Yoga para el tratamiento de la incontinencia urinaria en mujeres
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Design: parallel randomised controlled trial Country: USA Setting: study run through university but location of intervention delivery (e.g. clinic, community yoga studio) not specified | |
| Participants | 30 women with urge‐predominant urinary incontinence Types of incontinence: all women had urge‐predominant UI Diagnostic criteria for incontinence: not specified Severity and duration of incontinence: at baseline, the 3‐day average number of UI episodes for yoga participants was median 2.67 (range 1.67 to 6.33) and for MBSR participants was median 3.00 (1.67 to 9.33) Age: yoga median age 58 (range 22 to 79) years; MBSR median age 59 (range 34 to 74) years Pregnant/postpartum/menopausal status: "most were postmenopausal" Weight: BMI range 20.34 to 36.15 kg/m²; yoga median 25.82 (range 20.90 to 36.15) kg/m²; MBSR median 26.15 (range 20.34 to 33.22) kg/m² | |
| Interventions | Yoga group: 8 weekly yoga classes following "basic principles of yoga" and focusing on physical poses and relaxation. "Information was given on restorative yoga that emphasized the use of gravity, props, and floor poses for muscle relaxation. No education was given on breathing techniques in this yoga control program. Class time was also spent on education about the 7 chakras, self‐massage, and essential oils and how they can also assist in muscle relaxation." Home practice: not described Mindfulness‐based stress reduction (MBSR) group: 8 weekly group meetings following the traditional protocol of the Center for Mindfulness at the University of Massachusetts Medical Center. "The 8‐week MBSR program is a structured program that teaches participants a variety of meditation practices, mindful‐yoga, walking meditation, and discussions on the relationship between stress, illness, and health." Teacher(s): the classes were taught by a licensed occupational therapist with teacher training in mindfulness‐based therapy Home practice: women were given 'A Mindfulness‐Based Stress Reduction Workbook' and 15‐ to 30‐minute tapes to listen to. Women were asked to record instances of formal and informal techniques used in home practice sessions. "On average, the participants did a structured practice 5 times/wk (range, <1‐15.4 times/wk) and unstructured practice 9.7 times/wk (range, <1‐22 times/wk)." Adherence to yoga and comparison interventions: 11/15 (73%) yoga participants and 13/15 (87%) MBSR participants completed at least 5 of 8 sessions Common interventions: women were asked not to seek any other incontinence treatment while participating in the study. No women received any of the usual treatments of UUI, including bladder education, fluid management, or pelvic floor muscle exercises. None of the group sessions focused on bladder control. Number of withdrawals, with reasons: loss to follow‐up in the yoga group was 4/15 (27%) at 8 weeks, 5/15 (33.3%) at 6 months and 6/15 (40%) at 1 year. Loss to follow‐up in the MBSR group was 2/15 (13%) at 8 weeks, 5/15 (33.3%) at 6 months, and 3/15 (20%) at 1 year. It was not reported whether the women who did not complete follow‐up included withdrawals from treatment. Reasons for loss to follow‐up were not reported. | |
| Outcomes | Participant report of continence or improvement. Patient Global Impression of Improvement (PGI‐I). Women self reported their overall impression of improvement, and the outcome was dichotomised as much better or very much better versus other responses. Information reported at 8 weeks, 6 months and 1 year. Condition‐ or symptom‐specific quality of life. Overactive Bladder Health‐Related Quality of Life (OAB‐HRQL). The OAB‐HRQL score is obtained from summing the 13 items on the HRQL subscales of the Overactive Bladder Symptom and Health‐Related Quality of Life Questionnaire (OAB‐q). This score is transformed to a 0‐to‐100 scale in which higher scores reflect better quality of life. Median per cent change and IQR are reported at 8 weeks, 6 months and 1 year. Quantification of symptoms: number of incontinence episodes. The 3‐day average of incontinence episodes was collected from a diary. Median per cent change and IQR are reported at 8 weeks, 6 months and 1 year. Other measures of social or emotional impact of incontinence. Bothersomeness, as measured on the Overactive Bladder Symptom and Quality of Life‐Short Form (OABq‐SF). The score from this 6‐item scale is transformed to a 0‐to‐100 scale in which higher scores reflect greater bother and impact. Median per cent change and IQR are reported at 8 weeks, 6 months and 1 year. Other outcomes collected: urge incontinence episodes, daytime voids, nighttime voids and pad use | |
| Notes | Adverse events: no discussion of safety or adverse events | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was carried out by shuffling 'security tint' envelopes; the Cochrane Handbook for Systematic Reviews of Interventions indicates that shuffling envelopes corresponds to a low risk of bias for sequence generation. "Randomization was completed by block randomization at each of the 3 periods to maintain an equal number in each group. When an accurate count was obtained of women who signed the consent for participation in a group session, group assignments were placed in security envelopes and shuffled. Subjects were then allowed to pick an envelope. The envelope was opened in front of the research personnel and was noted on the randomization key along with the subjects’ study number. This randomization key was then placed in a sealed envelope. The randomization key was given to the data manager and was noted as either group 1 or group 2 on the data spread sheet. The statistician was given the randomization key." |
| Allocation concealment (selection bias) | Low risk | "When an accurate count was obtained of women who signed the consent for participation in a group session, group assignments were placed in security envelopes and shuffled. Subjects were then allowed to pick an envelope." |
| Blinding of participants and personnel (performance bias) | High risk | All participants and personnel were aware of the interventions being delivered. Study personnel may have been aware that MBSR was the intervention of interest and yoga considered an active control condition. |
| Blinding of outcome assessment (detection bias) | Unclear risk | All outcomes were assessed by the participants themselves, who were not blinded to the interventions. However, since both interventions were active, it is unclear to what extent this may have biased outcome assessment. |
| Blinding of outcome assessment (detection bias) | Unclear risk | All outcomes were assessed by the participants themselves through diary entries, and the participants were not blinded to the interventions. However, since both interventions were active, it is unclear to what extent this may have biased outcome assessment. |
| Incomplete outcome data (attrition bias) | High risk | There were high rates of loss to follow‐up, and rates differed between groups. Loss to follow‐up in the yoga group was 4/15 (27%) at 8 weeks, 5/15 (33.3%) at 6 months, and 6/15 (40%) at 1 year. Loss to follow‐up in the MBSR group was 2/15 (13%) at 8 weeks, 5/15 (33.3%) at 6 months, and 3/15 (20%) at 1 year. Reasons for loss to follow‐up are not described. |
| Selective reporting (reporting bias) | Unclear risk | Study was registered and the primary and secondary outcomes from the trial registration are reported. However, only 2 of the secondary outcomes reported in the article are listed in the protocol. |
| Other bias | Low risk | Groups were comparable on baseline characteristics and the study appeared to be free of conflicts of interest related to funding. |
| Methods | Design: parallel randomised controlled trial Country: USA Setting: study run through university but location of intervention delivery (e.g. clinic, community yoga studio) not specified | |
| Participants | 19 women with either stress or urgency urinary incontinence Types of incontinence: urgency‐predominant: all 12/19 (63%); yoga 6/10 (60%); control 6/9 (67%). Stress‐predominant: all 7/19 (37%); yoga 4/10 (40%); control 3/9 (33%). Diagnostic criteria for incontinence: not specified Severity and duration of incontinence: total incontinence episodes/day (based on 7‐day voiding diary) at baseline: yoga mean (SD) 2.77 (1.3); control mean (SD) 2.16 (1.2). Duration of incontinence not specified, but duration of 3 months or longer was an inclusion criterion. Age: yoga mean (SD) age 60.5 (8.4) years; control mean (SD) age 62.4 (8.3) years. Pregnant/postpartum/menopausal status: pregnancy in the last year was an exclusion criterion; menopausal status was not reported Weight: yoga BMI mean (SD) 24.7 (2.7) kg/m²; control BMI mean (SD) 25.8 (3.8) kg/m² | |
| Interventions | Yoga group: 90‐minute Iyengar yoga classes were provided twice per week for 6 weeks. The class focus was on physical poses and relaxation. "Tadasana (mountain Home practice: "Participants were also instructed to practice yoga at home for at least 1 additional hour per week and to record the dates and duration of practice in a home yoga diary. Participants were given a limited set of yoga props (mat, belt, and block) to take home and a manual with written descriptions and pictures depicting each of the key yoga postures featured in the classes. Tips on how to practice each posture safely and comfortably and how to adapt each posture to improve incontinence and pelvic floor function were also provided in the manual." Wait‐list control group: "Women randomized to the control group did not attend group yoga therapy classes and were instructed to avoid outside yoga instruction for 6 weeks. At the end of the 6‐week study, control group participants were given a $180 gift certificate for yoga classes at a local yoga studio and a limited set of home yoga props (block, mat, and strap) to take home." Adherence to yoga and comparison interventions: 9 (100%) women attended at least 1 group class, and 6/9 (67%) attended all group classes. 9 women (100%) completed at least 1 hour/week of home practice (self reported). Common interventions: women were given a pamphlet with standard education and behavioural management strategies for incontinence Number of withdrawals, with reasons: "After the randomization, but before the start of the yoga therapy program, 1 yoga therapy participant dropped out of the study citing worsened health." No other women in either group withdrew or were lost to follow‐up. | |
| Outcomes | Participant report of continence or improvement. Overall satisfaction with change in urine leakage was measured on a 5‐point Likert scale, ranging from ‘‘very unsatisfied’’ to ‘‘very satisfied’’, dichotomised as "moderately satisfied" or more versus less than "moderately satisfied". Assessed at 6 weeks. Condition‐ or symptom‐specific quality of life. “Incontinence Impact Questionnaire Short Form (IIQ‐7), a 7‐item measure of the impact of incontinence on physical activities, emotional health, travel, and social relationships.” The IIQ‐7 is measured on a scale from 0 to 100, with higher scores indicating more negative impact of incontinence upon activities, relationships and feelings. Mean (SD) of change is reported at 6 weeks. Quantification of symptoms: number of micturitions. The mean episodes/day of voiding in the toilet, as measured on a 7‐day voiding diary. Mean (SD) of change is reported at 6 weeks. Quantification of symptoms: number of incontinence episodes. The mean episodes/day of urinary incontinence, as measured on a 7‐day voiding diary. Mean (SD) of change is reported at 6 weeks. Other measures of social or emotional impact of incontinence. Bothersomeness, as assessed on the Urogenital Distress Inventory 6 (UDI‐6) (a 6‐item questionnaire that assesses subjective bother associated with incontinence‐related symptoms). Scale is 0 to 100, with higher scores indicating more negative impact of incontinence upon activities, relationships and feelings. Mean (SD) of change is reported at 6 weeks. Other outcomes collected: yoga adherence, yoga self efficacy, the Patient Perception for Bladder Condition (PPBC) ("a single‐item questionnaire assessing the degree to which participants consider their bladder condition to be a problem"), stress incontinence episodes/day, urgency incontinence episodes/day, daytime incontinence, nighttime incontinence, daytime voids and nighttime voids | |
| Notes | Adverse events: “During a 3‐week telephone call and a 6‐week clinic visit, coordinators asked participants about any negative changes in their health and recorded any reported negative changes as adverse events on standardized forms. Adverse events were considered 'serious adverse events' if they met the standard definition of resulting in death, disability, or hospitalization. Participants were also encouraged to call study staff to report any negative changes in their health between scheduled calls or visits.” | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Eligible participants were randomly assigned by a computer in a 1:1 ratio to participate in a 6‐week group‐based yoga therapy program (yoga therapy group) or receive no yoga instruction for 6 weeks followed by a gift certificate for local yoga studio classes (control group). Randomization was stratified by incontinence type (stress or stress‐predominant vs urgency or urgency‐predominant).” |
| Allocation concealment (selection bias) | Unclear risk | Although randomisation was carried out by computer, the exact procedures surrounding allocation were unclear. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and providers were aware of treatment assignment. |
| Blinding of outcome assessment (detection bias) | High risk | Participants self reported symptom improvement, bothersomeness and quality of life. They were not masked to their treatment assignments and the control condition was an inactive, waiting‐list control. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Participants recorded micturitions and incontinence episodes on 7‐day diaries, and the data were abstracted by masked assessors. However, since the participants were aware of treatment assignment, it is possible that this affected their assessment and recording of micturition and incontinence episodes. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition from yoga group at follow‐up was 10% (1/10), and there was no attrition from the control group. |
| Selective reporting (reporting bias) | Unclear risk | Study appears to be free of selective reporting. The primary outcome was prespecified in the trial registration, however none of the reported secondary outcomes are mentioned in the trial registration. |
| Other bias | Low risk | Although groups were different on the IIQ‐7 and in frequency of voiding in toilets at baseline, this is consistent with simple randomisation of a small sample. Funding is university, non‐profit and government, and there is no indication of researcher bias. First author was previously funded by pharma, which is disclosed. |
BMI: body mass index
IQR: interquartile range
MBSR: mindfulness‐based stress reduction
SD: standard deviation
UI: urinary incontinence
UUI: urgency urinary incontinence
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not an intervention of interest | |
| Not an intervention of interest | |
| Not an intervention of interest | |
| Not a primary study report (i.e. editorial about study) | |
| Not an intervention of interest |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Design: parallel randomised controlled trial Country: USA Setting: study run through university but location of intervention delivery (e.g. clinic, community yoga studio) not specified |
| Participants | 50 women with at least daily urinary incontinence Types of incontinence: not reported Diagnostic criteria for incontinence: not reported Severity and duration of incontinence: not reported Age: mean 65 (8) years (range 55 to 83 years) Pregnant/postpartum/menopausal status: age greater than 50 was an inclusion criterion; menopausal status was not reported Weight: not reported |
| Interventions | Yoga group: twice‐weekly Iyengar yoga classes were provided twice per week for 3 months. The class focus was on specialised Iyengar‐style yoga techniques. Home practice: once weekly Common interventions: women were given a brief instruction and written information on behavioural management strategies for incontinence Number of withdrawals, with reasons: 6/56 (11%) of women withdrew. Withdrawals by group and withdrawal reasons were not reported. |
| Outcomes | Quantification of symptoms: number of incontinence episodes. Change in mean episodes of urinary incontinence; how this was measured is not reported. Data for decrease in total UI frequency in the 2 groups are provided, together with P value for comparison between groups, but this cannot be used in a data analysis because the number of participants in each group is unclear. Other outcomes collected: not reported |
| Notes | Adverse events: no discussion of safety or adverse events |
UI: urinary incontinence
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.33 [1.44, 27.88] |
| Analysis 1.1  Comparison 1 Yoga versus no specific active intervention, Outcome 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 6 weeks). | ||||
| 2 Urinary incontinence condition‐ or symptom‐specific quality of life (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 1.74 [‐33.02, 36.50] |
| Analysis 1.2  Comparison 1 Yoga versus no specific active intervention, Outcome 2 Urinary incontinence condition‐ or symptom‐specific quality of life (at short term ‐ 6 weeks). | ||||
| 3 Adjusted analysis for condition‐ or symptom‐specific quality of life at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐27.7 [‐66.80, 11.40] | |
| Analysis 1.3  Comparison 1 Yoga versus no specific active intervention, Outcome 3 Adjusted analysis for condition‐ or symptom‐specific quality of life at short term (6 weeks). | ||||
| 4 Number of micturitions (daily) (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐0.77 [‐2.13, 0.59] |
| Analysis 1.4  Comparison 1 Yoga versus no specific active intervention, Outcome 4 Number of micturitions (daily) (at short term ‐ 6 weeks). | ||||
| 5 Adjusted analysis for number of micturitions at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐0.12 [‐1.73, 1.49] | |
| Analysis 1.5  Comparison 1 Yoga versus no specific active intervention, Outcome 5 Adjusted analysis for number of micturitions at short term (6 weeks). | ||||
| 6 Number of episodes of incontinence (daily) (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐1.57 [‐2.83, ‐0.31] |
| Analysis 1.6  Comparison 1 Yoga versus no specific active intervention, Outcome 6 Number of episodes of incontinence (daily) (at short term ‐ 6 weeks). | ||||
| 7 Adjusted analysis for number of incontinence episodes at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐1.4 [‐2.79, ‐0.01] | |
| Analysis 1.7  Comparison 1 Yoga versus no specific active intervention, Outcome 7 Adjusted analysis for number of incontinence episodes at short term (6 weeks). | ||||
| 8 Bothersomeness of symptoms (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.46, ‐0.34] |
| Analysis 1.8  Comparison 1 Yoga versus no specific active intervention, Outcome 8 Bothersomeness of symptoms (at short term ‐ 6 weeks). | ||||
| 9 Adjusted analysis for bothersomeness of symptoms at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐0.9 [‐1.40, ‐0.40] | |
| Analysis 1.9  Comparison 1 Yoga versus no specific active intervention, Outcome 9 Adjusted analysis for bothersomeness of symptoms at short term (6 weeks). | ||||
| 10 Adverse effects (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.38, 0.38] |
| Analysis 1.10  Comparison 1 Yoga versus no specific active intervention, Outcome 10 Adverse effects (at short term ‐ 6 weeks). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 8 weeks) Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.43] |
| Analysis 2.1  Comparison 2 Yoga versus an active intervention, Outcome 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 8 weeks). | ||||
| 2 Number of women who report cure or improvement of urinary incontinence (at intermediate term ‐ 6 months) Show forest plot | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.03, 1.42] |
| Analysis 2.2  Comparison 2 Yoga versus an active intervention, Outcome 2 Number of women who report cure or improvement of urinary incontinence (at intermediate term ‐ 6 months). | ||||
| 3 Number of women who report cure or improvement of urinary incontinence (at long term ‐ 1 year) Show forest plot | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.03, 1.53] |
| Analysis 2.3  Comparison 2 Yoga versus an active intervention, Outcome 3 Number of women who report cure or improvement of urinary incontinence (at long term ‐ 1 year). | ||||

PRISMA study flow diagram.

Study flow diagram for economics studies.
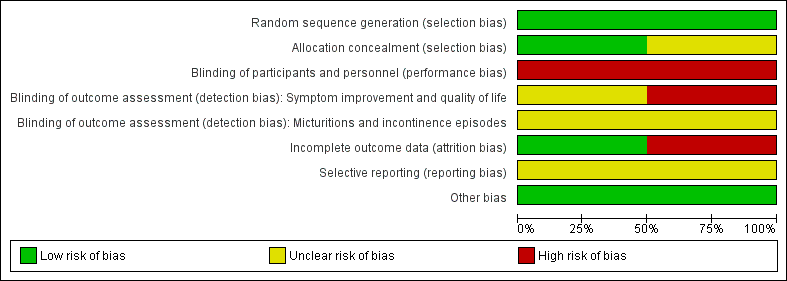
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Yoga versus no specific active intervention, Outcome 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 6 weeks).

Comparison 1 Yoga versus no specific active intervention, Outcome 2 Urinary incontinence condition‐ or symptom‐specific quality of life (at short term ‐ 6 weeks).
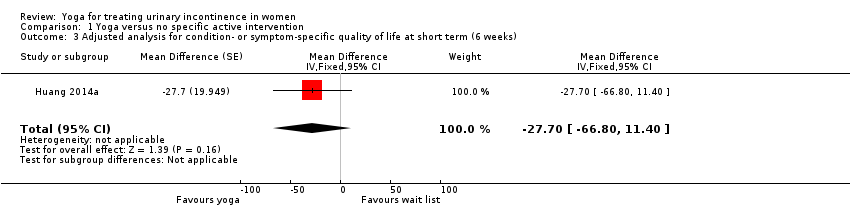
Comparison 1 Yoga versus no specific active intervention, Outcome 3 Adjusted analysis for condition‐ or symptom‐specific quality of life at short term (6 weeks).

Comparison 1 Yoga versus no specific active intervention, Outcome 4 Number of micturitions (daily) (at short term ‐ 6 weeks).
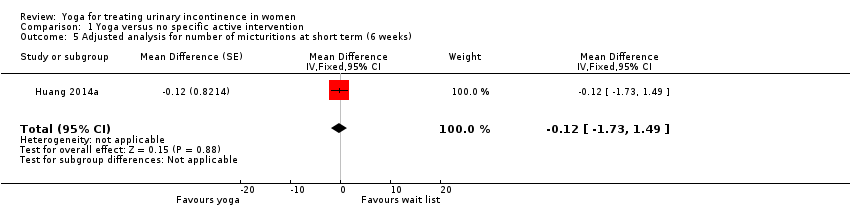
Comparison 1 Yoga versus no specific active intervention, Outcome 5 Adjusted analysis for number of micturitions at short term (6 weeks).

Comparison 1 Yoga versus no specific active intervention, Outcome 6 Number of episodes of incontinence (daily) (at short term ‐ 6 weeks).
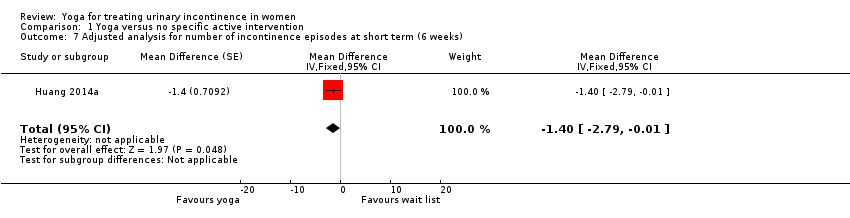
Comparison 1 Yoga versus no specific active intervention, Outcome 7 Adjusted analysis for number of incontinence episodes at short term (6 weeks).
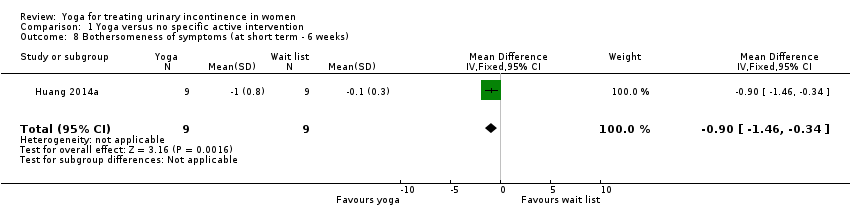
Comparison 1 Yoga versus no specific active intervention, Outcome 8 Bothersomeness of symptoms (at short term ‐ 6 weeks).

Comparison 1 Yoga versus no specific active intervention, Outcome 9 Adjusted analysis for bothersomeness of symptoms at short term (6 weeks).

Comparison 1 Yoga versus no specific active intervention, Outcome 10 Adverse effects (at short term ‐ 6 weeks).
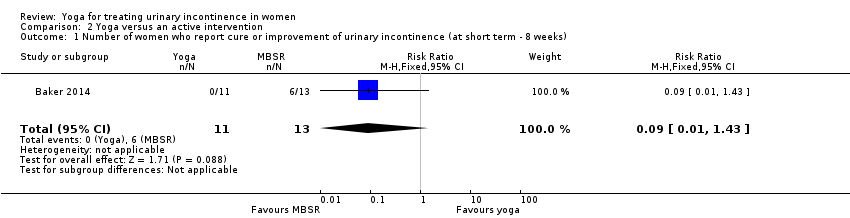
Comparison 2 Yoga versus an active intervention, Outcome 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 8 weeks).
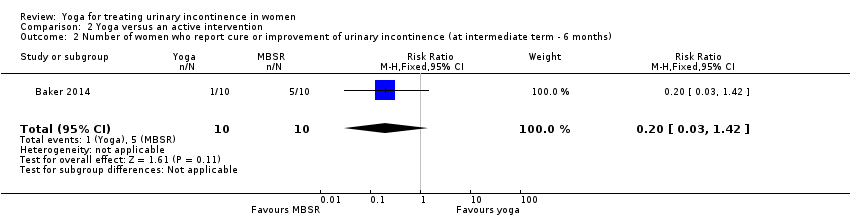
Comparison 2 Yoga versus an active intervention, Outcome 2 Number of women who report cure or improvement of urinary incontinence (at intermediate term ‐ 6 months).
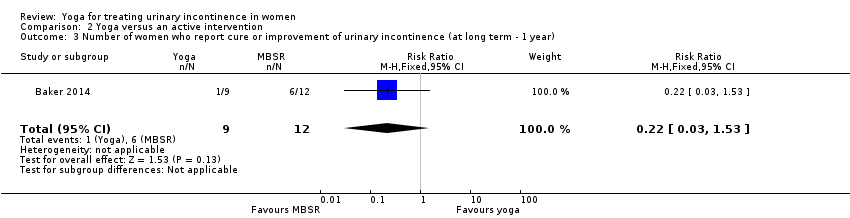
Comparison 2 Yoga versus an active intervention, Outcome 3 Number of women who report cure or improvement of urinary incontinence (at long term ‐ 1 year).
| Yoga compared with wait‐list for urinary incontinence in women | ||||||
| Patient or population: women with either stress‐predominant or urge‐predominant urinary incontinence Settings: community Intervention: yoga Comparison: wait‐list | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Wait‐list | Yoga | |||||
| Number of women who report they are cured (they no longer experience urinary incontinence) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
| Number of women who report cure or improvement of urinary incontinence at short term (six weeks) | 111 per 1000 | 703 per 1000 | RR 6.33 (1.44 to 27.88) | 18 | ⊕⊝⊝⊝ | Number of women who reported satisfaction with change in urine leakage. |
| Urinary incontinence condition‐ or symptom‐specific quality of life at short term (6 weeks) Measured by Incontinence Impact Questionnaire Short Form (IIQ‐7) (lower = better) | The mean change in the control group was a decrease of 31 units. | The mean change in the intervention group was 1.74 units higher (33.02 units lower to 36.50 units higher). | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Number of micturitions (daily) at short term (6 weeks) | The mean change in the control group was a decrease of 0.13 micturitions. | The mean change in the intervention group was | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Number of episodes of incontinence (daily) at short term (6 weeks) | The mean change in the control group was a decrease of 0.27 episodes. | The mean change in the intervention group was | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Bothersomeness of symptoms at short term (6 weeks) Measured by Urogenital Distress Inventory 6 (UDI‐6) (lower = better) | The mean change in the control group was a decrease of 0.1 units. | The mean change in the intervention group was 0.90 units lower (0.34 to 1.46 lower). | Not applicable | 18 | ⊕⊝⊝⊝ | |
| Adverse effects at short term (6 weeks) | 222 per 1000 | 222 per 1000 | RD 0% (‐38% to 38%) | 18 | ⊕⊝⊝⊝ | 2 women in each group reported an adverse effect. However, there were 7 adverse effects overall and the distribution of adverse effects between groups is not reported. None of the adverse effects were considered to be potentially related to the study and none were serious. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded two levels for risk of bias because there was no blinding of participants or providers (risk of performance bias), and outcome was self assessed and self recorded by participants (risk of detection bias). | ||||||
| Yoga compared with mindfulness‐based stress reduction (MBSR) for urinary incontinence in women | ||||||
| Patient or population: women with urge‐predominant urinary incontinence Settings: community Intervention: yoga Comparison: mindfulness‐based stress reduction (MBSR) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| MBSR | Yoga | |||||
| Number of women who report they are cured (they no longer experience urinary incontinence) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
| Number of women who report cure or improvement of urinary incontinence at short term (8 weeks) | 461 per 1000 | 42 per 1000 | RR 0.09 (0.01 to 1.43) | 24 | ⊕⊝⊝⊝ | |
| Urinary incontinence condition‐ or symptom‐specific quality of life at short term (8 weeks) Measured by the Overactive Bladder Health‐Related Quality of Life (OAB‐HRQL) scale (higher per cent improvement = better) | ‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent improvement at 8 weeks was 8.70 (IQR 1.75 to 20.59) in the yoga group (n = 11) and 29.27 (IQR 8.11 to 93.33) in the MBSR group (n = 13) (reported P value = 0.03). |
| Number of micturitions (daily) | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report this outcome. |
| Number of episodes of incontinence (daily) at short term (8 weeks) | ‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent improvement at 8 weeks was ‐33.33 (IQR ‐50.00 to 16.67) in the yoga group (n = 11) and ‐60 (IQR ‐88.89 to ‐50.00) in the MBSR group (n = 13) (reported P value = 0.03). |
| Bothersomeness of symptoms at short term (6 weeks) Measured by the Overactive Bladder Symptom and Quality of Life‐Short Form (OABq‐SF) (lower = better) | ‐ | ‐ | ‐ | ‐ | ⊕⊝⊝⊝ | The study reported medians and IQR, therefore we could not extract data for meta‐analysis. The authors reported that the median per cent change at 8 weeks was ‐25.0 (IQR ‐35 to 20) in the yoga group (n = 11) and ‐55.6 (IQR ‐50 to ‐87) in the MBSR group (n = 13) (reported P value = 0.005). |
| Adverse effects | ‐ | ‐ | ‐ | ‐ | ‐ | The study did not report on adverse effects. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded two levels for risk of bias because there was no blinding of participants or providers (risk of performance bias), and there was a high percentage of loss to follow‐up that was unbalanced across study arms (risk of attrition bias). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.33 [1.44, 27.88] |
| 2 Urinary incontinence condition‐ or symptom‐specific quality of life (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 1.74 [‐33.02, 36.50] |
| 3 Adjusted analysis for condition‐ or symptom‐specific quality of life at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐27.7 [‐66.80, 11.40] | |
| 4 Number of micturitions (daily) (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐0.77 [‐2.13, 0.59] |
| 5 Adjusted analysis for number of micturitions at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐0.12 [‐1.73, 1.49] | |
| 6 Number of episodes of incontinence (daily) (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐1.57 [‐2.83, ‐0.31] |
| 7 Adjusted analysis for number of incontinence episodes at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐1.4 [‐2.79, ‐0.01] | |
| 8 Bothersomeness of symptoms (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.46, ‐0.34] |
| 9 Adjusted analysis for bothersomeness of symptoms at short term (6 weeks) Show forest plot | 1 | Mean Difference (Fixed, 95% CI) | ‐0.9 [‐1.40, ‐0.40] | |
| 10 Adverse effects (at short term ‐ 6 weeks) Show forest plot | 1 | 18 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.38, 0.38] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women who report cure or improvement of urinary incontinence (at short term ‐ 8 weeks) Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.43] |
| 2 Number of women who report cure or improvement of urinary incontinence (at intermediate term ‐ 6 months) Show forest plot | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.03, 1.42] |
| 3 Number of women who report cure or improvement of urinary incontinence (at long term ‐ 1 year) Show forest plot | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.03, 1.53] |

