Contenido relacionado
Revisiones y protocolos relacionados
Jacqueline J Ho, Prema Subramaniam, Aarany Sivakaanthan, Peter G Davis | 15 octubre 2020
Peter G Davis, David J Henderson‐Smart | 23 octubre 2001
Brigitte Lemyre, Marc-Olivier Deguise, Paige Benson, Haresh Kirpalani, Osayame A Ekhaguere, Peter G Davis | 19 julio 2023
Jacqueline J Ho, Prema Subramaniam, Peter G Davis | 15 octubre 2020
Elizabeth V Blazek, Christine E East, Jacqueline Jauncey-Cooke, Fiona Bogossian, Caroline A Grant, Judith Hough | 29 marzo 2021
Nicolas Bamat, Julie Fierro, Yifei Wang, David Millar, Haresh Kirpalani | 26 febrero 2019
David J Henderson‐Smart, Prema Subramaniam, Peter G Davis | 23 octubre 2001
Peter G Davis, David J Henderson‐Smart | 22 abril 2003
Brigitte Lemyre, Peter G Davis, Antonio G De Paoli | 21 enero 2002
Brigitte Lemyre, Marc-Olivier Deguise, Paige Benson, Haresh Kirpalani, Antonio G De Paoli, Peter G Davis | 27 julio 2023


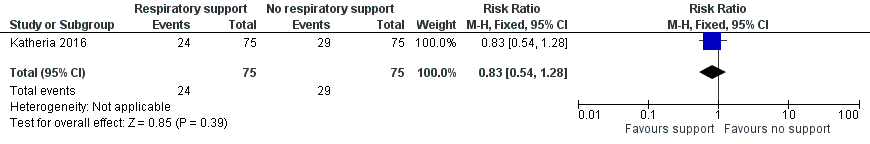
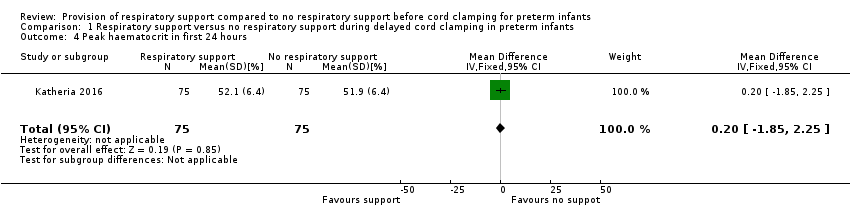
![Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.4 Peak haematocrit in first 24 hours [%].](/es/cdsr/doi/10.1002/14651858.CD012491.pub2/media/CDSR/CD012491/image_n/nCD012491-AFig-FIG05.png)

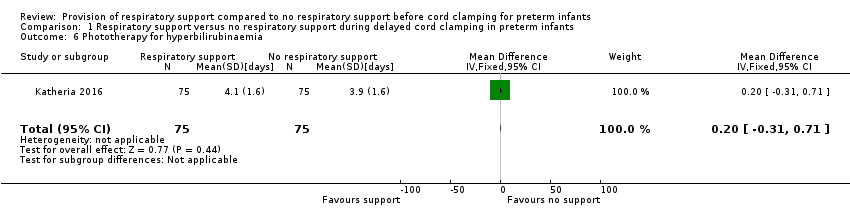
![Forest plot of comparison: 1 Respiratory support versus no respiratory support during delayed cord clamping in preterm infants, outcome: 1.6 Phototherapy for hyperbilirubinaemia [days].](/es/cdsr/doi/10.1002/14651858.CD012491.pub2/media/CDSR/CD012491/image_n/nCD012491-AFig-FIG07.png)