Interventions for treating proximal humeral fractures in adults
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised using sequentially numbered sealed envelopes | |
| Participants | Royal Liverpool Hospital, Liverpool, UK | |
| Interventions | Intervention started post surgery (mean 10 days; range 1 to 30 days after injury) Both mobilisation protocols were supervised by a team of specialist shoulder physiotherapists | |
| Outcomes | Length of follow‐up: 1 year; also assessed at 2 and 6 weeks, and 3 and 6 months (coinciding with outpatient visits) | |
| Notes | The early mobilisation regimen represented normal practice at the hospital. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description of method: "Patients were randomly allocated" |
| Allocation concealment (selection bias) | Unclear risk | "Randomization took place in the operating theater after the procedure, by use of sequentially numbered, sealed envelopes." |
| Blinding (performance bias and detection bias) | Unclear risk | "At the 6‐ and 12‐month visits, an independent blinded observer completed the Constant Shoulder Assessment and Oxford scores." However, care providers and participants were not blind to allocation and assessment of complications was not blinded either. |
| Blinding (performance bias and detection bias) | Unclear risk | No accounting of these, but lack of blinding unlikely to affect reporting of these. |
| Incomplete outcome data (attrition bias) | High risk | Incomplete account of participant flow, with exclusion of 10 participants from the analyses. |
| Incomplete outcome data (attrition bias) | High risk | No accounting of these outcomes, but incomplete account of participant flow, with exclusion of 10 participants from the analyses. |
| Selective reporting (reporting bias) | High risk | No protocol available. May have been stopped early, greater tuberosity migration not specifically listed in brief trial entry in the National Research Register (UK). |
| Balance in baseline characteristics? | Unclear risk | Incomplete data to back up claims of lack of baseline differences as these given only for 49 (10 excluded) but a 5 year difference in mean age (72 versus 67 years). |
| Free from performance bias? | Unclear risk | Although 3 upper limb surgeons performing the operations agreed to the same procedures a different uncemented prosthesis was used in 4 subsequently excluded participants. |
| Methods | Use of permutation table, single‐blind, independently administered | |
| Participants | Central hospital, Vasteras, Sweden | |
| Interventions | Interventions started 10 to 12 days post injury, after removal of sling. | |
| Outcomes | Length of follow‐up: 1 year; also assessed at 3, 8, 16 & 24 weeks | |
| Notes | The 2 excluded participants were in the control group: 1 died and 1 underwent an operation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Mention of "permutation table" and "randomized controlled" trial |
| Allocation concealment (selection bias) | Low risk | "A third person was responsible for the randomization procedure and kept the key to the permutation table" |
| Blinding (performance bias and detection bias) | Unclear risk | "A second physiotherapist examined the patients. She did not know to which group the patient belonged, and the patients were instructed not to tell her." However, there is no guarantee of blinding and, for practical reasons, neither participants nor care provider were blinded |
| Blinding (performance bias and detection bias) | Low risk | Lack of blinding unlikely to affect assessment of these outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | Participant flow provided but large loss to follow‐up (7/20 = 35%). |
| Incomplete outcome data (attrition bias) | Low risk | Participant flow provided |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. |
| Balance in baseline characteristics? | Unclear risk | Incomplete data to back up claims of lack of baseline differences but a 4 year difference in mean age between groups (66 versus 62 years). |
| Free from performance bias? | Low risk | No indication of performance bias. |
| Methods | Method of randomisation: referral to random list and randomisation timed at surgery | |
| Participants | Vienna General Hospital, Austria | |
| Interventions | Surgery started 7.3 days of injury (0 to 26 days). General anaesthesia used in all cases. Stems were cemented in place and bone grafting was performed using cancellous bone from patient's humeral head. | |
| Outcomes | Length of follow‐up: 1 year; also assessed at 12 days, 3 & 6 weeks, and 6 months | |
| Notes | Differences between the two prostheses include the type and position of fixation of the tuberosities and the volume of the stem in the metaphyseal area, thus allowing different amounts of additional (autologous) cancellous bone grafting. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The random list was designed to finally produce 2 groups of equal size." |
| Allocation concealment (selection bias) | Unclear risk | "Each surgeon was informed at the beginning of the operation as to which implant had randomly been selected." |
| Blinding (performance bias and detection bias) | High risk | No blinding. |
| Blinding (performance bias and detection bias) | Unclear risk | Lack of blinding unlikely to affect assessment of these outcomes. Standardisation of assessment. |
| Incomplete outcome data (attrition bias) | High risk | The group allocation and baseline data were not provided for 5 participants: 2 lost to follow‐up and 3 who had died. Standard deviations not provided. |
| Incomplete outcome data (attrition bias) | Unclear risk | Group allocation not provided for those who had died. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. |
| Balance in baseline characteristics? | Unclear risk | Incomplete baseline data (5 excluded) to confirm baseline comparability of those in analysis. |
| Free from performance bias? | Low risk | No indication of performance bias: a "general rehabilitation protocol was used for all patients regardless of the type of implant."; each of the 4 participating surgeons was experienced in joint replacement surgery. |
| Methods | Method of randomisation: use of computer software by independent hospital statistician; block size 12; use of numbered opaque sealed envelopes | |
| Participants | Olso University Hospital, Oslo, Norway | |
| Interventions | Interventions (and randomisation) started after hospital admission. (On admission to the hospital, all patients were immobilized in a modified Velpeau bandage.) | |
| Outcomes | Length of follow up: 2 years; also assessed at 2, 8, 12, 26 and 52 weeks | |
| Notes | Information on the trial received December 2006 from Dr Tore Fjalestad. More details on conservative treatment were provided in Fjalestad 2012. Tore Fjalestad also provided in an email (April 2012) the following clarification on the use of closed reduction for 8 conservatively treated participants (this had not been described in the protocol): "The primary X‐rays were assessed for classification and decision‐making for closed reduction. Those eight patients had a new radiographic examination after allocation to conservative treatment and after the procedure in the operating room, to confirm an acceptable position of the fragments. If not acceptable, the patients had to be treated with ORIF. Surprisingly, only one patient demonstrated unacceptable re‐displacement after two weeks, and was analyzed according to intention‐to‐treat principle in the conservative group at one year." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The [randomisation] procedure was designed by the statistician at the hospital research centre using the computer software S‐PLUS 6.0 for Windows 2002 ... Randomisation was based on equal blocks of length 12, with the exception of the last one, which was interrupted due to 50 patients." |
| Allocation concealment (selection bias) | Low risk | "Randomisation was performed by means of consecutively numbered and sealed non‐translucent envelopes containing each participant’s allocation to surgery or to conservative treatment." Independent statistician. |
| Blinding (performance bias and detection bias) | High risk | Two trained physiotherapists performed the 15D interviews. The physiotherapists were not blinded to group assignment. No provider or participant blinding. |
| Blinding (performance bias and detection bias) | Unclear risk | Lack of blinding unlikely to affect assessment of these outcomes, but may affect decisions for subsequent surgery. |
| Incomplete outcome data (attrition bias) | Low risk | Participant flow diagram provided and intention‐to‐treat analysis conducted. |
| Incomplete outcome data (attrition bias) | Low risk | Participant flow diagram provided and intention‐to‐treat analysis conducted. |
| Selective reporting (reporting bias) | Unclear risk | Trial registered after completion. Small discrepancies in trial inclusion criteria. |
| Balance in baseline characteristics? | Unclear risk | Statistically non significant imbalance in gender (5 versus 1 males) and baseline quality of life scores (higher in surgical group). |
| Free from performance bias? | Low risk | All the operations were performed by three surgeons experienced in the procedure performed. |
| Methods | Randomised using sequentially numbered sealed envelopes | |
| Participants | Royal Hallamshire Hospital, Sheffield, UK | |
| Interventions | Intervention started: at arrival at A&E. | |
| Outcomes | Length of follow‐up: 2 years, also 8 and 16 weeks and 1 year | |
| Notes | Information on this trial received from Mr Hodgson on several occasions. This included draft report of the 2 year follow‐up and notice of their plan to extend follow‐up to 5 years. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details: "using sequentially numbered sealed envelopes we randomly allocated patients" |
| Allocation concealment (selection bias) | Low risk | "using sequentially numbered sealed envelopes we randomly allocated patients". Also from phone conversation (08/08/2001): "physio opened envelopes when details entered on envelope". |
| Blinding (performance bias and detection bias) | Unclear risk | Blinded assessor of function but patients and care providers were not blinded. |
| Blinding (performance bias and detection bias) | Unclear risk | Lack of blinding unlikely to affect assessment of these outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | A full account of loss to follow‐up provided. While 14% at 2 years (12/86), it was under 5% (4/86) at 1 year. |
| Incomplete outcome data (attrition bias) | Low risk | Participant flow provided. |
| Selective reporting (reporting bias) | Unclear risk | Trial registration was incomplete and differed slightly from final reports. |
| Balance in baseline characteristics? | Unclear risk | More males in the early mobilisation group (11 versus 5). |
| Free from performance bias? | Low risk | Performance bias seemed unlikely. |
| Methods | Randomisation method unknown | |
| Participants | University Clinic Ulm, Germany | |
| Interventions | Interventions started within 14 days of fracture. | |
| Outcomes | Length of follow‐up: 1 year | |
| Notes | The plan for longer term follow‐up was announced in the Hoellen 1997 trial report. Further abstracts and a trial report (Holbein 1999) were identified for the review update (Issue 4, 2003). Holbein 1999 reported on 39 patients (19 versus 20), with 3‐ and 4‐part fractures, 31 (?/?) of whom had been followed up for 1 year and 24 (?/?) for 2 years. Requests (June 2003) for further information, including for denominators, resulted in the discovery that both Dr Holbein and Dr Hoellen were no longer at Ulm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details: prospective randomised trial |
| Allocation concealment (selection bias) | Unclear risk | No details: prospective randomised trial |
| Blinding (performance bias and detection bias) | High risk | No blinding. |
| Blinding (performance bias and detection bias) | Unclear risk | Lack of blinding unlikely to affect assessment of these outcomes |
| Incomplete outcome data (attrition bias) | High risk | Participant flow provided but large loss to follow‐up (12/30 = 40%); and potential exclusions. |
| Incomplete outcome data (attrition bias) | Unclear risk | Participant flow provided but large loss to follow‐up (12/30 = 40%). Serious outcomes though are less likely to be missed. |
| Selective reporting (reporting bias) | High risk | Insufficient information to judge this but the pragmatic removal of the power component of the Constant score was post hoc. Also non addressed difference in trial inclusion criteria between the two reports of this trial. |
| Balance in baseline characteristics? | Unclear risk | No information on baseline characteristics of the two treatment groups but inclusion criteria rule out some confounders. |
| Free from performance bias? | Unclear risk | Same post‐operative treatment but in all there is insufficient information to assess performance bias. |
| Methods | Method of randomisation: unknown, "randomly selected" | |
| Participants | Rigshospitalet, Copenhagen, Denmark | |
| Interventions | Interventions started: not stated. | |
| Outcomes | Length of follow‐up: 12 months; also assessed at 3 & 6 months | |
| Notes | In both groups, functional exercises were started under instruction during the first week. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details: "randomly selected for treatment" |
| Allocation concealment (selection bias) | Unclear risk | No details: "randomly selected for treatment" |
| Blinding (performance bias and detection bias) | High risk | No blinding reported. |
| Blinding (performance bias and detection bias) | Unclear risk | Unlikely to be affected by lack of blinding |
| Incomplete outcome data (attrition bias) | High risk | Exclusion of data for participants with treatment failure and early refracture from 12 month review. Large loss to follow‐up (10/31 = 32%). |
| Incomplete outcome data (attrition bias) | Low risk | Participant flow provided. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. |
| Balance in baseline characteristics? | Low risk | No information on the patient with bilateral fractures but a relatively minor unit of analysis issue. |
| Free from performance bias? | Unclear risk | No information on operator competence/expertise. |
| Methods | Method of randomisation: unknown | |
| Participants | Hvidovre University Hospital, Denmark | |
| Interventions | Interventions started immediately or after closed or open manipulation. | |
| Outcomes | Length of follow‐up: 2 years; also assessed at 1, 3, 6 & 12 months | |
| Notes | Post immobilisation for both groups: instructions given for Codman’s pendulum exercises as well as active movements of elbow and hand. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details: "Random allocation to immobilization for 1 to 3 weeks was performed" |
| Allocation concealment (selection bias) | Unclear risk | No details. |
| Blinding (performance bias and detection bias) | Unclear risk | Only claimed for outcome assessors at final follow‐up: "The 2‐year follow‐up examination was blind, as the examiners had no knowledge of the period of immobilization." |
| Blinding (performance bias and detection bias) | Unclear risk | No blinding but may not have affected appraisal of mortality (which was not split by treatment group). |
| Incomplete outcome data (attrition bias) | High risk | Large loss to follow‐up (46/85 = 54%). Numbers given for those available at follow‐up but incompletely reported data: only medians. |
| Incomplete outcome data (attrition bias) | High risk | Although numbers given for those available at follow‐up, only overall mortality data provided (extracted from graph). |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. |
| Balance in baseline characteristics? | Unclear risk | Although there appeared to be comparability between treatment groups in age and gender, the percentage of minimally displaced fractures (79% versus 70%: 33/42 versus 30/43) differed between the two groups and no information was available on the numbers who had open manipulation (thus entailing surgery). |
| Free from performance bias? | Unclear risk | Lack of information to judge on performance bias. |
| Methods | Randomised using block randomisation (under supervision of a statistician) and telephone to an independent researcher with patient details. | |
| Participants | Cochlin Hospital, Paris, France | |
| Interventions | Intervention started with 72 hours after fracture. Patients used oral analgesics to manage pain. After 4 to 6 weeks, patients were advised to perform daily exercises at home. Patients were discharged from the study at 6 months. | |
| Outcomes | Length of follow‐up: 6 months, also 6 weeks and 3 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Block randomization involved choosing randomly from among blocks of lengths 4 and 2 to prevent the risk of predictability." |
| Allocation concealment (selection bias) | Low risk | "After completion of the trial entry details, an independent researcher responsible for treatment allocation was contacted by telephone." |
| Blinding (performance bias and detection bias) | Unclear risk | "Outcome measures were recorded by two physicians, including one of the authors (F.F.), who were blinded to the treatment assignments." However, care providers and participants were not blinded to allocation. |
| Blinding (performance bias and detection bias) | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | Data were unavailable from 10 participants (5 in each group) who were lost to follow‐up because of difficulties in travelling to the hospital. Their characteristics were reported not to differ from those who attended. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this; retrospective trial registration. |
| Balance in baseline characteristics? | Low risk | |
| Free from performance bias? | Low risk | Rehabilitation was standardised and "delivered by physiotherapists who were experienced in the field". |
| Methods | Method of randomisation: unknown, double‐blind | |
| Participants | Mansfield District General Hospital, Mansfield, UK | |
| Interventions | Interventions started on average 8.6 days since injury, upon referral to physiotherapy department. | |
| Outcomes | Length of follow‐up: 6 months; also assessed at 1 & 2 months | |
| Notes | All patients received the same standardised physiotherapy regimen. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided: "patients were randomized into two groups" |
| Allocation concealment (selection bias) | Low risk | "double‐blind", and randomisation code was only broken at end of the trial period to permit analyses |
| Blinding (performance bias and detection bias) | Low risk | "double‐blind", use of sham control |
| Blinding (performance bias and detection bias) | Unclear risk | No report of these outcomes |
| Incomplete outcome data (attrition bias) | High risk | Although loss to follow‐up reported, no results were presented for the trial groups. |
| Incomplete outcome data (attrition bias) | Unclear risk | No report of these outcomes |
| Selective reporting (reporting bias) | High risk | Results not presented. |
| Balance in baseline characteristics? | Unclear risk | Baseline comparability. However, although the article claims "patients ... were referred to the physiotherapy department without delay", the ranges for average time from injury to start treatment were 0 to 17 days (active) and 0 to 27 days (sham). |
| Free from performance bias? | Unclear risk | "Standardized physiotherapy regimen". However, although the article claims "patients ... were referred to the physiotherapy department without delay", the ranges for average time from injury to start treatment were 0 to 17 days (active) and 0 to 27 days (sham). |
| Methods | Method of randomisation: unknown | |
| Participants | Gavle, Sweden | |
| Interventions | Interventions started 7 days post injury, after removal of sling. | |
| Outcomes | Length of follow‐up: > 1 year (mean 16 months); also assessed at 1 & 3 months | |
| Notes | No indication in the report of any loss to follow‐up at last follow‐up (> 1 year), but cannot be assumed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of method: "In all, 42 patients were randomly assigned into two groups." |
| Allocation concealment (selection bias) | Unclear risk | No details of method: "In all, 42 patients were randomly assigned into two groups." |
| Blinding (performance bias and detection bias) | High risk | No blinding, although independent assessment claimed: "Examination was made by physicians and physiotherapists independently at 1 month and 3 months.." |
| Blinding (performance bias and detection bias) | Unclear risk | No reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | Full data provided for 1 and 3 months follow‐up; but denominators not stated for long‐term (mean 16 months) follow‐up |
| Incomplete outcome data (attrition bias) | Unclear risk | Data not reported for these outcomes |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. |
| Balance in baseline characteristics? | Low risk | No major imbalances in baseline characteristics |
| Free from performance bias? | Low risk | No indications of performance bias. |
| Methods | Method of randomisation: used closed envelopes Assessor blinding: unknown Loss to follow‐up: 10 patients excluded from analysis following randomisation; 6 with polytrauma, 2 with neurologic deficiency and 2 (1 versus 1) who were converted to shoulder arthroplasty intraoperatively. There was no mention of group allocation at randomisation or evaluation in the paper ‐ these (8 versus 2) were notified after contact with the lead trial investigator. | |
| Participants | Ludwig‐Maximilians University, Munich, Germany Period of study recruitment: August 2006 to July 2008 76 patients, aged over 18 years, with displaced proximal humeral fractures with displacement > 1 cm and angulation of fragments > 45 degrees (Neer criteria). Exclusion criteria: poly‐traumatised patients, neurologic deficit or intra‐operative conversion to shoulder arthroplasty. (Paper noted there were no open or pathological fractures.) Of 66: 48 female, 18 male; mean age 68 years, range 29 to 92 years | |
| Interventions | 1. Polyaxial angular stable plate fixation (Non‐contact bridging – Proximal Humerus (NCB‐PH)). Polyaxial plating allows a range of 0 to 15‐degree angle off‐centre. After insertion, a threaded screw cap locks the axis of the screw. A deltopectoral approach was used for open reduction and internal fixation of all fractures. All patients received prophylactic intravenous antibiotic immediately before surgery. "The postoperative rehabilitation protocol included immediate passive and active‐assisted range of motion (ROM) up to 60‐degree angle of abduction and elevation without forced external rotation for 6 weeks. Full ROM with active exercises was started 6 weeks after operation.” Assigned: 39/37 Completed: 29/37 | |
| Outcomes | Length of follow‐up: 6 months (X‐rays 1 day, 6 weeks, 3 months and 6 months) Secondary varus displacement (> 10 degrees) Delayed union (due to osteonecrosis) Re‐operation: revision surgery and early hardware removal Infection (none) | |
| Notes | Request for information sent to Dr Ockert on 2 June 2012. Repeated on 8 June 2012, in email Peter Biberthaler regarding identification and further information on ongoing trial referred to in conference abstract (Biberthaler 2009) ‐ it seems highly likely that the ongoing trial was this trial. However, this was not clear from email from Ben Ockert on 18 June 2012; this also provided details on the method of randomisation, the numbers allocated and analysed in each group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "consecutive patients ... were prospectively randomized". No description of sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | "consecutive patients ... were prospectively randomized". Contact from trialist revealed they "used closed envelope technique for randomization". (Exclusion criteria appeared to be applied post‐randomisation.) |
| Blinding (performance bias and detection bias) | High risk | No mention of blinding. Radiographic assessment performed by two trained radiologists twice in separate sessions 8 weeks apart. Consensus decision for osteonecrosis and implant related failure. Criteria for healing stated. |
| Blinding (performance bias and detection bias) | Unclear risk | No mention of blinding, but unlikely to affect this. |
| Incomplete outcome data (attrition bias) | High risk | "Follow‐up rate was 71% of all radiographs taken 1 day, 6 weeks, 3 months, and 6 months after surgery." Numbers of patients allocated or assessed by intervention group provided after personal communication. Post‐randomisation exclusions (10/76 = 13%),was imbalanced (8 versus 2) and other loss to follow‐up not accounted for. |
| Incomplete outcome data (attrition bias) | Unclear risk | As above. Paper described cases of revision surgery and early removal of metalwork; however, group allocation not given. Information provided subsequently. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. |
| Balance in baseline characteristics? | Unclear risk | "The fracture types were equally distributed in both study groups." However, this applied to 66 participants. Does not state how many patients in each group or compare demographics. |
| Free from performance bias? | Low risk | Six experienced surgeons performed the surgery: "In advance of this study, all surgeons were trained in the respective monoaxial and polyaxial locking plate system”. Same antibiotic regimen and post‐op management. |
| Methods | Method of randomisation: opaque, sealed envelopes | |
| Participants | Stockholm Söder Hospital, Stockholm, Sweden | |
| Interventions | Interventions (and randomisation) started after hospital admission. | |
| Outcomes | Length of follow up: 2 years Subsequent surgery (reasons including deep infection, etc) | |
| Notes | Trial run concurrently with Olerud 2011b. Additional information on randomisation and trial location obtained from Dr Olerud (April 2012). Pain data received May 2012. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "After clearance by an anesthetist, the patients were randomized (independently prepared opaque, sealed envelopes) to open reduction and internal fixation with a locking plate or nonoperative treatment." trial report "the patients were randomised by numbered sealed opaque envelopes drawn consecutively. The envelopes were independently prepared and thoroughly mixed. After that the envelopes were numbered by another person. At the time of randomisation the envelopes were drawn in numerical order." personal communication |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding (performance bias and detection bias) | High risk | No assessor blinding, although "The final 24‐month follow‐up was performed by an independent orthopaedic surgeon not previously involved in the treatment." No provider or participant blinding. |
| Blinding (performance bias and detection bias) | Unclear risk | Lack of blinding unlikely to affect assessment of these outcomes, but may affect decisions for subsequent surgery. |
| Incomplete outcome data (attrition bias) | Low risk | "In the outcome analyses, all patients remained in their randomization group regardless of secondary procedures according to the intention‐to‐treat principle." Participant flow provided; no cause for concern. |
| Incomplete outcome data (attrition bias) | Low risk | As above. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. No protocol found. |
| Balance in baseline characteristics? | Low risk | No imbalances: baseline comparability. |
| Free from performance bias? | Low risk | "All operations in patients randomized to surgery were performed by 1 of 2 orthopaedic surgeons, both well experienced in shoulder surgery." While all surgical patients were referred to a physiotherapist after their surgery and conservatively treated patients were referred after 2 weeks, this was unlikely to influence results. Otherwise, similar exercise / rehabilitation schedules. |
| Methods | Method of randomisation: opaque, sealed envelopes | |
| Participants | Stockholm Söder Hospital, Stockholm, Sweden | |
| Interventions | Interventions (and randomisation) started after hospital admission. Cancellous bone graft from the head fragment was placed between the shaft and the tuberosities. (All patients had pre‐operative and 2 doses post‐operative antibiotics.) Post surgery, the arm was placed in a sling and patients were referred to a physiotherapist. The sling was used for 6 weeks; afterwards, the patients were allowed to use it at their own convenience. Pendulum exercises and passive elevation/abduction up to 90 degrees were started from the first postoperative day. After 6 weeks, the patients were allowed a free active range of movement. Strengthening exercises were begun after 3 months. | |
| Outcomes | Length of follow up: 2 years Subsequent surgery (reasons including non‐union, etc) | |
| Notes | Trial run concurrently with Olerud 2011a. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "After clearance by an anesthesiologist, the patients were randomized (opaque sealed envelopes prepared independently) to a primary HA or nonoperative treatment." trial report "the patients were randomised by numbered sealed opaque envelopes drawn consecutively. The envelopes were independently prepared and thoroughly mixed. After that the envelopes were numbered by another person. At the time of randomisation the envelopes were drawn in numerical order." personal communication |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding (performance bias and detection bias) | High risk | No assessor blinding, although "The final 24‐month follow‐up was performed by an independent orthopaedic surgeon not previously involved in the treatment." No provider or participant blinding. |
| Blinding (performance bias and detection bias) | Unclear risk | Lack of blinding unlikely to affect assessment of these outcomes, but may affect decisions for subsequent surgery. |
| Incomplete outcome data (attrition bias) | Low risk | "In the outcome analyses, all patients remained in their |
| Incomplete outcome data (attrition bias) | Low risk | As above. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. No protocol found. |
| Balance in baseline characteristics? | Low risk | No imbalances: baseline comparability. |
| Free from performance bias? | Unclear risk | "In patients randomized to surgery, all operations were performed by 1 of 2 orthopedic surgeons, both well experienced in shoulder surgery ..." While all surgical patients were referred to a physiotherapist after their surgery and conservatively treated patients were referred after 2 weeks, this was unlikely to influence results. As was the differences in timing for free ROM (6 versus 4 weeks). However, it was only reported for the surgical group that strengthening exercises were begun after 3 months. |
| Methods | Randomisation from closed envelopes | |
| Participants | Danderyd Hospital, Danderyd, Sweden | |
| Interventions | Interventions started 5 to 10 days post‐injury after removal of sling. | |
| Outcomes | Length of follow‐up: 1 year; also assessed at 3 weeks, 2 & 3 months | |
| Notes | Means (probably) presented without standard deviations. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details: "patients were randomized into two groups" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient details of safeguards: "randomized and given instructions in a sealed envelope" |
| Blinding (performance bias and detection bias) | Unclear risk | "All patients were examined by a physiotherapist who did not know which group each patient belonged to". However, no participant or care provider blinding nor mention of ways to prevent disclosure to assessor. |
| Blinding (performance bias and detection bias) | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) | High risk | The treatment group of the participant lost to follow‐up was not stated. Standard deviations not provided. Graphs only provided for female participants ‐ denominators not provided for these. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported. The treatment group of the participant lost to follow‐up was not stated. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. |
| Balance in baseline characteristics? | Unclear risk | Baseline data not provided for gender. |
| Free from performance bias? | Unclear risk | Uncertainty if any compensatory advice given for the control group. |
| Methods | Method of randomisation: alternation | |
| Participants | Leuven University Hospital, Belgium | |
| Interventions | Interventions started immediately. | |
| Outcomes | Length of follow‐up: until fracture consolidation; also assessed at 1 & 3 weeks | |
| Notes | Two fractures in the Gilchrist group required reduction. Seven participants had other fractures: 3 in group 1 (2 rib, 1 vertebra); 4 in group 2 (1 ankle, 1 hip, 1 rib, 1 vertebra). Trial reports in German; translation obtained. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised: alternation |
| Allocation concealment (selection bias) | High risk | Alternation |
| Blinding (performance bias and detection bias) | High risk | No mention of blinding |
| Blinding (performance bias and detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | While all participants were followed up and intention‐to‐treat analyses seemed to have been done, no data on function were presented nor were the criteria for judging fracture consolidation. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. |
| Balance in baseline characteristics? | Unclear risk | Small discrepancies (e.g. in other injuries or having fracture reduction) can have bigger consequences for small group sizes. |
| Free from performance bias? | Unclear risk | Differences in care programmes cannot be ruled out. |
| Methods | Method of randomisation: computer generated block randomisation with sealed envelopes Assessor blinding: no mention in the paper Loss to follow‐up: 4 lost to follow‐up and 2 died of breast cancer during the study period | |
| Participants | University Hospital in Hradec Králové, Czech Republic Period of study recruitment: January 2006 to January 2010 61 patients with AO type A2, A3, B1 and C1 (2 part and 3 part) proximal humerus fractures aged between 18 and 80 years able to give informed consent. Exclusion criteria: open fracture, associated injury (AIS > 2), open growth plates, or patient's health would limit the extent of surgery. 45 females, 10 males; mean age 61 years, range 21 to 81 years | |
| Interventions | Interventions started 0 to 24 days after injury. 2. Minimally invasive group: Zifko method of minimally invasive osteosynthesis with intramedullary K‐wire insertion (distally inserted) – figure in article shows 8 wires inserted into humeral head along medullary canal. Assigned: ?/? (total 61) Completed: 28/27 | |
| Outcomes | Length of follow‐up: mean 2 years Days to operation Constant‐Murley score (relative to healthy limb) Time to recover normal upper limb function Complications X‐ray exposure Length of operation Length of hospital stay | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “The patients were randomised to the groups by a computer programme which facilitates the maintenance of homogeneity of the groups compared.” Web‐based translation implied use of random numbers and permuted blocks so as to get similar numbers on each group. Produced independently by a statistical company. |
| Allocation concealment (selection bias) | Low risk | The sealed envelopes were created by a professional statistical company (Pharm test s. r. o., Hradec Králové): in accordance with randomization sheet each envelope their number and sealed inside information," zifko" or "LCP." The sealed envelopes were opened sequentially. |
| Blinding (performance bias and detection bias) | High risk | Not possible to blind patient / providers. No mention of outcome assessment. |
| Blinding (performance bias and detection bias) | Unclear risk | May not affect assessment |
| Incomplete outcome data (attrition bias) | High risk | Incomplete data (and group of 6 excluded participants not noted) |
| Incomplete outcome data (attrition bias) | High risk | Incomplete data (and group of 2 deaths not stated) |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Balance in baseline characteristics? | Unclear risk | Aside from age – no details or confirmation of this |
| Free from performance bias? | Unclear risk | No details – including of surgeon’s experience |
| Methods | Method of randomisation: unknown, "randomly selected" | |
| Participants | Bristol Royal Infirmary, Bristol, UK | |
| Interventions | Interventions started: within 5 days for surgery. | |
| Outcomes | Length of follow‐up: stated as 18 months to 12 years; but also assessed regularly up to 6 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details: "assigned by pre‐arranged random selection" |
| Allocation concealment (selection bias) | Unclear risk | No details: "assigned by pre‐arranged random selection" |
| Blinding (performance bias and detection bias) | High risk | Not blinded |
| Blinding (performance bias and detection bias) | Unclear risk | No blinding but may not have affected appraisal of mortality |
| Incomplete outcome data (attrition bias) | High risk | Large loss to follow‐up (46/85 = 54%). Numbers given for those available at follow‐up but incompletely reported data: only medians. |
| Incomplete outcome data (attrition bias) | Unclear risk | Slight discrepancy in trial report that 2 deaths are reported, one in each group, but long term denominators are as at baseline. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this, but the protracted nature of this trial makes selective reporting more likely. |
| Balance in baseline characteristics? | Unclear risk | Surgical group on average 4.5 years younger, but uncertainties mainly reflect Inadequate information in terms of other co‐morbidities and injuries for this broad category of patients. |
| Free from performance bias? | Unclear risk | Inadequate information on care programme comparability especially given the protracted nature of the trial recruitment. However, one surgeon operated throughout. |
| Methods | Method of randomisation: drawing balls from a bag by an independent person Assessor blinding: assessor blinding Loss to follow‐up at 12 months: 8/56 (did not complete follow‐up: 2 deaths, 4 drop‐outs, 2 excluded because of early secondary arthroplasty) | |
| Participants | Friederikenstift Hospital Hannover, Hannover, Germany Period of study recruitment: conducted over 18 month period (no dates) 56 patients with isolated Neer type 3‐ and 4‐part proximal humeral fractures, aged > 60 years. Exclusion criteria: fractures older than 2 weeks, open fractures, pathological fractures, refractures, neurologic disease and patients who would be clearly non‐compliant (e.g. alcoholics, patients of no fixed address) Of 48: 38 female, 10 male; Of 56: mean age 74 years, range 60 to 87 years | |
| Interventions | Interventions started: at surgical fixation (time to surgery from injury not given) 1) Polyaxial locked screws: Humeral Suture Plate (HSP) (Arthrex, Naples, FL) with polyaxially locked screws. Screws were blunt‐ended (considered better in the prevention of glenoid erosions in case of screw perforations). 2) Non‐polyaxial (monoaxial) implant: Proximal Humerus Internal Locking System (PHILOS) (Synthes, Bettlach, Switzerland) with nonpolyaxially locked screws. (Screws were pointed in the PHILOS plate.) All surgery performed under general anaesthesia using deltopectoral approach. Tuberosity fragments reduced with fibre wire, different approaches for head fragment depending on whether valgus or varus. Allocated plate positioned anatomically and fixed with a shaft screw. Patients' shoulders were immobilised in a sling for 2 days. Then, active‐assisted motion beyond 90 degrees flexion and abduction were initiated avoiding the provocation of pain. At 7 weeks, free range of motion was allowed. Assigned: 25/31 Completed: 20/28 (at 12 months) | |
| Outcomes | Length of follow‐up: 12 months Simple shoulder test Constant score (relative to contralateral limb) Range of active shoulder motion (flexion, abduction, internal rotation, external rotation) Fracture healing ‐ AP and axillary radiographs Duration of operation Fluoroscopy time | |
| Notes | Additional information and clarification of 8 participants who did not complete follow‐up and gender data for those who completed follow‐up obtained from Dr Voigt (May 2012). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “The randomization technique was blinded by drawing balls from a bag: one ball for HSP and the other ball for PHILOS by an independent person.” |
| Allocation concealment (selection bias) | Low risk | “The randomization technique was blinded by drawing balls from a bag: one ball for HSP and the other ball for PHILOS by an independent person.” |
| Blinding (performance bias and detection bias) | High risk | No mention of blinding of patients or personnel other than assessor blinding: "Follow‐up evaluations postoperatively were performed in a standardized fashion by an independent trauma surgeon" |
| Blinding (performance bias and detection bias) | Unclear risk | Unlikely to influence this. |
| Incomplete outcome data (attrition bias) | Unclear risk | Although clarification on loss to follow‐up (8 patients: 5 versus 3) received from author, the impact on the results for functional outcomes is unclear. |
| Incomplete outcome data (attrition bias) | Low risk | Clarification received from author on the loss to follow‐up: 2 were deaths and 2 were replacement arthroplasty. |
| Selective reporting (reporting bias) | Unclear risk | No protocol provided |
| Balance in baseline characteristics? | Unclear risk | Balance in 3 versus 4 part fractures, probably age and pre‐operative DASH. Incomplete data on gender, 2 versus 6 with diabetes (but no frozen shoulder). |
| Free from performance bias? | Unclear risk | No details of surgeon experience. |
| Methods | Method of randomisation: unknown, "random allocation" | |
| Participants | University Hospital, Homburg/Saar, Germany | |
| Interventions | Interventions started post‐operatively after percutaneous fixation (Kirschner wires plus in 38 cases, cannulated screws). | |
| Outcomes | Length of follow‐up: 9 to 36 (mean 14 months) months (in 59 participants), but also assessed at 1, 3 and 6 months | |
| Notes | Short report (1997) from conference proceedings gave interim results for 51 patients. Full report and some results provided by Dr Wirbel (February 2003). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details: "a random allocation of patients in 2 groups was done" |
| Allocation concealment (selection bias) | Unclear risk | No details: "a random allocation of patients in 2 groups was done" |
| Blinding (performance bias and detection bias) | High risk | No mention of blinding. |
| Blinding (performance bias and detection bias) | Unclear risk | Not blinded but less likely that these outcomes would be affected. |
| Incomplete outcome data (attrition bias) | High risk | Limited data on function using a non‐validated assessment instrument with a moderate loss to follow‐up at 6 months (17/77 = 17%). |
| Incomplete outcome data (attrition bias) | Unclear risk | Incomplete data. Although loss to follow‐up reported, reoperations were not sufficiently reported by treatment group. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. |
| Balance in baseline characteristics? | Low risk | No indication of any major baseline imbalance. |
| Free from performance bias? | Low risk | No indication of performance bias from differences in care programmes. |
| Methods | Method of randomisation: computer generated random numbers Assessor blinding: likely, "independent" assessor at follow‐up Loss to follow‐up: 4 patients within the first year after surgery due to moving out of the area and change of telephone number | |
| Participants | The Third Affiliated Hospital of Whenzou, Whenzou, China Period of study recruitment: October 2007 to September 2008 72 patients aged over 18 years with an acute closed 2, 3 or 4 part fracture (Neer classification) of the proximal humerus treated with open reduction and internal fixation using a locking plate. Exclusion criteria: pathological fractures, primary or metastatic tumour and fracture with non‐union. Of 68 followed‐up: 46 female, 22 male; mean age 63 years, range 32 to 78 years | |
| Interventions | Interventions started: both at surgery, time from injury not stated 1. ORIF with PHILOS locking plates (Synthes, Switzerland). Standard deltopectoral approach; reduction enabled with a K‐wire under fluoroscopy. Locking plate was placed 10 mm posterior to the intertubercular groove and 10 mm distal to the tip of greater tubercle. A cortical screw was inserted initially to fix the distal fragment. Four or five locking screws were used for the fixation of the proximal fragment. All proximal screws were inserted 5 mm below subchondral bone. One or two additional locking screws were inserted obliquely into the medio‐inferior region of the humeral head in this group. The tubercular fragments and rotator cuff tendon were fixed using Ethibond sutures. Autograft bone was used in comminuted fractures where there was a mass defect and for reconstruction of the medial support structures. Fracture reduction and screw length were finally assessed with fluoroscopy. 2. As above without medial support locking screws. All patients received prophylactic intravenous antibiotics before the procedure. Passive abduction and clock‐wise rotation exercises were allowed on the day after surgery. Active rehabilitation was started six weeks postoperatively. Assigned: 32/40 (total: 72) | |
| Outcomes | Length of follow‐up: average 30.8 months (also 4, 8, 12 weeks, 6, 9 and 12 months and yearly) Shoulder function (Constant shoulder score) Union Complications: osteonecrosis of the humeral head, early failure and loss of fixation | |
| Notes | Personal contact (email 14/05/2012) clarified method of randomisation, group of patients who were lost to follow‐up; and complications. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The patients were randomized into two groups for study according to computer‐generated random numbers" (Group sizes, however, were unequal.) |
| Allocation concealment (selection bias) | Unclear risk | There were insufficient safeguards (selection according to odd and even random numbers) to confirm allocation concealment. |
| Blinding (performance bias and detection bias) | Unclear risk | It is possible that the participants did not know which group they were in. The difference between the two interventions was not large. |
| Blinding (performance bias and detection bias) | Low risk | These outcomes are fairly robust regarding blinding. |
| Incomplete outcome data (attrition bias) | Unclear risk | Active surveillance but missing data for 4 participants lost to follow‐up. Personal correspondence gave details on complications. |
| Incomplete outcome data (attrition bias) | Unclear risk | Missing data for 4 participants. Personal correspondence provided information on re‐operations. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient data to judge this. No protocol available. |
| Balance in baseline characteristics? | Unclear risk | Although the baseline characteristics of 68 participants were comparable, data were missing for 4 participants loss to follow‐up. |
| Free from performance bias? | Low risk | “Operations were performed by two senior surgeons.” All participants received same rehabilitation. |
| Methods | Method of randomisation: computer generated random numbers list reviewed by nurse before surgery | |
| Participants | Beijing Ji Shui Tan Hospital, Beijing, China Period of study recruitment: November 2004 to December 2006 | |
| Interventions | Interventions started: surgery on average 9 days after injury (randomisation before surgery). 1. Open reduction with internal fixation using a locking plate: Locking Proximal Humeral Plate (LPHP; Synthes) or the Proximal Humeral Internal Locking System (PHILOS; Synthes). General anaesthesia combined with an interscalene block. Indirect reduction under image intensifier, with reduced fracture temporarily fixed by a Kirschner wire. After placement, position of the locking plate checked with the image intensifier intraoperatively, and the plate was fixed with locking screws. Finally, a thorough fluoroscopic screening was done to ensure that no screw was penetrating the articular surface of the humeral head. 2. Open reduction with internal fixation using a locking nail: the Proximal Humeral Nail (PHN; Synthes). An interscalene brachial plexus block was used. Nail was inserted under image control without reaming after the fracture was fully reduced. After insertion of the spiral blade and the distal locking screws, an end cap was screwed in to lock the spiral blade. The rotator cuff tendon and the deltoid were carefully repaired during wound closure. The affected extremity was protected by a sling for six weeks postoperatively. Passive range‐of‐motion exercises, supervised by a physical therapist, were initiated on the first postoperative day. Active and active‐assisted exercises began after six weeks, when early callus formation could be seen on radiographs. Strengthening exercises were started three months after the surgery. | |
| Outcomes | Length of follow up: 3 years (also 1 year) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was accomplished with use of a random numbers list generated by software and kept by the operating room nurse." |
| Allocation concealment (selection bias) | Unclear risk | "Before the surgery, the circulating nurse reviewed the random‐numbers list. Patients who had been assigned an odd number were subsequently treated with a locking nail, and those who had been assigned an even number were managed with a locking plate." |
| Blinding (performance bias and detection bias) | High risk | No mention of blinding. However: |
| Blinding (performance bias and detection bias) | Unclear risk | No mention of blinding. Lack of blinding less likely to affect these outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | Participant flow diagram provided; similar and modest losses in each group. |
| Incomplete outcome data (attrition bias) | Low risk | Ditto ‐ data reported. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge this. |
| Balance in baseline characteristics? | Unclear risk | No indication of any major baseline imbalance in 51 participants followed up at 3 years but no data for 6 participants lost to follow‐up. |
| Free from performance bias? | Low risk | All surgical procedures performed by senior surgeon and comparable rehabilitation. Although general anaesthesia used only for the plate group, this was considered unlikely to affect the findings.. |
| Methods | Method of randomisation: sealed envelopes | |
| Participants | Huddinge University Hospital, Stockholm, Sweden | |
| Interventions | Interventions started: surgery within 48 hours. | |
| Outcomes | Length of follow‐up: 3 to 5 years (listed as 50 months in trial report; patient questionnaire, clinical and radiological assessment); also after treatment and at 1 year: | |
| Notes | Both groups had the same physiotherapy regimen. Zyto's response to a letter from H. A. Karladani admits that there may have been some inaccuracy in their classification of the fracture patterns but stressed that the Neer classification system was flawed and that other factors such as osteoporotic bone need to be considered too. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomised by sealed envelopes" |
| Allocation concealment (selection bias) | Unclear risk | "randomised by sealed envelopes" (at time of admission) No indication of safeguards. |
| Blinding (performance bias and detection bias) | High risk | Some independent assessment by radiographer and potentially by main author but no blinding. |
| Blinding (performance bias and detection bias) | Unclear risk | No blinding but may not have affected appraisal of mortality (which was not split by treatment group). |
| Incomplete outcome data (attrition bias) | Unclear risk | Post‐randomisation exclusions and moderately large loss to follow‐up (14/43 = 32%; (11/40 = 28%)). |
| Incomplete outcome data (attrition bias) | High risk | Only whole group data presented for deaths out of 40 participants. |
| Selective reporting (reporting bias) | High risk | Insufficient information to judge this but some post‐randomisation exclusions and final follow‐up performed by first author who does not appear in the earlier reports of the trial. |
| Balance in baseline characteristics? | Low risk | No important imbalances in baseline characteristics. |
| Free from performance bias? | Low risk | No indications of serious performance bias: surgery performed by orthopaedic specialists who were experienced in the surgical technique. |
AO = Arbeitsgemeinschaft fur Osteosynthesefragen / Association for the Study of Internal Fixation (or ASIF)
AVN = avascular necrosis
A&E = accident and emergency
MI = myocardial infarction
PE = pulmonary embolism
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| This was a randomised clinical trial (sealed envelopes ‐ computer generated sequence ‐ held in a box), recruitment 03/11/1997 to 14/01/1999, that compared Rush pins fixation with Polaris nail fixation of displaced two part fractures of the proximal humerus. Contact with a Dr Sharma in July 2000 revealed 65 of the 80 patients in the trial had reached 2 year follow‐up. Abstract by Bing et al published in 2002 indicated 40 patients of whom 30 had been followed‐up for one year. Information gained via Alison Armstrong from Grahame Taylor (one of the authors of the Bing abstract) indicated that there were some concerns about the extent of missing data. Both groups had a high reoperation rate to remove metal ware causing impingement. This trial has been excluded because of insufficient data. It seems very likely, based on location and study dates, that the trial registration (Der Tavitian 2006) formerly awaiting classification is for this trial. | |
| No proximal humeral fractures in a randomised trial of humeral shaft fracture treatment. | |
| This is listed in the National Research Register as a multi‐centre randomised trial of the management of displaced surgical neck and displaced shaft fractures of the humerus with the Halder humeral nail. Contact with Mr Brownson revealed this to be part of the trial run from Nottingham (seeWallace 2000) which had been abandoned. Mr Brownson indicated that the very specific inclusion criteria (2‐part fractures with over 50% displacement) had reduced the potential sample size; patient consent had also been a problem. | |
| This is a prospective comparison of MIROS (Minimally Invasive Reduction and Osteosynthesis System®) versus traditional percutaneous pinning, each intervention being carried out at one of two hospitals in the same town in Italy. Not randomised. | |
| No proximal humeral fractures in a randomised trial of humeral shaft fracture treatment. | |
| No proximal humeral fractures in a quasi‐randomised trial of humeral shaft fracture treatment. | |
| This is a multi‐centre comparative study of locked internal fixators and non‐operative treatment. Not randomised. | |
| Trial abandoned. This randomised trial (random number sheets that are remotely administered) compared hemiarthroplasty versus fixation (generally suture reinforced with wires) versus conservative treatment (manipulation, sling for 2 weeks, then mobilisation) for 3‐ and 4‐part fractures of the proximal humerus. Trial started in 2001, with one year follow‐up (outcome was assessed by independent physiotherapists). Aimed for 90 to 100 participants, aged > 45 years. Contact with Alison Armstrong revealed that recruitment stalled at 11 patients (16 refusals) in 2008; centre stopped trial when it became a trial site for the ProFHER trial. | |
| Article mentions an abandoned randomised trial comparing "operative versus conservative care" which was unsuccessful "because patients insisted on proactively choosing rather than being assigned to a treatment group by lot"." No other details given. | |
| This is listed in the National Research Register as a randomised trial comparing conservative treatment and hemiarthroplasty for four‐part fractures of the proximal humerus. Contact with Mr Flannery revealed his centre failed to recruit anyone into the trial. Mr Turner, the lead investigator of the multi‐centre trial, involving the South Thames Shoulder and Elbow Group, confirmed that the trial was abandoned due to the inability to recruit patients. | |
| Prospective study involving 152 patients with unilateral displaced and unstable proximal humeral fractures treated either with an antegrade angular and sliding stable proximal interlocking nail or an angular stable plate. Not a randomised or quasi‐randomised trial. | |
| This is listed in the National Research Register as a randomised trial comparing conservative treatment and the Halder humeral nail for displaced fractures of the surgical neck and shaft of the humerus. Contact with Mr Hems revealed this to be part of the trial run from Nottingham (seeWallace 2000). Mr Hems indicated that they had had considerable difficulty in recruiting patients (only those with proximal humeral fractures were eligible in his centre) and had no results. | |
| While the English abstract claims that "70 senile patients" were "randomly divided into three groups to receive different surgical methods" the distribution and characteristics (age and fracture type) of the patients in the three groups indicated serious selection bias and implied this was not a randomised trial. For example: "21 patients in the group A receiving Kirschner tension band or screw internal fixation, 37 patients in group B receiving internal fixation of locking proximal humeral plate, and 12 patients in group C receiving humeral head replacement." There was no reply to request for clarification from the lead author. | |
| Contact with a trialist revealed that due to the discovery of problems with randomisation it was decided not to proceed with publication as the trial results could be compromised. | |
| This was originally registered as a randomised controlled trial comparing a plate with a hemiarthroplasty. However, it is now registered as a prospective study of fixation with a PHILOS plate. Inger Mechlenburg confirmed that no patients had been included in the trial ‐ the trial was abandoned because no funding was obtained. | |
| There has been no response from the lead author of this ‘trial’ (last contact attempted 8 June 2012), which appears to have been reported in a conference abstract only. In 2003, 50 patients with 3‐ and 4‐part fractures and fracture dislocations of the proximal humerus were "random selected" for surgery (closed or open reduction and external fixation or hemiarthroplasty) or conservative treatment. The very limited results are split descriptively according to three groups (2 reflecting the 2 different surgical methods). There is currently insufficient evidence to support this being a randomised trial. | |
| This is listed in the National Research Register Archive as a randomised trial comparing the T2 proximal humeral nail with the PHILOS plate system in patients with 2‐ or 3‐part proximal humeral fractures. the recruitment target was 100 patients (between 01/09/2005 to 01/09/2007), and follow‐up was 16 weeks. We have not located any other report of this study than the details provided in the National Research Register (UK) by, at that time, a Trauma and Orthopaedic Registrar who has now moved to another hospital. There was no response to a request for further information sent 8/6/2012. There is no indication that this study, which may not have started, will ever be reported. | |
| No proximal humeral fractures in a quasi‐randomised trial of humeral shaft fracture treatment. | |
| This is listed in the National Research Register Archive as a multi‐centre randomised trial of the management of four part fractures of proximal humerus that compared hemiarthroplasty versus conservative treatment. The recruitment target was 200 patients, with a one year follow‐up using the Constant‐Murley shoulder score and Oxford Shoulder score. The listed start and end dates were 01/01/2003 and 01/02/2005. No details were received of the other centres in the very limited further information received from Mr Shah in April 2003. There was no response to a request for further information sent 13/11/06. There is no indication that this study, which may not have started, will ever be reported. | |
| This was registered as a randomised study of reverse shoulder prosthesis and hemiarthroplasty for elderly patients with proximal humeral fractures. However, the principal investigator left the hospital (and country) before it started and a contact at Liverpool (Matthew Smith) confirmed that the study was closed after this. | |
| This is listed in the National Research Register as a multi‐centre randomised trial of the management of displaced surgical neck and displaced shaft fractures of the humerus with the Halder humeral nail. Contact with Prof Wallace's secretary revealed that the study had not gone ahead. The secretary mentioned three other sites (Halifax; Liverpool; and one in Scotland). No reason given. SeeBrownson 2001. | |
| This is a mixed population trial evaluating additional mobilisation therapy that included other fractures (e.g. clavicular and scapular fractures) as well as proximal humeral fractures. This trial was excluded because separate proximal humeral fracture data were not reported and the contact author is unavailable. | |
| A multicentre prospective study but not a randomised trial. | |
| This is listed in the National Research Register as a randomised comparison of operative and non‐operative management of proximal humeral fractures. This trial was abandoned due to poor recruitment, mainly due to lack of patient consent. | |
| Correspondence with the author revealed that this was not a randomised trial. The choice of surgery was dependent on the success of closed reduction. | |
| While the English abstract claims that "58 patients with 3 parts and 4 parts fractures of proximal humerus were randomly treated with AO locked compressive plates (LCP) or humeral head replacement." the characteristics ( fracture type) of the patients in the two groups indicated serious selection bias and implied this was not a randomised trial. Thus, 25 of 28 patients in the plate group had 3 part fractures (1 with a dislocation) and 3 had 4 part fractures (1 with dislocation) whereas 11 of 30 in the replacement group had 3 part fractures (2 with dislocation), 16 with 4 part fractures (4 with dislocation) and the other three had humeral head split fractures. There was no reply to request for clarification from the lead author. |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | "Randomized clinical study" |
| Participants | 54 patients (38 female, 26 male, mean age 61 years) with 2‐part surgical neck fractures or 3‐part valgus impacted fractures |
| Interventions | Surgery involving a titanium plate: 1. Minimally invasive fixation based on anterolateral deltoid split approach and percutaneous reduction |
| Outcomes | Constant score, instrumental activities of daily living, pain (VAS), range of motion, union, complications |
| Notes | Requests for further information sent to Dr Battistella (8 and 14 May 2012) were unsuccessful. |
| Methods | Randomised trial; 4 centres |
| Participants | 110 patients |
| Interventions | 1. Reversed shoulder prosthesis 2. ORIF with PHILOS plate |
| Outcomes | Primary / secondary outcomes will be: Constant score, possibly the Oxford Shoulder score, a QoL score, the “15D”, and a short patient self‐evaluation score in addition to the X‐ray and CT 3D scans |
| Notes | Proposal for this new trial was being finalised in May 2012 (personal communication from Tore Fjalestad) |
| Methods | Patients were randomly allocated via a random numbers table. |
| Participants | 60 patients (32 females, 28 males; age range: 39 to 62 years) treated operatively for fracture of the surgical neck of the humerus. |
| Interventions | 1. Acupuncture (electroacupuncture and infrared radiation) plus passive exercise of the shoulder joint Treatment lasted 1 month. |
| Outcomes | Follow‐up: 1 month |
| Notes | Trial in Chinese with English abstract. Translation of methods section (1.1) confirmed that this was a randomised trial. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Randomised study between intramedullary locking nails and locking plates for treatment of proximal humerus fractures (HUMERUS) |
| Methods | Single centre, randomised controlled trial. Unblinded. |
| Participants | 144 patients, aged between 40 and 85 years, with a type III or IV "cephalotuberosity" proximal humeral fracture (classification of Neer an DUPARC) |
| Interventions | 1. Intramedullary nail (Multilock, Synthes) 2. Locking plate (SURFIX, Integra) |
| Outcomes | Follow‐up: 1 year |
| Starting date | Start date: February 2012 |
| Contact information | Dr Patrick Boyer |
| Notes |
| Trial name or title | Effect of osteosynthesis, primary hemiarthroplasty, and non‐surgical management for displaced four‐part fractures of the proximal humerus in elderly: a multi‐centre, randomised clinical trial |
| Methods | Multi‐centre, randomised clinical trial (central randomisation unit) |
| Participants | 162 patients with displaced 4‐part fractures of the proximal humerus |
| Interventions | 1. Hemiarthroplasty |
| Outcomes | Follow‐up: 3 years (primary outcome: 1 year) |
| Starting date | Start date: April 2009 |
| Contact information | Dr Stig Brorson |
| Notes | Published protocol. * Correspondence from Stig Brorson (June 11 2012) reveals a slower than anticipated recruitment, |
| Trial name or title | Arthroplasty in three‐ and four‐part proximal humerus fracture: hemi or reverse? Prospective multi‐centre randomised clinical trial |
| Methods | Multi‐centre, randomised controlled trial. Unblinded. |
| Participants | 52 patients aged over 65 years with displaced 3 or 4 part proximal humerus fractures who are candidates for primary shoulder arthroplasty. |
| Interventions | 1. Aequalis fracture prosthesis 2. Aequalis reverse fracture prosthesis |
| Outcomes | Follow‐up: 1 year Primary outcome: Constant Shoulder Score Secondary outcomes: DASH (Disabilities of the Arm, Shoulder, and Hand) Score, SF‐12 questionnaire, Visual Analogue Score of pain |
| Starting date | Start date: July 2010 Estimated completion date: December 2014 |
| Contact information | Yde Engelsma Medisch Centrum Alkmaar Wilhelminalaan 12 1815 JD Alkmaar The Netherlands |
| Notes |
| Trial name or title | A multicentre prospective randomized control trial on the treatment of three and four part proximal humerus fractures in patients 70 years and older: comparing open reduction and internal fixation with non operative treatment |
| Methods | Randomised controlled trial: "randomly (like flipping a coin)" |
| Participants | 120 patients aged 70 years or over with a 3 or 4 part fracture. |
| Interventions | 1. Open reduction and internal fixation |
| Outcomes | Follow‐up: 1 year |
| Starting date | November 2010 |
| Contact information | Contact: Raman Johal ([email protected]) |
| Notes | As of registration update (17/02/2011) the study was recruiting. Start and end dates amended. |
| Trial name or title | Effectiveness and cost‐effectiveness of operative and conservative treatment of comminuted fractures of the proximal humerus. A randomised, controlled study. |
| Methods | Randomised single blind (outcomes assessor) |
| Participants | 150 older patients with comminuted, displaced fractures of the proximal humerus. Inclusion criteria: Age over 65 years; acute trauma with randomisation within 7 days of injury; 3‐ or 4‐part fracture with > 5 mm dislocation of the anatomic neck (AO classification C1‐2 for non‐luxation fractures; C3 for luxation fractures) |
| Interventions | 1. PHILOS locking plate: open reduction of the fracture (and GH joint), internal fixation with the PHILOS locking plate. Tuberculum fragments are sutured to the plate with thick non‐absorbable suture. |
| Outcomes | Follow‐up: 24 months |
| Starting date | November 2010 |
| Contact information | Tuomas Lähdeoja, MD: [email protected] Helsinki University, Helsinki, Finland |
| Notes | As of registration update (22/01/2012) the study was recruiting. Start and end dates amended. |
| Trial name or title | Hemiarthroplasty versus osteosynthesis in humeral fractures (HOMERUS): A multicentre randomised trial |
| Methods | Multi‐centre, randomised clinical trial. Single blinded (outcomes assessor). |
| Participants | 134 patients aged over 60 years with displaced 3 and 4 part proximal humeral fractures with more than 5 mm of dislocation in one of the fracture planes. |
| Interventions | 1. Hemiarthroplasty 2. Angle stable locking compression plate osteosynthesis |
| Outcomes | Follow‐up: 2 years Primary outcome: DASH (Disabilities of the Arm, Shoulder, and Hand) Score Secondary outcomes: VAS (Visual analogue score) for pain and patient satisfaction, Constant‐Murley Score, SF‐36, Radiographic evaluation, complications |
| Starting date | Start date: September 2010 Anticipated completion date: August 2012 |
| Contact information | Dr PA Verbeek Department of Orthopaedic Surgery University Medical Centre Groningen (UMCG) Groningen The Netherlands |
| Notes |
| Trial name or title | A randomised clinical trial comparing a lateral minimally invasive approach and the traditional anterior approach for plating of proximal humerus fractures |
| Methods | Randomised, single blind (outcome assessors), clinical trial |
| Participants | 90 patients, with humeral surgical neck fracture, Neer II valgus‐type, and Neer III. |
| Interventions | 1. Lateral minimally invasive approach (plate fixation) |
| Outcomes | Follow‐up: 3, 6, and 12 weeks, and at 6, 12, 18 and 24 months |
| Starting date | Start date: November 2007 |
| Contact information | Marie‐France Poirer |
| Notes | Entry for trial (clinicaltrials.gov) on April 10 2012, indicated that "The recruitment status of this study is unknown because the information has not been verified recently" |
| Trial name or title | Clinical outcome comparison between medial and lateral offset reverse shoulder arthroplasty |
| Methods | Randomised single blinded trial |
| Participants | 40 patients aged between the ages of 50 and 95 years of age who are a candidate for a reverse shoulder arthroplasty. This includes patients with rotator cuff tear arthroplasty, irreparable rotator cuff tears, significant proximal humerus fractures and malunions, and chronic proximal humerus dislocators. |
| Interventions | Tornier Reversed shoulder arthroplasty: |
| Outcomes | Follow‐up: 2 years Shoulder functional score |
| Starting date | May 2010 End date: April 2012 |
| Contact information | Wesley Phipatanakul, MD Principal investigator: Montri D Wongworawat, MD, |
| Notes | The future inclusion of this mixed population trial will depend on the numbers of participants with proximal humeral fractures. |
| Trial name or title | Effectiveness of intensive rehabilitation on shoulder function after a fracture of the proximal humerus treated by locked plate. A prospective randomized study |
| Methods | Randomised clinical trial |
| Participants | 80 patients aged over 18 years treated by PHILOS locked plate system for unstable closed fracture of the proximal humerus (two‐part and three‐part fractures according to the Neer classification) within 7 days on injury. |
| Interventions | 1. Early and intensive exercise programme versus 1. Standard rehabilitation programme |
| Outcomes | Length of follow‐up: 12 months |
| Starting date | December 2009 |
| Contact information | Hélène Côté, Reg. Nurse: [email protected] |
| Notes |
| Trial name or title | Primary hemiarthroplasty versus conservative treatment for comminuted fractures of the proximal humerus in the elderly (ProCon) ‐ a multicenter randomized trial |
| Methods | Randomised trial: "variable block randomisation will be accomplished via a trial website" |
| Participants | Patients (65 years or older) with a comminuted proximal humeral fracture. 80 patients (65 years or older) with a comminuted proximal humeral fracture: three‐part (Hertel classification type 9, 10, 11), four‐part (Hertel type 12), anatomical neck (Hertel type 2), or split‐head fractures of the humeral head |
| Interventions | 1. Hemiarthroplasty (Affinis® Fracture shoulder endoprosthesis) |
| Outcomes | Follow‐up: 1, 3 and 6 weeks, and 3, 6, 12 and 24 months Primary outcome (Constant Score) and secondary outcomes (DASH, pain, radiographic healing, secondary intervention rates, complication rates, mortality rates, SF‐36, and EQ‐5D) |
| Starting date | Start date: 15 June 2009 |
| Contact information | Dennis Den Hartog |
| Notes | Published protocol |
| Trial name or title | Pragmatic multi‐centre randomised trial of surgical versus non‐surgical treatment for proximal fracture of the humerus in adults |
| Methods | Multi‐centre randomised controlled trial |
| Participants | 250 patients, aged 16 or above, presenting to the participating trauma centre within 3 weeks of their injury with a radiologically confirmed displaced fracture of the proximal humerus involving the surgical neck |
| Interventions | 1. Surgery (fixation or joint replacement) |
| Outcomes | Follow‐up: 6, 12 and 24 months |
| Starting date | Start date: 1/10/2009 |
| Contact information | Prof Amar Rangan |
| Notes | Published protocol. Extension to recruitment period has resulted in a delay to the completion date (28/02/2014). Recruitment target achieved. |
| Trial name or title | Early vs delayed physical therapy (exercises) for non‐operatively‐treated proximal humerus fractures: a prospective randomized trial |
| Methods | Randomised trial |
| Participants | 60 patients, aged 18 years or over, with non‐operatively treated proximal humeral fractures |
| Interventions | 1. Physical therapy started immediately after diagnosis of injury |
| Outcomes | Follow‐up: 6 months |
| Starting date | Start date: February 2005 |
| Contact information | Prof David Ring |
| Notes | Changes to NCT00438633 on 27 May 2008 seemed to indicate that, despite its official title, this is now a prospective cohort study (accessed: April 10 2012). David Ring confirmed it was still an RCT (April 16 2012). |
| Trial name or title | Minimally invasive versus standard open reduction of proximal humerus fractures |
| Methods | Single‐centre, randomised controlled trial. Computer generated random list. Unblinded. |
| Participants | 90 patients with displaced proximal humeral fractures |
| Interventions | 1. Minimally invasive approach with closed reduction and temporary fixation with k‐wires, then the limited deltoid splitting approach (locking plate) |
| Outcomes | Follow‐up: 1 year Primary outcome: Constant Shoulder Score and DASH (Disabilities of the Arm, Shoulder, and Hand) Score Secondary outcomes: radiographic outcomes, complications, union rate |
| Starting date | Anticipated start date: October 2010 (however, study is not yet recruiting |
| Contact information | Jeremy Stanley 14 Grand Drive Remuera Auckland 1050 New Zealand |
| Notes | Trial was not recruiting (nor ethics approval) at time of registration (02/09/2010) |
| Trial name or title | Treatment of Proximal Humeral Fractures (TPHF) |
| Methods | Multi‐centre, randomised clinical trial. Single blinded (outcomes assessor) |
| Participants | 290 patients aged over 60 years with displaced 2‐, 3‐ and 4‐part proximal humeral fractures |
| Interventions | 1. PHILOS locking plate 2. Epoca prosthesis |
| Outcomes | Follow‐up: 2 years Primary outcome: DASH (Disabilities of the Arm, Shoulder, and Hand) score Secondary outcome: EQ‐5D Questionnaire |
| Starting date | Start date: January 2011 Estimated completion date: September 2016 |
| Contact information | Antti Launonen Tampere University Hospital Tampere Pirkanmaa Finland, 33521 |
| Notes | As of registration update (01/02/2011), trial was recruiting in Tampere University Hospital, but recruitment had not started in Oulu or Kuopio |
AO = Arbeitsgemeinschaft fur Osteosynthesefragen / Association for the Study of Internal Fixation (or ASIF)
LCP = Locking compression plate
NRR = National Research Register
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Shoulder disability: Croft Shoulder Disability Score Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 1 Shoulder disability: Croft Shoulder Disability Score. | ||||
| 1.1 Disability (1 or more problems) at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Severe disability (5 or more problems) at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Disability (1 or more problems) at 2 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Severe disability (5 or more problems) at 2 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Croft shoulder disability score: individual problems at 2 years Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 2 Croft shoulder disability score: individual problems at 2 years. | ||||
| 2.1 Pain on movement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Bathing difficulties | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Change position at night more often | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Disturbed sleep | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 No active pastimes or usual physical recreation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Lifting problems | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.7 Help needed | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.8 More accidents (e.g. dropping things) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of treatment sessions (until independent function achieved) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 3 Number of treatment sessions (until independent function achieved). | ||||
| 4 SF‐36 scores: pain & physical dimensions Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 4 SF‐36 scores: pain & physical dimensions. | ||||
| 4.1 Physical functioning (0‐100: excellent) at 16 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Physical functioning (0‐100: excellent) at 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Role limitation physical (0‐100: none) at 16 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Role limitation physical (0‐100: none) at 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Pain (0‐100: none) at 16 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.6 Pain (0‐100: none) at 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Adverse events Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 5 Adverse events. | ||||
| 5.1 Frozen shoulder | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Fracture displacement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.4 Reflex sympathetic dystrophy | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.5 Treated (injection) subacromial impingement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Constant shoulder score (ratio of affected/unaffected arm) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.6  Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 6 Constant shoulder score (ratio of affected/unaffected arm). | ||||
| 6.1 8 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 16 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Constant shoulder score (0 to 100: best) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.7  Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 7 Constant shoulder score (0 to 100: best). | ||||
| 7.1 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.4 6 months: subjective assessment (0 to 35: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.5 6 months: objective assessment range of motion and strength (0 to 65: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Changes in pain intensity (mm) from baseline: 100 mm visual analogue scale (positive change = less pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.8  Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 8 Changes in pain intensity (mm) from baseline: 100 mm visual analogue scale (positive change = less pain). | ||||
| 8.1 At 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 At 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Range of motion at 6 months (degrees): difference between two shoulders Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.9  Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 9 Range of motion at 6 months (degrees): difference between two shoulders. | ||||
| 9.1 Abduction | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Anterior elevation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Lateral rotation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Patient dissatisfied with treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.10  Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 10 Patient dissatisfied with treatment. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Problems with bandages Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Gilchrist bandage versus 'Classic' Desault bandage, Outcome 1 Problems with bandages. | ||||
| 1.1 Application of bandage was uncomfortable | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Premature bandage removal | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Fracture displacement by 3 weeks Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 Gilchrist bandage versus 'Classic' Desault bandage, Outcome 2 Fracture displacement by 3 weeks. | ||||
| 3 Poor or bad rating by patient at fracture consolidation Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 Gilchrist bandage versus 'Classic' Desault bandage, Outcome 3 Poor or bad rating by patient at fracture consolidation. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain at one year (scale 0 to 8: maximum pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 1 Pain at one year (scale 0 to 8: maximum pain). | ||||
| 2 Severe or moderate pain at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.2  Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 2 Severe or moderate pain at 3 months. | ||||
| 3 Requested change of therapy Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.3  Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 3 Requested change of therapy. | ||||
| 4 Adverse events (frozen shoulder: 1 v 2; unexplained prolonged pain: 0 v 1) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.4  Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 4 Adverse events (frozen shoulder: 1 v 2; unexplained prolonged pain: 0 v 1). | ||||
| 5 Neer's rating (0 to 100: best) at mean 16 months (exploratory analysis) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.5  Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 5 Neer's rating (0 to 100: best) at mean 16 months (exploratory analysis). | ||||
| 6 Active gleno‐humeral elevation (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.6  Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 6 Active gleno‐humeral elevation (degrees). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||
| 1 Functional scores at 12 months (higher = worse) Show forest plot | 3 | 153 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.42, 0.22] | ||||||||||||||||||||
| Analysis 4.1  Comparison 4 Surgery versus conservative treatment, Outcome 1 Functional scores at 12 months (higher = worse). | ||||||||||||||||||||||||
| 1.1 DASH (0 to 100: worst disability) (reversed) | 2 | 105 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.57, 0.19] | ||||||||||||||||||||
| 1.2 ASES (0 to 24: best) | 1 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.46, 0.67] | ||||||||||||||||||||
| 2 DASH (0 to 100: worst disability) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||
| Analysis 4.2  Comparison 4 Surgery versus conservative treatment, Outcome 2 DASH (0 to 100: worst disability). | ||||||||||||||||||||||||
| 2.1 at 4 months | 2 | 106 | Mean Difference (IV, Fixed, 95% CI) | 0.91 [‐7.00, 8.83] | ||||||||||||||||||||
| 2.2 at 12 months | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐4.51 [‐13.50, 4.48] | ||||||||||||||||||||
| 2.3 at 24 months | 2 | 99 | Mean Difference (IV, Fixed, 95% CI) | ‐7.43 [‐16.26, 1.41] | ||||||||||||||||||||
| 3 American Shoulder and Elbow Surgeons score (0 to 24: best) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.3  Comparison 4 Surgery versus conservative treatment, Outcome 3 American Shoulder and Elbow Surgeons score (0 to 24: best). | ||||||||||||||||||||||||
| 3.1 at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 3.2 at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 4 Activities of daily living Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.4  Comparison 4 Surgery versus conservative treatment, Outcome 4 Activities of daily living. | ||||||||||||||||||||||||
| 4.1 Unable to manage personal hygiene at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 4.2 Unable to comb hair at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 4.3 Unable to sleep on fractured side at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 4.4 Unable to carry 5 kg at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 4.5 Unable to manage personal hygiene at 50 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 4.6 Unable to comb hair at 50 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 4.7 Unable to sleep on fractured side at 50 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 4.8 Unable to carry 5 kg at 50 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 5 Quality of life assessment: EuroQol (0: dead to 1: best health) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||
| Analysis 4.5  Comparison 4 Surgery versus conservative treatment, Outcome 5 Quality of life assessment: EuroQol (0: dead to 1: best health). | ||||||||||||||||||||||||
| 5.1 at 3 to 4 months | 3 | 156 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.02, 0.05] | ||||||||||||||||||||
| 5.2 at 6 months | 3 | 156 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.01, 0.08] | ||||||||||||||||||||
| 5.3 at 12 months | 3 | 153 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.01, 0.08] | ||||||||||||||||||||
| 5.4 at 24 months | 2 | 101 | Mean Difference (IV, Fixed, 95% CI) | 0.15 [0.05, 0.25] | ||||||||||||||||||||
| 6 Quality of life assessment (Fjalestad 2010 data) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.6  Comparison 4 Surgery versus conservative treatment, Outcome 6 Quality of life assessment (Fjalestad 2010 data). | ||||||||||||||||||||||||
| 6.1 15D at 3 months (0: death; 1: perfect health) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 6.2 15D at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 6.3 15D at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 6.4 number of QALYs at 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 6.5 numbers of QALYs at 1 year (‐ deaths) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 7 Mortality Show forest plot | 4 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.55, 4.36] | ||||||||||||||||||||
| Analysis 4.7  Comparison 4 Surgery versus conservative treatment, Outcome 7 Mortality. | ||||||||||||||||||||||||
| 8 Additional surgery (re‐operation or secondary surgery) Show forest plot | 5 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.36 [1.33, 8.49] | ||||||||||||||||||||
| Analysis 4.8  Comparison 4 Surgery versus conservative treatment, Outcome 8 Additional surgery (re‐operation or secondary surgery). | ||||||||||||||||||||||||
| 8.1 at 6 to 12 months | 3 | 113 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.90 [0.54, 6.73] | ||||||||||||||||||||
| 8.2 at 2 years | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.83 [1.38, 24.70] | ||||||||||||||||||||
| 9 Adverse events / complications Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||
| Analysis 4.9  Comparison 4 Surgery versus conservative treatment, Outcome 9 Adverse events / complications. | ||||||||||||||||||||||||
| 9.1 Infection | 6 | 259 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.13 [0.91, 18.87] | ||||||||||||||||||||
| 9.2 Nerve injury / palsy | 3 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.20, 2.76] | ||||||||||||||||||||
| 9.3 Non union | 5 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.16, 1.40] | ||||||||||||||||||||
| 9.4 Avascular necrosis | 5 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.37, 1.16] | ||||||||||||||||||||
| 9.5 Post‐traumatic osteoarthritis (signs of) | 3 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.21, 1.51] | ||||||||||||||||||||
| 9.6 Screw penetration into joint | 3 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.49 [2.25, 58.76] | ||||||||||||||||||||
| 9.7 Impingement | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 20.86] | ||||||||||||||||||||
| 9.8 Redisplacement resulting in an operation | 2 | 81 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.03, 2.22] | ||||||||||||||||||||
| 9.9 Secondary dislocation or resorption of the greater tuberosity | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 15.18 [0.92, 249.78] | ||||||||||||||||||||
| 9.10 Tuberosity displacement at 50 months | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.71] | ||||||||||||||||||||
| 9.11 Wire penetration at 1 year | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 69.31] | ||||||||||||||||||||
| 9.12 Fixation failure resulting in an operation | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.30] | ||||||||||||||||||||
| 9.13 Refracture | 1 | 22 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 14.05] | ||||||||||||||||||||
| 10 Constant scores (overall: 0 to 100: best score) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||
| Analysis 4.10  Comparison 4 Surgery versus conservative treatment, Outcome 10 Constant scores (overall: 0 to 100: best score). | ||||||||||||||||||||||||
| 10.1 at 4 months | 2 | 107 | Mean Difference (IV, Fixed, 95% CI) | ‐1.33 [‐6.80, 4.14] | ||||||||||||||||||||
| 10.2 at 12 months | 3 | 152 | Mean Difference (IV, Fixed, 95% CI) | 2.36 [‐3.52, 8.24] | ||||||||||||||||||||
| 10.3 at 24 months | 2 | 101 | Mean Difference (IV, Fixed, 95% CI) | 0.48 [‐7.26, 8.22] | ||||||||||||||||||||
| 10.4 at 50 months | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐5.0 [‐17.52, 7.52] | ||||||||||||||||||||
| 11 Constant scores (difference between injured and uninjured shoulder): Normal = 0. Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.11  Comparison 4 Surgery versus conservative treatment, Outcome 11 Constant scores (difference between injured and uninjured shoulder): Normal = 0.. | ||||||||||||||||||||||||
| 11.1 at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 11.2 at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 12 Poor or unsatisfactory function at 1 year (Neer rating) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.12  Comparison 4 Surgery versus conservative treatment, Outcome 12 Poor or unsatisfactory function at 1 year (Neer rating). | ||||||||||||||||||||||||
| 13 Dependent in activities of daily living (or dead) at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.13  Comparison 4 Surgery versus conservative treatment, Outcome 13 Dependent in activities of daily living (or dead) at 6 months. | ||||||||||||||||||||||||
| 14 Pain at 2 years: VAS (0 to 100: worst pain) Show forest plot | 2 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐6.38 [‐14.18, 1.41] | ||||||||||||||||||||
| Analysis 4.14  Comparison 4 Surgery versus conservative treatment, Outcome 14 Pain at 2 years: VAS (0 to 100: worst pain). | ||||||||||||||||||||||||
| 15 Constant score at 50 months: overall and components Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.15  Comparison 4 Surgery versus conservative treatment, Outcome 15 Constant score at 50 months: overall and components. | ||||||||||||||||||||||||
| 15.1 Overall score (0‐100: best score) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 15.2 Pain (maximum score 15) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 15.3 Range of motion (maximum score 40) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 15.4 Power (maximum score 25) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 15.5 Activities of daily living (maximum score 20) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 16 Constant (often severe) pain at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.16  Comparison 4 Surgery versus conservative treatment, Outcome 16 Constant (often severe) pain at 6 months. | ||||||||||||||||||||||||
| 17 Failure to recover 75% muscle power relative to other arm (survivors) at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.17  Comparison 4 Surgery versus conservative treatment, Outcome 17 Failure to recover 75% muscle power relative to other arm (survivors) at 6 months. | ||||||||||||||||||||||||
| 17.1 Flexion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 17.2 Abduction | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 17.3 Lateral rotation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 18 Range of movement impairments in survivors at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.18  Comparison 4 Surgery versus conservative treatment, Outcome 18 Range of movement impairments in survivors at 6 months. | ||||||||||||||||||||||||
| 18.1 Flexion < 45 degrees | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 18.2 Unable to place thumb on mid spine (T12) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 18.3 Lateral rotation < 5 degrees | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 19 Costs at 1 year (Euros in 2005) Show forest plot | Other data | No numeric data | ||||||||||||||||||||||
| Analysis 4.19
Comparison 4 Surgery versus conservative treatment, Outcome 19 Costs at 1 year (Euros in 2005). | ||||||||||||||||||||||||
| 20 Total costs including indirect costs (Euros) at 1 year Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 4.20  Comparison 4 Surgery versus conservative treatment, Outcome 20 Total costs including indirect costs (Euros) at 1 year. | ||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||
| 1 American Shoulder and Elbow Surgeons (ASES) score (0 to 100: best) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 5.1  Comparison 5 Locking plate versus locking intramedullary nail, Outcome 1 American Shoulder and Elbow Surgeons (ASES) score (0 to 100: best). | ||||||||||||||||||||||||
| 1.1 At 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 1.2 At 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 2 Death, re‐operation and adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 5.2  Comparison 5 Locking plate versus locking intramedullary nail, Outcome 2 Death, re‐operation and adverse events. | ||||||||||||||||||||||||
| 2.1 Death | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 2.2 Any complication | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 2.3 Screw penetration into humeral head (all had re‐operation) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 2.4 Heterotopic ossification | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 2.5 Infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 2.6 Osteonecrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 2.7 Degenerative change of glenohumeral joint | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 2.8 Secondary varus collapse | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 2.9 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 3 Pain (VAS: 0 to 10: worst) Show forest plot | Other data | No numeric data | ||||||||||||||||||||||
| Analysis 5.3
Comparison 5 Locking plate versus locking intramedullary nail, Outcome 3 Pain (VAS: 0 to 10: worst). | ||||||||||||||||||||||||
| 4 Constant score (0 to 100: best) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 5.4  Comparison 5 Locking plate versus locking intramedullary nail, Outcome 4 Constant score (0 to 100: best). | ||||||||||||||||||||||||
| 4.1 At 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 4.2 At 3 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 5 Active range of motion (at 3 years) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 5.5  Comparison 5 Locking plate versus locking intramedullary nail, Outcome 5 Active range of motion (at 3 years). | ||||||||||||||||||||||||
| 5.1 Forward elevation (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 5.2 External rotation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 6 Range of movement: internal rotation (level on spine) Show forest plot | Other data | No numeric data | ||||||||||||||||||||||
| Analysis 5.6
Comparison 5 Locking plate versus locking intramedullary nail, Outcome 6 Range of movement: internal rotation (level on spine). | ||||||||||||||||||||||||
| 7 Strength of suprapinatus (relative to opposite side) % ‐ at 3 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 5.7  Comparison 5 Locking plate versus locking intramedullary nail, Outcome 7 Strength of suprapinatus (relative to opposite side) % ‐ at 3 years. | ||||||||||||||||||||||||
| 7.1 At 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 7.2 At 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 8 Operation times and blood loss Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 5.8  Comparison 5 Locking plate versus locking intramedullary nail, Outcome 8 Operation times and blood loss. | ||||||||||||||||||||||||
| 8.1 Duration of surgery (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 8.2 Blood loss (ml) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 9 Intra‐operative complication Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||
| Analysis 5.9  Comparison 5 Locking plate versus locking intramedullary nail, Outcome 9 Intra‐operative complication. | ||||||||||||||||||||||||
| 9.1 Pneumothorax | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| 9.2 Blood transfusion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Complications and [slight] malunion Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.1 ![Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 1 Complications and [slight] malunion.](/cdsr/doi/10.1002/14651858.CD000434.pub3/media/CDSR/CD000434/rel0003/CD000434/image_n/nCD000434-CMP-006-01.png) Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 1 Complications and [slight] malunion. | ||||
| 1.1 Any complication | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Malunion (usually slight) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Constant score (% of healthy limb) at mean 2 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.2  Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 2 Constant score (% of healthy limb) at mean 2 years. | ||||
| 3 Time to union and time to recover upper limb function (weeks) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.3  Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 3 Time to union and time to recover upper limb function (weeks). | ||||
| 3.1 Time to radiographic union | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Time to recover normal upper limb function | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Operation and fluoroscopic times Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.4  Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 4 Operation and fluoroscopic times. | ||||
| 4.1 Duration of operation (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 X‐ray exposure (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.5  Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 5 Length of hospital stay (days). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Re‐operation at 1 year Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.1  Comparison 7 Hemi‐arthroplasty versus tension band wiring (4 part fractures), Outcome 1 Re‐operation at 1 year. | ||||
| 2 Implant removal at 1 year Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.2  Comparison 7 Hemi‐arthroplasty versus tension band wiring (4 part fractures), Outcome 2 Implant removal at 1 year. | ||||
| 3 Pain at 1 year Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.3  Comparison 7 Hemi‐arthroplasty versus tension band wiring (4 part fractures), Outcome 3 Pain at 1 year. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 DASH score at 12 months (0 to 100: greatest disability) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.1  Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 1 DASH score at 12 months (0 to 100: greatest disability). | ||||
| 2 Simple shoulder test (0 to 12: best outcome) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.2  Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 2 Simple shoulder test (0 to 12: best outcome). | ||||
| 2.1 At 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 At 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Re‐operation Show forest plot | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.56, 3.67] |
| Analysis 8.3  Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 3 Re‐operation. | ||||
| 3.1 By 6 months | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.15, 4.76] |
| 3.2 By 1 year | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.86 [0.59, 5.88] |
| 4 Dead at 1 year Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.4  Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 4 Dead at 1 year. | ||||
| 5 Constant score at 12 months (% of contralateral limb) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.5  Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 5 Constant score at 12 months (% of contralateral limb). | ||||
| 6 Complications (radiological assessment) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.6  Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 6 Complications (radiological assessment). | ||||
| 6.1 Any complication | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Primary implant malposition | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Secondary loss of reduction and screw perforation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 Non‐union / delayed union due to osteonecrosis (6 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.5 Avascular necrosis at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.6 Varus deformity (> 10 / ≥20 degrees) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.7 Greater tuberosity displacement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.8 Screw cut‐out (intra‐articular) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Range of motion (degrees) at 12 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.7  Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 7 Range of motion (degrees) at 12 months. | ||||
| 7.1 Flexion | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Abduction | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 External rotation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.4 Internal rotation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Operation and fluoroscopic times Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.8  Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 8 Operation and fluoroscopic times. | ||||
| 8.1 Duration of operation (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Fluoroscopic time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 9.1  Comparison 9 Medial support screws versus control for locking plate fixation, Outcome 1 Adverse events. | ||||
| 1.1 Early loss of fixation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Re‐operation for early failure | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Osteonecrosis (asymptomatic) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Constant score (0 to 100: best) at 2.5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 9.2  Comparison 9 Medial support screws versus control for locking plate fixation, Outcome 2 Constant score (0 to 100: best) at 2.5 years. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||||||||||||
| 1 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||||||||||||
| Analysis 10.1  Comparison 10 Hemiarthoplasty: EPOCA prosthesis versus HAS prosthesis, Outcome 1 Adverse events. | ||||||||||||||||||||||||||||||||||
| 1.1 Deep infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||
| 1.2 Persistent pain ‐ scheduled for reoperation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||
| 2 Radiological assessment findings Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||||||||||||
| Analysis 10.2  Comparison 10 Hemiarthoplasty: EPOCA prosthesis versus HAS prosthesis, Outcome 2 Radiological assessment findings. | ||||||||||||||||||||||||||||||||||
| 2.1 Resorption of tuberosities | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||
| 2.2 Secondary dislocation of tuberosities | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||
| 2.3 Superior migration of prosthesis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||
| 2.4 Anterior subluxations | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||
| 2.5 Glenoid erosion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||
| 2.6 Aseptic loosening of stem | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||
| 3 Range of motion results at one year (degrees) Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||
| Analysis 10.3
Comparison 10 Hemiarthoplasty: EPOCA prosthesis versus HAS prosthesis, Outcome 3 Range of motion results at one year (degrees). | ||||||||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Neer score ≤ 80 points (unsatisfactory or failure) at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 11.1  Comparison 11 Post‐operative (percutaneous fixation) immobilisation for 1 week versus 3 weeks, Outcome 1 Neer score ≤ 80 points (unsatisfactory or failure) at 6 months. | ||||
| 2 Premature removal of Kirschner wires Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 11.2  Comparison 11 Post‐operative (percutaneous fixation) immobilisation for 1 week versus 3 weeks, Outcome 2 Premature removal of Kirschner wires. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oxford Shoulder Score at 1 year (adjusted: 0 to 100 best) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 12.1  Comparison 12 Post‐operative (hemiarthroplasty) mobilisation: early (2 weeks immobilisation) versus late (6 weeks), Outcome 1 Oxford Shoulder Score at 1 year (adjusted: 0 to 100 best). | ||||
| 2 Constant shoulder score (at 1 year) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 12.2  Comparison 12 Post‐operative (hemiarthroplasty) mobilisation: early (2 weeks immobilisation) versus late (6 weeks), Outcome 2 Constant shoulder score (at 1 year). | ||||
| 2.1 Overall score (0 to 100: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Pain component (0 to 15: best)) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Activities of daily living component (0 to 25: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Mobility component (0 to 40: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Strength component (0 to 25: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Radiological assessment findings Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 12.3  Comparison 12 Post‐operative (hemiarthroplasty) mobilisation: early (2 weeks immobilisation) versus late (6 weeks), Outcome 3 Radiological assessment findings. | ||||
| 3.1 Nonunion (with bone resorption) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Malunion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Greater tuberosity migration (all had severe pain at 6 & 12 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Superior luxation of prosthesis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Range of motion at 1 year Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 12.4  Comparison 12 Post‐operative (hemiarthroplasty) mobilisation: early (2 weeks immobilisation) versus late (6 weeks), Outcome 4 Range of motion at 1 year. | ||||
| 4.1 Elevation (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 External rotation (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 1 Shoulder disability: Croft Shoulder Disability Score.

Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 2 Croft shoulder disability score: individual problems at 2 years.

Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 3 Number of treatment sessions (until independent function achieved).

Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 4 SF‐36 scores: pain & physical dimensions.

Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 5 Adverse events.

Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 6 Constant shoulder score (ratio of affected/unaffected arm).

Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 7 Constant shoulder score (0 to 100: best).
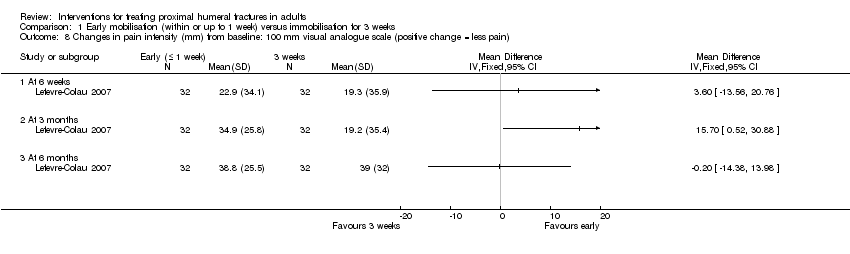
Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 8 Changes in pain intensity (mm) from baseline: 100 mm visual analogue scale (positive change = less pain).

Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 9 Range of motion at 6 months (degrees): difference between two shoulders.

Comparison 1 Early mobilisation (within or up to 1 week) versus immobilisation for 3 weeks, Outcome 10 Patient dissatisfied with treatment.

Comparison 2 Gilchrist bandage versus 'Classic' Desault bandage, Outcome 1 Problems with bandages.
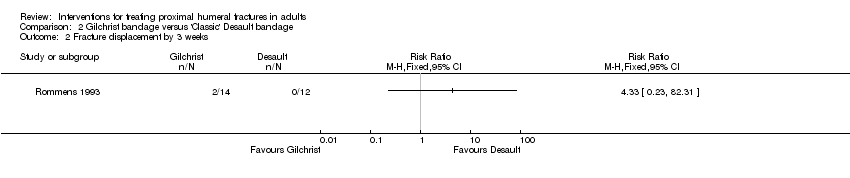
Comparison 2 Gilchrist bandage versus 'Classic' Desault bandage, Outcome 2 Fracture displacement by 3 weeks.
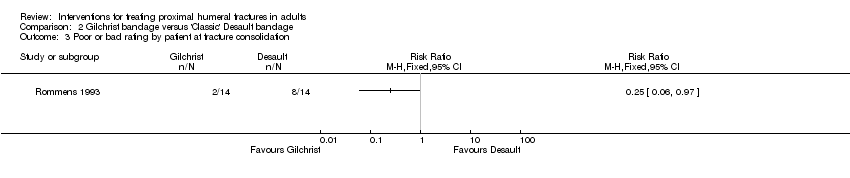
Comparison 2 Gilchrist bandage versus 'Classic' Desault bandage, Outcome 3 Poor or bad rating by patient at fracture consolidation.
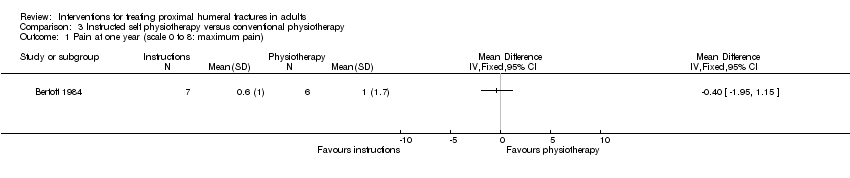
Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 1 Pain at one year (scale 0 to 8: maximum pain).

Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 2 Severe or moderate pain at 3 months.

Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 3 Requested change of therapy.

Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 4 Adverse events (frozen shoulder: 1 v 2; unexplained prolonged pain: 0 v 1).
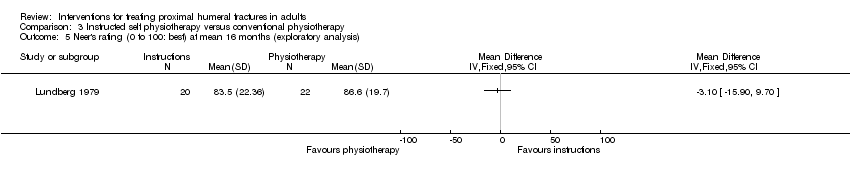
Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 5 Neer's rating (0 to 100: best) at mean 16 months (exploratory analysis).
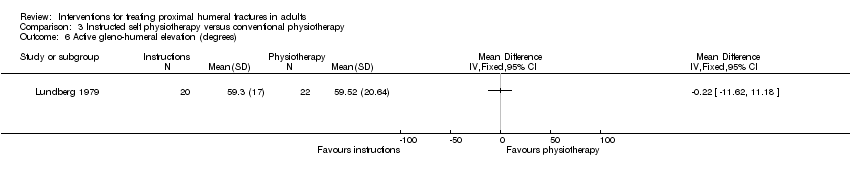
Comparison 3 Instructed self physiotherapy versus conventional physiotherapy, Outcome 6 Active gleno‐humeral elevation (degrees).

Comparison 4 Surgery versus conservative treatment, Outcome 1 Functional scores at 12 months (higher = worse).
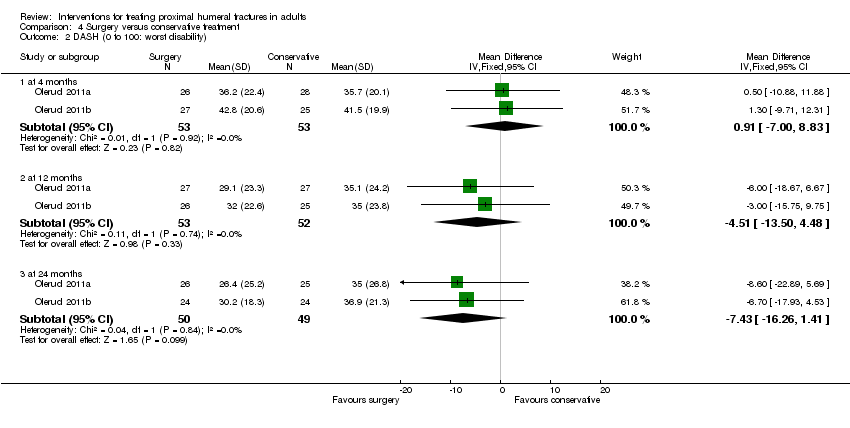
Comparison 4 Surgery versus conservative treatment, Outcome 2 DASH (0 to 100: worst disability).

Comparison 4 Surgery versus conservative treatment, Outcome 3 American Shoulder and Elbow Surgeons score (0 to 24: best).

Comparison 4 Surgery versus conservative treatment, Outcome 4 Activities of daily living.

Comparison 4 Surgery versus conservative treatment, Outcome 5 Quality of life assessment: EuroQol (0: dead to 1: best health).
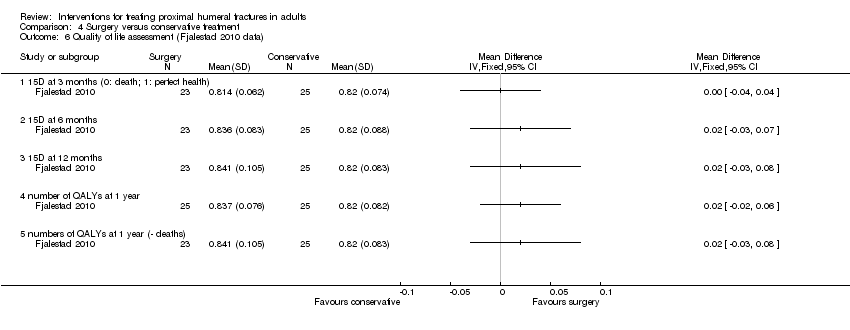
Comparison 4 Surgery versus conservative treatment, Outcome 6 Quality of life assessment (Fjalestad 2010 data).
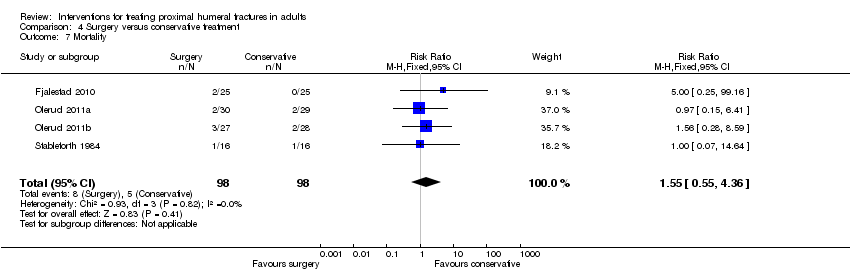
Comparison 4 Surgery versus conservative treatment, Outcome 7 Mortality.
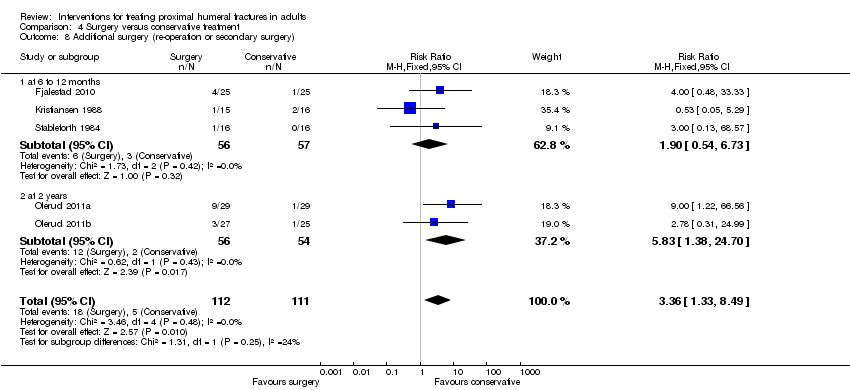
Comparison 4 Surgery versus conservative treatment, Outcome 8 Additional surgery (re‐operation or secondary surgery).

Comparison 4 Surgery versus conservative treatment, Outcome 9 Adverse events / complications.

Comparison 4 Surgery versus conservative treatment, Outcome 10 Constant scores (overall: 0 to 100: best score).

Comparison 4 Surgery versus conservative treatment, Outcome 11 Constant scores (difference between injured and uninjured shoulder): Normal = 0..

Comparison 4 Surgery versus conservative treatment, Outcome 12 Poor or unsatisfactory function at 1 year (Neer rating).
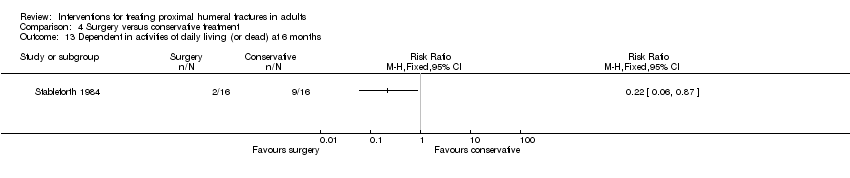
Comparison 4 Surgery versus conservative treatment, Outcome 13 Dependent in activities of daily living (or dead) at 6 months.

Comparison 4 Surgery versus conservative treatment, Outcome 14 Pain at 2 years: VAS (0 to 100: worst pain).
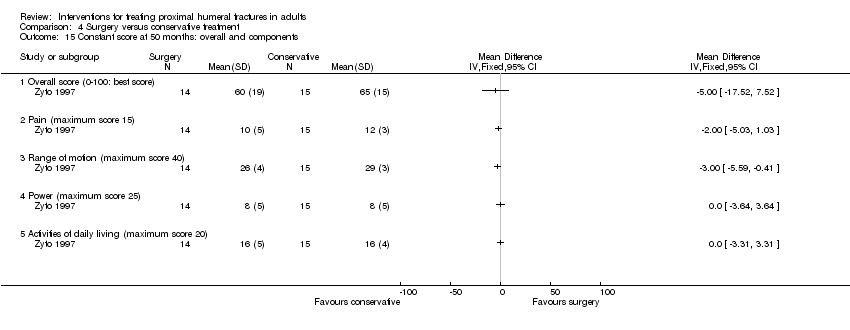
Comparison 4 Surgery versus conservative treatment, Outcome 15 Constant score at 50 months: overall and components.

Comparison 4 Surgery versus conservative treatment, Outcome 16 Constant (often severe) pain at 6 months.

Comparison 4 Surgery versus conservative treatment, Outcome 17 Failure to recover 75% muscle power relative to other arm (survivors) at 6 months.
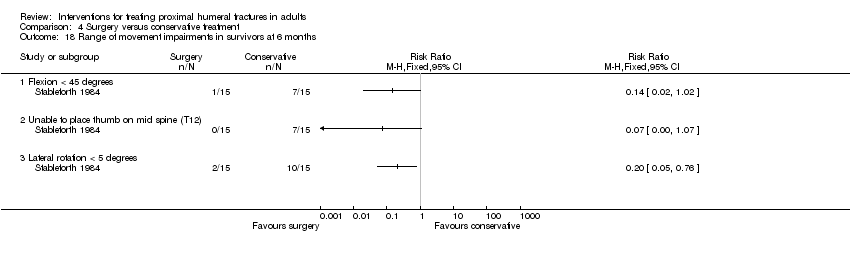
Comparison 4 Surgery versus conservative treatment, Outcome 18 Range of movement impairments in survivors at 6 months.
| Study | Measure | Surgery | Conservative treatment | Difference (conclusion) |
| Fjalestad 2010 | Total health‐care costs | mean = 10,367 | mean = 10,946 | Abstract: "the mean difference in total health‐care costs was 597 Euros in favour of surgery (95% CI = ‐5291, 3777)". No significant difference. |
| Fjalestad 2010 | Health‐care + indirect costs | mean = 23,953 | mean = 21,878 | Reformatted text: "Including indirect costs... the difference [was] 2,075 (95% CI = ‐15,949 to 20,100)". No significant difference, but favours the conservative group. |
Comparison 4 Surgery versus conservative treatment, Outcome 19 Costs at 1 year (Euros in 2005).

Comparison 4 Surgery versus conservative treatment, Outcome 20 Total costs including indirect costs (Euros) at 1 year.

Comparison 5 Locking plate versus locking intramedullary nail, Outcome 1 American Shoulder and Elbow Surgeons (ASES) score (0 to 100: best).

Comparison 5 Locking plate versus locking intramedullary nail, Outcome 2 Death, re‐operation and adverse events.
| Study | Measure | Locking plate | Locking nail | Reported significance |
| Zhu 2011 | Pain at 1 year | median = 0.5 interquartile range: 1.8 n = 29 | median = 1.0 interquartile range = 1.0 | P = 0.042 |
| Zhu 2011 | Pain at 3 years | median = 0 interquartile range = 0.8 | median = 0 interquartile range = 1.0 | P = 0.642 |
Comparison 5 Locking plate versus locking intramedullary nail, Outcome 3 Pain (VAS: 0 to 10: worst).
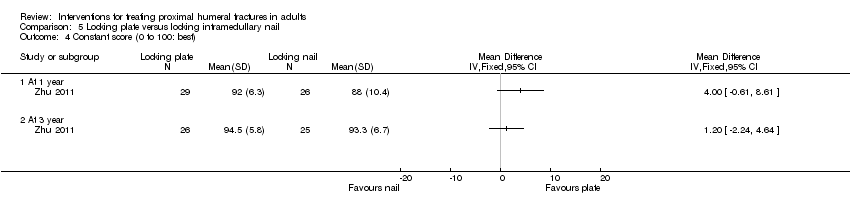
Comparison 5 Locking plate versus locking intramedullary nail, Outcome 4 Constant score (0 to 100: best).

Comparison 5 Locking plate versus locking intramedullary nail, Outcome 5 Active range of motion (at 3 years).
| Study | Measure | Locking plate | Locking nail | Reported significance |
| Zhu 2011 | At 1 year | mean location = T8 range = T4 to L2 | mean location = T9 range = T2 to buttock | P = 0.443 |
| Zhu 2011 | At 3 years | mean location = T8 range = T2 to buttock | mean location = T8 range = T2 to buttock | P = 0.636 |
Comparison 5 Locking plate versus locking intramedullary nail, Outcome 6 Range of movement: internal rotation (level on spine).

Comparison 5 Locking plate versus locking intramedullary nail, Outcome 7 Strength of suprapinatus (relative to opposite side) % ‐ at 3 years.

Comparison 5 Locking plate versus locking intramedullary nail, Outcome 8 Operation times and blood loss.

Comparison 5 Locking plate versus locking intramedullary nail, Outcome 9 Intra‐operative complication.
![Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 1 Complications and [slight] malunion.](/es/cdsr/doi/10.1002/14651858.CD000434.pub3/media/CDSR/CD000434/rel0003/CD000434/image_n/nCD000434-CMP-006-01.png)
Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 1 Complications and [slight] malunion.
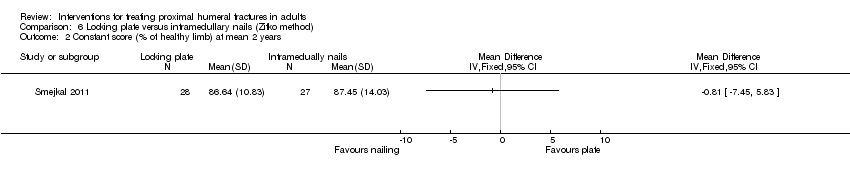
Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 2 Constant score (% of healthy limb) at mean 2 years.

Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 3 Time to union and time to recover upper limb function (weeks).

Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 4 Operation and fluoroscopic times.

Comparison 6 Locking plate versus intramedullary nails (Zifko method), Outcome 5 Length of hospital stay (days).

Comparison 7 Hemi‐arthroplasty versus tension band wiring (4 part fractures), Outcome 1 Re‐operation at 1 year.

Comparison 7 Hemi‐arthroplasty versus tension band wiring (4 part fractures), Outcome 2 Implant removal at 1 year.

Comparison 7 Hemi‐arthroplasty versus tension band wiring (4 part fractures), Outcome 3 Pain at 1 year.
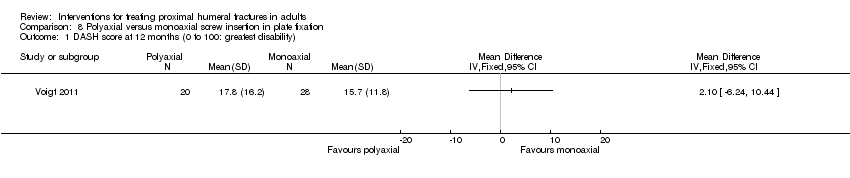
Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 1 DASH score at 12 months (0 to 100: greatest disability).
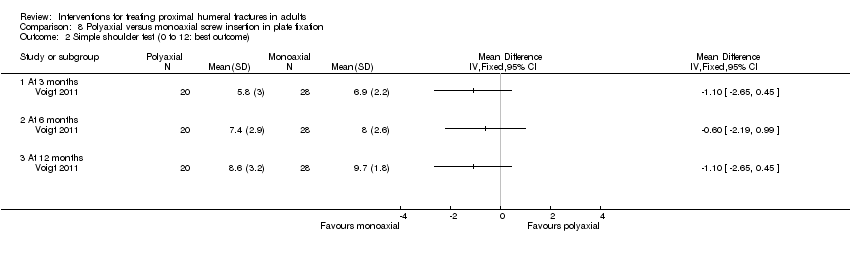
Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 2 Simple shoulder test (0 to 12: best outcome).

Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 3 Re‐operation.

Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 4 Dead at 1 year.
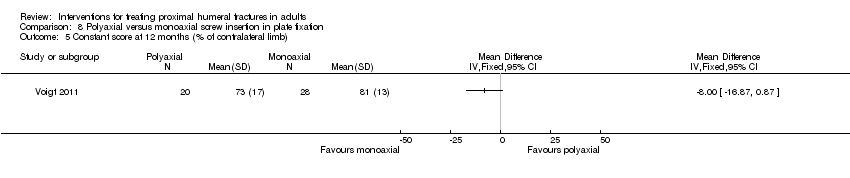
Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 5 Constant score at 12 months (% of contralateral limb).
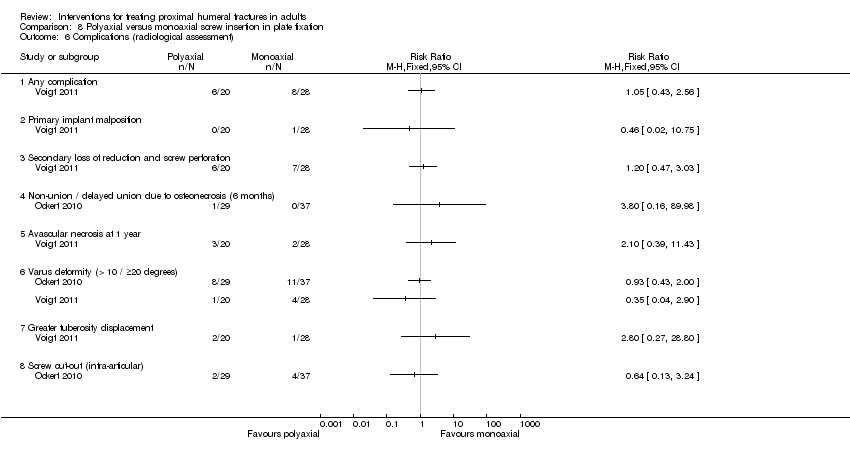
Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 6 Complications (radiological assessment).

Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 7 Range of motion (degrees) at 12 months.
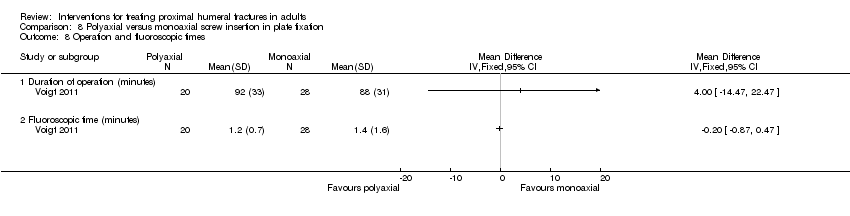
Comparison 8 Polyaxial versus monoaxial screw insertion in plate fixation, Outcome 8 Operation and fluoroscopic times.

Comparison 9 Medial support screws versus control for locking plate fixation, Outcome 1 Adverse events.

Comparison 9 Medial support screws versus control for locking plate fixation, Outcome 2 Constant score (0 to 100: best) at 2.5 years.
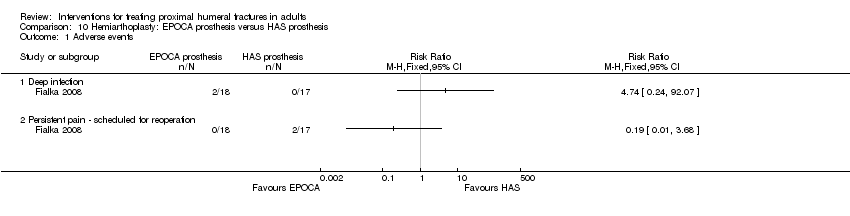
Comparison 10 Hemiarthoplasty: EPOCA prosthesis versus HAS prosthesis, Outcome 1 Adverse events.
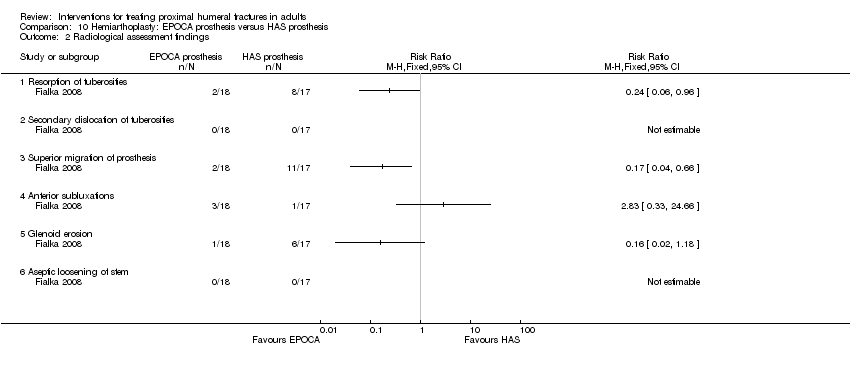
Comparison 10 Hemiarthoplasty: EPOCA prosthesis versus HAS prosthesis, Outcome 2 Radiological assessment findings.
| Study | Measure | EPOCA prosthesis n = 18 | HAS prosthesis n = 17 | Reported significance |
| Fialka 2008 | Active forward flexion | mean = 109° | mean = 62° | P < 0.001 |
| Fialka 2008 | Active abduction | mean = 101° | mean = 62° | P = 0.001 |
| Fialka 2008 | Active external rotation in 90° abduction | mean = 30° | mean = 17° | P = 0.01 |
| Fialka 2008 | Active external rotation in 90° abduction | mean = 45° | mean = 13° | P = 0.001 |
Comparison 10 Hemiarthoplasty: EPOCA prosthesis versus HAS prosthesis, Outcome 3 Range of motion results at one year (degrees).

Comparison 11 Post‐operative (percutaneous fixation) immobilisation for 1 week versus 3 weeks, Outcome 1 Neer score ≤ 80 points (unsatisfactory or failure) at 6 months.

Comparison 11 Post‐operative (percutaneous fixation) immobilisation for 1 week versus 3 weeks, Outcome 2 Premature removal of Kirschner wires.
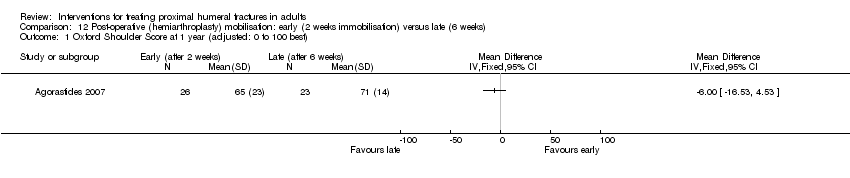
Comparison 12 Post‐operative (hemiarthroplasty) mobilisation: early (2 weeks immobilisation) versus late (6 weeks), Outcome 1 Oxford Shoulder Score at 1 year (adjusted: 0 to 100 best).

Comparison 12 Post‐operative (hemiarthroplasty) mobilisation: early (2 weeks immobilisation) versus late (6 weeks), Outcome 2 Constant shoulder score (at 1 year).

Comparison 12 Post‐operative (hemiarthroplasty) mobilisation: early (2 weeks immobilisation) versus late (6 weeks), Outcome 3 Radiological assessment findings.

Comparison 12 Post‐operative (hemiarthroplasty) mobilisation: early (2 weeks immobilisation) versus late (6 weeks), Outcome 4 Range of motion at 1 year.
| Study | Participants | Surgery | Conservative | Follow‐up |
|
| 50 patients with 3‐ or 4‐part fractures (Norway) | Open reduction and fixation with an interlocking plate device and metal cerclages | Immobilisation of the injured arm in a modified Velpeau bandage. Closed reduction in 8 patients. | 1 year so far (2 years in all) |
|
| 30 patients with 31 with 2‐, 3‐ or 4‐part fractures | Percutaneous reduction and external fixation
| Closed manipulation and sling immobilisation | 2 years |
| 60 patients with 3‐part fractures (all had displaced surgical neck fracture) | Open reduction and fixation with a PHILOS plate and non‐absorbable sutures | Sling immobilisation | 2 years | |
| 55 participants with 4‐part fractures | Humeral head replacement with the Global Fx prosthesis | Sling immobilisation | 2 years | |
| 32 participants with 4‐part fracture | Hemi‐arthroplasty | Closed manipulation and sling | 6 months | |
| 40 patients with 3‐ or 4‐part fractures (3 others excluded) | Internal fixation using surgical tension band or cerclage wiring | Sling immobilisation | 50 months |
| Clearly defined study population? | Interventions sufficiently described? | Main outcomes sufficiently | Appropriate timing of outcome measurement? | |
| Partial: exclusions not specified upfront | Yes | Yes | Yes: 1 year | |
| Partial: no exclusion criteria given (e.g. ability to understand instructions for exercises) | Yes | Yes | Yes: 1 year | |
| Yes | Yes | Yes | Yes: 1 year | |
| Yes | Yes | Yes | Yes: 2 years | |
| Yes: but some question over fracture type in that the Holbein 1999 report included 3‐part fractures too | Yes | Yes | Yes: 1 year | |
| Yes | Yes | Yes | Yes: 2 years | |
| Partial: no exclusion criteria given | Partial: incomplete description of timing of sling use and care of external fixator pin sites | Partial: no description of measurement procedures | Yes: 1 year | |
| Partial: no exclusion criteria given | Partial: although sling and body bandage are common expressions, some variation possible | Partial: no description of measurement procedures | Yes: 2 years | |
| Yes | Yes | Yes | Partial: 6 months | |
| Yes: although this included 4 patients under 20 years with epiphyseal fractures | Yes | Yes | Partial: 6 months | |
| Partial: no exclusion criteria given (e.g. ability to understand instructions for exercises) | Yes | Yes | Yes: 1 year or above (mean: 16 months) | |
| Partial: exclusion criteria described in context of post‐randomisation exclusions. | Yes | Yes | Partial: 6 months | |
| Yes | Yes | Yes | Yes: 2 years | |
| Yes | Yes | Yes | Yes: 2 years | |
| Yes | Partial: frequency of swimming sessions not stated | Yes | Yes: 1 year | |
| Yes: but to note that other fractures including rib (3 participants) were included | Yes | Partial: functional outcome assessment not described (sufficiently) | No: only until fracture consolidation | |
| Yes | Partial: Only minimal intra‐operative details given and nothing regarding post‐operative management including rehabilitation | Partial: this may have been ‘lost in translation’ (Czech article) | Yes: mean 2 years but range not stated (probably most / all > 1 year as recruitment had finished January 2010). | |
| Yes | Yes | Partial: no description of measurement procedures, incomplete description of pain categories | Partial: up to 6 months, then between 18 months to 12 years. This is too spread out. Most results applied to the 6 month follow‐up. | |
| Yes | Yes | Yes | Yes: 1 year | |
| Yes | Yes | Partial: no description of measurement procedures | Partial: between 9 and 36 months; < 1 year in 10 participants. Main results applied to 6 months. | |
| Yes | Yes | Partial: Insufficient information on measurement of complications and timing of their measurement. | Yes: All over 25 months (mean 30.8 months) | |
| Yes | Yes | Yes | Yes: 1 and 3 years | |
| Yes | Yes | Yes | Yes: 1 year, and 3 to 5 years |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Shoulder disability: Croft Shoulder Disability Score Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Disability (1 or more problems) at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Severe disability (5 or more problems) at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Disability (1 or more problems) at 2 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Severe disability (5 or more problems) at 2 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Croft shoulder disability score: individual problems at 2 years Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Pain on movement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Bathing difficulties | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Change position at night more often | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Disturbed sleep | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 No active pastimes or usual physical recreation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Lifting problems | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.7 Help needed | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.8 More accidents (e.g. dropping things) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of treatment sessions (until independent function achieved) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 SF‐36 scores: pain & physical dimensions Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Physical functioning (0‐100: excellent) at 16 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Physical functioning (0‐100: excellent) at 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Role limitation physical (0‐100: none) at 16 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Role limitation physical (0‐100: none) at 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Pain (0‐100: none) at 16 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.6 Pain (0‐100: none) at 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Adverse events Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 Frozen shoulder | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Fracture displacement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.4 Reflex sympathetic dystrophy | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.5 Treated (injection) subacromial impingement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Constant shoulder score (ratio of affected/unaffected arm) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 8 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 16 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Constant shoulder score (0 to 100: best) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.4 6 months: subjective assessment (0 to 35: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.5 6 months: objective assessment range of motion and strength (0 to 65: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Changes in pain intensity (mm) from baseline: 100 mm visual analogue scale (positive change = less pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 At 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 At 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Range of motion at 6 months (degrees): difference between two shoulders Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Abduction | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Anterior elevation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Lateral rotation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Patient dissatisfied with treatment Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Problems with bandages Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Application of bandage was uncomfortable | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Premature bandage removal | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Fracture displacement by 3 weeks Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Poor or bad rating by patient at fracture consolidation Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain at one year (scale 0 to 8: maximum pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Severe or moderate pain at 3 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Requested change of therapy Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Adverse events (frozen shoulder: 1 v 2; unexplained prolonged pain: 0 v 1) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Neer's rating (0 to 100: best) at mean 16 months (exploratory analysis) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Active gleno‐humeral elevation (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Functional scores at 12 months (higher = worse) Show forest plot | 3 | 153 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.42, 0.22] |
| 1.1 DASH (0 to 100: worst disability) (reversed) | 2 | 105 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.57, 0.19] |
| 1.2 ASES (0 to 24: best) | 1 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.46, 0.67] |
| 2 DASH (0 to 100: worst disability) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 at 4 months | 2 | 106 | Mean Difference (IV, Fixed, 95% CI) | 0.91 [‐7.00, 8.83] |
| 2.2 at 12 months | 2 | 105 | Mean Difference (IV, Fixed, 95% CI) | ‐4.51 [‐13.50, 4.48] |
| 2.3 at 24 months | 2 | 99 | Mean Difference (IV, Fixed, 95% CI) | ‐7.43 [‐16.26, 1.41] |
| 3 American Shoulder and Elbow Surgeons score (0 to 24: best) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Activities of daily living Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Unable to manage personal hygiene at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Unable to comb hair at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Unable to sleep on fractured side at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Unable to carry 5 kg at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Unable to manage personal hygiene at 50 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.6 Unable to comb hair at 50 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.7 Unable to sleep on fractured side at 50 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.8 Unable to carry 5 kg at 50 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Quality of life assessment: EuroQol (0: dead to 1: best health) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 at 3 to 4 months | 3 | 156 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.02, 0.05] |
| 5.2 at 6 months | 3 | 156 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.01, 0.08] |
| 5.3 at 12 months | 3 | 153 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.01, 0.08] |
| 5.4 at 24 months | 2 | 101 | Mean Difference (IV, Fixed, 95% CI) | 0.15 [0.05, 0.25] |
| 6 Quality of life assessment (Fjalestad 2010 data) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 15D at 3 months (0: death; 1: perfect health) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 15D at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 15D at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 number of QALYs at 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.5 numbers of QALYs at 1 year (‐ deaths) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Mortality Show forest plot | 4 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.55, 4.36] |
| 8 Additional surgery (re‐operation or secondary surgery) Show forest plot | 5 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.36 [1.33, 8.49] |
| 8.1 at 6 to 12 months | 3 | 113 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.90 [0.54, 6.73] |
| 8.2 at 2 years | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.83 [1.38, 24.70] |
| 9 Adverse events / complications Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Infection | 6 | 259 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.13 [0.91, 18.87] |
| 9.2 Nerve injury / palsy | 3 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.20, 2.76] |
| 9.3 Non union | 5 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.16, 1.40] |
| 9.4 Avascular necrosis | 5 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.37, 1.16] |
| 9.5 Post‐traumatic osteoarthritis (signs of) | 3 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.21, 1.51] |
| 9.6 Screw penetration into joint | 3 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.49 [2.25, 58.76] |
| 9.7 Impingement | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.19, 20.86] |
| 9.8 Redisplacement resulting in an operation | 2 | 81 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.03, 2.22] |
| 9.9 Secondary dislocation or resorption of the greater tuberosity | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 15.18 [0.92, 249.78] |
| 9.10 Tuberosity displacement at 50 months | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.71] |
| 9.11 Wire penetration at 1 year | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 69.31] |
| 9.12 Fixation failure resulting in an operation | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 70.30] |
| 9.13 Refracture | 1 | 22 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 14.05] |
| 10 Constant scores (overall: 0 to 100: best score) Show forest plot | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 at 4 months | 2 | 107 | Mean Difference (IV, Fixed, 95% CI) | ‐1.33 [‐6.80, 4.14] |
| 10.2 at 12 months | 3 | 152 | Mean Difference (IV, Fixed, 95% CI) | 2.36 [‐3.52, 8.24] |
| 10.3 at 24 months | 2 | 101 | Mean Difference (IV, Fixed, 95% CI) | 0.48 [‐7.26, 8.22] |
| 10.4 at 50 months | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐5.0 [‐17.52, 7.52] |
| 11 Constant scores (difference between injured and uninjured shoulder): Normal = 0. Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 at 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Poor or unsatisfactory function at 1 year (Neer rating) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 13 Dependent in activities of daily living (or dead) at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 14 Pain at 2 years: VAS (0 to 100: worst pain) Show forest plot | 2 | 101 | Mean Difference (IV, Fixed, 95% CI) | ‐6.38 [‐14.18, 1.41] |
| 15 Constant score at 50 months: overall and components Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Overall score (0‐100: best score) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 Pain (maximum score 15) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.3 Range of motion (maximum score 40) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.4 Power (maximum score 25) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.5 Activities of daily living (maximum score 20) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Constant (often severe) pain at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 17 Failure to recover 75% muscle power relative to other arm (survivors) at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 17.1 Flexion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 Abduction | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.3 Lateral rotation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Range of movement impairments in survivors at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18.1 Flexion < 45 degrees | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Unable to place thumb on mid spine (T12) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.3 Lateral rotation < 5 degrees | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Costs at 1 year (Euros in 2005) Show forest plot | Other data | No numeric data | ||
| 20 Total costs including indirect costs (Euros) at 1 year Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 American Shoulder and Elbow Surgeons (ASES) score (0 to 100: best) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 At 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 At 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Death, re‐operation and adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Death | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Any complication | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Screw penetration into humeral head (all had re‐operation) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Heterotopic ossification | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Osteonecrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.7 Degenerative change of glenohumeral joint | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.8 Secondary varus collapse | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.9 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Pain (VAS: 0 to 10: worst) Show forest plot | Other data | No numeric data | ||
| 4 Constant score (0 to 100: best) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 At 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 At 3 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Active range of motion (at 3 years) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Forward elevation (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 External rotation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Range of movement: internal rotation (level on spine) Show forest plot | Other data | No numeric data | ||
| 7 Strength of suprapinatus (relative to opposite side) % ‐ at 3 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 At 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 At 3 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Operation times and blood loss Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Duration of surgery (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Blood loss (ml) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Intra‐operative complication Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 Pneumothorax | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Blood transfusion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Complications and [slight] malunion Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Any complication | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Malunion (usually slight) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Constant score (% of healthy limb) at mean 2 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Time to union and time to recover upper limb function (weeks) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Time to radiographic union | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Time to recover normal upper limb function | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Operation and fluoroscopic times Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Duration of operation (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 X‐ray exposure (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Re‐operation at 1 year Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Implant removal at 1 year Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Pain at 1 year Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 DASH score at 12 months (0 to 100: greatest disability) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Simple shoulder test (0 to 12: best outcome) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 At 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 At 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 At 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Re‐operation Show forest plot | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.56, 3.67] |
| 3.1 By 6 months | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.15, 4.76] |
| 3.2 By 1 year | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.86 [0.59, 5.88] |
| 4 Dead at 1 year Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Constant score at 12 months (% of contralateral limb) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Complications (radiological assessment) Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 Any complication | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Primary implant malposition | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 Secondary loss of reduction and screw perforation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.4 Non‐union / delayed union due to osteonecrosis (6 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.5 Avascular necrosis at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.6 Varus deformity (> 10 / ≥20 degrees) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.7 Greater tuberosity displacement | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.8 Screw cut‐out (intra‐articular) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Range of motion (degrees) at 12 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 Flexion | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Abduction | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 External rotation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.4 Internal rotation | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Operation and fluoroscopic times Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Duration of operation (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Fluoroscopic time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Early loss of fixation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Re‐operation for early failure | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Osteonecrosis (asymptomatic) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Constant score (0 to 100: best) at 2.5 years Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Deep infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Persistent pain ‐ scheduled for reoperation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Radiological assessment findings Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Resorption of tuberosities | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Secondary dislocation of tuberosities | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Superior migration of prosthesis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Anterior subluxations | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Glenoid erosion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 Aseptic loosening of stem | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Range of motion results at one year (degrees) Show forest plot | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Neer score ≤ 80 points (unsatisfactory or failure) at 6 months Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Premature removal of Kirschner wires Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oxford Shoulder Score at 1 year (adjusted: 0 to 100 best) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Constant shoulder score (at 1 year) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Overall score (0 to 100: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Pain component (0 to 15: best)) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Activities of daily living component (0 to 25: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Mobility component (0 to 40: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 Strength component (0 to 25: best) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Radiological assessment findings Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Nonunion (with bone resorption) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Malunion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Greater tuberosity migration (all had severe pain at 6 & 12 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.4 Superior luxation of prosthesis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Range of motion at 1 year Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Elevation (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 External rotation (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

