Yoga para el tratamiento de la incontinencia urinaria en mujeres
Resumen
Antecedentes
La incontinencia urinaria en las mujeres se asocia con una calidad de vida deficiente y con dificultades en la funcionalidad social, psicológica y sexual. La enfermedad puede afectar hasta un 15% de mujeres de edad media o mayores en la población general. Los tratamientos conservadores como las intervenciones de estilo de vida, el entrenamiento vesical y el entrenamiento muscular del suelo pelviano (solas o en combinación con otras intervenciones) son los enfoques iniciales para el tratamiento de la incontinencia urinaria. Muchas mujeres están interesadas en tratamientos adicionales como el yoga, un sistema de filosofía, estilo de vida y práctica física que se originó en la India antigua.
Objetivos
Evaluar los efectos del yoga en el tratamiento de la incontinencia urinaria en mujeres.
Métodos de búsqueda
Se realizaron búsquedas en los registros especializados Cochrane de Incontinencia y de Medicina Complementaria. Se hicieron búsquedas en la World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) y en ClinicalTrials.gov para identificar cualquier estudio en curso o no publicado. Se hicieron búsquedas manuales de las actas de los congresos International Congress on Complementary Medicine Research y el European Congress for Integrative Medicine. Se buscaron estudios económicos en la NHS Economic Evaluation Database, y se complementó esta búsqueda con búsquedas de estudios económicos en MEDLINE y Embase a partir de 2015. Las búsquedas en la base de datos están actualizadas hasta el 21 de junio 2018.
Criterios de selección
Ensayos controlados aleatorios en mujeres con diagnóstico de incontinencia urinaria en que un grupo fue asignado al tratamiento con yoga.
Obtención y análisis de los datos
Dos autores de revisión de forma independiente cribaron los títulos y los resúmenes de todos los artículos recuperados, seleccionaron los estudios para la inclusión, extrajeron los datos, evaluaron el riesgo de sesgo y la certeza de la evidencia para cada resultado informado. Los desacuerdos se resolvieron mediante consenso. Se programó combinar los estudios clínicamente comparables en Review Manager 5 con el metanálisis de efectos aleatorios, y realizar los análisis de subgrupos y de sensibilidad. Se programó diseñar una tabla que enumerara los estudios económicos sobre el yoga para la incontinencia sin realizar análisis sobre estos estudios.
Resultados principales
Se incluyeron dos estudios (con un total de 49 mujeres). Cada estudio comparó el yoga con un comparador diferente, por lo que fue imposible combinar los datos en un metanálisis. Espera ser evaluado un tercer estudio que se ha completado pero aún no se informó en forma completa.
Uno de los estudios incluidos duró seis semanas y comparó el yoga con una lista de espera en 19 mujeres con incontinencia urinaria de urgencia o de esfuerzo. Se consideró que la certeza de la evidencia para todos los resultados informados fue muy baja debido al sesgo de rendimiento y de detección y a la imprecisión. No se presentó el número de mujeres que informó de curación. No puede precisarse si el yoga resulta en satisfacción con la curación o mejoría de la incontinencia (cociente de riesgos [CR] 6,33; intervalo de confianza [IC] del 95%: 1,44 a 27,88; un aumento de 592 a 111 por 1000; IC del 95%: 160 a 1000). No puede precisarse si hay una diferencia entre el yoga y la lista de espera en la calidad de vida específica de la enfermedad, medida con el Incontinence Impact Questionnaire Short Form (diferencia de medias [DM] 1,74; IC del 95%: ‐33,02 a 36,50); el número de micciones (DM ‐0,77; IC del 95%: ‐2,13 a 0,59); la cantidad de episodios de incontinencia (DM ‐1,57; IC del 95%: ‐2,83 a ‐0,31); o las molestias ocasionadas por la incontinencia según el Urogenital Distress Inventory 6 (DM ‐0,90; IC del 95%: ‐1,46 a ‐0,34). No hubo evidencia de una diferencia en la cantidad de mujeres que presentaron al menos un evento adverso (diferencia de riesgos 0%, IC del 95%: ‐38% a 38%; ninguna diferencia de 222 por 1000; IC del 95%: 380 menos a 380 más).
El segundo estudio incluido duró ocho semanas e incorporó a 30 mujeres con incontinencia urinaria de urgencia; comparó la reducción del estrés basada en la atención plena (REBAP) con una intervención de control activo de clases de yoga. El estudio no fue cegado y presentaba un alto desgaste en ambos grupos del estudio para todas las evaluaciones de resultados. La certeza de la evidencia para todos los resultados informados se consideró muy baja debido al sesgo de rendimiento y de desgaste, a la imprecisión y a la falta de direccionalidad. No se presentó el número de mujeres que informó de curación. No se sabe si fue menos probable que las pacientes del grupo de yoga informaran sobre la mejoría de la incontinencia a las ocho semanas en comparación con las pacientes del grupo de REBAP (CR 0,09; IC del 95%: 0,01 a 1,43; una disminución de 419 a 461 por 1000 (IC del 95%: 5 a 660). La certeza es muy baja acerca del efecto de la RSBA en comparación con el yoga en los informes de curación o mejoría de la incontinencia, la mejoría de la calidad de vida específica de la enfermedad medida con la Overactive Bladder Health‐Related Quality of Life Scale, la reducción de los episodios de incontinencia o la reducción de las molestias causadas por la incontinencia según se midieron en el Overactive Bladder Symptom and Quality of Life‐Short Form a las ocho semanas. Los ensayos no informaron sobre los efectos adversos.
Conclusiones de los autores
Se identificaron pocos ensayos sobre el yoga para la incontinencia, y los ensayos existentes eran pequeños y de alto riesgo de sesgo. Además, no se encontraron estudios de los resultados económicos relacionados con el yoga para la incontinencia urinaria. Debido a la falta de evidencia para responder a la pregunta de la revisión, no se sabe si el yoga es útil para las pacientes con incontinencia urinaria. Se necesitan más ensayos, bien realizados y con tamaños de la muestra más grandes.
PICO
Resumen en términos sencillos
Yoga para el tratamiento de la incontinencia urinaria en mujeres
Pregunta de la revisión
Se examinó si el yoga es útil para el tratamiento de la incontinencia urinaria en mujeres. Se comparó el yoga con ningún tratamiento y con otros tratamientos para la incontinencia. También se comparó el yoga junto con otros tratamientos versus otros tratamientos solos. El análisis se centró en los síntomas de incontinencia, la calidad de vida y los efectos adversos. También se buscó información acerca de la relación entre coste y beneficio del tratamiento con yoga.
Antecedentes
Hasta un 15% de mujeres de edad media o mayores pueden presentar incontinencia urinaria. La incontinencia puede clasificarse como incontinencia urinaria de urgencia (definida como una pérdida involuntaria de orina asociada con un deseo repentino e imperioso de orinar) e incontinencia urinaria de esfuerzo (en que la pérdida involuntaria de orina resulta de una actividad como el estornudo). Ambos tipos pueden afectar negativamente la calidad de vida y la funcionalidad social, psicológica y sexual. El tratamiento de la incontinencia generalmente comienza con asesoramiento sobre los cambios del estilo de vida, como reducir el consumo de cafeína, intervenciones conductuales como el entrenamiento vesical o ejercicios para los músculos del suelo pelviano. Sin embargo, muchas mujeres están interesadas en tratamientos adicionales como el yoga, un sistema de filosofía, estilo de vida y práctica física que se originó en la India antigua.
¿Cuál es el grado de actualización de esta revisión?
La evidencia está actualizada hasta el 21 de junio de 2018.
Características de los estudios
Se encontraron dos estudios con un total de 49 mujeres. Uno era un estudio de seis semanas que comparó el yoga con una lista de espera (tratamiento retrasado) en las pacientes con incontinencia urinaria de esfuerzo o urgencia. El otro era un estudio de ocho semanas que comparó el yoga con la reducción del estrés basada en la atención plena (REBAP) de mujeres con incontinencia urinaria de urgencia. También se identificó un estudio en curso que incorporó a 50 mujeres, cuyo objetivo es comparar el yoga con el estiramiento; este estudio se incluirá cuando se presenten los resultados.
Resultados clave
El ensayo que compara el yoga con una lista de espera no presentó datos de la cantidad de mujeres que informaron sobre la curación aunque sí presentó datos sobre los síntomas, la calidad de vida específica de la enfermedad y los efectos adversos. Aunque esta comparación en general favoreció la intervención con yoga, debido a la certeza muy baja de la evidencia no puede precisarse si mejora la incontinencia urinaria. No hubo diferencias entre los grupos en la cantidad de mujeres que informaron de un evento adverso, y no se informó ningún evento adverso grave (aunque no puede precisarse si el yoga aumenta el daño ya que la certeza de la evidencia es muy baja).
El ensayo que comparó el yoga con la REBAP informó sobre los síntomas y la calidad de vida específica de la enfermedad pero no presentó datos sobre la cantidad de mujeres que informaron de la curación. Aunque en general esta comparación favoreció la intervención de REBAP, no puede precisarse si el yoga mejora la incontinencia urinaria debida a la certeza muy baja de la evidencia. No había información sobre eventos adversos.
No se encontró información sobre la relación entre coste y beneficio del yoga para la incontinencia urinaria.
Calidad de la evidencia
Aunque se identificó cierta evidencia del tratamiento con yoga para la incontinencia urinaria en mujeres, los estudios incluidos fueron muy pequeños y presentaron problemas en el modo en que se realizaron, lo que limita la confianza en los resultados. Debido a la naturaleza de los tratamientos, las participantes y el personal del ensayo que compara el yoga con una lista de espera sabían a qué grupos fueron asignadas las pacientes, y es posible que las del grupo de yoga informaran de algunos beneficios porque esperaban que el yoga fuese útil. El objeto del ensayo que compara el yoga con la REBAP no fue analizar el yoga como tratamiento para la incontinencia. En cambio, el ensayo analizó la REBAP como tratamiento y utilizó clases de yoga para asegurarse de que las mujeres del grupo de comparación recibieran atención del personal del estudio. Además, el ensayo que compara el yoga con la REBAP no obtuvo resultados en todas las pacientes, y es posible que en las que informaron de resultados los hallazgos fuesen mejores o peores que las que no informaron de resultados. La evidencia de buena calidad es insuficiente para decidir si el yoga es útil para las pacientes con incontinencia urinaria.
Conclusiones de los autores
Summary of findings
| Yoga compared with wait‐list for urinary incontinence in women | ||||||
| Patient or population: women with either stress‐predominant or urge‐predominant urinary incontinence Settings: community Intervention: yoga Comparison: wait‐list | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Wait‐list | Yoga | |||||
| Number of women who report they are cured (they no longer experience urinary incontinence) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
| Number of women who report cure or improvement of urinary incontinence at short term (six weeks) | 111 per 1000 | 703 per 1000 | RR 6.33 (1.44 to 27.88) | 18 | ⊕⊝⊝⊝ | Number of women who reported satisfaction with change in urine leakage. |
| Urinary incontinence condition‐ or symptom‐specific quality of life at short term (6 weeks) Measured by Incontinence Impact Questionnaire Short Form (IIQ‐7) (lower = better) | The mean change in the control group was a decrease of 31 units. | The mean change in the intervention group was 1.74 units higher (33.02 units lower to 36.50 units higher). | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Number of micturitions (daily) at short term (6 weeks) | The mean change in the control group was a decrease of 0.13 micturitions. | The mean change in the intervention group was | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Number of episodes of incontinence (daily) at short term (6 weeks) | The mean change in the control group was a decrease of 0.27 episodes. | The mean change in the intervention group was | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Bothersomeness of symptoms at short term (6 weeks) Measured by Urogenital Distress Inventory 6 (UDI‐6) (lower = better) | The mean change in the control group was a decrease of 0.1 units. | The mean change in the intervention group was 0.90 units lower (0.34 to 1.46 lower). | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Adverse effects at short term (6 weeks) | 222 per 1000 | 222 per 1000 | RD 0% (‐38% to 38%) | 18 | ⊕⊝⊝⊝ | 2 women in each group reported an adverse effect. However, there were 7 adverse effects overall and the distribution of adverse effects between groups is not reported. None of the adverse effects were considered to be potentially related to the study and none were serious. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded two levels for risk of bias because there was no blinding of participants or providers (risk of performance bias), and outcome was self assessed and self recorded by participants (risk of detection bias). | ||||||
| Yoga compared with mindfulness‐based stress reduction (MBSR) for urinary incontinence in women | ||||||
| Patient or population: women with urge‐predominant urinary incontinence Settings: community Intervention: yoga Comparison: mindfulness‐based stress reduction (MBSR) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| MBSR | Yoga | |||||
| Number of women who report they are cured (they no longer experience urinary incontinence) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
| Number of women who report cure or improvement of urinary incontinence at short term (8 weeks) | 461 per 1000 | 42 per 1000 | RR 0.09 (0.01 to 1.43) | 24 | ⊕⊝⊝⊝ | |
| Urinary incontinence condition‐ or symptom‐specific quality of life at short term (8 weeks) Measured by the Overactive Bladder Health‐Related Quality of Life (OAB‐HRQL) scale (higher per cent improvement = better) | ‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent improvement at 8 weeks was 8.70 (IQR 1.75 to 20.59) in the yoga group (n = 11) and 29.27 (IQR 8.11 to 93.33) in the MBSR group (n = 13) (reported P value = 0.03). |
| Number of micturitions (daily) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
| Number of episodes of incontinence (daily) at short term (8 weeks) | ‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent improvement at 8 weeks was ‐33.33 (IQR ‐50.00 to 16.67) in the yoga group (n = 11) and ‐60 (IQR ‐88.89 to ‐50.00) in the MBSR group (n = 13) (reported P value = 0.03). |
| Bothersomeness of symptoms at short term (6 weeks) Measured by the Overactive Bladder Symptom and Quality of Life‐Short Form (OABq‐SF) (lower = better) | ‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent change at 8 weeks was ‐25.0 (IQR ‐35 to 20) in the yoga group (n = 11) and ‐55.6 (IQR ‐50 to ‐87) in the MBSR group (n = 13) (reported P value = 0.005). |
| Adverse effects | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report on adverse effects. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded two levels for risk of bias because there was no blinding of participants or providers (risk of performance bias), and there was a high percentage of loss to follow‐up that was unbalanced across study arms (risk of attrition bias). | ||||||
Antecedentes
Descripción de la afección
La International Continence Society (ICS) y la International Urogynecological Association definen la incontinencia urinaria como "la pérdida involuntaria de orina" (Bø 2017; Haylen 2010). Los cálculos de la prevalencia de la incontinencia urinaria son controvertidos y varían mucho según las definiciones de casos así como los métodos de verificación. Las pacientes a menudo tardan en buscar ayuda para la incontinencia urinaria, y es probable que esta afección estigmatizada no sea informada en grado suficiente (Wójtowicz 2014). En las pacientes embarazadas o posparto, los cálculos de la prevalencia de la incontinencia urinaria alcanzan el 30% o más (Milsom 2017). En las mujeres de edad media o mayores de la población general, la incontinencia urinaria diaria se estima entre un 5% y un 15%, mientras la prevalencia de los síntomas de incontinencia entre todas las mujeres adultas se estima entre 25% y 45% (Milsom 2017). La mayor edad es el factor de riesgo aceptado más ampliamente, aunque la cantidad de partos (sobre todo partos vaginales asistidos), la obesidad y el estado menopáusico a menudo también se consideran factores de riesgo importantes (Milsom 2017).
Existen tres tipos principales de incontinencia urinaria, que se definen según los síntomas: la incontinencia urinaria de esfuerzo (IUE), la incontinencia urinaria de urgencia (IUU) y la incontinencia urinaria mixta (IUM). Aunque las tasas de prevalencia específicas no son congruentes entre los estudios, la IUE es de modo sistemático el tipo más frecuente de incontinencia urinaria, responsable de cerca de la mitad de todos los casos, seguida de la IUM y luego por la IUU (Milsom 2017).
La incontinencia urinaria de esfuerzo se define como la pérdida involuntaria de orina con el esfuerzo/ejercicio físico o con el estornudo o la tos (Bø 2017; Haylen 2010). La incontinencia urinaria de esfuerzo ocurre cuando aumenta la presión intraabdominal frente a un esfuerzo o durante un estornudo o la tos y cuando la presión sobre la vejiga es mayor que la presión de cierre del esfínter uretral (Cannon 2004). Aunque la IUE puede tener varias causas, a menudo se asocia con debilidad de los músculos de la pelvis y el tejido dependiente del colágeno, que puede llevar a una falta de sostén uretral y la incapacidad para mantener la presión del esfínter uretral (Long 2008).
La incontinencia urinaria de urgencia se define como la pérdida involuntaria de orina asociada con la urgencia (Bø 2017; Haylen 2010). El tenesmo es el deseo súbito e imperioso de orinar, que es difícil de posponer (Abrams 2013). La incontinencia urinaria de urgencia es una forma de vejiga hiperactiva, que incluye síntomas de urgencia, polaquiuria y despertar de noche para orinar (nicturia). Las causas de vejiga hiperactiva y de la IUU específicamente no están claras, pero se cree que los factores fisiopatológicos subyacentes incluyen trastornos del urotelio e hiperactividad de los nervios y del músculo liso detrusor (Steers 2002).
La incontinencia urinaria mixta se define como la presencia de síntomas tanto de IUE como de IUU (Bø 2017; Haylen 2010).
La incontinencia urinaria en las mujeres se asocia con una calidad de vida deficiente y repercute negativamente en la funcionalidad social, psicológica y sexual (Sinclair 2011). La depresión parece asociarse con la incontinencia urinaria, aunque no puede precisarse si los efectos físicos y sociales de la incontinencia llevan a la depresión o si la presencia de depresión acentúa las molestias de los síntomas de incontinencia (Abrams 2013). Aunque todas las formas de incontinencia urinaria se asocian con una calidad de vida deficiente y las formas más graves parecen tener una mayor repercusión sobre esta, puede ser más probable que las pacientes con IUU o IUM informen molestias "importantes" debidas a la incontinencia en comparación con las pacientes con IUE. Además, en las pacientes con un grado severo de IUM puede ser mayor la repercusión sobre la calidad de vida en comparación con las pacientes con un grado severo de IUU o IUE (Minassian 2013; Monz 2007).
Descripción de la intervención
El yoga, un sistema de práctica física, estilo de vida y filosofía, originado en la India antigua, ha aumentado su popularidad en Occidente durante el último siglo. Aunque tradicionalmente se describen ocho "ramas" o "pasos" en la práctica del yoga, en la actualidad se practican muchos estilos que enfatizan sobre todo la integración de las posturas corporales (asanas), el control de la respiración (pranayama) y la concentración (dharana) o la meditación (dhyana) (Hewitt 2001; Taneja 2014). La popularidad del yoga en Occidente ha seguido en aumento durante la última década. Por ejemplo, según la National Health Interview Survey (NHIS) de EE.UU., realizada en 2002, 2007 y 2012, el uso informado de yoga en los EE.UU. aumentó de aproximadamente 5,1% de adultos en 2002 a más de 9,5% en 2012 (Clarke 2015). En la NHIS 2012, el uso del yoga fue mayor en mujeres que en hombres, y mayor en adultos de 18 a 44 años de edad que para los grupos de más edad (Cramer 2016).
Se ha sugerido la utilidad del yoga para el control de diversos trastornos médicos, incluidas las enfermedades musculoesqueléticas y cardiovasculares, el estrés, la depresión y la ansiedad (Taneja 2014). En el NHIS 2012, los usos terapéuticos más frecuentes del yoga fueron para el dolor lumbar (19,7%), el estrés (6,4%) y la artritis (6,4%) (Cramer 2016).
El yoga parece ser una práctica relativamente segura. En una revisión de los informes de casos y series de casos de eventos adversos del yoga, se identificaron los problemas musculoesqueléticos como los más frecuentes, y las técnicas de yoga que con mayor frecuencia se asociaron a eventos adversos fueron: postura del pino, postura de la vela, posición de loto y respiración forzada (Cramer 2013). Cramer 2013 recomendó que las prácticas de yoga se adapten a los trastornos médicos preexistentes y se realicen bajo la supervisión de un profesor capacitado. En una revisión reciente de ensayos aleatorios sobre yoga se halló que el yoga se asocia con un riesgo mayor efectos adversos no graves y relacionados con la intervención que las intervenciones psicológicas o educativas, aunque no con un mayor riesgo de eventos adversos graves. La revisión también sostuvo que el yoga se asocia con el mismo riesgo de efectos adversos graves, no graves y relacionados con la intervención que la atención habitual o las intervenciones de ejercicios no relacionados con el yoga (Cramer 2015). La tasa general de eventos adversos graves en los grupos de yoga de los ensayos fue de un 0,6% (Cramer 2015).
De qué manera podría funcionar la intervención
Por lo general, la incontinencia urinaria se controla inicialmente con terapias conservadoras (Abrams 2013). Éstas incluyen intervenciones en el estilo de vida, el entrenamiento vesical y el entrenamiento muscular del suelo pelviano (solas o en combinación con otros tratamientos activos como la biorretroalimentación) (Ayeleke 2015; Dumoulin 2018; Herderschee 2011; Imamura 2015; Wallace 2004).
Hay evidencia sólida para apoyar el uso del entrenamiento muscular del suelo pelviano como un primer enfoque para el control de la incontinencia urinaria, particularmente la IUE (Dumoulin 2018). Con el entrenamiento muscular del suelo pelviano, las contracciones musculares del piso pelviano conscientes y cronometradas adecuadamente pueden aumentar la presión uretral y prevenir la pérdida urinaria asociada con la IUE (DeLancey 1988; Miller 1998). El fortalecimiento de los músculos del suelo pelviano también puede mejorar el sostén del cuello vesical y reducir la incontinencia urinaria (Bø 2004). Finalmente, las contracciones musculares del suelo pelviano pueden inhibir las contracciones musculares del detrusor y prevenir la pérdida urinaria asociada con la IUU (Bø 2000).
Algunos estudios indican que algunas técnicas de respiración del yoga, de relajación y de control muscular pueden ayudar en el fortalecimiento del suelo pelviano (Bø 2013; Tenfelde 2014). Se cree que las posturas específicas del yoga que son útiles y se han estudiado incluyen: Utkatasana (postura de la silla), Trikonasana (postura del triángulo) y Malasana (postura de la guirnalda) (Huang 2014b). El yoga puede ayudar a mejorar la alineación corporal general, la flexibilidad, la fuerza, el control y la percepción, y se cree que estos efectos ayudan a fortalecer los músculos del suelo pelviano (Tenfelde 2014). Por lo tanto, el yoga puede funcionar como método alternativo de entrenamiento muscular del suelo pelviano o como complemento del entrenamiento. El yoga también puede ser útil para los problemas de salud mental y de calidad de vida mediantes sus posibles efectos sobre la depresión, el estrés y la ansiedad, y ayuda a los pacientes a controlar su trastorno médico.
Por qué es importante realizar esta revisión
La incontinencia urinaria es una enfermedad de alta prevalencia, que genera grandes molestias en las pacientes. Aunque se dispone de muchos tratamientos para la incontinencia urinaria, ningún tratamiento es universalmente efectivo y aceptable, y pueden ser de utilidad los enfoques adicionales al tratamiento. El yoga es una práctica de mente‐cuerpo cada vez más popular en Occidente, sobre todo en mujeres. Un estudio pre y post experimental sobre entrenamiento muscular del suelo pelviano con yoga Hatha adyuvante en mujeres con incontinencia de esfuerzo informó que la intervención combinada fue efectiva para mejorar la incontinencia (Kim 2015). Además, al menos en un ensayo aleatorio de yoga Iyengar para la incontinencia urinaria se han obtenido resultados alentadores en el tratamiento de la IUE y la IUU con yoga (Huang 2014b). Sin embargo, falta evidencia sobre la efectividad del yoga para la incontinencia y no se dispone de ninguna guía para los médicos ni las pacientes. Por lo tanto, es importante evaluar si el yoga puede ser efectivo como tratamiento primario o adyuvante para la incontinencia urinaria en mujeres.
Objetivos
Evaluar los efectos del yoga en el tratamiento de la incontinencia urinaria en mujeres.
Métodos
Criterios de inclusión de estudios para esta revisión
Tipos de estudios
Se incluyeron ensayos controlados aleatorios (ECA) y el primer período de ECA cruzados. Se excluyeron los ensayos controlados cuasialeatorios (ensayos en que la asignación al tratamiento se hizo mediante un método no aleatorio como la alternancia) porque el método de asignación puede llevar a sesgo en los cálculos del efecto. No se restringió la elegibilidad de los estudios por el idioma ni el estado de publicación.
Sólo se incluyeron estudios de economía sanitaria realizados junto con los estudios incluidos en el componente clínico de esta revisión sistemática (Shemilt 2011).
Tipos de participantes
Se incluyeron estudios que incorporaron a mujeres a partir de los 18 años con diagnóstico de incontinencia urinaria sobre la base de los signos, los síntomas o la evaluación urodinámica (según la definición de los autores de los ensayos). Sólo se incluyeron ensayos que incorporaron a hombres y mujeres si al menos un 90% de los participantes eran mujeres o si el ensayo presentaba datos de resultados y demográficos de las mujeres por separado. Se incluyeron ensayos que incorporaron mujeres con diagnóstico de incontinencia urinaria de esfuerzo, urgencia o mixta, así como ensayos con participantes que presentaban tipos mixtos o no clasificados de incontinencia urinaria.
Se incluyeron ensayos realizados en mujeres que presentaban incontinencia urinaria durante el período pre o posnatal. Dado que este grupo presenta diferencias fisiológicas con respecto a las mujeres no embarazadas o después del parto, y la evolución natural de la incontinencia en esta población es diferente de las pacientes no embarazadas, pueden diferir en este grupo los efectos de la intervención observados. Por lo tanto, no se agrupó a esta población con las pacientes que no estaban embarazadas o en posparto y se programó analizar los estudios por separado en toda la revisión.
Se excluyeron los estudios de pacientes en quienes la incontinencia urinaria se asoció a factores no relacionados con las vías urinarias, como los trastornos neurológicos o psiquiátricos, la deficiencia cognitiva o los trastornos de movilidad. También se excluyeron los estudios centrados en mujeres con enuresis nocturna.
Tipos de intervenciones
Se incluyeron estudios de yoga como tratamiento para la incontinencia urinaria, cuando el informe del estudio especificaba que la intervención era de "yoga" proporcionado en cualquier dosis, con cualquier frecuencia y de cualquier duración, porque se piensa que es probable que estos factores tengan variabilidad en la práctica.
Se incluyeron intervenciones que pertenecían a cualquier tradición de yoga pero se excluyeron los estudios en que la intervención de yoga no comprendía un componente de práctica física. Se incluyeron estudios que compararon el yoga con ningún tratamiento o con otro tratamiento activo. También se incluyeron estudios que compararon el yoga como complemento de otros tratamientos versus los mismos tratamientos sin el yoga. Los tipos de comparaciones incluidas fueron los siguientes.
-
Yoga versus ninguna intervención activa específica (p.ej. atención habitual, lista de espera).
-
Yoga versus una intervención activa (p.ej. intervención del estilo de vida o entrenamiento muscular del suelo pelviano), para la que se consideraron diferentes comparadores activos por separado (p.ej. yoga versus asesoramiento del estilo de vida, yoga versus entrenamiento muscular del suelo pelviano).
-
Yoga más una intervención versus la misma intervención sin yoga (p.ej. yoga como intervención adicional al entrenamiento del suelo pelviano versus entrenamiento del suelo pelviano solo), para lo cual se consideraron diferentes intervenciones por separado.
Se incluyeron estudios en que se proporcionaron cointervenciones si eran similares entre los grupos de intervención (p.ej. los grupos de yoga y de comparación recibieron asesoramiento sobre técnicas de terapia conductual).
No parecen ser habituales los estudios que comparan el yoga con una intervención de yoga simulada (Park 2014). Sin embargo, se programó considerar que estudios representen un tipo adicional de comparación (es decir, yoga versus yoga simulada) y se los analizaría por separado.
Se excluyeron los estudios de intervenciones basadas en el yoga (p.ej. ejercicios basados en las posturas de yoga) pero no caracterizadas como yoga, así como los estudios de intervenciones multimodales en que el yoga es sólo un componente entre otros, como la reducción del estrés basada en la atención plena (REBAP).
Tipos de medida de resultado
Se utilizaron los resultados sugeridos por el Standardisation Committee of the International Continence Society (Bø 2017; Haylen 2010). Las cinco categorías de resultados siguientes se recomiendan para la investigación del efecto de las intervenciones terapéuticas en mujeres con incontinencia urinaria (Lose 2001):
-
observaciones de la paciente (p.ej. síntomas);
-
cuantificación de los síntomas de la paciente (p.ej. pérdida de orina);
-
observaciones del médico (signos anatómicos y funcionales);
-
calidad de vida de la paciente (incontinencia urinaria: específica y general);
-
medidas económicas.
En esta revisión, se consideró al menos un resultado de cada una de las cuatro primeras categorías. Se incluyeron resultados específicos hallados comúnmente en otras revisiones Cochrane sobre incontinencia urinaria en mujeres, de modo que con esta revisión se puedan obtener resultados que se puedan comparar o combinar fácilmente con los de otras revisiones sobre el tratamiento para la misma enfermedad.
Resultados primarios
-
Número de mujeres que informan de curación (ya no presentan incontinencia urinaria).
-
Número de mujeres que informan de curación o mejoría de la incontinencia urinaria.
-
Calidad de vida específica de los síntomas o de la incontinencia urinaria, medida con cualquier escala relevante (p.ej. la Urinary Incontinence Quality of Life scale [Patrick 1999], el Incontinence Impact Questionnaire [Uebersax 1995], el International Consultation on Incontinence Modular Questionnaire Lower Urinary Tract Symptoms Quality of Life [ICIQ‐LUTSqol] [Nystrom 2015] o el Pelvic Floor Distress Inventory [PFDI] y el Pelvic Floor Impact Questionnaire [PFIQ] (Barber 2001)).
Resultados secundarios
-
Cuantificación de los síntomas
-
Número de micciones (diarias).
-
Número de episodios de incontinencia (diarios).
-
Pérdida de orina medida con la prueba del peso de la toalla o protector sanitario (pruebas a corto o largo plazo).
-
Síntomas, según el informe de las participantes del estudio en cualquier escala específica de la enfermedad (p.ej. el Severity Index for Urinary Incontinence in Women (Sandvik 1993)).
-
-
Observaciones del médico (signos anatómicos y funcionales)
-
Evaluación clínica de la presencia de la incontinencia, como la pérdida de orina durante una prueba de la tos.
-
Medición de la función muscular del suelo pelviano, como por electromiografía, presión de contracción vaginal, fuerza muscular del suelo pelviano y mediciones morfológicas (dinamometría, ecografía).
-
-
Calidad de vida
-
Calidad de vida medida en una escala que no es específica de la enfermedad ni de los síntomas (p.ej. la 36‐Item Short Form Health Survey [SF‐36]).
-
Depresión, ansiedad o molestias según escalas relevantes (p.ej. Beck Depression Inventory [BDI], Hospital Anxiety and Depression Scale [HADS]).
-
Otras medidas de repercusión emocional y social del trastorno, como las molestias causadas por la enfermedad, la repercusión social y la funcionalidad sexual.
-
-
Efectos adversos
-
Número de efectos adversos (p.ej. dolor, malestar).
-
Resultados principales de las tablas de "Resumen de resultados"
El GRADE Working Group recomienda incluir hasta siete resultados críticos en una revisión sistemática (Guyatt 2011a; Guyatt 2011b). Por lo tanto, se consideraron los siguientes resultados para evaluar la certeza de la evidencia:
-
Número de mujeres que informan de curación (ya no presentan incontinencia urinaria);
-
Número de mujeres que informan de curación o mejoría de la incontinencia urinaria;
-
Calidad de vida específica de los síntomas o de la incontinencia urinaria
-
Número de micciones (diarias);
-
Número de episodios de incontinencia (diarios);
-
Efectos adversos.
Momento de evaluación de los resultados
Se agruparon todos los resultados en tres puntos temporales: a corto plazo (más cercano a los tres meses después de la asignación al azar), a medio plazo (más cercano a los seis meses después de la asignación al azar) y a largo plazo (más cercano al año después de la asignación al azar). Cuando un ensayo incluido presentaba puntos temporales múltiples, se consideró el punto temporal a corto plazo primario y otros puntos temporales como secundarios.
Métodos de búsqueda para la identificación de los estudios
We did not impose any restrictions, for example language or publication status, on the literature searches described below.
Búsquedas electrónicas
Cochrane Incontinence Specialised Register
We drew on the search strategy developed for Cochrane Incontinence. We identified relevant trials from the Cochrane Incontinence Specialised Register. For more details of the search methods used to build the Specialised Register, please see the Group's webpages where details of the Register's development (from inception) and the most recent searches performed to populate the Register can be found. To summarise, the register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, MEDLINE In‐Process, MEDLINE Epub Ahead of Print, CINAHL, the US National Institutes of Health Ongoing Trials Register, ClinicalTrials.gov, the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) and handsearches of journals and conference proceedings. Many of the trials in the Cochrane Incontinence Specialised Register are also contained in CENTRAL.
The terms used to search the Cochrane Incontinence Specialised Register are provided in Appendix 1. The search is up‐to‐date as of 21 June 2018.
We searched for all eligible published and unpublished trials in all languages. We planned to translate any non‐English language abstracts for potential inclusion. We based our search strategy on concepts of types of study population, types of study design and symptoms of urinary incontinence such as leakage of urine.
Other electronic bibliographic databases
We also used the terms in Appendix 1 to search the Cochrane Complementary Medicine Field Specialised Register for relevant trials of yoga. The Complementary Medicine Field Specialised Register contains trials identified from CENTRAL, Chinese databases, Korean databases and multiple small databases that have been identified as good sources of complementary medicine trials (Wieland 2013). The search was last updated on 21 June 2018.
We performed searches of the NHS Economic Evaluation Database (NHS EED) in order to identify potential economic studies. As the last database searches for NHS EED were carried out in December 2014, we used the NHS EED search filters on 25 September 2017 to search MEDLINE and Embase for economics studies from January 2015 onwards. To retrieve the maximum number of potentially relevant records, we searched the NHS EED for 'yoga' and combined the term 'yoga' with the NHS EED search filters when searching MEDLINE and Embase. See Appendix 2 for the NHS EED search filters. A further updated search of MEDLINE and Embase was conducted on 22 January 2019 adding an additional set of terms to identify urinary incontinence related studies. This set of urinary incontinence related terms was combined with the NHS EED filters and the yoga terms ‐ further details can be found in Appendix 2.
We did not search AMED (Allied and Complementary Medicine Database), CINAHL (Cumulative Index to Nursing and Allied Health Literature) and IndMED for this version of the review because we ran preliminary test searches of these databases for the protocol and, after de‐duplication against the Cochrane Incontinence Specialised Register, they did not yield any additional records that met our inclusion criteria (Wieland 2017). For full details, please see Appendix 3 (AMED), Appendix 4 (CINAHL) and Appendix 5 (IndMED).
Búsqueda de otros recursos
We checked the reference lists of all included studies and systematic reviews for additional references. We contacted experts in the field and authors of included studies to identify additional unpublished studies. We also checked the proceedings of the following conferences for relevant research:
-
International Congress on Complementary Medicine Research (ICCMR) (2010 to 2017); and
-
European Congress for Integrative Medicine (ECIM) (2009, 2011 to 2017).
Obtención y análisis de los datos
Per our published protocol (Wieland 2017), we conducted the following data collection and analysis in accordance with the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a).
Selección de los estudios
Two review authors independently screened the titles and abstracts of all retrieved references in Covidence (Covidence 2017). We retrieved the full‐text study reports for all citations that at least one review author considered potentially relevant. Two review authors independently screened the full‐text articles and identified studies for inclusion and identified and recorded reasons for excluded studies in the Characteristics of excluded studies. Any disagreements were resolved by discussion.
We collated multiple reports of the same study so that each study, rather than each report, was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram (Moher 2009).
Extracción y manejo de los datos
We used a standardised piloted data collection form in Microsoft Excel 2018 for Mac Version 16.20 and extracted the following study characteristics and outcome data.
-
Methods: study design.
-
Participants: number randomised, number with each type(s) of incontinence and how incontinence was diagnosed, if participants were pregnant or postpartum, how many were pregnant and how many were postpartum, severity and duration of urinary incontinence if reported, study participant mean age or age range, study location and setting, recruitment methods and inclusion and exclusion criteria.
-
Interventions: description of yoga intervention characteristics, dose and duration of yoga intervention, description of comparison intervention characteristics, adherence to the yoga and comparison interventions, description of any co‐interventions, length of follow‐up, number of withdrawals and reasons for withdrawal.
-
Outcomes: description of primary and secondary outcomes in the review that were reported in the trial, and listing of other outcomes collected in the trial.
-
Notes: funding for trial and notable conflicts of interest of trial authors.
-
'Risk of bias' assessment.
Two review authors independently extracted outcome data from the included studies into Microsoft Excel 2018 spreadsheets and compared the data to identify any discrepancies in data entry. Any disagreements were resolved by consensus. We noted in the Characteristics of included studies if a trial did not report outcome data in a usable way. We transferred all outcome data into Cochrane’s Review Manager 5 software (Review Manager 2014).
In addition to extracting data from included studies as described above, we planned to include an appendix of bibliographic detail of any identified economic studies. As such, we did not conduct a further review of potential economic studies.
Evaluación del riesgo de sesgo de los estudios incluidos
Two review authors (LSW, ZSL) independently assessed the risk of bias for each included trial using Cochrane's 'Risk of bias' tool (Higgins 2011a). Any disagreements were resolved by discussion. We assessed the risk of bias for the following domains: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment for each outcome (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias) and other bias (such as validity of outcome measure and baseline comparability).
We assessed each potential source of bias as either high, low, or unclear and provided a quotation from the study report together with a justification for our judgement in the 'Risk of bias’ tables. We summarised the judgements across different studies for each of the domains listed.
The participants and personnel in most yoga trials are not blinded. As the primary outcomes of this review depended upon the perception and reporting of the study participant, we have not included blinding of personnel, participants or outcome assessors in our dichotomising of trials into higher versus lower risk of bias. Instead, for our sensitivity analyses of the primary outcomes by higher versus lower risk of bias, we classified studies as having a relatively lower risk of bias if they had a low risk of bias for random allocation, allocation concealment and incomplete outcome assessment, and did not have a high risk of bias for selective outcome reporting or other bias (see Sensitivity analysis).
Medidas del efecto del tratamiento
We uploaded the outcome data for each study into the data tables in Review Manager 5 to calculate treatment effects (Review Manager 2014). We used the risk ratio (RR) for dichotomous outcomes related to benefit of treatment (e.g. cure). We used the absolute risk difference (RD) for adverse events. We used the mean difference (MD) for continuous outcomes reported on the same scale, and the standardised mean difference (SMD) for continuous outcomes measured on different scales in different trials included in the same meta‐analysis. We expressed the uncertainty with 95% confidence intervals (CIs) for all effect estimates.
If the included studies only reported effect estimates and their CIs, standard errors or exact P values, we uploaded these data into Review Manager 5 in order to apply the generic inverse variance method (Review Manager 2014). We ensured that higher scores for continuous outcomes had the same meaning for a given outcome and explained the direction to the reader. When we were unable to enter the results in either of the above ways, we described them in the Characteristics of included studies or entered the data into the Additional tables.
Cuestiones relativas a la unidad de análisis
Where appropriate, we planned to include the first period of cross‐over studies. We also planned to include cluster‐randomised studies if they were suitable according to the guidance in Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b).
Manejo de los datos faltantes
We contacted investigators or study sponsors in order to verify key study characteristics and to obtain missing numerical outcome data where possible. If numerical outcome data such as standard deviations (SDs) or correlation coefficients were missing, we attempted to calculate them from other available statistics, such as P values, according to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). If we were unable to obtain a full report even after contacting the study authors, we listed the study as 'awaiting classification'.
Evaluación de la heterogeneidad
We assessed clinical heterogeneity (i.e. differences in study populations, interventions and outcomes) between studies qualitatively. For studies that we judged to have sufficient clinical homogeneity to combine in a meta‐analysis, we planned to assess heterogeneity in three ways: visual examination of the forest plots; the Chi² test (P ≤ 0.10) for heterogeneity; and the I² statistic, which describes the per cent of the variability in the estimate that is due to clinical or methodological heterogeneity rather than to chance. We planned to consider the implications of the observed value of the I² statistic as follows:
-
0% to 40%: might not be important;
-
30% to 60%: may represent moderate heterogeneity;
-
50% to 90%: may represent substantial heterogeneity;
-
75% to 100%: considerable heterogeneity (Deeks 2011).
We planned to assess the importance of the value of the I² statistic in light of the range and direction of effects as observed from the forest plots and the strength of the evidence for heterogeneity based upon the Chi² test (Deeks 2011). We planned to seek and discuss plausible explanations for observed statistical heterogeneity. We planned to investigate causes of heterogeneity between trials, qualitatively assessing any differences between individual trials in the populations and interventions. We also planned to explore heterogeneity through the use of subgroup and sensitivity analyses.
Evaluación de los sesgos de notificación
We searched study registries of prospectively registered trials to identify completed, but not published, trials. We planned to use a funnel plot and Egger's test to assess the potential for publication bias in meta‐analyses with more than 10 trials (Egger 1997; Sterne 2011).
Síntesis de los datos
Where trials were clinically comparable (i.e. clinical comparability of population, intervention, comparison, outcome and timing of measurement), we planned to combine the outcome data from the individual trials in a meta‐analysis using Review Manager 5 (Review Manager 2014). We planned to analyse pregnant and postpartum women separately in call cases. However, for non‐pregnant, non‐postpartum populations, we planned to group together women with SUI, UUI, MUI and mixed or unclear urinary incontinence diagnoses in the primary analysis, and examine different types of urinary incontinence diagnoses using subgroup analyses (see Subgroup analysis and investigation of heterogeneity).
As yoga is a complex intervention with variations in practice components and implementation and we expected some between‐study variation due to these factors, we planned to use the random‐effects model for meta‐analysis.
When outcome data from individual trials were not sufficiently similar to be combined quantitatively, we planned to narratively describe the results from clinically comparable trials.
Análisis de subgrupos e investigación de la heterogeneidad
As the mechanisms of SUI and UUI are different, the effects of yoga may vary across types of urinary incontinence. We planned that if there were sufficient data, we would carry out subgroup analyses by type of urinary incontinence in the following groups:
-
SUI;
-
UUI;
-
MUI; and
-
a range of urinary incontinence diagnoses, where data are not reported separately by urinary incontinence subgroup.
If sufficient data become available, we also plan to conduct subgroup analyses of trials conducted in older (mean age 65 years or greater) versus younger populations, as populations from different age groups may vary in their ability to perform yoga. Among women who are pregnant or postpartum, we plan to perform subgroup analyses of trials conducted in women who are pregnant versus postpartum, as the natural history of incontinence is different in the two states. We also intend to carry out subgroup analyses by style (e.g. Iyengar yoga, Viniyoga, Yin yoga), dose and duration of yoga intervention to determine whether type of yoga, amount of yoga or duration of yoga modifies the effect of the yoga intervention.
Análisis de sensibilidad
When both endpoint and change data were available, we used endpoint data for our primary analysis and carried out a sensitivity analysis to check whether the results varied according to endpoint versus change data. In cases where study participants were lost to follow‐up and intention‐to‐treat analyses were conducted using imputation alongside available‐case analyses, we used the observed data for our primary analysis and performed a sensitivity analysis to check whether the results varied according to imputed versus available‐case data. In cases where both unadjusted and adjusted data were available, we used the unadjusted data for our primary analysis and performed a sensitivity analysis to check whether the results varied according to adjusted versus unadjusted data.
If sufficient data become available, we plan to assess the robustness of our conclusions by excluding studies that we judge to have a high risk of bias from our meta‐analyses for the primary outcomes.
'Summary of findings' tables
We created a 'Summary of findings' table using the GRADE criteria (Guyatt 2011a; Guyatt 2011b). We planned to prepare separate 'Summary of findings' tables for trials carried out with women who were pregnant or postpartum.
Two review authors (LSW and ZSL) independently undertook GRADE assessments and compared results. Consensus was reached through discussion when necessary. We justified all decisions to downgrade the certainty of the evidence using footnotes and made comments to aid readers’ understanding of the review.
We considered the following factors in our assessment of the certainty of the evidence.
-
Limitations in the study design and conduct (i.e. risk of bias).
-
Inconsistency of results.
-
Indirectness of evidence.
-
Imprecision.
-
Publication bias.
We downgraded the certainty of the evidence for a given outcome by one level according to the performance of the included studies against each of the five factors.
Results
Description of studies
Results of the search
The search produced a total of 42 titles and abstracts, from which 14 records were selected for full‐text review. Two trials in seven reports were eligible for inclusion in the review. The full report of one study for which we were able to obtain a trial register record and an unpublished abstract was not available, therefore we assessed this study as 'awaiting classification' as per our protocol (Huang 2018). We excluded five studies in five reports; the reasons for exclusion are provided in the Characteristics of excluded studies. The PRISMA flow chart in Figure 1 illustrates the flow of literature through the search and selection process.
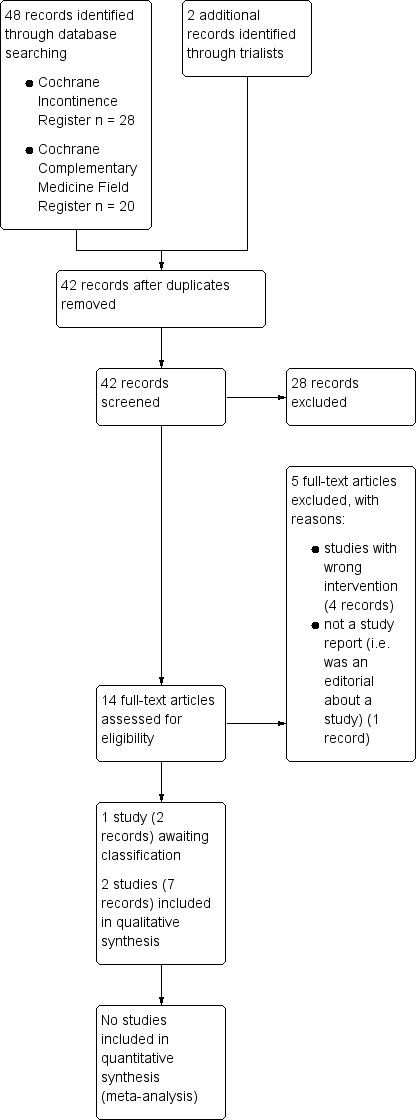
PRISMA study flow diagram.
Our search for economic studies produced a total of 608 titles and abstracts, from which none were selected for further assessment. The PRISMA flow chart in Figure 2 illustrates the flow of economic literature through the search and selection process. Economic studies are not considered further in this review.

Study flow diagram for economics studies.
Included studies
Both included trials were two‐arm parallel randomised controlled trials conducted in the USA (Baker 2014; Huang 2014a). The trials included a total of 49 women.
Sample characteristics
Baker 2014 included participants ranging in age from 22 to 79 years, with a median age of 58 years in the yoga group and 59 years in the comparison group. Huang 2014a required participants to be aged at least 40, resulting in a sample with a mean age of 61 years. Most participants in Baker 2014 were postmenopausal, while pregnancy during the past year was an exclusion criterion for Huang 2014a.
In Baker 2014, all participants had urge‐predominant urinary incontinence. In Huang 2014a, 63% of participants had urge‐predominant urinary incontinence and 37% of participants had stress‐predominant urinary incontinence. Neither trial specified how urinary incontinence was diagnosed.
Interventions and comparators
The comparisons to yoga differed in the two trials. In Baker 2014, yoga was an active control for mindfulness‐based stress reduction (MBSR), which was the intervention of interest. The yoga intervention was described as following the basic principles of yoga and focusing on asanas and relaxation. It did not include any postures or muscle contractions designed to treat incontinence. In Huang 2014a, which was a pilot study to determine the feasibility of a group‐based yoga therapy intervention for women with urinary incontinence, a specially designed yoga program based on Iyengar yoga was compared to a wait‐list control.
Outcomes
Both trials collected and reported information on improvement in incontinence, condition‐ or symptom‐specific quality of life, daily episodes of incontinence, and other measures of emotional and social impact of incontinence. Huang 2014a reported additional information on daily micturitions and adverse events. Baker 2014 reported all outcomes other than improvement in incontinence using medians and ranges, and these data were not extracted for analysis.
Further details about participants, interventions, comparators and outcomes are provided in the Characteristics of included studies.
Excluded studies
We excluded four trials in which yoga was not an intervention. We excluded an additional article because it was not a primary study report but rather an editorial on an included study (Huang 2014a). Reasons for exclusion of the five records are provided in the Characteristics of excluded studies.
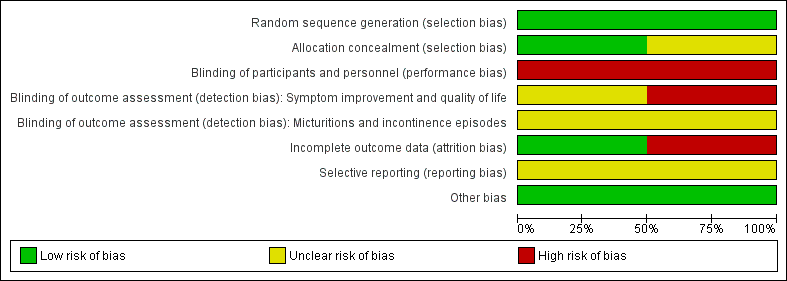
Risk of bias in included studies
Figure 3 and Figure 4 summarise the risk of bias of the included trials.
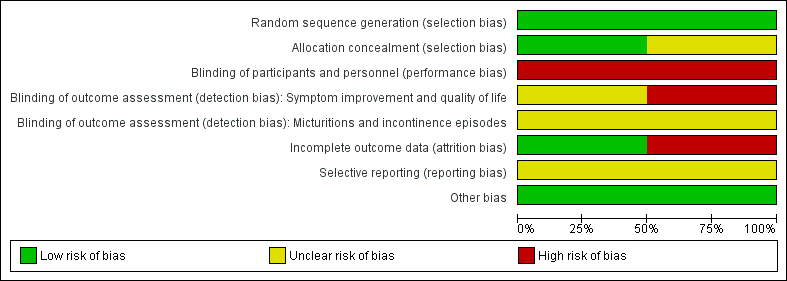
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We considered the risk of bias for random sequence generation to be low for one trial reporting that random sequence generation was carried out by computer (Huang 2014a). However, allocation concealment was not described, therefore we considered the risk of bias for allocation concealment to be unclear. In the other trial, the shuffling of 'security tint' envelopes containing the group assignment was used to generate the random sequence (Baker 2014). We therefore considered the risk of bias for both random sequence generation and allocation concealment to be low, given the processes followed.
Blinding
There was no indication in either study that participants and personnel were unaware of the intervention assignments and, given the nature of yoga interventions, we considered blinding to be highly unlikely. We therefore considered the risk of performance bias to be high in both studies. Because participants were not blinded and the control condition in Huang 2014a was a waiting list, we considered outcomes that relied upon participant judgement (e.g. overall improvement) to be at high risk of detection bias. We considered more objective outcomes that relied upon participant identification of events (e.g. diary recording of incontinence episodes) to be at unclear risk of detection bias, despite the use of masked assessors to extract diary data. In Baker 2014, both interventions were active and, because it is possible that the participants were unaware whether MBSR or yoga was the intervention of interest, we considered that the risk of detection bias was unclear for all outcomes.
Incomplete outcome data
In Baker 2014, there were high rates of loss to follow‐up and, as the rates of loss to follow‐up differed between groups and reasons for loss to follow‐up were not described, we considered the study to be at high risk of attrition bias. In Huang 2014a, only one participant was lost to follow‐up, and we considered the study to be at low risk of attrition bias.
Selective reporting
Both included studies were registered at ClinicalTrials.gov and reported primary outcomes consistent with the trial registration, but also reported secondary outcomes that were not included in the trial registration. We considered the risk of reporting bias to be unclear for both trials.
Other potential sources of bias
We identified no other potential sources of bias for either trial.
Effects of interventions
See: Summary of findings for the main comparison Yoga versus no specific active intervention; Summary of findings 2 Yoga versus an active intervention
The two included trials compared yoga to a wait‐list condition (one trial with 19 women) and to a mindfulness‐based stress reduction (MBSR) intervention (one trial with 30 women). Neither trial included information on the number of women reporting continence, but both trials reported data on the number of women who reported improvement in urinary incontinence. Both trials also reported condition‐ or symptom‐specific quality of life outcomes. Both trials reported on the change in number of episodes of incontinence, but neither trial reported data on clinical observations of clinical or anatomical functioning. The following results were reported.
Yoga versus no specific active intervention
One small trial (n = 19) compared the effects of a yoga intervention to a waiting list in women with urge‐predominant urinary incontinence (n = 12) or stress‐predominant urinary incontinence (n = 7) (Huang 2014a). All outcomes were measured at six weeks after randomisation, and all evidence was assessed as of very low certainty due to the very small sample size and lack of blinding of study participants, personnel and outcome assessors. See summary of findings Table for the main comparison for a summary of the main results.
Primary outcome measures
Number of women who report they are cured (they no longer experience incontinence)
Not reported.
Number of women who report cure or improvement of urinary incontinence
Women were not asked directly whether their incontinence had been cured or improved but were asked whether they were satisfied with the change in urine leakage, which is an indirect measure of improvement of urinary incontinence. There was very low‐certainty evidence that women in the yoga group were six times more likely than women in the wait‐list group to be at least moderately satisfied with the change in their urine leakage (risk ratio (RR) 6.33, 95% confidence interval (CI) 1.44 to 27.88; Analysis 1.1).
Urinary incontinence condition‐ or symptom‐specific quality of life
There was very low‐certainty evidence of no difference between the yoga and wait‐list groups in quality of life as measured on the Incontinence Impact Questionnaire Short Form (IIQ‐7) (mean difference (MD) 1.74, 95% CI ‐33.02 to 36.50; Analysis 1.2). At baseline, the yoga group had lower mean scores on the IIQ‐7 and, after adjusting for the baseline scores, the difference in changes between groups was in the opposite direction favouring the wait‐list group, but there was still no difference between groups (MD ‐27.70, 95% CI ‐66.80 to 11.40; Analysis 1.3).
Secondary outcome measures
Number of micturitions (daily)
There was very low‐certainty evidence of little or no difference in the frequency of total daily micturitions between groups (MD ‐0.77, 95% CI ‐2.13 to 0.59; Analysis 1.4). At baseline, the yoga group had a slightly higher mean number of total daily micturitions compared to the wait‐list group and, after the analysis adjusted for baseline micturitions, the difference in changes between groups was further reduced (MD ‐0.12, 95% CI ‐1.73 to 1.49; Analysis 1.5).
Number of episodes of incontinence (daily)
There was very low‐certainty evidence of a greater reduction in the yoga group compared to the wait‐list group in the frequency of total daily episodes of incontinence (MD ‐1.57, 95% CI ‐2.83 to ‐0.31; Analysis 1.6). After adjusting for baseline outcome levels, the difference between groups was consistent with the unadjusted analysis (MD ‐1.40, 95% CI ‐2.79 to ‐0.01; Analysis 1.7).
Urine loss as measured with a pad or paper towel weight test
Not reported.
Symptoms as reported by study participants on any condition‐specific scale
Not reported.
Clinical assessment of presence of incontinence
Not reported.
Measurement of pelvic floor muscle function
Not reported.
Quality of life measured on a scale that is not condition‐ or symptom‐specific
Not reported.
Depression, anxiety or distress
Not reported.
Other measures of emotional and social impact of the disorder
There was very low‐certainty evidence of a greater reduction in the yoga group compared to the wait‐list group in the subjective bothersomeness of incontinence symptoms as measured on the Urogenital Distress Inventory 6 (UDI‐6) (MD ‐0.90, 95% CI ‐1.46 to ‐0.34; Analysis 1.8). After adjusting for baseline outcome levels, the difference between groups was nearly identical to the unadjusted analysis (MD ‐0.90, 95% ‐1.40 to ‐0.40; Analysis 1.9).
Adverse effects
There was very low‐certainty of no evidence of a difference between yoga and wait‐list groups in the number of women who experienced one or more adverse events (risk difference (RD) 0.00, 95% CI ‐0.38 to 0.38; Analysis 1.10).
Yoga versus an active intervention
One small trial (n = 30) compared the effects of a yoga intervention to a mindfulness‐based stress reduction (MBSR) intervention in women with urgency urinary incontinence (Baker 2014). The yoga intervention was conceived as an active control for the MBSR intervention, which was the treatment of interest. The yoga intervention did not include any postures, techniques or instructions intended to improve bladder control or reduce incontinence. All outcomes were measured at eight weeks, six months and one year and were reported in the publication as medians and ranges, likely due to highly skewed data and a small sample size, with the exception of the number of women reporting improvement in incontinence. We extracted data on improvement in incontinence into Review Manager 5; all other data reported below are as presented in the study publication. We assessed all evidence as of very low certainty due to the very small sample size, lack of blinding (i.e. performance bias), attrition bias and indirectness (i.e. the yoga intervention was not an intervention designed to improve incontinence). See summary of findings Table 2 for a summary of the main results.
Primary outcome measures
Number of women who report they are cured (they no longer experience incontinence)
Not reported.
Number of women who report cure or improvement of urinary incontinence
There was very low‐certainty evidence of no difference between women in the MBSR group and women in the yoga group in improvement in incontinence, as measured on the Patient Global Impression of Improvement (PGI‐I) at eight weeks (RR 0.09, 95% CI 0.01 to 1.43; Analysis 2.1); six months (RR 0.20, 95% CI 0.03 to 1.42; Analysis 2.2); and one year (RR 0.22, 95% CI 0.03 to 1.53; Analysis 2.3).
Urinary incontinence condition‐ or symptom‐specific quality of life
There was very low‐certainty evidence that women in the MBSR group had greater improvement in urinary incontinence‐specific quality of life compared to women in the yoga group, as measured on the Overactive Bladder Health‐Related Quality of Life (OAB‐HRQL) scale. The median per cent improvement at eight weeks was 8.70 in the yoga group (interquartile range (IQR) 1.75 to 20.59, n = 11) and 29.27 in the MBSR group (IQR 8.11 to 93.33, n = 13; reported P value = 0.03). The median per cent improvement at six months was 8.0 in the yoga group (IQR 5.17 to 17.39, n = 10) and 43.90 in the MBSR group (IQR 2.92 to 84.62, n = 10; reported P value = 0.38). The median per cent improvement at one year was 13.04 in the yoga group (IQR 10.34 to 20.75, n = 9) and 36.09 in the MBSR group (IQR 4.55 to 79.76, n = 12; reported P value = 0.52). The trialists carried out intention‐to‐treat (ITT) analyses in which baseline values were carried forward for missing participants and results of the ITT analyses were consistent with the results of the analyses of women who completed the study.
Secondary outcome measures
Number of micturitions (daily)
Not reported.
Number of episodes of incontinence (daily)
There was very low‐certainty evidence that women in the MBSR group had a greater reduction in number of daily urinary incontinence episodes compared to women in the yoga group at each outcome assessment time. The median per cent improvement at eight weeks was ‐33.33 in the yoga group (IQR ‐50.00 to 16.67, n = 11) and ‐60 in the MBSR group (IQR ‐88.89 to ‐50.00, n = 13; reported P value = 0.03). The median per cent improvement at six months was ‐22.62 in the yoga group (IQR ‐50.00 to ‐16.67, n = 10) and ‐71.43 in the MBSR group (IQR ‐100.00 to ‐40.00, n = 10; reported P value = 0.01). The median per cent improvement at one year was ‐41.67 in the yoga group (IQR ‐66.67 to ‐28.57, n = 9) and ‐69.11 in the MBSR group (IQR ‐91.43 to ‐49.17, n = 12; reported P value = 0.04). The trialists carried out ITT analyses in which baseline values were carried forward for missing participants and the results of the ITT analyses were consistent with the results of the analyses of women who completed the study.
Urine loss as measured with a pad or paper towel weight test
Not reported.
Symptoms as reported by study participants on any condition‐specific scale
Not reported.
Clinical assessment of presence of incontinence
Not reported.
Measurement of pelvic floor muscle function
Not reported.
Quality of life measured on a scale that is not condition‐ or symptom‐specific
Not reported.
Depression, anxiety or distress
Not reported.
Other measures of emotional and social impact of the disorder
There was very low‐certainty evidence that women in the MBSR group had greater reductions in bothersomeness compared to women in the yoga group, as measured on the Overactive Bladder Symptom and Quality of Life‐Short Form (OABq‐SF). The score from this six‐item scale is transformed into a 0‐to‐100 scale in which higher scores reflect greater bother and impact. The median per cent change at eight weeks was ‐25.0 in the yoga group (IQR ‐35 to 20, n = 11) and ‐55.6 in the MBSR group (IQR ‐50 to ‐87, n = 13; reported P value = 0.005). The median per cent improvement at six months was ‐25 in the yoga group (IQR ‐30 to ‐11.67, n = 10) and ‐54.13 in the MBSR group (IQR ‐66.67 to 0, n = 10; reported P value = 0.13). The median per cent improvement at one year was ‐35.29 in the yoga group (IQR ‐50 to ‐8.33, n = 9) and ‐73.91 in the MBSR group (IQR ‐80 to ‐9.52, n = 12; reported P value = 0.14). The trialists carried out ITT analyses in which baseline values were carried forward for missing participants and the results of the ITT analyses were consistent with the results of the analyses of women who completed the study.
Adverse effects
Not reported.
Yoga plus an intervention versus the same intervention without yoga
We did not find any eligible trials for this comparison.
Sensitivity analyses
We planned to assess the robustness of our conclusions by excluding studies that we judged to have a high risk of bias from our meta‐analyses for the primary outcomes. However, only a single study was included for each comparison.
For one included study, both available‐case and imputed data were reported but we were unable to extract data from any analyses into Review Manager 5. We have reported both available‐case and imputed analysis information from the study publication.
For the other study, we extracted information for analyses adjusted for outcomes at baseline and included this sensitivity analysis in the reporting of results from the study.
Discusión
Resumen de los resultados principales
Se consideraron para la inclusión en esta revisión dos estudios pequeños a corto plazo que analizaron el yoga en mujeres con incontinencia. Un estudio comparó seis semanas de yoga con una lista de espera en mujeres con incontinencia urinaria de urgencia o esfuerzo (Huang 2014a), mientras el otro estudio comparó ocho semanas de REBAP con una intervención de yoga en mujeres con incontinencia urinaria de urgencia (Baker 2014). Por lo general, las comparaciones entre el yoga y una lista de espera favorecieron la intervención con yoga, mientras las comparaciones entre la REBAP y el yoga favorecieron la intervención de REBAP. Sin embargo, ambos estudios fueron muy pequeños y tenían problemas relacionados con el riesgo de sesgo. No se encontraron ensayos que compararan el yoga con más una intervención versus la misma intervención sin yoga. En consecuencia, la información no fue suficiente para establecer conclusiones acerca de si el yoga es efectivo para el tratamiento de la incontinencia urinaria de urgencia o de esfuerzo en mujeres. No se identificó ninguna evaluación económica potencialmente relevante.
Compleción y aplicabilidad general de las pruebas
Los estudios incluidos incorporaron mujeres con una frecuencia mínima de incontinencia urinaria. Un estudio incorporó a mujeres con incontinencia urinaria de urgencia (Baker 2014). Huang 2014a incluyó a mujeres con incontinencia urinaria de urgencia o esfuerzo, aunque la mayoría presentaba incontinencia de urgencia. El estudio que comparó el yoga con la REBAP estaba diseñado para analizar los efectos de la REBAP, y el yoga era un brazo de control activo que no estaba destinado a mejorar la incontinencia. Ambos estudios proporcionaron intervenciones a corto plazo de ocho semanas o menos, y aunque un estudio siguió a los participantes un año después de la asignación al azar (Baker 2014), hubo desgaste significativo en ambos grupos del estudio en todas las evaluaciones realizadas. Hay evidencia muy limitada sobre la efectividad a corto o largo plazo del yoga en comparación con ninguna intervención o la REBAP, y una falta de evidencia en cuanto al yoga comparado con otras intervenciones activas o como complemento de las intervenciones activas.
Calidad de la evidencia
Limitaciones de los estudios (riesgo de sesgo)
No hubo preocupaciones importantes acerca de la asignación al azar, la ocultación de la asignación ni el informe selectivo. Ambos estudios fueron no ocultados y por lo tanto eran sensibles al sesgo de rendimiento. En Huang 2014a, todos los resultados fueron autoevaluados y, por lo tanto, se consideró que este estudio presentaba riesgo de sesgo de detección a causa de la evaluación de resultado por participantes no cegados. Aunque Baker 2014 también dependió de los resultados evaluados por el participante, el estudio incluyó dos grupos de intervención activa, que pueden haber moderado el sesgo que se origina de la evaluación de resultados por participantes no cegados. Sin embargo, Baker 2014 tuvo altos niveles de desgaste, que varió entre los grupos de estudio, en cada momento de evaluación de resultados. Se disminuyó la certeza de la evidencia de Huang 2014a una vez por el riesgo de sesgo de rendimiento y una vez por el riesgo de sesgo de detección, y la de Baker 2014 una vez por el riesgo de sesgo de rendimiento y una vez por el riesgo de sesgo de desgaste.
Consistencia
Como había un solo estudio para cada comparación, no pudo evaluarse la consistencia.
Falta de direccionalidad
No hubo falta de direccionalidad en Huang 2014a. El estudio que compara la REBAP y el yoga incluía el yoga como un grupo de control "activo" para la REBAP, que era la intervención de interés (Baker 2014). La intervención con yoga fue un programa de yoga restaurativo que no estaba diseñado para mejorar la incontinencia. Por lo tanto, se disminuyó la certeza de la evidencia para cada resultado de Baker 2014 por la falta de direccionalidad.
Imprecisión
Como los estudios fueron muy pequeños, se disminuyó una vez la certeza de la evidencia de ambos estudios por la imprecisión.
Sesgo de publicación
Se consultó con expertos, se realizaron búsquedas manuales en actas de congresos y en registros de ensayos, y no se identificaron estudios no publicados adicionales además de un ensayo recientemente completado, cuya inclusión se evaluará cuando los autores publiquen la totalidad de resultados. No se disminuyó la certeza de la evidencia por el sesgo de publicación.
Se disminuyó a muy baja la certeza de la evidencia para cada resultado en la comparación del yoga con la lista de espera (Huang 2014a). Se disminuyó la evidencia en un nivel debido al riesgo de sesgo de rendimiento, un nivel por el riesgo de sesgo de detección y un nivel debido a la imprecisión. Se disminuyó a muy baja la certeza de la evidencia para cada resultado en la comparación del yoga con la REBAP (Baker 2014). Se disminuyó la evidencia en un nivel debido al riesgo de sesgo de realización, un nivel por el riesgo de sesgo de desgaste, un nivel debido a la falta de direccionalidad y un nivel debido a la imprecisión.
Sesgos potenciales en el proceso de revisión
El Registro Especializado Cochrane de Incontinencia y el Registro Especializado Cochrane del Área de Medicina Complementaria se basan en fuentes múltiples de ensayos y se cree que en las búsquedas de estos registros y en las búsquedas de los registros de ensayos, se identificaron todos los ensayos relevantes existentes. Sin embargo, no fue posible descartar que quizás se hayan identificado más ensayos en las búsquedas de las bases de datos especializadas adicionales.
Acuerdos y desacuerdos con otros estudios o revisiones
No hay otras revisiones sistemáticas que se centren en el yoga para la incontinencia en mujeres. Se encontró una revisión sistemática de tratamientos no quirúrgicos para la incontinencia en mujeres que mencionó el yoga y se identificaron los dos mismos ensayos incluidos en esta revisión (AHRQ 2018). La revisión agrupó el yoga con otras intervenciones como la educación, la biorretroalimentación, la electroacupuntura y la pérdida de peso en la categoría de intervenciones conductuales y no informó de conclusiones específicas para el yoga.

PRISMA study flow diagram.

Study flow diagram for economics studies.
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Yoga versus no specific active intervention, Outcome 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 6 weeks).

Comparison 1 Yoga versus no specific active intervention, Outcome 2 Urinary incontinence condition‐ or symptom‐specific quality of life (at short term ‐ 6 weeks).
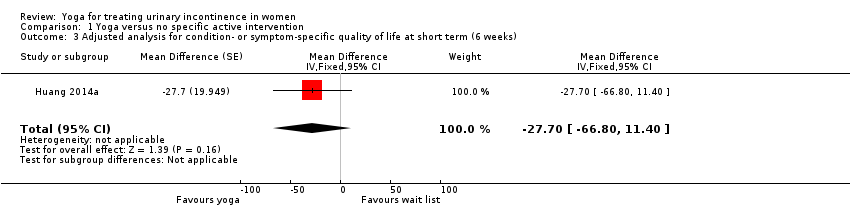
Comparison 1 Yoga versus no specific active intervention, Outcome 3 Adjusted analysis for condition‐ or symptom‐specific quality of life at short term (6 weeks).

Comparison 1 Yoga versus no specific active intervention, Outcome 4 Number of micturitions (daily) (at short term ‐ 6 weeks).
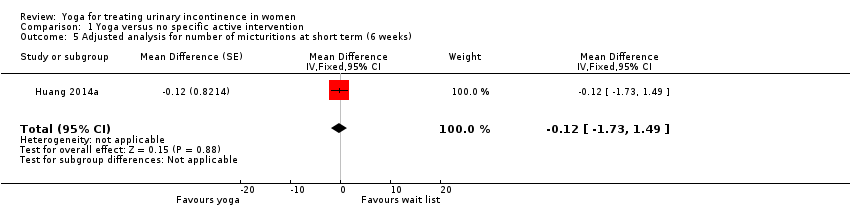
Comparison 1 Yoga versus no specific active intervention, Outcome 5 Adjusted analysis for number of micturitions at short term (6 weeks).

Comparison 1 Yoga versus no specific active intervention, Outcome 6 Number of episodes of incontinence (daily) (at short term ‐ 6 weeks).
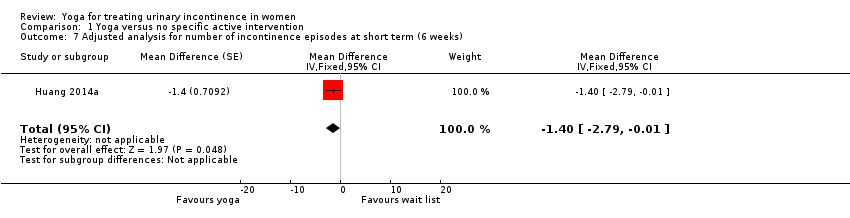
Comparison 1 Yoga versus no specific active intervention, Outcome 7 Adjusted analysis for number of incontinence episodes at short term (6 weeks).
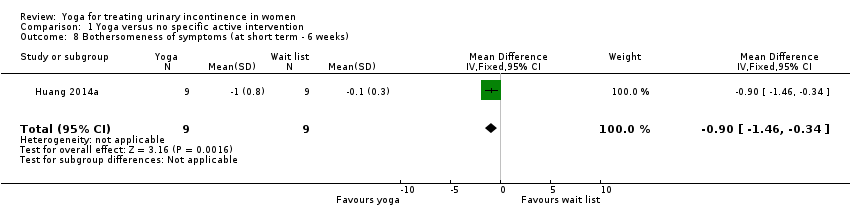
Comparison 1 Yoga versus no specific active intervention, Outcome 8 Bothersomeness of symptoms (at short term ‐ 6 weeks).

Comparison 1 Yoga versus no specific active intervention, Outcome 9 Adjusted analysis for bothersomeness of symptoms at short term (6 weeks).

Comparison 1 Yoga versus no specific active intervention, Outcome 10 Adverse effects (at short term ‐ 6 weeks).
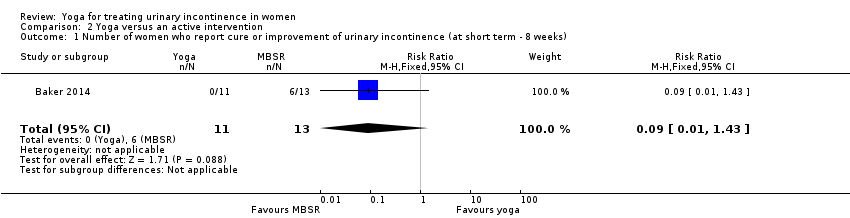
Comparison 2 Yoga versus an active intervention, Outcome 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 8 weeks).
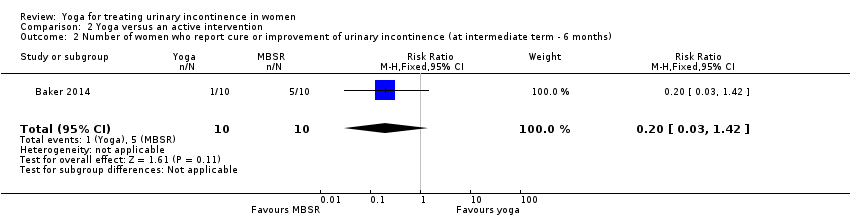
Comparison 2 Yoga versus an active intervention, Outcome 2 Number of women who report cure or improvement of urinary incontinence (at intermediate term ‐ 6 months).
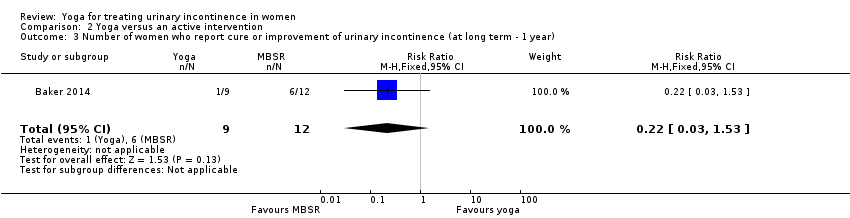
Comparison 2 Yoga versus an active intervention, Outcome 3 Number of women who report cure or improvement of urinary incontinence (at long term ‐ 1 year).
| Yoga compared with wait‐list for urinary incontinence in women | ||||||
| Patient or population: women with either stress‐predominant or urge‐predominant urinary incontinence Settings: community Intervention: yoga Comparison: wait‐list | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Wait‐list | Yoga | |||||
| Number of women who report they are cured (they no longer experience urinary incontinence) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
| Number of women who report cure or improvement of urinary incontinence at short term (six weeks) | 111 per 1000 | 703 per 1000 | RR 6.33 (1.44 to 27.88) | 18 | ⊕⊝⊝⊝ | Number of women who reported satisfaction with change in urine leakage. |
| Urinary incontinence condition‐ or symptom‐specific quality of life at short term (6 weeks) Measured by Incontinence Impact Questionnaire Short Form (IIQ‐7) (lower = better) | The mean change in the control group was a decrease of 31 units. | The mean change in the intervention group was 1.74 units higher (33.02 units lower to 36.50 units higher). | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Number of micturitions (daily) at short term (6 weeks) | The mean change in the control group was a decrease of 0.13 micturitions. | The mean change in the intervention group was | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Number of episodes of incontinence (daily) at short term (6 weeks) | The mean change in the control group was a decrease of 0.27 episodes. | The mean change in the intervention group was | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Bothersomeness of symptoms at short term (6 weeks) Measured by Urogenital Distress Inventory 6 (UDI‐6) (lower = better) | The mean change in the control group was a decrease of 0.1 units. | The mean change in the intervention group was 0.90 units lower (0.34 to 1.46 lower). | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Adverse effects at short term (6 weeks) | 222 per 1000 | 222 per 1000 | RD 0% (‐38% to 38%) | 18 | ⊕⊝⊝⊝ | 2 women in each group reported an adverse effect. However, there were 7 adverse effects overall and the distribution of adverse effects between groups is not reported. None of the adverse effects were considered to be potentially related to the study and none were serious. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded two levels for risk of bias because there was no blinding of participants or providers (risk of performance bias), and outcome was self assessed and self recorded by participants (risk of detection bias). | ||||||
| Yoga compared with mindfulness‐based stress reduction (MBSR) for urinary incontinence in women | ||||||
| Patient or population: women with urge‐predominant urinary incontinence Settings: community Intervention: yoga Comparison: mindfulness‐based stress reduction (MBSR) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| MBSR | Yoga | |||||
| Number of women who report they are cured (they no longer experience urinary incontinence) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
| Number of women who report cure or improvement of urinary incontinence at short term (8 weeks) | 461 per 1000 | 42 per 1000 | RR 0.09 (0.01 to 1.43) | 24 | ⊕⊝⊝⊝ | |
| Urinary incontinence condition‐ or symptom‐specific quality of life at short term (8 weeks) Measured by the Overactive Bladder Health‐Related Quality of Life (OAB‐HRQL) scale (higher per cent improvement = better) | ‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent improvement at 8 weeks was 8.70 (IQR 1.75 to 20.59) in the yoga group (n = 11) and 29.27 (IQR 8.11 to 93.33) in the MBSR group (n = 13) (reported P value = 0.03). |
| Number of micturitions (daily) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
| Number of episodes of incontinence (daily) at short term (8 weeks) | ‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent improvement at 8 weeks was ‐33.33 (IQR ‐50.00 to 16.67) in the yoga group (n = 11) and ‐60 (IQR ‐88.89 to ‐50.00) in the MBSR group (n = 13) (reported P value = 0.03). |
| Bothersomeness of symptoms at short term (6 weeks) Measured by the Overactive Bladder Symptom and Quality of Life‐Short Form (OABq‐SF) (lower = better) | ‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent change at 8 weeks was ‐25.0 (IQR ‐35 to 20) in the yoga group (n = 11) and ‐55.6 (IQR ‐50 to ‐87) in the MBSR group (n = 13) (reported P value = 0.005). |
| Adverse effects | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report on adverse effects. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded two levels for risk of bias because there was no blinding of participants or providers (risk of performance bias), and there was a high percentage of loss to follow‐up that was unbalanced across study arms (risk of attrition bias). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.33 [1.44, 27.88] |
| 2 Urinary incontinence condition‐ or symptom‐specific quality of life (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 1.74 [‐33.02, 36.50] |
| 3 Adjusted analysis for condition‐ or symptom‐specific quality of life at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐27.7 [‐66.80, 11.40] | |
| 4 Number of micturitions (daily) (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐0.77 [‐2.13, 0.59] |
| 5 Adjusted analysis for number of micturitions at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐0.12 [‐1.73, 1.49] | |
| 6 Number of episodes of incontinence (daily) (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐1.57 [‐2.83, ‐0.31] |
| 7 Adjusted analysis for number of incontinence episodes at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐1.4 [‐2.79, ‐0.01] | |
| 8 Bothersomeness of symptoms (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.46, ‐0.34] |
| 9 Adjusted analysis for bothersomeness of symptoms at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐0.9 [‐1.40, ‐0.40] | |
| 10 Adverse effects (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.38, 0.38] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 8 weeks) Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.43] |
| 2 Number of women who report cure or improvement of urinary incontinence (at intermediate term ‐ 6 months) Show forest plot | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.03, 1.42] |
| 3 Number of women who report cure or improvement of urinary incontinence (at long term ‐ 1 year) Show forest plot | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.03, 1.53] |

