Angioplastia con parche versus cierre primario para la endarterectomía carotídea
Resumen
Antecedentes
La angioplastia de carótida con parche (con parche venoso o con parche sintético) podría reducir el riesgo de reestenosis de la arteria carótida y accidente cerebrovascular isquémico posterior. Ésta es una actualización de una revisión Cochrane publicada originalmente en 1995 y actualizada anteriormente en 2004.
Objetivos
Evaluar la seguridad y la eficacia de la angioplastia de carótida con parche sistemática o selectiva en comparación con la endarterectomía carotídea con cierre primario.
Métodos de búsqueda
Se hicieron búsquedas en el Registro de ensayos del Grupo Cochrane de Accidentes Cerebrales Vasculares (Cochrane Stroke Group) (última búsqueda 5 de mayo de 2009), Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL) (The Cochrane Library, número 1, 2009), MEDLINE (1966 hasta noviembre de 2008), EMBASE (1980 hasta noviembre de 2008) y en Index to Scientific and Technical Proceedings (1980 hasta noviembre de 2008). Se realizaron búsquedas manuales en revistas y actas de congresos, se verificaron las listas de referencias y se estableció contacto con expertos en el campo.
Criterios de selección
Ensayos aleatorizados y cuasialeatorizados que compararon la angioplastia de carótida con parche con el cierre primario en cualquier paciente sometido a endarterectomía carotídea.
Obtención y análisis de los datos
Dos autores de la revisión de forma independiente evaluaron la elegibilidad y la calidad de los ensayos y extrajeron los datos.
Resultados principales
Se incluyeron diez ensayos con un total de 1967 pacientes sometidos a 2157 operaciones. La calidad de los ensayos fue generalmente deficiente. El seguimiento varió desde el alta hospitalaria hasta los cinco años. La angioplastia de carótida con parche se asoció con una reducción del riesgo de accidente cerebrovascular ipsilateral durante el período perioperatorio (odds ratio [OR] 0,31; intervalo de confianza [IC] del 95%: 0,15 a 0,63; p = 0,001) y el seguimiento a largo plazo (OR 0,32; IC del 95%: 0,16 a 0,63; p = 0,001). También se asoció con un menor riesgo de obstrucción arterial perioperatoria (OR 0,18; IC del 95%: 0,08 a 0,41; p = 0,0001), y a una disminución de la reestenosis durante el seguimiento a largo plazo en ocho ensayos (OR 0,24; IC del 95%: 0,17 a 0,34; p < 0,00001). Estos resultados son más seguros que los de la revisión anterior, ya que el número de operaciones y eventos es mayor. Sin embargo, los tamaños de la muestra son todavía relativamente pequeños, no estuvieron disponibles los datos de todos los ensayos y hubo pérdidas significativas durante el seguimiento. Se registraron muy pocas complicaciones arteriales, como hemorragia, infección, parálisis de pares craneales y formación de pseudoaneurisma, tanto con el parche como con el cierre primario. No se encontró una correlación significativa entre el uso de la angioplastia con parche y el riesgo de tasas de mortalidad por todas las causas perioperatorias o a largo plazo.
Conclusiones de los autores
La evidencia limitada indica que la angioplastia de carótida con parche podría reducir el riesgo de obstrucción arterial perioperatoria y de reestenosis. Aparentemente, reduce el riesgo de accidente cerebrovascular ipsilateral y existe una tendencia no significativa hacia una reducción en la tasa de cualquier accidente cerebrovascular perioperatorio y de mortalidad por todas las causas.
PICOs
Resumen en términos sencillos
Angioplastia con parche versus cierre primario para la endarterectomía carotídea
La evidencia de esta revisión de diez ensayos, con 1967 pacientes sometidos a 2157 operaciones, ahora indica un efecto beneficioso a partir del uso habitual de la angioplastia con parche durante la endarterectomía carotídea. Cerca del 20% de los accidentes cerebrovasculares se producen por un estrechamiento de la arteria carótida (la principal arteria que suministra sangre al cerebro). La endarterectomía carotídea es una operación que implica abrir la arteria carótida para eliminar este estrechamiento y así, reducir el riesgo de accidente cerebrovascular. Sin embargo, existe un riesgo del 2% al 10% de que la operación en sí misma provoque un accidente cerebrovascular. Algunos cirujanos recomiendan la introducción de un parche de material sintético o realizado con la propia vena del paciente en el cierre arterial. Este procedimiento puede ayudar a reducir el riesgo de estrechamiento de la arteria durante la sutura y puede, por consiguiente, reducir el riesgo de bloqueo recurrente y el consecuente accidente cerebrovascular o muerte, o ambos. Sin embargo, el uso de un parche puede aumentar la dificultad quirúrgica y la duración de la operación. Además, los parches de venas con paredes finas pueden romperse con consecuencias potencialmente mortales y los materiales sintéticos son vulnerables a la infección.
Authors' conclusions
Background
Carotid endarterectomy has been shown in large, well‐conducted randomised controlled trials to reduce the risk of stroke in patients with recently symptomatic, severe (greater than 70%) internal carotid artery stenosis (Rothwell 2003). There is also some evidence that it is beneficial for asymptomatic patients (ACAS 1995; Halliday 2004). What is less clear at present is whether different surgical techniques affect the outcome. One such technique is carotid patch angioplasty, with either a venous patch or a synthetic patch. Might this be as safe as primary closure, reduce the risk of restenosis and, more importantly, improve the long‐term clinical outcome?
There are relatively few good prospective studies of restenosis following carotid endarterectomy and studies are difficult to compare because of differences in the definitions of stenosis and lengths of follow up. However, it appears that carotid restenosis of greater than 50% diameter reduction (as detected by Doppler ultrasound) occurs in 6% to 36% of patients during long‐term follow up (Bernstein 1990; Knudsen 1990; Ouriel 1987; Volteas 1994; Zierler 1982). The majority of stenoses occur in the first two years (Frericks 1998). Carotid patch angioplasty may reduce the risk of restenosis, and so reduce the long‐term risk of recurrent ipsilateral ischaemic stroke (Awad 1989; Ouriel 1987). However, the risk of symptomatic restenosis appears to be much lower ‐ about 2% to 4% (Das 1985; Frericks 1998), and patch angioplasty may also be associated with certain perioperative risks: routine patching involves a longer carotid occlusion time, two suture lines instead of one and the use of a patch material, all of which may increase the risk of early re‐occlusion, arterial rupture, infection or pseudoaneurysm formation (Awad 1989; Bernstein 1992). In addition, if a venous patch is used, there may be morbidity associated with vein harvesting, such as neuralgia, haemorrhage, and infection.
A survey from the United Kingdom in a trial showed considerable variations among vascular surgeons in the use of carotid patching, which may reflect uncertainty in its benefits: 76% of surgeons always used patching, 19.4% sometimes and 4.6% never (Girn 2008). Analysis of the ECST trial data showed significant heterogeneity in frequency of use of patch angioplasty at an individual surgeon, national and international level (ECST 1991). Given the uncertainty implied by such variation in practice, it is clearly important to establish whether routine or selective patching is more effective than, and as safe as, primary closure. Randomised controlled trials provide the most reliable evidence on which to base these assessments. We, therefore, performed a systematic review of all such trials that compared routine or selective patching with primary closure.
NB: The first version of this review included trials comparing one type of patch with another. These trials have now been included in a separate Cochrane review (Bond 2003).
This is an update of a Cochrane Review originally published in 1995 and previously updated in 2004.
Objectives
To assess the safety and efficacy of routine or selective carotid patch angioplasty with either a venous patch or a synthetic patch compared to primary closure. We wished to test the primary hypothesis that carotid patch angioplasty resulted in a lower rate of significant arterial restenosis and therefore fewer recurrent strokes and stroke‐related deaths without a significant increase in perioperative complications.
Methods
Criteria for considering studies for this review
Types of studies
We sought to identify all unconfounded randomised trials of carotid patching. We included quasi‐randomised trials in which allocation to different treatment regimens was not adequately concealed (e.g. allocation by alternation, date of birth, hospital number, day of the week, or by using an open random number list), but foreknowledge of treatment allocation might lead to biased treatment allocation and exaggerated treatment effects (Schulz 1995).
Types of participants
We considered trials that included any type of patient undergoing carotid endarterectomy as eligible, whether the initial indication for endarterectomy was symptomatic or asymptomatic carotid disease.
Types of interventions
We sought to identify all trials comparing routine carotid patch angioplasty (i.e. patching attempted in all patients) with primary closure. Any type of patch material was eligible e.g. venous, Dacron, or polytetrafluoroethylene (PTFE). We also intended to include trials comparing selective patch angioplasty (i.e. patching attempted only in patients thought likely to benefit) with primary closure, but we failed to identify any such trials. Trials which compared one type of patch with another are included in a separate Cochrane review (Bond 2003).
Types of outcome measures
We aimed to extract from each trial the number of patients originally allocated to each treatment group to allow an intention‐to‐treat analysis. Within each treatment group we then extracted the number of patients:
-
who died within 30 days of the operation and during subsequent follow up. We tried to classify each death as stroke‐related or not;
-
who had any stroke within 30 days of the operation and during subsequent follow up. A separate analysis of strokes ipsilateral to the endarterectomy was also performed;
-
who had known occlusion of the artery that was operated on within 30 days of the operation;
-
who had a significant complication related to surgery, such as haemorrhage from or rupture of the artery, infection of the endarterectomy site, cranial nerve palsy or pseudoaneurysm formation;
-
who developed restenosis greater than 50% or occlusion of the artery that was operated on during follow up.
Search methods for identification of studies
See the 'Specialized register' section in the Cochrane Stroke Group module.
We searched the Cochrane Stroke Group trials register, which was last searched by the Managing Editor in May 2009. We also updated the electronic searches and handsearched additional issues of relevant journals as follows.
-
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, Issue 1, 2009); MEDLINE (1966 to November 2008) (Appendix 1), EMBASE (1980 to November 2008) (Appendix 2), and Index to Scientific and Technical Proceedings (1980 to November 2008), which was searched using the terms "carotid" and ("trial* or random*").
-
We handsearched the following journals, including conference supplements:
-
Annals of Surgery (1981 to September 2008);
-
Annals of Vascular Surgery (1994 to September 2008);
-
Cardiovascular Surgery (now Vascular) (1994 to September 2008);
-
European Journal of Vascular Surgery (now European Journal of Vascular and Endovascular Surgery) (1987 to September 2008);
-
Journal of Vascular Surgery (1994 to September 2008);
-
Stroke (1994 to September 2008).
-
-
We reviewed the reference lists of all relevant studies.
-
We contacted experts in the field to identify further published and unpublished studies
-
For the previous version of the review:
-
we hand‐searched the following journals, including conference supplements:
-
American Journal of Surgery (1994 to 2001);
-
British Journal of Surgery (1985 to 2001);
-
World Journal of Surgery (1978 to 2001).
-
-
we handsearched abstracts of the following meetings for the years 1995 to 2001:
-
AGM of the Vascular Surgical Society (UK);
-
AGM of the Association of Surgeons of Great Britain and Ireland;
-
AHA Stroke Conference;
-
Annual Meeting of the Society for Vascular Surgery (USA);
-
European Stroke Conference.
-
-
We did not apply any language restriction in the searches and arranged translation of all possibly relevant non‐English language publications.
Data collection and analysis
One review author (KR) selected those trials that met the inclusion criteria, and the other review author (PMR) independently reviewed these decisions. We resolved all disagreements through discussion.The same two review authors also assessed the methodological quality of each trial. We decided not to use a scoring system to assess quality but simply to record the following details: the randomisation method, the blinding of the clinical and Doppler assessments, whether outcomes were reported for all patients originally randomised in each group irrespective of whether they received the operation they were allocated to or whether the patient was excluded after randomisation, and the number of patients lost to follow up. We sought data on the number of outcome events in all patients originally randomised to allow an intention‐to‐treat analysis. We extracted and cross‐checked all data. In addition, we also extracted details about the patients included in the trial, the inclusion and exclusion criteria, the comparability of the treatment and control groups for important prognostic factors, the type of patch, the type of anaesthetic, the use of shunts, and the use of antiplatelet therapy during follow up. If any of the above data were not available from the publication, we sought further information by correspondence with the trialists.
All of the trials included both patients who had unilateral carotid endaterectomies and patients who had bilateral carotid endarterectomies, and in most the artery was randomised to a particular procedure rather than the patient (Al‐Rawi 2006; Lord 1989; Mannheim 2005; Myers 1994; Pratesi 1986; Ranaboldo 1993; Vleeschauwer 1987). In these trials, it was therefore possible for one patient to have primary closure on one side and carotid patching on the other side. Indeed, in one trial if a patient required bilateral endarterectomies, each artery had to have a different procedure (Myers 1994). In the reporting of these trials, the results were given for each artery that was randomised rather than for each individual patient. This makes sense for arterial complications such as haemorrhage or occlusion, for ipsilateral events, and for complication within 30 days of surgery (since most patients waited at least this period between the first and second operation), but it is not ideal for patient‐related long‐term clinical outcome events such as death or any stroke. In patients with bilateral endarterectomies who had both patching and primary closure, it would not be possible to relate death or stroke to one particular procedure. Therefore, In trials where it was possible for a patient to have both procedures, we analysed death and any stroke only in those who had unilateral procedures or the same procedure to both arteries. These data were available from the authors in all except two trials (Lord 1989; Myers 1994). In one trial, the investigators no longer had the original data on patients with unilateral operations and so this trial was excluded from the analyses of these outcomes (Lord 1989). In the other trial (Myers 1994), the number of patients undergoing unilateral endarterectomies was reported and we were able to estimate the number of clinical events per patient in each group using the number of events per artery and the total number of deaths that were reported.
A separate analysis of only strokes ipsilateral to the operated artery was also performed for each artery. However, this may be less useful as the more important outcome is the total number of strokes and not just the ipsilateral strokes. We analysed arterial complications, such as occlusion, haemorrhage from the endarterectomy site, restenosis, infection at the operation site, or pseudoaneurysm formation for all arteries rather than patients. The analyses based on arteries assumed that, in patients who had bilateral endarterectomies, outcome events in each carotid artery were independent. This is unlikely to be true but given that relatively few patients had bilateral procedures (10% overall) we felt it reasonable to perform such analyses. However, their results should be interpreted with caution.
About 40 patients were lost to follow up. For the intention‐to‐treat analyses, we assumed that patients who were lost to follow up did not have an outcome event. For the main analyses, we assumed that patients who were lost did not have an outcome event. In the previous version of this review, where statistically significant results were found, worst‐case sensitivity analyses were performed to determine whether the results were robust. These analyses assumed that all patients lost from the patching arm had an adverse outcome, whereas none of those lost from the control arm did. However, for this review these analyses have not been included since the current authors consider them to be unreasonably critical.
We calculated proportional risk reductions based on a weighted estimate of the odds ratio using the Peto method (APT 1994). Since all the outcome events assessed were rare, the odds ratios quoted will be similar to the relative risks. We calculated absolute risk reductions from the crude risks of each outcome in all trials combined (APT 1994). We assessed heterogeneity between study results using the I2 statistic (Higgins 2003). This examined the percentage of total variation across studies due to heterogeneity rather than to chance. Values of I2 over 75% indicate a high level of heterogeneity.
Results
Description of studies
Seven trials that fulfilled the eligibility criteria were identified by the 2004 version of this review, but only two new randomised controlled trials have been reported since then (Al‐Rawi 2006; Mannheim 2005). We also found one trial published in 1986 that was not identified in the previous verison of the review and it is included in this version (Pratesi 1986). We have not identified any additional ongoing trials, and there are no trials presently awaiting assessment. We excluded two trials: in one unpublished trial, an intention‐to‐treat analysis was not possible because one‐third of the 300 patients randomised did not receive their allocated operation and results for these patients were not available (Gale 1985); in the discussion section of one of the published papers (Eikelboom 1988), another unpublished trial was quoted but after discussion with the principal investigator, it became apparent that this trial was not in fact random or quasi‐random (Hertzer 1987).
All of the trials we included compared routine patching with primary closure. Three of the trials used only saphenous vein patches (Eikelboom 1988; Myers 1994; Vleeschauwer 1987), and three used synthetic patches (Al‐Rawi 2006; Katz 1994; Mannheim 2005). Four trials used both vein and synthetic ‐ PTFE or Dacron ‐ patches (AbuRahma 1996; Lord 1989; Pratesi 1986; Ranaboldo 1993), but in two of these (Pratesi 1986; Ranaboldo 1993), results were not recorded by the type of patch that the patient received. In the previous review, the results of one of these trials (Lord 1989) were presented by splitting them into vein patching versus control and synthetic patching versus control. However, on hindsight, this was incorrect since it allowed the number of operations with primary closure to be counted twice in the overall analysis. Therefore, for the updated review we have analysed these three trials as any patch versus no patch.
One of the trials included a group that was allocated to obligate patching without randomisation (Myers 1994). This group of patients was not included in the analyses. All operations were performed under general anaesthetic, and most were also performed with shunting. Most of the patients in all the trials received antiplatelet or anticoagulant drugs long term after the operation. All the trials with follow up beyond hospital discharge included Doppler ultrasound of the arteries during follow up, and one also included intravenous digital subtraction angiography (Eikelboom 1988).
The average age of patients involved in these trials was about 67 years and there were approximately twice as many men as women. All of the trials included patients with asymptomatic carotid disease with the proportion varying from 8% (Ranaboldo 1993) to 51% (Mannheim 2005). All trials compared routine patching in all patients in the treatment group with primary closure. In four trials, narrow carotid arteries were excluded before randomisation on the basis that it was not safe to close these with primary closure: in one trial, 38 out of a total of 163 arteries were excluded because the internal diameter (assessed at operation) was less than 5 mm (Myers 1994); in one trial, one patient out of a possible 110 patients was excluded because the arterial diameter was less than 3.5 mm (assessed from the preoperative angiogram) (Katz 1994); in one trial, 12 out of 399 carotid endarterectomies were excluded if internal carotid artery diameter was less than 4 mm (AbuRahma 1996); and in one trial, 24 out of 422 were excluded if small diameter internal carotid artery or the need for an interposition graft. In the remaining trials, only one patient randomised to primary closure required a patch because the artery was felt to be too narrow (Eikelboom 1988). Seven other patients randomised to primary closure required patching either because the stenosis was very high (two patients) or because the artery became occluded postoperatively (five patients). Seven patients from the patch group did not receive a patch either because no vein was available (two patients), because rapid closure was required due to possible ischaemic changes on an EEG during the operation (one patient), or for no apparent reason (four patients). The average follow up varied from hospital discharge (Lord 1989) to five years (Eikelboom 1988; Myers 1994). In all trials in which the data were available, the treatment groups were comparable for important prognostic factors.
Risk of bias in included studies
There were several significant flaws in most of the trials. Firstly, allocation concealment was only adequate in six trials which used numbered, sealed, opaque, envelopes as the method of randomisation (AbuRahma 1996; Al‐Rawi 2006; Lord 1989; Mannheim 2005; Myers 1994; Ranaboldo 1993). One study used envelope randomisation but they were not numbered or opaque (Vleeschauwer 1987). Two trials used quasi‐random allocation based on the patient's hospital number (Eikelboom 1988) or social security number (Katz 1994). Secondly, adequate blinding is important in order to reduce bias in the detection of certain outcome events. For instance, ultrasound assessment of restenosis should probably be assessed blind, although experienced practitioners may be able to detect the slight dilatation associated with a carotid patch even when blinded. Correspondence with the authors confirmed that clinical assessment was definitely blinded in only three trials (AbuRahma 1996; Ranaboldo 1993; Vleeschauwer 1987), but that restenosis was assessed blind in all except two trials (Katz 1994; Lord 1989).
As mentioned previously, one of the main flaws in eight of the trials was that a patient undergoing bilateral carotid endarterectomy could be randomised twice and have their two carotid arteries randomised to different treatment groups (AbuRahma 1996; Al‐Rawi 2006; Lord 1989; Mannheim 2005; Myers 1994; Pratesi 1986; Ranaboldo 1993; Vleeschauwer 1987). In these trials, it was unclear from the published reports exactly how many patients (as opposed to arteries) were randomised to each group and how many patients with bilateral endarterectomies had different procedures to each artery (Table 1). We were able to obtain these data from all except one trial (Lord 1989). Demographic features, such as age and sex, as well as results were usually reported for each randomised artery rather than per patient. True intention‐to‐treat analysis was only possible for three trials after we obtained additional data from the authors (AbuRahma 1996; Al‐Rawi 2006; Ranaboldo 1993). In the other trials, data on patients lost to follow up were not available, and in one trial four patients who did not have the procedure that they were randomised to receive were excluded from the analysis (Lord 1989).
| Study | Total patients | Total operations | Patch lost at 30 days | Patch lost at end | Primary lost at 30 days | Primary lost at end | Number of exclusions | Crossover patch ‐ non | Crossover non ‐ patch |
| 357 | 399 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | |
| 315 | 338 | 0 | 7 | 0 | 8 | 10 | Data not available | Data not available | |
| 126 | 129 | 0 | 10 patients lost to doppler FU but not clinical FU | 0 | 7 to doppler FU but not clinical FU | 0 | 3 | 3 | |
| 87 | 100 | 0 | 5 | 0 | 7 | 0 | 0 | 0 | |
| 123 | 140 | 0 | 0 | 0 | 0 | 4 | Between 0 and 4 | Between 0 and 4 | |
| 404 | 422 | 0 | Data not available | 0 | Data not available | Data not available | 0 | 0 | |
| 136 (109 after exclusion of 27 patients undergoing obligatory vein patching) | 152 (122 analysed as 30 operations got obligatory vein patches) | 0 | 6 | 0 | 8 | 30 operations underwent obligatory vein patch closure and 16 patients had both sides done (total 46) | 0 | 0 | |
| 100 | 100 | Data not available | Data not available | Data not available | Data not available | Data not available | Data not available | Data not available | |
| 199 | 213 | 0 | 5 | 0 | 12 | 0 | 0 | 0 at 30‐day FU but 4 at 1‐year FU | |
| 126 | 174 | 0 | Data not available | 0 | Data not available | 0 | 0 | 0 |
FU: follow up
Effects of interventions
We included data from 10 trials (1967 patients, 2157 operations) in this review. The results presented may differ from those in the published reports where additional information has been obtained from the authors. There was no statistical heterogeneity in any of the analyses.
Outcomes within 30 days of operation
Stroke
Any stroke (fatal, non‐fatal, contralateral, ipsilateral, brainstem, haemorrhage, or infarct)
The overall perioperative risk of any stroke was 2.5% (45/1769). Patching was associated with a non‐significant reduction in the odds of any stroke (odds ratio (OR) 0.57, 95% confidence interval (CI) 0.31 to 1.03, P = 0.06) (Analysis 1.1). Within each closure type there was no heterogeneity, but there was significant between‐group heterogeneity (I2 = 60.3). None of the trials recorded the severity of stroke in terms of residual disability, but only three of these strokes were fatal (one in the patch group, two in the primary closure group).
Ipsilateral stroke (haemorrhage or infarct)
If effective, patching would be expected to reduce mainly stroke ipsilateral to the operated artery. The number of ipsilateral strokes per artery randomised was available from seven trials, although in several instances we required additional data from the authors. No data were available from the three new trials. In total, 2.8% (33/1201) of operations were associated with an ipsilateral stroke. Carotid patching was associated with a statistically significant reduction in the relative odds of perioperative ipsilateral stroke (OR 0.31, 95% CI 0.15 to 0.63, P = 0.001) (Analysis 1.3).
Death
There were only 11 deaths in the nine trials with available data (overall risk = 0.6%, 11/1869), and so it remains unclear whether patching is associated with a higher or lower perioperative mortality than primary closure (OR 0.62, 95% CI 0.18 to 2.09, P = 0.4) (Analysis 1.4).
Stroke or death
Combined stroke/death rate was non‐significantly lower in the patching group (OR 0.58, 95% CI 0.33 to 1.01, P = 0.06) (Analysis 1.5).
Arterial complications
As noted in the Methods section, these results should be interpreted with caution since, in patients who underwent bilateral endarterectomies, outcomes in each artery were probably not independent. We were unable to identify how many patients with bilateral endarterectomies had outcomes events in both arteries.
Arterial occlusion
Three trials did not provide data on perioperative arterial occlusion (Mannheim 2005; Pratesi 1986; Vleeschauwer 1987). Of the other trials, four used ultrasound (Duplex) scanning (AbuRahma 1996; Al‐Rawi 2006; Katz 1994; Ranaboldo 1993), two used intravenous digital subtraction angiography (Eikelboom 1988; Lord 1989) and one used ocular pneumoplethysmography (Myers 1994). At least 26 of the randomised arteries were not assessed within 30 days of operation (14 patch, 12 primary closure) and these arteries were assumed to be not occluded for the purpose of this analysis. Patching was associated with a highly statistically significant 82% reduction (OR 0.18 P < 0.0001) in the odds of perioperative arterial occlusion. However, this result was based on small numbers (4/794 (0.5%) patching versus 20/641 (3.1%) primary closure) and so the confidence interval was wide (OR 0.18, 95% CI 0.08 to 0.41 P < 0.0001) (Analysis 1.6). As documented above, however, the consequences to the patients (in terms of stroke‐related death and non‐fatal stroke) resulting from this reduction in arterial occlusion were unclear.
Arterial rupture/haemorrhage
The overall risk of rupture and haemorrhage in all patients combined was low (1.5%). There was no significant difference between patching and primary closure but the confidence interval was wide (OR 1.24, 95% CI 0.61 to 2.54) (Analysis 1.7). None of the arterial haemorrhages was associated with a fatal or major stroke.
Local infection
There was only a two reported case of infection at the endarterectomy site (Katz 1994; Mannheim 2005). These occured in two patients in the synthetic patching group and six patients in the primary closure group. There was no significant difference between patching and primary closure but the confidence interval was wide (OR 0.38, 95% CI 0.09 to 1.54) (Analysis 1.8). Within each closure type there was significant heterogeneity (I2 = 61).
Cranial nerve palsy
Only four trials supplied data on this outcome (AbuRahma 1996; Katz 1994; Mannheim 2005; Myers 1994), and in one of these no outcomes occurred. The risk of nerve palsy was low (2.6%) with no significant difference between patching and primary closure (OR 0.78, 95% CI 0.36 to 1.69) (Analysis 1.9).
Complications requiring return to theatre
When the number of complications (occlusion, haemorrhage, infection) that required return to theatre for re‐operation within 30 days of the first operation were considered, there was a significant trend in favour of carotid patching, that is carotid patching was associated with fewer returns to theatre (OR 0.35, 95% CI 0.16 to 0.79) (Analysis 1.10).
Outcomes during long‐term follow up (at least one year) including events during the first 30 days
One trial followed up patients for 30 days only (Lord 1989) and this trial has been excluded from these analyses. In the remaining trials, at least 56 patients (28 patch, 28 primary closure) were lost to follow up. These patients were assumed to be event free for the main analyses.
Stroke
Any stroke (fatal, non‐fatal, ipsilateral, contralateral, brainstem, infarct or haemorrhage)
There was a significant reduction in the risk of any stroke during follow up with patching (OR 0.49, 95% CI 0.27 to 0.90, P = 0.02) (Analysis 2.1). A similar reduction was seen in fatal strokes (OR 0.27 0.05 to 1.6 P = 0.15) (Analysis 2.2) but this was based on only five events. Within each closure type there was no heterogeneity, but there was significant between‐group heterogeneity (I2 = 72.5).
Ipsilateral stroke
Thirty‐three strokes were definitely ipsilateral and one other stroke was assumed to be ipsilateral although it was unclear whether it actually was (Eikelboom 1988). The reduction in risk of ipsilateral stroke with patching was similar to that for all strokes (OR 0.32, 95% CI 0.16 to 0.63, P = 0.001) (Analysis 2.3).
Death
One‐hundred‐and‐forty‐three patients died during follow up (10.7%). Even if all patients lost to follow up were assumed to be alive, patching was associated with a non‐significant reduction in the risk of death (OR 0.78, 95% CI 0.54 to 1.12, P = 0.18)(Analysis 2.4). Again, as outlined above, few of these deaths were directly attributable to stroke.
Any stroke or death
Patching was associated with a significant reduction in the risk of stroke or death (OR 0.59, 95% CI 0.42 to 0.84, P = 0.004) (13% patch versus 20.6% primary closure) (Analysis 2.5).
Arterial complications
As noted in the Methods section, these results should be interpreted with caution since, in patients who underwent bilateral endarterectomies, outcomes in each artery were probably not independent. We were unable to identify how many patients with bilateral endarterectomies had outcomes events in both arteries.
Occlusion or restenosis greater than 50%
Patching was associated with a highly significant reduction in the risk of arterial occlusion or restenosis (OR 0.24, 95% CI 0.17 to 0.34, P < 0.00001) (Analysis 2.6). Within each closure type there was significant heterogeneity (I2 = 65) and there was significant between‐group heterogeneity (I2 = 72.4). Lack of data meant that it was not possible to correct for those patients who had died during follow up. However, the result appears to be particularly robust and is likely to remain significant even if corrected for the small numbers who died. Another problem is that the clinical significance of a reduction in occlusion or restenosis is unknown: the important outcome from the patient's point of view is a reduction in the risk of stroke. The trial by Eikelboom et al suggested that the reduction in restenosis or occlusion was confined to women, but this may be a chance subgroup effect or because women had an increased absolute risk of restenosis and so the numbers who developed restenosis were greater (Eikelboom 1988).
Pseudoaneurysm formation
No pseudoaneurysms were documented during follow up of at least one year in 1141 arteries.
Discussion
The results of this systematic review when first published in 1995 were considered to be inconclusive, although there appeared to be promising and potentially clinically important trends in favour of routine patching in terms of both short and long‐term reductions in risks of ipsilateral stroke. The results were felt to be unreliable because they were based on small number of outcome events (33 ipsilateral strokes in total), there were a number of losses to follow up and because methodological quality of the trials was on the whole poor (Table 1). However, in the 2004 update a good quality trial including 399 operations and 45 perioperative and long term events was added (AbuRahma 1996) and contributed additional weight to the conclusions drawn in the previous analyses. In the current update, three new small trials have been added, which has resulted in loss of statistical significance of the apparently reduced risk of any perioperative stroke in the patching group.
The significant reductions in the risk of acute occlusion or long‐term restenosis with patching may be less useful than data on clinically important outcomes such as stroke. Acute occlusion, though feared, is not always associated with stroke. Similarly, restenosis detected by routine Duplex scanning may not be clinically important. In some cases, remodelling of the arterial wall after endarterectomy can be mistaken for stenosis and in other cases spontaneous regression of Duplex defined stenosis has occurred (Bernstein 1990; Ranaboldo 1993). Moreover, in one study there was no significant association between restenosis and recurrent neurological symptoms (Knudsen 1990), whilst in another, patients with restenosis greater than 50% had a better long‐term prognosis in terms of death or stroke than patients with no significant restenosis (Bernstein 1990)!
Most surgeons agree that carotid patching does play a role in carotid endarterectomy since they are faced with situations when this type of closure is either unavoidable or positively desirable, for example an artery with a very narrow internal diameter or a very long plaque (Eikelboom 1988). However, it is unclear how frequently such situations arise and how narrow an artery should be before it has to be patched. For example, only two trials in this review excluded narrow arteries on the grounds that they must be patched. One trial excluded 23% of arteries because they were less than 5 mm diameter (Myers 1994), whilst another trial excluded only 1% of arteries because they were less than 3.5 mm diameter (Katz 1994). In the other trials, very few patients had to cross over from primary closure to patching because the artery was deemed too narrow for primary closure. A British survey also demonstrated that there is divided opinion on how often patching is required: some surgeons use it all of the time, others rarely or never (Girn 2008). The trials of patch versus no patch included in this review tested the policy of routinely patching all arteries against a policy of never patching in those patients in whom there was no definite indication for a patch. A policy of selective patching of only those arteries thought to require a patch at the time of operation compared to no patching has not been tested in randomised controlled trials.
It is possible that if patching is effective its benefit may be restricted to narrow arteries (Golledge 1996). This would be analogous to carotid endarterectomy for symptomatic carotid stenosis where the benefit is restricted to those with severe artery stenosis (ECST 1991). We were unable to test this hypothesis because the results of the trials were not reported according to the degree of narrowing of the artery. One trial did exclude a significant number of arteries because they were less than 5 mm diameter (Myers 1994). The results of this trial were no worse than those of the other trials, which might suggest that there is little difference in the effect of patching between arteries greater than or less than 5 mm diameter. However, such indirect comparisons between trials are unreliable.
There were significant methodological flaws in these trials which should be addressed in future trials. Inadequate methods of randomisation and blinding were frequently used, which can seriously bias the results of trials (Schulz 1995). In most trials, the blinding of outcome assessment was unclear. Three trials mentioned blinding, but no trial assessed outcome by neurologists or stroke physicians. It is well known that studies that have neurologists as assessors are associated with higher stroke and death rates (Rothwell 1995). The trials were generally too small to achieve adequate statistical power and none were analysed on a true intention‐to‐treat basis, partly because there were significant losses to follow up. Problems arose with the randomisation of arteries rather than patients, and there was poor reporting of the numbers of ipsilateral strokes and disabling strokes in each treatment group.
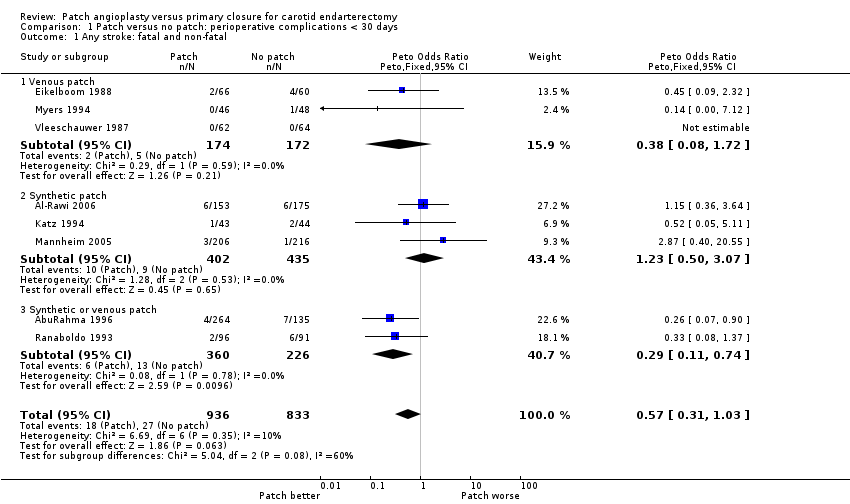
Comparison 1 Patch versus no patch: perioperative complications < 30 days, Outcome 1 Any stroke: fatal and non‐fatal.
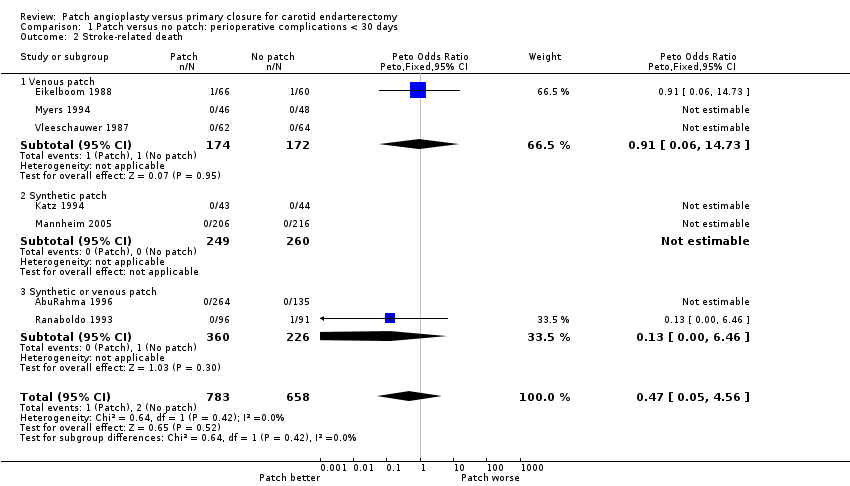
Comparison 1 Patch versus no patch: perioperative complications < 30 days, Outcome 2 Stroke‐related death.

Comparison 1 Patch versus no patch: perioperative complications < 30 days, Outcome 3 Stroke ipsilateral to endarterectomy site.
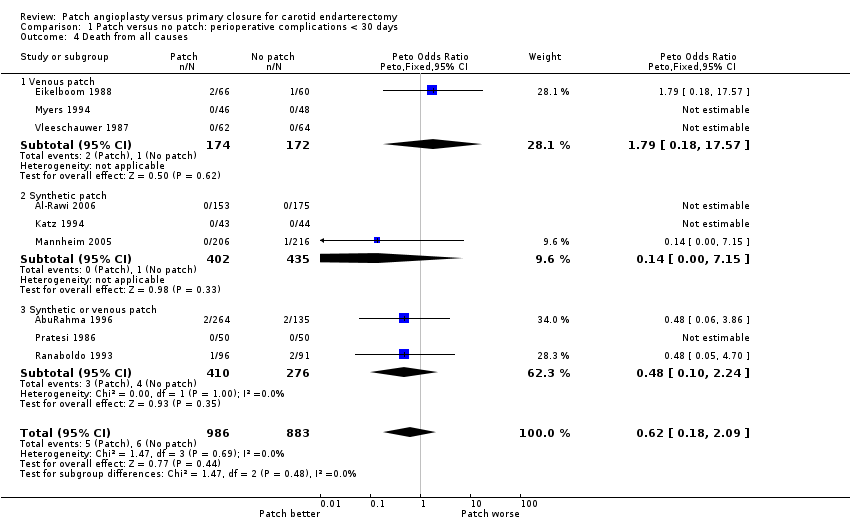
Comparison 1 Patch versus no patch: perioperative complications < 30 days, Outcome 4 Death from all causes.
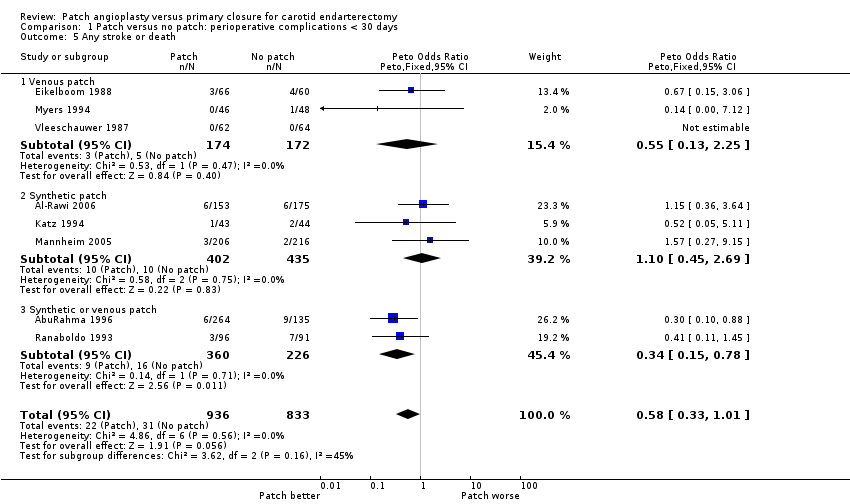
Comparison 1 Patch versus no patch: perioperative complications < 30 days, Outcome 5 Any stroke or death.

Comparison 1 Patch versus no patch: perioperative complications < 30 days, Outcome 6 Occlusion of the artery operated on.

Comparison 1 Patch versus no patch: perioperative complications < 30 days, Outcome 7 Rupture/haemorrhage of endarterectomy site.

Comparison 1 Patch versus no patch: perioperative complications < 30 days, Outcome 8 Infection of the endarterectomy site.
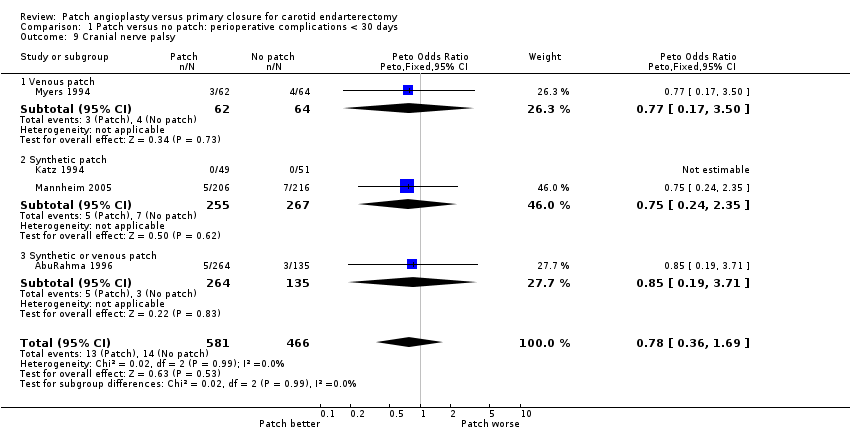
Comparison 1 Patch versus no patch: perioperative complications < 30 days, Outcome 9 Cranial nerve palsy.

Comparison 1 Patch versus no patch: perioperative complications < 30 days, Outcome 10 Complication with return to theatre.
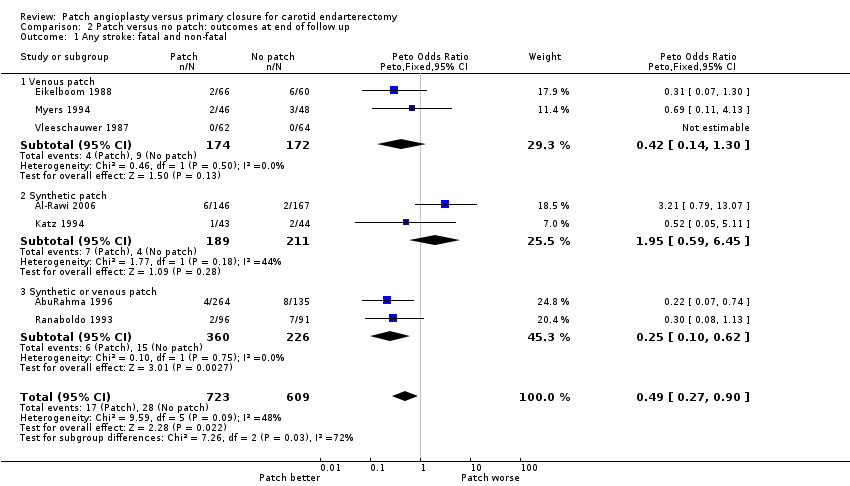
Comparison 2 Patch versus no patch: outcomes at end of follow up, Outcome 1 Any stroke: fatal and non‐fatal.
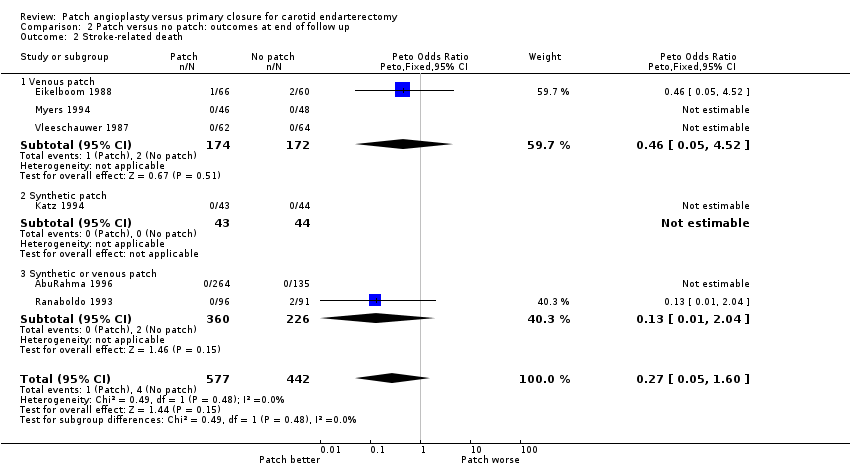
Comparison 2 Patch versus no patch: outcomes at end of follow up, Outcome 2 Stroke‐related death.
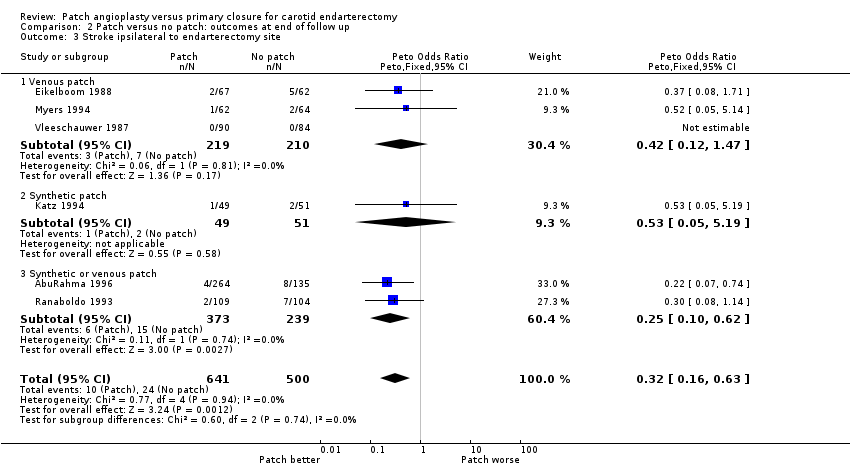
Comparison 2 Patch versus no patch: outcomes at end of follow up, Outcome 3 Stroke ipsilateral to endarterectomy site.
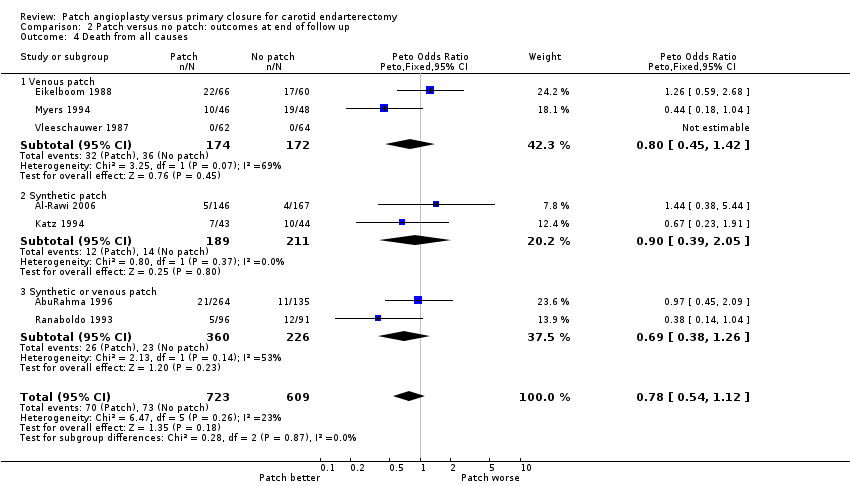
Comparison 2 Patch versus no patch: outcomes at end of follow up, Outcome 4 Death from all causes.

Comparison 2 Patch versus no patch: outcomes at end of follow up, Outcome 5 Any stroke or death.

Comparison 2 Patch versus no patch: outcomes at end of follow up, Outcome 6 Restenosis/occlusion of the operated artery.
| Study | Total patients | Total operations | Patch lost at 30 days | Patch lost at end | Primary lost at 30 days | Primary lost at end | Number of exclusions | Crossover patch ‐ non | Crossover non ‐ patch |
| 357 | 399 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | |
| 315 | 338 | 0 | 7 | 0 | 8 | 10 | Data not available | Data not available | |
| 126 | 129 | 0 | 10 patients lost to doppler FU but not clinical FU | 0 | 7 to doppler FU but not clinical FU | 0 | 3 | 3 | |
| 87 | 100 | 0 | 5 | 0 | 7 | 0 | 0 | 0 | |
| 123 | 140 | 0 | 0 | 0 | 0 | 4 | Between 0 and 4 | Between 0 and 4 | |
| 404 | 422 | 0 | Data not available | 0 | Data not available | Data not available | 0 | 0 | |
| 136 (109 after exclusion of 27 patients undergoing obligatory vein patching) | 152 (122 analysed as 30 operations got obligatory vein patches) | 0 | 6 | 0 | 8 | 30 operations underwent obligatory vein patch closure and 16 patients had both sides done (total 46) | 0 | 0 | |
| 100 | 100 | Data not available | Data not available | Data not available | Data not available | Data not available | Data not available | Data not available | |
| 199 | 213 | 0 | 5 | 0 | 12 | 0 | 0 | 0 at 30‐day FU but 4 at 1‐year FU | |
| 126 | 174 | 0 | Data not available | 0 | Data not available | 0 | 0 | 0 | |
| FU: follow up | |||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any stroke: fatal and non‐fatal Show forest plot | 8 | 1769 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.57 [0.31, 1.03] |
| 1.1 Venous patch | 3 | 346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.38 [0.08, 1.72] |
| 1.2 Synthetic patch | 3 | 837 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.23 [0.50, 3.07] |
| 1.3 Synthetic or venous patch | 2 | 586 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.29 [0.11, 0.74] |
| 2 Stroke‐related death Show forest plot | 7 | 1441 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.47 [0.05, 4.56] |
| 2.1 Venous patch | 3 | 346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.91 [0.06, 14.73] |
| 2.2 Synthetic patch | 2 | 509 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 Synthetic or venous patch | 2 | 586 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.00, 6.46] |
| 3 Stroke ipsilateral to endarterectomy site Show forest plot | 7 | 1201 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.31 [0.15, 0.63] |
| 3.1 Venous patch | 3 | 349 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.39 [0.09, 1.75] |
| 3.2 Synthetic patch | 1 | 100 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.53 [0.05, 5.19] |
| 3.3 Synthetic or venous patch | 3 | 752 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.27 [0.11, 0.62] |
| 4 Death from all causes Show forest plot | 9 | 1869 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.62 [0.18, 2.09] |
| 4.1 Venous patch | 3 | 346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.79 [0.18, 17.57] |
| 4.2 Synthetic patch | 3 | 837 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.14 [0.00, 7.15] |
| 4.3 Synthetic or venous patch | 3 | 686 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.48 [0.10, 2.24] |
| 5 Any stroke or death Show forest plot | 8 | 1769 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.58 [0.33, 1.01] |
| 5.1 Venous patch | 3 | 346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.55 [0.13, 2.25] |
| 5.2 Synthetic patch | 3 | 837 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.10 [0.45, 2.69] |
| 5.3 Synthetic or venous patch | 2 | 586 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.34 [0.15, 0.78] |
| 6 Occlusion of the artery operated on Show forest plot | 7 | 1435 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.18 [0.08, 0.41] |
| 6.1 Venous patch | 2 | 255 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.01, 1.99] |
| 6.2 Synthetic patch | 2 | 428 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.33 [0.06, 1.95] |
| 6.3 Synthetic or venous patch | 3 | 752 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.16 [0.06, 0.42] |
| 7 Rupture/haemorrhage of endarterectomy site Show forest plot | 9 | 2031 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.24 [0.61, 2.54] |
| 7.1 Venous patch | 3 | 429 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 6.86 [0.14, 346.63] |
| 7.2 Synthetic patch | 3 | 850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.92 [0.39, 2.14] |
| 7.3 Synthetic or venous patch | 3 | 752 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.32 [0.56, 9.57] |
| 8 Infection of the endarterectomy site Show forest plot | 7 | 1563 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.38 [0.09, 1.54] |
| 8.1 Venous patch | 3 | 429 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Synthetic patch | 2 | 522 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.38 [0.09, 1.54] |
| 8.3 Synthetic or venous patch | 2 | 612 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Cranial nerve palsy Show forest plot | 4 | 1047 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.78 [0.36, 1.69] |
| 9.1 Venous patch | 1 | 126 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.77 [0.17, 3.50] |
| 9.2 Synthetic patch | 2 | 522 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.75 [0.24, 2.35] |
| 9.3 Synthetic or venous patch | 1 | 399 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.85 [0.19, 3.71] |
| 10 Complication with return to theatre Show forest plot | 7 | 1281 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.35 [0.16, 0.79] |
| 10.1 Venous patch | 3 | 429 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.98 [0.06, 15.64] |
| 10.2 Synthetic patch | 1 | 100 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.53 [0.05, 5.19] |
| 10.3 Synthetic or venous patch | 3 | 752 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.29 [0.12, 0.73] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any stroke: fatal and non‐fatal Show forest plot | 7 | 1332 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.49 [0.27, 0.90] |
| 1.1 Venous patch | 3 | 346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.42 [0.14, 1.30] |
| 1.2 Synthetic patch | 2 | 400 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.95 [0.59, 6.45] |
| 1.3 Synthetic or venous patch | 2 | 586 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.25 [0.10, 0.62] |
| 2 Stroke‐related death Show forest plot | 6 | 1019 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.27 [0.05, 1.60] |
| 2.1 Venous patch | 3 | 346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.46 [0.05, 4.52] |
| 2.2 Synthetic patch | 1 | 87 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 Synthetic or venous patch | 2 | 586 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.01, 2.04] |
| 3 Stroke ipsilateral to endarterectomy site Show forest plot | 6 | 1141 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.32 [0.16, 0.63] |
| 3.1 Venous patch | 3 | 429 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.42 [0.12, 1.47] |
| 3.2 Synthetic patch | 1 | 100 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.53 [0.05, 5.19] |
| 3.3 Synthetic or venous patch | 2 | 612 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.25 [0.10, 0.62] |
| 4 Death from all causes Show forest plot | 7 | 1332 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.78 [0.54, 1.12] |
| 4.1 Venous patch | 3 | 346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.80 [0.45, 1.42] |
| 4.2 Synthetic patch | 2 | 400 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.90 [0.39, 2.05] |
| 4.3 Synthetic or venous patch | 2 | 586 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.69 [0.38, 1.26] |
| 5 Any stroke or death Show forest plot | 6 | 1019 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.59 [0.42, 0.84] |
| 5.1 Venous patch | 3 | 346 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.69 [0.40, 1.20] |
| 5.2 Synthetic patch | 1 | 87 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.62 [0.23, 1.66] |
| 5.3 Synthetic or venous patch | 2 | 586 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.51 [0.30, 0.86] |
| 6 Restenosis/occlusion of the operated artery Show forest plot | 8 | 1719 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.24 [0.17, 0.34] |
| 6.1 Venous patch | 3 | 429 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.34 [0.17, 0.66] |
| 6.2 Synthetic patch | 3 | 678 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.46 [0.22, 0.98] |
| 6.3 Synthetic or venous patch | 2 | 612 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.15 [0.09, 0.25] |

