Bisphosphonates for osteoporosis in people with cystic fibrosis
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised controlled trial, parallel design, trial duration 2 years. | |
| Participants | Single centre, university hospital, USA; Inclusion criteria:‐ CF, 1 to 12 months post‐lung transplantation, ambulatory; N = 34 (16 in treatment group); 17 female (7 in treatment group). Groups similar in age, gender, baseline T‐scores, renal function, hospitalisation rates, immunosuppressant levels, change in lung function and body mass index over study period. 13 in treatment group and 12 controls had baseline T‐scores < ‐2.5 at a minimum of one site; all others ‐1 < T < ‐2.5 at a minimum of one site. | |
| Interventions | Intravenous pamidronate (30 mg every 3 months) for study duration of 2 years; All participants received oral vitamin D (800IU/day) and oral calcium (1g/day). | |
| Outcomes | Primary outcome: Secondary outcomes: | |
| Notes | 44 people with CF were eligible during the course of this study, 7 died immediately post‐operatively and were therefore not eligible for this trial. As outlined above, 3 people died during the course of the study before the first primary end point measurement. 34 people were included in the final analyses. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "Blocks of four" design stated (stratified on basis of gender and severity of osteoporosis using spine z‐score of ‐3.0), but actual method of randomisation is not discussed. |
| Allocation concealment? | Unclear risk | Not discussed. |
| Blinding? | High risk | Person(s) responsible for participants care and participants were not blinded. Of outcome assessors, only the radiologist who interpreted the DXA scans was blinded. |
| Incomplete outcome data addressed? | Unclear risk | It was described that 3 participants died during the course of the study before the first primary end point measurement. These participants were excluded from the final analysis of baseline characteristics and outcome data. However, it was not reported which treatment group they were in. |
| Free of selective reporting? | High risk | Serum and urine biochemical measurements that were measured at 2 days (only after first pamidronate infusion in intervention group) were not reported. |
| Methods | Randomised controlled trial; parallel design; double‐blind placebo‐controlled; trial duration 1 year for primary outcome measure (trial was intended to be 2 years duration). Generation of allocation sequence was stated ("blocks of four" design). Allocation concealment was unclear. Withdrawals ‐ before 6‐month DXA Withdrawals ‐ between 6 and 12 months Withdrawals between 1 and 2 years | |
| Participants | Single centre, adult CF centre, USA. Inclusion criteria: CF, ambulatory, DXA showed a spine or femur T‐score of ‐1 or less; 101 participants consented to be screened, 86 qualified and 53 started protocol and were randomised. N = 48 (24 in treatment group); 23 female (9 in treatment group). At baseline, osteoporosis was found in 3 participants and osteopenia was present in 20 participants in both the treatment and control group. | |
| Interventions | Oral alendronate (10mg daily); All participants received oral vitamin D (800IU/day) and oral calcium carbonate (1000mg/day). | |
| Outcomes | Primary outcome: Secondary outcomes: | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "Blocks of four" design stated, but actual method of randomisation is not discussed. |
| Allocation concealment? | Unclear risk | Not discussed. |
| Blinding? | Unclear risk | Described as "double‐blind". Clinicians or persons delivering treatment: unclear if clinicians involved in the study and clinicians managing the medical problems of the participants were all blinded. Participants: blinded. Outcome assessors: stated that the musculoskeletal radiologist who analysed baseline and end‐of‐study chest radiographs for fracture were blinded, not specifically stated that other outcome assessors were blinded. |
| Incomplete outcome data addressed? | Unclear risk | Described that protocol was originally designed to be 2 years in length, but few participants were willing to consent to such a lengthy study, so protocol was revised to measure the primary endpoint at 12 months. 5 withdrawals between commencement of protocol and 6‐month outcome measures were described, but not delineated whether they were in treatment or control group. 4 withdrawals from each group (between 6 months and 12 months outcome measures) were described. The primary end‐point measure was analysed in 40/53 (75%) participants, hence there is a risk of attrition bias. Stated that an intention‐to‐treat principle was used in the analyses of the treatment endpoints. |
| Free of selective reporting? | Low risk | Outcome measures that were described in the methods section were reported in the results section. |
| Methods | Randomised, double‐blinded, placebo‐controlled trial; parallel design. Trial duration 6 months (originally intended for 12 months). | |
| Participants | N = 40 planned for enrolment but only 5 enrolled (3 in treatment group) before study stopped by Data and Safety Monitoring Board (see notes). Inclusion criteria: CF; osteopenia of the lumbar spine (T‐scores ‐1.0 to ‐2.5); serum 25‐hydroxyvitamin D levels ≥ 20ng/ml prior to infusion. | |
| Interventions | Intravenous zoledronate, 5 mg infusion administered on a single occasion over 20 minutes. All participants received supplemental oral vitamin D (800 IU) and oral calcium (1000mg) daily. | |
| Outcomes | BMD (lumbar spine) ‐ 0, 6 months (originally planned additionally for 12 month). Change from baseline in serum C‐telopeptides at 3, 6 months (originally planned additionally for 9 and 12 months). | |
| Notes | The study was stopped by its Data and Safety Monitoring Board after 3 participants experienced dramatic musculoskeletal pain, 2 requiring emergency room assessment. Symptoms began 6 to 8 hours after infusion, peaked at 12 to 18 hours, and were characterized by severe chest and back pain. Along with musculoskeletal pain, one participant also experienced a fever of 104oF lasting for several hours and a rise in Tumour Necrosis Factor‐α. Although the most severe symptoms resolved within 48 to 72 hours, participants reported continued arthralgias for up to a week. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported. |
| Allocation concealment? | Unclear risk | Not discussed. |
| Blinding? | Unclear risk | Described as 'double‐blind'. Participants: blinded. Not discussed if clinicians or persons delivering treatment and outcome assessors were both blinded. |
| Incomplete outcome data addressed? | Low risk | Based on interpretation of data, we have presumed that the 3 participants who had severe bone pain were the 3 in the treatment group. Clarification from the author was requested but not received. |
| Free of selective reporting? | High risk | Abstract only but outcome measures were described in the results. |
| Free of other bias? | Unclear risk | Insufficient data in abstract to be clear. |
| Methods | Randomised, double‐blinded, placebo‐controlled trial; parallel design. Trial duration 24 months. | |
| Participants | Multientre, 2 sites, CF clinics, Australia. Inclusion criteria: CF (diagnosis previously made by sweat chloride test and an appropriate CF phenotype); ≥ 18 years; bone density T‐score <‐1.5 in at least one of three sites (hip (femoral neck), lumbar spine 2 to 4 (L2 to L4) and distal forearm) in the month before study commencement. Exclusion criteria: pre‐existing, symptomatic, fragility fractures; untreated hyperthyroidism, primary hyperparathyroidism or hypogonadism; bisphosphonate treatment in the three months before starting the study; serum calcium concentration below the lower limit of the laboratory normal range; serum creatinine concentration more than 1.5 times the upper limit of the laboratory normal range; serum ALT, ALP or bilirubin more than three times the upper limit of the laboratory normal range; on the waiting list for lung transplantation; pregnant or lactating; considered unlikely to complete the study. N=22 (10 in treatment group); 17 male (7 in treatment group), 5 females (3 in treatment group). Treatment group: mean (SD) age 30.1 (2.2) years; control group: mean (SD) age 28.6 (2.4) years. Age range over all: males 21 to 47 years, females 19 to 28 years. | |
| Interventions | Treatment group: intravenous zoledronic acid (zoledronate) in 100mls of normal saline infused over 15 minutes every 3 months for 21 months (eight infusions in total). For 5 out of 63 doses, 4mg zoledronate was administered, then dose reduced to 2mg for subsequent doses (due to febrile reactions to the higher dose in several participants). Placebo group: 100 mls normal saline as above. All participants were prescribed calcium carbonate 600 mg and vitamin D2 1000 IU each twice daily at least 3 days before the first treatment infusion and continued throughout the study. All participants were prescribed prednisolone 25 mg orally per day for 3 days starting on the morning of the first infusion; repeated with subsequent infusions if a reaction to the first infusion was thought likely. If there were side effects of the study infusion that were considered to be possibly due to the infusion during the first or any subsequent infusion, at the discretion of the investigator and participant, oral analgesia (paracetamol) was also administered for subsequent infusions. | |
| Outcomes | Bone density at hip (femoral neck), lumbar spine (L2‐L4) and distal forearm:‐ baseline, 6, 12 and 24 months. Plain x‐rays of thoracic and lumbar spine: baseline and 24 months (additional films taken as indicated to confirm any suspected fractures). Biochemical measurements (baseline and two weeks before the 6, 12, 18 and 24 months time‐points: urea; creatinine; ALP; ALT; bilirubin; calcium (corrected); calcium (ionised); phosphate; 25‐hydroxyvitamin D; PTH; complete blood count and differential. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not discussed. |
| Allocation concealment? | Unclear risk | Not discussed. |
| Blinding? | Unclear risk | Described as 'double‐blind'. Participants: blinded. Outcome assessors: DXA scans were performed and analysed by personnel blinded to treatment assignment. Not specifically discussed if clinicians or persons delivering treatment and other outcome assessors were all blinded. |
| Incomplete outcome data addressed? | Unclear risk | Withdrawals described. In the treatment group, 2 participants withdrew due to side‐effects, 1 due to psychiatric illness. In the placebo group, one participant was lost to follow‐up, one participant's BMD decreased to withdrawal threshold, 2 participants were poorly compliant to study protocols and in one participant, both of the latter two reasons were applicable. However, it was unclear which specific participants had BMD measurements available at each time‐point, particularly for forearm measures (fewer measurements compared with lumbar spine and femoral neck). |
| Free of selective reporting? | Low risk | Outcome measures that were described in the methods section were reported in the results section. |
| Methods | Randomised controlled trial; parallel design. Trial duration planned for 1 year, but was shortened to 6 months because of adverse events. Generation of allocation sequence and allocation concealment were unclear. Not stated if participants, providers or outcome assessors (or all) were blinded. 3 participants did not complete the study (1 participant in the treatment group received a double lung transplant and 1 participant in each group died of respiratory failure). | |
| Participants | Single centre, UK. Inclusion criteria: CF; no organ transplantation; 70% of all eligible participants in a longitudinal BMD study recruited after one year of follow‐up; no prior treatment with bone sparing agents; BMD Z‐score of < or = ‐2 at lumbar spine, proximal femur or distal forearm. N = 31 (15 in treatment group); 9 female (more in treatment group but exact number not reported). Mean (SD) age 26.1 (5.8) years; BMI 21.1 (2.7) kg/m2; FEV1 50.9 (20.3) % of predicted treatment. Groups similar with respect to age, initial BMD, bone biochemistry and respiratory disease severity. 3 participants (2 from treatment group) withdrew. | |
| Interventions | Intravenous pamidronate 30 mg every 3 months for 6 months (2 doses). All participants with pancreatic insufficiency (relevant to all except one in control group) continued long term oral vitamin D (900 IU/day); all participants in both groups received oral calcium (1g daily). | |
| Outcomes | BMD (lumbar spine; proximal femur (total hip); 0, 6 months; DXA Hologic QDR 4500 Waltham MA); | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not reported. |
| Allocation concealment? | Unclear risk | Not discussed. |
| Blinding? | Unclear risk | Not reported. |
| Incomplete outcome data addressed? | Low risk | Withdrawals were reported; one participant in each group died of respiratory failure and one participant in the treatment group underwent a double lung transplant. |
| Free of selective reporting? | Low risk | Outcome measures that were described in the methods section were reported in the results section. |
| Free of other bias? | Unclear risk | Given insufficient data, we are unclear of other bias. |
ALP: alkaline phosphatase
ALT: alanine aminotransferase
BMD: bone mineral density
BMI: body mass index
CF: cystic fibrosis
DXA: dual‐energy x‐ray absorptiometry
FEV1: forced expiratory volume in one second
PTH: parathyroid hormone
SD: standard deviation
SXA:single energy x‐ray absorptiometry
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| This study was a prospective open design, not a randomised controlled trial. | |
| This study assessed the effect of growth hormone on total‐body bone mineral content in pre‐pubertal children with CF. It did not assess the effect of bisphosphonates. |
CF: cystic fibrosis
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomized, placebo‐controlled trial. 6 Canadian CF specialty clinics. Computer‐ generated randomization code (stratified according to institution) prepared by an independent randomization center (McMaster In‐Patient Pharmacy; Hamilton, ON, Canada), and block allocation employed to ensure equitable distribution to each treatment group. The medication treatment arm was concealed, and all participants, central and local site coordinators, Participants who received at least 80% of the study drug were classified Stopping and study withdrawal rules were monitored by external Data Safety Monitoring Committee. A medical physicist, who was blinded to the study treatment arm and study status, reviewed all DXA scans. Radiographs were sent to the central methods center, and read independently by two radiologists who were |
| Participants | 56 adults randomised. Participants had CF confirmed by positive sweat test result or DNA acid analysis and a BMD T score of 1.0, as determined by dual‐energy radiograph absorptiometry. Participants who had undergone organ transplantation; had endoscopy‐proven oesophagitis, gastritis, and ulceration; had metabolic bone disorders; had severe renal disease; had used systemic corticosteroids (dose, 7.5 mg/d) or other drugs known to influence bone metabolism in the previous 6 months; or had osteomalacia and other documented contraindications were excluded from the study. Alendronate group: 27 randomised (17 male, 10 female) mean (SD) age 28.1 (7.7) years. 4 withdrew (2 non‐compliance, 1 due to adverse event, 1 withdrew consent). 23 completed study. Placebo group: 29 randomised (17 male, 12 female) mean (SD) age 30.9 (9.7) years. 5 withdrew (2 non‐compliance, 2 due to adverse event, 1 lost to follow‐up). 24 completed study. |
| Interventions | Placebo or oral alendronate, 70 mg once weekly for 12 months. Medication was taken while sitting upright and with water only on an empty stomach at least 30 min before first food or beverage of the day. In addition, |
| Outcomes | Compliance was measured through pill counts at each visit and patient self‐report during telephone contact. In‐clinic assessments at 6 and 12 months, and telephone follow‐up was conducted by study staff at months 3 and 9. Clinic assessments at baseline and 12 months included a physical examination, vital signs, biochemistry (serum and urine) tests, pulmonary Adverse events and drug reactions reported spontaneously and responses elicited at each contact. Safety analyses included all vertebral fractures, osteoporosis‐related fractures, adverse reactions, and abnormal findings that |
| Notes |
BMD: bone mineral density
CF: cystic fibrosis
DXA: dual‐energy radiograph absorptiometry
FEV1: forced expiratory volume at one second
FVC: forced vital capacity
SD: standard deviation
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Vertebral fractures Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 1 Vertebral fractures. | ||||
| 1.1 12 months | 2 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 24 months | 1 | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Non‐vertebral fractures Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 2 Non‐vertebral fractures. | ||||
| 2.1 12 months | 2 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.11 [0.18, 25.35] |
| 2.2 24 months | 1 | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Total Fractures Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 3 Total Fractures. | ||||
| 3.1 12 months | 2 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.11 [0.18, 25.35] |
| 3.2 24 months | 1 | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Percent change in BMD, lumbar spine, DXA (Time‐points) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 4 Percent change in BMD, lumbar spine, DXA (Time‐points). | ||||
| 4.1 6 months | 4 | 101 | Mean Difference (IV, Fixed, 95% CI) | 4.61 [3.90, 5.32] |
| 4.2 12 months | 2 | 59 | Mean Difference (IV, Fixed, 95% CI) | 6.38 [5.21, 7.54] |
| 4.3 24 months | 1 | 19 | Mean Difference (IV, Fixed, 95% CI) | 5.70 [4.55, 6.85] |
| 5 Percent change in BMD, lumbar spine, DXA (End of study) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 5 Percent change in BMD, lumbar spine, DXA (End of study). | ||||
| 5.1 End of study | 4 | 92 | Mean Difference (IV, Fixed, 95% CI) | 5.90 [4.94, 6.87] |
| 6 Percent change in BMD, total hip / femur, DXA (Time‐points) Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.6  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 6 Percent change in BMD, total hip / femur, DXA (Time‐points). | ||||
| 6.1 6 months | 3 | 96 | Mean Difference (IV, Random, 95% CI) | 3.35 [1.63, 5.07] |
| 6.2 12 months | 2 | 59 | Mean Difference (IV, Random, 95% CI) | 4.84 [2.73, 6.96] |
| 6.3 24 months | 1 | 19 | Mean Difference (IV, Random, 95% CI) | 6.73 [5.51, 7.95] |
| 7 Percent change in BMD, total hip/femur, DXA (End of study) Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 7 Percent change in BMD, total hip/femur, DXA (End of study). | ||||
| 7.1 End of study | 3 | 87 | Mean Difference (IV, Random, 95% CI) | 4.58 [1.92, 7.24] |
| 8 Percent change in BMD, distal radius, SXA (Time‐points) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.8  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 8 Percent change in BMD, distal radius, SXA (Time‐points). | ||||
| 8.1 6 months | 2 | 48 | Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐2.42, 1.45] |
| 8.2 12 months | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.30, 0.94] |
| 8.3 24 months | 1 | 14 | Mean Difference (IV, Random, 95% CI) | 1.5 [0.41, 2.59] |
| 9 Percent change in BMD, distal radius, SXA (End of study) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.9  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 9 Percent change in BMD, distal radius, SXA (End of study). | ||||
| 9.1 End of study | 2 | 42 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐3.12, 3.14] |
| 10 Percent change in BMD, ultradistal radius, SXA Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.10  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 10 Percent change in BMD, ultradistal radius, SXA. | ||||
| 10.1 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Bone pain Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.11  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 11 Bone pain. | ||||
| 11.1 Oral bisphosphonates | 1 | 48 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Intravenous bisphosphonates | 3 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 14.17 [3.64, 55.17] |
| 11.3 All routes of bisphosphonate administration | 4 | 108 | Odds Ratio (M‐H, Fixed, 95% CI) | 14.17 [3.64, 55.17] |
| 12 Fever Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.12  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 12 Fever. | ||||
| 12.1 Oral bisphosphonates | 1 | 48 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Intravenous bisphosphonates | 3 | 55 | Odds Ratio (M‐H, Fixed, 95% CI) | 12.64 [2.31, 69.11] |
| 12.3 All routes of bisphosphonate administration | 4 | 103 | Odds Ratio (M‐H, Fixed, 95% CI) | 12.64 [2.31, 69.11] |
| 13 Withdrawals, due to adverse events Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.13  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 13 Withdrawals, due to adverse events. | ||||
| 13.1 6 months | 2 | 53 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.95 [0.14, 108.09] |
| 13.2 12 months | 2 | 70 | Odds Ratio (M‐H, Fixed, 95% CI) | 7.35 [0.31, 173.13] |
| 13.3 24 months | 1 | 22 | Odds Ratio (M‐H, Fixed, 95% CI) | 7.35 [0.31, 173.13] |
| 14 Withdrawals, total Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.14  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 14 Withdrawals, total. | ||||
| 14.1 6 months | 2 | 53 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.83 [0.39, 20.73] |
| 14.2 12 months | 2 | 70 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.31, 3.73] |
| 14.3 24 months | 1 | 22 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.07, 2.50] |
| 15 Survival Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.15  Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 15 Survival. | ||||
| 15.1 6 months | 2 | 36 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.05, 16.39] |
| 15.2 12 months | 1 | 48 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.13 [0.12, 80.68] |
| 15.3 24 months | 1 | 22 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Vertebral fractures Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 1 Vertebral fractures. | ||||
| 1.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Non‐vertebral fractures Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 2 Non‐vertebral fractures. | ||||
| 2.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Total Fractures Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 3 Total Fractures. | ||||
| 3.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Percent change in BMD, lumbar spine, DXA Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.4  Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 4 Percent change in BMD, lumbar spine, DXA. | ||||
| 4.1 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Percent change in BMD, femur, DXA Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.5  Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 5 Percent change in BMD, femur, DXA. | ||||
| 5.1 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Bone pain Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.6  Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 6 Bone pain. | ||||
| 6.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Withdrawals, due to adverse events Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.7  Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 7 Withdrawals, due to adverse events. | ||||
| 8 Withdrawals, total Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.8  Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 8 Withdrawals, total. | ||||
| 8.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Survival Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.9  Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 9 Survival. | ||||
| 9.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
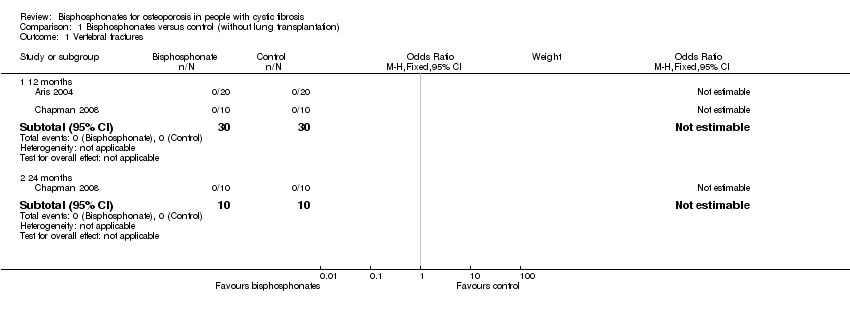
Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 1 Vertebral fractures.

Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 2 Non‐vertebral fractures.

Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 3 Total Fractures.
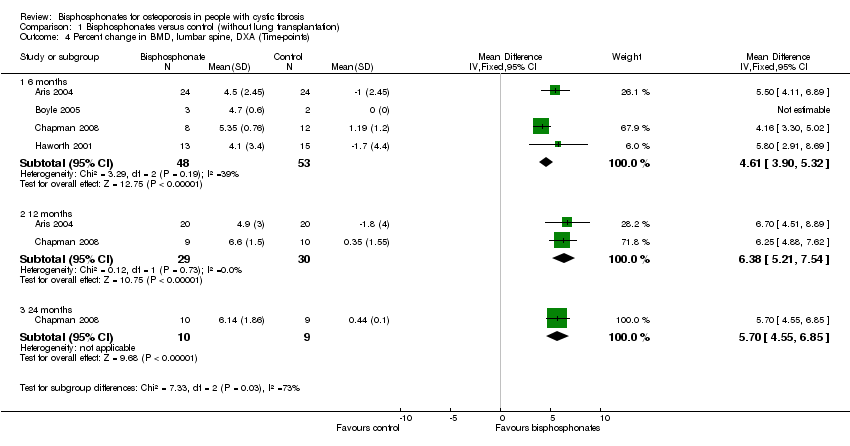
Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 4 Percent change in BMD, lumbar spine, DXA (Time‐points).
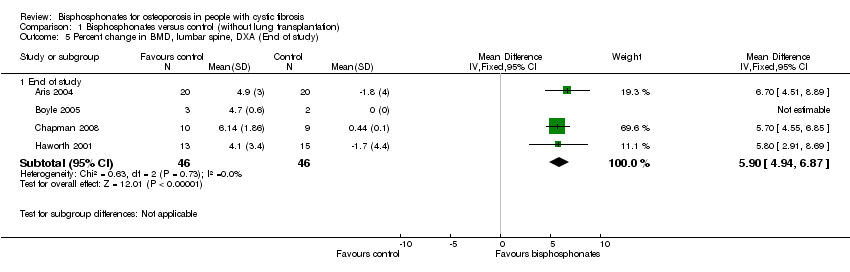
Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 5 Percent change in BMD, lumbar spine, DXA (End of study).

Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 6 Percent change in BMD, total hip / femur, DXA (Time‐points).

Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 7 Percent change in BMD, total hip/femur, DXA (End of study).
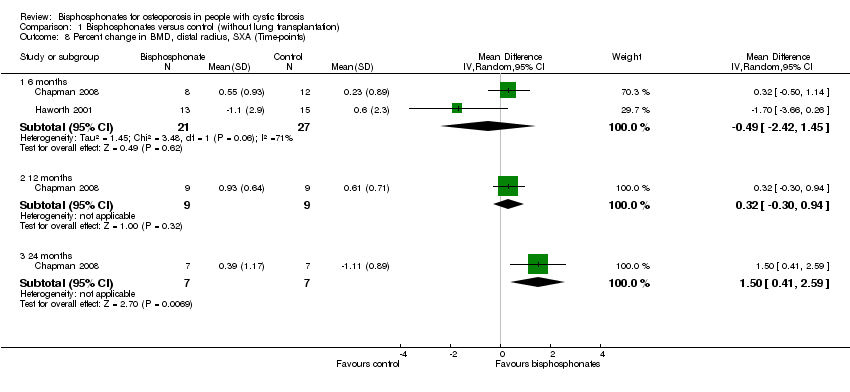
Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 8 Percent change in BMD, distal radius, SXA (Time‐points).

Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 9 Percent change in BMD, distal radius, SXA (End of study).
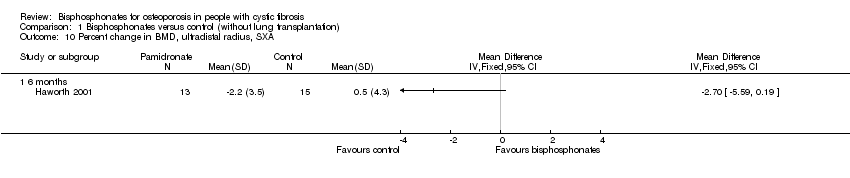
Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 10 Percent change in BMD, ultradistal radius, SXA.
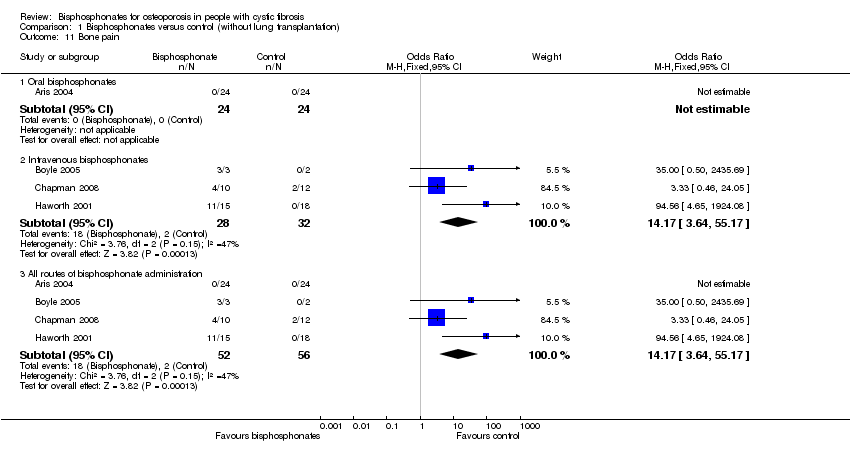
Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 11 Bone pain.
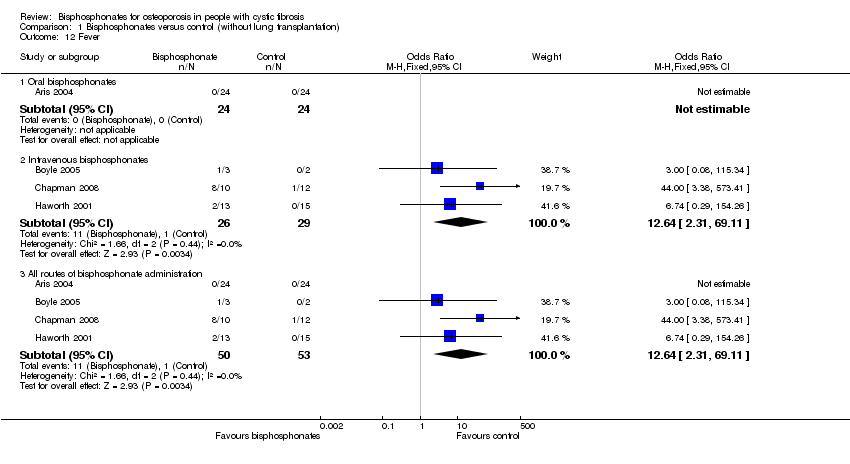
Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 12 Fever.

Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 13 Withdrawals, due to adverse events.

Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 14 Withdrawals, total.
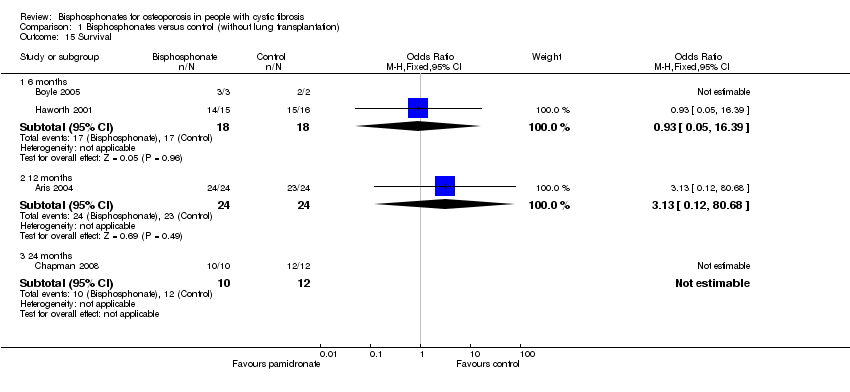
Comparison 1 Bisphosphonates versus control (without lung transplantation), Outcome 15 Survival.
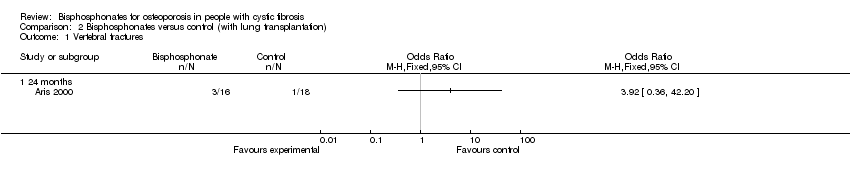
Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 1 Vertebral fractures.

Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 2 Non‐vertebral fractures.
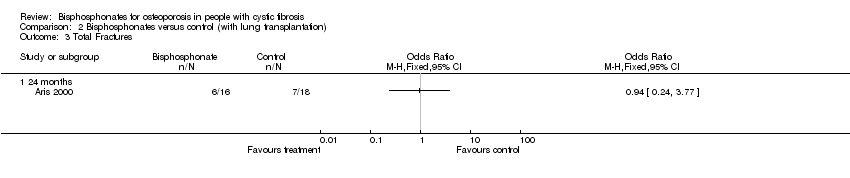
Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 3 Total Fractures.

Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 4 Percent change in BMD, lumbar spine, DXA.
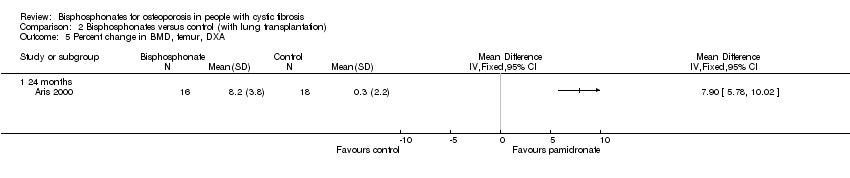
Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 5 Percent change in BMD, femur, DXA.

Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 6 Bone pain.
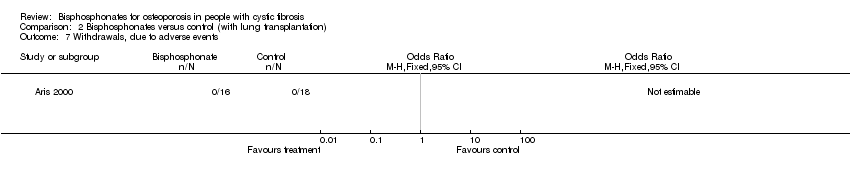
Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 7 Withdrawals, due to adverse events.

Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 8 Withdrawals, total.

Comparison 2 Bisphosphonates versus control (with lung transplantation), Outcome 9 Survival.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Vertebral fractures Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 12 months | 2 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 24 months | 1 | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Non‐vertebral fractures Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 12 months | 2 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.11 [0.18, 25.35] |
| 2.2 24 months | 1 | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Total Fractures Show forest plot | 2 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 12 months | 2 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.11 [0.18, 25.35] |
| 3.2 24 months | 1 | 20 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Percent change in BMD, lumbar spine, DXA (Time‐points) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 6 months | 4 | 101 | Mean Difference (IV, Fixed, 95% CI) | 4.61 [3.90, 5.32] |
| 4.2 12 months | 2 | 59 | Mean Difference (IV, Fixed, 95% CI) | 6.38 [5.21, 7.54] |
| 4.3 24 months | 1 | 19 | Mean Difference (IV, Fixed, 95% CI) | 5.70 [4.55, 6.85] |
| 5 Percent change in BMD, lumbar spine, DXA (End of study) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 End of study | 4 | 92 | Mean Difference (IV, Fixed, 95% CI) | 5.90 [4.94, 6.87] |
| 6 Percent change in BMD, total hip / femur, DXA (Time‐points) Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 6 months | 3 | 96 | Mean Difference (IV, Random, 95% CI) | 3.35 [1.63, 5.07] |
| 6.2 12 months | 2 | 59 | Mean Difference (IV, Random, 95% CI) | 4.84 [2.73, 6.96] |
| 6.3 24 months | 1 | 19 | Mean Difference (IV, Random, 95% CI) | 6.73 [5.51, 7.95] |
| 7 Percent change in BMD, total hip/femur, DXA (End of study) Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 End of study | 3 | 87 | Mean Difference (IV, Random, 95% CI) | 4.58 [1.92, 7.24] |
| 8 Percent change in BMD, distal radius, SXA (Time‐points) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 6 months | 2 | 48 | Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐2.42, 1.45] |
| 8.2 12 months | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.30, 0.94] |
| 8.3 24 months | 1 | 14 | Mean Difference (IV, Random, 95% CI) | 1.5 [0.41, 2.59] |
| 9 Percent change in BMD, distal radius, SXA (End of study) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 End of study | 2 | 42 | Mean Difference (IV, Random, 95% CI) | 0.01 [‐3.12, 3.14] |
| 10 Percent change in BMD, ultradistal radius, SXA Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Bone pain Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 Oral bisphosphonates | 1 | 48 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Intravenous bisphosphonates | 3 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 14.17 [3.64, 55.17] |
| 11.3 All routes of bisphosphonate administration | 4 | 108 | Odds Ratio (M‐H, Fixed, 95% CI) | 14.17 [3.64, 55.17] |
| 12 Fever Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Oral bisphosphonates | 1 | 48 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Intravenous bisphosphonates | 3 | 55 | Odds Ratio (M‐H, Fixed, 95% CI) | 12.64 [2.31, 69.11] |
| 12.3 All routes of bisphosphonate administration | 4 | 103 | Odds Ratio (M‐H, Fixed, 95% CI) | 12.64 [2.31, 69.11] |
| 13 Withdrawals, due to adverse events Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 6 months | 2 | 53 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.95 [0.14, 108.09] |
| 13.2 12 months | 2 | 70 | Odds Ratio (M‐H, Fixed, 95% CI) | 7.35 [0.31, 173.13] |
| 13.3 24 months | 1 | 22 | Odds Ratio (M‐H, Fixed, 95% CI) | 7.35 [0.31, 173.13] |
| 14 Withdrawals, total Show forest plot | 3 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 6 months | 2 | 53 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.83 [0.39, 20.73] |
| 14.2 12 months | 2 | 70 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.31, 3.73] |
| 14.3 24 months | 1 | 22 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.07, 2.50] |
| 15 Survival Show forest plot | 4 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 6 months | 2 | 36 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.05, 16.39] |
| 15.2 12 months | 1 | 48 | Odds Ratio (M‐H, Fixed, 95% CI) | 3.13 [0.12, 80.68] |
| 15.3 24 months | 1 | 22 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Vertebral fractures Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Non‐vertebral fractures Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Total Fractures Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Percent change in BMD, lumbar spine, DXA Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Percent change in BMD, femur, DXA Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 24 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Bone pain Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Withdrawals, due to adverse events Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8 Withdrawals, total Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Survival Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 24 months | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

