square=16.93 df=8 p=0.031) | 39/2483 (1,5%) | 164/7550 (2,1%) | 0.34 (0.20,0.91) |
| Barreca 2000 | 0/63 (0%) | 0/84 (0%) | Not Estimable |
| Escartín 1999 | 3/144 (2%) | 10/133 (7,5%) | 0.26 (0.07,0.97) |
| Gilbert 1993 | 10/1150 (0,8%) | 4/684 (0,6%) | 1.49 (0.47,4.77) |
| Morales 2000 | 4/237 (1,6%) | 6/287 (2,1%) | 0.80 (0.22,2.88) |
| Musella 2001 | 1/293 (0,3%) | 6/284 (2,1%) | 0.16(0.02,1.33) |
| Vara 1993 | 2/141 (1,4%) | 9/137 (6,5%) | 0.20 (0.04,0.97) |
| Yerdel 2001 | 1/136 (0,7%) | 12/133 (9%) | 0.07 (0.01,0.58) |
| Otaiza 2004 | 1/124 (0,8%) | 0/123 (0%) | Not Estimable |
| SUBTOTAL HERNIOPLASTIES (heterogeneity chi‐square=10.61 df=5 p=0.06) | 22/2288 (0,9%) | 47/1865 (2,5%) | 0.37 (0.15,0.90) |
| T O T A L (heterogeneity chi‐square=28.21 df=14 p=0.013) | 61/4771 (1,3%) | 211/9415 (2,2%) | 0.41 (0.24,0.71) |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Wound infection Show forest plot | 8 | 2907 | Odds Ratio (M‐H, Random, 95% CI) | 0.65 [0.35, 1.21] |
| 1.1 Herniorraphies | 5 | 1867 | Odds Ratio (M‐H, Random, 95% CI) | 0.84 [0.53, 1.34] |
| 1.2 Hernioplasties | 3 | 1040 | Odds Ratio (M‐H, Random, 95% CI) | 0.48 [0.07, 3.37] |

