Medical day hospital care for the elderly versus alternative forms of care
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT (A) | |
| Participants | Patients referred to day hospital | |
| Interventions | Day hospital care by multidisciplinary rehabilitation team, principally nursing assessment, occupational therapy and physiotherapy | |
| Outcomes | 12 month follow up | |
| Notes | Total of 105 patients of whom 23 had a stroke diagnosis, 14 osteoarthritis, 13 fracture, 9 Parkinsonism | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT (B) | |
| Participants | Patients referred for inpatient rehabilitation | |
| Interventions | Day hospital attendance 5 days a week | |
| Outcomes | 3 month follow up | |
| Notes | A total 96 patients recruited of whom 55 had a stroke diagnosis, | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT (B) | |
| Participants | Patients referred from the community to 2 geriatricians or about to be discharged from hospital | |
| Interventions | Day hospital attendance 2 days a week | |
| Outcomes | 12 month follow up | |
| Notes | Total of 113 patients of whom 26 had a stroke diagnosis, 32 a diagnosis of depression and 19 a diagnosis of degenerative joint disease | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT (A) | |
| Participants | Patients discharged home from hospital after acute stroke | |
| Interventions | Domiciliary rehabilitation team (2 half time physiotherapists, 1 occupational therapist) | |
| Outcomes | 12 month follow up | |
| Notes | All stroke patients (155) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT (A) | |
| Participants | To be eligible for this Veterans Administration service patients had one of the following: at risk of nursing home placement, 'Service connected disability', hospital inpatient, in home care programme, in a VA domiciliary service | |
| Interventions | Adult day health care attendance | |
| Outcomes | 12 month follow up | |
| Notes | No accurate information on patient diagnosis given | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT (A) | |
| Participants | Patients admitted to a rehabilitation ward one week after acute stroke | |
| Interventions | Conventional inpatient rehabilitation by a neurology team with medical clinic follow up | |
| Outcomes | 6 month follow up | |
| Notes | Stroke patients only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT (C) | |
| Participants | Patients receiving home care in a rural community in Finland | |
| Interventions | Day hospital attendance | |
| Outcomes | 12 month follow up | |
| Notes | Total of 174 patients of whom 40 had a stroke diagnosis, 54 a diagnosis of coronary heart disease, 53 arthrosis, 33 'moderate' or 'severe' dementia | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
| Methods | RCT (A) | |
| Participants | Inclusion: Patients with newly diagnosed stroke admitted to a Poole Hospital NHS Trust hospital, or community referrals. | |
| Interventions | Day hospital: 5 day hospitals with coordinated care from multidisciplinary teams, both individual and group therapies In both cases therapy as provided until maximum potential for recovery reached, patients were then placed on review, and if no further therapy required, discharged. | |
| Outcomes | 6 month follow‐up: | |
| Notes | All stroke patients, previous stroke: DH 23 (32%), | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT (B) | |
| Participants | Patients over 55 years | |
| Interventions | Day hospital attendance | |
| Outcomes | 5 months follow up | |
| Notes | No information on number of patients screened for inclusion | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT (B) (pilot study) | |
| Participants | Consecutive patients attending 2 day hospitals were eligible for trial if: | |
| Interventions | Day hospital attendance | |
| Outcomes | 2 month follow up | |
| Notes | Total of 59 patients of whom 16 had a stroke diagnosis, 12 fractured neck of femur, 5 osteo‐arthritis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | RCT (B) | |
| Participants | New service established and advertised | |
| Interventions | Day care services | |
| Outcomes | 12 month follow up | |
| Notes | Little information on patient diagnosis (only circulatory disorders (225, 41% and injuries 55 (10%)) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT (B) | |
| Participants | Patients (n=331) from a consecutive series of 500 former geriatric unit inpatients (169 had died, left area, or not traced) | |
| Interventions | Day hospital attendance | |
| Outcomes | 12 month follow up | |
| Notes | No information on patient diagnosis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT (B) | |
| Participants | Patients discharged home from hospital after new stroke event. | |
| Interventions | Day hospital attendance | |
| Outcomes | 6 months follow up | |
| Notes | Stroke patients only (124) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Patients were randomised to treatment at home or to outpatient/day hospital attendance, patients attending day hospital not reported separately. | |
| Evaluation of adult day care rather than day hospital. | |
| Median age of patients was 53 years. | |
| Not an evaluation of a medical day hospital: patients attended a chronic care clinic for half‐day visits every 3‐4 months. | |
| Not a randomised controlled trial. | |
| Retrospective review of patients: not a randomised controlled trial. | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial. | |
| Observational study. | |
| Evaluated the effect of a chronic illness self‐managment programme delivered in a senior centre. All participants attended the senior centre. | |
| Prospective study: not a randomised controlled trial. | |
| Not a randomised controlled trial. | |
| Evaluation of different treatment approaches: all patient attended the day hospital. | |
| All patients were in receipt of day services and were then randomised to attend a water exercise program once or twice a week or to a social activity control group. | |
| Not day hospital intervention, Group meeting for 90 minutes once a month. | |
| Not a randomised or quasi‐randomised study. | |
| Day hospital arm confounded by other interventions. | |
| Evaluation of treatment for patients with Parkinsons disease. Intervention provided by a specialist multidisciplinary team to patients with Parkinsons disease in a day hospital setting. | |
| Not a randomised or quasi‐randomised study. | |
| Not a randomised controlled trial. | |
| Not a randomised controlled trial. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Post acute rehabilitation: A randomised controlled trial of day hospital and domiciliary care versus Rehabilitation in the Home for deconditioned patients following hospitalisation to improve functional and nutritional status |
| Methods | |
| Participants | Patients with: neurological injury, |
| Interventions | Group 1: Day hospital ‐ rehabilitation service provided in hospital 3‐5 times per week for a minimum of six weeks. |
| Outcomes | Primary outcome: Assessment of Motor and Process Skills, |
| Starting date | 20/07/05 |
| Contact information | Professor Maria Crotty |
| Notes | Recruitment completed |
| Trial name or title | Multifactorial day hospital intervention to reduce falls in high risk older people in primary care: a multi‐centre randomised controlled trial |
| Methods | |
| Participants | Inclusion: the study population will comprise men and women aged 70 and over identified as being at high risk of falling by a postal screening questionnaire, registered with the participating general practices in Nottinghamshire and Derbyshire. |
| Interventions | Intervention arm: screening questionnaire, information leaflet, leaflet on falls prevention and invitation to attend the day hospital for assessment and any subsequent intervention. Control arm: screening questionnaire, information leaflet, leaflet on falls prevention and usual care from primary care service until outcome data collected, then offer of day hospital intervention. |
| Outcomes | Primary outcome: The proportion of older people who fall over one year, identified in primary care as being at high risk of falling |
| Starting date | 01/09/2004 |
| Contact information | Professor Tahir. Masud, Department of Rehabilitation and the Clinical Gerontology Research Unit |
| Notes |
| Trial name or title | Rehabilitation of older patients: day hospital compared to rehabilitation at home |
| Methods | |
| Participants | All elderly patients receiving rehabilitation (multi‐disciplinary assessment and treatment) will be eligible for recruitment. Not more than a third of the total number of patients recruited in the pilot study will be from a single diagnostic category (such as movement disorder, stroke, fracture etc). Participants will be over 65. Elderly patients attending the day hospital but not receiving multi‐disciplinary assessment and rehabilitation will not be eligible for inclusion |
| Interventions | Intervention: medical day hospital care. Control group: rehabilitation at home. |
| Outcomes | Patients: Hospital anxiety and depression scale, Euro‐qol 5D, Nottingham Extended Activities of Daily Living, socio‐economic data, survival, Therapy outcome measures, views of treatment by qualitative interview. Carers: general health questionnaire, socio‐economic data, views of treatment. |
| Starting date | 01/09/2002 End date: 01/09/08 |
| Contact information | Dr Stuart Parker Telephone: 0114 271 4939 Fax: 0114 271 5771 E‐mail: [email protected] |
| Notes | http://www.ncchta.org/project/1218.asp http://www.controlled‐trials.com/ISRCTN71801032 https://portal.nihr.ac.uk/Profiles/NRR.aspx?Publication_ID=N0071140216 |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||||||||||||||||||
| 1 Death by the end of follow up Show forest plot | 13 | 2852 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.03 [0.84, 1.27] | ||||||||||||||||||||||||||||||||||||
| Analysis 1.1  Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 1 Death by the end of follow up. | ||||||||||||||||||||||||||||||||||||||||
| 1.1 Day Hospital vs Comprehensive elderly care | 5 | 1287 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.26 [0.93, 1.70] | ||||||||||||||||||||||||||||||||||||
| 1.2 Day hospital vs Domiciliary care | 5 | 583 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.86 [0.52, 1.42] | ||||||||||||||||||||||||||||||||||||
| 1.3 Day hospital vs No comprehensive elderly care | 3 | 982 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.86 [0.60, 1.22] | ||||||||||||||||||||||||||||||||||||
| 2 Death or institutional care by the end of follow up Show forest plot | 11 | 2438 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.81 [0.68, 0.97] | ||||||||||||||||||||||||||||||||||||
| Analysis 1.2  Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 2 Death or institutional care by the end of follow up. | ||||||||||||||||||||||||||||||||||||||||
| 2.1 Day hospital vs Comprehensive elderly care | 4 | 1181 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.04 [0.82, 1.33] | ||||||||||||||||||||||||||||||||||||
| 2.2 Day hospital vs Domiciliary care | 4 | 443 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.87 [0.54, 1.40] | ||||||||||||||||||||||||||||||||||||
| 2.3 Day hospital vs No comprehensive elderly care | 3 | 814 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.52 [0.38, 0.71] | ||||||||||||||||||||||||||||||||||||
| 3 Death or deterioration in activities of daily living (ADL) Show forest plot | 7 | 1268 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.98 [0.78, 1.23] | ||||||||||||||||||||||||||||||||||||
| Analysis 1.3  Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 3 Death or deterioration in activities of daily living (ADL). | ||||||||||||||||||||||||||||||||||||||||
| 3.1 Day hospital vs Comprehensive elderly care | 1 | 174 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.17 [0.64, 2.17] | ||||||||||||||||||||||||||||||||||||
| 3.2 Day hospital vs Domiciliary care | 4 | 443 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.34 [0.90, 1.99] | ||||||||||||||||||||||||||||||||||||
| 3.3 Day hospital vs No comprehensive elderly care | 2 | 651 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.76 [0.56, 1.05] | ||||||||||||||||||||||||||||||||||||
| 4 Death or Poor Outcome (institutional care, disability or deterioration) Show forest plot | 13 | 2831 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.93 [0.79, 1.09] | ||||||||||||||||||||||||||||||||||||
| Analysis 1.4  Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 4 Death or Poor Outcome (institutional care, disability or deterioration). | ||||||||||||||||||||||||||||||||||||||||
| 4.1 Day hospital vs Comprehensive elderly care | 5 | 1268 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.06 [0.84, 1.34] | ||||||||||||||||||||||||||||||||||||
| 4.2 Day hospital vs Domiciliary care | 5 | 581 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.03 [0.72, 1.49] | ||||||||||||||||||||||||||||||||||||
| 4.3 Day hospital vs No comprehensive elderly care | 3 | 982 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.73 [0.55, 0.96] | ||||||||||||||||||||||||||||||||||||
| 5 Deterioration in activities of daily living (ADL) in survivors Show forest plot | 7 | 905 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.99 [0.73, 1.34] | ||||||||||||||||||||||||||||||||||||
| Analysis 1.5  Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 5 Deterioration in activities of daily living (ADL) in survivors. | ||||||||||||||||||||||||||||||||||||||||
| 5.1 Day hospital vs Comprehensive elderly care | 1 | 149 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.21 [0.58, 2.50] | ||||||||||||||||||||||||||||||||||||
| 5.2 Day hospital vs Domiciliary care | 4 | 349 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.51 [0.94, 2.44] | ||||||||||||||||||||||||||||||||||||
| 5.3 Day hospital vs No comprehensive elderly care | 2 | 407 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.60 [0.38, 0.96] | ||||||||||||||||||||||||||||||||||||
| 6 Activities of daily living (ADL) scores Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| Analysis 1.6
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 6 Activities of daily living (ADL) scores. | ||||||||||||||||||||||||||||||||||||||||
| 6.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 6.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 6.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 7 Subjective health status Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| Analysis 1.7
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 7 Subjective health status. | ||||||||||||||||||||||||||||||||||||||||
| 7.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 7.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 7.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 8 Patient satisfaction Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| Analysis 1.8
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 8 Patient satisfaction. | ||||||||||||||||||||||||||||||||||||||||
| 8.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 8.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 8.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 9 Carer Distress Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| Analysis 1.9
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 9 Carer Distress. | ||||||||||||||||||||||||||||||||||||||||
| 9.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 9.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| 9.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||||||||||||||||||||
| 1 Requiring institutional care at the end of follow up Show forest plot | 11 | 2438 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.80 [0.64, 0.99] | ||||||||||||||||||||||||||||||||||||||
| Analysis 2.1  Comparison 2 Day Hospital vs Alternative Care ‐ Resource outcomes, Outcome 1 Requiring institutional care at the end of follow up. | ||||||||||||||||||||||||||||||||||||||||||
| 1.1 Day hospital vs Comprehensive elderly care | 4 | 1181 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.91 [0.70, 1.19] | ||||||||||||||||||||||||||||||||||||||
| 1.2 Day hospital vs Domiciliary care | 4 | 443 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.13 [0.58, 2.23] | ||||||||||||||||||||||||||||||||||||||
| 1.3 Day hospital vs No comprehensive elderly care | 3 | 814 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.50 [0.33, 0.77] | ||||||||||||||||||||||||||||||||||||||
| 2 Hospital bed use during follow up Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||
| Analysis 2.2
Comparison 2 Day Hospital vs Alternative Care ‐ Resource outcomes, Outcome 2 Hospital bed use during follow up. | ||||||||||||||||||||||||||||||||||||||||||
| 2.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||
| 2.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||
| 2.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||
| 3 Resource use Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||
| Analysis 2.3
Comparison 2 Day Hospital vs Alternative Care ‐ Resource outcomes, Outcome 3 Resource use. | ||||||||||||||||||||||||||||||||||||||||||
| 3.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||
| 3.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||
| 3.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||
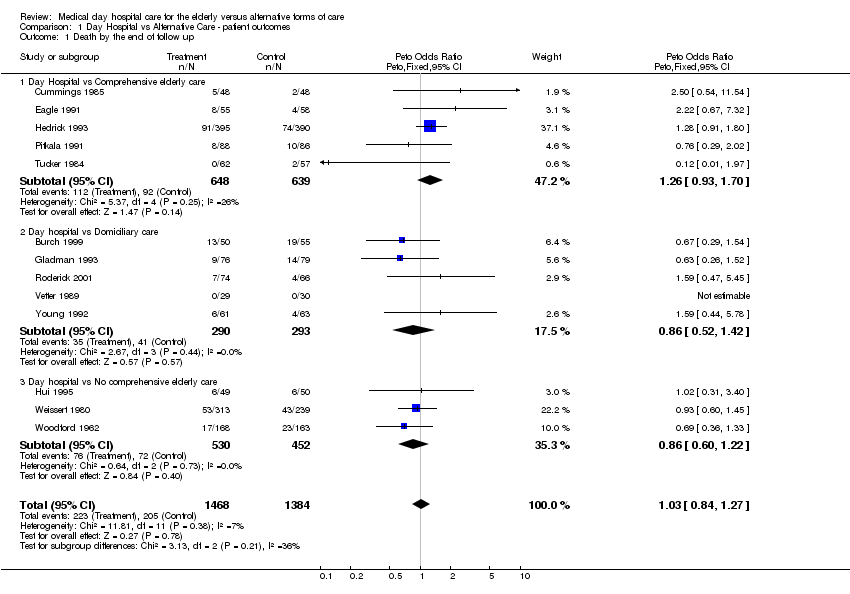
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 1 Death by the end of follow up.
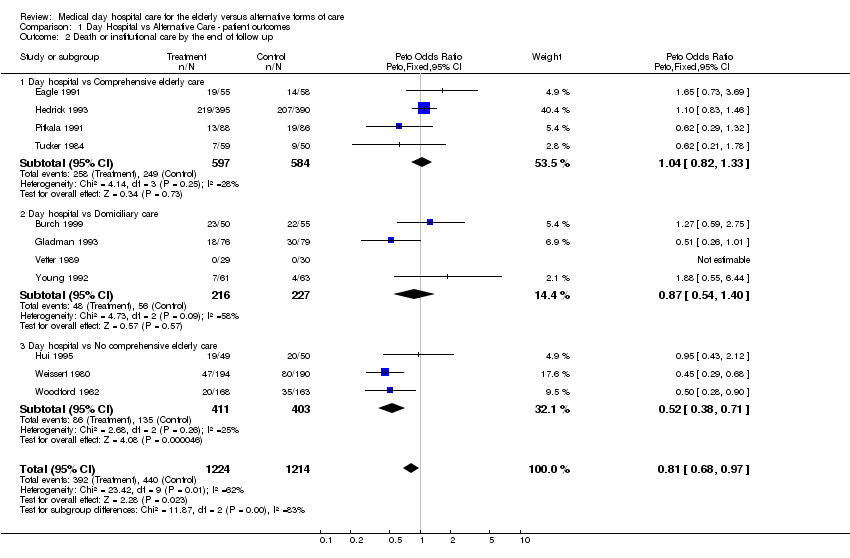
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 2 Death or institutional care by the end of follow up.

Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 3 Death or deterioration in activities of daily living (ADL).
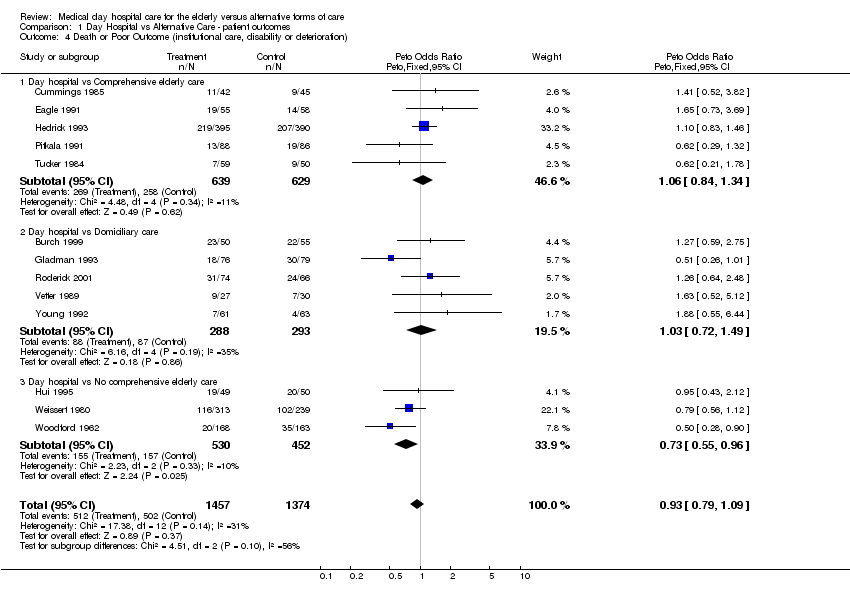
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 4 Death or Poor Outcome (institutional care, disability or deterioration).

Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 5 Deterioration in activities of daily living (ADL) in survivors.
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | No significant difference in the Kenny ADL score ‐ |
| Eagle 1991 | No significant difference in the Geriatric Quality of Life Questionnaire ADL score ‐ |
| Hedrick 1993 | No significant in the physical dimension of the Sickness Impact Profile (NB high score indicates increased disability) ‐ |
| Pitkala 1991 | No data in this form |
| Tucker 1984 | No significant difference in the mean change in Northwick Park ADL score from baseline (NB high score indicates increased disability) : |
| Day hospital vs Domiciliary care | |
| Burch 1999 | No significant difference in Barthel index ‐ |
| Gladman 1993 | No significant difference in median Barthel index ‐ |
| Roderick 2001 | Significant improvement in Barthel score in both groups. |
| Vetter 1989 | No significant difference in mean Barthel index ‐ |
| Young 1992 | Significantly (P=0.01) lower Barthel ADL score ‐ |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | No significant difference in mean Barthel index ‐ |
| Weissert 1980 | No comparable data |
| Woodford 1962 | No comparable data |
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 6 Activities of daily living (ADL) scores.
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | No significant difference in the modified Dupay assessment ‐ |
| Eagle 1991 | No significant difference in the General Health Questionnaire ‐ |
| Hedrick 1993 | No significant difference in the Sickness Impact Profile ‐ |
| Pitkala 1991 | No comparable data |
| Tucker 1984 | No significant difference in the change in Zung index between baseline and end of follow up ‐ |
| Day hospital vs Domiciliary care | |
| Burch 1999 | No significant difference in the change in the Philidelphia Geriatric Morale scale during follow up ‐ |
| Gladman 1993 | No significant difference in the number of patients with distress (Nottingham Health Profile >30) ‐ |
| Roderick 2001 | No between groups significant difference for SF‐36 physical or mental health scales. |
| Vetter 1989 | No significant difference in the Sickness Impact Profile |
| Young 1992 | No significant difference in the number of patients with distress (Nottingham Health Profile >30) ‐ |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | No significant difference in the Geriatric Depression Scale |
| Weissert 1980 | No comparable data |
| Woodford 1962 | No comparable data |
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 7 Subjective health status.
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | No available data |
| Eagle 1991 | No available data |
| Hedrick 1993 | No comparable data |
| Pitkala 1991 | No comparable data |
| Tucker 1984 | No available data |
| Day hospital vs Domiciliary care | |
| Burch 1999 | No available data |
| Gladman 1993 | No available data |
| Roderick 2001 | No available data |
| Vetter 1989 | No available data |
| Young 1992 | No available data |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | No significant difference in the level of satisfaction |
| Weissert 1980 | No available data |
| Woodford 1962 | No available data |
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 8 Patient satisfaction.
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | No comparable data |
| Eagle 1991 | No available data |
| Hedrick 1993 | No comparable data |
| Pitkala 1991 | No comparable data |
| Tucker 1984 | No data available |
| Day hospital vs Domiciliary care | |
| Burch 1999 | No significant difference in the mean change in Caregiver Strain Index between baseline and 3 months ‐ |
| Gladman 1993 | No significant difference at 6 months in the median Life Satisfaction Index ‐ |
| Roderick 2001 | No available data |
| Vetter 1989 | No data available |
| Young 1992 | Proportion of carers showing distress (General Health Questionnaire 28 score > 5) ‐ |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | No available data |
| Weissert 1980 | No available data |
| Woodford 1962 | No available data |
Comparison 1 Day Hospital vs Alternative Care ‐ patient outcomes, Outcome 9 Carer Distress.

Comparison 2 Day Hospital vs Alternative Care ‐ Resource outcomes, Outcome 1 Requiring institutional care at the end of follow up.
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | Day hospital: 206 bed days for 48 patients (4.3 days per patient) |
| Eagle 1991 | Day hospital: 1388 bed days for 55 patients (25.2 days per patient) |
| Hedrick 1993 | Day hospital: 8020 bed days for 411 patients (19.5 days per patient) |
| Pitkala 1991 | Day hospital: 3538 bed days for 88 patients (40.2 days per patient) |
| Tucker 1984 | Day hospital: 472 bed days for 62 patients (7.6 days per patient) |
| Vetter 1989 | No comparable data |
| Day hospital vs Domiciliary care | |
| Burch 1999 | Day hospital: 923 bed days for 50 patients (18.5 per patient) |
| Gladman 1993 | Day hospital: 436 bed days for 76 patients (5.7 days per patient) |
| Roderick 2001 | Day hospital: 296 bed days for 74 patients ( 4 days per patient) |
| Vetter 1989 | No bed days used in either group |
| Young 1992 | Day hospital: 311 bed days for 61 patients (5.1 days per patient) |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | Day hospital: 81 bed days for 59 patients (1.4 days per patient) |
| Weissert 1980 | Day hospital: 3443 bed days for 313 patients (11.0 days per patient) |
| Woodford 1962 | Day hospital: 2534 bed days for 168 patients (15.1 days per patient) |
Comparison 2 Day Hospital vs Alternative Care ‐ Resource outcomes, Outcome 2 Hospital bed use during follow up.
| Study | |
| Day hospital vs Comprehensive elderly care | |
| Cummings 1985 | Average treatment cost per patient to 3 months post discharge ‐ |
| Eagle 1991 | No cost data |
| Hedrick 1993 | Mean total costs over 12 months ‐ |
| Pitkala 1991 | No costing data |
| Tucker 1984 | Average cost for 5 months care ‐ |
| Day hospital vs Domiciliary care | |
| Burch 1999 | Total annual cost per attendance ‐ |
| Gladman 1993 | Mean total health service cost per patient ‐ |
| Roderick 2001 | Median costs per patient: Rehabilitation costs: Day hospital:£1090 (IQR 513‐1475), |
| Vetter 1989 | No cost data |
| Young 1992 | Mean total costs for 8 weeks treatment ‐ |
| Day hospital vs No comprehensive elderly care | |
| Hui 1995 | Mean cost of treatment to the health service over 6 months ‐ |
| Weissert 1980 | Average cost for 1 year ‐ |
| Woodford 1962 | No formal costing |
Comparison 2 Day Hospital vs Alternative Care ‐ Resource outcomes, Outcome 3 Resource use.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death by the end of follow up Show forest plot | 13 | 2852 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.03 [0.84, 1.27] |
| 1.1 Day Hospital vs Comprehensive elderly care | 5 | 1287 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.26 [0.93, 1.70] |
| 1.2 Day hospital vs Domiciliary care | 5 | 583 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.86 [0.52, 1.42] |
| 1.3 Day hospital vs No comprehensive elderly care | 3 | 982 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.86 [0.60, 1.22] |
| 2 Death or institutional care by the end of follow up Show forest plot | 11 | 2438 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.81 [0.68, 0.97] |
| 2.1 Day hospital vs Comprehensive elderly care | 4 | 1181 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.04 [0.82, 1.33] |
| 2.2 Day hospital vs Domiciliary care | 4 | 443 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.87 [0.54, 1.40] |
| 2.3 Day hospital vs No comprehensive elderly care | 3 | 814 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.52 [0.38, 0.71] |
| 3 Death or deterioration in activities of daily living (ADL) Show forest plot | 7 | 1268 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.98 [0.78, 1.23] |
| 3.1 Day hospital vs Comprehensive elderly care | 1 | 174 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.17 [0.64, 2.17] |
| 3.2 Day hospital vs Domiciliary care | 4 | 443 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.34 [0.90, 1.99] |
| 3.3 Day hospital vs No comprehensive elderly care | 2 | 651 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.76 [0.56, 1.05] |
| 4 Death or Poor Outcome (institutional care, disability or deterioration) Show forest plot | 13 | 2831 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.93 [0.79, 1.09] |
| 4.1 Day hospital vs Comprehensive elderly care | 5 | 1268 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.06 [0.84, 1.34] |
| 4.2 Day hospital vs Domiciliary care | 5 | 581 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.03 [0.72, 1.49] |
| 4.3 Day hospital vs No comprehensive elderly care | 3 | 982 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.73 [0.55, 0.96] |
| 5 Deterioration in activities of daily living (ADL) in survivors Show forest plot | 7 | 905 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.99 [0.73, 1.34] |
| 5.1 Day hospital vs Comprehensive elderly care | 1 | 149 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.21 [0.58, 2.50] |
| 5.2 Day hospital vs Domiciliary care | 4 | 349 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.51 [0.94, 2.44] |
| 5.3 Day hospital vs No comprehensive elderly care | 2 | 407 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.60 [0.38, 0.96] |
| 6 Activities of daily living (ADL) scores Show forest plot | Other data | No numeric data | ||
| 6.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 6.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 6.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||
| 7 Subjective health status Show forest plot | Other data | No numeric data | ||
| 7.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 7.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 7.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||
| 8 Patient satisfaction Show forest plot | Other data | No numeric data | ||
| 8.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 8.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 8.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||
| 9 Carer Distress Show forest plot | Other data | No numeric data | ||
| 9.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 9.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 9.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Requiring institutional care at the end of follow up Show forest plot | 11 | 2438 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.80 [0.64, 0.99] |
| 1.1 Day hospital vs Comprehensive elderly care | 4 | 1181 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.91 [0.70, 1.19] |
| 1.2 Day hospital vs Domiciliary care | 4 | 443 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.13 [0.58, 2.23] |
| 1.3 Day hospital vs No comprehensive elderly care | 3 | 814 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.50 [0.33, 0.77] |
| 2 Hospital bed use during follow up Show forest plot | Other data | No numeric data | ||
| 2.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 2.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 2.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||
| 3 Resource use Show forest plot | Other data | No numeric data | ||
| 3.1 Day hospital vs Comprehensive elderly care | Other data | No numeric data | ||
| 3.2 Day hospital vs Domiciliary care | Other data | No numeric data | ||
| 3.3 Day hospital vs No comprehensive elderly care | Other data | No numeric data | ||

