Intervenciones telefónicas proporcionadas por profesionales sanitarios para la educación y el apoyo psicosocial de los cuidadores informales de pacientes adultos con enfermedades diagnosticadas
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised trial (pilot study) (grant dates April 1st 1994‐March 31 1998) | |
| Participants | Caregivers of stroke survivors recruited from a university medical centre in Rhode Island USA. Caregiver age ranged from 21‐86 years with a mean of 56.8 (16.4). The majority were female (65.3%). Caregivers were spouses (45%), daughters (33%), sons (10%) or other (e.g. sister, partner, mother) (2%). Forty‐nine percent had an annual household income of $15,000‐29,999, 26.5% of $30,000‐49,000, 18.3% of $0‐14,999 and 6.1% had an annual income ≥ $50,000. Care‐recipients: Stroke survivors were required to be fully oriented and able to follow a 3‐step command and had either evidence of stroke on neuroimaging or were hemiparetic. Stroke survivors were mainly female (65.3%) with an age range of 44‐87 years (mean (SD) 70.1 (11.6)). Fifty‐one percent were married, 42.9% divorced/separated/widowed and 6.1% were single. Annual household income was $0‐14,999 (32.6%), $15,000‐29,999 (46.9%), or $30,000‐49,000 (20.4%). | |
| Interventions | Intervention: Family Intervention: Telephone Tracking (FITT) plus usual care (n = 23) Aim: The primary goal of FITT is to assist stroke survivors and their caregivers in identifying problems during their transition back home. It consists of two main components: psychoeducation and follow‐up. Interventionist(s): Four individuals with prior clinical experience of either family therapy or stroke (a psychiatric resident, family therapy graduate students, a stoke rehabilitation nurse, a master’s level family therapist). Mode of delivery: Telephone Duration: 6 months: Weekly for 6 weeks, biweekly for next 2 months, for a total of 13 calls to each individual (26 calls per dyad). Content: FITT focuses on 5 key areas: (1) family functioning, (2) mood, (3) neurocognitive functioning, (4) functional independence, and (5) physical health. Expectations and transitional challenges within each of these areas are discussed. To reinforce attention to these areas, during the calls, participants were asked to rate themselves and their partner in the 5 areas (worse, same, better) using a structured grid. Telephone contacts were designed to identify and address problems in these key areas, provide psychoeducation, facilitate the dyad’s problem‐solving, and provide follow‐up support. No direct treatment of psychiatric or family problems was given, but participants were supported in seeking referrals for special assessment or treatment as required. Standardisation: All interventionists received didactic instruction, familiarization with the FITT manual, role playing, and group supervision. Therapist adherence and competence was monitored and found to be acceptable. Comparison group: Standard medical follow‐up (n = 26) | |
| Outcomes | 1. Psychological health (depression): 13‐item Geriatric Depression Scale (GDS) Short Form which uses yes/no responses. Higher scores indicate higher levels of depression. 2. Health status and well‐being:
3. Family functioning: The Family Assessment Device (FAD) and the Perceived Criticism Scale (PCS). Higher scores indicate better family functioning. Outcome data were collected at 3 and 6 months post‐stroke (end of intervention is 6 month time point). | |
| Notes | Unpublished information requested via email but no response received from the contact author. Professor Ivan Miller, a named author on the paper did provide some additional information via email to enable categorisation of the paper. For the outcome physical health, the Frenchay Activity Index mean change scores as reported were used in this review. For family functioning, the global family functioning score was used in the review and reported in Additional Table 4. Funding source: National Institute for Mental Health (NIMH) grant 1 R21 MH54182‐01 (p.S72). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Urn randomisation (S64) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | “Data collectors were blinded to group assignment” (S66). |
| Incomplete outcome data (attrition bias) | Unclear risk | 11 caregivers left for reasons including stroke survivor death (n = 2), caregiver death (n = 1), self‐withdrawal/repeated failures to return calls (n = 3), permanent nursing home placement of stroke survivor (n = 3), and refusal to complete assessments (n = 2); not differentiated by intervention or control groups (S67). |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported (S69). |
| Other bias | Unclear risk | Caregiver characteristics were not reported separately for each group. "...an urn randomisation procedure was used and this should have balanced our imbalances" (S64). |
| Methods | Randomised controlled trial (study dates not reported) | |
| Participants | Caregivers were wives of people with dementia recruited from the Michigan Alzheimer’s Disease Research Center (MADRC) and local chapters of the Alzheimer’s Association (AA) in Michigan and Ohio. The average age of the sample was 66.8 years (SD = 9.4), the majority (65.7%) had at least some education beyond high school and described themselves as white/caucasian (92.7%). About one‐fifth (21.9%) were employed part‐ or full‐time. | |
| Interventions | Intervention: Health First (n = 74) Aim: To assess whether compared with baseline, participants in the Health First showed greater improvements in selected outcomes than the control group Interventionist(s): Trained behaviour change counsellors who were current or retired health or social service professionals (confirmed by author via email) Mode of delivery: Telephone Duration: 14 telephone calls over a 6‐month period (weekly for 2 months, biweekly for 2 months, monthly for 2 months). Content: During the first two calls, caregivers were directed to complete daily activity logs (to establish baseline levels of physical activity) and to set a realistic long‐term exercise goal that specified the type of exercise as well as duration and frequency. They were encouraged to set a goal that consisted of a minimum of 30 minutes of low to moderate intensity aerobic exercise at least 3 times a week, supplemented with stretching and strength training. During subsequent calls, participants set short‐term goals for exercise and a problem‐solving process was used to address barriers to goal attainment. They also received a Health First video featuring spouse caregivers discussing strategies for fitting physical activity into their daily routine as a way to model desired behaviour, a choice of exercise videos, a copy of the booklet “Pep up our Life”, and a Health First workbook that explains each step of the program. Standardisation: Counsellors participated in a day‐long training session to address program fidelity that included opportunities for role play and performance feedback to promote appropriate and accurate delivery of the program. A project manager monitored several calls made by each counsellor to confirm that the intervention was being delivered correctly and uniformly. Comparison group: No intervention/usual care (n = 63). | |
| Outcomes | 1. Burden:
2. Psychological health (depression): The 11‐item Iowa short form of the Center for Epidemiologic Studies Depression Scale (CES‐D). Participants were asked the frequency with which they experienced symptoms in the past week (hardly ever or never, some of the time, or much or most of the time). Possible scores range from 0 to 22; higher scores were associated with more symptoms. 3. Psychological health (stress): Perceived stress was measured with the 14‐item Cohen Perceived Stress Scale. Participants rate the degree to which events in the past month were perceived as stressful using a 5‐point scale ranging from never (0) to very often (4); higher scores indicating higher levels of perceived stress. 4. Health status and well‐being (self‐efficacy):
All outcomes were collected using follow‐up interviews administered at the end of intervention short‐term approximately 6 months and approximately 12 months from baseline. | |
| Notes | For the outcome burden, data from the subjective burden questionnaire was used in our analysis. For the outcome self‐efficacy, the data for self‐efficacy for self‐care was used. Funding source: A grant from the National institute on Aging to the Michigan Alzheimer’s Disease Research Center (p.172). Unpublished data sought via email, author responded and all available data were provided. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to assess |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to assess |
| Incomplete outcome data (attrition bias) | Unclear risk | 15.9% overall (n = 27) (17 intervention versus 9 control) (p.179) |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported |
| Other bias | High risk | At baseline, there was a difference between the groups noted in depression scores (intervention 9.4 SD 2.9; control 7.9, SD 2.8) (p.181). |
| Methods | Randomised controlled trial (pilot study) (September 2009‐September 2015) | |
| Participants | Caregivers of people with multiple sclerosis (PwMS) recruited from 3 neurological sites (n = 70) in the Republic of Ireland. Caregiver mean age was 51.3 years (SD 13.4), range 22‐84 years; 47.1% were male and 52.9% were female. The majority had at least secondary level education (51.5%) or tertiary education (41.4%). The remaining 7.1% had primary education. Twelve (17.1%) were single, 50 (71.4%) were married and 2 (2.9%) were living as married. Three (4.3%) were separated or divorced and three (4.3%) widowed. An average of 8.8 hours (SD 9.04) were spent caring in a 24‐hour period and the average number of years caring for the PwMS was 11 (SD 7.69). Most (60%) were living with the care‐recipient. Twenty‐five (35.3%) were in paid employment with hours ranging from 6 to 90 hours per week. Thirty‐six (51.4%) were not employed. | |
| Interventions | Intervention: Nurse‐led pro‐active telephone support (n = 33) Aim: To enable nurse specialists in multiple sclerosis (NSMS) help family members and caregivers of PwMS learn problem management skills in order to be better prepared for their role in supporting a person with MS Interventionist(s): Three NSMS who had completed a postgraduate diploma in clinical practice along with a certificate in MS nursing Mode of delivery: Telephone Duration:3 months (four calls; two in month one, one in month two and one in month three) Content: In advance of receiving the calls, the support persons received the support person guidebook. During the calls, the NSMS referred to the guidebook. The support person guidebook was designed to facilitate the process and enable nominated support persons prepare for the calls from the nurse specialists. Scripted interviews were designed to provide a focus for the telephone contacts and help the NSMS and support persons structure their interaction using a problem management approach. Standardisation: Standardisation of interventionist training was maximised through the inclusion of a training section in the intervention manual. Training for delivery of the intervention was provided in accordance with the intervention manual. Each NSMS received a minimum of two hours one‐to‐one training. Comparison group: Usual care (n = 38). | |
| Outcomes | 1. Quality of life: WHOQoL BREF instrument ‐ 26 questions covering four domains (physical, psychological, social relations, and environmental). Higher scores indicated better quality of life. 2. Burden: Caregiver Reaction Assessment (CRA), a 24‐item scale, which assesses how caregivers react to caring for an ill person in 5 domains: how caring affects caregivers health, daily schedule (schedule disruption), finances, their sense of self‐worth (self‐esteem), and their family. Higher scores indicated greater burden. 3. Skill acquisition (preparedness to care): using the support person preparedness scale, an 8‐item subscale with a five point rating scale developed as part of The Family Care Inventory in the early 1980s (Archbold 1990). Higher scores indicated greater perceived preparedness to care. 4. Health status and well‐being (self‐efficacy): Self‐Efficacy for Problem‐solving scale, a 4‐item caregiver self‐efficacy in problem management scale and Self‐Efficacy for Obtaining Respite subscale. Higher scores indicated greater self‐efficacy. 5. Satisfaction with the intervention: Client Satisfaction Questionnaire‐8 (CSQ‐8), an 8‐item questionnaire with a four option response ranging from 1‐4, with higher scores indicating greater satisfaction. Data were collected at the 4‐week time point which was prior to completion of the intervention, and at the 3‐month time point (approximately week 12), which was the end of the intervention time point. | |
| Notes | The term support person (SP) was used for caregivers. Standard deviation data for burden and preparedness to care were obtained from the author. Following email communication with the originators of the burden instrument (CRA), the subscale result for 'schedule disruption' was used for 'Burden' in the review. Funding source: Fellowship from the Health Research Board Ireland | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random list of numbers for the control and intervention groups at each site was generated by a statistician independent of the study (p.174). |
| Allocation concealment (selection bias) | Low risk | Allocation held by a person independent of the trial and sent via email on enrolment to the trial (p.174) |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | High risk | Not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Overall attrition minimal (2 per group) and reasons provided (p.238) |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes were reported. |
| Other bias | High risk | The interventionists who delivered the intervention delivered care to both groups. |
| Methods | Randomised controlled trial (study dates not reported) | |
| Participants | Informal caregivers of people with dementia whose care‐recipient was admitted to a nursing home in Rhode Island, USA. The mean age of the caregivers (data provided by the author) was 60.26 years (SD = 11.42) for the entire group. The majority of caregivers were adult children, 83% in the intervention group and 72% in the control group. The majority of caregivers were female (87% data provided by author) for the entire group. The mean years of education was 15.17 (SD = 3.03) in the intervention group and 14.82 (SD = 3.54) in the control group. The mean duration in months of caregiving for the intervention group was 49.23 (SD = 37.59), and for the control group 46.30 (SD = 38.11). Twenty‐seven caregivers received the intervention and 26 caregivers received standard care. Care‐recipients: mean care recipient age in the intervention group was 82.54 (SD = 5.48) and in the control group 82.73 (SD = 9.05). The mean length of time since dementia diagnosis (months) for the intervention group was 41.14 (SD = 30.15) and control group 42.05 (SD = 33.01). Care‐recipients nursing home placement (weeks) for the intervention group was 6.58 (SD = 3.88) and control group 5.50 (SD = 3.64). | |
| Interventions | Intervention: Family Intervention: Telephone Tracking‐Nursing Home (FITT‐NH) plus a resource pack containing local resources and educational material (n = 27) Aim: The intervention was designed to help caregivers adjust to the new burdens and stresses of nursing home placement in the first few months after placement has occurred. Interventionist(s): A trained Master’s level therapist (counsellor – confirmed by author via email) Mode of delivery: Telephone Duration: 3 months (initial call, followed by 7 weekly follow‐up calls, and 2 biweekly termination calls over the third month. Initial contact lasted 60 minutes and follow‐up and termination calls lasted 35‐45 minutes. Content: The FITT‐NH was delivered by a standardised method based on a detailed treatment manual that included sample dialogue, a behavioural problems guide to generate solutions with the caregiver, and a specific interventions guide matched to specific caregiver situations. The FITT model assesses caregiver and care‐recipient functioning in key areas (i.e. the caregiver’s emotional functioning, health, social support, family functioning, and communication with staff; care‐recipient’s emotional adjustment, behaviour, and cognition). These key areas are repeatedly assessed throughout the treatment, and particular interventions are applied based on these assessments. Specific interventions include supportive approaches (i.e. empathy, giving permission, normalising, validation, or venting) and active strategies (i.e. bibliotherapy, interpretation, positive reframing, problem‐solving, reference to resource packet, referral, and setting task directive). In the first contact, caregivers are provided with a rationale for the FITT, description of future telephone contacts, an introduction to resource materials, and an assessment of key areas thought to be instrumental in addressing caregiver coping and adjustment. The psychoeducation component reviews information about dementia, specialty care units, and common psychological and physical effects of caregiving. Scheduled telephone contacts identify new problems, discuss positive and negative changes, provide psychoeducation, and caregiver problem‐solving is assisted. The final two calls (biweekly) address termination by anticipating FITT contacts coming to an end and fostering reliance on the support network established in FITT‐NH. This phase reviews caregiver progress and reinforces success, coping strategies, and positive change. The therapist summarised these sessions in a post‐treatment letter sent to the caregiver. Standardisation: States that it was delivered in a standardised way. The intervention was administered according to the written manual procedures (confirmed by author via email). Comparison group: Control group (no formal intervention, received a resource pack containing local resources and educational material) (n = 26) | |
| Outcomes | 1. Quality of life: SF‐36. Higher scores indicated better quality of life. 2. Burden: Burden Interview (ZBI) a 22‐item inventory assessed caregivers’ subjective feelings of the impact of caregiving on emotional and physical health functioning, social life, and financial status. Higher scores reflected greater burden. 3.Psychological Health (depression): Center for Epidemiology Studies Depression Scale, a 20‐item measure of depressive symptoms. Higher scores reflected higher level of depression. 4. Satisfaction:
Outcome data were collected using face‐to‐face assessments with the caregivers at their home or nursing home at the end of intervention (3 months from baseline). | |
| Notes | Outcome data on quality of life and Information on interventionist training was provided by the author via email. Funding source: Grant from the National Institute on Aging (AG026122; J.Davis, PI) (p.387). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Urn randomised to balance groups to gender relationships and facility type (p.381) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | A trained research assistant, blind to group membership, conducted face‐to‐face assessments with the caregivers at their home or nursing home at baseline and at the end of the intervention (p.382). |
| Incomplete outcome data (attrition bias) | Low risk | Overall attrition low (13%) and balanced between groups (3 and 4); reasons for attrition provided (death n = 5; discharge from nursing home n = 1, and withdrawal n = 1) (p.384). |
| Selective reporting (reporting bias) | High risk | Quality of life was not reported (Table 3, p.385). |
| Other bias | Low risk | Groups did not differ in caregiver age, education, gender, relationship (spouse versus adult child), and length of caregiving, length of dementia diagnosis or time since placement.(Table 2, p.384, table 3, p.385). |
| Methods | Randomised clinical trial (Study dates not reported) | |
| Participants | Chinese family caregivers of people with dementia in the San Francisco Bay area, United States of America (USA). All caregivers were female (n = 55, 100%) and were included in the study if they were at least 21 years of age, caring for a family member with significant memory loss or deterioration in cognitive abilities, spending at least 8 hours/week caregiving for at least 6 months, owned a phone, planning to remain in the area for 6 months, and agreed to random assignment to both conditions. Care‐recipients were required to have a score of 23 or less on the Mini‐Mental State Examination (MMSE) and be unable to perform one or more activities of daily living (ADLs) and two or more Instrumental ADL (IADLs), or have a documented dementia diagnosis. The mean age of the caregivers who completed the study was 59.3 (SD 12.23), were in the USA for 31.13 years (SD ‐20.93), and had a mean number of years in education of 13.42 (SD 4.10). Most were non‐spousal family relationships (mean spouse caregiver in telephone support condition (TSC) (7, SD 30.4), in‐home behavioural management program (IHBMP) (7, SD 31.8); mean non‐spouse caregiver TSC (16, SD 69.6) IHBMP (15, SD 68.2). Average duration of caregiving was roughly four years (TSC (41.26 months, SD 29.77), IHBMP group (48.32 months, SD 42.86)). More than 75% of caregivers were married: TSC (single (n = 2, 8.7%) , married (n = 18, 78.3%), widowed (n = 1 4.3%), divorced (n = 2, 8.7%)); IHBMP group (single (n = 4, 18.2%), married (n = 17, 77.3%), widowed (n = 1, 4.5), divorced (0)). About 80% of them had children: TSC: (n = 18, 78.3%), IHBMP (n = 18, 81.8%)). At least 75% reported that they had some help with caregiving (n = 20, 87% of the TSC and n = 6, 27.3% of the IHBMP group). About 30% said they were having financial difficulties and over 30% said that they assumed the primary caregiver role because no one else was available. | |
| Interventions | Intervention: Telephone support groups (n = 28) Aim: To evaluate the efficacy of an in‐home intervention, based on cognitive behaviour therapy principles, to relieve stress and depression in female Chinese‐American caregivers Interventionists: Advanced doctoral students in psychology from a local university program Mode of delivery: Telephone Duration: 12 weeks (six phone calls at two week intervals) Content: Calls began with a general inquiry as to caregiver and care‐recipient well‐being, then one or more problems were identified for discussion. Common themes were incontinence, incessant questioning, temper outbursts, and nocturnal awakenings. The interventionist remained empathic and supportive, and at a comfortable moment, indicated that written information was available to help. Consumer‐friendly materials (in Chinese or English) were mailed if requested. The next phone call was scheduled and the session ended with expressions of concern for the welfare of caregiver and care‐recipient. Standardisation: No detail provided Comparison group: IHBMP is comprised of six modules that focus on learning new skills to help the caregivers cope with caregiving stress. Each module required one or more 90‐minute sessions; one additional session was used for any module requiring extra time (n = 27). | |
| Outcomes | 1. Psychological health (depression): 20‐item Center for Epidemiological Studies Depression scale (CES‐D). Higher scores indicated higher level of depression. 2. Psychological health (stress): The 10‐item Perceived Stress Scale and the Conditional Bother Subscale (CBS) is derived from the Revised Memory and Behavior Problems Checklist (RMBPC). Higher scores indicated higher level of stress. 3. Health status and well‐being (self‐efficacy): The revised self‐efficacy scale (SE). Higher scores indicated better perceived self‐efficacy. Time point for data collection not stated | |
| Notes | For the outcome 'stress', the results from the 10‐item Perceived Stress Scale were used in the analysis for this review. Funding source: Research grant from the National office of the Alzheimer’s Association, Chicago – grant IIRG‐01‐3157 to DGT (p.433). Unpublished data sought via email but not received; author did provide information to enable categorisation of the study during the data screening process. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to assess |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to assess |
| Incomplete outcome data (attrition bias) | Low risk | Ten of the 55 (18%) participants dropped out either before or in the early stages of treatment — five from each group (p.427). |
| Selective reporting (reporting bias) | Low risk | Reports on all prespecified outcomes (p.431). |
| Other bias | Low risk | “The two groups were statistically equivalent at baseline, although the IHBMP appears to be higher than the TSC on CES‐D" (p.431). |
| Methods | Randomised pilot trial (Study start date: October 2008, end date was not reported but final data collection date for primary outcome was February 2012) | |
| Participants | Informal caregivers of people with dementia recruited from 2 memory disorder clinics, the local Alzheimer’s caregiver organisations, local newspapers, and self‐referral based on information from a friend in Jacksonville‐Tallahassee, USA. Caregivers (CGs) were included if they were 18 years of age and older, provided direct care to their care‐recipients (CR) for a minimum of 6 hours per week for at least 6 months, reported specific caregiving problems amenable to change within a 12‐week intervention frame (e.g. increasing CG social and recreational activities and managing effectively CR agitation and aggressive behaviours), scored a minimum of 10 on the Patient Health Questionnaire‐9 indicating a moderate level of depression, and reported no difficulties in hearing over the phone.The caregivers consisted of husbands (n = 1), wives (n = 5), daughters (n = 4), granddaughter (n = 1) of the care‐recipients. Five of the 7 caregivers randomised to the intervention group completed the intervention and 6 of the 7 randomised to the control group completed the study. The mean age of the caregivers who completed the study was 58.09 (SD = 10.11) years and 1 was male and 10 female. All caregivers had an average of 14.18 (SD = 1.78) years education. Care‐recipients: All care‐recipients were African‐Americans with mean age in years 76.73 (SD = 6.60) and education (years) 12.27 (SD = 3.80), independence in activity of daily living mean score of 2.64 (SD = 1.91) and independence in instrumental activities of daily living mean score of 20.36 (SD = 2.46). Care‐recipients were required to have a medical diagnosis of possible Alzheimer’s disease or other type of progressive dementia verified by a physician at a memory disorder clinic approved by the Alzheimer’s Disease Initiative and at least one limitation in basic activities of daily living and 2 dependencies in IADL. | |
| Interventions | Intervention: A cognitive behavioural program (CBT) (group and individual format) (n = 7) Aim: To assess CGs appraisal of the intervention process and its impact on daily caregiving experiences and to conduct a preliminary analysis of the effects of face‐to‐face and telephone‐based CBT on changes in subjective burden, assistance support, depression, and health status in African‐American dementia CGs. Interventionist(s): Four African American counsellors, 3 females and 1 male, and were randomly assigned to the groups. All counsellors had a master’s degree in a counselling related profession and at least 1 year of group intervention experience. All 4 regularly used CBT in their practices but none had participated in a formal CBT workshop prior to the study. Average age of counsellors (66 years, SD = 9.2), average years of education (21.5, SD = 1.29), average years in professional practice (30.75, SD = 13.38). Mode of delivery: Telephone Duration: Twelve, 1‐hr, weekly sessions Content: Telephone‐based CBT took place at the CGs’ homes mediated by either a Florida State University or Mayo Clinic Jacksonville teleconferencing system. The intervention program consisted of seven group and five individual CG goal‐setting and implementation sessions. The small group format was used to encourage discussion and clarification about the rationale for and application of fundamental, cognitive–behavioural skills (e.g. assertiveness and effective thinking), as well as to enhance social support among participants. Individual sessions concentrated on the development of problem‐solving skills, beginning with the identification of key caregiving problems and the performance of focused problem histories, followed by goal setting, rehearsal of goal‐related behaviours, goal implementation, and monitoring change over time. Acquisition of such skills was time‐intensive and required tailoring of the intervention to the specific circumstances, characteristics and preferences of the CG, thus necessitating a one‐on‐one format. All participants received a CBT guidebook and a copy of The 36 Hour Day, and information about local dementia care resources prior to the first training session. Standardisation: Interventionist training consisted of two 6‐hour training workshops performed over a period of 2 months by two of the authors who were doctoral‐level licensed clinicians. The authors concluded that overall findings of treatment fidelity analysis suggested that pilot counsellors adhered to implementation guidelines in conducting the CBT program. Comparison group: Face‐to‐face CBT was performed at a university‐based conference room or in a private, soundproof room at a public library. The structure and contents of the programme were the same as that for the telephone intervention (n = 7). | |
| Outcomes | 1. Burden: The subjective burden scale of the Caregiver Appraisal Inventory – a subscale of the Caregiver Appraisal Inventory (CAI). Higher scores indicated greater burden. 2. Psychological health (depression): Center for Epidemiological Studies Survey‐Depression scale (CES‐D) is a 20‐item self‐report scale that assesses depression in non‐clinical community populations. Respondents rate the frequency of a variety of depressive symptoms they have experienced over the past week on a 0 to 3 scale. A total score ranging from 0 to 60 is derived by summing the item scores. Individuals scoring 16 or higher on the CES‐D are generally considered to be at risk for developing clinical depression. 3. Psychological health (stress): The Revised Memory and Behaviour Problem Checklist (RMBPC) ‐ The disruptive behaviour and depression subscales (17 items) measure CG distress associated with CR disruptive behaviours and CR difficulties with depression. Higher scores indicated higher levels of stress. 4. Health status and well‐being (physical health): Physical symptoms subscale of the modified Caregiver Health and Behaviour inventory (CHHB). The modified CG Health and Health Behaviors inventory (CHHB) is a 42‐item scale to assess dementia CG perceived health, sleep quality, unhealthy behaviours, chronic health conditions, and physical symptoms. Two items ask respondents to rate their general health; two items measure quality of sleep; four items assess involvement in unhealthy behaviours such as smoking and drinking alcohol to excess; 15 items assess the presence of CG health problems, such as high blood pressure, diabetes, cancer, and arthritis; and 21 items measure physical symptoms, such as headaches, shortness of breath, heartburn, and sore throat. Higher scores indicated greater physical ill‐health. Outcome data were collected via the telephone at the end of intervention, approximately 1 week after the 12 week CBT program. | |
| Notes | Funding source: Grants from the National Institute of Mental Health (R34MH078999) Florida State University College of Medicine, and University of South Florida Health Byrd Alzheimer’s Institute (p.124). Unpublished data sought via email but not received, author did provide information to enable categorisation of the study during the data screening process. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to assess |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | "Post treatment assessments were also administered over the telephone by an independent interviewer..." (p.130). "The interviewer was unaware of assignment to treatment condition" (p.130) . |
| Incomplete outcome data (attrition bias) | Low risk | Minimal attrition (3:1 intervention and control) and reasons provided, p.133 |
| Selective reporting (reporting bias) | High risk | Results for stress not reported (p.134) |
| Other bias | Low risk | Groups fairly balanced on all baseline characteristics and measures, although Jacksonville CRs had a significantly greater number of years of education than their Tallahassee counterparts (p.134). |
| Methods | A single‐blinded randomised controlled trial (recruitment February 2011‐March 2012) | |
| Participants | Family caregivers of persons with dementia (PWD) in Hong Kong. Caregivers were the primary caregivers of care‐recipients who had a clinical diagnosis of dementia. The majority of caregivers were in the mean age category of between 41‐50 years (n = 21, 55.2%). The remaining study participant ages in years were 31‐40 (n = 3, 7.89%), 51‐60 (8, 21.05%), 61‐70 (n = 3, 7.89%), 71‐80 (n = 1, 2.63%) and > 80 (n = 2, 5.62%). The majority were female (n = 24, 63.15%) and males accounted for 28.94% (n = 11). The caregivers were children of the care‐recipients (n = 30, 78.9%), spouses (n = 4, 10.52%), grandchild (n = 1, 2.63%), son/daughter in‐law (n = 3, 7.89%). Education ranged from secondary education (n = 27, 71.05%), tertiary (n = 8, 21.05%), primary (n = 2, 5.26%) or Illiterate (n = 1, 2.63%). In the intervention group, caregiver monthly income ranged from $10,000 or less, n = 3 (16.7%), $ 10,001‐$20.000, n = 9 (50%), $20.001‐$30,000, n = 2 (11.1%), $30,001‐$40,000, n = 2 (11.1%), $40,001‐$50,000, n = 2 (11.1%). In the control group, monthly income was $10,000 or less, n = 5 (25%), $10,001‐$20.000, n = 9 (45%), $20.001‐$30,000, n = 2 (10%), $30,001‐$40,000, n = 2 (10%), $40,001‐$50,000, n = 1 (5%), and more than $50,000, n = 1 (5%). Caregivers spent between 1‐9 hours caregiving in the intervention group (1 hour (n = 3, 16.7%), 1‐3 hours (n = 2, 11.1%), 4‐6 hours (n = 6, 33.3%), 7‐9 hours (n = 1, 5.6%), 9 hours (n = 6, 33.3%)). In the control group, caregivers also spent between 1 and 9 hours caregiving (1 hour (n = 1, 5.3%), 1‐3 hours (n = 4, 21.1%), 4‐6 hours (n = 9, 47.7%), 7‐9 hours (n = 1, 5.3%), 9 hours (n = 4, 21.1%)). | |
| Interventions | Intervention: A psychoeducation intervention plus a DVD that contained educational information about dementia caregiving (n = 20; of whom 18 received the intervention) Aim: To investigate the effectiveness of a telephone‐delivered psychoeducational intervention in supporting dementia caregivers in the community Interventionist(s): Registered social workers Mode of delivery: Telephone Duration:12 weeks (approximately 30 minutes per session, one session per week; the day and time of phone calls were flexible to the agreement between the participants and the social workers). Content: Participants in the intervention group were educated and given advice on topics related to dementia caregiving, including knowledge of dementia, skills of communicating with the patient, management of behavioural and psychological symptoms of dementia (BPSD), caregivers’ own emotional issues, resources available in the community, and long‐term care plan. The topics covered and the schedule of presentation were similar to typical psychoeducation interventions held 'on site' at community centres. The focus was on providing emotional support; directing caregivers to appropriate resources; encouraging them to attend to their own physical, emotional, and social needs; and educating them on strategies to cope with ongoing problems. Standardisation: no detail provided Comparison: Caregivers in the control group were given a DVD containing educational information about dementia caregiving (n = 22, of whom 20 remained as control). | |
| Outcomes | 1. Burden: Zarit Burden Interview Chinese version (ZBI) which consisted of 22 items pertaining to dementia caregiving in areas of perceived physical and psychological well‐being, social life, and finances. The participants indicated, on a 5‐point scale (0 = not at all to 4 = nearly always) during pretest and post‐test, how often they experienced distress resulting from caring for a relative with dementia. Higher scores indicated greater burden. 2. Health status and well‐being (self‐efficacy): Chinese version of The Revised Scale for Care giving Self Efficacy: Obtaining respite (SE‐OR), Responding to Disturbing Behaviours (SE‐RDB), Controlling Upsetting Thoughts (SE‐CUT). Higher scores indicated greater self‐efficacy. Outcome data were collected at the end of intervention i.e. approximately 3 months after the pretest. | |
| Notes | For the outcome self‐efficacy the results for the sub‐scale 'Responding to Disturbing Behaviours (SE‐RDB)' were used in the analysis. Funding source: none stated Unpublished information requested and received at the data screening stage | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A "computerised randomisation program" was used (p.1192). |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | "...research assistant blind to group assignment" (p.1192) |
| Incomplete outcome data (attrition bias) | Low risk | Overall attrition (for each group; with reasons) very low, and balanced (p.1194) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported (p.1195, table 4) |
| Other bias | Low risk | No significant differences at baseline on demographic variables and baseline measures (p.1194, table 2) |
| Methods | Randomised controlled trial (February 2005‐June 2007 (Final data collection date for primary outcome)) | |
| Participants | Caregivers of people with dementia (n = 154), Memphis, USA. Caregiver age in years ranged from 37.9‐86.5 (mean age 65.6, SD 12.4). The sample consisted of 83.3% (n = 129) females and 16.2% (n = 25) males of which n = 38 (24.7%) were employed and n = 132 (85.7%) were married. The majority of the caregivers were white (n = 108, 70.1%), black (n = 45, 29.2%), other (n = 1, 0.6%). Most were married (n = 132, 85.7%); n = 38 (24.7%) were employed and mean years of education were 12.8 (SD = 2.0) (i.e. almost a year beyond high school). | |
| Interventions | Intervention: CONNECT (individual and group delivery, 5‐6 caregivers/group; 15 groups) (n = 77) Aim: To determine if telephone support groups for dementia caregivers have an effect on bother with patient behaviours, burden, depression, and general well‐being Interventionist(s): 3 group leaders each with a case load (one with an MSc in divinity, one an MSc in psychology, one an MA in Sociology) Mode of delivery: Telephone Duration: One year (biweekly for 2 months and monthly thereafter for a year, for a total of 14 hour‐long sessions) Content: Content and structure of the intervention were based on the 6‐month REACH II intervention of 12 individual in‐home and by‐telephone sessions and five telephone support group sessions. Session materials consisted of a Caregiver Notebook and commercially available pamphlets. The Notebook, initially developed for a primary care intervention comprised behaviour management chapters and 17 caregiver stress/coping chapters. Each participant received a one‐on‐one introductory telephone call. Like REACH, the multicomponent intervention targeted caregiving risks, including risks associated with emotional and physical well‐being, safety, burden, social support, and patient behaviour management. Standardisation: Training and certification helped to ensure consistency across group leaders. During the final certifying role play, each prospective Group Leader provided the entire first session and two additional educational presentations. Study investigators evaluated behaviourally anchored ratings of specific procedural techniques (e.g. correct use of forms) and clinical skills (e.g. active listening). Comparison group: Caregivers received pamphlets on dementia and safety as well as telephone numbers for local resources. At the end of the study, they received the Caregiver Notebook and a workshop focusing on knowledge, safety, health, well‐being, behaviour management, and stress (n = 77). | |
| Outcomes | 1. Burden: The 12‐item Zarit Burden Interview (ZBI) assessed caregiver burden. Scoring was 0 (never) to 4 (nearly always); a higher score indicated greater burden. 2. Psychological health (depression): The 10‐item Center for Epidemiological Studies Depression Scale (CES‐D) assessed depressive symptoms within the past week. Scoring was 0 (rarely, none of the time) to 3 (most, almost all the time), for a score of 0 to 30; higher scores indicated greater symptoms. 3. Satisfaction:
Outcome data were collected at the end of intervention which was the 12‐month post‐discharge time point. | |
| Notes | For the outcome 'satisfaction', the satisfaction scores from the 19‐item social support items were used in the analysis for this review. The author provided additional information on the interventionist training and outcome data for satisfaction with supports. Funding source: This work was supported by the Veterans Health Administration, Health Services Research and Development Service, US Department of Veterans Affairs with additional support from the Memphis Veterans Affairs Medical Center (p.47). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to assess |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to assess |
| Incomplete outcome data (attrition bias) | Low risk | Overall attrition low, n = 15 (9.7%), Reasons for attrition similar for both groups: Intervention group, N = 8 (refused contact, n = 3; not interested n = 2; illness, n = 1; other reasons n = 2); control group, N = 7 (refused contact, n = 2; illness, n = 3; other reasons n = 2) (p.38 figure 1 and p.39). |
| Selective reporting (reporting bias) | High risk | Physical health outcomes not analysed |
| Other bias | Low risk | No significant group differences reported at baseline and baseline data on outcome measures was similar for both groups (p.40 table 1 and p.41 table 2). |
| Methods | A randomised, treatment/comparison, repeated‐measures experimental design (July 2005‐February 2010) | |
| Participants | Spouse/partner caregivers of stroke survivors, Kansas, USA. Caregivers were included if they were aged 55 years or older, married or married equivalent, living with and caring for a spouse or/partner surviving a first‐ever stroke occurring 6‐36 months before enrolment, could participate by telephone and spoke English. | |
| Interventions | Intervention: Self‐Care TALK (detail on number not available) Mode of delivery: Telephone Aim: To test the effectiveness of a self‐care intervention for older, spouse caregivers of persons with stroke in reducing caregiving strain, promoting caregiver health and well‐being, self‐efficacy related to health, and in reducing depressive symptoms Comparison: No intervention (detail on numbers not available) | |
| Outcomes | 1. Burden: M‐CSI: modified (caregiver strain) 2. Psychological health (depression): CED‐D (depression) 3. Health status and well‐being (physical health): SF‐36 v2, PCS (perceived physical health) 4. Health status and well‐being (self‐efficacy): SRAHP (self‐efficacy for health) No detail available on the scoring system for any of the outcomes Data collection time points: 2 and 6 months post‐enrolment | |
| Notes | The principal investigator Cynthia Teel, University of Kansas School of Nursing, confirmed via email on 27 August 2017 that the trial registration was the only publication for this trial. Study data requested; author replied that no study data were available for inclusion in this review. Funding sources: none stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No detail available |
| Allocation concealment (selection bias) | Unclear risk | No detail available |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | No detail available |
| Incomplete outcome data (attrition bias) | Unclear risk | No detail available |
| Selective reporting (reporting bias) | Unclear risk | No detail available |
| Other bias | Unclear risk | No detail available |
| Methods | Randomised controlled trial (recruitment March 2007‐October 2009) | |
| Participants | Caregivers of persons with stroke at two large rehabilitation facilities in the greater metropolitan area of Stuttgart Germany, and from a statutory health insurance program. Consenting participants included 27 men (22.1%, mean age 69.78 years, SD 9.09) and 95 women (77.9%, mean age 65.13, SD 10.01). The sample comprised native Germans (n = 100, 82.0%), ethnic German repatriates from Eastern European states (n = 10, 8.2%), and individuals with various European migration backgrounds (n = 12, 9.8%). At enrolment, participants, n = 23 (18.9%), had worked while providing care. The caregivers were spouses or partners (n= 106, 86.9%), children (n= 15, 12.3%), or grandchildren (n= 1, 0.8%) of the care‐recipient and had been providing care for a mean period of 28 months (SD 33). During the 3 months before enrolment, they provided care and support in activities of daily living for 1.98 hr (SD 1.70) per day on average, additional support (e.g. preparing meals, buying goods, doing the laundry, providing outdoor assistance) for 3.72 hr (SD 2.32), and supervision due to cognitive impairment (e.g. disorientation, impaired memory, poor judgment) for 1.75 hr (SD 3.62). Fifteen caregivers (12.3%) were also responsible for the care of a second person who had not been enrolled in the study. Care‐recipients included 84 men (68.9%, mean age in years 73.05, SD 7.33) and 38 women (31.1%, mean age in years 73.37, SD 7.89). Thirty‐five stroke survivors (28.7%) had already experienced more than one stroke in the past. Forty‐one care‐recipients (33.6%) had aphasia, 37 (30.3%) had dysphagia symptoms, and 71 (58.2%) were incontinent. | |
| Interventions | Intervention: Problem‐Solving Intervention (PSI) and usual support (n = 60) Aim: To examine the effectiveness of a problem‐solving intervention (PSI) for stroke caregivers who provided care for at least 6 months and who experienced significant strain in their role Interventionist(s): Two clinical psychologists experienced in providing cognitive behavioural interventions with older persons conducted the PSI. Mode of delivery: Telephone Duration: 12 months (an initial in‐home visit, five weekly (month 1), and four biweekly (months 2 and 3) telephone sessions. In the following maintenance period (months 4–12), the second component consisted of another in‐home visit (month 4) and nine monthly telephone sessions. Each call was 60 minutes. Content: During the initial in‐home face‐to‐face session, the interventionist explained the purpose of the intervention in detail and gave a short introduction into the principles of problem‐solving and the written problem‐solving guide. The intervention started with capturing the facts and identifying specific burdensome issues the caregiver was willing to change as a basis for a shared agenda. A card sorting task was used to facilitate problem identification. At the end of the card‐sorting task, the caregiver was asked to select and prioritise the burdensome problems that needed immediate attention. The caregiver was instructed to seek all available facts related to the selected problem and was then assisted in articulating a specific, realistic goal to overcome the identified problem and in determining possible obstacles to meeting the established goal. In the following step, the caregiver was instructed to think of as many possible solutions or obstacles to the problem and to write them on a worksheet. Various techniques were offered to increase the number of alternative solutions. After completing a comprehensive list of possible solutions, caregivers were encouraged to consider the potential outcomes of the chosen solutions and weigh the perceived benefit and feasibility of each on a 5‐point rating scale. The final phase in the problem‐solving process was the act of implementing the chosen and carefully planned solution. The PSI group also received the same monthly information leaflets like the information‐only control group. Standardisation: The therapists were supervised every 6‐8 weeks for 3‐4 hr by the third author, who had access to the protocols of the sessions. During these contacts, all participants in the PSI group were discussed on the basis of the interventionists’ records and in regard to study protocol and adherence, intervention progress, and possible difficulties. If needed, telephone‐based supervision was possible at each point in time. Comparison group: An information‐only control group and usual support. Participants assigned to this group received monthly information letters with care‐specific topics like relaxation, pain, depression, and nutrition, as well as addresses for supporting services or groups in the region corresponding to available written material offered by health insurances or local information centres. They also received the usual support that was regulated by law and the various benefits provided by the compulsory long‐term care insurance (n = 62). | |
| Outcomes | 1. Psychological health (depression): The 20‐item Center for Epidemiological Studies–Depression Scale (CES–D). Total scores range from 0 to 60. A score of 16 or higher was used as an indicator of clinical severity. 2. Skill acquisition (competence): The Sense of Competence Questionnaire (SCQ). The SCQ contains 27 items, each rated on a 4‐point scale. The three domains of the SCQ — satisfaction with the stroke patient as a recipient of care, satisfaction with one’s own performance as a caregiver, and consequences of involvement in care for the personal life of the caregiver — have been confirmed for informal caregivers of older adults with diagnosed stroke. A higher total score indicated a greater sense of competence or with a reversed scaling, a higher burden. Total scores ranged from 27 to 135. 3. Skill acquisition (problem‐solving): The short version of the Social Problem‐Solving Inventory–Revised (SPSI ‐R). The SPSI–R:S has 25 items that are rated on a 5‐point scale ranging from 0 (not very true of me) to 4 (extremely true of me). The total score ranges from 0 to 100. Two constructive dimensions (positive problem orientation (PPO), rational problem‐solving (RPS)) and three dysfunctional dimensions (negative problem orientation (NPO), impulsivity/carelessness style (ICS), and avoidance style (AS)) can be differentiated. The total score serves as a global index of problem‐solving ability. Higher scores indicated better problem‐solving abilities. 4. Health status and well‐being (physical health): Physical complaints were assessed with the Giessen Subjective Complaints List. The intensity of each complaint is rated on a 5‐point scale, ranging from 0 (not existing) to 4 (strong). The scores of the 24 items are summed to a total score (from 0 to 96). Higher scores indicated greater physical ill‐health. 5. Satisfaction:
Outcome data were assessed at baseline (T0), following the intensive intervention period at 3 months (end of intervention) and after the maintenance period at 12 months. | |
| Notes | We used the 3‐month outcome data because the maintenance period included a second in‐home visit at month 4 which is not consistent with the review's inclusion criteria. Funding source: Grants of the GKV‐Spitzenverband (National Association of Statutory Health Insurance Funds) Berlin, Germany (p.628) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated – remote location (p.631) |
| Allocation concealment (selection bias) | Low risk | Remote randomisation centre provided by an "...independent randomisation center at the University of Tübingen" (p.631) |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome "Assessors were trained research assistants who were blind to the treatment condition ..." (p.631) |
| Incomplete outcome data (attrition bias) | Low risk | Overall attrition low: intervention n = 2 (death of care‐recipient, n = 1, and moved outside the region, n = 1); control n = 4 (death of care‐recipient, n = 1 and discontinued participation, n = 3) (Figure 1, p.630) |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported (Table 2, p.637) |
| Other bias | Low risk | "At pretreatment, PSI and control groups evidenced no significant differences (P > .05) on demographic characteristics or primary and secondary outcomes" (see Table 2) (p.636). "More caregivers in the control condition than the PSI group received ambulant therapies like physiotherapy, massage or sports therapy ...and had relatives, friends or neighbours who assisted care‐recipients in ADL‐related tasks ... there was a trend for a greater use of home care services for ADL assistance and a higher rate of aphasia among the care‐recipients in the PSI group ..." (p.636). |
| Methods | A mixed‐method design with random assignment (pilot study) (Study dates not reported) | |
| Participants | African‐American caregivers of people with heart failure recruited from an outpatient cardiology HF follow‐up clinic in a Midwestern Medical Centre, USA. Caregivers were spouses (65%, N = 13) of patients or were other family members (35%, N = 7), i.e. sister, parent, daughter or granddaughter. Of 20 dyads, 15 (75%) lived in the same household, while 25% (5 dyads) lived separately. Ten caregivers were assigned to the intervention group and 10 to the standard care group. Caregiver age ranged from 40‐78 years with a mean age of 61.4 years (SD 10.0). The majority, n = 17 (85%), were female, 8 (40%) high school or lower, 12 (60%) vocational, college or more. The majority were married, 14 (70%), and employed, 12 (60%). Seven caregivers in the intervention group had vocational or higher education versus 5 in the standard care group. Caregivers reported their chronic health conditions: hypertension (n = 11), myocardial infarction or cardiovascular disease (n = 4), diabetes mellitus (n = 4), osteoarthritis/pain (n = 4), and one caregiver each reported the conditions of depression, thyroid problems, asthma, and HIV. | |
| Interventions | Intervention: The adapted FamHFcare coaching intervention plus standard care (n = 10). Aim: To test whether a culturally‐sensitive telephone coaching intervention could reduce patients’ HF‐related re‐hospitalisation and family caregiver burden and depression, and increase family caregiver confidence, social support, and preparedness to care Interventionist(s): Experienced nurse interventionist Mode of delivery: Telephone Duration: 4 weeks (weekly calls 60‐90 minutes depending on caregiver questions and need for reinforcement). Content: FamHFcare includes 4 weeks of post‐hospital coaching via telephone on specific HF home care skills using teach‐back strategies. FamHFcare aligns with all ACCF/AHA clinical guideline based instructions for daily sodium/fluid restrictions, medication adherence, and symptom monitoring and reporting. Prior to the first telephone session, each family received the coaching program materials by mail: (1) two AHA home caregiving guides (symptoms checklist and staying healthy guidelines for caregivers); (2) a list of local support organizations; (3) the national award winning book Comfort of Home for Chronic Heart Failure: A Guide for Caregivers; (4) low‐sodium booklet, and (5) a plastic daily pill organiser. The nurse interventionist engaged each dyad in four weekly FamHFcare coaching sessions scheduled at their convenience. Standardisation: no details provided Comparison group: Standard care. This included the education and materials routinely given to all HF patients through hospital discharge planning. The standard medical and nursing clinical care in both groups was not changed for this study. Standard care information is not specific to the needs of African‐Americans or to caregivers (n = 10). | |
| Outcomes | 1. Burden: a 17‐item five‐point Likert‐type scale in which higher scores indicated more burden or difficulty in providing caregiving. Response options were: 1 = providing caregiving but the task was not difficult to 5 = extremely difficult. Option “N/A = not applicable” was provided and selected by caregivers who did not provide a specific caregiving task. Higher scores indicated greater perceived burden. 2. Psychological health (depression): The Center for Epidemiologic Studies Depression Scale (CES‐D). A higher score indicated higher level of depression. 3. Skill acquisition (preparedness to care): A one‐item Likert type scale (1 = not at all, 4 = very well prepared); higher scores indicating caregivers felt better prepared. Outcome data were collected at 6 months (medium‐term follow‐up > 3 to ≤ 6 month time point). | |
| Notes | Author provided detail via email, which was used in the evaluation of the quality of the intervention, for example, detail on monitoring of delivery of the intervention and adherence to trial protocol. Funding source: Award from Kansas City Life Science Institute, Blue Cross Blue Shield, Kansas City, Kansas (p.466). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make assessment |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make assessment |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | "Data collectors were trained research nurses who were blinded to random assignment" (p.468) |
| Incomplete outcome data (attrition bias) | Low risk | Minimal attrition (Intervention: 2 withdrew after completing and evaluating the first two intervention sessions (one was too ill to continue and the other had a busy work schedule); Control group: 1 patient died) (p.470) |
| Selective reporting (reporting bias) | Low risk | None evident – all caregiver outcomes reported in Table 3 (p.471) |
| Other bias | Low risk | No statistically significant differences were found for caregivers or patients (p.469). |
| Methods | A randomised 2‐group design (June 2008‐April 2013) | |
| Participants | Caregivers of adult patients with traumatic brain injury (TBI) from an inpatient rehabilitation unit of a level I trauma centre, Washington, USA. Caregiver age ranged from 19 to 89 years (mean 49.7; SD 13.5). The sample comprised of 82% female, 18% male, of which 79% were of a white non‐Hispanic race and 69% were married. The majority of caregivers had post‐high school education (75%), with employment ranging from working full‐time at time of injury (49%); working part‐time (18%); student (not working) (1%); unemployed (5%) and not in workforce or other (27%). Most were spouses or partners (54%) of the care‐recipient and 35% were parents. | |
| Interventions | Intervention: An individualised education and mentored problem‐solving intervention plus usual care (n = 77). Aim: To investigate the effect of a solely telephone‐based, individualised, combined education and problem‐solving intervention on the quality of life (QoL) and emotional well‐being of caregivers of persons with moderate to severe TBI. Interventionist(s): A master’s level social worker with experience in prior studies of TBI and problem‐solving treatment approaches. Mode of delivery: Telephone Duration: Planned maximum 10 calls (20 weeks), with a target of 8 calls and 2 additional calls at the caregiver’s discretion. Content: The experimental intervention combined education and mentored problem‐solving for topics relating to caregiving and TBI recovery and management (in addition to usual care). The focus of the intervention was on self‐management of issues by the caregivers through applied problem‐solving rather than the provision of solutions or direction to resources, or both, by study personnel. The study interventionist began each call by asking open‐ended questions to ascertain what, if any, issues had arisen or had been resolved since the last call. The caregiver was then asked to identify the concern that he or she wished to address on the call. The final choice of the concern(s) to be targeted on each call was left up to the caregiver, with no requirement to address a new issue or a previously targeted one with action plans in progress. The interventionist then mentored the caregiver in a problem‐solving approach aimed at addressing the concern. Standardisation: No details provided, only one interventionist Comparison group: Usual care (n = 76) | |
| Outcomes | 1. Quality of life: Adapted Bakas Caregiving Outcomes Scale (BCOS), a 15‐item, 7‐point scale that measures change in social functioning, emotional well‐being, and physical health related to caregiving. Higher scores reflected better quality of life. 2. Psychological health (depression): Brief Symptom Inventory (BSI‐18), an 18‐item instrument designed to quantify symptoms of somatisation, depression, and anxiety. Respondents use a 5‐point Likert scale to indicate the extent to which each symptom bothered them over the preceding 2 weeks. Higher scores indicated greater symptoms of depression. 3. Psychological health (coping): Modified Caregiver Appraisal (MCA); higher scores indicated better coping. 4. Health Status and Well‐Being (social activity): The PART‐O (Participation Assessment with Recombined Tools–Objective) as a measure of community participation; higher scores indicated greater social activity. 5. Knowledge and understanding (knowledge): No instrument specified, stated structured interview and Likert ratings; no detail provided on the scoring system Data were collected at the end of intervention which was 6 months after discharge of the survivor to the community. | |
| Notes | Funding source: Funded by the Department of Education, National Institute on Disability and Rehabilitation Research, TBI Model Systems: University of Washington Traumatic Brain Injury Model System (H133A070032) (p.180). Author confirmed that the abstract was linked to the study. Additonal information requested from the author but not provided at the time of submission of this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated (p.182) |
| Allocation concealment (selection bias) | Low risk | Password‐protected database, "The study coordinator entered identifying information into the database and was given the group assignment (p.182). |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | "An examiner blinded to the group allocation conducted the follow‐up assessments..." (p.182). |
| Incomplete outcome data (attrition bias) | Unclear risk | Sample size estimates allowed for a 10% loss to follow‐up. Loss to follow‐up, however, was greater, and there was an imbalance in loss to follow‐up across the groups (23% in the intervention group and 13% in the control group). Withdrawn from the intervention group (n = 4); withdrawn from the control group (n = 0) (Figure 1, p.185). |
| Selective reporting (reporting bias) | High risk | Unclear how or if the prespecified secondary outcome of knowledge was reported; satisfaction not assessed due to insufficient responses at follow‐up (Table 4, p.187) |
| Other bias | High risk | Fewer caregivers in the intervention group providing direct financial support which could potentially influence outcome measures of QoL and emotional well‐being (p.185) |
| Methods | A parallel randomised trial (April 2010‐March 2013) | |
| Participants | Caregivers of consenting people with gastrointestinal cancers receiving treatment at one of four metropolitan hospitals in Sydney, Australia, for a newly diagnosed or recurrent primary upper GI cancer, metastatic liver disease, or stage 4 colorectal cancer. Caregivers were recruited either during the patient’s hospital admission or within 2 weeks of patient discharge. Mean caregiver age in years was 54.18 (SD 13.5) and most were female (n = 93, 73%); male (n = 35, 27%). Relationship to care‐recipient was spouse or partner (n = 89, 69.5%), child (n = 29, 22.6%), parent (n = 3, 2.3%), sibling (n = 3, 2.3%), other family member (n = 1, < 1%), and friend (n = 3, 2.3%). Education ranged from none or primary (n = 6, 4.7%), intermediate certificate year 10 (n = 24, 19%), leaving certificate or year 12 (n = 20, 15.6%), technical certificate or diploma (n = 33, 25.8%), tertiary (n = 45, 35.1%). Most were employed full‐time (n = 56, 43.7%), part‐time (n = 21, 16.4%), retired (n = 28, 21.9%), unemployed (n = 5, 3.9%), or engaged in home duties (n = 18, 14.1%). | |
| Interventions | Intervention: The Family Connect intervention (n = 64) Aim: To investigate the effectiveness of a standardised, telephone‐based intervention to improve caregivers’ QoL in the first 3 months following a patient’s discharge from hospital. Secondary aims included evaluating the interventions effectiveness in reducing caregivers’ unmet supportive care needs, caregiver burden, and distress. The study also aimed to establish whether a caregiver‐focused intervention could also indirectly reduce patient distress, unmet need, and unplanned hospital presentations to improve overall patient QoL. Interventionist(s): Experienced healthcare professionals (clinical psychologists with training in clinical aspects of cancer care) Mode of delivery: Telephone Duration: 10 weeks (biweekly for the first 3 calls and one month later the final call, mean call length ranged from 32 minutes at 2 weeks to 17 minutes at 10 weeks) Content: The intervention involved a manualised, standardised assessment of caregiver need across the domains of patient care, maintaining family relationships and emotional and physical self‐care, as well as an assessment of information and practical needs. Within each of these domains, the manual provided a list of resources and strategies that might address identified needs, to guide the health professionals delivering the intervention. The resources provided and the level of discussion that was related to management strategies were tailored to individual caregiver needs. Strategies were based on published evidence and clinical experience. Standardisation: All intervention calls were recorded. Recordings were used during regular sessions to provide support and further training to intervention staff and for quality assurance purposes to confirm intervention fidelity. The intervention fidelity was assessed throughout the study and remained high Comparison group: Usual care (n = 64) | |
| Outcomes | 1. Quality of life: The Short Form (SF)‐12 v2, a 12‐item QoL questionnaire with two subscales that assesses physical and mental well‐being; higher scores indicated better quality of life. 2. Burden: Caregiver Reaction Assessment (CRA), a 26‐item questionnaire which comprises five subscales (disrupted schedule, financial problems, lack of family support, health impact, and impact on self‐esteem). Higher scores indicated greater burden. Outcome data were assessed at 3 (end of intervention) and 6 months post‐hospital discharge (short‐term time point ≤ 3 months) using self‐administered mailed questionnaires. | |
| Notes | The study did not specify that the intervention group also received usual care. Usual care was not defined. Following email communication with the originators of the burden instrument (CRA), the subscale result for 'schedule disruption' was used in the analysis for this review. For the QoL outcome data, the result from the physical health subscale was used. The authors used a substitution method to impute the data for the entire sample and that is why the number 64 was used (confirmed via email November 2017). Authors confirmed the study outcome data collection time point and provided further detail on the study and intervention. Funding source: The study was funded by the National Health Medical Research (NHMRC) Project Grant 632645 (p.594). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "... computer generated randomisation list" (p.587) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to assess |
| Incomplete outcome data (attrition bias) | Low risk | Attrition balanced across groups (19% versus 17% at 6 mths; and reasons given (Figure 1, p.589) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported (Table 3, p.592) |
| Other bias | Low risk | Baseline characteristics were similar for both groups. Demographic and clinical characteristics for participating and non‐participating patients were similar, although non‐participating patients were slightly older (p.588 and Table 1, p.590), table 2, p.591). |
| Methods | A randomised controlled trial design (recruitment May 2011‐May 2012) | |
| Participants | Caregivers of people with colorectal cancer recruited from the colorectal cancer clinic of Queen Mary Hospital in Hong Kong. Caregivers were caring for a family member diagnosed with colorectal cancer in the preceding four weeks, were at least 18 years old and spoke Cantonese. Domestic helpers, those who were cognitively impaired, and those who did not speak Cantonese were excluded. Caregivers age ranged from 19‐86 years; mean age in years was 54 (SD = 14.6). Most were females (n = 103, 74%) and 37 men comprised 26% of the sample. Education ranged from Illiterate (n = 14, 10%), primary (n = 37, 26%), secondary (n = 69, 49%), tertiary (n = 19, 14%), doctorates (n = 1, < 1%). Monthly family income in Hong Kong dollars (£) for the entire sample (n = 140) ranged from, less than 10,000 (769) (n = 55, 39.28%), 10,001‐20,000 (770‐1,539) (n = 42, 30%), 20,001‐30,000 (1,540‐2,307) (n = 26, 18.57%), 30,001‐40,000 (2,308‐3,079) (n = 8, 5.71%), 40,001‐50,000 (3,080‐3,846) (n = 9, 6.4%). | |
| Interventions | Intervention: Nurse‐led, telephone, psychoeducation programme plus usual care (n = 70) Aim: To evaluate the efficacy of the programme in reducing depression, anxiety, stress and burden of care among caregivers of patient with colorectal cancer Interventionist(s): Colorectal nurse specialist Mode of delivery: Telephone Duration: Five weeks (three structured telephone calls to the caregivers at 1, 3, and 5 weeks after discharge. Each call lasted no longer than 45 minutes). Content: The calls sought to understand the caregivers’ situation and identify their problems so that information, as well as education and psychosocial support, could be provided. The interval between telephone calls and the content of the intervention followed a telecare protocol called individual support condition (Taylor 2008). Each call began with an enquiry about the patient’s and carer’s general condition. Specific caring problems or psychological issues were identified, and related information or psychological support was given to caregivers. The nurse also provided education to caregivers according to the patient’s needs at different recovery stages. Before the end of the call, the nurse asked about any additional problems and ensured that caregivers’ needs had been met. Standardisation: The content of the telephone checklists and field notes were reviewed regularly to ensure accuracy and consistency and conversations were documented. Comparison group: Caregivers received routine education on home care on discharge using an information sheet. In addition, a telephone help line number was provided (n = 70). | |
| Outcomes | 1. Quality of life: The World Health Organization Quality of Life Measure‐BREF (WHOQoLBREF) Hong Kong (HK) was used to assess quality of life and consists of 28 items covering four domains: physical health, psychological health, social relationships and environment. Higher scores indicated better quality of life. 2. Burden: The Chinese version of the Zarit Burden Scale is a 22‐item, self‐report inventory that measures carer burden. Each question was scored on a five‐point Likert scale, ranging from 0 for ‘never’ to four for ‘nearly always present’. The total score ranged from 0 to 60, with a higher score indicating greater burden. 3. Psychological health (depression, anxiety and stress): The Chinese version of the Depression, Anxiety and Stress Scale‐21 (DASS‐21) (a self‐report instrument that measures a patient’s state over the preceding week). It consists of 21 items, spread equally across three scales: depression, anxiety, and stress. Each item uses a four‐point Likert scale, ranging from 0 (‘did not apply to me at all’) to three (‘applied to me very much, or most of the time’). For depression, a score less than nine was regarded as normal, 10‐13 as mild, 14‐20 as moderate, 21‐27 as severe, and higher than 28 as extremely severe. For anxiety, a score less than seven was regarded as normal, 8‐9 as mild, 10‐14 as moderate, 15‐19 as severe, and higher than 20 as extremely severe. For stress, a score less than 14 was regarded as normal, 15‐18 as mild, 19‐25 as moderate, 26‐33 as severe, and higher than 37 as extremely severe. Outcome data were collected at week 2 (end of intervention), 4, and 8 weeks (short‐term time point) after the intervention. | |
| Notes | Funding sources: none stated For the QoL outcome, the physical health subscale result was used in the analysis for this review. Additional information requested on the published registered trial. The author responded to the queries and emailed the linked published paper. Additional data were requested in October 2018 but these data have not been provided by the author. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A person not involved in participant recruitment generated the randomisation schedule ..." (p.32) ‐ detail of method not provided. |
| Allocation concealment (selection bias) | Low risk | "...sequentially numbered, sealed, opaque envelopes..." (p.32) |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | "The research nurses responsible for carrying out the interviews were masked to the treatment assignment" (p.32). |
| Incomplete outcome data (attrition bias) | Low risk | Details not provided in the paper, figure 1 (p.33); attrition minimal and accounted for |
| Selective reporting (reporting bias) | Low risk | All outcomes reported upon (Page 8, table 2&3) |
| Other bias | Low risk | No significant differences in baseline characteristics of the caregivers (p.4 and 5, table 1) |
| Methods | A randomised study (study dates not reported) | |
| Participants | Ninety‐seven caregivers of frail older persons, adult child caregivers (n = 61) and spouse caregivers (n= 36) from a 16‐county area that included urban, suburban, and rural settings, New York, USA. Participants were recruited via newspaper advertisements, direct mailings, appearances before civic and religious organisations, radio announcements and referrals from geriatrics professionals. Caregivers were included if they had a minimum score of 7 or higher on the Caregiver Strain Index. Care‐recipients had to exhibit two or more activities of daily living (ADL)/instrumental activities of daily living (IADL) impairments as reported by the caregiver. Thirty‐one adult child caregivers and 33 spouses received the intervention. The mean adult child caregiver age in years in the intervention group was 54 and in the control group was 54.9. Years spent in education was 14.3 for the intervention group and 15 for the control group. Most were female (77.4% in the intervention group and 96.7% in the control group). Male caregivers accounted for 22.6% in the intervention group and 3.3% in the control group. Most were of white race or ethnicity (87.7% in the intervention group and 96.7% in the control group); black race or ethnicity accounted for 12.9% of the intervention group and 3.3% of the control group. Relationship status ranged from married (intervention group 35.3%, control group 46.2%), single/never married (intervention group 17.6%, control group 23.1%), divorced (intervention group 29.4%, control group 30.8%), separated (intervention group 11.8%, control group 0%) and widowed (intervention group 5.9%, control group 0%). The mean spouse caregiver age in years in the intervention group was 70.2 and in the control group was 66.2. Years spent in education was 14.1 for the intervention group and 14.3 for the control group. Most were female (86.4% in the intervention group and 92.9% in the control group). Male caregivers accounted for 13.6% in the intervention group and 7.1% in the control group. Most were of white race or ethnicity (90.5% in the intervention group and 85.7% of the control group); black race/ethnicity accounted for 9.5% of the intervention group and 7.1% of the control group. Relationship status ranged from married (intervention group 95.2%, control group 100%), single/never married, divorced, separated, and widowed (0% across groups) and 'other' accounted for 4.8% of the intervention group and 0% of the control group). | |
| Interventions | Intervention: The telephone support group (TSG) intervention (group‐delivered) (n = 31) Aim: To evaluate the effectiveness of a telephone support Interventionist(s): License Master’s prepared social worker (who had several years of clinical geriatric social work experience) led all groups. Mode of delivery: Telephone Duration: Weekly for 12 weeks. Each weekly session lasted 90 minutes (15 minutes for hook‐up and 75 for group meeting). Content: A multicomponent intervention that includes education about the effects of chronic illness and about emotion‐focused coping strategies, problem‐solving, and support. A leader’s manual and a participant workbook was developed. The leader’s manual was used to train the group leader and a workbook was given to each member in the TSG arm of the study. The leader instructed members to turn to the appropriate pages in the workbook each week during telephone meetings and to follow along using the structured agendas and the educational materials provided. The first half of each weekly meeting began with conference call connections using a voice‐over internet provider. After the initial period in which the leader called each member in turn, the group leader gave a brief overview of the previous meeting. Following this was a ‘‘check‐in’’ with group members regarding their progress on target goals between meetings. In order to help group members develop supportive relationships beyond the TSG program, the leader asked each of them to select a telephone buddy to call between group meetings. Conversations between telephone buddies were to focus on caregiving issues and the coping and problem‐solving skills that participants were learning. Emotion‐focused coping strategies were taught and practiced during the first half of each weekly TSG meeting. The group leader introduced problem‐focused coping skills during the second half of each meeting and practised them with the members. Standardisation: Delivery was monitored, with one interventionist for all groups, and a leaders manual was used to train the group leader. Comparison group: Usual services offered by the senior services centre (n = 30) | |
| Outcomes | 1. Burden: Zarit Burden Interview (ZBI), a 22‐item Likert‐type scale that measures the total strain, role strain, and personal strain that caregivers experience as a result of the impact of the patient’s disabilities on their life. For each item, caregivers indicate how often they have felt a certain way: (0) never, (1) rarely, (2) sometimes, (3) quite frequently, or (4) nearly always. Higher scores signified greater burden. 2. Psychological health (depression): Center for Epidemiologic Studies–Depression Scale (CES‐D). Respondents were asked how frequently they had experienced 20 different events in the past 7 days. These events were indicative of depression. Each event had a score of 0 (happened rarely or not at all) to 3 (most or all of the time). Higher scores indicated more depression. 3. Psychological health (anxiety): State–Trait Anxiety Inventory (STAI) —This scale measures anxiety for caregivers. It presents 20 statements that people use to describe themselves and asks caregivers the extent to which they agree (4) or disagree (1) with each statement. The final score is a summary of the answers to the 20 statements. Higher scores indicated more anxiety. 4. Skill acquisition (problem‐solving): Pressing Problems Index (PPI). Researchers developed the 18‐item PPI in order to assess the extent to which participants’ health and social service problems were being addressed. The PPI contains a list of problems that caregivers frequently encounter when caring for a family member with a chronic illness. For each problem, we asked the caregiver how stressful the problem was, from (0) not at all to (4) extremely; how much their stress had changed, from ‐3 (much worse) to 3 (completely better); how effective they had been in dealing with this problem, from 0 (not at all effective) to 4 (extremely effective); and how much their effectiveness had changed from ‐3 (much worse) to 3 (completely better). Higher scores indicated better problem‐solving. 5. Knowledge and understanding (knowledge): the 'Community Services Inventory' subscales (of services and how to access them); higher scores indicated greater knowledge. Outcome data were collected at the end of intervention and within 2 weeks of completing the intervention. | |
| Notes | For the outcome 'problem‐solving', the reported results for 'how effective' were used in the analysis for this review. Mean scores for the two subscales of the 'Community Services Inventory' subscales were used for the analysis. Unpublished data was requested; the author replied on 11 October 2017 stating that the data was no longer available. Funding source: Project supported in part by United States Administration on Aging Grant (p.620) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to assess |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | "Interviewers remained blind to the participants’ assigned condition ..." (p.622). |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information on post‐test data to assess |
| Selective reporting (reporting bias) | High risk | Adult children subsample only, reported as this group ‘drove the overall effects’ (p.625) |
| Other bias | High risk | Adult child demographics showed significant differences between groups in terms of education with the control group having more years of education than intervention group (table 3, p.626). |
| Methods | Parallel group, single‐blind, randomised controlled trial (recruitment April 2015‐November 2015) | |
| Participants | Caregivers of older people discharged from the medical assessment unit within a metropolitan tertiary hospital in Western Australia with over 600 beds. Caregivers were recruited in the hospital at the time of patient discharge. A family caregiver was defined as a family member or friend who provides unpaid personal care, support, and assistance. Inclusion criteria for dyads were that they comprised a patient aged 70 years or older being discharged to their home or the home of their family caregiver, plus a family caregiver who could speak and read English. Caregiver mean age in years for the intervention group was 63.1 (12.6 SD) and the control group 61.3 (13.4 SD). Females comprised 74% (n = 104) and males 26% (n = 37). Relationship to care‐recipient was husband (n = 13), wife (n = 29), son (n = 62), daughter (n = 14) and other (n = 104). | |
| Interventions | Intervention: Further Enabling Care at Home (FECH) program and usual discharge care (n = 86). Aim: The FECH intervention is intended to identify family caregivers of older patients during the hospital admission, help ensure their understanding of discharge information that has implications for the caregiving role, prompt reflection by the caregiver on this role and what is needed to help sustain this, and guide the caregiver as they identify and address prioritised needs for support (information provided by author via email). Interventionist(s): A nurse with acute care knowledge relevant to the care of older people in poor health, knowledge of how to access local services, understanding of the family caregiver role, the capacity to work flexible hours to fit in with caregivers’ needs, and the skills to support the caregiver during the process of reflection and self‐assessment. Mode of delivery: Telephone Duration: Up to 40 days (planned calls were delayed). Planned calls were weekly to biweekly (call 1: within a week post‐discharge, call 2: 7‐10 days post‐discharge, call 3: 14 days after discharge). Actual call delivery: call 1 within and up to 9 (instead of 7), contact 2 within 24 (instead of 10) and contact 3 within 40 (instead of 14), days post‐discharge. Mean and standard deviation call contact time in minutes was contact 1: 15.4 (9.6), contact 2: 59.7 (24.1) and contact 3: 28.3 (17.7). Content: The Further Enabling Care at Home program involved the implementation of a strict telephone protocol by the specially trained nurse, using the Carer Support Needs Assessment Tool, which has fourteen items covering: (a) support that enables the caregiver to care for the patient at home, and (b) support for the caregiver in their caring role. There were three, sequential, telephone contacts. Contact 1 was planned to take place within a week post‐discharge. Contact 2 was designated to occur from 7 to 10 days post‐discharge. Contact 3 was planned to follow within 14 days of the discharge. Standardisation: The delivery of the intervention was monitored at regular meetings with investigators responsible for this issue. Field notes were taken by the FECH nurse during intervention contacts to provide a record that allowed the discussion of cases during these meetings so that fidelity could be assured. Using this process, intervention delivery was as planned and consistent, except with respect to the planned time of the contacts, which were delayed in some instances because of the busy schedules of the caregivers. The selection and preparation of the FECH nurse, plus the use of a pre‐prepared resource manual, also helped to ensure the standardised quality of the intervention (information provided by author via email). Comparison group: Usual discharge care (n = 89). | |
| Outcomes | 1. Burden: Caregiver strain subscale of the Family Appraisal of Caregiving Questionnaire – Palliative Care; higher scores indicated greater burden. 2. Skill acquisition (preparedness to care): Preparedness for Caregiving Scale from the Family Care Inventory; higher scores indicated better perceived preparedness to care. 2. Family functioning: Family Well‐Being subscale of the Family Appraisal of Caregiving Questionnaire – Palliative Care; higher scores indicated better family functioning. 3. Health status and well‐being (physical health): SF‐12 v2 Health Survey used for assessing physical health and not as a QoL outcome (caregiver ratings of their own health and well‐being). Higher scores indicated better physical health. Cost: No specific instrument (intervention costs recorded include (i) nurse time for the duration of each contact; (ii) nurse time to implement and organise resources; (iii) nurse time to write notes following each contact for each patient‐carer dyad; (iv) cost of training the FECH nurse; (v) telephone charges; and (vi) stationary and postage costs. Costs in the control group were estimates of nurse time for usual discharge procedures). Higher scores indicated greater cost. Outcome data were collected at Time 1 (within 4 days of discharge), Time 2 (15–21 days after discharge) and Time 3 (end of intervention time point, six weeks after discharge). | |
| Notes | Unpublished mean and standard deviations along with details of the cost data collected were obtained from authors via email. Author confirmed via email that care‐recipients may have included those with an exacerbation of a chronic condition or an additional acute illness or both. Funding source: A Department of Health Western Australia, SHRAC Research Translation Project grant (p.40). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated list of random allocations prepared prior to the study commencing, using a permuted random blocks strategy (p.35) |
| Allocation concealment (selection bias) | Low risk | Allocation schedule held by researcher not involved in recruitment (p.35) |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | All researchers involved in quantitative data collection were blinded to the allocation schedule and actual group assignment (p.35). |
| Incomplete outcome data (attrition bias) | Low risk | Attrition Intervention group 19.5%; control group 8.1% (p.37). “From the 12 dyads withdrawing after randomisation without providing data, most failed to provide a reason but three caregivers had concerns about, or difficulties with, the planned telephone data collection and one experienced a bereavement (p.37)”. |
| Selective reporting (reporting bias) | High risk | Physical and mental health outcomes not reported |
| Other bias | Low risk | No significant difference in caregiver characteristics between the groups (p.37) No significant differences in baseline measures for outcomes (Table 2, p.38; table 3 page 39) |
| Methods | A randomised controlled trial (study dates not reported) | |
| Participants | Caregivers of people with dementia recruited from memory disorder clinics, support groups, and newspaper or television advertisements in the Southern New England region of the United States of America. Caregivers were aged 21 years or older; lived with a relative with dementia in the community; and provided a minimum of four hours of supervision or direct care per day for at least six months prior to enrolment. Sixty caregivers were enrolled in the study at baseline, with 32 assigned to the treatment condition and 28 assigned to standard care. By the 12‐month assessment point, 33 caregivers had data for analysis, with 16 caregivers in the FITT‐D group and 17 caregivers in standard care. There were 20 spousal caregivers and 13 adult child caregivers. Caregiver age ranged from 41‐87 years with an overall group mean of 63.30 years (SD 11.836). The majority were female (n = 26) and male (n = 7). Both groups were similar in terms of years of education; mean caregiver years of education in the intervention group was 14.22 (3.41) and in the control group 15.88 (2.14). | |
| Interventions | Intervention: Family Intervention: Telephone Tracking – Dementia (FITT‐D) plus a binder containing local resource information (e.g. list of support groups, adult day care centres) and educational material from the Alzheimer’s Association (n = 32) Aim: To examine the preliminary efficacy of FITT‐D, a multicomponent intervention that is delivered in 23 telephone contacts over 12 months Interventionist(s): Master’s level therapists (counsellors, nurses, social workers – confirmed by author email) Mode of delivery: Telephone Duration: One year (one initial call, then weekly for 6 weeks, 12 additional contacts every 2 weeks and 4 monthly termination calls. Initial contacts lasted 60 minutes, follow‐up contact 15‐30 minutes giving approximately 12 hours of contact between the therapist and caregiver). Content: The calls focused on providing emotional support, directing caregivers to appropriate resources, encouraging caregivers to attend to their own physical, emotional and social needs, and teaching caregivers strategies to cope with ongoing problems. The intervention addressed a broad range of issues and problems related to caregiving. The FITT method consists of two stages. The initial stage, orientation and psychoeducation, involved providing caregivers with a rationale for the FITT, an introduction to educational and resource materials, a description of what would happen during future phone contacts and an assessment of key areas thought to be instrumental in addressing caregiver burden and mental health (i.e. caregivers’ health, functioning, mood, thinking, and family life). The psychoeducation component of this initial stage involved reviewing information about dementia and common psychological, emotional, psychosocial, and medical effects of caregiving. The second stage, follow‐up, involved weekly and biweekly contacts in which new problems were identified, positive and negative changes in caregivers or care‐recipients were discussed, and psychoeducational information was reviewed and applied for particular situations. The initial and follow‐up calls were structured around assessment of key areas of functioning in both the caregiver and care‐recipient. Specific interventions were applied at therapists’ discretion, including supportive approaches (i.e. empathy, giving permission, normalising, provision of information, validation, or venting) or more active strategies (i.e. bibliotherapy, interpretation, positive reframing, problem‐solving, reference to resource packet, referral, and setting task directives). The final four follow‐up calls (monthly) addressed issues of termination by allowing caregivers to anticipate FITT contacts coming to an end and to foster reliance on the support network established during the intervention. Standardisation: The two therapists were trained in the FITT‐D procedure and were required to achieve at least 80% correct on a 50‐item multiple choice test about dementia and the FITT treatment manual prior to initiating treatment. Doctoral staff supervised therapists weekly to ensure adherence to the protocol and minimise drift. Comparison group: No telephone intervention. They received a binder containing local resource information e.g. list of support groups, adult day care centres, and educational material from the Alzheimer’s Association (n = 28). | |
| Outcomes | 1. Quality of life: SF‐36 General Health; higher scores indicated better quality of life. 2. Burden:
3. Psychological health (depression) Geriatric Depression Scale (GDS). The GDS is a 30‐item self‐report yes/no measure that is designed specifically for older adults by excluding somatic signs and symptoms of depression. Total scores range from 0 to 30. Higher scores indicated depression. 4. Knowledge and understanding: Alzheimer’s Disease Knowledge Test; higher scores indicated greater knowledge. 5. Health status and well‐being (self‐efficacy): Self‐Efficacy Scale; higher scores indicated greater self‐efficacy. 6. Satisfaction with the intervention: Treatment satisfaction, caregivers in the FITT‐D group completed a 12‐item treatment satisfaction questionnaire. Higher scores indicated greater satisfaction. Date were collected at 12 months (end of intervention) via face‐to‐face assessments with caregivers at their homes. | |
| Notes | For the outcome burden, the results from the Revised Memory and Behavior Problem Checklist (RMBPC) are used in this review. Funding source: Grant from National Institute of Mental Health (MH62561; G.Tremont, PI) (p.516). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Urn randomisation (p.507) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Research assistants were blinded to group membership (p.507). |
| Incomplete outcome data (attrition bias) | High risk | Intervention group: n = 15 (47%) (n = 11 due to death of care‐recipient); control group: n = 12 (43%) (n = 4 due to death of care‐recipient) (p.511) |
| Selective reporting (reporting bias) | High risk | Provided results on the main outcomes (burden and depression) and reported on the additional measure to address secondary goal of the intervention but did not report actual statistics for QoL, self‐efficacy, knowledge, and satisfaction with the intervention (p.513). |
| Other bias | Low risk | No baseline imbalances (Table 1, p.511). Analysis of differences between those who completed and did not complete the 12‐month assessment and whose care‐recipients had died showed that care‐recipient age was the only statistically significant difference between the groups (p.511). |
| Methods | Randomised controlled trial (pilot study) (November 2014 ‐December 2015) | |
| Participants | Non‐professional caregivers of people with various conditions recruited from an official register of caregivers maintained by the Ministry of Labor and Welfare of the Government of the Autonomous Community of Galicia to North West Spain. Conditions included: diseases of the musculoskeletal system, connective tissue, cardiovascular and respiratory (19.7%, n = 12), chromosomal, congenital and perinatal abnormalities (23.0%, n = 14), mental disorders, neurological diseases, brain damage (18.0%, n = 11), dementia (39.3%, n = 24). Caregiver mean age was 58.4 (SD 8.0, range 42‐75 years). The majority (93.4%, n = 57) were female and 6.6% (n = 4) were male. Caregivers were caring for either father or mother (n = 21, 34.5%), son or daughter (n = 24, 39.3%) or other (n = 16, 26.2%) and had been involved in caregiving for an average of 12.3 years (SD 5.7) providing an average of 17.1 hours of care per day (SD 2.1). Forty caregivers (65.6%) were couples (married or had partners), 50.8% (n = 31) were of low or low middle social class, 49.2% (n = 30) were from middle, middle high or high social class. The majority (65.6%, n = 40) were literate or had a primary education; 34.4% (n = 21) had high school or university education. Most (63.9%, n = 39) had responsibility for housework and 36.1% (n = 22) were retired, employed or unemployed. | |
| Interventions | Intervention: A cognitive behavioural intervention via group conference call (CBC) (n = 20) and a behavioural activation intervention through group conference call (BAC) (n = 22) (group delivered conference calls, approximately 5/group) Aim: To assess the feasibility/acceptability of a preventive cognitive‐behavioural intervention implemented via conference call for caregivers, and to conduct a preliminary assessment of the efficacy of the behavioural activation component alone compared to the complete cognitive behavioural intervention Interventionist(s): Four psychologists Mode of delivery: Telephone Duration: 5 weeks (weekly 90‐minute sessions) Content: Prior to the study, CBC and BAC intervention protocols were developed. The CBC intervention was based on a multifactorial integrative model of depression and was adapted from a proven indicated prevention program for depression previously implemented as a face‐to‐face group format. The BAC intervention was also adapted from prior work but in this case the intervention focused solely on the behavioural activation component. Standardisation: Training consisted of 35 hours for each of the interventions including contents, viewing videos, and role‐playing exercises and was administered by two clinical experts in both therapies, each with over 20 years of experience. Each intervention session was audio‐taped and protocol adherence was evaluated by one of two experienced clinicians. These clinicians also provided weekly therapist supervision. Therapist protocol adherence was 93% for CBC and 95% for BAC, indicating that the primary elements of the protocol were all administered. Comparison group: No intervention (n = 19) | |
| Outcomes | 1. Psychological health (depression)
2. Satisfaction with the intervention: Client Satisfaction Questionnaire [CSQ‐8]. The CSQ‐8 is an 8‐item scale with 4 response options and a total score ranging from 8 to 32, with a higher score indicating greater satisfaction with the service received. Outcome data were collected at the end of intervention. | |
| Notes | For the outcome depression, the reported results for 'The Center for Epidemiologic Studies Depression Scale (CES‐D‐Spanish version)' were used in the analysis for this review. On behalf of the principal investigator, Prof. Fernando L. Vázquez , Patricia Otero, PhD advised via email on the 6th August 2017 that at the time of this review a doctoral thesis was being finalised in which the efficacy of the clinical trial was being analysed. The pilot study for the trial which was published is included in this review for analysis. Patricia Otero PhD advised that the findings of the doctoral thesis are in the line with the pilot study. Details of the pilot study in terms of characteristics of the care‐recipients, the adaptation of the intervention, and intervention monitoring for the pilot study linked to this registered trial were provided by the study authors. Funding source: Work supported by the Ministry of Economy and Competitiveness of Spain (2012‐PN162 (PSI2012‐37396)) (p.594). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent statistician randomly assigned participants to groups using the table of random numbers (p.939). |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | "All pre‐ and post‐treatment assessments were conducted face‐to‐face by trained interviewers not directly involved in the research study and who were blind to the group to which each participant had been assigned" (p.940). |
| Incomplete outcome data (attrition bias) | Low risk | Minimal attrition (2:2:1); balanced across groups and reasons provided (Figure 1, p.939) |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported (p.943) |
| Other bias | Low risk | No remarkable or clinically relevant baseline differences, suggesting that randomisation had resulted in a balanced pilot study (p.940) |
| Methods | Randomised controlled trial (October 20018‐July 2010) | |
| Participants | Informal caregivers of people with dementia recruited mainly from the areas of Berlin/Brandenburg and Thuringia, Germany. Most of the caregivers were recruited via print media (80%). Some participants learned about the study via the internet (6%), cooperating institutions (5%), relatives and friends (4%), practitioners (2%), television (2%), or radio (1%). Caregivers were included if they had the main responsibility for caregiving for a patient with a diagnosis of Alzheimer’s disease and a Global Deterioration Score > 3 as rated by the screening person based on the caregiver’s report. Caregivers were also required to have no simultaneous psychotherapy, no obvious cognitive impairment (estimated in the comprehensive screening procedure through assessor’s evaluation), and no severe acute mental and/or physical illness. Mean caregiver age was 62.01 years (SD = 9.33) and females comprised 82.2% (n = 157) of the sample. Most were spouses or partners (n = 76, 39.8%) and daughters or daughters‐in law (n = 75, 39.3%) of the care‐recipients. Of the male participants, more partners (n = 21, 11%) than sons or sons‐in‐law (n = 12, 6.3%) were included. | |
| Interventions | Intervention: CBT (n = 50) Aim: To analyse whether caregivers of the intervention group reported better well‐being and health post‐treatment than caregivers of an untreated control group and an attention control group (treated with progressive muscle relaxation (PMR)), and whether these benefits were maintained at 6‐month follow‐up Interventionist(s): Six experienced clinical therapists (Master’s Degree) Mode of delivery: Telephone Duration: 3 months Content: This is a multicomponent intervention focused on managing the behaviour problems and personality changes of the care‐recipient, reduction of social isolation, assisting in utilization of professional and informal support, stress reduction, emotion regulation, reinforcement of positive activities, and supporting acceptance of role change and loss. The intervention included a therapeutic manual consisting of five CBT intervention modules, matched to the needs of the caregivers of people with dementia. Standardisation: Interventionists attended intensive pre‐intervention training with twice‐monthly supervision during the delivery of the intervention, which was carefully monitored based on intervention documentation (date, duration, content) and audiotaping of each session. Comparison group: Untreated control group (n = 50) | |
| Outcomes | 1. Psychological health (depression) German version of the 20‐item Center for Epidemiologic Studies Depression Scale (CES‐D). Higher scores indicated greater symptoms of depression. 2. Satisfaction with the intervention: A 5‐point Likert scale (where 1 = very good, 2 = good, 3 = average, 4 = below average, 5 = unsatisfactory). Lower scores indicated greater satisfaction. Data were collected at the end of intervention and at 6 months, the medium‐term follow‐up time point. | |
| Notes | In this study, a second 'selected' non‐randomised experimental group was created where all sessions were delivered by telephone. This non‐randomised arm of the study did not fulfil our inclusion criteria. The study was deemed as meeting our inclusion criteria because the findings from the randomised experimental group were provided by the author. The attention‐only arm was excluded from our review as it was administered over the phone. Funding source: The study was supported by a grant from the German Federal Ministry of Health (LTDEMENZ‐44‐092) (p.43). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent data management and biometry centre was involved to ensure blinded randomisation. The random number generator Random.org was used for randomisation (p.30). |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient information to assess |
| Blinding of outcome assessment (detection bias) | Low risk | An independent data management and biometry centre was involved for blinded assessment (p.30). |
| Incomplete outcome data (attrition bias) | Unclear risk | The experimental group to which the reported loss to follow‐up related was not specified. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes for this review were reported (p.38 and 39). |
| Other bias | High risk | Significant differences between untreated control group and experimental group in terms of perceived health (p.31) |
| Methods | A randomised, controlled, 2‐group design (study dates not reported) | |
| Participants | Female caregivers of community‐dwelling individuals with dementia from Philadelphia in United States of America. Caregivers were included in the study if they were female, 50 years of age or older, providing care for a minimum of 6 months to a relative with a physician’s diagnosis of Alzheimer’s disease or related disorders (ADRD), and having weekly access to a telephone for at least 1 hour. Caregiver mean age was 66.6 years (SD = 9.1; range, 51‐86); 68.3% were white, and the remaining caregivers were African‐American. Most were educated beyond high school (51.0%), 35.6% were high school graduates, and 10.6% had less than 12 years of education. Wives constituted 57.7% of the sample. | |
| Interventions | Intervention: Telesupport groups (group delivered teleconference, approximately 5/group) (n = 58) Aim: To enhance caregiver ability to manage daily stressors by providing emotional support and validation Duration: 6 months (weekly for one hour) Interventionist(s): Trained social workers Mode of delivery: Telephone Content: Caregivers used their own telephones with no charge. Initially, facilitators focus on developing group cohesion. As groups progress, disclosure of intimate problems and personal conflicts emerge. Caregivers express emotions and share coping strategies including cognitive reframing and practical approaches to organising care routines. They also assist each other in problem‐solving and share educational resources. The mutual support and validation provided by group members normalise experiences and provide a supportive social network, core to the service model. Standardisation: No detail provided Comparison group: Usual care (n = 45) | |
| Outcomes | 1. Burden: The 22‐item Zarit Burden scale. Caregivers report the extent of agreement on a scale ranging from 0 (never/not at all) to 4 (always/extremely) in accordance with the scale item. Responses were summed to produce a total score ranging from 0 to 88, with high scores indicating greater burden. 2. Psychological health (depression): The 20‐item Centers for Epidemiological Studies–Depression Scale (CES‐D). The response format for each item is 0 (never or rarely) to 4 (always). Scores were summed, with higher scores indicating greater depression and a score of 16 or higher indicative of depressive symptoms. 3. Skill acquisition (competence): The 6‐item scale adapted from Kaye’s Gain Through Group Involvement Scale to assess the extent to which caregivers perceive personal gains over the past few months in new friendships, knowing what to do when lonely, how to handle the blues, how to handle stress, how to find health care or other resources, and ability to deal with family relationships. Responses to each item were not at all (1), a little (2), or a great deal (3). The sum of the 6 items was calculated, yielding a possible range from 6 to 18. The actual range was 7. Higher scores indicated greater competence. Outcome data were collected at 6 months from baseline i.e. the end of intervention. | |
| Notes | Funding source: Funds from the Alzheimer’s Association awarded to Laura N. Gitlin, PhD (p.391). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to assess |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information to assess |
| Incomplete outcome data (attrition bias) | Unclear risk | Just stated that 94 (91.3%) were available for the 6‐month telephone interviews. Among these, 81 were still caregiving at home; the remaining had placed their relative in nursing home facilities or were bereaved (p.393). |
| Selective reporting (reporting bias) | Low risk | All outcomes reported (p.394 table 2) |
| Other bias | High risk | Those randomised to the experimental group were significantly older than those in the control group. Control group subjects scored slightly higher than the treatment group on gains (p.393 and table 1). |
| Methods | A prospective 2 × 3 randomised control group design (September 2005‐April 2007) | |
| Participants | Spouse or partner caregivers of veterans with moderate‐to‐severe dementia identified via (a) the Veterans Information System Technology Architecture Patient Care database activity indicating an encounter coded for a dementia diagnosis, (b) clinician referral, (c) self or family referral in response to information and publicity about the study. The study was conducted in New York, United States of America. Caregivers were primary caregivers who lived with the person for at least one year, and exhibited at least a moderate level of caregiving strain as defined by a score of 7 or more. Caregivers mean age was 73.94 years (SD not reported). Mean years of caregivers education in the intervention group was 12.69 (SD 3.04) and in the control group 12.34 (SD 2.40). Mean monthly income (US dollars) was similar across the two groups; intervention group (2784.22, SD 1351.47) and control group (2420.75, SD 1376.32). | |
| Interventions | Intervention: The Telehealth Education Program (TEP) (group‐delivered, up to 8/group) (n = 83) Aim: To address major areas that can be problematic for caregivers who want to continue to take care of the veteran with dementia at home: (a) verbal and nonverbal communication, (b) effective structuring of caregiver–patient interactions, (c) management of challenging behavioural problems, and (d) accessing resources and planning for the future. Interventionist(s): Four trained group leaders (three masters‐prepared social workers and one nurse dementia care manager) with expertise in geriatrics led the support groups. Mode of delivery: Telephone Duration: 10 weeks (group format in groups of up to 8, 1 hour telephone meetings) Content: A TEP participant workbook and leader manual were developed for the project. Caregiver participants followed a TEP participant workbook at each of the sessions and weekly homework assignments were included. The TEP group intervention protocol included three primary components: (a) education about dementia and its symptoms and about caregiving skills and resources to address these symptoms, (b) emotion‐focused (such as relaxation and self‐care strategies) and problem‐focused coping strategies (such as problem‐solving and caregiving skills), and (c) group support. TEP content was designed to address major areas that can be problematic for caregivers who want to continue to take care of the veteran with dementia at home: (a) verbal and nonverbal communication, (b) effective structuring of caregiver–patient interactions, (c) management of challenging behavioural problems, and (d) accessing resources and planning for the future. Standardisation: No detail provided Comparison group: Usual care (n = 75) | |
| Outcomes | Cost: No specific instruments. Veteran health care cost and utilisation data were collected from national abstracts of the VA’s Decision Support System (DSS) and the fee basis files hosted at the VA Austin Automation Center (AAC). For each participant, all cost and utilisation data were summed over 6‐month time intervals, resulting in a total value for each of three data collection periods: baseline (0–6 months before the intervention), short‐term follow‐up time point (from intervention start to 6 months following the start of the intervention), and medium‐term follow‐up time point (from 6 to 12 months after the start of the intervention). | |
| Notes | The information reported was from a paper linked to the registered trial. VA and VMCA were not explained but they appear to be the names or linked to the name of the health care centres/organisations. Additional unpublished results requested via email in October 2017; results not received at the time of submission of this review Funding source: Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (IIR 03‐076‐01) (p.631) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to assess |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess |
| Blinding of participants and personnel (performance bias) | Unclear risk | Unable to blind due to nature of the intervention |
| Blinding of outcome assessment (detection bias) | Low risk | Stated that “…data were extracted by one of the investigators (Jian Gao) who was blind to the participants’ group membership” (p.626) |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information to assess |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported |
| Other bias | Unclear risk | Insufficient information to assess. Stated “no statistically significant differences between participants in the two conditions at baseline” (p.627). This referred to caregivers only but results were based on patient hospitalisation and this may have impacted on outcomes. |
AA: Alzheimer's association
AAC: Austin Automation Center
ADL: Activities of daily living
ADRD: Alzheimer's disease or related disorders
AHA: American Heart Association
BAC: Behavioural activation intervention through group conference call
BCOS: Bakas caregiver outcomes scale
BPSD: Behavioural and psychological dimensions of depression
BSI‐18: Brief symptom inventory ‐ 18
CAI: Caregiver appraisal instrument
CBC: Cognitive behavioural intervention via group conference call
CBS: Conditional bother scale
CBT: Cognitive behavioural therapy
CED‐D: Definition unable to be found
CES‐D: Center for epidemiological depression scale
CGs: Caregivers
CHHB: Caregiver health and behaviour inventory
CONNECT: Definition unable to be found, may not be an acronym
CR: Care recipient
CRA: Caregiver reaction assessment
CSQ‐8: Client satisfaction questionnaire ‐ 8
DASS‐21: Depression, anxiety and stress scale ‐ 21
DSM‐IV: Diagnostic and statistical of mental disorders ‐ IV
DSS: Decision support system
DVD: Digital video disc
FAD: Family assessment devise
FAI: Frenchley activities index
FamHFcare: Family heart failure care
FECH: Further enabling care at home
FITT: Family intervention telephone tracking
FITT‐D: Family intervention telephone tracking ‐ dementia
FITT‐NH: Family intervention telephone tracking ‐ nursing home
GDS: Geriatric depression scale
GI: Gastrointestinal
HF: Heart failure
hr: hour
IADL: Instrumental activities of living
IHBMP: In‐home behavioural management program
MA: Masters of Arts
MADRC: Michigan Alzheimer’s Disease Research Center
MCA: Modified caregiver appraisal
M‐CSI: Modified caregiver strain index
MMSE: Mini‐mental state examination
MS: Multiple sclerosis
MSc: Master of Science
NHMRC: National health medical research
NIMH: National institute for mental health
NSMS: Nurse specialist in multiple sclerosis
PART‐O:Participation assessment with recombined tools–objective
PCS: Perceived criticism scale
PMR: Progressive muscle relaxation
PPI: Pressing problems index
PPO:Positive problem orientation
PSI: Problem solving intervention
PWD: People with dementia
PwMS: People with multiple sclerosis
REACH:Resources for enhancing alzheimer's caregiver health
RMBPC: Revised memory and behavior problem checklist
RPS: Rational problem‐solving
SCIDCV: Structured clinical Interview for disease and statistics manual ‐IV Axis I disorders clinician version
SCQ: Sense of competence questionnaire
SE: Self‐efficacy
SE‐CUT: Self‐efficacy: controlling upsetting thought
SE‐OR: Self‐eficacy: obtaining respite
SE‐RDB: Self‐efficacy: responding to disturbing behaviours
SF‐12: Short Form ‐ 12
SF‐36: Short Form ‐36
SP: Support person
SPSI‐R: Social problem‐solving inventory–revised
SPSI‐S: Short version of the social problem solving inventory – revised
SRAHP: Self‐rated abilities for health practices scale
STAI: State–trait anxiety inventory
TALK: Defintion not able to be found, may not be an acronym
TBI: Traumatic brain injury
TEP:Telehealth education program
TO: baseline
TSC: Telephone support condition
TSG: Telephone support group
WHOQoLBREF: World Health Organisation Quality of Life Abbreviated Version
ZBI: Zarit Burden Interview
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Wrong population and Intervention: caregivers only received the intervention if they choose to join and they did not receive a telephone intervention (confirmed by authors via email 24 June 2017). | |
| Trial withdrawn due to a lack of funding. | |
| Wrong design: not an randomised trial. | |
| Wrong comparator: comparator also included the telephone for 'attention only' purposes. | |
| Wrong intervention: care‐recipients and caregivers (dyads) received the intervention together. | |
| Wrong design: not an randomised trial. | |
| Wrong comparator: was also a telephone intervention. | |
| Wrong comparator: was also a telephone intervention. | |
| Wrong intervention: not a telephone‐only intervention (email from author 29 September 2017). | |
| Wrong design: not a randomised trial (confirmed by author via email 23 June 2017). | |
| Wrong design: not a randomised trial. | |
| Wrong population: not caregivers. | |
| Wrong intervention: not a telephone intervention. | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong comparator: included telephone calls (confirmed via email by author on 26 June 2017). | |
| Wrong design: participants were not randomised. | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong comparator: comparator was also a telephone intervention. | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong comparator: included a telephone component. | |
| Wrong study design: not a randomised trial. | |
| Wrong intervention: not a telephone intervention. | |
| Wrong intervention: in‐person delivery. | |
| Wrong study design: not a randomised design, study was a pre‐post test design. | |
| Wrong intervention (visuals introduced ‐ confirmed by author via email on 27 June 2017). | |
| Wrong intervention: intervention was patient‐focused. | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong design: not a randomised trial. | |
| Wrong Intervention: not a telephone‐only intervention (intervention included both text and voice). | |
| Wrong comparator: comparator was also a telephone intervention. | |
| Wrong intervention: not a telephone‐only intervention (results for telephone component not reported separately). | |
| Wrong intervention: not a telephone‐only intervention (telephone component was responsive and ad hoc). | |
| Wrong design: not a randomised design. | |
| Wrong intervention: not a telephone‐only intervention (results for telephone component not reported separately). | |
| Wrong intervention: not a telephone‐only intervention (results for telephone component not reported separately). | |
| Wrong intervention: not a telephone‐only intervention (results for telephone component not reported separately). | |
| Wrong intervention: both groups received the intervention face‐to‐face. | |
| Wrong intervention: not a telephone‐only intervention (telephone component was a follow‐up to the face‐to‐face sessions). | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong intervention: first face‐to‐face session was more than an introductory session. | |
| Wrong intervention: first face‐to‐face session was more than an introductory session. | |
| Wrong design: not a randomised study. | |
| Wrong intervention: not a telephone‐only intervention (confirmed by author via email on 19 July 2017). | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong design: participants were not randomised to the intervention and control groups. | |
| Wrong population: intervention was given to the caregiver and patient together. | |
| Wrong intervention: not a telephone‐only intervention (had more than one introductory session). | |
| Wrong intervention: not a telephone‐only intervention (had a home visit after an introductory telephone contact). | |
| Wrong intervention: intervention was patient‐focused. | |
| Wrong intervention: not a telephone‐only intervention (more than one in‐person visit). | |
| Wrong intervention: not a telephone‐only intervention (more than one face‐to‐face before the telephone calls). | |
| Wrong intervention: not a telephone‐only intervention (DVD given to both groups). | |
| Wrong study design: not a randomised trial. | |
| Wrong intervention: both groups received telephone calls. | |
| Wrong comparator: the telephone was also used in the comparator (confirmed via email by author on 31 July 2017). | |
| Wrong intervention: not a telephone intervention. | |
| Wrong intervention: both groups received the intervention. | |
| Wrong comparator: comparator also received telephone calls (confirmed by the author via email on 30 July 2017). | |
| Wrong intervention and comparator also received telephone calls (confirmed by the author via email on 30 July 2017). | |
| Wrong comparator: comparator also received telephone calls. | |
| Wrong population: intervention focused on patients, not caregivers. | |
| Wrong study design: not a randomised design. | |
| Wrong comparator: comparator was also telephone‐based. | |
| Wrong comparator: comparator was also telephone‐based. | |
| Wrong population: patients not caregivers. | |
| Wrong population: patients not caregivers. | |
| Wrong population: patients not caregivers. | |
| Wrong population: intervention was targeted to the patients not caregivers. | |
| Wrong population: patients not caregivers. | |
| Wrong population: patients not caregivers. | |
| Wrong population: intervention was targeted to patients not caregivers (confirmed via email by authors on 29 July 2017). | |
| Wrong intervention: intervention not a telephone‐only intervention. | |
| Wrong comparator: comparator was also an active telephone intervention. | |
| Wrong population: patients not caregivers. | |
| Wrong comparator: comparator was also a telephone intervention. | |
| Wrong intervention: not a telephone‐only intervention (confirmed by author via email on 17 November 2018) | |
| Wrong population: patients not caregivers. | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong intervention: not a telephone‐only intervention (included an online component), | |
| Wrong intervention: not a telephone intervention (delivered via webcam using a computer ‐ confirmed by author via email on 1 August 2017). | |
| Wrong population: patients not caregivers. | |
| Wrong intervention: not a telephone intervention. | |
| Wrong intervention: not a telephone‐only intervention (most caregivers received a minimum of 3 face‐to‐face contacts and mode of delivery was not used for analysis, confirmed by author via email on 8 November 2018) | |
| Wrong intervention: not a telephone‐only intervention (telephone component was linked to the online component and not analysed separately ‐ confirmed by author via email on 5 August 2017). | |
| Wrong population: healthy persons, not caregivers. | |
| Wrong design: not a randomised controlled trial. | |
| Wrong comparator: usual care group also received two brief calls. | |
| Wrong intervention: not a telephone‐only intervention (web‐based and smart phones were used to complete homework, confirmed by author via email 9 November 2018) | |
| Wrong comparator: comparator also delivered by telephone. | |
| Wrong design: not a randomised controlled trial. | |
| Wrong intervention: not a telephone intervention. | |
| Wrong intervention: not a telephone‐only intervention (had two baseline home visits ‐ confirmed by author via email 3 August 2017). | |
| Wrong design: not a randomised design (one group feasibility study ‐ confirmed by author via email 3 August 2017). | |
| Wrong design: not a randomised study. | |
| Wrong intervention: not a telephone intervention. | |
| Wrong design: not a randomised trial. | |
| Wrong population: care‐recipients and caregiver received the intervention together. | |
| Wrong intervention: not a telephone intervention. | |
| Wrong intervention: paper focused on treatment fidelity of a caregiver intervention tested using a randomised trial but the intervention was not telephone‐only. | |
| Wrong intervention: neither of the two intervention groups were telephone‐only. | |
| Wrong design: not a randomised trial. | |
| Wrong intervention: not a telephone‐only intervention (comparator was telephone‐only but the intervention included in‐home visits plus telephone contacts). | |
| Wrong population: patients not caregivers. | |
| Wrong design: not a randomised study. | |
| Wrong intervention: not a telephone intervention. | |
| Wrong intervention: not a telephone intervention. | |
| Wrong design: not a randomised controlled trial. | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong comparator: comparator was telephone based (confirmed by principal investigators via email on 22 August 2017). | |
| Wrong intervention: intervention was an automated telephone system. | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong design: not a randomised controlled trial. | |
| Wrong design: not a randomised study (focus was on intervention development). | |
| Wrong design: participants were not randomised to the groups. | |
| Wrong comparator: comparator was also telephone‐based. | |
| Wrong comparator: comparator was also telephone‐based. | |
| Wrong comparator: comparator was also telephone‐based. | |
| Wrong design: not a randomised controlled trial. | |
| Wrong intervention: not a telephone‐only intervention (combination of online and telephone). | |
| Wrong design: not a randomised study. | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong intervention: not a telephone intervention. | |
| Wrong design: not a randomised trial for the informal caregiver component of the study (confirmed via email by author on 23 October 2017). | |
| Wrong comparator: comparator was also delivered by telephone. | |
| Wrong intervention: not a telephone‐only intervention. | |
| Wrong intervention: not a telephone intervention. | |
| Wrong intervention: not a telephone‐only intervention. |
DVD: Digital video disc
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Parallel randomised controlled trial |
| Participants | Informal caregivers of people with dementia where the caregiver was the primary full‐time carer (for at least 6 months), were aged 25 years and were able to read and speak Chinese/Cantonese. The caregivers consisted of spouses, daughters/sons, and daughter/son‐in‐laws of the patients.Thirty caregivers received the intervention and 30 caregivers received standard care. The mean age of caregivers who completed the study were: intervention group 58.1 (SD 12.4); control group 55.1 (SD 11.3). Gender (intervention group, male 6 (21.4%), female 22 (78.6%) and control group, male 7 (22.6%), female 24 (77.4%). In the intervention group, education ranged from none 2 (7.1%), primary/kindergarten 6 (21.4%), junior secondary 6 (21.4%), senior secondary 8 (28.6%), form 6‐7/vocational institutes 2 (0%), college sub‐degree 2 (7.1%), college, bachelor degree 4 (14.3%). In the control group, participants education levels were: none 1 (3.2%), primary/kindergarten 12 (41.9%), junior secondary 2 (6.5%), senior secondary 10 (32.2%), form 6‐7/vocational institutes 2 (6.5%), college sub‐degree 2 (6.5%), college, bachelor degree 1 (3.2%). The mean duration in years of caregiving for the intervention group was 3.2 ± 2, and for the control group 3.3 ± 2.3. Patients: Mean age in years for the intervention group was 80.1 ± 6 and for the control group 79.9 ± 8.6. Relationship to caregivers for the intervention group were spouse 12 (42.9%), children 15 (53.6%), children‐in‐laws 3 (3.6%) and for the control group, spouse 11 (35.5%), children 14 (45.2%), children‐in‐laws 4 (12.9%), relatives 1 (6.5%). The mean duration of dementia (in years) for the intervention group was 3.4 ± 2 and for the control group was 3.3 ± 2.2. Care‐recipients in the intervention group were in receipt of average hours of care per day of 8.3 ± 7; those in the control group received a mean of 7 9.1 ± 9.5 hours of care per day. |
| Interventions | Title of the intervention: Telephone‐assisted pleasant‐event scheduling (TAPES) Aim: To evaluate the effectiveness of TAPES on enhancing the psychological well‐being of community‐dwelling family caregivers.\ Interventionist(s): no details provided Duration: 4 weeks (2 calls for first two weeks and one call per week for weeks 3 and 4). Each call was 20 minutes in duration. Content: The intervention had three components. First, the project rationale of behavioural activation was introduced, and the Pleasant Event Schedule (revised from California Older Person’s Pleasant Events Schedule) was administered. An information package was distributed to advise on how to access social and psychological services in the community. Participants were then asked to decide on one or two activities that they would like to work on for the coming weeks. Second, six telephone calls were made. In the first phone call, participants were taught to schedule pleasant events according to the procedures of behavioural activation by working through the Pleasant Activity Planning Worksheet. To monitor individual progress, participants were asked to fill the Pleasant Event Tracking Form and the Daily Mood Record Form on a daily basis. Participants then mailed the completed progress charting forms back to the researcher. Third, concepts of adaptive coping were discussed from weeks 2 to 4: active coping, passive coping, and the goodness of fit between coping and situations, problem‐solving coping (e.g. making preparations), emotion‐regulation coping (e.g. distancing) and using situation‐appropriate strategies (e.g. stepping back and taking a break when no immediate solution was available). The compliance of treatment was closely monitored. Participants had to complete the preceding component first before moving on the next component. The completion of the tasks was recorded on the intervention protocol. Regular weekly meetings were carried out by the intervention team to review the progress of caregivers. Standardisation: no details provided Comparision group: Usual care (TAU) – treatment‐as‐usual (standard care provided by a psychogeriatric team with regular psychiatric follow‐up for the care‐recipients and support from social workers upon request). |
| Outcomes | 1. The Centre for Epidemiologic Studies Depression Scale (CES‐D) 2. Revised Scale for Caregiving Self‐Efficacy (SE) Data were collected pre‐intervention (1‐3 days before the first intervention call), post‐intervention (1‐3 days after the last intervention call), and at follow‐up (1 month after post‐intervention). |
| Notes | Professional status of the interventionists unknown (awaiting author response) |
| Methods | Stated that three randomised trials were underway |
| Participants | Caregivers (one study for caregivers of people with dementia, one for caregivers of people with depression and one for people with multiple chronic conditions) |
| Interventions | Title of the intervention: Care Consultation Aim: To help caregivers and care receivers by providing information about health problems and available resources mobilising and facilitating the use of informal supports and formal services; and providing emotional support. Interventionist(s): Care consultants (social workers or nurses) Duration: no details provided Content: no details provided Standardisation: no details provided. Comparison group: usual care (no details provided) |
| Outcomes | Not stated |
| Notes | Reference was from the Rosalynn Carter Institute for Caregiving website which provided a brief outline of the study. Unclear as to whether the intervention focused on helping caregivers or primarily focused on patients. |
| Methods | Randomised controlled trial |
| Participants | Dementia caregivers |
| Interventions | Title of the intervention: An evidence‐based dementia care management (DCM) Aim: To implement an evidence‐based dementia care management (DCM) program in a Medicare managed care plan and evaluate the program’s effectiveness and costs Interventionist(s): Care managers (social workers specially trained in evidence‐based dementia care) Duration: no details provided Content: no details provided Standardisation: no details provided Comparison group: usual care (no details provided) |
| Outcomes | No detail provided on specific outcome measurement instruments. Stated that caregiver surveys and medical records were used to estimate between‐group differences on measures of recommended dementia care within areas of 1) assessment, 2) treatment, 3) safety, and 4) education and support. The abstract indicated that the date of caregiver satisfaction, burden, social support, self‐efficacy, and healthcare utilisation costs were collected. Data were collected at 9 and 18 months. Method of data collection was not specified. |
| Notes | Abstract only available. It was unclear if the caregivers got the intervention separately to the patients. Author contacted and stated that the manuscript was in process and no further details are available at the time of contact. |
| Methods | Unclear |
| Participants | Informal caregivers in a rural area |
| Interventions | Title of the intervention: Southern Illinois Rural Caregiver Telehealth Project Aim: To specifically meet the needs of informal caregivers in a rural area Interventionist(s): Masters level psychologist Duration: Eight‐session structured telephone intervention Content: Stated that caregiver knowledge, problem‐solving skills, help‐seeking behaviour, and affect were the major components addressed Standardisation: no details provided Comparison group: Call‐in helpline |
| Outcomes | No detail provided |
| Notes | Reference was from the Rosalynn Carter Institute for Caregiving website which provided a brief outline of the study. The study design was unclear. |
| Methods | Randomised trial |
| Participants | Family caregivers of veterans with dementia |
| Interventions | Title of the intervention: Information only Aim: This was an attention‐only comparator for the face‐to‐fact TAP‐VA Interventionist(s): Masters level team member Duration: no details provided Content: 8 telephone sessions with information on relevant topics (home, safety, dementia), with no discussion of activity or behavioural activity. Standardisation: no details provided Comparison group: TAP‐VA: 8 in‐home sessions delivered by occupational therapists |
| Outcomes | Caregiver assessment of function and upset scale (CAFU) |
| Notes | Study control group received the telephone intervention. We need to confirm if the individuals delivering the telephone calls were healthcare professionals and assess the intervention in greater detail for inclusion in the update of this review. |
| Methods | Randomised controlled design |
| Participants | Caregivers of veterans diagnosed with dementia |
| Interventions | Title of the intervention: Telephone Education program Aim: To facilitate resource connection and provide education, psychosocial support, and care management for individuals caring for veterans with dementia Interventionist(s): no details provided Duration: no details provided Content: Caregivers received education, continuous support, skills training and monitoring of veterans medication adherence, symptoms and service needs Standardisation: no details provided Comparison group: Participants were sent general material about VA and community resources for patients with dementia and their caregivers, as well as brochures for the caregivers. In addition, they received usual care and were free to seek medical, psychological, social support, and social services that are available through VAMCs or any other non‐VA/community resource. |
| Outcomes | Caregivers were asked to complete an assessment battery of standardised measures of care‐recipient and caregiver characteristics. |
| Notes | This is a brief summary of a study from the Health Services Research and Development website. The study needs to be further assessed prior to inclusion in the update of this review. |
| Methods | Randomised controlled trial |
| Participants | Caregivers of patients with stroke recruited from patient admissions to Rhode Island Hospital following an acute stroke. Caregivers were 18 years or over (confirmed by named principle investigator. Professior Ivan W. Miller). Patients inclusion criteria: age > 35 years, MRI or CAT scan proof of stroke or definitive hemiplegia, and competency to sign an informed consent form |
| Interventions | Title of the intervention: Family Intervention: Telephone Tracking (FITT) plus standard medical care Aim: To determine if a family intervention administered by telephone to stroke patients and their caregivers increases adaptation and functioning after stroke Interventionist(s): no details provided Duration: six‐month period (participants contacted by telephone every week for 6 weeks, then every 2 weeks for 2 months, and then monthly for 2 months) Content: no details provided Standardisation: no details provided Comparison group: no intervention plus standard medical care |
| Outcomes | During the trial, specially trained staff will carefully monitor the progress of the stroke patient and his/her family member, checking for changing in thinking, concentration, attention, memory, mood, and family functioning that sometimes occurs in stroke. The telephone calls will check on how the participants are doing after discharge and will assist with questions and concerns. |
| Notes | Unclear as to whether the interventionist was a healthcare professional or not |
| Methods | Randomised controlled trial |
| Participants | Family member or friend who was identified as the primary caregiver. Both recently diagnosed HIV‐infected individuals and primary caregiver were included. |
| Interventions | Title of the intervention: Family Intervention: Telephone Tracking (FITT) plus regular medical care Aim: To evaluate the effectiveness of FITT in improving family functioning, enhancing coping skills, and reducing depression in HIV‐infected individuals and their caregivers. Interventionist(s): no details provided Duration: 12 months Content: FITT is a telephone‐based intervention program that assists in identifying problems and resolving them through referrals to medical and community organisations that provide HIV‐related support and services. It is also an educational resource that provides information on the many medical and psychological aspects of HIV infection. Standardisation: no details provided Comparison group: an assessment‐only group that did not receive FITT but received regular medical care throughout the study |
| Outcomes | Outcome measurements were self‐assessments of depression, coping, and family functioning. In addition, participants receiving FITT were asked to evaluate the effectiveness of the telephone intervention. No details provided on outcome measures. All measurements were assessed at baseline, and months 3, 6, and 12. |
| Notes | This is a registered trial on the ClinicalTrials.gov website. The site indicates that the study has been completed. It is unclear if the age of participants refers to the caregiver of the person with HIV and if the caregivers received the intervention separately to the care‐recipient. |
| Methods | Randomised trial |
| Participants | Caregivers of people with Alzheimer's disease |
| Interventions | Title of the intervention: Customary care and monthly brief telephone calls Aim: Not stated Interventionist(s): Project staff Duration: Six months Content: Caregiver brief supportive telephone calls for 6 months embedded in one year of customary care Standardisation: No detail provided Comparison group: Customary care and access to an intensive, interactive online education and support website |
| Outcomes | 1. Burden: Zarit Short Burden Scale, a 12‐item instrument that utilises a Likert scale 1‐5 rating of frequency (range 12 (never) to 60 (nearly always)), higher scores were more indicative of caregiver burden. 2. Depression: Beck Depression Inventory. The Beck Depression Inventory is a 21‐item Likert scale instrument with a total range of 0 to 63. Higher scores indicated increased endorsement of depressive symptoms. 3. Frequency of Patient Problematic Behavior: Frequency of Problematic Behaviors on the Revised Memory and Behavior Problem Checklist (a 24‐item instrument that measures the frequency of a behaviour on a 0‐4 Likert scale (range 0‐96, higher numbers indicated greater frequency of problematic behaviour). 4. Caregiver Negative Reactions to Problematic Behavioural Patterns: Negative Reactions Scale from the Revised Memory and Behavior Problem Checklist. The scale measures the caregiver's level of reaction to a series of potential problematic behaviours on a 0‐4 Likert scale; higher numbers indicated a greater degree of distress. The range is 0‐96. Data were collected at 6 months (end of intervention). |
| Notes | This study is complete and to be evaluated for inclusion in the next update of this review. Unclear as to what 'customary care' refers to. Not stated if project staff were health care professionals. More detail is required on the telephone arm, which is the comparator arm of this study. |
| Methods | Parallel randomised trial |
| Participants | Partners of African‐American Prostate Cancer survivors |
| Interventions | Title of the intervention: PA‐CST intervention Aim: To help African‐American prostate cancer survivors and their partners cope with challenges after surgery for early‐stage prostate cancer Interventionist(s): African‐American doctoral clinical psychologists Duration: 8 weeks (weekly for six weeks) Content:· Partner‐assisted coping skills training (PA‐CST): Survivor/partner dyads underwent a telephone‐based culturally sensitive PA‐CST intervention relating to knowledge about prostate cancer. Participants were trained in a variety of cognitive and behavioural skills to manage symptom‐related distress and to improve their quality of life after prostate cancer treatment. The skills included strategies for communication (i.e. effective speaking and listening); behavioural coping methods (i.e. activity pacing, applied relaxation techniques, and goal setting to increase pleasant activities); and skills for managing negative mood and reducing emotional stress. They also received guidance in working co‐operatively with their partners to improve symptom management, including joint practicing of coping skills and problem‐solving strategies. Standardisation: Not stated Comparison group: Wait‐list control: Survivor/partner dyads received usual care and were placed on a wait‐list. After completing the study, survivors and their partners had the option of participating in either the CST or cancer education interventions. |
| Outcomes | 1. Burden: Caregiver Strain Index (CSI) 2. Depression: Profile of Mood States‐SF (POMS‐SF) 3. Self‐efficacy: Partners' self‐efficacy for symptom control as assessed by the Self‐Efficacy for Symptom Control Inventory; EPIC; and CSI at baseline, 2 months, and 5 months 4. Relationship quality: Dyadic Adjustment Scale and the Miller Social Intimacy Scale at baseline, 2 months, and 5 months 5. Coping: a measure of coping strategies Outcomes measured at baseline, 2 months, and 5 months |
| Notes | Trial recruitment completed. Trial registration site last updated February 25, 2013. Need to determine that caregivers and care‐recipients received the intervention separately. |
| Methods | Randomised controlled trial |
| Participants | Parents of young adults leaving residential substance abuse treatment |
| Interventions | Title of the intervention: Home‐based Continuing Care (HCC) Aim: To help parents support the recovery of their Young Adult (YA) child who was leaving residential substance abuse treatment Interventionist(s): Masters or doctoral level therapists in social work or psychology Duration: Not specified (5 individual sessions and 1 joint session with their child, each session was 45‐50 min). Content: All sessions occurred over the phone or Cisco WebEx meetings. Parents participated in 5 individual sessions and 1 joint session with their child (45‐50 minutes each). Young Adults (YAs) participated in 1‐3 individual meetings (30‐45 minutes each) and 1 joint session (45‐50 minutes). In addition, YAs were contacted weekly for the first 8 weeks of HCC, then every other week for the remaining 24 weeks (20 calls total). He or she were asked questions addressing risk and protective factors for relapse. Finally, parents were trained to collect and test their child's urine sample and deliver incentives to the YA contingent upon biologically‐verified abstinence and verified engagement in continuing service plan activities. Urine samples were collected regularly over a 32‐week period. Standardisation: No detail provided Comparison group: Continuing service plan recommended by the residential treatment program. Parents were told to support this and were sent information on continuing care developed by the Treatment Research Institute and the Partnership @ Drugfree.org (continuingcare.drugfree.org). No supplemental services were provided during the study. Parents were trained to collect urine samples for research purposes only. Parents and YAs were offered separate 4‐hour workshops after they had completed participation as an added study participation incentive for this group. |
| Outcomes | 1. Satisfaction: Parent Happiness with Youth 2. Parent and Young Adult Treatment Retention 3. Parent and Young Adult Treatment: Treatment Evaluation Inventory 4. Parent and Young Adult Engagement in HCC by number of calls completed 5. Parent and Young Adult Recruitment Rate by monthly recruitment rate Data were collected week 16 and 32 |
| Notes | Author confirmed that the interventionists were healthcare professionals. Results have yet to be submitted for publication. Author stated almost all of the sessions were conducted by phone ‐ full detail of the intervention and its delivery needs to be assessed prior to inclusion in this review. |
| Methods | Parallel randomised trial |
| Participants | Caregivers of people with traumatic brain injury (TBI) Inclusion Criteria: age ≥ 19 years old, meets study project definition of a military caregiver, documentation or determination of an Operation Iraqi Freedom/Operation Enduring Freedom (OIF/OEF) deployment‐related TBI Service member will have presented to a Veterans Administration Medical Center (VAMC) or military medical centre, English‐speaking, has access to a telephone for the administration of measures and/or intervention calls, has no significant cognitive or communication problems that might significantly interfere with adequately understanding information or talking on the telephone which will be determined by the clinical judgment of the person consenting the participant. |
| Interventions | Title of the intervention: Problem‐Solving Training (PST) Aim: To evaluate the impact of a telehealth‐based, cognitive behavioural therapy (CBT) intervention (problem‐solving training: PST) for adult informal military family/friend caregivers of OIF/OEF service members with a deployment‐related TBI Interventionist(s): no details provided Duration: 6 weeks (one hour per week) Content: Problem‐Solving Training (PST) is a cognitive‐behavioural intervention. PST consists of education related to problem‐solving skills/problem‐solving model and application to caregiving and managing caregiver‐related problems. Standardisation: no details provided Comparison group: Sham Comparator: Attention control/social contact control. Health education (non‐skill focused). |
| Outcomes | Patient Health Questionnaire‐9 (PHQ‐9) Data collection time points are baseline and post‐program (3 months follow‐up). |
| Notes | The type of interventionist i.e. professional/non‐professional was not stated. The study is ongoing and the final data collection date for the primary outcome measure was September 2017. |
| Methods | Randomised controlled trial |
| Participants | Caregivers of people with heart failure |
| Interventions | Title of the intervention: ENABLE CHF‐PC Aim: The primary aim is to encourage participant empowerment; however, occasionally the nurse coaches may provide feedback directly to the HF teams (or palliative care teams) about specific issues (e.g. unrelieved pain) or make referrals to other resources Interventionist(s): Nurses Duration: 48 weeks or until patient death Content: This includes an in‐person comprehensive Palliative Care team (PCT) consultation as soon as possible after enrolment and a Palliative Care Nurse Coach (PNC) embedded within HF teams with phone based 4‐session caregiver manualised curriculum titled Charting Your Course (CYC), followed by monthly phone‐based supportive care. Standardisation: No detail provided Comparison group: Usual care, this includes any available supportive care resources and heart failure patient medical management based on national HF guidelines. |
| Outcomes | 1. Quality of life: Bakas Caregiving Outcomes Scale (BCOS) 2. Burden: Montgomery Borgatta Caregiver Burden Scale (MBCB) 3. Depression: the Hospital Anxiety and Depression Scale (HADS) 4. Health status: PROMIS SF Global Health Data were collected 8 and 16 weeks following baseline |
| Notes | Need to determine if caregivers received the intervention separate to the care‐recipients |
| Methods | Randomised controlled trial |
| Participants | Caregivers of patients with dementia |
| Interventions | Title of the intervention: Telesupport psychoeducation and support Aim: No detail provided Interventionist(s): No detail provided Duration: Eight weeks Content: In addition to usual primary health care, participants will receive psychoeducational guidelines and support in the management of their relatives with dementia. They will have access to a number of phones to spontaneously contact specific guidelines during the eight weeks of intervention. Standardisation: No detail provided Comparison group: Control group with usual follow‐up at primary health care |
| Outcomes | 1. Quality of life: WHOQoL 2. Burden: Zarit Burden Interview 3. Depression: Beck Depression Inventory |
| Notes | More detail is required on the guidelines that participants in the intervention group will have access to during the intervention. Interventionists need to be identified. |
BCOS: Bakas caregiver outcomes scale
CAFU: Caregiver assessment of function and upset scale
CAT: Computerised tomography scan
CBT: Cognitive behavioural therapy
CES‐D: Center for epidemiological depression scale
CHF‐PC: Comprehensive heartcare for patients and caregivers
CSI: Caregiver strain index
CYC:Charting your course
DCM: Dementia care management
ENABLE: Educate, nurture, advise, before life ends, comprehensive heartcare for patients and caregivers
EPIC: Expanded prostate cancer index composite scale
FITT: Family Intervention: telephone tracking
HADS: Hospital anxiety and depression scale
HCC: Home‐based continuing care
HF: Heart failure
HIV: Human immunodeficiency virus
MBCB: Montgomery Borgatta caregiver burden scale
MRI: Magnetic resonance imaging
PA‐CST: Partner‐assisted coping skills training
PCT: Palliative care team
PHQ‐9: Patient health questionnaire‐9
PNC: Palliative care nurse coach
POMs‐SF:Profile of mood states‐ short form
PROMIS SF: Patient reported outcomes measurement information system short form
PST:Problem‐solving training
OEF:Operation enduring freedom
OIF:Operation Iraqi freedom
SE: Self‐efficacy
TAPES: Telephone‐assisted pleasant‐event scheduling
TAP‐VA: Tailored activity program ‐ Veterans Affairs
TAU: Treatment as usual
TBI: Traumatic brain injury
VA: Veterans Affairs
VAMC:Veterans Administration Medical Center
YA: Youth adult
WHOQoL: World health organisation quality of life
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A non‐pharmacologic approach to address challenging behaviours of veterans with dementia: description of the tailored activity program‐VA randomised trial |
| Methods | Randomised controlled trial |
| Participants | Caregivers of people with dementia |
| Interventions | Title of intervention: Telephone attention control Aim: The telephone component of the study is the attention control and serves three purposes: 1) creates clinical equipoise, ensuring that ethical treatment is provided to all study participants; 2) controls for the one‐on‐one attention to caregivers in the Tailored Activity treatment group to rule out potential effects of professional contact; and 3) serves as a retention tool to keep control group caregivers meaningfully connected to the trial. Interventionist(s): Trained healthcare professional Mode of delivery: Telephone Duration: Sixteen weeks (biweekly telephone contact (up to 8 contacts), each contact is approximately 30 minutes in length) Content: In each session, caregivers are provided with important information about dementia and strategies for managing the disease at home. Each telephone contact begins with a brief overview of the specific purpose of the session, followed by a description of the key facts about the session topic, and concludes with a question and answer period. Standardisation: Not stated Comparison group: The Tailored Activity Program – Veterans Administration (TAP‐VA) provides an assessment of the veterans home environment and provides caregivers with the requisite knowledge and skills to use activities. Caregivers are instructed in specific skills such as ways to simplify activities, the environment and their communication, and how to help the veteran initiate and follow a sequence. The overall goal is to provide predictability, familiarity, and structure in the daily life of the veteran and establish a level of environmental stimulation appropriate to that person’s abilities. |
| Outcomes | 1. Burden: Zarit Short Form Burden Scale 2. Depression: The Center for Epidemiologic Studies Depression Scale (CES‐D) 3. Cost: Cost‐effectiveness is measured as the cost of achieving one additional unit of benefit as defined by caregiver hours per day “doing things” and hours per day “being on duty.” |
| Starting date | August 2012 |
| Contact information | Laura N Gitlin, Johns Hopkins University, 525 N. Wolfe Street, Baltimore, MD 21205, USA Email: [email protected] |
| Notes | This is a protocol for a registered trial (ClinicalTrials.gov Identifier NCT01357564). The registered trial primary completion date was June 2016 with an estimated study completion date of August 2018. The ClinicalTrials.gov site indicates that the study is not yet recruiting. |
| Trial name or title | Implementing a multi‐modal support service model for the family caregivers of persons with age‐related macular degeneration: a study protocol for a randomised controlled trial |
| Methods | Randomised controlled trial |
| Participants | Caregivers of persons with late age‐related macular degeneration (AMD) |
| Interventions | Title: Mail‐delivered cognitive behavioural therapy (M‐CBT) and Telephone‐delivered group counselling sessions Aim: To empower family caregivers by improving their coping strategies, enhancing hopeful feelings such as self‐efficacy and helping them make the most of available sources of social and financial support. Interventionists: Practising dietician (confirmed by author via email on 22 November 2018) Mode of delivery: Telephone Duration: 10 weeks Content: The intervention group will receive a multi‐modal support service programme consisting of a brief mail‐delivered (M‐CBT) treatment delivered fortnightly as five individual modules and five Talk‐Link group counselling sessions. The Talk‐Link Counselling and M‐CBT will occur weekly on an alternating basis. M‐CBT of fortnightly modules formatted in Microsoft PowerPoint, with additional homework worksheets and accompanying templates for practising acquired skills, will be mailed to participants in the intervention group. Each module will target a specific stressor and/or train a new adaptive coping method and will be supported by targeted homework assignments for the caregiver to practice between sessions. Standardisation: Not stated Comparator group: Active wait‐list control group will receive reading materials concerning AMD and caring for persons diagnosed with the condition. All control participants will be offered the opportunity to receive the multicomponent intervention after the study ends (12–18 months after inclusion). |
| Outcomes | 1. Quality of life: EUROQoL ‐ EQ‐5D 5‐level scale 2. Burden: Caregiver Burden Scale (CBS) 3. Depression: Centre for Epidemiologic Studies Depression Scale. 4. Cost effectiveness of intervention: conducted from the perspective of the national health provider in Australia and will determine the cost per person to deliver the support service model and the cost‐effectiveness compared with usual care. Data on health‐related quality of life will be collected during 12 months post‐treatment using the EQ‐5D‐5L questionnaire. EQ‐5D scores will be converted into utility values using a valuation algorithm for the Australian population. Data will be collected at baseline and 12‐month follow‐up. |
| Starting date | 25 January 2017 |
| Contact information | Dr Bamini Gopinath; [email protected] |
| Notes | Dr. Gopinath confirmed via email on 22 November 2018 that the interventionist is a health care professional. |
| Trial name or title | Acceptability and utility of a telephone outcall program for carers of persons diagnosed with cancer |
| Methods | Randomised trial |
| Participants | Caregivers of persons with cancer recruited from four Australian health services. One hundred and eight carer/person with cancer dyads were randomised to the intervention group and 108 to the control group. Participants who completed the study: 54% were female with the majority (81%) caring for their spouse/partner; mean age of carers was 58 years. All caregivers were 18 or over (confirmed via email by the author). |
| Interventions | Title of intervention: Telephone outcall program Aim: To evaluate acceptability and utility of a telephone outcall program to reduce burden and depression among carers of persons newly diagnosed with cancer Interventionist(s): Cancer Council Helpline nurse Mode of delivery: Telephone Duration: 3 months (carers received three telephone outcalls (mean call duration: 3 min) at three time points (7‐10 days after recruitment, 1 and 3 months later). Content: Carers were screened for distress using the Distress Thermometer (range: 0‐10) and given tailored information and support. Carers with a distress score of > 4 were referred to their GP for follow‐up. Standardisation: no details provided Comparison group: two comparison groups, sham outcalls and a usual support group. 1. Participants in the sham group received three sham outcalls (mean call duration: 22 min) at the same time points as the intervention group and were provided with the Cancer Council Helpline number to contact as needed. 2. Participants in the control arm who chose to contact the Cancer Council Helpline received usual support provided by Helpline nurses (not the outcall program). |
| Outcomes | Participants completed a utility survey one month post‐intervention. |
| Starting date | No details provided |
| Contact information | Leila Heckel, email: [email protected] |
| Notes | Abstract only. Author advised via email that data collection and analysis have been finalised and they are in the process of preparing a manuscript reporting on the main outcomes of the RCT for publication. |
| Trial name or title | A randomised pilot trial of a telephone‐based collaborative care management program for caregivers of individuals with dementia |
| Methods | Randomised trial |
| Participants | Caregivers of older veterans with dementia |
| Interventions | Title of the intervention: Modified Telehealth Education Program (TEP) and the Behavioural Health Laboratory (BHL) Aim: To provide caregiver education and psychosocial support Interventionist(s): Care manager (nurse) Mode of delivery: Telephone Duration: Three months (minimum of 3 contacts) Content: Two components: An individualised dementia care manager (CM) provided regular and extended contact between the caregiver (CG), care manager, and when appropriate, the veteran’s primary care provider (PCP). The care manager monitored veterans’ symptoms via CG report and provided support to CGs. TEP was modified for use with individual CGs and was formatted so that CGs could select from a menu of up to seven modules in workbook format covering various content areas evaluated during the course of the CM assessments (e.g. communication skills, behavioural management techniques, stress management and coping skills, long‐term planning). They also received all material made available in the usual care arm. During the first contact, the care manager provided a general overview of the format, content, and goals of the TEP. In addition, the care manager reviewed the recommended subject areas and the CG and care manager collaboratively finalised the list of TEP modules to be covered throughout the course of the individualised program. CGs were permitted to choose as many or as few of the modules as they felt necessary. All CGs, however, were encouraged to participate in a minimum of two introductory sessions. These two sessions explained how symptoms of dementia differ from normal aging and how symptoms change over the course of the illness and introduced problem‐solving techniques. Sessions were scheduled depending upon the availability and preference of the CG. Even if the CG declined all modules, the care manager still contacted the CG for the individualised care management as described above. Standardisation: No detail provided Comparison group: Usual care (were mailed general material providing information about VA and community resources) |
| Outcomes | 1.Burden: Zarit Burden Interview 12‐item (range 0–48) 2. Bother or upset: Revised Memory and Behavior Problems Checklist RMBPC caregiver reaction subscale (range 0–96) 3.Distress Neuropsychiatric Inventory Questionnaire caregiver distress subscale (range 0–50) 4.Coping: Management of Meaning — Reduction of Expectations subscale of the Pearlin Caregiving and Stress Process Scale 3 items, range 3–12) 5. Mastery: Caregiving Mastery subscale of the Lawton Caregiving Appraisal (6‐item scale ranging from 6–30) Data were collected at baseline and at 3‐ and 6‐month follow‐ups. |
| Starting date | Study is complete. |
| Contact information | Shahrzad Mavandadi email: [email protected] |
| Notes | Full paper published in 2017 following completion and submission of the review; to be evaluated for inclusion in the next update. |
| Trial name or title | The effects of telephone counselling and education on breast cancer screening in family caregivers of breast cancer patients |
| Methods | Randomised trial |
| Participants | Caregivers of people with breast cancer |
| Interventions | Title of the intervention: Counselling and education intervention Aim: not stated Interventionist(s): MSc Nurse Mode of delivery: Telephone Duration: Not stated Content: Counselling and education according to the protocol about breast cancer screening in three phone calls of 60‐90 minutes for each call Standardisation: not stated Comparison group: control group (no intervention but received the counselling and education intervention after the study) |
| Outcomes | Structured questionnaire (demographics, breast cancer screening knowledge, breast cancer risk perception |
| Starting date | Start date not stated but data were collected between May and October 2011 |
| Contact information | |
| Notes | Study complete (results to be included in the review update) |
| Trial name or title | Self‐Care Talk Study ‐ promoting Alzheimer's Disease (AD) spousal caregiver health |
| Methods | A randomised controlled trial |
| Participants | Caregivers of persons with dementia |
| Interventions | Title of the intervention: Self‐Care TALK Aim: No detail provided Interventionist(s): Advanced practice nurses Mode of delivery: Telephone Duration: Six weeks Content: The intervention includes creating a health‐promoting, self‐care education and support partnership between caregivers and nurses through the use of weekly telephone conversations. Each conversation focuses on a health‐related topic. The conversations follow a basic format, but are also individualised. Standardisation: No detail provided Comparison group: No intervention; they received written materials related to self‐care and health promotion post‐time 3 (week 24). |
| Outcomes | 1. Physical health: SF‐36 v2, PCS (perceived physical health), SF‐36 v2, MCS (perceived mental health) 2. Burden: M‐CSI; modified (caregiver strain) 3. Self‐efficacy: SRAHP (self‐efficacy for health) 4. Depression: CES‐D Data were collected at baseline, 8 weeks (time 2), and 24 weeks (time 3) after baseline. |
| Starting date | July 2006 |
| Contact information | Cynthia Teel, PhD, RN |
| Notes | Trial registration website indicated that recruitment was complete. |
| Trial name or title | Telephone‐based counselling for depression in Parkinson's disease (TH‐CBT) |
| Methods | Parallel randomised trial |
| Participants | Caregiver: A family member or friend (care‐partner) of a person with Parkinson's Disease (PD). Age ranged from 35 to 85 years (confirmed by author via email). Care‐recipients: 35 to 85 years (adult, senior), all sexes eligible for the study, confirmed diagnosis of Parkinson's disease, clinically significant depressive symptoms (e.g. symptoms are pervasive, distressing, and make life harder), the presence of a formal depressive disorder will be determined by study staff based on standardised criteria, stable medication regimen ≥ 6 weeks, no change in mental health treatment in the past 2 months, family member or friend willing to participate, access to a telephone, live in the United States of America (USA). |
| Interventions | Title of the intervention: Telephone‐guided cognitive behavioural self‐help program (TH‐CBT) plus enhanced usual care Aim: To evaluate a 10‐session telephone‐guided cognitive behavioural self‐help program (TH‐CBT) for depression in PD (dPD). Interventionist(s): no details provided. Author confirmed they were licensed Clinical Psychologists and Masters level therapists. Mode of delivery: Telephone Duration: 3‐4 separate educational sessions (30‐60 minutes each), evenly dispersed throughout the 10‐week TH‐CBT treatment period. Content: TH‐CBT will be delivered to the participant with PD and works by teaching people with PD (PWP) the coping skills needed to manage their emotional reactions to the numerous challenges posed by the disease (specifically, the treatment targets maladaptive thought patterns (e.g. I have no control; I am helpless) and behaviours (e.g. social isolation, lack of exercise, poor sleep habits, excessive worry)), and, critically, provides caregivers with the tools needed to encourage the PWPs' practice of their newly acquired coping skills.The study treatment provided to the care‐partner will teach the care‐partner how to best support the participant with PD as he/she tries to incorporate the information learned during the study treatment, in day‐to‐day life. The care‐partner will be asked to participate in separate sessions. Standardisation: no details provided Comparison group: enhanced usual care (routine medical treatment with the provision of written educational materials for effective coping with PD, the close clinical monitoring of depressive symptoms by study staff, and the provision of counselling resources in the local community). Participants assigned to the control group with have the opportunity to receive the experimental intervention (TH‐CBT) after the data collection period (e.g. after the 6‐month follow‐up evaluation). |
| Outcomes | Caregiver distress inventory (confirmed by author via email) |
| Starting date | July 2015 |
| Contact information | Roseanne D Dobkin, PhD email: [email protected] |
| Notes | Roseanne Dobkin contacted and confirmed that no data are available to share for this review. |
| Trial name or title | Talking Time: telephone support groups for informal caregivers of people with dementia |
| Methods | Cluster‐adjusted randomised controlled trial |
| Participants | Caregivers are eligible if they are 18 or older, have cared for the PwD for at least four hours on four days per week in the last six months, have access to a telephone connection for participation in the intervention and study evaluation. Exclusion criteria are lack of knowledge of the German language of informal caregiver, risk of suicide in the informal caregiver, actual psychiatric diagnosis of mental illness of the caregiver and ICD‐10 diagnosis of 'dementia in other diseases classified elsewhere', except dementia in primary Parkinson disease and Lewy Body disease. |
| Interventions | Aim: The Talking Time project aims to close the supply gap (i.e. caregivers ability to attend on‐site support groups) by providing structured telephone‐based support groups in Germany for the first time. Interventionist(s): no details provided Mode of delivery: Telephone Duration: Three months Title of intervention: Telephone‐based structured support groups Content:Telephone‐based Support Groups, information booklet, and telephone‐based preparatory meeting prior to the telephone‐based support groups Standardisation: no details provided Comparison group: Usual care (intervention as experimental group after T1 data collection (end of intervention, after 3 months). |
| Outcomes | 1. Well‐being: Subjective well‐being using the Mental Component Summary of the General Health Questionaires Short Form 12 (SF‐12), psychological quality of life of the caregivers 2. Physical Component Summary of the SF‐12, physical quality of life of the caregivers 3. Social support: Perceived Social Support Caregiving Scale, perceived social support of the caregivers 4. Burden: Caregiver Reaction Scale, caregivers burden Data were collected at baseline and T1 (end of intervention, the 3‐month time point). |
| Starting date | November 2015 |
| Contact information | Martin Berwig, Dr. University of Leipzig email: [email protected]‐leipzig.de |
| Notes | Dr. Berwig has confirmed that the trial is at the data analysis stage. |
| Trial name or title | The Tele.TAnDem intervention: study protocol for a psychotherapeutic intervention for family caregivers of people with dementia |
| Methods | Non‐blinded two‐armed parallel RCT |
| Participants | Caregiving partners, children and children‐in‐law who have key responsibility for the relative with at least a low grade dementia diagnosis. Caregivers are excluded if they are in receipt of ongoing psychotherapeutic treatment, have a severe physical illness/medically diagnosed psychiatric disorder or the person with dementia is institutionalised or institutionalisation is planned for the next 6 months. |
| Interventions | Aim: The primary objective was to evaluate whether telephone‐based cognitive‐behavioural therapy (TEL) improves depressiveness, burden of care, health complaints, and problem‐solving ability compared to usual care. Interventionist(s): Psychotherapists Mode of delivery: Telephone Duration: 6 months (weekly for 4 weeks, two‐weekly for 6 further sessions and monthly for the last two sessions) Title of intervention: Cognitive‐behavioural telephone‐based intervention for family caregivers of people with dementia. Content: The intervention is based on the principles and methods used in cognitive behavioural therapy. Therapy strategies were adapted for caregivers of people with dementia. The intervention which is standardised and manualised consists of 10 different therapy modules individualised by the therapist to the needs of each participant. Standardisation: according to the manual Comparison group: usual care |
| Outcomes | 1. Quality of life using the WHOQoL‐BREF, a standardised and normed questionnaire with 26 items measuring subjective physical and mental well‐being as well as satisfaction with social relations and the environment 2. Burden: A self‐developed thermometer scale (0‐100, vertical) 3. Depression: A self‐developed thermometer scale (0‐100, vertical) and the Allgemeine Depressionsskala (ADS). ADS consists of 20 item covering emotional, motivational, cognitive, and somatic aspects. 4. Physical health: complaints assessed on four domains (fatigue, stomach problems, heart problems, and joint pain) by using the Gießener Beschwerdebogen instrument. 5. Problem‐solving using the Goal Attainment Scaling, a non‐standardised manual‐based instrument providing process‐orientated information on how far participants are from reaching individual therapy goals 6. Anxiety: The anxiety subscale of the Hospital Anxiety and Depression Scale 7. Cost: Cost‐effectiveness analysis will be conducted from the perspective of statutory health insurance with a time horizon of 6 months. This consisted of the costs of the intervention and of the health care utilisation of the caregiving relatives. The latter were assessed by the FIMA questionnaire. Time spent on informal care was measured by a modified version of the Resource Utilisation in Dementia (RUD) questionnaire. Effectiveness was measured using the subjectively rated health status of caregiving relatives and quality of life, measured through the EQ‐5D. Data were collected at T1, end of intervention (6‐month time point) and T2, 12 months (the 6‐month follow‐up time point). |
| Starting date | Not stated |
| Contact information | Renate Soellner email:soellner@uni‐hildesheim.de |
| Notes | Findings for this study were not published at the time of our search. |
| Trial name or title | The Tele.TAnDem Intervention: telephone‐based CBT for family caregivers of people with dementia |
| Methods | Randomised trial |
| Participants | Family caregivers of people with dementia |
| Interventions | Title of the intervention: CBT‐based telephone intervention Aim: To improve caregiver depressiveness, burden of care, health complaints, and problem‐solving Interventionist(s): Psychotherapists Mode of delivery: Telephone Duration: Six months (12 50‐minute therapy sessions, weekly first 4 sessions, biweekly for 6 sessions, monthly for the two last sessions) Content: Cognitive behaviour therapy consisting of 10 different therapy modules which could be used and combined by the therapist according to the individual needs of the participant Standardisation: Standardised and manual‐based Comparison group: Usual care group. Received written information on dementia and caregiving |
| Outcomes | 1. Burden: A self‐developed thermometer scale (0‐100, vertical) 2. Depression: The German Version of the Center for Epidemiologic Studies Depression Scale 3. Emotional well‐being: Visual analogue scale (0‐100) 4. Physical health: The four domains (fatigue, stomach problems, heart problems, and joint pain) by using the Gießener Beschwerdebogen instrument 5. Coping: Coping with burden of care (single item rating scale 0‐4); coping with challenging behaviour (single item from the German Version of BEHAVE‐AD rating scale 0‐4). Data were collected at T1, end of intervention (6‐month time point) and T2, 12 months (6‐month follow‐up). |
| Starting date | Not stated |
| Contact information | Gabriele Wilz email: gabriele.wilz@uni‐jena.de |
| Notes | Draws on the work of Soellner 2015; the design has been changed. Full paper published in 2018 following completion and submission of the review; to be evaluated for inclusion in the next update of this review. |
AD: Alzheimer's disease
ADS: Allgemeine Depressionsskala
AMD: Age‐related macular degeneration
BEHAVE‐AD: Behavioral pathology in alzheimer’s disease rating scale
BHL: Behavioural health laboratory
CBS: Caregiver burden scale
CES‐D: Center for epidemiological depression scale
CM: care manager
dPD: Depression in Parkinson's disease
EQ‐5D: EuroQol health related quality of life ‐ 5 dimensions
EQ‐5D‐5L: EuroQol health related quality of life ‐ 5 dimensions ‐5 levels
EUROQoL: EuroQol health related quality of life
FIMA: Questionnaire for the use of medical and non‐medical services in old age
GP: General practitioner
ICD‐10: International statistical classification of disease ‐ 10
M‐CBT: Mail‐delivered cognitive behavioural therapy
MCS: Mental component summary
M‐CSI: Modified caregiver strain index
MSc: Master of science
PCP: Primary care provider
PD: Parkinson's disease
PwD: People with dementia
PWP: Persons with Parkinson's
RMBPC: Revised memory and behavior problems checklist
RUD: Resource utilisation in dementia
SF‐12: Short Form ‐ 12
SF‐36 v2: Short Form ‐36 version 2
SRAHP: Self‐rated abilities for health practices scale
TALK: Definition unable to be found, may not be an acronym
TAP‐VA: Tailored activity program – veterans administration
TEL: Telephone‐based cognitive‐behavioural therapy
Tele.TAnDem: Telephone‐based short‐term intervention for family caregivers of people with dementia
TEP: Telehealth education program
TH‐CBT: Telephone‐based cognitive behavioural therapy
T1: Time 1
T2: Time 2
VA: Veteran Affairs
WHOQoL‐BREF: World Health Organisation Quality of Life Abbreviated Version
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quality of Life Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Telephone intervention versus Usual care, Outcome 1 Quality of Life. | ||||
| 1.1 Quality of life (End of intervention) | 4 | 364 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.24, 0.19] |
| 2 Quality of life (Short‐term follow‐up) Show forest plot | 1 | 128 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐4.43, 4.43] |
| Analysis 1.2  Comparison 1 Telephone intervention versus Usual care, Outcome 2 Quality of life (Short‐term follow‐up). | ||||
| 2.1 Quality of life (Short‐term follow‐up ≤ 3 months) | 1 | 128 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐4.43, 4.43] |
| 3 Burden Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Telephone intervention versus Usual care, Outcome 3 Burden. | ||||
| 3.1 End of intervention | 9 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.30, 0.07] |
| 3.2 Medium‐term follow up > 3 to ≤ 6 months | 2 | 147 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.32, 0.33] |
| 4 Burden (Short‐term follow‐up) Show forest plot | 1 | 128 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.75, 0.35] |
| Analysis 1.4  Comparison 1 Telephone intervention versus Usual care, Outcome 4 Burden (Short‐term follow‐up). | ||||
| 4.1 Short‐term follow‐up ≤ 3 months | 1 | 128 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.75, 0.35] |
| 5 Skill acquisition: Problem‐Solving Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 Telephone intervention versus Usual care, Outcome 5 Skill acquisition: Problem‐Solving. | ||||
| 5.1 End of intervention | 3 | 236 | Std. Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.21, 0.71] |
| 6 Skill acquisition: Preparedness to Care Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.6  Comparison 1 Telephone intervention versus Usual care, Outcome 6 Skill acquisition: Preparedness to Care. | ||||
| 6.1 End of intervention | 2 | 208 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [0.09, 0.64] |
| 7 Skill acquisition: Preparedness to Care (medium‐term follow‐up) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 Telephone intervention versus Usual care, Outcome 7 Skill acquisition: Preparedness to Care (medium‐term follow‐up). | ||||
| 7.1 Medium‐term follow‐up > 3 months to ≤ 6 months | 1 | 17 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.02, 0.42] |
| 8 Skill acquisition:Competence Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.8  Comparison 1 Telephone intervention versus Usual care, Outcome 8 Skill acquisition:Competence. | ||||
| 8.1 End of intervention | 1 | 107 | Mean Difference (IV, Random, 95% CI) | 4.10 [‐2.19, 10.39] |
| 9 Psychological health: Depression Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.9  Comparison 1 Telephone intervention versus Usual care, Outcome 9 Psychological health: Depression. | ||||
| 9.1 End of intervention | 9 | 792 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.70, ‐0.05] |
| 9.2 Medium‐term follow‐up > 3 months to ≤ 6 months | 3 | 227 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.56, 0.45] |
| 10 Psychological health: Anxiety Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.10  Comparison 1 Telephone intervention versus Usual care, Outcome 10 Psychological health: Anxiety. | ||||
| 10.1 End of intervention | 1 | 61 | Mean Difference (IV, Random, 95% CI) | ‐4.00 [‐11.68, ‐0.32] |
| 11 Psychological health: Coping Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.11  Comparison 1 Telephone intervention versus Usual care, Outcome 11 Psychological health: Coping. | ||||
| 11.1 End of intervention | 1 | 121 | Mean Difference (IV, Random, 95% CI) | 1.0 [‐0.45, 2.45] |
| 12 Psychological health: Stress Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.12  Comparison 1 Telephone intervention versus Usual care, Outcome 12 Psychological health: Stress. | ||||
| 12.1 End of intervention | 1 | 137 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.30, 0.10] |
| 12.2 Medium‐term follow‐up > 3 to ≤ 6 months | 1 | 130 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.11, 0.31] |
| 13 Knowledge and understanding: Knowledge Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.13  Comparison 1 Telephone intervention versus Usual care, Outcome 13 Knowledge and understanding: Knowledge. | ||||
| 13.1 End of intervention | 1 | 61 | Mean Difference (IV, Random, 95% CI) | 1.90 [‐0.63, 4.43] |
| 14 Health status and well‐being: Physical health Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.14  Comparison 1 Telephone intervention versus Usual care, Outcome 14 Health status and well‐being: Physical health. | ||||
| 14.1 End of intervention | 2 | 248 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.35, 0.17] |
| 15 Health status and well‐being: Self‐efficacy Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.15  Comparison 1 Telephone intervention versus Usual care, Outcome 15 Health status and well‐being: Self‐efficacy. | ||||
| 15.1 End of intervention | 2 | 175 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.26, 0.33] |
| 16 Health status and well‐being: Self‐efficacy (Medium‐term follow‐up) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.16  Comparison 1 Telephone intervention versus Usual care, Outcome 16 Health status and well‐being: Self‐efficacy (Medium‐term follow‐up). | ||||
| 16.1 Medium‐term follow‐up > 3 to ≤ 6 months | 1 | 130 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.29, 0.29] |
| 17 Health status and well‐being: Social activity Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.17  Comparison 1 Telephone intervention versus Usual care, Outcome 17 Health status and well‐being: Social activity. | ||||
| 17.1 End of intervention | 1 | 121 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.10, 0.18] |
| 18 Satisfaction: Satisfaction with supports Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.18  Comparison 1 Telephone intervention versus Usual care, Outcome 18 Satisfaction: Satisfaction with supports. | ||||
| 18.1 End of intervention | 3 | 291 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.24, 0.44] |
| 19 Family functioning Show forest plot | 1 | 141 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.04, 0.44] |
| Analysis 1.19  Comparison 1 Telephone intervention versus Usual care, Outcome 19 Family functioning. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Burden Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Telephone versus non‐telephone support intervention, Outcome 1 Burden. | ||||
| 1.1 End of intervention | 1 | 11 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.74, 0.34] |
| 2 Depression Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.2  Comparison 2 Telephone versus non‐telephone support intervention, Outcome 2 Depression. | ||||
| 2.1 End of intervention | 1 | 11 | Mean Difference (IV, Random, 95% CI) | ‐4.3 [‐9.57, 0.97] |
| 2.2 Unknown time point | 1 | 45 | Mean Difference (IV, Random, 95% CI) | 1.20 [‐5.35, 7.75] |
| 3 Stress Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.3  Comparison 2 Telephone versus non‐telephone support intervention, Outcome 3 Stress. | ||||
| 3.1 Unknown time point | 1 | 45 | Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐3.17, 1.97] |
| 4 Physical Health Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.4  Comparison 2 Telephone versus non‐telephone support intervention, Outcome 4 Physical Health. | ||||
| 4.1 End of intervention | 1 | 11 | Mean Difference (IV, Random, 95% CI) | 1.9 [‐0.65, 4.45] |
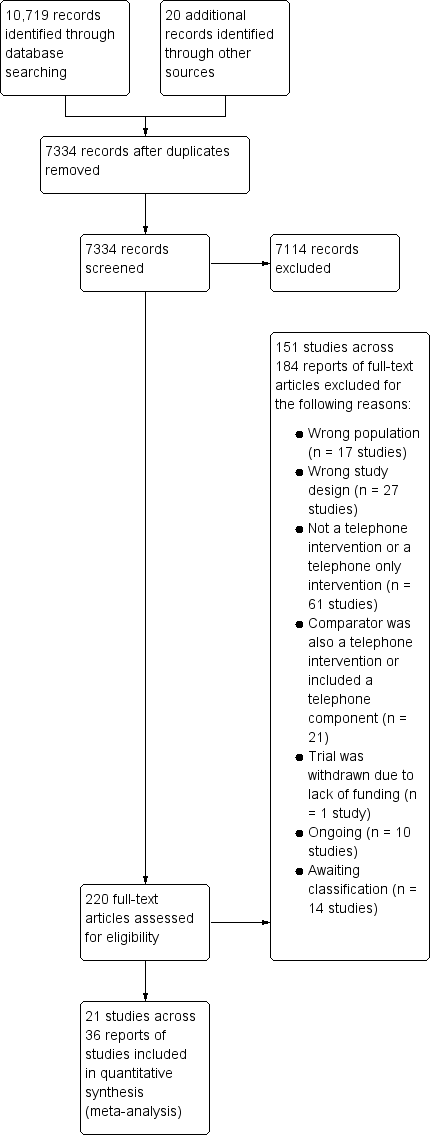
Study flow diagram.
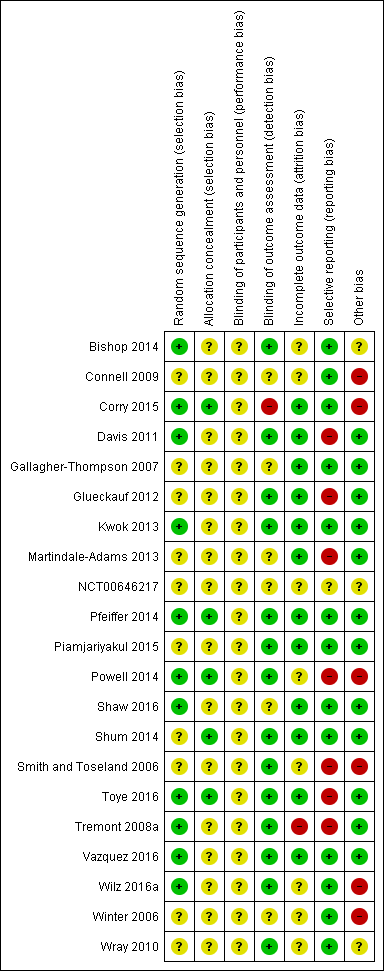
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
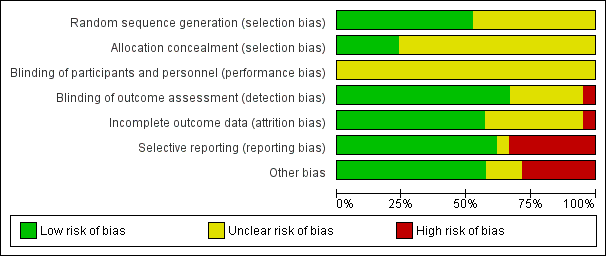
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
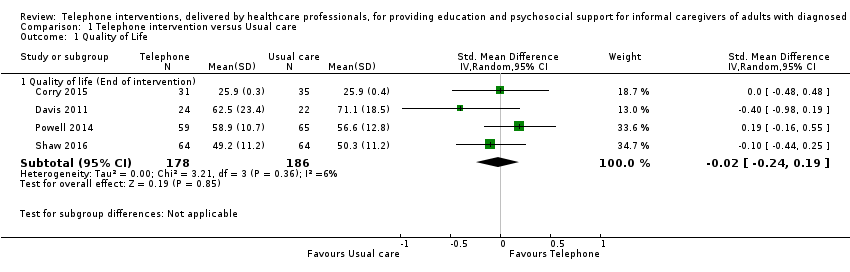
Comparison 1 Telephone intervention versus Usual care, Outcome 1 Quality of Life.
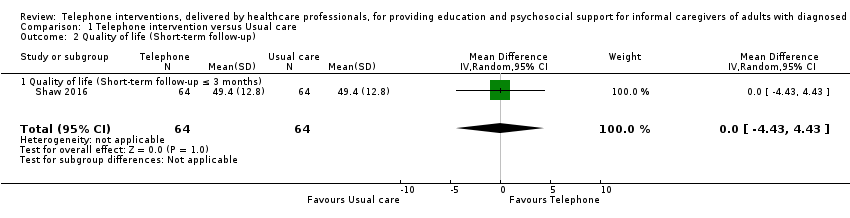
Comparison 1 Telephone intervention versus Usual care, Outcome 2 Quality of life (Short‐term follow‐up).

Comparison 1 Telephone intervention versus Usual care, Outcome 3 Burden.
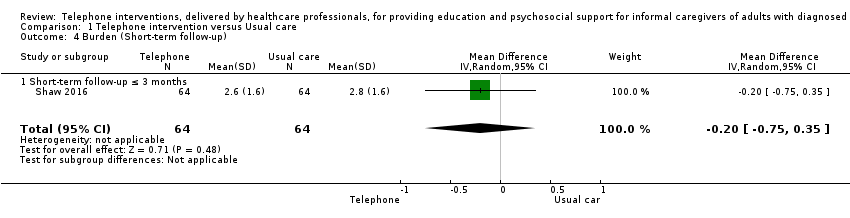
Comparison 1 Telephone intervention versus Usual care, Outcome 4 Burden (Short‐term follow‐up).
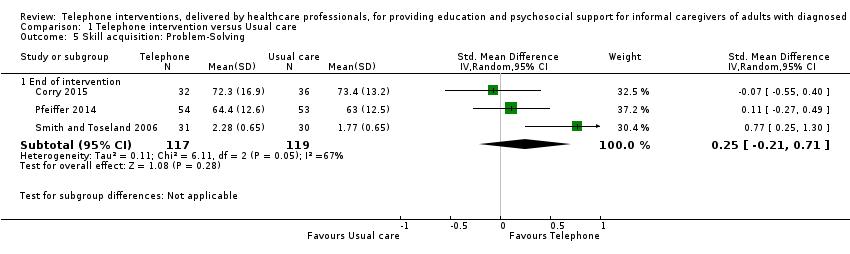
Comparison 1 Telephone intervention versus Usual care, Outcome 5 Skill acquisition: Problem‐Solving.

Comparison 1 Telephone intervention versus Usual care, Outcome 6 Skill acquisition: Preparedness to Care.

Comparison 1 Telephone intervention versus Usual care, Outcome 7 Skill acquisition: Preparedness to Care (medium‐term follow‐up).
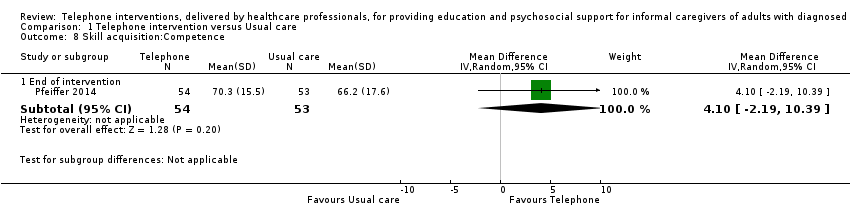
Comparison 1 Telephone intervention versus Usual care, Outcome 8 Skill acquisition:Competence.
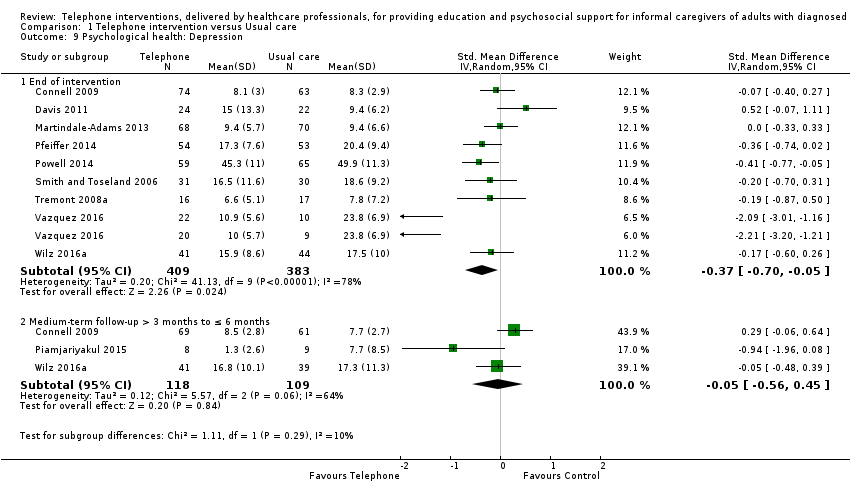
Comparison 1 Telephone intervention versus Usual care, Outcome 9 Psychological health: Depression.

Comparison 1 Telephone intervention versus Usual care, Outcome 10 Psychological health: Anxiety.

Comparison 1 Telephone intervention versus Usual care, Outcome 11 Psychological health: Coping.
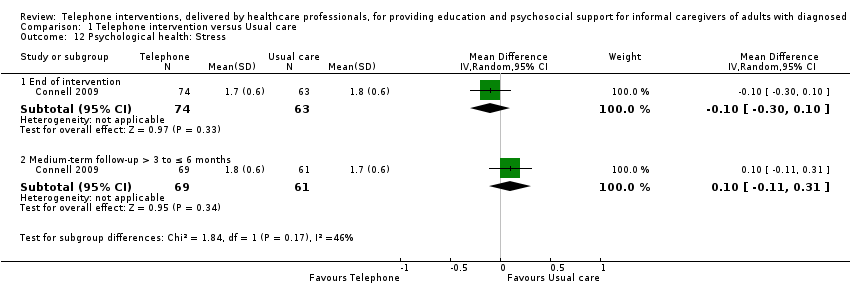
Comparison 1 Telephone intervention versus Usual care, Outcome 12 Psychological health: Stress.
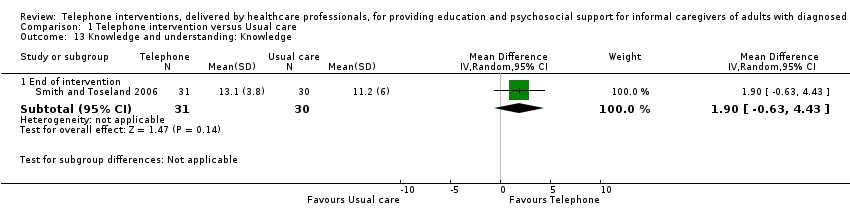
Comparison 1 Telephone intervention versus Usual care, Outcome 13 Knowledge and understanding: Knowledge.

Comparison 1 Telephone intervention versus Usual care, Outcome 14 Health status and well‐being: Physical health.

Comparison 1 Telephone intervention versus Usual care, Outcome 15 Health status and well‐being: Self‐efficacy.
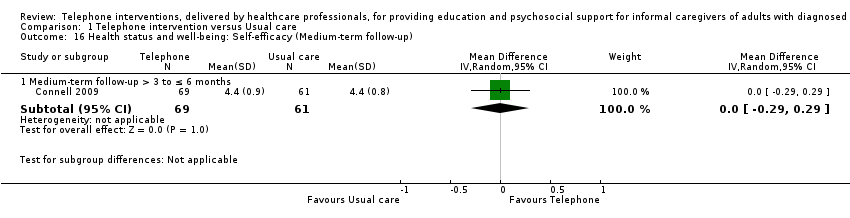
Comparison 1 Telephone intervention versus Usual care, Outcome 16 Health status and well‐being: Self‐efficacy (Medium‐term follow‐up).
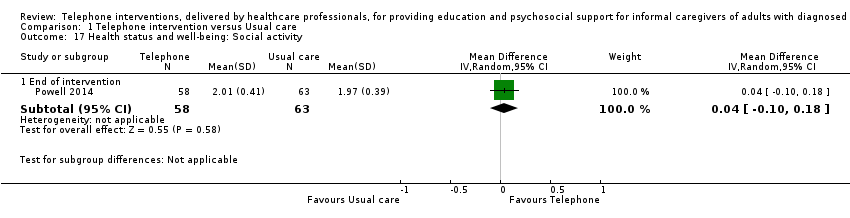
Comparison 1 Telephone intervention versus Usual care, Outcome 17 Health status and well‐being: Social activity.

Comparison 1 Telephone intervention versus Usual care, Outcome 18 Satisfaction: Satisfaction with supports.
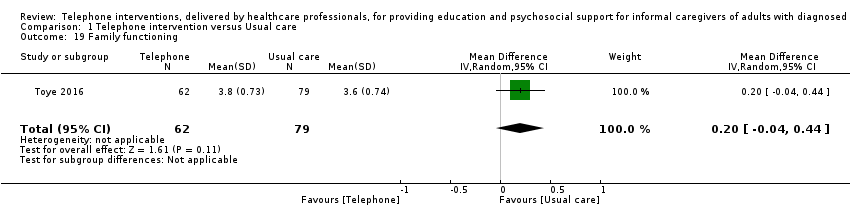
Comparison 1 Telephone intervention versus Usual care, Outcome 19 Family functioning.

Comparison 2 Telephone versus non‐telephone support intervention, Outcome 1 Burden.

Comparison 2 Telephone versus non‐telephone support intervention, Outcome 2 Depression.
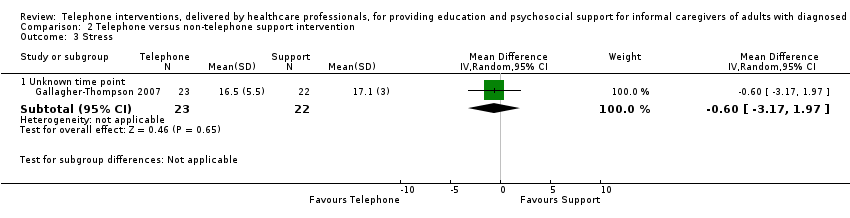
Comparison 2 Telephone versus non‐telephone support intervention, Outcome 3 Stress.
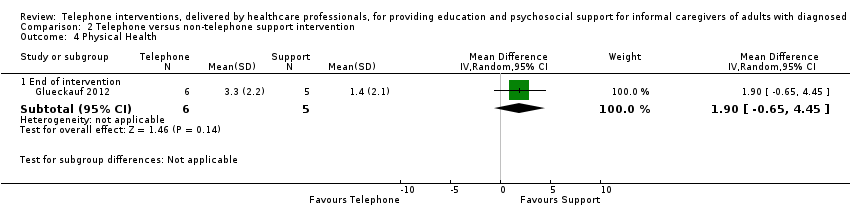
Comparison 2 Telephone versus non‐telephone support intervention, Outcome 4 Physical Health.
| Telephone intervention compared to Usual care for providing education and psychosocial support for informal caregivers of adults with diagnosed illnesses | ||||
| Patient or population: Informal caregivers of adults with diagnosed illnesses | ||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants | Certainty of the evidence | Comments |
| Risk with Telephone intervention | ||||
| Quality of Life End of intervention For all scales, higher scores indicated higher QoL. | The mean score for QoL in the intervention group was 0.02 standard deviations lower (0.24 lower to 0.19 higher) | 364 | ⊕⊕⊕⊝ | One further study reported that caregivers receiving a telephone intervention may have slightly higher QoL at end of intervention, compared with usual care. Overall, at the end of intervention, telephone interventions probably have little or no effect on caregiver QoL |
| Burden End of intervention Assessed with: Revised Memory and Behaviour Problem Checklist (0‐24 range), 24‐ and 26‐item Caregiver Reaction Assessment, Family Appraisal of Caregiving Questionnaire (Caregiver Strain subscale – Palliative Care), Burden Interview (22‐ and 12‐item inventories; 0‐4 scale), Modified BKOS scale (22‐item, 5‐point scale) For all scales, higher scores indicated higher burden. | The mean score for Burden in the telephone group was 0.11 standard deviations lower | 788 | ⊕⊕⊝⊝ | Two further studies reported caregiver burden. One reported that telephone interventions may decrease burden; the other reported no change in the intervention group, compared with usual care. Overall, at the end of intervention, telephone interventions may have little or no effect on caregiver burden. |
| Psychological health: Depression End of intervention Assessed with: Center for Epidemiologic Studies Depression Scale 11‐item SF, 10‐item and, 20‐item measures (including German version) (0‐3 scales), Brief Symptom Inventory (18‐item, 5‐point scale), and the Geriatric Depression Scale (30‐item, score range 0‐30) For all scales, higher scores were associated with increased depression/symptoms of depression. | The mean score for depression in the telephone group was 0.37 standard deviations lower (0.7 to 0.05 lower ) | 792 | ⊕⊝⊝⊝ | Three further studies reported caregiver depression. One reported that telephone interventions may decrease depression; the other two reported no change in the intervention group, compared with usual care. Overall, we are uncertain of the effects of telephone interventions on caregiver depression at the end of intervention. |
| Satisfaction with the intervention End of intervention | See comment | ‐ | ‐ | No study was found that assessed this outcome comparatively. Six studies measured satisfaction with the intervention in the intervention group only. All six reported high levels of satisfaction with the intervention (i.e. 'mostly', 'very much so', 'good' or 'excellent'). |
| Adverse events including suicide and suicide ideation | See comment | ‐ | ‐ | No studies measured these outcomes. |
| GRADE Working Group grades of evidence | ||||
| 1 Although participant numbers were relatively few at n = 364, they were deemed sufficient for studies evaluating these types of intervention in a population of informal caregivers; we therefore did not downgrade on sample size (imprecision) for this reason. 2 Most information was from studies at low or unclear risk of bias on most items in the 'risk of bias' tool, although in some studies, one or two risk of bias criteria were assessed as having high risk of bias. We therefore downgraded by 1 level for plausible risk of bias that could seriously alter the results. 3 Some variation in the effect estimates and moderate heterogeneity; evidence downgraded by 1 level (serious inconsistency). 4 Variation in the effect estimates across studies and substantial heterogeneity; evidence downgraded by 2 levels (very serious inconsistency). BKOS: Bakas Caregiver Outcomes Scale | ||||
| Telephone compared to non‐telephone support intervention for providing education and psychosocial support for informal caregivers of adults with diagnosed illnesses | ||||
| Patient or population: Informal caregivers of adults with diagnosed illnesses | ||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants | Certainty of the evidence | Comments |
| Risk with Telephone | ||||
| Quality of Life | No studies measured this outcome | ‐ | ‐ | |
| Burden End of intervention Higher scores indicated greater burden. | The mean score for burden in the telephone group was 0.2 lower | 11 | ⊕⊝⊝⊝ | We are uncertain of the effects of telephone interventions on caregiver burden at the end of intervention. |
| Psychological health: Depression: End of intervention Assessed with: Center for Epidemiological Studies Survey‐Depression scale (20‐item, 0‐3 scale) Higher scores indicated higher levels of depression. | The mean score for depression in the telephone group was 4.3 lower (9.57 lower to 0.97 higher) | 11 | ⊕⊝⊝⊝ | We are uncertain of the effects of telephone interventions on caregiver depression at the end of intervention |
| Satisfaction with the intervention | No studies measured this outcome | ‐ | ‐ | |
| Adverse events including suicide and suicide ideation | No studies measured these outcomes | ‐ | ‐ | |
| GRADE Working Group grades of evidence | ||||
| 1 Most information from the 1 included study indicated low or unclear risk of bias on most items on the 'risk of bias' tool, although risk of bias was high for selective reporting. We therefore downgraded by 1 level for plausible risk of bias that could seriously alter the results. 2 Participant numbers were deemed insufficient at 11 and the upper and lower CI limits were > 0.5 from the effect size (downgraded by 2 levels for imprecision). | ||||
| Y=YES, PY=Partly YES, N=NO | |||||||||||||||||||||||
| ITEM | 1 | 2* | 3 | 4 | 5* | 6* | 7 | 8* | 9 | 10 | 11 | 12* | 13 | 14 | 15 | 16 | 17 | 18 | 19* | 20 | 21 | 22 | Overall rating |
| Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | PY | N | Y | PY | Y | Y | Y | N | N/A | High | |
| PY | PY | PY | Y | PY | PY | Y | PY | N | Y | N | N | N | N | N/A | Y | N | Y | Y | N | N | N/A | Medium | |
| Y | Y | Y | Y | Y | Y | Y | N/A | Y | Y | N | Y | PY | PY | N/A | Y | N | Y | Y | Y | Y | PY | Medium | |
| Y | Y | PY | Y | Y | PY | Y | N | N/A | N/A | Y | N | PY | N | Y | PY | N | Y | Y | Y | PY | N | Medium | |
| Y | PY | PY | N | PY | PY | N/A | N | N | N | N | N | N | N | N/A | N | N | N | Y | N | N | N/A | Low | |
| Y | Y | Y | Y | Y | Y | PY | Y | PY | Y | N | N | N | PY | N/A | Y | Y | Y | Y | Y | N | N/A | High | |
| Y | PY | Y | PY | PY | PY | N/A | N | N | N | N/A | N | N | Y | N | N | N | N | N | N/A | N | N/A | Low | |
| Y | PY | Y | PY | PY | PY | Y | N | N | Y | N | N | N | N | Y | N | N | Y | N | N/A | N | N/A | Medium | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | No information | |
| PY | PY | Y | N | PY | PY | PY | PY | N | N | PY | N | N | N | PY | N | N | N | PY | N | N | N | Medium | |
| Y | Y | Y | Y | Y | PY | Y | PY | N/A | PY | Y | N | PY | N | N/A | PY | Y | PY | Y | N | N | N/A | Medium | |
| Y | PY | Y | PY | PY | PY | Y | N | N/A | N/A | Y | N | N | N | Y | PY | Y | Y | PY | Y | PY | N | Medium | |
| Y | PY | Y | Y | Y | PY | Y | Y | N/A | N/A | Y | N | N | N | PY | Y | N | N | Y | N | N | N/A | Medium | |
| Y | PY | Y | N | PY | PY | Y | PY | N/A | PY | Y | N | N | N | Y | PY | PY | PY | Y | N | PY | N | Medium | |
| Y | PY | Y | PY | PY | Y | Y | PY | N/A | N/A | N/A | N | PY | N | Y | PY | N | Y | Y | PY | PY | N | Medium | |
| Y | PY | Y | PY | Y | PY | Y | Y | N/A | N/A | PY | N | N | N | Y | PY | PY | Y | Y | N | PY | PY | Medium | |
| Y | Y | Y | PY | Y | PY | PY | PY | N | Y | NA | N | N | N | Y | Y | Y | Y | Y | Y | N | N/A | Medium | |
| Y | Y | Y | PY | Y | PY | N/A | PY | Y | PY | PY | N | N | PY | Y | Y | Y | Y | Y | N | N | N/A | Medium | |
| Y | PY | Y | PY | Y | PY | PY | PY | Y | Y | N/A | N | N | PY | PY | Y | Y | Y | Y | Y | N | N/A | Medium | |
| Y | Y | Y | N | PY | Y | N/A | PY | N/A | N | N/A | N | N | N | N/A | N | N | N | N | N/A | N | N/A | Medium | |
| Y | Y | Y | N | Y | Y | PY | PY | PY | N | PY | N | N | N | N | PY | N | N | N | N/A | N | N/A | Medium | |
| Items assessed (Inclusion of detail for all Items with a * was essential for a high rating) 1. Did the researchers/authors provide a clear definition of the intervention so it could be replicated?* (this should include type, overview of content but very in‐depth details such as the manual do not have to be included) 2. Were the aims/goal of the intervention clearly stated?* (the aim/goal of the intervention may be the same/similar to the goal of the study) 3. Did the researchers/authors provide clear rationale for the intervention? 4. Did the researchers/authors provide an overview of the theory underpinning the intervention/framework used to develop the intervention? 5. Was the content of the intervention consistent with the stated aim/goal of the intervention?* 6. Was a clear description provided of how (method) the intervention was delivered? (e.g. phoned using mobile phone, skype, landline)* 7. If appropriate, did the researchers/authors provide an overview of other materials used e.g. Guidebook, information sent by post, etc? 8. Did the researchers/authors justify the selection of interventionists?* (e.g. appropriateness in terms of professional background/education of the person delivering the intervention) 9. If relevant, did the researchers/authors provide appropriate justification for the selection of co‐interventionists? 10. If more than one interventionist was involved in delivery of the intervention, did the researchers/authors indicate how delivery of the intervention was standardised across interventionists?* 11. Did the researchers/authors indicate that the intervention was delivered at an appropriate time period for the caregivers, which was in accordance to the overall goal? (e.g. if the goal is to support caregivers who are new to the role then it should be delivered during the early stages of caregiving) 12. Was there any potential risk of intervention contamination across the study groups?* 13. Did the researchers/authors justify the intensity of the intervention (in terms of frequency of delivery and duration of each session)? 14. Duration: Did the researchers/authors indicate that the complete intervention was delivered to the participants i.e. 100% of the intervention was delivered? 15. If the intervention was tailored/modified/adapted, did the researchers/authors indicate why? what? and how? 16. Did the researchers assess consistency in intervention delivery? 17. Did the researchers/authors state that the intervention was delivered in accordance with the trial protocol? 18. Was interventionist training standardised? 19. Did the authors indicate that intervention delivery was monitored?* 20. If yes/PY to item 19, was intervention delivery monitored using an objective measure? 21. Did the authors indicate that caregiver receipt of the intervention was monitored? (i.e. Caregivers’ understanding of and use of the intervention) 22. If ‘yes/PY’ to item 21, was caregiver receipt of the intervention monitored using an objective measure? | |||||||||||||||||||||||
| N/A: not applicable | |||||||||||||||||||||||
| Sequence generation | Allocation concealment | Blinding | Incomplete outcome data (attrition bias) | Selective outcome reporting (reporting bias) | Other potential sources of bias | ||
| Burden | Low | ||||||
| High | |||||||
| Unclear | |||||||
| Psychological Health: Depression | Low | ||||||
| High | |||||||
| Unclear | |||||||
| Psychological Health: Stress | Low | ||||||
| High | |||||||
| Unclear | |||||||
| Health Status and Well‐Being: Physical Health | Low | ||||||
| High | |||||||
| Unclear | |||||||
| Health Status and Well‐Being: Self‐efficacy | Low | ||||||
| High | |||||||
| Unclear | |||||||
| Outcome and time point | Study | Result (as presented by study authors) | Notes/comments |
| QoL End of intervention | Intervention group mean 67.87, n = 70, versus control group mean 67.42, n = 69 | No data available for each group SD or 95% CI | |
| Short‐term | Intervention group mean 73.25 versus control group 70.84, N = 140 | Reported numbers assessed by group, n = 68 intervention group and n = 67 control group. No data available for each group SD or 95% CI | |
| Burden End of intervention | Intervention group mean 17.37, n = 70 versus control group mean 26.26, n = 69, P < 0.001 | No data available for each group SD. Reported mean change data with 95% CI | |
| Mean and SD: Intervention group mean 31.7, SD 15.2 versus control group mean 31.7, SD 17.3, N = 81, P = 0.49 | No data available for the numbers by study group. No response from author contact | ||
| Short‐term | Intervention group mean 8.6 versus control group mean 17.34, N = 140, P < 0.001 | Reported numbers assessed by group, n = 68 intervention group and n = 67 control group. No data available for each group SD | |
| Skill Acquisition: Competence End of intervention | Intervention group mean 13.52, SD 2.85 versus control mean 14.17, SD 2.57, total N = 94, P = 0.932 | No data available for the numbers by study group. No response from author contact | |
| Psychological Health: Caregiver Depression End of intervention | Intervention group mean 18.17, SD 7.19 versus control group 20.2, SD 7.2, N = 94, P = 0.121 | No data available for the numbers by study group. No response from author contact | |
| Intervention group mean 4.57, n = 70 versus control group mean 7.45, n = 69, P = 0.013 | No data available for each group SD | ||
| intervention mean ‐0.16, SD 2.6 versus control mean ‐1.22, SD 3.1, P > 0.05 | Mean change data from baseline only provided. No mean difference for each arm available. No data available for the numbers in each group, SD or 95% CI | ||
| Psychological Health: Caregiver Depression Short‐term | Intervention group mean 2.41, versus control group mean 4.21, N = 70, P = 0.144 | Reported numbers assessed by group, n = 68 intervention group and n = 67 control group. No data available for each group SD | |
| Psychological Health: Caregiver Anxiety End of intervention | Intervention group mean 3.97, n = 70 versus control group 6.41, n = 69 | No data available for each group SD or 95% CI | |
| Short‐term | Intervention group mean 1.15 versus control group 2.90, N = 140 | Reported numbers assessed by group, n = 68 intervention group and n = 67 control group. No data available for each group SD or 95% CI | |
| Psychological Health: Caregiver Stress End of intervention | Intervention group mean 9.06, n =70 versus control group 12.45, n = 69 | Reported numbers assessed by group, n = 68 intervention group and n = 67 control group. No SD or 95% CI | |
| Short‐term | Intervention group mean 3.71 versus control group 7.79, N = 140 | Reported numbers assessed by group, n = 68 intervention group and n = 67 control group. No data available for each group SD or 95% CI | |
| Health Status and Well‐Being: Physical Health End of intervention | Mean change ‐0.84, SD 4.5 intervention and mean change 1.74, SD 3.8 control group; P < 0.10 | Mean change data only provided. No participant number, means or standard deviation score reported. No response from author contact | |
| Family Functioning End of intervention | Mean change scores from baseline of 2.7, SD 6.4 and ‐2.8, SD 4.0: P < 0.05 | Mean change data from baseline only provided. No mean difference for each arm available. No participant number, means or standard deviation score reported. No response from author contact | |
| Cost End of intervention | Intervention mean 352.53 Australian Dollars, SD = 81.5, n = 62 versus control mean 15.89 Australian Dollars, SD = N/A, n = 69 | Reported figures for total acute care costs which included hospital admissions, ED presentations, and ambulance services, and were not isolated to the intervention costs. Communication with the author resulted in retrieving further cost data specific to intervention costs (e.g. nurses time, cost, of training and telephone charges, etc). | |
| Short‐term | Mean (SD) and study numbers (US Dollars): Intervention mean 7008.3 SD 9226.2, n = 83 versus control mean 8831.4 SD 13,245.8, n = 75 | Cost utility analysis, mean, SD and study group numbers provided by the authors | |
| Medium‐term | Mean (SD) and study numbers (US Dollars): Intervention mean 6783.9, SD 7767, n = 83 versus control mean 5648, SD 6353.4, n = 75 | ||
| CI:Confidence interval | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quality of Life Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Quality of life (End of intervention) | 4 | 364 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.24, 0.19] |
| 2 Quality of life (Short‐term follow‐up) Show forest plot | 1 | 128 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐4.43, 4.43] |
| 2.1 Quality of life (Short‐term follow‐up ≤ 3 months) | 1 | 128 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐4.43, 4.43] |
| 3 Burden Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 End of intervention | 9 | 788 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.30, 0.07] |
| 3.2 Medium‐term follow up > 3 to ≤ 6 months | 2 | 147 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.32, 0.33] |
| 4 Burden (Short‐term follow‐up) Show forest plot | 1 | 128 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.75, 0.35] |
| 4.1 Short‐term follow‐up ≤ 3 months | 1 | 128 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.75, 0.35] |
| 5 Skill acquisition: Problem‐Solving Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 End of intervention | 3 | 236 | Std. Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.21, 0.71] |
| 6 Skill acquisition: Preparedness to Care Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 End of intervention | 2 | 208 | Std. Mean Difference (IV, Random, 95% CI) | 0.37 [0.09, 0.64] |
| 7 Skill acquisition: Preparedness to Care (medium‐term follow‐up) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Medium‐term follow‐up > 3 months to ≤ 6 months | 1 | 17 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.02, 0.42] |
| 8 Skill acquisition:Competence Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 End of intervention | 1 | 107 | Mean Difference (IV, Random, 95% CI) | 4.10 [‐2.19, 10.39] |
| 9 Psychological health: Depression Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 End of intervention | 9 | 792 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.70, ‐0.05] |
| 9.2 Medium‐term follow‐up > 3 months to ≤ 6 months | 3 | 227 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.56, 0.45] |
| 10 Psychological health: Anxiety Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 End of intervention | 1 | 61 | Mean Difference (IV, Random, 95% CI) | ‐4.00 [‐11.68, ‐0.32] |
| 11 Psychological health: Coping Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 End of intervention | 1 | 121 | Mean Difference (IV, Random, 95% CI) | 1.0 [‐0.45, 2.45] |
| 12 Psychological health: Stress Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 End of intervention | 1 | 137 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.30, 0.10] |
| 12.2 Medium‐term follow‐up > 3 to ≤ 6 months | 1 | 130 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.11, 0.31] |
| 13 Knowledge and understanding: Knowledge Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 End of intervention | 1 | 61 | Mean Difference (IV, Random, 95% CI) | 1.90 [‐0.63, 4.43] |
| 14 Health status and well‐being: Physical health Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 14.1 End of intervention | 2 | 248 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.35, 0.17] |
| 15 Health status and well‐being: Self‐efficacy Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 End of intervention | 2 | 175 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.26, 0.33] |
| 16 Health status and well‐being: Self‐efficacy (Medium‐term follow‐up) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 16.1 Medium‐term follow‐up > 3 to ≤ 6 months | 1 | 130 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.29, 0.29] |
| 17 Health status and well‐being: Social activity Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 17.1 End of intervention | 1 | 121 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.10, 0.18] |
| 18 Satisfaction: Satisfaction with supports Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 18.1 End of intervention | 3 | 291 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.24, 0.44] |
| 19 Family functioning Show forest plot | 1 | 141 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.04, 0.44] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Burden Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 End of intervention | 1 | 11 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.74, 0.34] |
| 2 Depression Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 End of intervention | 1 | 11 | Mean Difference (IV, Random, 95% CI) | ‐4.3 [‐9.57, 0.97] |
| 2.2 Unknown time point | 1 | 45 | Mean Difference (IV, Random, 95% CI) | 1.20 [‐5.35, 7.75] |
| 3 Stress Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Unknown time point | 1 | 45 | Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐3.17, 1.97] |
| 4 Physical Health Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 End of intervention | 1 | 11 | Mean Difference (IV, Random, 95% CI) | 1.9 [‐0.65, 4.45] |

