Reducción o interrupción de los antipsicóticos y antipsicóticos como tratamientos específicos para la discinesia tardía
Resumen
Antecedentes
Desde los años cincuenta, la medicación antipsicótica se ha usado ampliamente para tratar a las personas con enfermedades mentales crónicas, como la esquizofrenia. Estos fármacos, sin embargo, también se han asociado con una gama amplia de efectos adversos, incluidos los trastornos del movimiento como la discinesia tardía (DT) – un problema que a menudo se observa como movimientos involuntarios repetitivos cerca de la boca y la cara. Se han examinado diversas estrategias para reducir la exposición acumulativa de los pacientes a los antipsicóticos. Estas estrategias incluyen reducción de dosis, estrategias de dosificación intermitente, como días de descanso del fármaco e interrupción del antipsicótico.
Objetivos
Determinar si una reducción o interrupción de los fármacos antipsicóticos se asocia con una reducción de la DT para los pacientes con esquizofrenia (u otras enfermedades mentales crónicas) con DT. Un objetivo secundario fue determinar si el uso de antipsicóticos específicos para grupos similares de pacientes podía ser un tratamiento para la DT establecida.
Métodos de búsqueda
Se actualizaron las búsquedas anteriores en el registro de ensayos basado en estudios del Grupo Cochrane de Esquizofrenia (Cochrane Schizophrenia's study‐based Register of Trials), incluidos los registros de ensayos clínicos (16 de julio de 2015 y 26 de abril de 2017). Se realizaron búsquedas de referencias de todos los estudios identificados para obtener citas de ensayos adicionales. También se estableció contacto con los autores de los ensayos para obtener información adicional.
Criterios de selección
Se incluyeron informes cuando evaluaban a los pacientes con esquizofrenia u otras enfermedades mentales crónicas que presentaban DT inducida por antipsicóticos establecida, y habían sido asignados al azar a (a) el mantenimiento de los antipsicóticos versus interrupción de los antipsicóticos (placebo o ninguna intervención), (b) el mantenimiento de los antipsicóticos versus reducción de los antipsicóticos (incluidas las estrategias intermitentes), (c) antipsicóticos específicos para el tratamiento de la DT versus placebo o ninguna intervención, y (d) antipsicóticos específicos versus otros antipsicóticos o versus otros fármacos para el tratamiento de la DT.
Obtención y análisis de los datos
Se extrajeron los datos de estos ensayos de forma independiente y se calcularon los riesgos relativos (RR) o las diferencias de medias (DM), con intervalos de confianza (IC) del 95%. Los autores de la revisión supusieron que los pacientes que abandonaron no presentaron mejoría.
Resultados principales
Se incluyeron 13 ECAs con 711 participantes; ocho de estos estudios fueron incluidos recientemente en esta actualización de 2017. Un ensayo está en curso.
Hubo evidencia de baja calidad de una diferencia clara en ninguna mejoría clínicamente importante en la DT a favor del cambio a la risperidona en comparación con la interrupción de los antipsicóticos (con placebo) (un ECA, 42 pacientes, RR 0,45; IC 0,23 a 0,89; evidencia de baja calidad). Debido a que la evidencia fue de muy baja calidad para la reducción de la dosis de antipsicóticos versus mantenimiento de los antipsicóticos (dos ECA, 17 pacientes, RR 0,42; IC del 95%: 0,17 a 1,04; evidencia de muy baja calidad), y para el cambio a un nuevo antipsicótico versus cambio a otro antipsicótico nuevo (cinco comparaciones, cinco ECA, 140 pacientes, ningún metanálisis, efectos equívocos para todas las comparaciones), no existe seguridad en cuanto a estos efectos. Hubo evidencia de baja calidad de una diferencia significativa en los síntomas extrapiramidales: el uso de medicación antiparkinsoniana que favorece el cambio a la quetiapina en comparación con el cambio al haloperidol (un ECA, 45 pacientes, RR 0,45; IC: 0,21 a 0,96; evidencia de baja calidad). No hubo evidencia de una diferencia para el cambio a la risperidona o el haloperidol comparado con la interrupción de los antipsicóticos (con placebo) (RR un ECA, 48 pacientes, RR 2,08; IC del 95%: 0,74 a 5,86; evidencia de baja calidad) y el cambio a la risperidona en comparación con el cambio al haloperidol (RR un ECA, 37 pacientes, RR 0,68; IC del 95%: 0,34 a 1,35; evidencia de muy baja calidad).
Los ensayos también informaron sobre los resultados secundarios como los resultados de otros síntomas de la DT, los resultados de otros eventos adversos, el estado mental y el abandono del estudio temprano, aunque la calidad de la evidencia para todos estos resultados fue muy baja debido principalmente a los tamaños de la muestra pequeños, los IC del 95% muy amplios y el riesgo de sesgo. Ningún ensayo informó sobre la confianza social, la inclusión social, las redes sociales o la calidad de vida personalizada, resultados que se designaron como importantes para los pacientes.
Conclusiones de los autores
Los datos limitados de los estudios pequeños que utilizaron la reducción de los antipsicóticos o fármacos antipsicóticos específicos como tratamientos para la DT no aportaron evidencia convincente del valor de estos enfoques. Se necesitan ensayos más grandes con una duración más prolongada para investigar plenamente esta área.
PICO
Resumen en términos sencillos
Reducción o interrupción de los antipsicóticos y antipsicóticos como tratamientos específicos para la discinesia tardía
Pregunta de la revisión
Determinar si la suspensión o la reducción de los fármacos antipsicóticos ayudan en la reducción de la discinesia tardía para los pacientes con esquizofrenia. Examinar si los fármacos antipsicóticos específicos podrían ser un tratamiento para la discinesia tardía.
Antecedentes
Los pacientes con esquizofrenia a menudo oyen voces y ven cosas (alucinaciones) y tienen creencias extrañas (delirios). El tratamiento principal para la esquizofrenia son los fármacos antipsicóticos. Sin embargo, estos fármacos pueden causar efectos secundarios debilitantes. La discinesia tardía es un movimiento involuntario que causa que la cara, la boca, la lengua y la mandíbula presenten convulsiones, espasmos y muecas. Es causada por el uso a largo plazo o las dosis altas de los fármacos antipsicóticos, es difícil de tratar y puede ser incurable. Se han propuesto diversas estrategias para reducir la exposición del paciente a los fármacos antipsicóticos. Las mismas incluyen la reducción de la dosis de la medicación, “días de descanso del fármaco” intermitentes, y la interrupción de la medicación antipsicótica por completo.
Características de los estudios
La revisión incluye 13 ensayos con un total de 711 pacientes con esquizofrenia y otros diagnósticos psiquiátricos.
Resultados clave
Debido a la baja calidad, el tamaño pequeño y los datos limitados de los 13 estudios, existe evidencia limitada. No se conoce si las estrategias como la reducción de la dosis, los “días de descanso del fármaco”, y la interrupción de la medicación son útiles en el tratamiento de la discinesia tardía. Hay evidencia limitada sobre los fármacos antipsicóticos específicos en el tratamiento de la discinesia tardía.
Calidad de la evidencia
La evidencia es deficiente, en pequeña escala y de poca duración. Se necesitan ensayos más grandes de mayor duración para investigar completamente esta área.
Este resumen en términos sencillos fue adaptado por los autores de la revisión a partir de un resumen escrito originalmente por Ben Gray, Investigador Superior Externo, McPin Foundation (http://mcpin.org/).
Authors' conclusions
Summary of findings
| Reduced dose of antipsychotic compared with antipsychotic maintenance for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: psychiatric patients (schizophrenia or schizoaffective disorder) with antipsychotic‐induced tardive dyskinesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with antipsychotic maintenance | Risk with reduced dose of antipsychotic | |||||
| Tardive dyskinesia: no clinically important improvement | Study population | RR 0.42 | 17 | ⊕⊝⊝⊝ | ||
| 875 per 1000 | 368 per 1000 | |||||
| Tardive dyskinesia: deterioration of symptoms | Study population | RR 0.61 | 17 | ⊕⊝⊝⊝ | ||
| 250 per 1000 | 153 per 1000 | |||||
| General mental state: relapse | Study population | RR 3.00 | 8 | ⊕⊝⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Adverse effect: any ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Adverse effect: extrapyramidal symptoms ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Acceptability of the treatment: leaving the study early | Study population | RR 0.33 | 8 | ⊕⊝⊝⊝ | ||
| 750 per 1000 | 248 per 1000 | |||||
| Social confidence, social inclusion, social networks, or personalised quality of life ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level for risk of bias: none of the studies adequately described allocation concealment, one study was a subsample from one site of an RCT, and one study's baseline characteristics were not balanced between study groups. | ||||||
| Antipsychotic cessation compared with antipsychotic maintenance for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: psychiatric patients with antipsychotic‐induced tardive dyskinesia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Antipsychotic maintenance | Antipsychotic cessation | |||||
| There is no evidence about the effects of withdrawal of antipsychotics compared with continuation of antipsychotics; none of the included studies evaluated this comparison. | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| Switch to another antipsychotic compared with antipsychotic cessation for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: psychiatric patients (schizophrenia) with antipsychotic‐induced tardive dyskinesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with antipsychotic cessation (placebo) | Risk with switch to another antipsychotic | |||||
| Tardive dyskinesia: no clinically important improvement | Study population | RR 0.45 | 42 | ⊕⊕⊝⊝ | ||
| 700 per 1000 | 315 per 1000 | |||||
| Tardive dyskinesia: deterioration of symptoms ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| General mental state: average endpoint score (BPRS, high = poor) | The mean general mental state average endpoint score (BPRS, high = poor) was 19 | MD 4.30 lower | ‐ | 42 | ⊕⊝⊝⊝ | |
| Adverse effect: any ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Adverse effects: use of antiparkinsonism drugs | Study population | RR 2.08 | 48 | ⊕⊝⊝⊝ | Another study reported ESRS scale data for parkinsonism and also found little or no difference between groups (MD ‐0.4 95% CI ‐1.25 to 0.45, 42 participants). | |
| 273 per 1000 | 567 per 1000 | |||||
| Acceptability of the treatment: leaving the study early | Study population | RR 0.60 | 50 | ⊕⊝⊝⊝ | ||
| 200 per 1000 | 120 per 1000 | |||||
| Social confidence, social inclusion, social networks, or personalised quality of life ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level for risk of bias: generation of random sequence and allocation concealment not adequately described. | ||||||
| Switch to specific antipsychotic compared with switch to a different specific antipsychotic for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: psychiatric patients (mainly schizophrenia) with antipsychotic‐induced tardive dyskinesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with specific antipsychotic 1 | Risk with specific antipsychotic 2 | |||||
| Tardive dyskinesia: no clinically important improvement Follow‐up: 3‐50 weeks | Study population | ‐ | 140 | ⊕⊝⊝⊝ | No meta‐analysis, studies stratified by antipsychotic. The following comparisons found no clinically important improvement: THI vs HAL, ZUC vs HAL, OLZ vs RIS, QUE vs HAL | |
| See comment | See comment | |||||
| Tardive dyskinesia: deterioration Follow‐up: 3‐4 weeks | Study population | ‐ | 35 | ⊕⊝⊝⊝ | No meta‐analysis, studies stratified by antipsychotic. The following comparisons found no difference in deterioration: THI vs HAL, ZUC vs HAL | |
| See comment | See comment | |||||
| General mental state: deterioration Follow‐up: 3‐50 weeks | Study population | ‐ | 120 | ⊕⊝⊝⊝ | No meta‐analysis, studies stratified by antipsychotic. The following comparisons found no difference in mental state deterioration: ZUC vs HAL, OLZ vs RIS, QUE vs HAL | |
| See comment | See comment | |||||
| Adverse events: extrapyramidal symptoms (need of antiparkinsonism drugs) Follow‐up: 8‐50 weeks | Study population | ‐ | 53 | ⊕⊕⊝⊝ | No meta‐analysis, studies stratified by antipsychotic. HAL more likely to need antiparkinsonism drugs than QUE (1 RCT, 45 participants, RR 0.45, 95% CI 0.21 to 0.96). No difference: RIS vs HAL | |
| See comment | See comment | |||||
| Adverse effects: general adverse events (UKU Average change score) Follow‐up: 24 weeks | See comment | See comment | ‐ | 80 | ⊕⊝⊝⊝ | No meta‐analysis, 3‐arm study comparing OLZ, ASP and unspecified FGAs found no difference in general adverse events for all pairwise comparisons. |
| Acceptability of the treatment: leaving the study early Follow‐up: 2 weeks ‐ 18 months | Study population | ‐ | 466 | ⊕⊝⊝⊝ | RIS more likely to leave study early than OLZ (2 RCTs, 130 participants, RR 0.73, 95% CI 0.57 to 0.95). Remaining studies no meta‐analysis, no difference (6 RCTs, 450 participants): MOL/THI/CLO/QUE vs HAL, OLZ/ASP vs unspecified FGAs, OLZ vs QUE/ZIP, QUE vs ZIP/RIS, ZIP vs RIS | |
| See comment | See comment | |||||
| Social confidence, social inclusion, social networks, or personalised quality of life ‐ not reported | None of the included studies reported on this outcome. | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one step for risk of bias: randomisation procedure, allocation concealment or blinding were not adequately described. | ||||||
| Specific antipsychotic compared with other drugs for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: psychiatric patients (mainly schizophrenia) with antipsychotic‐induced tardive dyskinesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with tetrabenazine | Risk with haloperidol | |||||
| Tardive dyskinesia: not improved to a clinically important extent | Study population | RR 1.07 | 13 | ⊕⊝⊝⊝ | ||
| 667 per 1000 | 713 per 1000 | |||||
| Tardive dyskinesia: deterioration of symptoms | Study population | RR 0.86 | 13 | ⊕⊝⊝⊝ | ||
| 167 per 1000 | 143 per 1000 | |||||
| Mental state ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Adverse effect: any ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Adverse effect: extrapyramidal symptoms ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Acceptability of the treatment: leaving the study early | Study population | RR 4.38 | 13 | ⊕⊝⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Social confidence, social inclusion, social networks, or personalised quality of life ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one step for risk of bias: randomisation procedure, allocation concealment and blinding were not adequately described. | ||||||
Background
Description of the condition
Since the 1950s antipsychotic (neuroleptic) medication has been extensively used to treat people with chronic mental illnesses such as schizophrenia. These drugs can effectively control symptoms such as abnormal perceptions (hallucinations), disordered thinking, and fixed false beliefs (delusions). In addition, maintenance therapy with antipsychotic medication is associated with reduced risk of relapse (Schooler 1993). Antipsychotic medication, however, has also been associated with a wide range of adverse effects, including movement disorders. The appearance of these disorders can be extremely disfiguring, compounds stigma, and is associated with poor compliance to antipsychotic treatment (Barnes 1993; Tarsy 2011).
Tardive dyskinesia (TD) is one such iatrogenic movement disorder and it is characterised by abnormal repetitive and involuntary movements. The clinical features include: tongue protrusion, side‐to‐side or rotatory movement of the jaw, lip smacking, puckering and pursing, and rapid eye blinking (Casey 1999). In some people rapid movements of the arms, legs, and trunk may also occur. TD is a chronic condition of insidious onset, the severity of which fluctuates spontaneously (APA 1992). Although the most frequent cause of TD is the use of antipsychotic medication, it is striking that dose reduction can lead to a temporary exacerbation in symptoms. Conversely, increasing the dose is often associated with a temporary remission (Cavallaro 1993; Smith 1980).
The exact mechanisms of the pathophysiology of TD are unknown. Antipsychotic drugs block certain chemical receptor sites in the brain ‐ one of these is specific for dopamine (Casey 1994). One hypothesis explaining the cause of antipsychotic‐induced TD is that chronic blockade of dopamine receptors in specific cells of the brain (neurones from the nigrostriatum) causes an overgrowth of these receptors (Casey 1994). However, there is some suggestion that the chronic use of antipsychotics may also cause an abnormal production of highly active atoms and chemical groups (cytotoxic free radicals), which may damage specific cells in the brain. This, in turn, could be responsible for the appearance of TD (Cadet 1989). This theory is supported by the persistent nature of the syndrome, once established.
Studies on the natural history of TD have reported widely variable remission rates (1% to 62%) depending on patient age, psychiatric diagnosis, course of the psychiatric disorder, and duration of therapy (Bergen 1989; Fernandez 2001; Glazer 1990). TD occurs in more than 20% of people that use first‐generation antipsychotic drugs (FGAs) continually for longer than three months (Tarsy 2011). Every year 4% to 5% of adults and 25% to 30% of elderly people who continually use these drugs begin to show signs of TD (APA 1992; Correll 2004). Advancing age is a risk factor for both TD's prevalence and severity, with those who are under 60 years of age being three times more likely to spontaneously remit (Smith 1980).
When the second‐generation antipsychotic drugs were introduced in the 1990s many hoped that they would not cause TD (Miller 2007; Rosenheck 2007). Although the risk of developing TD with second‐generation antipsychotic drugs does seem to be reduced, TD risks have not been eliminated (Miller 2007; Tarsy 2011). There is even some evidence to indicate that rates of TD do not differ at all between first‐ and second‐generation anti‐psychotic drugs (Leucht 2009; Rosenheck 2007; Woods 2010). The large, definitive, US randomised trial of antipsychotic treatments for schizophrenia (CATIE), with a four‐year period of follow‐up, obtained an incidence rate of TD of around 17% (Miller 2008). Due to widespread use of second‐generation antipsychotic drugs, increased off‐label use, and an ageing population, the frequency of TD is likely to be higher than thought (Cloud 2014; Maher 2012) and increasing. The problem will be considerably greater for people in countries where use of newer drugs is less prevalent (Ballesteros 2000; Martins 2011).
Description of the intervention
Various strategies have been examined in order to reduce a person's cumulative exposure to antipsychotics. These strategies include dose reduction, intermittent dosing strategies, such as drug holidays, and antipsychotic cessation. The prevention and treatment of TD provided much of the impetus for these studies. While antipsychotic reduction or cessation, or both would seem to be a logical first step in the management of antipsychotic‐induced TD, this is not always possible in the clinical setting because of the overriding need to manage current psychotic symptoms or to reduce the risk of relapse, or both. In this review we undertook a comprehensive study of the impact of antipsychotic dose reduction and/or cessation strategies for those who were already presenting with TD.
In the search for ways to manage antipsychotic‐induced TD, certain antipsychotic medications have themselves been proposed as specific treatments for the condition. The usual rationale for such trials relates to variations in receptor‐blocking profile that distinguishes the compound of interest from antipsychotics in general.
How the intervention might work
Although the pathophysiology of TD is not entirely clear, one of the possible underlying mechanisms is believed to be hypersensitivity of postsynaptic dopamine receptors (Margolese 2005). The risk appears to increase with higher cumulative exposure to antipsychotics, especially those with stronger D2 dopamine receptor blockade. Newer antipsychotic medications, which cause less dopamine D2 blockade, have been shown to cause less TD (Correll 2004). The primary intervention of interest (reduction/cessation of antipsychotics), is likely to help by reducing the cumulative exposure to antipsychotics. The other intervention (specific antipsychotics) is likely to work as a result of the reduction in the levels of dopamine D2 receptor blockade, a characteristic property of many of the newer antipsychotic medications.
Why it is important to do this review
TD can result in considerable social and physical disability (Barnes 1993) and symptoms are often irreversible (Bergen 1989; Fernandez 2001; Gerlach 1988; Glazer 1990). Additionally, TD is frequently associated with lower quality of life (Ascher‐Svanum 2008) and a greater mortality rate (Chong 2009). Several antipsychotic medications have been produced in recent decades that claim to cause less or no TD (Lieberman 1996). These claims may or may not be true, and certainly evidence does suggest that thoughtful use of older generation drugs is not associated with more TD than newer treatments (Chouinard 2008). However, in a global context, it is likely that the less expensive and more familiar drugs ‐ such as chlorpromazine or haloperidol ‐ will continue to be the mainstay of treatment of people with schizophrenia (WHO Essential List 2010). Use of drugs such as these is associated with emergence of TD and, therefore, this condition will remain a problem for years to come.
Given the high incidence and prevalence of TD among people taking antipsychotic medication, the need for prevention or treatment is clear. Unfortunately, there has been sparse evidence to guide clinicians (NICE 2014; Taylor 2009). Although many treatments have been tested, no one intervention has been shown clearly to be effective.
This review is one in a series of Cochrane Reviews (see Table 1) evaluating treatments for antipsychotic‐induced TD, and is an update of a Cochrane Review first published in 1998 (McGrath 1998), and previously updated in 2000 (McGrath 2000) and in 2006 (Soares‐Weiser 2006).
Objectives
To determine whether a reduction or cessation of antipsychotic drugs is associated with a reduction in TD for people with schizophrenia (or other chronic mental illnesses) who have existing TD. Our secondary objective was to determine whether the use of specific antipsychotics for similar groups of people could be a treatment for already established TD.
Methods
Criteria for considering studies for this review
Types of studies
We included all relevant randomised controlled trials. Had there been trials that were described as double‐blind, but that did not mention whether the study was randomised, we would have included them in a sensitivity analysis. If there had been no substantive difference within primary outcomes (see 'Types of outcome measures') when these studies were added, then we would have included them in the final analysis. If there had been a substantive difference, we would have used only clearly randomised trials and described the results of the sensitivity analysis in the text. We excluded quasi‐randomised studies, such as those allocating by using alternate days of the week.
Types of participants
We included people with schizophrenia or any other serious mental illness, diagnosed by any criteria, irrespective of gender, age, or nationality who required the use of antipsychotics for more than three months and who developed TD (diagnosed by any criteria) during antipsychotic treatment, and for whom the dose of antipsychotic medication had been stable for one month or more. We made a post hoc change to include studies that did not require antipsychotic medication to have been stable for one month prior to randomisation. We felt it important to include these studies as they provide additional important information. However, we planned to analyse these separately, so that they would not change existing outcome data.
Types of interventions
-
Reduction or cessation of the dose of antipsychotic drugs compared with the continuation of standard dose of the same compound. For the purposes of this review, we divided these trials into those that aimed to reduce the total dosage of antipsychotic medication, for example reduced‐dose and intermittent‐dosage schedule studies, and those that ceased antipsychotics (sometimes after variable periods of dose reduction).
-
Specific antipsychotic drugs proposed to have TD‐lessening qualities compared with placebo or no intervention. We made a decision post hoc to broaden this criteria to also include antipsychotic versus antipsychotic and antipsychotic versus other drugs for the treatment of TD.
Types of outcome measures
We have defined clinical efficacy as an improvement in the symptoms of TD of more than 50%, on any scale. We grouped outcomes into short term (less than six weeks), medium term (between six weeks and six months) and long term (more than six months).
Primary outcomes
1. Tardive dyskinesia (TD) symptoms
No clinically important improvement in the symptoms of individuals, defined as more than 50% improvement on any TD scale ‐ any time period.
2. Adverse effects
No clinically significant extrapyramidal adverse effects ‐ any time period.
Secondary outcomes
1. Tardive dyskinesia (TD) symptoms
1.1 Any improvement in the symptoms of individuals on any TD scale, as opposed to no improvement
1.2 Deterioration in the symptoms of individuals, defined as any deleterious change on any TD scale
1.3 Average change in severity of TD during the trial period
1.4 Average difference in severity of TD at the end of the trial
2. General mental state changes
2.1 The number of people per treatment group who were defined as relapsed (according to any definition)
2.2 Deterioration in general psychiatric symptoms (such as delusions and hallucinations) defined as any deleterious change on any scale
2.3 Average difference in severity of psychiatric symptoms at the end of the trial
3. Acceptability of the treatment
3.1 Acceptability of the intervention to the participant group as measured by numbers of people leaving the study early (dropping out) during the trial.
4. Adverse effects
4.1 The number of people per treatment group who had any adverse effect (other than deterioration of symptoms of TD or relapse).
4.2 Use of any antiparkinsonism drugs
4.3 Average score/change in extrapyramidal adverse effects
4.4 Acute dystonia
5. Other adverse effects, general and specific
6. Hospital and service utilisation outcomes
6.1 Hospital admission
6.2 Average change in days in hospital
6.3 Improvement in hospital status (for example: change from formal to informal admission status, use of seclusion, level of observation)
7. Economic outcomes
7.1 Average change in total cost of medical and mental health care
7.2 Total indirect and direct costs
8. Social confidence, social inclusion, social networks, or personalised quality‐of‐life measures
8.1. No significant change in social confidence, social inclusion, social networks, or personalised quality‐of‐life measures
8.2 Average score/change in social confidence, social inclusion, social networks, or personalised quality‐of‐life measures
9. Behaviour
9.1 Clinically significant agitation
9.2 Use of adjunctive medication for sedation
9.3 Aggression to self or others
10. Cognitive state
10.1 No clinically important change
10.2 No change, general and specific
In Effects of interventions we reported on all TD symptom outcomes grouped together and all adverse effects outomes grouped together, whether or not they were primary or secondary, and we indicated primary outcomes with a '*'.
'Summary of findings' table
We used the GRADE approach to interpret findings (Schünemann 2011) and used GRADEpro to export data from this review to create 'Summary of findings' tables. These tables provide outcome‐specific information concerning the overall quality of evidence from the included studies in the comparison, the magnitude of effects of interventions examined, and the sum of available data on all outcomes rated as important to patient care and decision making. We selected the following main outcomes for inclusion in the 'Summary of findings' table:
1. Tardive dyskinesia
1.1 Improved to a clinically important extent
1.2 Deteriorated
2. Mental state
3. Adverse effect
3.1 Any adverse event
3.2 Adverse effects: no clinically significant extrapyramidal adverse effects
4. Acceptability of treatment
4.1 Leaving the study early
5. Social confidence, social inclusion, social networks, or personalised quality of‐life‐measures
5.1 No significant change in social confidence, social inclusion, social networks, or personalised quality‐of‐life measures for either recipients of care or caregivers
We used this summary to guide our conclusions.
Personalised quality‐of‐life is an outcome designated important to patients. We wished to add perspectives from people’s personal experience with TD to the research agenda. We planned a consultation with service users, where the previously published version of a review in the Cochrane TD series (Soares‐Weiser 2011; Table 1) and a lay overview of that review gave the foundation for the discussions. The session was planned to provide time to reflect on current research on TD and to consider gaps in knowledge. The report is published in the Health Technology Assessment (HTA) report for the UK National Institute of Health Research (Bergman 2017). We have added one figure showing one service user's expression of frustration concerning this neglected area of research (Figure 1). Informed by the results of the consultation, for this review, we have included outcomes of the consultation in the 'Summary of findings' tables.
Message from one of the participants of the public and patient involvement consultation of service user perspectives on tardive dyskinesia research
Search methods for identification of studies
Electronic searches
The 2017 review update was carried out in parallel with updating eight other Cochrane TD Reviews and the search covered all nine reviews; see Table 1 for details.
1. Cochrane Schizophrenia Group’s Study‐Based Register of Trials
On July 16, 2015 and April 26, 2017, the Information Specialist searched the register using the following string:
*Tardive Dyskinesia* in Healthcare Condition Field of Study
In a study‐based register, searching the major concept retrieves all the synonyms and relevant studies because all the studies have already been organised based on their interventions and linked to the relevant topics (Shokraneh 2017).
This register is compiled by systematic searches of major resources (AMED, BIOSIS, CINAHL, ClinicalTrials.Gov, Embase, MEDLINE, PsycINFO, PubMed, WHO ICTRP) and their monthly updates, ProQuest Dissertations and Theses A&I and its quarterly update, Chinese databases (CBM, CNKI, and Wanfang) and their annual updates, hand‐searches, grey literature, and conference proceedings (see Group’s Module). There is no language, date, document type, or publication status limitations for inclusion of records into the register.
For previous searches, please see Appendix 1.
Searching other resources
1. Reference searching
We inspected references of all identified studies for further relevant studies.
2. Personal contact
We contacted the first author of each included study for information regarding unpublished trials.
Data collection and analysis
Selection of studies
For the 2017 update, reviewers RA and AG (see Acknowledgements) inspected all abstracts of studies identified as above and identified potentially relevant reports. We resolved disagreement by discussion, or where there was still doubt, we acquired the full article for further inspection. We acquired the full articles of relevant reports/abstracts meeting initial criteria for reassessment and carefully inspected for a final decision on inclusion (see Criteria for considering studies for this review). RA and AG were not blinded to the names of the authors, institutions or journal of publication. Where difficulties or disputes arose, we asked review author HB for help and where it was impossible to decide or if adequate information was not available to make a decision, we added these studies to those awaiting assessment and contacted the authors of the papers for clarification.
Data extraction and management
1. Extraction
For the 2017 update, reviewers RA and HB independently extracted data from all included studies. Again, we discussed any disagreement and documented decisions. We extracted data presented only in graphs and figures whenever possible, but we included data only if two review authors independently had the same result. We attempted to contact study authors through an open‐ended request in order to obtain missing information or for clarification whenever necessary. If studies were multi‐centre, where possible, we extracted data relevant to each component centre separately.
2. Management
2.1 Forms
For the 2017 update we extracted data online in Covidence. Extracted data are available here with a link to the original source PDF for each item.
2.2 Scale‐derived data
We included continuous data from rating scales only if:
a) the psychometric properties of the measuring instrument had been described in a peer‐reviewed journal (Marshall 2000); and
b) the measuring instrument had not been written or modified by one of the trialists for that particular trial.
Ideally the measuring instrument should either have been (a) a self‐report or (b) completed by an independent rater or relative (not the therapist). We realise that this is not often reported clearly, and we noted in Description of studies if this was the case or not.
2.3 Endpoint versus change data
There are advantages of both endpoint and change data. Change data can remove a component of between‐person variability from the analysis. On the other hand, calculation of change needs two assessments (baseline and endpoint), which can be difficult in unstable and difficult‐to‐measure conditions such as schizophrenia. We decided to primarily use endpoint data, and only to use change data if the former were not available. We combined endpoint and change data in the analysis as we preferred to use mean differences (MD) rather than standardised mean differences throughout (Higgins 2011a).
2.4 Skewed data
Continuous data on clinical and social outcomes are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data, we applied the following standards to relevant data before inclusion.
Please note, we entered data from studies of at least 200 participants in the analysis because skewed data pose less of a problem in large studies. We also entered all relevant change data, as when continuous data are presented on a scale that includes a possibility of negative values (such as change data), it is difficult to tell whether data are skewed or not.
For endpoint data from studies with fewer than 200 participants:
(a) for scales starting from the finite number zero, we subtracted the lowest possible value from the mean, and divided this by the standard deviation. If this value was lower than 1, it strongly suggested a skew and we excluded these data. If this ratio was higher than one but below 2, there was suggestion of skew. We entered these data and tested whether their inclusion or exclusion changed the results substantially. Finally, if the ratio was larger than 2 we included these data, because skew was less likely (Altman 1996; Higgins 2011a).
(b) for scales starting from a positive value (such as the Positive and Negative Syndrome Scale (PANSS, Kay 1986), which can have values from 30 to 210), we modified the calculation described above to take the scale starting point into account. In these cases skew is present if 2 SD > (S‐S min), where S is the mean score and 'S min' is the minimum score.
2.5 Common measure
Where relevant, to facilitate comparison between trials, we converted variables that can be reported in different metrics, such as days in hospital (mean days per year, per week, or per month) to a common metric (e.g. mean days per month).
2.6 Conversion of continuous to binary
Where possible, we converted continuous outcome measures to dichotomous data. This can be done by identifying cut‐off points on rating scales and dividing participants accordingly into 'clinically improved' or 'not clinically improved'. It is generally assumed that if there is a 50% reduction in a scale‐derived score such as the Brief Psychiatric Rating Scale (BPRS, Overall 1962) or the PANSS (Kay 1986), this can be considered as a clinically significant response (Leucht 2005a; Leucht 2005b). If data based on these thresholds were not available, we used the primary cut‐off presented by the study authors.
2.7 Direction of graphs
Where possible, we entered data in such a way that the area to the left of the line of no effect indicated a favourable outcome for reduction or cessation of antipsychotic. Where keeping to this made it impossible to avoid outcome titles with clumsy double‐negatives (e.g. 'not un‐improved') we presented data where the left of the line indicated an unfavourable outcome and noted this in the relevant graphs.
Assessment of risk of bias in included studies
RA (see Acknowledgements) and HB independently assessed risk of bias within the included studies by using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions to assess trial quality (Higgins 2011b). This set of criteria is based on evidence of associations between overestimate of effect and high risk of bias of the article such as sequence generation, allocation concealment, blinding, incomplete outcome data, and selective reporting.
If the raters disagreed, we made the final rating by consensus, with the involvement of another member of the review group. Where inadequate details of randomisation and other characteristics of trials were provided, we contacted authors of the studies in order to obtain further information. If non‐concurrence occurred, we reported this.
We noted the level of risk of bias in the text of the review and in Figure 2; Figure 3 and 'Summary of findings' tables.
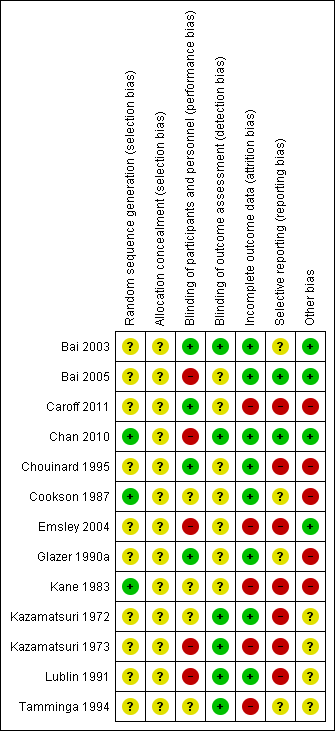
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
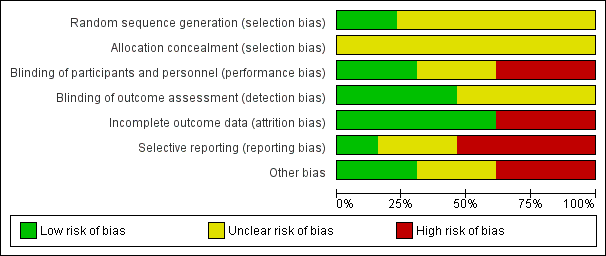
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Measures of treatment effect
1. Binary data
For binary outcomes we calculated a standard estimation of the risk ratio (RR) and its 95% confidence interval (CI). It has been shown that RR is more intuitive (Boissel 1999) than odds ratios, as odds ratios tend to be interpreted as RR by clinicians (Deeks 2000).
2. Continuous data
For continuous outcomes we estimated mean difference (MD) between groups. We preferred not to calculate effect size measures (standardised mean difference (SMD)). However, if scales of very considerable similarity were used, we presumed there was a small difference in measurement, and calculated effect size and transformed the effect back to the units of one or more of the specific instruments.
Unit of analysis issues
1. Cluster‐randomised trials
Studies increasingly employ 'cluster randomisation' (such as randomisation by clinician or practice) but analysis and pooling of clustered data poses problems. Firstly, study authors often fail to account for intra‐class correlation in clustered studies, leading to a 'unit of analysis' error (Divine 1992) whereby P values are spuriously low, confidence intervals unduly narrow, and statistical significance overestimated. This causes type I errors (Bland 1997; Gulliford 1999).
If any of the included trials had randomised participants by clusters, and where clustering was not accounted for in primary studies, we would have presented such data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. In subsequent versions of this review we will seek to contact first authors of studies to obtain intra‐class correlation coefficients for their clustered data and to adjust for this by using accepted methods (Gulliford 1999). Where clustering had been incorporated into the analysis of primary studies, we presented these data as if from a non‐cluster‐randomised study, but adjusted for the clustering effect.
We have sought statistical advice and have been advised that the binary data as presented in a report should be divided by a 'design effect'. This is calculated using the mean number of participants per cluster (m) and the intra‐class correlation coefficient (ICC) (design effect=1+(m‐1)*ICC) (Donner 2002). If the ICC was not reported we would assume it was 0.1 (Ukoumunne 1999).
If cluster studies were appropriately analysed, taking into account intra‐class correlation coefficients and relevant data documented in the report, synthesis with other studies would be possible using the generic inverse variance technique.
2. Cross‐over trials
A major concern of cross‐over trials is the carry‐over effect. The carry‐over effect occurs if an effect (e.g. pharmacological, physiological or psychological) of the treatment in the first phase is carried over to the second phase. As a consequence, on entry to the second phase the participants can differ systematically from their initial state despite a washout phase. For the same reason, cross‐over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both effects are very likely in severe mental illness, we only used data of the first phase of cross‐over studies.
3. Studies with multiple treatment groups
Where a study involved more than two treatment arms, if relevant, we presented the additional treatment arms in comparisons. If data were binary we simply added and combined within the two‐by‐two table. If data were continuous we combined data following the formula in section 7.7.3.8 (Combining groups) of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). We did not use data where the additional treatment arms were not relevant.
Dealing with missing data
1. Overall loss of credibility
At some degree of loss of follow‐up, data must lose credibility (Xia 2009). We decided that, for any particular outcome, should more than 50% of data be unaccounted for, we would not reproduce these data or use them within analyses. If, however, more than 50% of those in one arm of a study were lost, but the total loss was less than 50%, we addressed this within the 'Summary of findings' tables by down‐rating quality. We also downgraded quality within the 'Summary of findings' tables should loss be 25% to 50% in total.
2. Binary
In the case where attrition for a binary outcome was between 0% and 50%, and where these data were not clearly described, we presented data on a 'once‐randomised‐always‐analyse' basis (an intention‐to‐treat (ITT) analysis). We assumed that all those leaving the study early had seen no improvement in TD symptoms. We undertook a sensitivity analysis, testing how prone the primary outcomes were to change by comparing data only from people who had completed the study to that point to the ITT analysis using the above assumptions.
3. Continuous
3.1 Attrition
We reported and used data where attrition for a continuous outcome was between 0% and 50%, and data only from people who had completed the study to that point were reported.
3.2 Standard deviations
If standard deviations were not reported, we first tried to obtain the missing values from the study authors. If not available, where there were missing measures of variance for continuous data, but an exact standard error and confidence intervals available for group means, and either P value or 't' value available for differences in mean, we calculated them according to the rules described in the Cochrane Handbook for Systemic reviews of Interventions (Higgins 2011c). When only the standard error (SE) is reported, standard deviations (SDs) are calculated by the formula SD = SE * square root (n). Chapters 7.7.3 and 16.1.3 of the Cochrane Handbook for Systemic reviews of Interventions (Higgins 2011a; Higgins 2011c) present detailed formulae for estimating SDs from P values, t or F values, confidence intervals, ranges, or other statistics. If these formulae did not apply, we calculated the SDs according to a validated imputation method which was based on the SDs of the other included studies (Furukawa 2006). Although some of these imputation strategies can introduce error, the alternative would be to exclude a given study’s outcome and thus lose information. We nevertheless examined the validity of the imputations in a sensitivity analysis excluding imputed values.
3.3 Assumptions about participants who left the trials early or were lost to follow‐up
Various methods are available to account for participants who left the trials early or were lost to follow‐up. Some trials just present the results of study completers, others use the method of last observation carried forward (LOCF), while more recently, methods such as multiple imputation or mixed effects models for repeated measurements (MMRM) have become more of a standard. While the latter methods seem to be somewhat better than LOCF (Leon 2006), we feel that the high percentage of participants leaving the studies early and differences in the reasons for leaving the studies early between groups is often the core problem in randomised schizophrenia trials. We therefore did not exclude studies based on the statistical approach used. However, we preferred to use the more sophisticated approaches (e.g. MMRM or multiple‐imputation) and only presented completer analyses if some kind of ITT data were not available at all. Moreover, we addressed this issue in the item "incomplete outcome data" of the risk of bias tool.
Assessment of heterogeneity
1. Clinical heterogeneity
We considered all included studies initially, without seeing comparison data, to judge clinical heterogeneity. We simply inspected all studies for clearly outlying people or situations that we had not predicted would arise and discussed in the text if they arose.
2. Methodological heterogeneity
We considered all included studies initially, without seeing comparison data, to judge methodological heterogeneity. We simply inspected all studies for clearly outlying methods that we had not predicted would arise and discussed in the text if they arose.
3. Statistical heterogeneity
3.1 Visual inspection
We visually inspected graphs to investigate the possibility of statistical heterogeneity.
3.2 Employing the I2 statistic
We investigated heterogeneity between studies by considering the I2 statistic method alongside the Chi2 P value. The I2 statistic provides an estimate of the percentage of inconsistency thought to be due to chance (Higgins 2003). The importance of the observed value of I2 statistic depends on (a) magnitude and direction of effects and (b) strength of evidence for heterogeneity (e.g. P value from Chi2 test, or a confidence interval for I2 statistic). An I2 estimate greater than or equal to around 50% accompanied by a statistically significant Chi2 statistic can be interpreted as evidence of substantial levels of heterogeneity (section 9.5.2 Cochrane Handbook for Systematic Reviews of InterventionsDeeks 2011). We explored and discussed in the text potential reasons for substantial levels of heterogeneity (see Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results (Egger 1997). These are described in section 10 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We are aware that funnel plots may be useful in investigating reporting biases but are of limited power to detect small‐study effects. We did not use funnel plots for outcomes where there were ten or fewer studies, or where all studies were of similar sizes. In future versions of this review, if funnel plots are possible, we will seek statistical advice in their interpretation.
Data synthesis
We understand that there is no closed argument for preference for use of fixed‐effect or random‐effects models. The random‐effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This often seems to be true to us and the random‐effects model takes into account differences between studies even if there is no statistically significant heterogeneity. There is, however, a disadvantage to the random‐effects model. It puts added weight onto small studies which often are the most biased ones. Depending on the direction of effect, these studies can either inflate or deflate the effect size. We chose the fixed‐effect model for all analyses.
Subgroup analysis and investigation of heterogeneity
1. Subgroup analyses
1.1 Primary outcomes
We anticipated one subgroup analysis to test the hypothesis that the use of antipsychotic reduction, cessation or specific antipsychotics is most effective for those with early‐onset TD (less than five years). We hoped to present data for this subgroup for the primary outcomes.
1.2 Clinical state, stage or problem
We proposed to undertake this review and provide an overview of the effects of antipsychotic reduction/cessation or specific antipsychotics for people with TD in general. In addition, however, we tried to report data on subgroups of people in the same clinical state, stage, and with similar problems.
2. Investigation of heterogeneity
We reported that inconsistency was high. First, we investigated whether data were entered correctly. Second, if data were correct, we visually inspected the graph and successively removed studies outside of the company of the rest to see if homogeneity was restored. For this review we decided that, should this occur with data contributing to the summary finding of no more than around 10% of the total weighting, we would present the data. If not, we did not pool such data and discussed issues. We know of no supporting research for this 10% cut‐off but are investigating use of prediction intervals as an alternative to this unsatisfactory state.
When unanticipated clinical or methodological heterogeneity were obvious, we simply discussed. We did not undertake sensitivity analyses relating to these.
Sensitivity analysis
1. Implication of randomisation
If trials were described in some way as to imply randomisation we undertook a sensitivity analysis for the primary outcomes. We included these studies in the analyses, and if there was no substantive difference when the implied randomised studies were added to those with better description of randomisation, we used relevant data from these studies.
2. Assumptions for lost binary data
Where we had to make assumptions regarding people lost to follow‐up (see Dealing with missing data) we compared the findings of the primary outcomes when we used our assumption compared with completer data only. If there was a substantial difference, we reported and discussed these results but continued to employ our assumption.
Where we had to make assumptions regarding missing SD data (see Dealing with missing data), we compared the findings on primary outcomes when we used our assumption compared with completer data only. We undertook a sensitivity analysis, testing how prone results were to change when completer data only were compared with the imputed data using the above assumption. If there was a substantial difference, we reported and discussed these results but continued to employ our assumption.
3. Risk of bias
We analysed the effects of excluding trials that we judged to be at high risk of bias across one or more of the domains of randomisation (implied as randomised with no further details available) allocation concealment, blinding, and outcome reporting for the meta‐analysis of the primary outcome. If the exclusion of trials at high risk of bias did not substantially alter the direction of effect or the precision of the effect estimates, we included data from these trials in the analysis
4. Imputed values
Had cluster‐randomised trials been included, we would have undertaken a sensitivity analysis to assess the effects of including data from trials where we used imputed values for ICC in calculating the design effect.
If we found substantial differences in the direction or precision of effect estimates in any of the sensitivity analyses listed above, we did not pool data from the excluded trials with the other trials contributing to the outcome, but presented them separately
5. Fixed‐effect and random‐effects models
We synthesised data using a fixed‐effect model; however, we also synthesised data for the primary outcome using a random‐effects model to evaluate whether this altered the significance of the results.
Results
Description of studies
Please see Characteristics of included studies, Characteristics of excluded studies and Characteristics of ongoing studies.
Results of the search
The 2015 and 2017 searches for the 2017 review update also covered updates for the other eight Cochrane Reviews in the TD series, see Table 1.
The 2015 search retrieved 704 references for 344 studies, see Figure 4 for study flow diagram (Moher 2009). We also screened all references of the previously published review, 99 of which were not covered in the updated search. We identified 18 new potentially relevant studies for this review for which we conducted full‐text screenings. Five of these studies are newly included in this review (Bai 2005; Caroff 2011; Chan 2010; Chouinard 1995; Kazamatsuri 1973). A study previously awaiting classification was included as several more publications were identified in the new search (Bai 2003). Two studies were previously excluded because there was no placebo group, but as head‐to‐head comparisons of antipsychotic drugs for the treatment of TD has been added to the inclusion criteria in this review, these studies were subsequently included (Lublin 1991; Tamminga 1994). We also added 13 new excluded studies, and three studies previously awaiting classification were also excluded (Barnes 2002; Cai 1988; Zeng 1994).
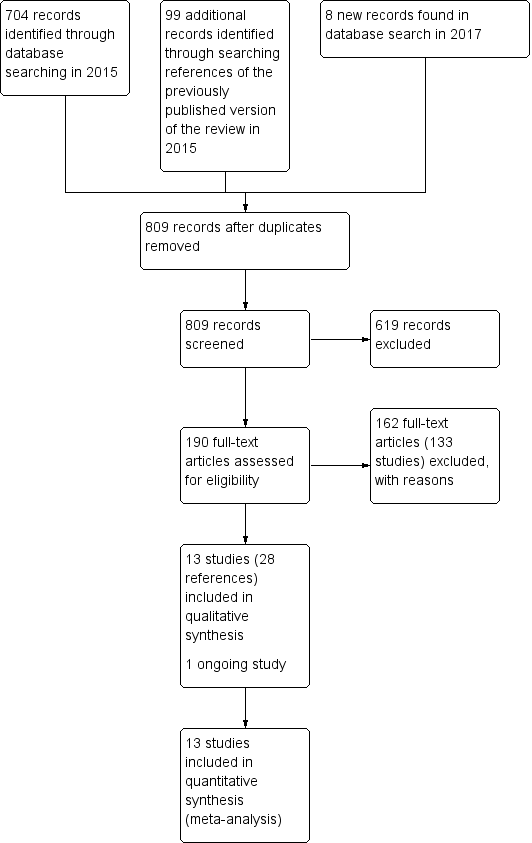
Study flow diagram for 2015 and 2017 searches for this review
The 2017 search found 8 records (5 studies). Editorial base of Cochrane Schizophrenia screened these records and no new studies were relevant to this review. They could be relevant to the other reviews in this series of TD reviews (see Table 1), and have been put into awaiting assessment of the Miscellaneous treatments review Soares‐Weiser 2006 and the benzodiazepines review Bhoopathi 2006.
Thirteen studies are now included in this review (Tamminga 1994; Cookson 1987; Kane 1983; Kazamatsuri 1973; Glazer 1990a; Bai 2005; Caroff 2011; Chan 2010; Emsley 2004; Chouinard 1995; Bai 2003; Kazamatsuri 1972; Lublin 1991).
Included studies
Overall the review now includes 13 studies with 711 participants published between 1972 and 2011.
1. Methods
Most studies stated that they were randomised and double‐blind. Two studies reported being only single‐blind (Bai 2005; Chan 2010). For further details please see sections below on allocation and blinding.
2. Design
All included studies presented a parallel longitudinal design. One of the 13 studies used a cross‐over design with two periods (Lublin 1991). We had considered this as likely when embarking on the review and have used only the data from before the first cross‐over for the reasons outlined above (Unit of analysis issues).
3. Duration
We included three short‐term studies reporting data at two to four weeks (Glazer 1990a; Kazamatsuri 1972; Lublin 1991). Five studies reported data at medium‐term, 8 to 24 weeks (Bai 2003; Bai 2005; Chan 2010; Chouinard 1995; Kazamatsuri 1973), and there were five long‐term studies reporting data at 44 weeks to 18 months (Caroff 2011; Cookson 1987; Emsley 2004; Kane 1983; Tamminga 1994).
4. Participants
Participants, now totaling 711 people, were mostly men with aged 50 to 60 years with diagnoses of various chronic psychiatric disorders, but mainly schizophrenia. All had antipsychotic‐induced TD diagnosed using Schooler and Kane’s research diagnostic criteria, except Lublin 1991, which did not report any criteria for the diagnosis of TD. The number of participants ranged from 8 to 200 (median 32).
5. Setting
Most trials were conducted in hospital. The studies themselves were from around the world, with six conducted in the USA (Caroff 2011; Glazer 1990a; Kane 1983; Kazamatsuri 1972; Kazamatsuri 1973; Tamminga 1994), three in Taiwan (Bai 2003; Bai 2005; Chan 2010), and one each in South Africa (Emsley 2004), Canada (Chouinard 1995), Denmark/Finland (Lublin 1991), and the UK (Cookson 1987).
6. Interventions
6.1 Antipsychotic reduction
6.1.1 cis(z)‐flupenthixol decanoate
Cookson 1987 used a reduction of 50% of the standard dose of cis(z)‐flupenthixol decanoate.
6.1.2 Fluphenazine decanoate
Kane 1983 compared a low dose of fluphenazine decanoate (1.25 mg to 5 mg for two weeks) to the standard dose (12.5 mg to 50 mg for two weeks).
6.2 Specific antipsychotics
6.2.1 Clozapine
Tamminga 1994 used clozapine in a mean (± SD) dose of 293.8 mg ± 171.9 mg a day for 12 months.
6.2.2 Risperidone
Four studies used risperidone in a dose ranging from 1.5 mg a day to 16 mg a day (Bai 2003; Caroff 2011; Chan 2010; Chouinard 1995).
6.2.3 Olanzapine
Three studies used olanzapine in a dose ranging from 7.5 mg a day to 12.6 mg a day (Caroff 2011; Chan 2010), Bai 2005 did not report the dose.
6.2.4 Amisulpride
Bai 2005 used amisulpride but did not report the dose.
6.2.5 Quetiapine
Two studies used quetiapine in a dose ranging from 100 mg a day to 400 mg a day (Caroff 2011; Emsley 2004).
6.2.6 Ziprasidone
Caroff 2011 used ziprasidone in a flexible dose of 40 mg.
6.2.7 Haloperidol
Seven studies used haloperidol in doses ranging from 2 mg a day to 34 mg a day (Chouinard 1995; Emsley 2004; Glazer 1990a; Kazamatsuri 1972; Kazamatsuri 1973; Lublin 1991; Tamminga 1994).
6.2.8 Molindone
Glazer 1990a used molindone in a dose from 75 mg to 145 mg.
6.2.9 Thiopropazate
Kazamatsuri 1972 used thiopropazate in a dose of 10 mg a day to 80 mg a day.
6.2.10 Zuclopenthixol
Lublin 1991 used zuclopenthixol in a dose from 16.5 mg a day to 26.6 mg a day.
6.3 Other drugs
6.3.1 Tetrabenazine
Kazamatsuri 1973 used tetrabenazine in a dose of 50 mg twice a day.
7. Outcomes
7.1 General
The included studies presented outcomes in graphs, inexact P values of differences, or a statement of significant or non‐significant difference. This made it impossible to acquire raw data for synthesis. We were unable to extract some continuous outcomes due to missing number of participants or missing means, standard deviations, or standard errors. All included studies used the LOCF strategy for the ITT analysis of dichotomous data.
7.2 Scales used to measure the TD symptoms
We have shown details of the scales that provided usable data below. We have provided reasons for exclusions of data under 'Outcomes' in the Characteristics of included studies tables.
7.2.1 Abnormal Involuntary Movement Scale (AIMS)
The AIMS (Guy 1970) is a 12‐item scale consisting of a standardised examination followed by questions rating orofacial, extremity, and trunk movements, as well as three global measurements. Each of these 10 items can be scored from 0 (none) to 4 (severe). Two additional items assess dental status. The AIMS ranges from 0 to 40, with higher scores indicating greater severity.
7.2.2 Extrapyramidal symptom rating scale (ESRS)
The ESRS was developed to assess four types of drug‐induced movement disorders (DIMD): parkinsonism, akathisia, dystonia, and TD (Chouinard 2005). The score for TD, ranging from 0 to 42, is based on the sum of all seven items in the TD objective examination.
7.2.3 St. Hans Rating Scale for extrapyramidal syndromes (SHRS)
The SHRS is a multidimensional rating scale for the evaluation of antipsychotic‐induced hyperkinesia, parkinsonism, akathisia, and dystonia (Gerlach 1993). Each item is rated from 0 (not present) to 6 (present to an extreme degree). This gives a total score from 0 to 48 for hyperkinesia and parkinsonism.
7.3 Scales used to measure adverse events related to antipsychotic medication
7.3.1 Simpson‐Angus Scale (SAS)
The SAS (Simpson 1970) is a 10‐item scale, with a scoring system of 0 to 4 for each item, that measures drug‐induced parkinsonism, a short‐term drug‐induced movement disorder. A low score indicates low levels of parkinsonism.
7.3.2 Barnes Akathisia Scale (BAS)
The BAS (Barnes 1989) is a 12‐item scale consisting of a standardised examination followed by questions rating orofacial, extremity, and trunk movements, as well as three global measurements. Each of these 10 items can be scored from 0 (none) to 4 (severe). Two additional items assess dental status. The BAS ranges from 0 to 40, with higher scores indicating greater severity.
7.3.3 UKU‐Side Effect Rating Scale
The UKU was developed to provide a comprehensive side effect rating scale with well‐defined and operationalised items to assess the side effects of psychopharmacological medications (Lingjaerde 1987). The scoring sheet includes 48 items with higher scores indicating more side effects.
7.4 Scales used to measure mental state and behaviour
7.4.1 Brief Psychiatric Rating Scale (BPRS)
The BPRS is an 18‐item scale measuring positive symptoms, general psychopathology and affective symptoms (Overall 1962). The original scale has 16 items, although a revised 18‐item scale is commonly used. Total scores can range from 0 to 126. Each item is rated on a seven‐point scale, with high scores indicating more severe symptoms.
7.4.2 Positive and Negative Syndrome Scale (PANSS)
The PANSS is a medical scale used for measuring symptom severity of people with schizophrenia (Kay 1986). The individual is rated from 1 to 7 on 30 different symptoms based on the interview as well as reports of family members or primary care hospital workers.
7.4.3 Clinical Global Impression
The CGI is a three‐item scale commonly used in studies on schizophrenia to enable clinicians to quantify severity of illness and overall clinical improvement (Guy 1976). The items are: severity of illness, global improvement, and efficacy index. A seven‐point scoring system is usually employed with low scores indicating decreased severity or greater recovery, or both.
Excluded studies
There are 133 excluded studies (163 references); the majority (n = 74) were excluded because they were not randomised. Thirty‐nine studies included participants with schizophrenia or other mental disorders who did not have TD. One study did not provide separate data from the included minority with TD; we contacted study authors who confirmed that these data were not available. Five studies investigated interventions that were not relevant for this review. Seven studies were cross‐over studies that did not provide data from the phase before crossing over to the next treatment. We contacted authors for three of these studies: author of Lal 1974 confirmed that no separate data were available, and we received no reply from authors of Lieberman 1988 or NDSG 1986, which were also excluded as they were published over 20 years ago and we assumed it very unlikely to receive a reply with data so many years later. We did not find up‐to‐date contact details for authors of four of the cross‐over studies (Bateman 1979; Delwaide 1979; Schwartz 1990; Singer 1971), and decided to also exclude these as they were published 25 to 45 years ago and we assumed it very unlikely to receive a reply so many years later. Seven studies did not provide any usable data. Authors of five of these studies (Herz 1991; Johnson 1987; Quinn 1984; Spohn 1988; Spohn 1993) confirmed that no further data were available. Authors of one of these studies did not reply (Andia 1998) and we could not find up‐to‐date contact details for authors of a final study (Borison 1987). We excluded these two studies as they were published 15 to 25 years ago and we assumed it very unlikely to receive a reply with data so many years later.
Studies awaiting classification
There are currently no studies awaiting assessment for inclusion in this review.
Ongoing studies
There is one ongoing study (N0546099389), which compares quetiapine and risperidone. This study was excluded in the previous review, but we have decided to move it to the ongoing studies section. It is a record from a trial registry, and at the time of preparing this update we were unable to locate author contact details or any more information about the study.
Risk of bias in included studies
Please refer to Figure 2 and Figure 3 for graphical overviews of the risk of bias in the included studies.
Allocation
While all 13 included studies stated that they randomised participants, we considered only three studies to be at low risk of selection bias. Two of these studies explicitly described how they generated the randomisation sequence (Chan 2010; Kane 1983), whereas one described block randomisation with stratification, and we assumed low risk of bias (Cookson 1987). None of the studies described how they concealed allocation and we rated all of them at unclear risk of selection bias.
Blinding
Eight studies stated that they were conducted on a double‐blind basis, but none tested the blindness of raters, clinicians and trial participants. Only four studies (Bai 2003; Caroff 2011; Chouinard 1995; Glazer 1990a) explicitly described how they blinded participants and personnel, and we rated them at low risk of performance bias. Five studies did not mention blinding of participants or personnel, or that the study was double‐blind (Bai 2005; Chan 2010; Emsley 2004; Kazamatsuri 1973; Lublin 1991); these studies were at high risk of performance bias. The remaining four studies were at unclear risk of performance bias; they stated that the study was double‐blind but did not describe further details of blinding.
Six studies had blinded raters and were at low risk of detection bias (Bai 2003; Chan 2010; Kazamatsuri 1972; Kazamatsuri 1973; Lublin 1991; Tamminga 1994). The remaining seven studies were at unclear risk of detection bias.
Incomplete outcome data
Eight studies were at low risk of attrition bias; they either had no dropouts (Cookson 1987) or low dropout rate and reported on dropouts adequately (Bai 2003; Bai 2005; Chan 2010; Chouinard 1995; Glazer 1990a; Kazamatsuri 1972; Lublin 1991). Five studies had a greater than 30% loss to follow‐up (Caroff 2011; Emsley 2004; Kane 1983; Tamminga 1994), or unbalanced loss to follow‐up between groups (Kazamatsuri 1973), and did not report outcomes for participants lost to follow‐up. These studies were rated at high risk of attrition bias. In all cases, however, we tried to ensure that every person randomised was analysed.
Selective reporting
The majority of data in this review originates from published reports. Most of the included studies reported expected outcomes (impact on TD symptoms). Only two trials fully reported outcomes outlined in protocols and were at low risk of reporting bias (Bai 2005; Chan 2010). Four trials were at unclear risk of bias, as we have had no opportunity to see protocols of these trials to compare the outcomes reported in the full publications with what was measured during the conduct of the trial (Bai 2003; Cookson 1987; Glazer 1990a; Tamminga 1994). Seven studies did not report results of all outcomes listed in the methods section fully (Caroff 2011; Chouinard 1995; Emsley 2004; Kane 1983; Kazamatsuri 1972; Kazamatsuri 1973; Lublin 1991) and were at high risk of reporting bias. Attempts to contact authors of trials for additional data were mostly unsuccessful, but we did receive some additional data from four of the trialists (Cookson 1987; Caroff 2011; Chouinard 1995; Kane 1983).
Other potential sources of bias
Four studies reported details such as baseline characteristics with sufficient detail to rate them at low risk of other bias. Four studies were at unclear risk of other bias, three (Kazamatsuri 1973; Kazamatsuri 1972; Lublin 1991) because of insufficiently detailed reporting to rule out any other bias, and one (Tamminga 1994) because the report was on a preliminary analysis with four of 49 subjects not yet having completed the study. Despite randomisation, two studies reported having unequal groups at baseline on important prognostic factors, and thus were at high risk of other bias (Cookson 1987; Glazer 1990a). Three studies randomised participants with schizophrenia, and this review included secondary reports of post hoc analyses of participants with TD. These studies were therefore at high risk of other bias (Caroff 2011; Chouinard 1995; Kane 1983).
Effects of interventions
See: Summary of findings for the main comparison Reduced dose of antipsychotics compared with antipsychotic maintenance for antipsychotic‐induced tardive dyskinesia; Summary of findings 2 Antipsychotic cessation compared with antipsychotic maintenance for antipsychotic‐induced tardive dyskinesia; Summary of findings 3 Switch to another antipsychotic compared with antipsychotic cessation for antipsychotic‐induced tardive dyskinesia; Summary of findings 4 Switch to a specific antipsychotic compared with switch to a different specific antipsychotic for antipsychotic‐induced tardive dyskinesia; Summary of findings 5 Specific antipsychotic compared with other drugs for antipsychotic‐induced tardive dyskinesia
* indicates primary outcomes.
Comparison 1. Reduced overall dose of antipsychotic versus antipsychotic maintenance
1.1 TD symptoms
We had chosen 'No clinically important improvement in TD symptoms' for any time period as a primary outcome, with clinically important improvement defined as more than 50% improvement on any TD scale. Although the data we found in trials did not fit this exactly we feel that the outcome 'not improved to a clinically important extent' fits best with what we had hoped to find.
The authors of two RCTs of antipsychotic reduction provided additional data (Cookson 1987; Kane 1983).
1.1.1 No clinically important improvement*
No clinically important improvement in TD severity was associated with antipsychotic reduction compared with antipsychotic maintenance at 44 to 48 weeks (very low‐quality evidence, 2 RCTs, 17 people, RR 0.42 95% CI 0.17 to 1.04, Analysis 1.1).
1.1.2 Not any improvement
When the outcome criterion was broadened from clinically significant improvement to improvement of any degree in TD severity, the result persisted at 44 to 48 weeks (very low‐quality evidence, 2 RCTs, 17 people, RR 0.42 95% CI 0.17 to 1.04, Analysis 1.2).
1.1.3 Deterioration of symptoms
Antipsychotic reduction was not associated with deterioration of TD symptoms compared with continued dose at 44 to 48 weeks (very low‐quality evidence, 2 RCTs, 17 people, RR 0.61 95% CI 0.11 to 3.31, Analysis 1.3).
1.2 General mental state
1.2.1 Relapse
The number of those relapsing was equivocal over the long term (1 RCT, 8 people, RR 3.00 95% CI 0.16 to 57.36, Analysis 1.4).
1.3 Acceptability of the treatment: leaving the study early
The number of people leaving the study early was not statistically different for either the antipsychotic reduction group (1/4) or the antipsychotic maintained group (3/4) at 44 to 48 weeks (very low‐quality evidence, 1 RCT, 8 people, RR 0.33 95% CI 0.06 to 1.99, Analysis 1.5).
We did not identify any studies that reported on adverse events, hospital and service utilisation outcomes, economic outcomes, social confidence, social inclusion, social networks, personalised quality of life, behaviour, or cognitive state.
1.4 Subgroup analysis
1.4.1 Clinical stage: recent‐onset TD
It was not possible to evaluate whether those with recent‐onset TD responded differently to those with more established problems, since neither trial reported data for groups with different durations of TD that could be extracted for separate analyses.
1.4.2 Duration of follow‐up
We were unable to investigate any effects that a reduced dose of antipsychotics may have had in relation to duration of follow‐up because both studies had very similar length: 44 and 48 weeks.
1.5 Heterogeneity
Data were homogeneous. We did not detect clinical, methodological or statistical heterogeneity as described in Assessment of heterogeneity.
1.6 Sensitivity analyses
1.6.1 Implication of randomisation
We aimed to include trials in a sensitivity analysis if they were described in some way as to imply randomisation. As both studies stated that they randomised participants, we have not undertaken this sensitivity analysis.
1.6.2 Assumptions for lost binary data
At the time of updating this review, we were unable to compare the findings with completer data only, as the previous review authors held data received from study authors.
1.6.3 Risk of bias
We judged both studies in this comparison to be at high risk of bias across one or more domains. Therefore, we were unable to perform a sensitivity analysis in this instance.
1.6.4 Imputed values
We would have undertaken a sensitivity analysis to assess the effects of including data from cluster‐randomised trials where we used imputed values for ICC in calculating the design effect, however, no cluster‐randomised trials were included in this comparison.
1.6.5 Fixed‐effect and random‐effects models
We also synthesised data for the primary outcome using a random‐effects model. This did not alter the significance of the results (2 RCTs, 17 people, RR 0.43, 95% CI 0.17 to 1.08).
Comparison 2. Switch to a specific antipsychotic versus placebo (cessation of antipsychotic)
2.1 TD symptoms
2.1.1 No clinically important improvement*
One study found a benefit in favour of antipsychotics against placebo for clinically important improvement in TD symptoms at 12 weeks (low‐quality evidence, 1 RCT, 42 people, RR 0.45 95% CI 0.23 to 0.89, Analysis 2.1).
2.1.2 Average difference in severity of TD at the end of the trial
TD symptoms were also measured using the continuous AIMS scale (see Description of studies, Outcomes). One study found a beneficial effect of antipsychotics when comparing average endpoint scores of the AIMS to placebo at 12 weeks (very low‐quality evidence, 1 RCT, 42 people, MD ‐5.50 95% CI ‐8.60 to ‐2.40, Analysis 2.2).
2.2 General mental state
2.2.1 Average difference in severity of psychiatric symptoms at the end of the trial
General mental state was measured using the continuous BPRS scale (see Description of studies, Outcomes). One study found no difference between antipsychotics and placebo on average endpoint score of the BPRS at 12 weeks (1 RCT, 42 people, MD ‐4.30 95% CI ‐10.48 to 1.88, Analysis 2.3).
2.3 Acceptability of the treatment: leaving the study early
Using antipsychotics did not significantly increase the chances of a person leaving the study early at 12 weeks (very low‐quality evidence, 1 RCT, 50 people, RR 0.60 95% CI 0.16 to 2.25, Analysis 2.4).
2.4 Adverse effects
2.4.1 Extrapyramidal symptoms*: need of antiparkinsonism drugs
We found no difference in the use of antiparkinsonism drugs between antipsychotic and placebo at 12 weeks (1 RCT, 48 people, RR 2.08 95% CI 0.74 to 5.86, Analysis 2.5).
2.4.2 Average change in extrapyramidal adverse effects: Parkinsonism
One study measured parkinsonism on the continuous ESRS scale (see above). No difference was found between antipsychotics and placebo at 12 weeks (1 RCT, 42 people, MD ‐0.40 95% CI ‐1.25 to 0.45, Analysis 2.6).
2.4.3 Average change in extrapyramidal adverse effects: Dystonia
One study measured dystonia using the continuous ESRS scale. No difference was found between those allocated to antipsychotics or placebo at 12 weeks (1 RCT, 42 people, MD ‐0.70 95% CI ‐1.76 to 0.36, Analysis 2.7).
We did not identify any studies that reported on hospital and service utilisation outcomes, economic outcomes, social confidence, social inclusion, social networks, personalised quality of life, behaviour, or cognitive state.
We also did not identify any studies that investigated the effect on TD of antipsychotic cessation compared with antipsychotic maintenance.
2.5 Subgroup and sensitivity analyses
There was only one included study in this comparison, and this study did not report on subgroups. Consequently, subgroup and sensitivity analyses were not carried out.
Comparison 3. Switch to a specific antipsychotic versus switch to another specific antipsychotic
3.1 TD symptoms
3.1.1 No clinically important improvement*
None of the four studies that reported on this outcome found a clinically important difference on improvement in TD symptoms between two specific antipsychotics (Analysis 3.1): short‐term: thiopropazate versus haloperidol (low‐quality evidence, 1 RCT, 20 people, RR 1.53, 95% CI 0.58 to 4.05), zuclopenthixol versus haloperidol (low‐quality evidence, 1 RCT, 15 people, RR 1.00, 95% CI 0.79 to 1.27); medium‐term: olanzapine versus risperidone (low‐quality evidence, 1 RCT, 60 people, RR 1.25, 95% CI 0.82 to 1.90), quetiapine versus haloperidol (low‐quality evidence, 1 RCT, 45 people, RR 0.80, 95% CI 0.52 to 1.22); long‐term: quetiapine versus haloperidol (low‐quality evidence, 1 RCT, 45 people, RR 0.88, 95% CI 0.64 to 1.21).
3.1.2 Not any improvement
Neither of the two studies that reported on any improvement of TD symptoms found a difference between two specific antipsychotics (Analysis 3.2): short‐term: thiopropazate versus haloperidol (low‐quality evidence, 1 RCT, 20 people, RR 0.41, 95% CI 0.05 to 3.28), zuclopenthixol versus haloperidol (low‐quality evidence, 1 RCT, 15 people, RR 0.88, 95% CI 0.16 to 4.68).
3.1.3 Deterioration of symptoms
Neither of the two studies that reported on deterioration of TD symptoms found a difference between two specific antipsychotics (Analysis 3.3): short‐term: thiopropazate versus haloperidol (low‐quality evidence, 1 RCT, 20 people, RR 1.22, 95% CI 0.09 to 16.92), zuclopenthixol versus haloperidol (low‐quality evidence, 1 RCT, 15 people, RR 0.88, 95% CI 0.16 to 4.68).
3.1.2 Average difference in severity of TD at the end of the trial
A short‐term (two weeks) study of people with established withdrawal‐exacerbated TD found no difference on endpoint AIMS scores after the first week (1 RCT, 18 people, MD 1.87, 95% CI ‐0.20 to 3.94) for the groups receiving molindone or haloperidol at the standard dosage range. Results for the second week, using higher 'masking' dosages, significantly favoured the haloperidol group (1 RCT, 18 people, MD 3.44, 95% CI 1.12 to 5.76). Another short‐term study comparing zuclopenthixol and haloperidol found no difference between groups on endpoint SHRS scores (1 RCT, 15 people, MD ‐4.81, 95% CI ‐12.15 to 2.53). Finally, a medium‐term study found no difference between olanzapine and risperidone on endpoint AIMS scores (1 RCT, 60 people, MD 2.20, 95% CI ‐0.53 to 4.93). See Analysis 3.4.
3.1.4 Average change in severity of TD during the trial period
One study found amisulpride favourable to olanzapine in reducing TD symptoms measured by AIMS change from baseline scores at medium term (1 RCT, 54 people, MD 2.48, 95% CI 0.44 to 4.52). Three other comparisons found no difference between specific antipsychotics at medium term: olanzapine versus unspecified FGAs (1 RCT, 53 people, MD 1.66, 95% CI ‐0.45 to 3.77), amisulpride vs unspecified FGAs (1 RCT, 53 people, MD ‐0.82, 95% CI ‐2.85 to 1.21), and olanzapine vs risperidone (1 RCT, 60 people, MD 1.20, 95% CI ‐2.58 to 4.98, Analysis 3.5).
3.2 General mental state
3.2.1 Deterioration of mental state
No difference was found in the proportion with deterioration of mental state between specific antipsychotics: zuclopenthixol versus haloperidol at short term (1 RCT, 15 people, RR 0.30, 95% CI 0.01 to 6.29), olanzapine versus risperidone at medium term (1 RCT, 60 people, RR 1.00, 95% CI 0.15 to 6.64), quetiapine versus haloperidol at long term (1 RCT, 45 people, RR 1.83, 95% CI 0.62 to 5.39, Analysis 3.6).
3.2.2 Average difference in severity of psychiatric symptoms at the end of the trial
No difference was found in average endpoint scores of the PANSS between quetiapine and haloperidol at long term (1 RCT, 45 people, MD ‐2.20, 95% CI ‐6.02 to 1.62, Analysis 3.7).
3.2.3 Average change in severity of psychiatric symptoms during the trial period
There was also no difference on the average endpoint scores on the BPRS between specific antipsychotics at medium term: olanzapine versus unspecified FGAs (1 RCT, 53 people, MD ‐1.14, 95% CI ‐4.79 to 2.51), amisulpride versus unspecified FGAs (1 RCT, 53 people, MD ‐2.46, 95% CI ‐6.27 to 1.35), olanzapine versus risperidone (1 RCT, 60 people, MD ‐1.70, 95% CI ‐8.37 to 4.97), and olanzapine versus amisulpride (1 RCT, 54 people, MD 1.32, 95% CI ‐1.94 to 4.58, Analysis 3.8).
3.3 Acceptability of the treatment: leaving the study early
In the short term, a specific antipsychotic did not significantly increase the chances of a person leaving the study early compared with another specific antipsychotic: molindone versus haloperidol (1 RCT, 18 people, MD not estimable, there were no events), thiopropazate versus haloperidol (1 RCT, 20 people, MD 0.24, 95% CI 0.01 to 4.44, Analysis 3.9). In the medium term, switching to olanzapine significantly reduced the chances of a person leaving the study early compared with switching to risperidone (2 RCTs, 170 people, RR 0.73 95% CI 0.57 to 0.95, I2 = 0, Analysis 3.10) or compared with switching to quetiapine (1 RCT, 116 people, RR 0.70 95% CI 0.54 to 0.90). For all other comparisons between specific antipsychotics at medium term, there was no difference in the chances of a person leaving the study early: olanzapine versus unspecified FGAs (1 RCT, 56 people, RR 1.86, 95% CI 0.18 to 19.38), amisulpride versus unspecified FGAs (1 RCT, 55 people, RR 0.96, 95% CI 0.06 to 14.65), olanzapine versus amisulpride (1 RCT, 57 people, RR 1.93, 95% CI 0.19 to 20.12), olanzapine versus ziprasidone (1 RCT, 82 people, RR 0.77, 95% CI 0.56 to 1.05), quetiapine versus risperidone (1 RCT, 118 people, RR 1.05, 95% CI 0.88 to 1.25), quetiapine versus ziprasidone (1 RCT, 90 people, RR 1.10, 95% CI 0.86 to 1.40), ziprasidone versus risperidone (1 RCT, 84 people, RR 0.95, 95% CI 0.74 to 1.23). Finally, in the long term, there was no difference between clozapine and haloperidol (1 RCT, 39 people, RR 3.36, 95% CI 0.45 to 25.16), or between quetiapine and haloperidol on the number leaving the study early (1 RCT, 45 people, RR 1.31, 95% CI 0.63 to 2.69, see Analysis 3.11).
3.4 Adverse events
3.4.1 Extrapyramidal symptoms*: need of antiparkinsonism drugs
A study comparing risperidone and haloperidol found no difference between groups at medium term (1 RCT, 37 people, RR 0.68, 95% CI 0.34 to 1.35, Analysis 3.12). Another study found that participants allocated to haloperidol were more likely to need antiparkinsonism drugs than those allocated to quetiapine in the long term (1 RCT, 45 people, RR 0.45, 95% CI 0.21 to 2.96, Analysis 3.12).
3.4.2 Average change in extrapyramidal adverse effects: Parkinsonism
Symptoms of parkinsonism were measured using the continuous SAS, SHRS, and ESRS scales (see Description of studies, Outcomes). At short term, one study found no difference in parkinsonism symptoms measured by SHRS endpoint scores between zuclopenthixol and haloperidol (1 RCT, 15 people, MD ‐4.81, 95% CI ‐12.15 to 2.53, Analysis 3.13). One study found those allocated to olanzapine were less likely to develop symptoms of parkinsonism than those allocated to risperidone measured by ESRS change scores at medium term (1 RCT, 60 people, MD ‐0.70, 95% CI ‐1.33 to ‐0.07). For all other comparisons between specific antipsychotics at medium term, there was no difference in symptoms of parkinsonism as measured by average change scores: olanzapine versus unspecified FGAs (1 RCT, 53 people, MD ‐0.85, 95% CI ‐2.55 to 0.85), amisulpride versus unspecified FGAs (1 RCT, 53 people, MD ‐0.50, 95% CI ‐2.45 to 1.45), and olanzapine versus amisulpride (1 RCT, 54 people, MD ‐0.35, 95% CI ‐2.44 to 1.74, Analysis 3.14).
3.4.3 Average change in extrapyramidal adverse effects: Dyskinesia
Symptoms of dyskinesia were measured using the continuous ESRS scale. There was no difference in symptoms of dyskinesia between those switching to olanzapine and those switching to risperidone (1 RCT, 60 people, MD 0.30, 95% CI ‐0.91 to 1.51, Analysis 3.15).
3.4.4 Average change in extrapyramidal adverse effects: Akathisia
Symptoms of akathisia were measured using the continuous BAS and ESRS scales (see Description of studies, Outcomes, Analysis 3.16). There was no difference in symptoms of akathisia for those switching to olanzapine (1 RCT, 53 people, MD 0.08 95% CI ‐0.30 to 0.46) or amisulpride (1 RCT, 53 people, MD ‐0.11 95% CI ‐0.42 to 0.20) compared with those remaining on unspecified FGAs. There was also no difference for those switching to olanzapine compared with those switching to risperidone (1 RCT, 60 people, MD ‐0.80 95% CI ‐1.76 to 0.16) or amisulpride (1 RCT, 54 people, MD 0.19 95% CI ‐0.12 to 0.50).
3.4.5 Average change in extrapyramidal adverse effects: Dystonia
Symptoms of dystonia were measured using the continuous ESRS scale. There was no difference in symptoms of dystonia in those switching to olanzapine compared with those switching to risperidone (1 RCT, 60 people, MD ‐0.70 95% CI ‐1.41 to 0.01, Analysis 3.17).
3.4.6 Average change in general adverse events
General adverse events were measured using the continuous UKU scale (see Description of studies, Outcomes, Analysis 3.18). There was no difference in general adverse events for those switching to olanzapine (1 RCT, 53 people, MD 0.08 95% CI ‐1.85 to 2.01) or amisulpride (1 RCT, 53 people, MD ‐0.55 95% CI ‐2.33 to 1.23) compared with those remaining on unspecified FGAs. There was also no difference for those switching to olanzapine compared with those switching to amisulpride (1 RCT, 54 people, MD 0.63 95% CI ‐0.93 to 2.19).
3.5 Global state
3.5.1 Average change in global state
Global state was measured using the continuous CGI scale (see Description of studies, Outcomes, Analysis 3.19). There was no difference in change scores of global state in those switching to olanzapine (1 RCT, 53 people, MD ‐0.07 95% CI ‐0.41 to 0.27) or amisulpride (1 RCT, 53 people, MD ‐0.19 95% CI ‐0.47 to 0.09) compared with those remaining on FGA. There was also no difference in those switching to olanzapine compared with those switching to risperidone (1 RCT, 60 people, MD 0.10 95% CI ‐0.61 to 0.81) or amisulpride (1 RCT, 54 people, MD 0.12 95% CI ‐0.19 to 0.43).
We did not identify any studies that reported on hospital and service utilisation outcomes, economic outcomes, social confidence, social inclusion, social networks, personalised quality of life, behaviour, or cognitive state.
3.6 Subgroup and sensitivity analyses
There were no meta‐analyses for the primary outcomes of this comparison because studies were stratified by antipsychotic medication. Consequently, we did not carry out subgroup and sensitivity analyses.
Comparison 4. Specific antipsychotic versus other drug
4.1 TD symptoms
4.1.1 No clinically important improvement*
One study found no difference between haloperidol and tetrabenazine for clinically important improvement in TD symptoms at 24 weeks (very low‐quality evidence, 1 RCT, 13 people, RR 1.07 95% CI 0.51 to 2.23, Analysis 4.1).
4.1.2 Not any improvement
One study found no difference between haloperidol and tetrabenazine for the outcome 'no improvement in TD symptoms' at 24 weeks (1 RCT, 13 people, RR 2.57 95% CI 0.35 to 18.68, Analysis 4.2).
4.1.3 Deterioration of symptoms
One study found no difference on deterioration of TD symptoms between haloperidol and tetrabenazine at 24 weeks (very low‐quality evidence, 1 RCT, 13 people, RR 0.86 95% CI 0.07 to 10.96, Analysis 4.3).
4.2 Acceptability of the treatment: leaving the study early
One study found no difference in the proportion of people leaving the study early between haloperidol and tetrabenazine at 24 weeks (very low quality‐evidence, 1 RCT, 13 people, RR 4.38 95% CI 0.25 to 76.54, Analysis 4.4).
We did not identify any studies that reported on mental state, adverse events, hospital and service utilisation outcomes, economic outcomes, social confidence, social inclusion, social networks, personalised quality of life, behaviour, or cognitive state.
4.3 Subgroup and sensitivity analyses
There was only one included study in this comparison, and this study did not report on subgroups. Consequently, we did not carry out subgroup and sensitivity analyses.
Discussion
Summary of main results
1. The search
This area of research does not seem to be active. We have identified additional data, but most trials predate the year 2000; only three were carried out after, published in 2004 to 2011. This could be due to a decreased concern with TD, or less emergence of the problem in research‐active communities because of more thoughtful use of antipsychotic drugs or loss of faith in potential treatments.
2. Few data
Only a little over 700 people were included in this review. It is possible that real and important effects have not been highlighted because of the necessarily wide CIs of the findings. Many outcomes were not measured at all by the included studies (see Overall completeness and applicability of evidence), including one of our outcome measures that was selected as important. We may have been overambitious in hoping for some of these outcomes in TD trials, but simple reporting of social impact and quality of life is of particular interest to patients and carers. Finally, we did not identify any RCTs of participants with TD that compared antipsychotic cessation with antipsychotic maintenance.
3. Outcomes
3.1 Tardive dyskinesia symptoms
We found low‐quality evidence of clinically important improvement in TD symptoms for switching antipsychotic to risperidone compared with antipsychotic cessation (with placebo) after 12 weeks (RR 0.45, 95% CI 0.23 to 0.89, 1 study, 42 participants). Because the quality of the evidence is low, we have limited confidence in the effect estimates and CIs; the true effects may be substantially different.
For the remaining comparisons: antipsychotic reduction versus maintenance, switch to a new antipsychotic versus switch to a different new antipsychotic, and specific antipsychotic versus other drug, we found low to very low‐quality evidence of little or no difference between groups for no clinically important improvement in TD symptoms and deterioration of TD symptoms, but again, our confidence in these results is limited due to the poor‐quality evidence, not least because there were few participants (13 to 60 participants per comparison).
3.2 Adverse effects
There was low‐quality evidence of fewer people that needed antiparkinsonism medication due to extrapyramidal side effects after switching to quetiapine compared with haloperidol after one year (RR 0.45, 95% CI 0.21 to 0.96, 1 study, 45 participants). Due to the low quality of this evidence, our confidence in these results is limited. For the other comparisons, switch to haloperidol or risperidone versus antipsychotic cessation, and risperidone versus haloperidol, we found very low‐quality evidence of little or no difference between groups. Therefore, we are very uncertain about these results, not least because there were few participants (37 and 48 participants per comparison).
3.3 Mental state
We found low‐ to very low‐quality evidence of little or no difference in mental state: relapse, deterioration of mental state, or average endpoint scores on scales measuring mental state, between groups of the following comparisons: antipsychotic reduction versus maintenance, switch to risperidone versus antipsychotic cessation, switch to zuclopenthixol versus haloperidol, switch to olanzapine versus risperidone, and switch to quetiapine versus haloperidol. Again, our confidence in these results is limited due to the poor quality of evidence, not least because there were few participants (8 to 60 participants per comparison).
3.4 Acceptability of treatment: leaving the study early
It is always unclear what leaving a study early means. It could be related to the participant not accepting treatment for a series of reasons, or to participants finding the trial intolerable. It also could be a function of a trial design in which willing participants are still asked to leave because of some degree of protocol violation.
There was very low‐quality evidence for most of the comparisons that the number of participants leaving the study early was no different in either group. The small number of people randomised in these comparisons (8 to 170 participants) made the likelihood of an unequivocal outcome unlikely. However, we found very low‐quality evidence that fewer participants allocated to olanzapine left the study early compared with risperidone and compared with quetiapine. Since evidence was of very low quality for both comparisons, we have very little confidence in the effect estimates and CIs; the true effects are likely to be substantially different.
3.5 Social confidence, social inclusion, social networks, or personalised quality of life
We selected this group of outcomes for the 2017 review update following a service‐user consultation, as being of importance to patients. We did not identify any studies that reported on any of these outcomes.
Overall completeness and applicability of evidence
1. Completeness
No outcomes in this review involved large numbers of people. There is a large literature of trials assessing the impact of antipsychotic reduction or cessation, or both, on outcomes such as symptoms and relapse. Much of the initial impetus for these trials was derived from concerns about antipsychotic‐induced TD. It was disappointing to note that many of these trials did not systematically assess TD, and thus were not suitable for inclusion in this review. While many trials of antipsychotic reduction and/or cessation assess TD, the baseline and endpoint means are rarely presented for those with TD at baseline. Two authors (Cookson 1987; Kane 1983) kindly provided raw data from which we could extract the impact of antipsychotic reduction on those with TD at baseline. The very small sample size limits the confidence that one can place on the equivocal results.
Post hoc analyses of the main efficacy and safety analyses for the newer atypicals have also been undertaken (for example, Caroff 2011 and Chouinard 1995). The analyses of results from these trials need to be interpreted with caution for several reasons: (a) suboptimal design for the assessment of treatment of TD (for example, pre‐entry washout or gradual conversion to study drug); (b) the analyses were post hoc; and (c) differences in results between different arms in the studies may reflect antipsychotic suppression due to differing dosing strategies.
There were no data on the patient‐designated important outcomes social confidence, social inclusion, social networks, or personalised quality of life, nor were there data on hospital and service utilisation outcomes, economic outcomes, behaviour or cognitive response.
2. Applicability
Trial participants were mostly men in their 50s with schizophrenia in hospital, but were nevertheless people who would be recognisable in everyday care.
Reducing or stopping antipsychotic medication may not be clinically prudent in some situations. The current lack of evidence showing any improvement in TD with such strategies means that clinicians may be less inclined to use them in mentally stable patients. On the other hand, high‐quality evidence in this area would be very useful and applicable in everyday clinical practice to aid in the decision making around the risk and benefits of reducing or stopping antipsychotic medication following the emergence of TD.
Quality of the evidence
Overall, the quality of the evidence is low to very low. This means that we have limited to very little confidence in the effect estimates, and the true effect may be, or is likely to be, substantially different from the estimate of the effect. The main reasons for our low confidence in the evidence were:
-
poor study methodology and reporting of methods resulting in downgrading evidence for risk of bias;
-
very small sample sizes resulting in downgrading evidence for imprecision;
-
wide CIs (often due to low event rates) that included appreciable benefit or harm for the intervention as well as no effect, resulting in downgrading evidence for imprecision.
Please see summary of findings Table for the main comparison; summary of findings Table 2; summary of findings Table 3; summary of findings Table 4; summary of findings Table 5 for full details.
Potential biases in the review process
1. Missing studies
Every effort was made to identify relevant trials. However, these studies were all small and it is likely that we have failed to identify other studies of limited power. We do not, however, think it likely that we have failed to identify large relevant studies.
2. Missing data
We excluded 14 studies published between 1971 and 1998 that did not provide any usable data, see Excluded studies. We contacted study authors and six replied to confirm no usable data were available. Authors of three studies did not reply, and we could not find up‐to‐date contact details for authors of five studies (all over 25 years old). We find it very unlikely that we would receive a reply from study authors regarding research conducted so many years ago; therefore, we also excluded these studies.
3. Introducing bias
We have tried to be balanced in our appraisal of the evidence but could have inadvertently introduced bias. We welcome comments or criticisms. New methods and innovations now make it possible to report data where, in the past, we could not report data at all or had to report data in a different way. We believe the 'Summary of findings' tables are a valuable innovation – but problematic to those not ‘blind’ to the outcome data. It is possible to ‘cherry pick’ significant findings for presentation in this table. We have tried to decrease the chance of doing this by asking a new reviewer (HB) to select outcomes relevant for this table before becoming familiar with the data.
Agreements and disagreements with other studies or reviews
While the reduction or cessation, or both, of antipsychotics appears a rational first line of treatment for TD, the evidence from systematic reviews such as Gilbert 1995 highlights the very high risk of relapse associated with both antipsychotic cessation and antipsychotic reduction. In addition, there is evidence from the literature that intermittent therapy may be associated with more unfavourable TD outcomes (higher scores, fewer eventual remissions etc.) (Bergin 1992; Jeste 1979; NDSG 1986).
It is of interest to note that naturalistic studies suggest that TD fluctuates over time, and often improves in spite of continuing antipsychotic exposure (Casey 1986). Kane 1986 analysed data on 98 people followed up for at least seven years and reported that those on lower doses of antipsychotics were more likely to have an improvement in their TD. Gardos 1988 reported that improvement in TD was associated with lower antipsychotic doses after TD onset. Using a sophisticated epidemiological approach, Morgenstern 1993 looked at risk factors for new cases of TD. Higher average antipsychotic medication was associated with an increased risk of developing persistent TD. However, Cavallaro 1993 assessed TD prognosis (persistent, remitting etc) with respect to antipsychotic dose change (decreased, increased, unchanged) in 125 inpatients followed up for three years. They found no significant association between antipsychotic reduction and improved TD outcome. As with all uncontrolled studies, these data need to be interpreted cautiously, because those who have less responsive psychoses may require higher doses and have higher rates of TD regardless of treatment.
Also of note, in more recent years commentators are more likely to concede that no change in antipsychotic medications may be required for those with TD (Gardos 1994). Casey 1986 suggested, "therefore, antipsychotics in low to moderate doses are not contra‐indicated in patients with psychosis and will not inevitably aggravate TD" (p. 89). There is some evidence to suggest that younger people (under 60 years) who develop TD are three times more likely to recover when compared with those who develop TD after that age (Smith 1980). One interpretation of the data would suggest that, for younger people who develop TD that is not associated with significant impairment, no change to treatment is required other than regular monitoring and reassurance.
Message from one of the participants of the public and patient involvement consultation of service user perspectives on tardive dyskinesia research
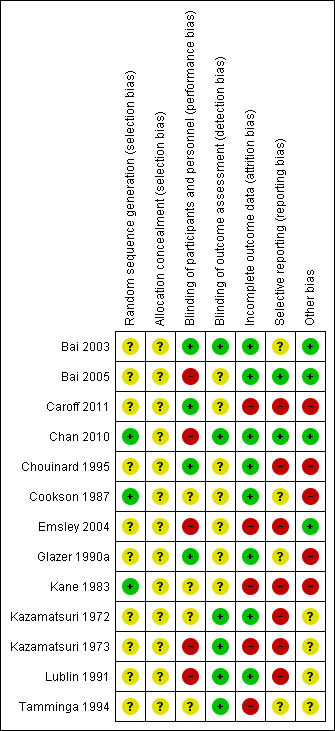
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
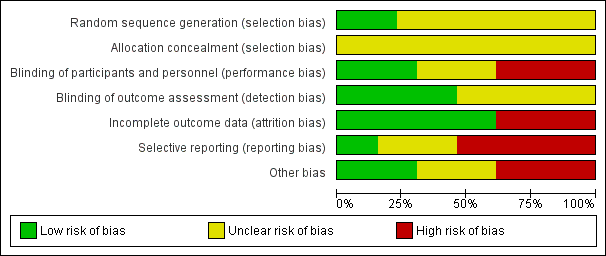
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
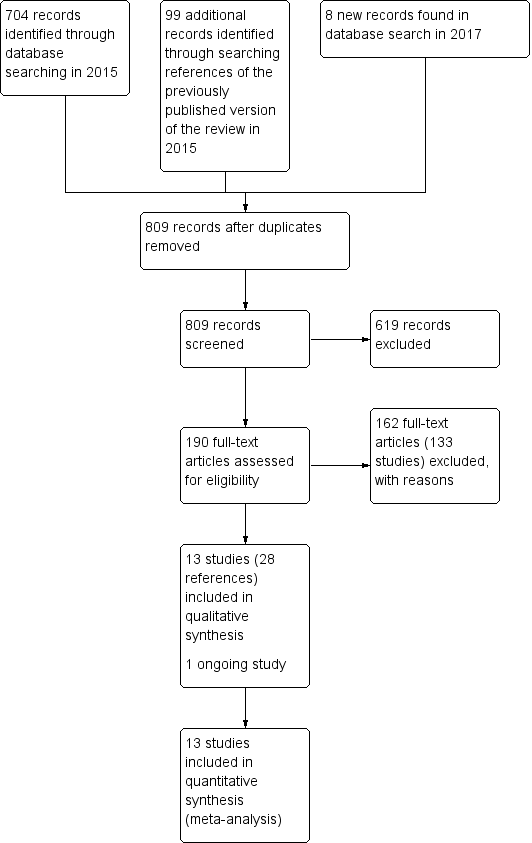
Study flow diagram for 2015 and 2017 searches for this review
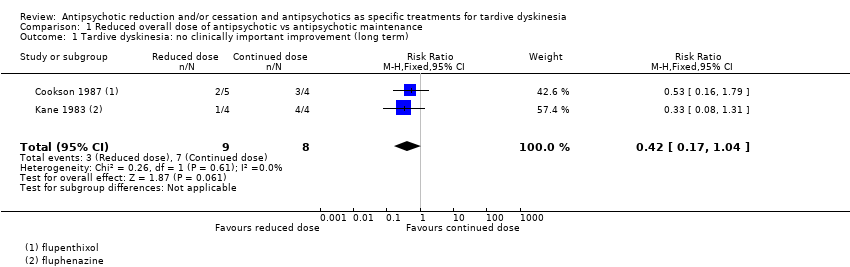
Comparison 1 Reduced overall dose of antipsychotic vs antipsychotic maintenance, Outcome 1 Tardive dyskinesia: no clinically important improvement (long term).
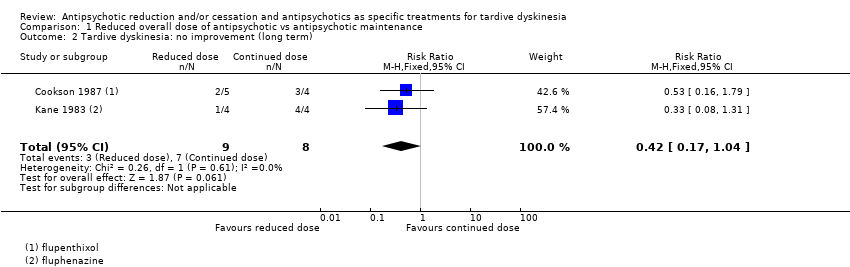
Comparison 1 Reduced overall dose of antipsychotic vs antipsychotic maintenance, Outcome 2 Tardive dyskinesia: no improvement (long term).
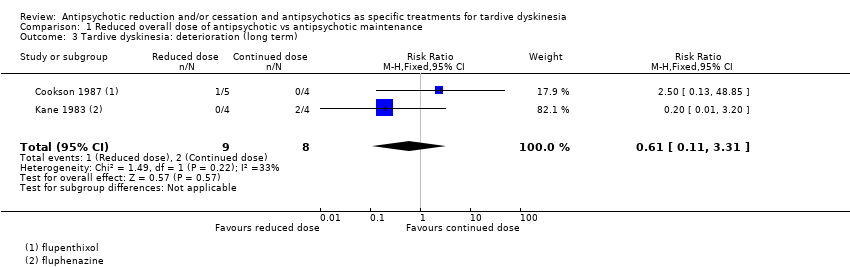
Comparison 1 Reduced overall dose of antipsychotic vs antipsychotic maintenance, Outcome 3 Tardive dyskinesia: deterioration (long term).
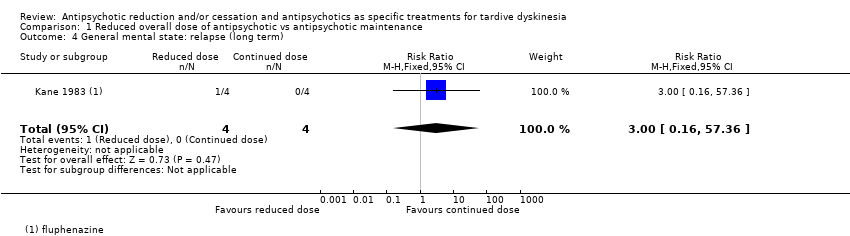
Comparison 1 Reduced overall dose of antipsychotic vs antipsychotic maintenance, Outcome 4 General mental state: relapse (long term).
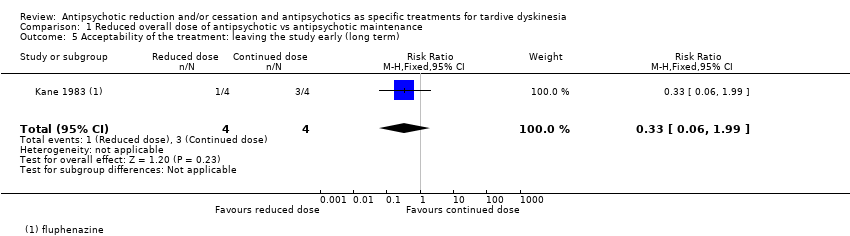
Comparison 1 Reduced overall dose of antipsychotic vs antipsychotic maintenance, Outcome 5 Acceptability of the treatment: leaving the study early (long term).
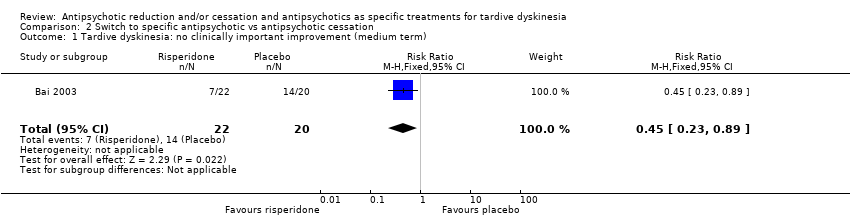
Comparison 2 Switch to specific antipsychotic vs antipsychotic cessation, Outcome 1 Tardive dyskinesia: no clinically important improvement (medium term).
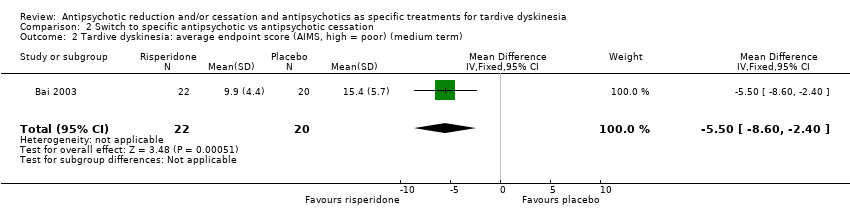
Comparison 2 Switch to specific antipsychotic vs antipsychotic cessation, Outcome 2 Tardive dyskinesia: average endpoint score (AIMS, high = poor) (medium term).
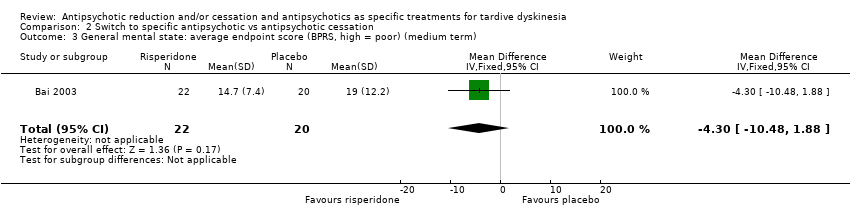
Comparison 2 Switch to specific antipsychotic vs antipsychotic cessation, Outcome 3 General mental state: average endpoint score (BPRS, high = poor) (medium term).
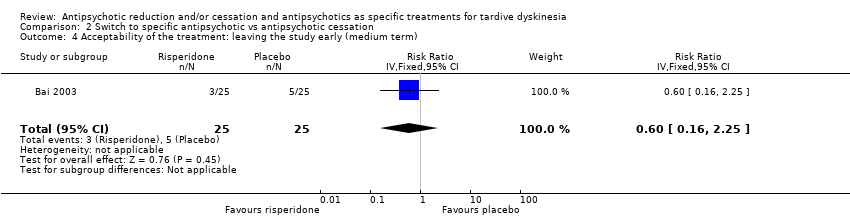
Comparison 2 Switch to specific antipsychotic vs antipsychotic cessation, Outcome 4 Acceptability of the treatment: leaving the study early (medium term).
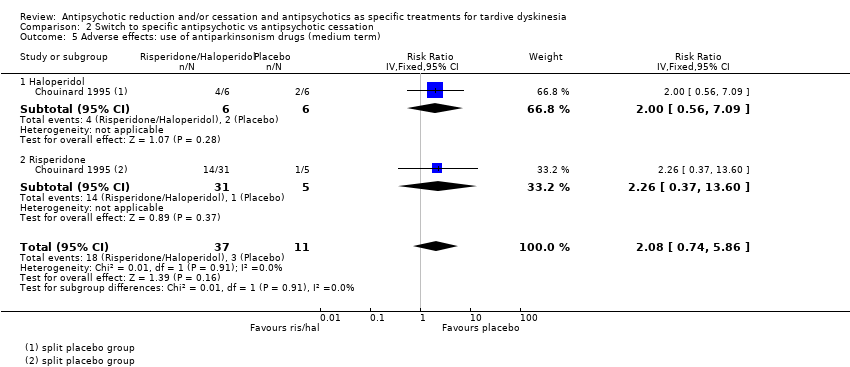
Comparison 2 Switch to specific antipsychotic vs antipsychotic cessation, Outcome 5 Adverse effects: use of antiparkinsonism drugs (medium term).
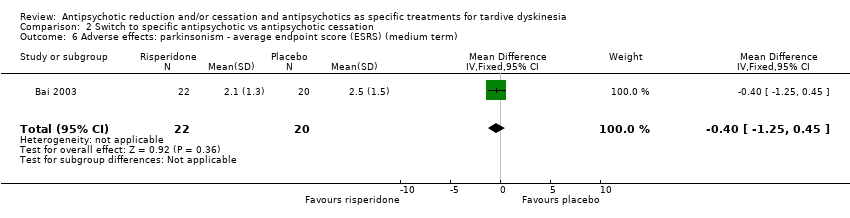
Comparison 2 Switch to specific antipsychotic vs antipsychotic cessation, Outcome 6 Adverse effects: parkinsonism ‐ average endpoint score (ESRS) (medium term).
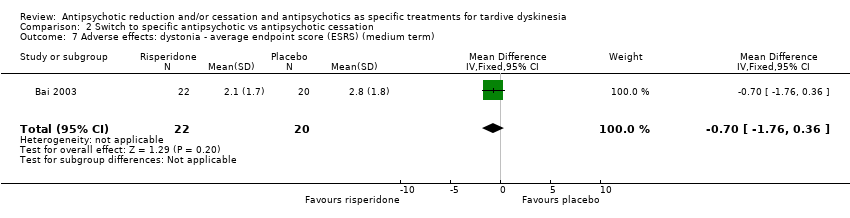
Comparison 2 Switch to specific antipsychotic vs antipsychotic cessation, Outcome 7 Adverse effects: dystonia ‐ average endpoint score (ESRS) (medium term).
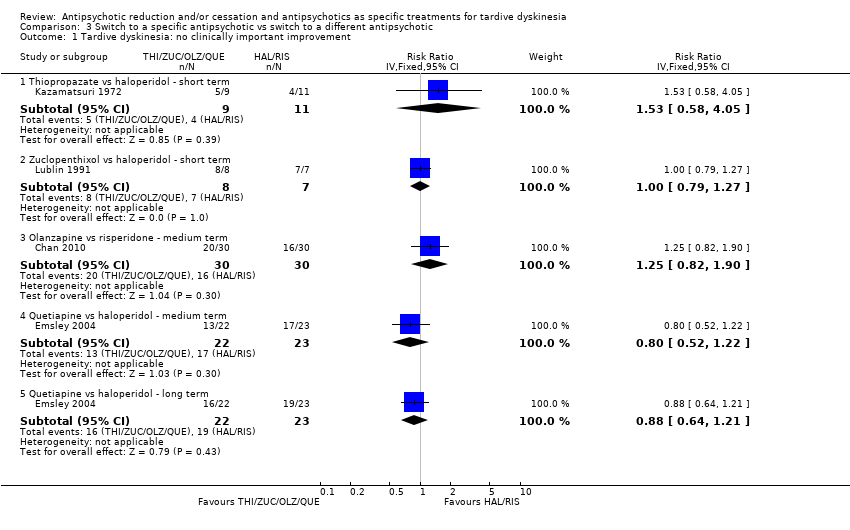
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 1 Tardive dyskinesia: no clinically important improvement.
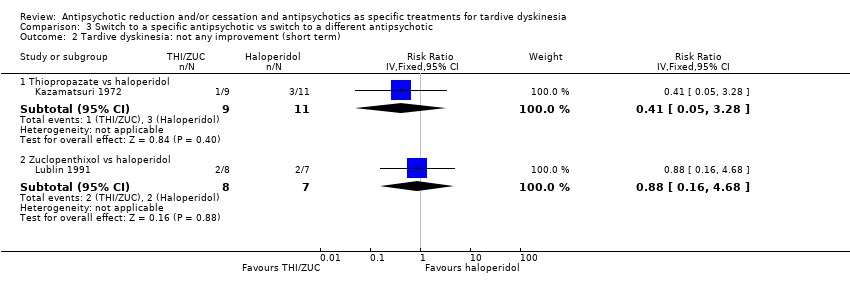
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 2 Tardive dyskinesia: not any improvement (short term).
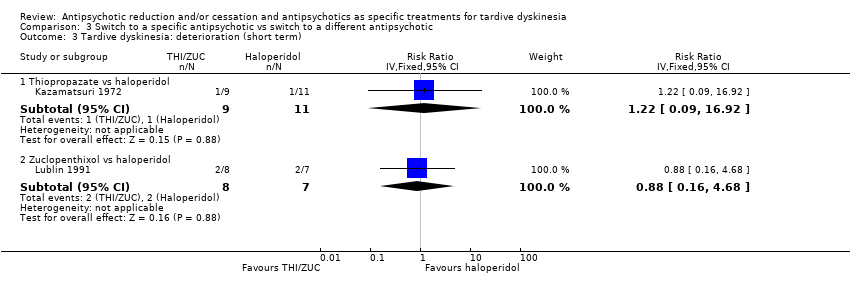
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 3 Tardive dyskinesia: deterioration (short term).
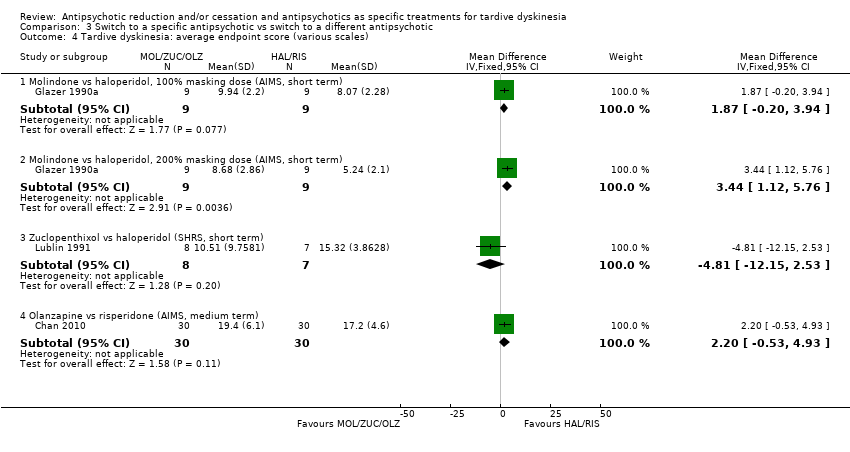
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 4 Tardive dyskinesia: average endpoint score (various scales).
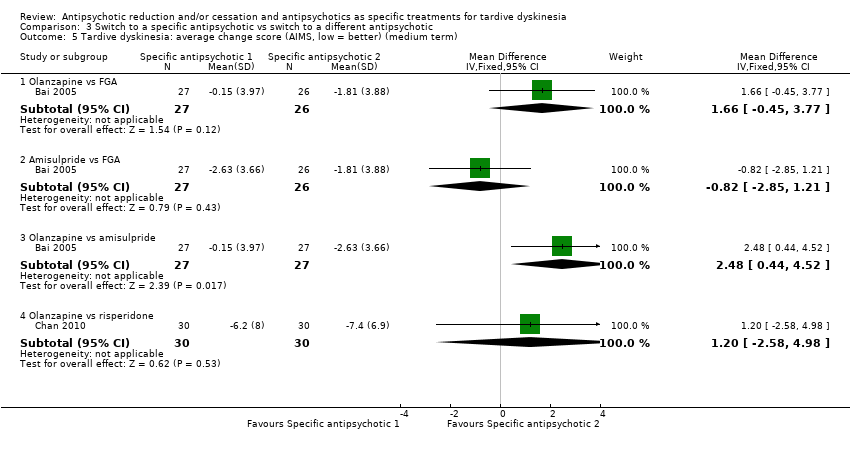
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 5 Tardive dyskinesia: average change score (AIMS, low = better) (medium term).
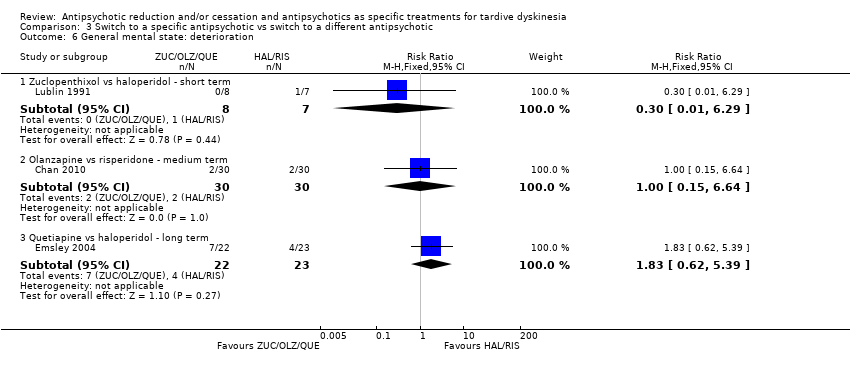
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 6 General mental state: deterioration.
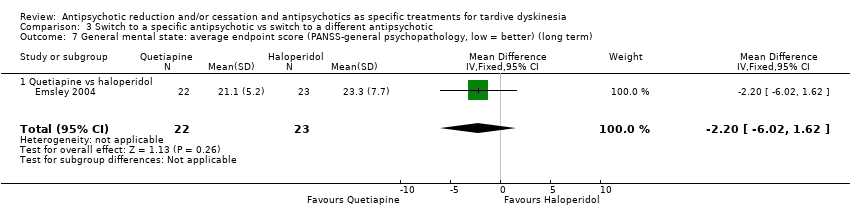
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 7 General mental state: average endpoint score (PANSS‐general psychopathology, low = better) (long term).
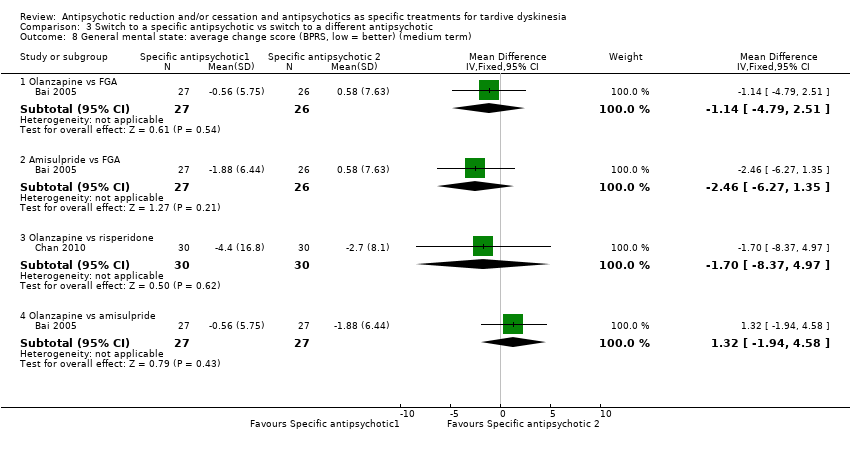
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 8 General mental state: average change score (BPRS, low = better) (medium term).
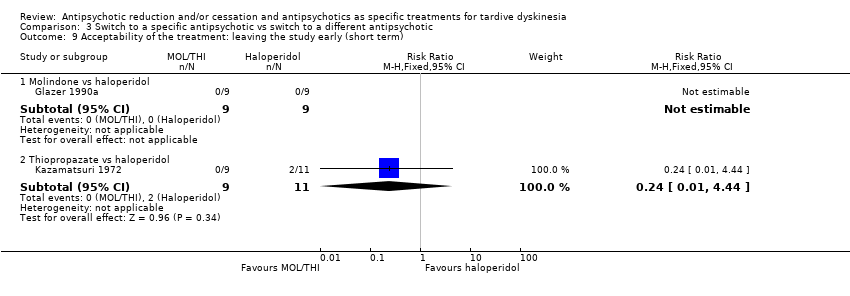
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 9 Acceptability of the treatment: leaving the study early (short term).
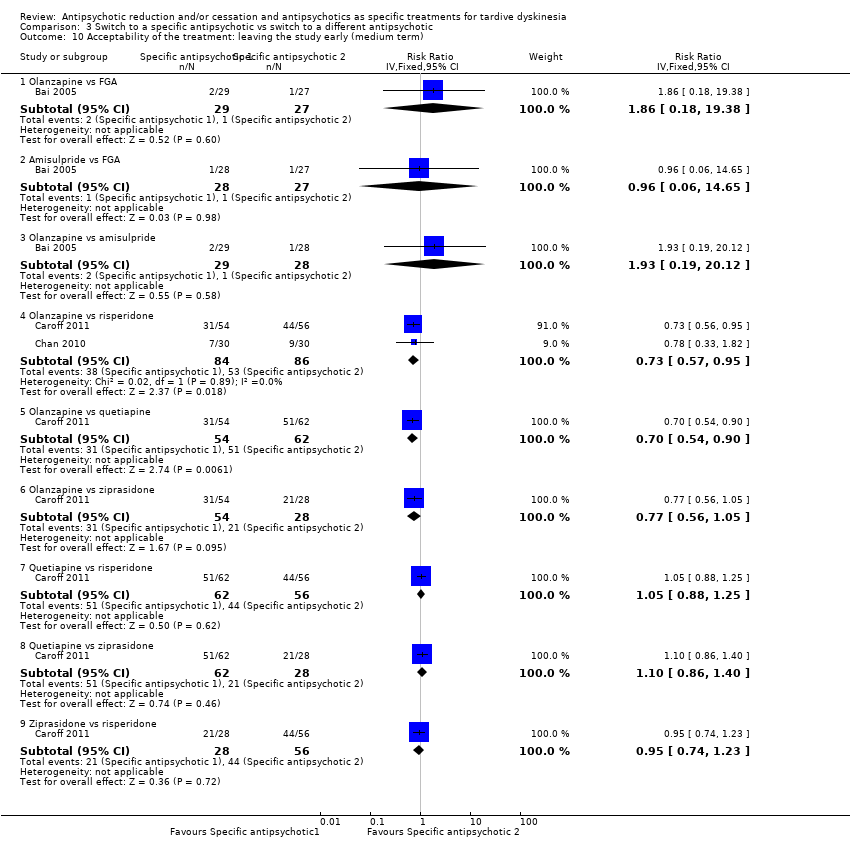
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 10 Acceptability of the treatment: leaving the study early (medium term).
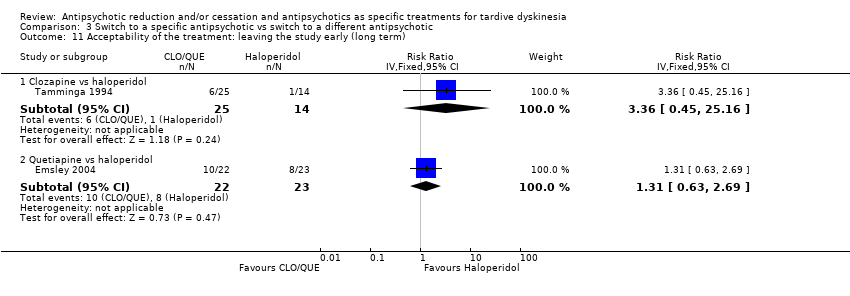
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 11 Acceptability of the treatment: leaving the study early (long term).
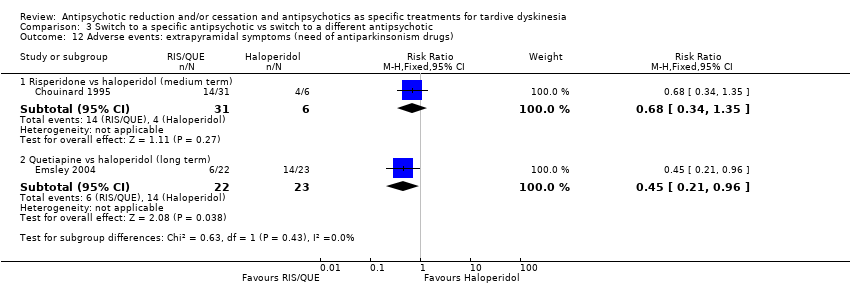
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 12 Adverse events: extrapyramidal symptoms (need of antiparkinsonism drugs).
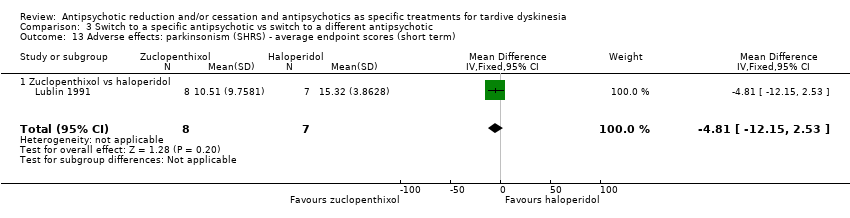
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 13 Adverse effects: parkinsonism (SHRS) ‐ average endpoint scores (short term).
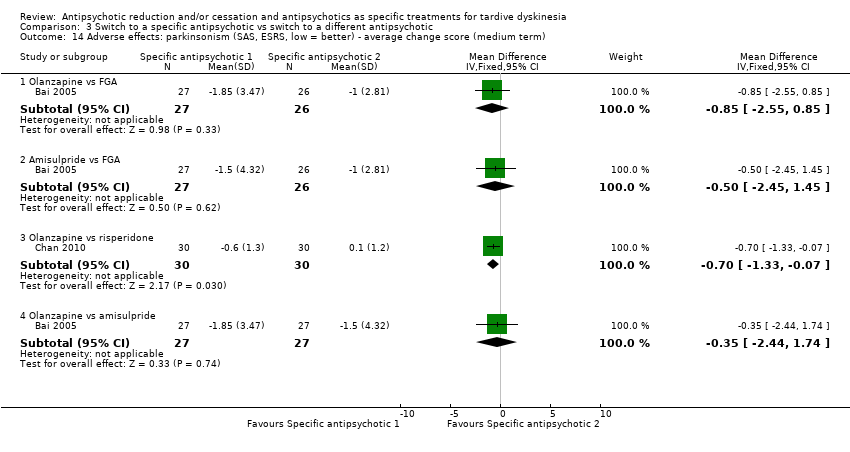
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 14 Adverse effects: parkinsonism (SAS, ESRS, low = better) ‐ average change score (medium term).
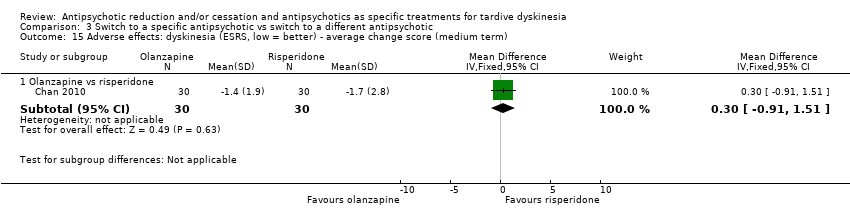
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 15 Adverse effects: dyskinesia (ESRS, low = better) ‐ average change score (medium term).
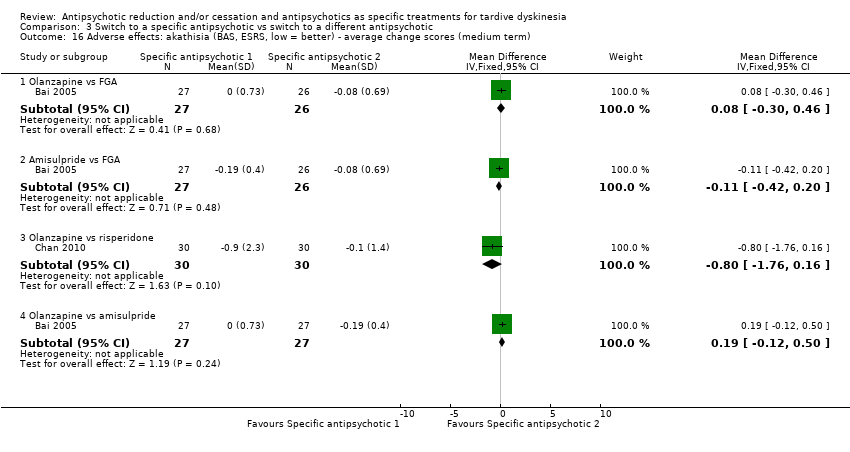
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 16 Adverse effects: akathisia (BAS, ESRS, low = better) ‐ average change scores (medium term).
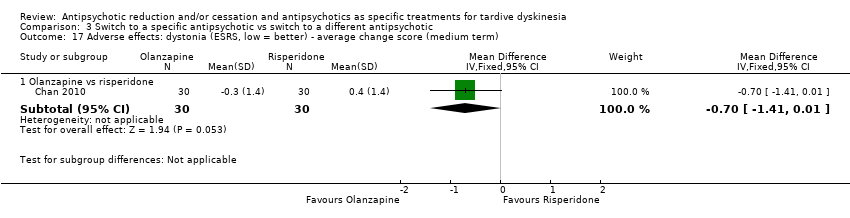
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 17 Adverse effects: dystonia (ESRS, low = better) ‐ average change score (medium term).
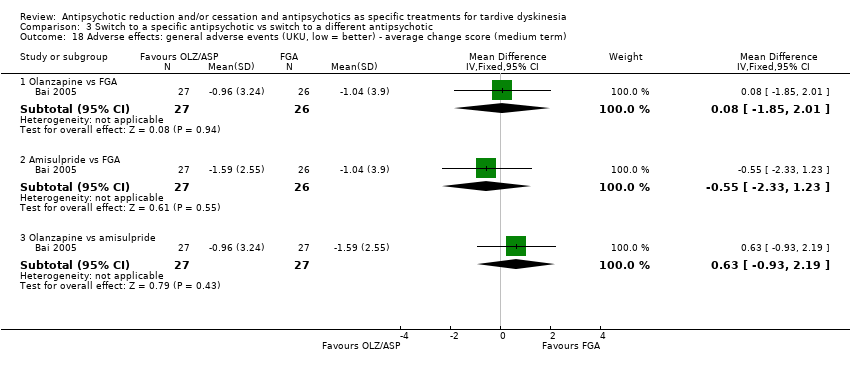
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 18 Adverse effects: general adverse events (UKU, low = better) ‐ average change score (medium term).
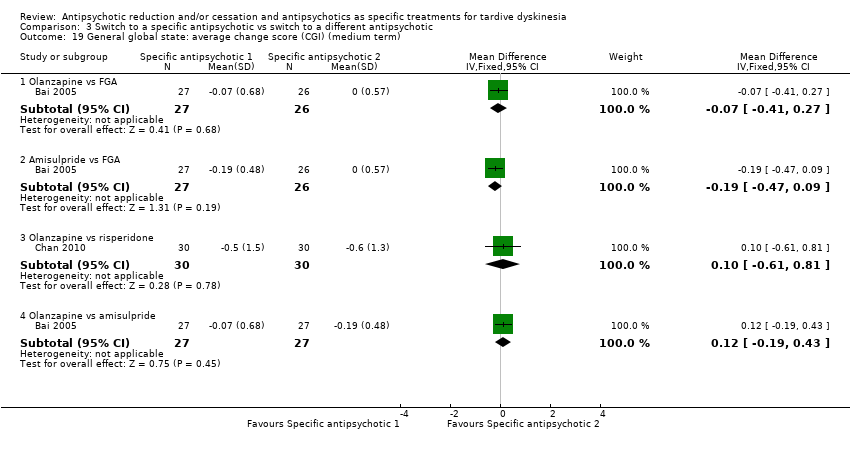
Comparison 3 Switch to a specific antipsychotic vs switch to a different antipsychotic, Outcome 19 General global state: average change score (CGI) (medium term).
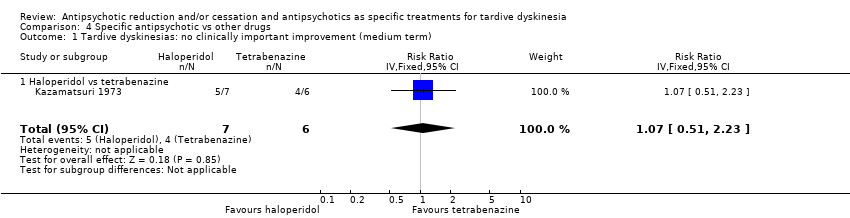
Comparison 4 Specific antipsychotic vs other drugs, Outcome 1 Tardive dyskinesias: no clinically important improvement (medium term).
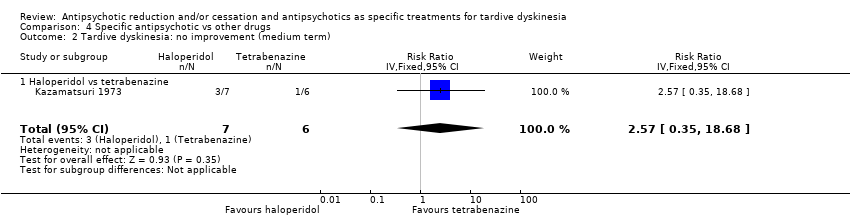
Comparison 4 Specific antipsychotic vs other drugs, Outcome 2 Tardive dyskinesia: no improvement (medium term).
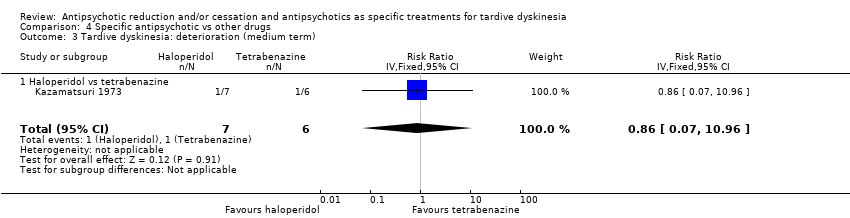
Comparison 4 Specific antipsychotic vs other drugs, Outcome 3 Tardive dyskinesia: deterioration (medium term).
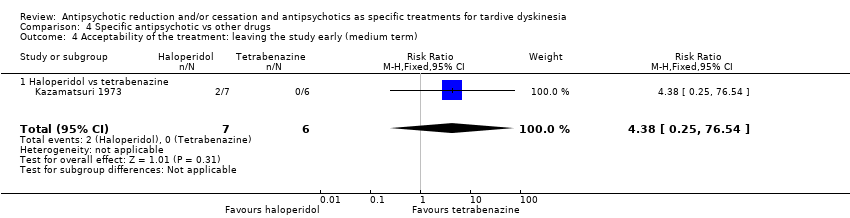
Comparison 4 Specific antipsychotic vs other drugs, Outcome 4 Acceptability of the treatment: leaving the study early (medium term).
| Study ID | Participants – people with: | Intervention | Comparison for review | Cochrane Review |
| Tardive dyskinesia | 1‐stepholidine vs placebo | 1‐stepholidine for schizophrenia | ‐ | |
| Schizophrenia | Amisulpride vs haloperidol | Amisulpride versus haloperidol for schizophrenia | ||
| Tardive dyskinesia | Biperiden vs no treatment | Anticholinergic drugs for tardive dyskinesia | ||
| Chlorprothixene versus haloperidol vs perphenazine vs haloperidol + biperiden | ||||
| Biperiden vs placebo | ||||
| Schizophrenia | Ethopropazine vs benztropine | Anticholinergics for parkinsonism | ||
| Abrupt neuroleptic cessation vs neuroleptic maintenance | Antipsychotic reduction or withdrawal for schizophrenia | |||
| Abrupt neuroleptic cessation vs neuroleptic maintenance | ||||
| Fluphenazine/flupenthixol decanoate continuation vs withdrawal | ||||
| Withdrawal of fluphenazine decanoate vs continuation | ||||
| Trifluoperazine withdrawal vs trifluoperazine continuation | ||||
| Dose reduction vs maintenance (both arms used flupenthixol decanoate) | ||||
| Olanzapine with different timings of dose‐reduction periods | ||||
| Fluphenazine withdrawal vs continuation | ||||
| Low‐ vs conventional‐dose maintenance therapy with fluphenazine decanoate | ||||
| Haloperidol dose reduction vs maintained dose | ||||
| Abrupt neuroleptic cessation vs neuroleptic maintenance | ||||
| Tardive dyskinesia | Flunarizine vs placebo | Calcium channel blockers for neuroleptic‐induced tardive dyskinesia | ||
| Schizophrenia | Chlorpromazine schedule A vs chlorpromazine schedule B | Chlorpromazine timing of dose for schizophrenia. | ||
| Tardive dyskinesia | Chlorprothixene vs haloperidol vs perphenazine vs haloperidol + biperiden | Chlorprothixene for schizophrenia. | ||
| Schizophrenia | Clozapine vs haloperidol | Clozapine versus haloperidol for schizophrenia | ||
| Clozapine vs haloperidol | ||||
| Clozapine vs olanzapine | Clozapine versus olanzapine for schizophrenia | |||
| Clozapine vs olanzapine | ||||
| Gilles de la Tourette's, Huntington's disease and drug‐induced atypical dyskinesia | Clozapine vs placebo | Clozapine versus placebo for schizophrenia. | ||
| Schizophrenia | Clozapine versus risperidone | Clozapine versus risperidone for schizophrenia | ||
| Haloperidol decanoate vs fluphenazine decanoate | Depot fluphenazine for schizophrenia | |||
| Fluphenazine decanoate vs haloperidol decanoate | ||||
| Fluphenazine decanoate vs placebo | ||||
| Fluphenazine decanoate vs intermittent pimozide | ||||
| Fluphenazine decanoate vs vitamin B complex | ||||
| Fluphenazine ethanoate vs pipothiazine palmitate | ||||
| Haloperidol decanoate vs fluphenazine decanoate | Depot haloperidol decanoate for schizophrenia. | |||
| Fluphenazine ethanoate vs pipothiazine palmitate | Depot pipothiazine for schizophrenia. | |||
| Progabide vs placebo | GABA for schizophrenia | |||
| Tardive dyskinesia and psychiatric history | Metoclopramide (10 mg, 20 mg or 40 mg) vs haloperidol (5 mg or 10 mg) | Haloperdiol dose for schizophrenia | ||
| Schizophrenia | Haloperidol vs olanzapine | Haloperidol vs olanzapine for schizophrenia | ||
| Tardive dyskinesia | Chlorprothixene vs haloperidol vs perphenazine vs haloperidol + biperiden | Haloperidol vs perphenazine for schizophrenia | ||
| Schizophrenia | Haloperidol vs risperidone | Haloperidol vs risperidone for schizophrenia | ||
| Brief intermittent antipsychotic treatment vs fluphenazine decanoate | Intermittent antipsychotic treatment for schizophrenia | |||
| Fluphenazine decanoate vs intermittent pimozide | ||||
| Haloperidol with 'drug holiday' vs haloperidol | ||||
| Withdrawal of fluphenazine decanoate vs continuation | ||||
| Lithium vs placebo | Lithium for schizophrenia | |||
| Molidone vs haloperidol | Molidone vs haloperidol for schizophrenia | |||
| Olanzapine 1 mg vs olanzapine 10 mg versus placebo | Olanzapine dose for schizophrenia. | |||
| Olanzapine vs "conventional antipsychotic drugs" | Olanzapine for schizophrenia | |||
| First‐generation antipsychotic vs second‐generation antipsychotic | ||||
| Olanzapine with different timings of dose reduction periods | Olanzapine reduction for schizophrenia | |||
| First‐generation antipsychotic versus second‐generation antipsychotic | Olanzapine vs other atypical antipsychotics for schizophrenia | |||
| Olanzapine 1 mg vs olanzapine 10 mg vs placebo | Olanzapine vs placebo for schizophrenia | |||
| First‐generation antipsychotic vs second‐generation antipsychotic | Perphenazine for schizophrenia | |||
| Fluphenazine decanoate vs intermittent pimozide | Pimozide for schizophrenia | |||
| Quetiapine vs continuation of usual antipsychotic | Quetiapine vs continuation of usual antipsychotic for schizophrenia | |||
| First generation antipsychotic vs second‐generation antipsychotic | Quetiapine vs other atypical antipsychotics for schizophrenia | |||
| Quetiapine vs typical antipsychotic medications for schizophrenia | ||||
| Risperidone vs olanzapine for schizophrenia | ||||
| Risperidone vs other atypical antipsychotics for schizophrenia | ||||
| Quetiapine vs continuation of usual antipsychotic | Switching antipsychotic for schizophrenia. | |||
| Tardive dyskinesia | Thiopropazate vs placebo | Thiopropazate for schizophrenia | ||
| Schizophrenia | Thiopropazine vs trifluoperazine vs placebo | Thiopropazine vs placebo for schizophrenia | ||
| Thiopropazine vs trifluoperazine for schizophrenia | ||||
| Tardive dyskinesia | Thioproperazine and tiapride vs placebo | Thioproperazine for schizophrenia | ||
| Tiapride for schizophrenia | ||||
| Tiapride vs placebo | ||||
| Schizophrenia | Trifluoperazine high‐dose vs trifluoperazine low‐dose vs placebo | Trifluoperazine dose for schizophrenia | ||
| Trifluoperazine vs placebo for schizophrenia | ||||
| Thiopropazine vs trifluoperazine vs placebo | ||||
| Fluphenazine decanoate vs vitamin B complex | Vitamins for schizophrenia | |||
| First‐generation antipsychotic vs second‐generation antipsychotic | Ziprasidone vs other atypical antipsychotics for schizophrenia |
| Methods | Allocation: randomised, with sequence generation and concealment of allocation clearly described |
| Participants | People with antipsychotic‐induced tardive dyskinesiaa |
| Interventions | 1. Antipsychotic reduction/cessation (N = 150) vs antipsychotic maintenance (N = 150) OR 2. Specific antipsychotic (N = 150) vs other specific antipsychotic (N = 150) |
| Outcomes | Tardive dyskinesia: any clinically important improvement in tardive dyskinesia, any improvement, deteriorationc |
| Notes | aThis could be diagnosed by clinical decision. If funds were permitting all participants could be screened using operational criteria, otherwise a random sample should suffice. bSize of study with sufficient power to highlight about a 10% difference between groups for primary outcome. |
| Reduced dose of antipsychotic compared with antipsychotic maintenance for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: psychiatric patients (schizophrenia or schizoaffective disorder) with antipsychotic‐induced tardive dyskinesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with antipsychotic maintenance | Risk with reduced dose of antipsychotic | |||||
| Tardive dyskinesia: no clinically important improvement | Study population | RR 0.42 | 17 | ⊕⊝⊝⊝ | ||
| 875 per 1000 | 368 per 1000 | |||||
| Tardive dyskinesia: deterioration of symptoms | Study population | RR 0.61 | 17 | ⊕⊝⊝⊝ | ||
| 250 per 1000 | 153 per 1000 | |||||
| General mental state: relapse | Study population | RR 3.00 | 8 | ⊕⊝⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Adverse effect: any ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Adverse effect: extrapyramidal symptoms ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Acceptability of the treatment: leaving the study early | Study population | RR 0.33 | 8 | ⊕⊝⊝⊝ | ||
| 750 per 1000 | 248 per 1000 | |||||
| Social confidence, social inclusion, social networks, or personalised quality of life ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level for risk of bias: none of the studies adequately described allocation concealment, one study was a subsample from one site of an RCT, and one study's baseline characteristics were not balanced between study groups. | ||||||
| Antipsychotic cessation compared with antipsychotic maintenance for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: psychiatric patients with antipsychotic‐induced tardive dyskinesia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Antipsychotic maintenance | Antipsychotic cessation | |||||
| There is no evidence about the effects of withdrawal of antipsychotics compared with continuation of antipsychotics; none of the included studies evaluated this comparison. | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| Switch to another antipsychotic compared with antipsychotic cessation for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: psychiatric patients (schizophrenia) with antipsychotic‐induced tardive dyskinesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with antipsychotic cessation (placebo) | Risk with switch to another antipsychotic | |||||
| Tardive dyskinesia: no clinically important improvement | Study population | RR 0.45 | 42 | ⊕⊕⊝⊝ | ||
| 700 per 1000 | 315 per 1000 | |||||
| Tardive dyskinesia: deterioration of symptoms ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| General mental state: average endpoint score (BPRS, high = poor) | The mean general mental state average endpoint score (BPRS, high = poor) was 19 | MD 4.30 lower | ‐ | 42 | ⊕⊝⊝⊝ | |
| Adverse effect: any ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Adverse effects: use of antiparkinsonism drugs | Study population | RR 2.08 | 48 | ⊕⊝⊝⊝ | Another study reported ESRS scale data for parkinsonism and also found little or no difference between groups (MD ‐0.4 95% CI ‐1.25 to 0.45, 42 participants). | |
| 273 per 1000 | 567 per 1000 | |||||
| Acceptability of the treatment: leaving the study early | Study population | RR 0.60 | 50 | ⊕⊝⊝⊝ | ||
| 200 per 1000 | 120 per 1000 | |||||
| Social confidence, social inclusion, social networks, or personalised quality of life ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level for risk of bias: generation of random sequence and allocation concealment not adequately described. | ||||||
| Switch to specific antipsychotic compared with switch to a different specific antipsychotic for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: psychiatric patients (mainly schizophrenia) with antipsychotic‐induced tardive dyskinesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with specific antipsychotic 1 | Risk with specific antipsychotic 2 | |||||
| Tardive dyskinesia: no clinically important improvement Follow‐up: 3‐50 weeks | Study population | ‐ | 140 | ⊕⊝⊝⊝ | No meta‐analysis, studies stratified by antipsychotic. The following comparisons found no clinically important improvement: THI vs HAL, ZUC vs HAL, OLZ vs RIS, QUE vs HAL | |
| See comment | See comment | |||||
| Tardive dyskinesia: deterioration Follow‐up: 3‐4 weeks | Study population | ‐ | 35 | ⊕⊝⊝⊝ | No meta‐analysis, studies stratified by antipsychotic. The following comparisons found no difference in deterioration: THI vs HAL, ZUC vs HAL | |
| See comment | See comment | |||||
| General mental state: deterioration Follow‐up: 3‐50 weeks | Study population | ‐ | 120 | ⊕⊝⊝⊝ | No meta‐analysis, studies stratified by antipsychotic. The following comparisons found no difference in mental state deterioration: ZUC vs HAL, OLZ vs RIS, QUE vs HAL | |
| See comment | See comment | |||||
| Adverse events: extrapyramidal symptoms (need of antiparkinsonism drugs) Follow‐up: 8‐50 weeks | Study population | ‐ | 53 | ⊕⊕⊝⊝ | No meta‐analysis, studies stratified by antipsychotic. HAL more likely to need antiparkinsonism drugs than QUE (1 RCT, 45 participants, RR 0.45, 95% CI 0.21 to 0.96). No difference: RIS vs HAL | |
| See comment | See comment | |||||
| Adverse effects: general adverse events (UKU Average change score) Follow‐up: 24 weeks | See comment | See comment | ‐ | 80 | ⊕⊝⊝⊝ | No meta‐analysis, 3‐arm study comparing OLZ, ASP and unspecified FGAs found no difference in general adverse events for all pairwise comparisons. |
| Acceptability of the treatment: leaving the study early Follow‐up: 2 weeks ‐ 18 months | Study population | ‐ | 466 | ⊕⊝⊝⊝ | RIS more likely to leave study early than OLZ (2 RCTs, 130 participants, RR 0.73, 95% CI 0.57 to 0.95). Remaining studies no meta‐analysis, no difference (6 RCTs, 450 participants): MOL/THI/CLO/QUE vs HAL, OLZ/ASP vs unspecified FGAs, OLZ vs QUE/ZIP, QUE vs ZIP/RIS, ZIP vs RIS | |
| See comment | See comment | |||||
| Social confidence, social inclusion, social networks, or personalised quality of life ‐ not reported | None of the included studies reported on this outcome. | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one step for risk of bias: randomisation procedure, allocation concealment or blinding were not adequately described. | ||||||
| Specific antipsychotic compared with other drugs for antipsychotic‐induced tardive dyskinesia | ||||||
| Patient or population: psychiatric patients (mainly schizophrenia) with antipsychotic‐induced tardive dyskinesia | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with tetrabenazine | Risk with haloperidol | |||||
| Tardive dyskinesia: not improved to a clinically important extent | Study population | RR 1.07 | 13 | ⊕⊝⊝⊝ | ||
| 667 per 1000 | 713 per 1000 | |||||
| Tardive dyskinesia: deterioration of symptoms | Study population | RR 0.86 | 13 | ⊕⊝⊝⊝ | ||
| 167 per 1000 | 143 per 1000 | |||||
| Mental state ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Adverse effect: any ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Adverse effect: extrapyramidal symptoms ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| Acceptability of the treatment: leaving the study early | Study population | RR 4.38 | 13 | ⊕⊝⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Social confidence, social inclusion, social networks, or personalised quality of life ‐ not reported | See comment | See comment | Not estimable | (0 studies) | ‐ | None of the included studies reported on this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one step for risk of bias: randomisation procedure, allocation concealment and blinding were not adequately described. | ||||||
| Interventions | Current reference (updates underway) |
| Anticholinergic medication | |
| Benzodiazepines | |
| Calcium channel blockers | |
| Cholinergic medication | |
| Gamma‐aminobutyric acid agonists | |
| Miscellaneous treatments | |
| Neuroleptic reduction and/or cessation and neuroleptics | This review |
| Non‐neuroleptic catecholaminergic drugs | |
| Vitamin E |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Tardive dyskinesia: no clinically important improvement (long term) Show forest plot | 2 | 17 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.17, 1.04] |
| 2 Tardive dyskinesia: no improvement (long term) Show forest plot | 2 | 17 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.17, 1.04] |
| 3 Tardive dyskinesia: deterioration (long term) Show forest plot | 2 | 17 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.11, 3.31] |
| 4 General mental state: relapse (long term) Show forest plot | 1 | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.16, 57.36] |
| 5 Acceptability of the treatment: leaving the study early (long term) Show forest plot | 1 | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.06, 1.99] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Tardive dyskinesia: no clinically important improvement (medium term) Show forest plot | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.23, 0.89] |
| 2 Tardive dyskinesia: average endpoint score (AIMS, high = poor) (medium term) Show forest plot | 1 | 42 | Mean Difference (IV, Fixed, 95% CI) | ‐5.5 [‐8.60, ‐2.40] |
| 3 General mental state: average endpoint score (BPRS, high = poor) (medium term) Show forest plot | 1 | 42 | Mean Difference (IV, Fixed, 95% CI) | ‐4.30 [‐10.48, 1.88] |
| 4 Acceptability of the treatment: leaving the study early (medium term) Show forest plot | 1 | 50 | Risk Ratio (IV, Fixed, 95% CI) | 0.6 [0.16, 2.25] |
| 5 Adverse effects: use of antiparkinsonism drugs (medium term) Show forest plot | 1 | 48 | Risk Ratio (IV, Fixed, 95% CI) | 2.08 [0.74, 5.86] |
| 5.1 Haloperidol | 1 | 12 | Risk Ratio (IV, Fixed, 95% CI) | 2.0 [0.56, 7.09] |
| 5.2 Risperidone | 1 | 36 | Risk Ratio (IV, Fixed, 95% CI) | 2.26 [0.37, 13.60] |
| 6 Adverse effects: parkinsonism ‐ average endpoint score (ESRS) (medium term) Show forest plot | 1 | 42 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐1.25, 0.45] |
| 7 Adverse effects: dystonia ‐ average endpoint score (ESRS) (medium term) Show forest plot | 1 | 42 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐1.76, 0.36] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Tardive dyskinesia: no clinically important improvement Show forest plot | 4 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Thiopropazate vs haloperidol ‐ short term | 1 | 20 | Risk Ratio (IV, Fixed, 95% CI) | 1.53 [0.58, 4.05] |
| 1.2 Zuclopenthixol vs haloperidol ‐ short term | 1 | 15 | Risk Ratio (IV, Fixed, 95% CI) | 1.0 [0.79, 1.27] |
| 1.3 Olanzapine vs risperidone ‐ medium term | 1 | 60 | Risk Ratio (IV, Fixed, 95% CI) | 1.25 [0.82, 1.90] |
| 1.4 Quetiapine vs haloperidol ‐ medium term | 1 | 45 | Risk Ratio (IV, Fixed, 95% CI) | 0.80 [0.52, 1.22] |
| 1.5 Quetiapine vs haloperidol ‐ long term | 1 | 45 | Risk Ratio (IV, Fixed, 95% CI) | 0.88 [0.64, 1.21] |
| 2 Tardive dyskinesia: not any improvement (short term) Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Thiopropazate vs haloperidol | 1 | 20 | Risk Ratio (IV, Fixed, 95% CI) | 0.41 [0.05, 3.28] |
| 2.2 Zuclopenthixol vs haloperidol | 1 | 15 | Risk Ratio (IV, Fixed, 95% CI) | 0.88 [0.16, 4.68] |
| 3 Tardive dyskinesia: deterioration (short term) Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Thiopropazate vs haloperidol | 1 | 20 | Risk Ratio (IV, Fixed, 95% CI) | 1.22 [0.09, 16.92] |
| 3.2 Zuclopenthixol vs haloperidol | 1 | 15 | Risk Ratio (IV, Fixed, 95% CI) | 0.88 [0.16, 4.68] |
| 4 Tardive dyskinesia: average endpoint score (various scales) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Molindone vs haloperidol, 100% masking dose (AIMS, short term) | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 1.87 [‐0.20, 3.94] |
| 4.2 Molindone vs haloperidol, 200% masking dose (AIMS, short term) | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 3.44 [1.12, 5.76] |
| 4.3 Zuclopenthixol vs haloperidol (SHRS, short term) | 1 | 15 | Mean Difference (IV, Fixed, 95% CI) | ‐4.81 [‐12.15, 2.53] |
| 4.4 Olanzapine vs risperidone (AIMS, medium term) | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 2.20 [‐0.53, 4.93] |
| 5 Tardive dyskinesia: average change score (AIMS, low = better) (medium term) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Olanzapine vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | 1.66 [‐0.45, 3.77] |
| 5.2 Amisulpride vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | ‐0.82 [‐2.85, 1.21] |
| 5.3 Olanzapine vs amisulpride | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 2.48 [0.44, 4.52] |
| 5.4 Olanzapine vs risperidone | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐2.58, 4.98] |
| 6 General mental state: deterioration Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Zuclopenthixol vs haloperidol ‐ short term | 1 | 15 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.01, 6.29] |
| 6.2 Olanzapine vs risperidone ‐ medium term | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.64] |
| 6.3 Quetiapine vs haloperidol ‐ long term | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.83 [0.62, 5.39] |
| 7 General mental state: average endpoint score (PANSS‐general psychopathology, low = better) (long term) Show forest plot | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐2.20 [‐6.02, 1.62] |
| 7.1 Quetiapine vs haloperidol | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐2.20 [‐6.02, 1.62] |
| 8 General mental state: average change score (BPRS, low = better) (medium term) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Olanzapine vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | ‐1.14 [‐4.79, 2.51] |
| 8.2 Amisulpride vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | ‐2.46 [‐6.27, 1.35] |
| 8.3 Olanzapine vs risperidone | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐1.70 [‐8.37, 4.97] |
| 8.4 Olanzapine vs amisulpride | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 1.32 [‐1.94, 4.58] |
| 9 Acceptability of the treatment: leaving the study early (short term) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Molindone vs haloperidol | 1 | 18 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Thiopropazate vs haloperidol | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.01, 4.44] |
| 10 Acceptability of the treatment: leaving the study early (medium term) Show forest plot | 3 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Olanzapine vs FGA | 1 | 56 | Risk Ratio (IV, Fixed, 95% CI) | 1.86 [0.18, 19.38] |
| 10.2 Amisulpride vs FGA | 1 | 55 | Risk Ratio (IV, Fixed, 95% CI) | 0.96 [0.06, 14.65] |
| 10.3 Olanzapine vs amisulpride | 1 | 57 | Risk Ratio (IV, Fixed, 95% CI) | 1.93 [0.19, 20.12] |
| 10.4 Olanzapine vs risperidone | 2 | 170 | Risk Ratio (IV, Fixed, 95% CI) | 0.73 [0.57, 0.95] |
| 10.5 Olanzapine vs quetiapine | 1 | 116 | Risk Ratio (IV, Fixed, 95% CI) | 0.70 [0.54, 0.90] |
| 10.6 Olanzapine vs ziprasidone | 1 | 82 | Risk Ratio (IV, Fixed, 95% CI) | 0.77 [0.56, 1.05] |
| 10.7 Quetiapine vs risperidone | 1 | 118 | Risk Ratio (IV, Fixed, 95% CI) | 1.05 [0.88, 1.25] |
| 10.8 Quetiapine vs ziprasidone | 1 | 90 | Risk Ratio (IV, Fixed, 95% CI) | 1.10 [0.86, 1.40] |
| 10.9 Ziprasidone vs risperidone | 1 | 84 | Risk Ratio (IV, Fixed, 95% CI) | 0.95 [0.74, 1.23] |
| 11 Acceptability of the treatment: leaving the study early (long term) Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 Clozapine vs haloperidol | 1 | 39 | Risk Ratio (IV, Fixed, 95% CI) | 3.36 [0.45, 25.16] |
| 11.2 Quetiapine vs haloperidol | 1 | 45 | Risk Ratio (IV, Fixed, 95% CI) | 1.31 [0.63, 2.69] |
| 12 Adverse events: extrapyramidal symptoms (need of antiparkinsonism drugs) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Risperidone vs haloperidol (medium term) | 1 | 37 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.34, 1.35] |
| 12.2 Quetiapine vs haloperidol (long term) | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.21, 0.96] |
| 13 Adverse effects: parkinsonism (SHRS) ‐ average endpoint scores (short term) Show forest plot | 1 | 15 | Mean Difference (IV, Fixed, 95% CI) | ‐4.81 [‐12.15, 2.53] |
| 13.1 Zuclopenthixol vs haloperidol | 1 | 15 | Mean Difference (IV, Fixed, 95% CI) | ‐4.81 [‐12.15, 2.53] |
| 14 Adverse effects: parkinsonism (SAS, ESRS, low = better) ‐ average change score (medium term) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 14.1 Olanzapine vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | ‐0.85 [‐2.55, 0.85] |
| 14.2 Amisulpride vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | ‐0.5 [‐2.45, 1.45] |
| 14.3 Olanzapine vs risperidone | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.7 [‐1.33, ‐0.07] |
| 14.4 Olanzapine vs amisulpride | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | ‐0.35 [‐2.44, 1.74] |
| 15 Adverse effects: dyskinesia (ESRS, low = better) ‐ average change score (medium term) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 15.1 Olanzapine vs risperidone | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.91, 1.51] |
| 16 Adverse effects: akathisia (BAS, ESRS, low = better) ‐ average change scores (medium term) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 16.1 Olanzapine vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.30, 0.46] |
| 16.2 Amisulpride vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐0.42, 0.20] |
| 16.3 Olanzapine vs risperidone | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.8 [‐1.76, 0.16] |
| 16.4 Olanzapine vs amisulpride | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.12, 0.50] |
| 17 Adverse effects: dystonia (ESRS, low = better) ‐ average change score (medium term) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 17.1 Olanzapine vs risperidone | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.7 [‐1.41, 0.01] |
| 18 Adverse effects: general adverse events (UKU, low = better) ‐ average change score (medium term) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 18.1 Olanzapine vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐1.85, 2.01] |
| 18.2 Amisulpride vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | ‐0.55 [‐2.33, 1.23] |
| 18.3 Olanzapine vs amisulpride | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 0.63 [‐0.93, 2.19] |
| 19 General global state: average change score (CGI) (medium term) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 19.1 Olanzapine vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.41, 0.27] |
| 19.2 Amisulpride vs FGA | 1 | 53 | Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.47, 0.09] |
| 19.3 Olanzapine vs risperidone | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.61, 0.81] |
| 19.4 Olanzapine vs amisulpride | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 0.12 [‐0.19, 0.43] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Tardive dyskinesias: no clinically important improvement (medium term) Show forest plot | 1 | 13 | Risk Ratio (IV, Fixed, 95% CI) | 1.07 [0.51, 2.23] |
| 1.1 Haloperidol vs tetrabenazine | 1 | 13 | Risk Ratio (IV, Fixed, 95% CI) | 1.07 [0.51, 2.23] |
| 2 Tardive dyskinesia: no improvement (medium term) Show forest plot | 1 | 13 | Risk Ratio (IV, Fixed, 95% CI) | 2.57 [0.35, 18.68] |
| 2.1 Haloperidol vs tetrabenazine | 1 | 13 | Risk Ratio (IV, Fixed, 95% CI) | 2.57 [0.35, 18.68] |
| 3 Tardive dyskinesia: deterioration (medium term) Show forest plot | 1 | 13 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.07, 10.96] |
| 3.1 Haloperidol vs tetrabenazine | 1 | 13 | Risk Ratio (IV, Fixed, 95% CI) | 0.86 [0.07, 10.96] |
| 4 Acceptability of the treatment: leaving the study early (medium term) Show forest plot | 1 | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.38 [0.25, 76.54] |
| 4.1 Haloperidol vs tetrabenazine | 1 | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.38 [0.25, 76.54] |

