Rehabilitación después de la cirugía por lesiones del tendón flexor de la mano
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Study characteristics | ||
| Methods | Design: parallel group randomised controlled trial. Setting: single centre trial. Physical Medicine and Rehabilitation Department, El Demerdash Hospital, Ain Shams University, Egypt. Study conducted in 2015 to 2016 Unit of randomisation: participant Unit of analysis: tendon | |
| Participants | Details of sampling frame: Total eligible: 53 participants Total excluded pre‐randomisation: 20 participants Baseline characteristics: Total randomised: 33 participants (45 tendons) Place and hold group randomised: 15 participants (21 tendons) Sex distribution: 21 males; 5 females Place and hold group: not reported Age: mean (range): Mean 26.8 years (15 to 60 years) Place and hold group: not reported Flexor tendon zones: zone I: 7; zone II: 22; zone III: 7 Inclusion criteria:
Exclusion criteria:
Surgical technique for flexor repair: All flexor tendons were two‐strand repairs. The wound was extended using Bruner incisions, and a flap was raised to expose the tendon preserving the functionally important A2 and A4 pulleys. Pull out suture was made for zone I injury with short distal stump (< 1 cm). The suture materials were 3/0 or 4/0 prolene for core suture modified Kessler technique and 5/0 or 6/0 prolene for epitendinous sutures. Associated digital nerve and arterial injuries were repaired by the 8/0 or 9/0 Ethibond. Characteristics of participants lost to follow‐up/dropouts and included in analysis: Total lost to follow‐up: 7 participants (9 tendons) Place and hold group lost to follow‐up: 4 participants (5 tendons) Total available for follow‐up: 26 participants (36 tendons) Total analysed: 26 participants (36 tendons) Place and hold group: 11 participants (16 tendons) | |
| Interventions | Intervention 1: Place and hold exercise regimen Components of the intervention: exercise regimen was commenced at three days after tendon repair. Place and hold mobilisation regimen consisting of passive digit flexion of the affected finger and then the participant tries to maintain the flexed posture through active contraction of the involved muscle for five seconds (i.e. place the finger in the desired flexed position and then participant attempts to hold the finger using their flexor muscles in the same position); individual passive range of motion for all joints; passive flexion active extension. These were progressed to active tenodesis exercises. Dose: 25 repetitions of each exercise. Frequency of administration: every waking hour for the first six weeks post‐surgery. Intervention 2: Controlled passive exercise regimen Components of the intervention: passive exercise regimen using the modified Kleinert method consisting of composite passive flexion and active extension of the digits plus passive range of motion to each joint of each finger. Exercise regimen was commenced at three days after tendon repair. Dose: 25 repetitions of each exercise Frequency of administration: every waking hour for the first six weeks post‐surgery. Both groups: Components of the intervention: dorsal blocking orthosis with wrist in 20° flexion, MCP joint in 70° flexion and IP joints in full extension. Dose: orthosis worn all of the time. Frequency of administration: worn all of the time for six weeks post‐surgery. At six weeks, the orthosis was discarded. | |
| Outcomes | Outcomes were assessed at six weeks through to six months post‐surgery:
| |
| Funding and conflicts of interest statements | Funding source: not reported | |
| Notes | Trial registered: PACTR201708002483416 Unit of analysis is tendons not fingers/participants | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: 'We randomised patients into two groups by random sequence‐generating website' as per clinical trials registry: www.randomizer.org." |
| Allocation concealment (selection bias) | Low risk | Quote: as per the clinical trials registry, "allocation was determined by the holder of the sequence who is situated offsite". |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not reported but due to the nature of the intervention (participation in an exercise programme) it is unlikely participants were blinded to the intervention group they were assigned. Due to the nature of the intervention, healthcare providers could not be blinded to the intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: non‐blinded participants, who may have had different expectations about the benefits of the intervention they received when rating the Disabilities of the Arm, Shoulder and Hand questionnaire and satisfaction. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: it is not stated whether the outcome assessors were blinded for range of motion and adverse events. We attempted to contact the authors but did not receive a response. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Low risk | Quote: "A total of 33 patients (45 tendons) were enrolled in the study, and only 26 (36 tendons) continued in the study, as seven patients were lost to follow‐up." Data for each group is also reported. |
| Incomplete outcome data (3 to 6 months) (attrition bias) | Unclear risk | Quote: "We conducted our study for 12 weeks….". However, the DASH appears to have been conducted at six months. Comment: it is unclear what data were collected beyond 12 weeks. Clarification from the authors was not received on request for further data. The authors do not report when adverse events were measured. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes that were reported in the clinical trials register and in the methods section of the paper are reported in the results. |
| Other bias (outcomes appropriately analysed) | High risk | Comment: the authors have used the unit of analysis as tendons. However, some of the outcomes that were measured such as range of motion, scar adhesion and DASH are measured at the finger or person level. A unit of analysis error appears to have occurred for these outcomes as measurements are per tendon. No further sources of bias were detected. |
| Study characteristics | ||
| Methods | Study design: parallel group randomised controlled trial Setting: Sweden Unit of randomisation: participant Unit of analysis: digit; thumbs analysed separately | |
| Participants | Details of sampling frame: Total eligible: 96 participants (106 digits) Total excluded pre‐randomisation: 0* Baseline characteristics: Total randomised: 96 participants (106 digits, 81 fingers and 25 thumbs) Sex distribution at baseline: 68 males; 28 females Age: not reported in baseline characteristics Flexor tendon zone: zone II: 106 digits Inclusion criteria:
Exclusion criteria:
Surgical technique for the flexor tendon repair: Surgery within 24 hours of injury. Repaired with a modified Kessler suture using 4/0 Maxon (Davis and Geck) and a running circumferential 6/0 Prolene (Ethicon) suture. Characteristics of participants lost to follow‐up/dropouts and included in analysis: Total drop‐outs: 14 participants (six ruptured in the first three weeks and eight were lost to follow‐up)* Total available for follow‐up: 82 participants (68 fingers and 23 thumbs) Total included in analysis: 82 participants (68 fingers and 23 thumbs) 8‐week group: 38 participants (45 digits (35 fingers; 10 thumbs); 15 fingers contributed 2 tendons) 10‐week group: 44 participants (46 digits (33 fingers; 13 thumbs); 12 fingers contributed 2 tendons) Sex distribution at follow‐up (only reported for those included in analysis): 8‐week group: 28 males; 10 females 10‐week group: 26 males; 18 females Age: mean ± SD (range) (only reported for those included in analysis): 8‐week group: mean 36 years 10‐week group: mean 38 years | |
| Interventions | Intervention 1: Unrestricted activity from 8 weeks post‐surgery Components of the intervention: at 6 weeks, participants were instructed in a programme to gradually increase the load on the involved hand, allowing unrestricted activity at eight weeks after the surgery. Dose: not reported. Frequency of administration: not reported. Intervention 2: Unrestricted activity from 10 weeks post‐surgery Components of the intervention: at 6 weeks, participants were instructed in a programme with slower gradual increase of load on the involved hand allowing unrestricted activity at 10 weeks. Dose: not reported. Frequency of administration: not reported. Both groups: Components of the intervention: all participants received the same therapy for the first six weeks: dorsal blocking orthosis with transverse palmar component and rubber band traction; week one to four passive exercise regimen; week 5 to 6 active exercise regimen. Dose: orthosis: full time wear except for exercises. Exercise regimen: 6 repetitions of each exercise. Frequency of administration: for the first six weeks: orthosis applied immediately after surgery, worn all the time except for exercises. Exercise regimen: 10 times per day. | |
| Outcomes | Outcomes were assessed at 8, 16, 24 weeks for intervention 1 group, and 10, 16, 24 weeks for intervention 2 group. Thus, groups were measured on the commencement of the intervention and were only measured at the same time points at 16 and 24 weeks.
Goniometric measurements were then used to calculate the following classifications:
| |
| Funding and conflicts of interest statements | Funding source: Not reported | |
| Notes | * Data provided or clarified by correspondence from the authors ***Outcomes were measured at different time points in the groups, except for the 6 month time interval. Hence, only six months outcomes were reported in the paper, and in this review. ****Incomplete data reporting for these outcomes prevented their inclusion in this review's analyses. No clinical trial registration found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After the 6th week the patients were randomised into two groups…."; and correspondence received from the authors "Randomization was performed by an independent OT, using concealed envelopes at four weeks after surgery. 120 envelopes had been prepared beforehand. The envelopes were prepared, randomly mixed and then delivered in a pile to the OTs who consecutively picked them up in the order they came. " Comment: the randomisation sequence appears to have been generated using an adequate method. |
| Allocation concealment (selection bias) | Low risk | Quote: "After the 6th week the patients were randomised into two groups…."; and correspondence received from the authors "Randomization was performed by an independent OT, using concealed envelopes at four weeks after surgery. 120 envelopes had been prepared beforehand." Comment: information provided by the authors confirms that the allocation sequence was concealed prior to randomisation. An adequate method was used to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "The rehabilitation was supervised by any OT on duty who was not blinded to the allocation and performed the intermediate measurements at 8, 10 and 16 weeks." Comment: not reported but due to the nature of the intervention (participation in graded hand function) it is unlikely participants were blinded to the intervention group they were assigned. Due to the nature of the intervention, care providers could not be blinded to the intervention. Participants were not blind to |
| Blinding of outcome assessment (detection bias) | High risk | Comment: non‐blinded participants, who may have had different expectations about the benefits of the intervention the received (function using VAS). |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "The rehabilitation was supervised by any OT on duty who was not blinded to the allocation and performed the intermediate measurements at 8, 10 and 16 weeks. The assessor (author 2 or 3) doing the final examination after 24 weeks was however blinded to the rehabilitation program at that point." Comment: the outcome assessment was blinded at 24 weeks, but not at the earlier time points. |
| Incomplete outcome data (less than 3 months) (attrition bias) | High risk | Comment: the number of participants and digits contributed to the study was provided via correspondence from the authors. The 82 participants who were included in the analysis does not include (n = 14) drop‐outs. Eight of these were lost to follow‐up. It is unclear from which group the 14 drop‐outs were excluded from or the reasons for lost to follow‐up.This drop‐out rate may have had an impact on the results. No further data could be obtained from the authors. |
| Incomplete outcome data (3 to 6 months) (attrition bias) | High risk | Comment: the number of participants and digits contributed to the study was provided via correspondence from the authors. The 82 patients who were included in the analysis does not include 14 drop‐outs. Eight of these were lost to follow‐up. It is unclear from which group the 14 drop‐outs were excluded from or the reasons for lost to follow‐up. This drop‐out rate may have had an impact on the results. No further data could be obtained from the authors. |
| Selective reporting (reporting bias) | High risk | Comment: outcomes were measured at various time points between 6 and 12 weeks. However, these data are not reported in the results section of the publication. Also, without a trial protocol is unclear whether other outcomes were measured but not reported. Correspondence from the authors indicated that these data are no longer available. |
| Other bias (outcomes appropriately analysed) | Low risk | Comment: randomisation occurred at the participant level. However, some of the outcomes are reported at the participant level (function, strength and work), some at the digit level (range of motion), and some at the tendon level (e.g. ruptures). The number of participants, fingers, thumbs and tendons in each group appears to be clearly stated in the manuscript. No other sources of bias were detected. |
| Study characteristics | ||
| Methods | Study design: parallel group randomised controlled trial Setting: single centre; Hand Therapy Clinic, Tehran, Iran Unit of randomisation: participant Unit of analysis: digit | |
| Participants | Details of sampling frame: Total eligible: 70 participants Total excluded pre‐randomisation: 16 participants Baseline Characteristics: Total randomised: 54 participants (64 digits) Passive group: 28 participants (33 digits) Place and hold group: 26 participants (31 digits) Sex distribution: 37 males; 17 females Passive group: 19 males; 9 females PAH group: 18 males; 8 females Age: mean ± SD (range) Passive group: 28 ± 9 years (17 to 50 years) PAH group: 29 ± 8 years (13 to 47 years) Flexor tendon zone: zone II: 64 digits Inclusion criteria:
Exclusion criteria:
Surgical technique for flexor tendon repair: FDP tendon repair: 2‐strand modified Kessler core 3‐0 prolene and simple running Epitendinous suture using 5‐0 prolene. FDS tendon repair: 2 x figure‐of‐eight sutures using 4‐0 prolene. Characteristics of participants lost to follow‐up/dropouts and included in analysis: Total available for follow‐up: 54 participants (64 fingers) Total analysed: 54 participants (64 fingers) Passive group: 28 participants (33 fingers) PAH group: 26 participants (31 fingers) | |
| Interventions | Intervention 1: Controlled passive exercise regimen Components of the intervention: orthosis: dorsal blocking orthosis with rubber band traction (attached to a hook placed on the fingernail and passed under a pulley to cause passive flexion of the IP joints) ‐ the rubber band traction was the only difference between groups and was used to perform the controlled passive exercises. Exercise regimen: passive flexion caused by the rubber band traction followed by active finger extension within the dorsal blocking orthosis. Exercises commenced three days after swelling reduced (this means exercises were started at different time points for each participant). Dose: orthosis: worn full time. Exercises: minimum of 10 repetitions per exercise. Frequency of administration: orthosis: worn full time. Exercises: every waking hour for 21 days Intervention 2: Place and hold exercise regimen Components of the intervention: orthosis: as described in both groups. Exercise regimen: patients were advised to passively flex their fingers using the other hand with the wrist in 30 degrees of extension (out of the orthosis), and then hold the finger position actively, holding for three to five seconds. Dose: orthosis: worn full time except for exercises. Exercises: 10 repetitions per exercise Frequency of administration: orthosis: worn full time except for exercises. Exercises: four times per day for 21 days. Both groups: Orthosis: protection of the tendons using a dorsal static blocking orthosis with wrist positioned at 0 to 30 degrees of flexion and the MCP joints in 70 to 90 degrees flexion. Exercises: commenced three days after swelling reduced (this means exercises were started at different time points for each participant). At 21 days, all patients were allowed to actively flex their fingers. At four weeks, gliding exercises (extension of the MP joints while holding IPs in flexion, flexion of the MP joints with IPs in extension and composite flexion). At six weeks, blocking exercises (flexion of the PIP joint while the MCP joint is kept in extension; flexion of the DIP joint when MCP and PIP joints are held in extension) and resistive exercises (e.g. therapist) were initiated. Exercises commenced three days after swelling reduced (this means exercises were started at different time points for each participant). Dose: not reported. Frequency of administration: not reported. | |
| Outcomes | Outcomes measured at eight weeks post‐surgery: by an independent research therapist, blinded to group allotment and not involved in the care of the participants.
| |
| Funding and conflicts of interest statements | Funding source: not reported | |
| Notes | *Unit of Analysis is fingers NOT participants. No clinical trials registration found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " After providing informed consent, patients referred in the first week after surgery to the hand rehabilitation clinic were randomised equally to either place and active hold or modified Kleinert according to a computerized random number generator." Comment: the randomisation sequence appears to have been generated using an adequate method. |
| Allocation concealment (selection bias) | Unclear risk | Comment: information was insufficient to reveal whether the allocation sequence was adequately concealed until interventions were assigned. We attempted to contact the authors but did not receive a response. |
| Blinding of participants and personnel (performance bias) | Low risk | Comment: there were no self‐reported outcome measures used in this study. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Eight weeks after surgery an independent research therapist not involved in the care of the patients and blinded to group allotment evaluated patients." Comment: the outcome assessor was blinded to the intervention groups. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Low risk | Comment: the data set probably was complete as no withdrawals were reported throughout the study period. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all outcome measures specified in the methods were reported in the results section. However, without a trial protocol, it is unclear whether other outcomes were assessed but not reported. |
| Other bias (outcomes appropriately analysed) | Low risk | Comment: range of motion was measured for each digit, and was reported with the unit being digits. Other outcomes appeared to have been measured at the participant level as appropriate. It is unlikely that a unit of analysis error occurred. No further sources of bias were detected. |
| Study characteristics | ||
| Methods | Study design: parallel group randomised controlled trial (allocation to the three non‐concurrent intervention groups was not randomised) Setting: single centre; Medical College Hospital, Chennai, India Unit of randomisation: participant Unit of analysis: digit | |
| Participants | Details of sampling frame: Total eligible: 106 participants (139 digits) Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: 72 participants (99 digits) ultrasound groups; 34 (40 digits) control group Total lost to follow‐up in all groups: 6 participants (8 digits) Sex distribution: not reported at baseline Age: not reported at baseline Flexor tendon zone: zone II: 139 digits Inclusion criteria:
Exclusion criteria:
Surgical technique: Operations performed by senior residents. 2‐strand modified Kessler Mason suture for tendon repair. Characteristics of participants lost to follow‐up/dropouts and included in analysis: Total available for follow‐up: ultrasound (US) groups: 66 participants (91 digits) Total available for follow‐up: control group: 34 participants (40 digits) Number included in analyses: Total analysed: ultrasound group: 66 participants (93 digits)
Total analysed: control group: 34 participants (40 digits) Attrition: dropouts and exclusions:
Sex distribution at follow‐up: Of 100 followed up: 89 males; 11 females US group: 59 males; 7 females Control group: 30 males; 4 females Age: mean ± SD (range) age at follow‐up: US group 1: incomplete information (range 10 to 45 years listed for 42 of 66 followed‐up participants) Control group: 35 years (22 to 50 years) | |
| Interventions | Both intervention groups were immobilised a dorsal plaster of Paris cast for three weeks with wrist in neutral and MCP joints in 70 degrees flexion and commenced the same mobilisation from three weeks. Intervention: Ultrasound Components of the intervention: ultrasound: with the orthosis in place, the dressings were removed. The ultrasound coupling gel was applied to the zone II region. The ultrasound treatment head was placed over the site of the tendon repair and gently moved in order to "iron out the irregularities in the near field and to avoid standing waves due to reflection". Care was taken not to cause undue movements to the repaired finger. After ultrasound therapy, the dressings were reapplied. Standard hand therapy: as described below was commenced at three weeks. Dose: the dosage of the ultrasound changed twice during the five year recruitment period; this was not randomised and appears to have been selected by the therapist. Frequency of administration: 5 minutes. Not reported how many sessions were performed and how often they were performed.
The ultrasound group also received the same standard hand therapy programme as the control. Control: Standard hand therapy programme Components of the intervention: orthosis: dorsal plaster of Paris orthosis with wrist in neutral position, MCPs in 70 degrees flexion and IPJs in extension. Hand therapy: three to six weeks, orthosis removed, scar massage; exercise regimen consisting of active exercises, blocking exercises and place hold exercises. Between six to eight weeks: exercise regimen consisting of additional passive stretching and resisted exercises. After eight weeks: lift weights; allowed to return‐to‐work Dose: orthosis: full time; hand therapy: once per day. Frequency of administration: orthosis: full time for three weeks; hand therapy: daily from three to at least eight weeks. | |
| Outcomes | Outcomes were assessed at three months post‐surgery:
| |
| Funding and conflicts of interest statements | Funding source: Medical College Hospital Chenai | |
| Notes | *All outcomes were measured at 3 months. Although the methods stated that range of motion was also measured weekly from 3 weeks, this was not reported in the results section. ** A unit of analysis error appears to have occurred. This is a per hand level measure where the unit of analysis used was digits. Clinical Trials Registry of India; Ref: CTRI/2013/04/003576 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were asked to draw a card indiscriminately from an envelope containing a pack of cards labelled as ultrasound or immobilisation in 2:1 ratio"; and from correspondence received from Geetha: "There were two ultrasound cards for one immobilisation card. Specifically, out of 15 cards, 10 were ultrasound and 5 were immobilisation. Patients were asked to select a card at random from the envelope." However, comparisons are made between the three ultrasound groups, where randomisation did not occur, and it appears that the therapist selected which ultrasound dose was applied to the participant. Comment: the randomisation sequence appears to have been generated using an adequate method between the ultrasound and the control groups. It is important to note that within the ultrasound group, patients received one of three different ultrasound regimens, which was not randomised. |
| Allocation concealment (selection bias) | Low risk | Quote: "The patients were asked to draw a card indiscriminately from an envelope containing a pack of cards labelled as ultrasound or immobilisation in 2:1 ratio."; and from correspondence received from Geetha: "Patients were asked to select a card at random from the envelope. The cards were kept in a large opaque envelope. They were not visible to the patient or to the person performing the randomisation." Comment: although the cards could have potentially be seen during the selection from the one large opaque envelope, the authors reported that precautions were taken to blind the patient and the person performing the randomisation. Thus, it appears an adequate method was used to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) | Low risk | Comment: there were no self‐reported outcomes. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Results were assessed by an independent observer who was not involved in the study" and from email correspondence from Geetha, "The assessment was done by the physiatrist who was not part of the study. She was blinded to the intervention group of the patients." Comment: the outcome assessor was blinded to the intervention group. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Low risk | Comment: no data were collected before 3 months. However, there were few dropouts at 3 months. |
| Incomplete outcome data (3 to 6 months) (attrition bias) | Low risk | Comment: participants who were lost to follow‐up or were withdrawn from the study due to an adverse event are clearly reported. Withdrawals and how they were dealt with are clearly reported. Also, the number of participants that dropped out from each group were low (range 1 to 3). |
| Selective reporting (reporting bias) | High risk | Comment: range of motion data were collected at weekly intervals, but only 12 week data were reported in the results section. However it is likely that these data were recorded between 3 to 11 weeks, and therefore it is unlikely to have practical implications. However, without a trial protocol, it is unclear whether other outcomes were assessed but not reported. Additionally, ROM and grip strength is reported in ranges; no means or standard deviations were reported. Authors also used different range classifications that are not consistent across the four groups and are also recorded at different time intervals. |
| Other bias (outcomes appropriately analysed) | High risk | Comment: grip strength was calculated in a non‐standardised way: % of contralateral side. In the grip strength analysis, it appears that a unit of analysis error has also occurred. The grip strength is reported per digit; however, this is at a per hand not per digit level outcome. For range of motion, authors also appeared to use different range classifications that are not consistent across the four groups and are also recorded at different time intervals. |
| Study characteristics | ||
| Methods | Study design: parallel group quasi‐randomised trial Setting: multi‐centre; three hospital sites in USA Unit of randomisation: participant | |
| Participants | Details of sampling frame: Total eligible: not reported Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: unclear whether those analysed were also the same number as those randomised Intervention: unclear whether those analysed were also the same number as those randomised Control: unclear whether those analysed were also the same number as those randomised Sex distribution: Not reported Age: mean: Intervention: 26.2 years Control: 32.8 years Flexor tendon zone: zone II: 60 digits (analysed) Inclusion criteria:
Exclusion criteria:
Surgical technique for flexor tendon repair: Flexor tendons were exposed through palmar zig‐zag incisions. The proximal tendon stumps were isolated by either flexing the wrist and digits or probing the tendon sheaths with a blunt tendon passer. The tendon stumps were delivered atraumatically into the tendon sheath defect. A funnel shaped enlargement was created in the tendon sheath through the non critical membranous region when necessary to accomplish repair, as described by Lister. The tendons were repaired in the manner described by Kessler and Missim, with 4‐0 braided Dacron sutures (Ethicon, Somerville, New Jersey) under a magnification factor of 3.5. A continuous 6‐0 nylon epitenon suture was used to invaginate the free tendon ends. Digital sheath defects were not repaired. Similar operative technique was reported to have been used across all three sites. Characteristics of participants lost to follow‐up/dropouts and included in analysis: Total available for follow‐up: 51 participants (60 digits, 102 tendons) Total lost to follow‐up: not reported Total analysed: 51 participants (60 digits, 102 tendons) CPM group: 26 participants (29 digits, 48 tendons) Passive group: 25 participants (31 digits, 54 tendons) | |
| Interventions | Intervention: Continuous passive‐motion (CPM) machine Intervention components: CPM, light dressings, orthosis: dorsal extension lock orthosis fabricated extending from the proximal forearm to the proximal interphalangeal joints positioned with wrist flexed 30 degrees and metacarpophalangeal joints flexed 45 degrees to be used during CPM use. Palmar straps supporting the forearm, wrist, transverse palmar arch, and proximal phalanges maintained the extremities securely in the orthosis. A second dorsal extension‐block orthosis, which extended to the fingertips, was fabricated during the first therapy session. This was worn if the CPM machine was not in use. In addition to being taught how to apply, operate, and remove the CPM machine, participants were instructed in early motion exercises that were to be performed if the device malfunctioned. The exercises were the same as those taught to participants of group 2. Technical description of the CPM device and use: CPM 5000, Sutter Biomedical, San Diego, California. Dose: CPM: Both rate and force parameters of CPM motion were maintained at the medium setting: 160 cycles of interphalangeal joint flexion and extension per hour (i.e. one cycle every 25 seconds). Frequency of administration: commenced one day post‐surgery. Participants were instructed to wear the device for eight to 12 hours a day for six weeks. Week 5 to 6: Intervention components: CPM alternated with active exercise regimen. The CPM and splinting were discontinued six weeks postoperatively. Dose: CPM: both rate and force parameters of CPM motion were maintained at the medium setting: 160 cycles of interphalangeal joint flexion and extension per hour (i.e. one cycle every 25 seconds). Frequency of administration: commenced one day post‐surgery. Participants were instructed to wear the device for 8 to 12 hours a day for six weeks. Week 8 to 12: Intervention components: resistive exercises commenced. The exercise regimen gradually progressed to full activity by the 12th postoperative week. Control: Controlled passive progressed to active exercise regimen Intervention components: orthosis: dorsal blocking orthosis applied on the first postoperative day, positioned with wrist in 30 degree flexion, the metacarpophalangeal joints in 60 to 70 degree flexion, and the interphalangeal joints either in neutral or flexion through rubber band traction. The protective orthosis was discontinued at six weeks. Exercise regimen: Week 1 to 4: patients performed active extension exercises to the confines of the orthosis and passive flexion to the distal palmar crease. Week 4: active finger flexion initiated. Week 6 to 8: progressive resistive exercises gradually introduced and progressed until full activity achieved. Week 12: no restrictions. Frequency of administration: the rehabilitation protocol varied slightly in cycle number and duration depending upon the facility at which the patient was treated. Both groups: All patients begun therapy at one day post operation. Orthosis: post‐operatively, bulky long‐arm dressings with dorsal plaster splints were applied, with the wrist in 30 degrees flexion and the metacarpophalangeal joints in 70 degrees flexion. | |
| Outcomes | Outcomes were assessed at a minimum of 6 months post‐surgery (mean follow‐up period was 10.8 months (6 to 38 months)):
| |
| Funding and conflicts of interest statements | Funding source: not reported | |
| Notes | Only patients with a minimum follow‐up time of six months from repair to re‐examination were included. The authors did not report on how many were eligible or randomised into the study, only those whose data were analysed. No clinical trial registration found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Postoperatively, patients were placed in one of two study groups depending upon the month in which they were born. Group 1 included those patients born in even‐numbered months (February, April, June, August, October, and December). Group 2 consisted of those patients born in odd numbered months (January, March, May, July, September, and November)." Comment: the sequence appears to have been generated using a quasi‐randomised method. |
| Allocation concealment (selection bias) | High risk | Quote: "Postoperatively, patients were placed in one of two study groups depending upon the month in which they were born. Group 1 included those patients born in even‐numbered months (February, April, June, August, October, and December). Group 2 consisted of those patients born in odd numbered months (January, March, May, July, September, and November)." Comment: due to the use of quasi‐randomisation, the allocation sequence was not concealed prior to randomisation. |
| Blinding of participants and personnel (performance bias) | Low risk | Comment: there were no self‐reported outcomes. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Final evaluations were performed by the therapists…" Comment: the treating therapists performed the outcome evaluations and thus could not be blinded to the intervention. |
| Incomplete outcome data (over 6 months) (attrition bias) | High risk | Quote: "Only patients with a minimum follow‐up time of six months from repair to re‐examination were included." Comment: the number of participants who were randomised into the study is not reported. It is unclear how many participants dropped‐out, and how this might have affected the data analysis. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all outcomes prespecified in the methods section of the publication, were reported in the results section of the publication. However, without a trial protocol, it is unclear whether other outcomes were assessed but not reported. |
| Other bias (outcomes appropriately analysed) | Low risk | Comment: participants were randomised per person, but some of the statistical analyses were conducted per digit. The authors state the number of participants/digits/tendons in the analysis. It is unlikely that this would likely impact the outcomes. No further sources of bias were identified. |
| Study characteristics | ||
| Methods | Study design: parallel group randomised controlled trial Setting: single‐centre; Physiotherapy clinic in Germany Unit of randomisation: participant Unit of analysis: unclear | |
| Participants | Details of sampling frame: Total eligible: not reported Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: 62 participants (digits not reported) Exoskeleton group: 31 (probably) Sex distribution: 44 males; 18 females (not reported by group) Age: mean (range): Mean 29.5 years (18 to 60 years) (not reported by group) Flexor tendon zone: zone II: 62 participants Inclusion criteria:
Exclusion criteria:
Surgical technique for flexor repair: Tendons were repaired using absorbable PDS sutures. Two‐strand core Kirchmayer ‐ Kessler sutures (4.0 PDS) and simple continuous epitendinous (6.0 PDS) was used to repair the tendon. In the distal zone II, the radial and ulnar slip of the FDS was repaired using a Z suture (4.0 PDS) or analogue to FDP. Characteristics of participants lost to follow‐up and included in analysis: Total excluded from analysis: 3 participants (2 complications and 1 lost to follow‐up) Total available at 18 weeks follow‐up: 59 participants (digits not reported). Total available at earlier time‐points not reported. | |
| Interventions | Intervention: Exoskeleton Intervention components: this group commenced use of exoskeleton at two weeks post surgery, three times a week for 30 min administered by the physiotherapists at the hospital. Exoskeleton was attached dorsally on the finger with Velcro with the wrist held in 30 degrees flexion. Due to the circular motion arms of the exoskeleton, the pressure on the extension side of the finger was always perpendicular to the axis of motion. In the beginning of each session, ROM was measured and the exoskeleton was adjusted to the individual finger. Control: Physiotherapy Intervention components: participants only received the treatments common to both groups (see below). Dose: the duration of the treatment was variable. Frequency of administration: three times a week. Physiotherapy was stopped when the doctor found that the participant had free function or the patient was satisfied with the functional result. Both groups: Intervention components: modified Kleinert orthosis consisting of a dorsal blocking splint with rubber band traction applied to the fingertips. All participants were in the hospital for four days post surgery and provided with education and an exercise regimen. Exercises included finger active and passive (if required) extension of the finger in the orthosis. If passive flexion through dynamic pull of the orthosis could not be achieved, patient was advised to assist full flexion with the unaffected hand. Scar management was initiated 2 weeks after surgery following removal of stitches. Arm was bathed in lukewarm chamomile tea, scar massaged, moisturised and orthosis was reapplied. All treatments including were completed in 30 degrees wrist flexion. Dose: exercises: 10 x each exercise. Scar management: 10 minutes. Chamomile tea bath: not reported. Frequency of administration: exercises: every hour, for six weeks duration. Scar management: three times per day. Chamomile tea bath: not reported. Moisturiser application: not reported. | |
| Outcomes | Outcomes were assessed at 6, 12 and 18 weeks post‐flexor tendon repair (at following the commencement of treatments):
| |
| Funding and conflicts of interest statements | Funding source: not reported | |
| Notes | German language paper ‐ data extracted by translators (see Acknowledgements for translators) No clinical trial registration found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: patients were assigned to one of two groups using standardised controlled block randomisation. The allocation was based on a randomisation sheet, created by an established randomisation program. The randomisation sequence appears to have been generated using an adequate method. |
| Allocation concealment (selection bias) | Unclear risk | Comment: it appears that the randomisation sequence was kept on a randomisation sheet. However, it is unclear who held this sheet (e.g. external person versus a member of the research team) and whether this sheet was kept for the duration of the recruitment using a concealed method. We attempted to contact the authors but did not receive a response by the time of publication. |
| Blinding of participants and personnel (performance bias) | High risk | Comment: given the nature of the interventions, participants were not blind to treatment, and may have had different expectations about the benefits of the intervention they received. Given the nature of the interventions, trial personnel (treaters) were not blind to treatment, and may have had different expectations about the benefits of the treatments they were delivering. |
| Blinding of outcome assessment (detection bias) | High risk | Comment: non‐blinded participants, who may have had different expectations about the benefits of the intervention they received. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: it was not reported whether the outcome assessors were blinded to the intervention. We attempted to contact the authors but had not received a response by the time of publication. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Unclear risk | Comment: participants lost to follow‐up and due to complications have been reported as overall numbers for both groups combined. We are therefore unsure in which group the three excluded participants were assigned and at which time point. In addition, how many participants were randomised to each group is not reported in the publication; we have assumed it was 31 in each group. We attempted to contact the authors to clarify but had not received a response. However, it appears that these were excluded from the analysis, and were likely to be accounted for. |
| Incomplete outcome data (3 to 6 months) (attrition bias) | Unclear risk | Comment: participants lost to follow‐up and due to complications have been reported as overall numbers for both groups combined. We are therefore unsure in which group the three excluded participants were assigned and at which time point. In addition, how many participants were randomised to each group is not reported in the publication; we have assumed it was 31 in each group. We attempted to contact the authors to clarify but had not received a response. However, it appears that these were excluded from the analysis, and were likely to be accounted for. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all outcomes prespecified in the methods section of the publication, were reported in the results section of the publication. Also without a trial protocol, it is unclear whether other outcomes were assessed but not reported. |
| Other bias (outcomes appropriately analysed) | Unclear risk | Comment: participants contributed more than one tendon and data appears to have been reported at the participant level. Therefore, a unit of analysis error may have occurred. We attempted to contact the authors to clarify but had not received a response by the time of publication. No other sources of bias were identified. |
| Study characteristics | ||
| Methods | Study design: parallel group randomised trial* Setting: Sweden Unit of randomisation: participant Unit of analysis: unclear | |
| Participants | Details of sampling frame: Total eligible: not reported Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: 100 participants (108 digits) Active group: not reported Controlled passive group: not reported Sex distribution: not reported Age: not reported Flexor tendon zone: zone II: 108 digits Inclusion criteria:
Exclusion criteria: Not reported. Surgical technique for the flexor tendon repair: Direct tendon repair in zone II. Characteristics of participants lost to follow‐up and included in analysis: Not reported | |
| Interventions | Intervention 1: Early active flexion exercise regimen Intervention component: active flexion exercise regimen for the first three weeks post‐surgery. No other treatments reported in the publication.* Dose: not reported Frequency of administration: not reported Intervention 2: Controlled passive exercise regimen Intervention components: early controlled passive exercise regimen with rubber band traction (assumed to be attached to a dorsal blocking split). No other treatments reported in the publication.* Dose: not reported Frequency of administration: not reported Both groups: all participants were permitted active mobilisation at 3 weeks after surgery. | |
| Outcomes | Outcomes were measured at 3, 4, 6, 8 weeks; 4 months and 1 year:
| |
| Funding and conflicts of interest statements | Funding source: not reported | |
| Notes | *This was a conference proceeding. Hence, very little information was reported in the publication. No other publications of the trial were found. No clinical trial registration or publication of the full trial found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "One hundred consecutive patients with flexor tendon laceration in 108 digits were stratified according to type of injuries after having direct tendon repair and were randomised to either early active mobilisation or early controlled mobilisation with rubber band traction." Comment: there is insufficient information in the publication to judge whether the allocation sequence was generated in a random manner. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "One hundred consecutive patients with flexor tendon laceration in 108 digits were stratified according to type of injuries after having direct tendon repair and were randomised to either early active mobilisation or early controlled mobilisation with rubber band traction." Comment: there is insufficient information in the publication to judge whether the allocation sequence was adequately concealed prior to the randomisation. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: due to the nature of the interventions, it is not likely that the participants or the intervention personnel would have been blinded to the intervention. However, no self‐reported measures were reported in the results. As this was a conference proceeding, we are unsure whether there were additional outcomes included. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: it is not reported in the publication whether the outcome assessors were blinded to the intervention. We were unable to contact the authors to clarify. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Unclear risk | Comment: data were collected at 3, 4, 6 and 8 weeks. Yet, no outcome data were reported for less than 12 weeks in the publication. This was a conference abstract and attempts to contact the authors were unsuccessful and a full paper of the study has not been published. |
| Incomplete outcome data (3 to 6 months) (attrition bias) | Unclear risk | Comment: it is unclear in the publication the flow through of participants from baseline, to randomisation, to outcome measurement at follow up. The numbers of participants randomised to each group are not provided and no information is provided on whether all of these participants continued through the study to the 12 month follow‐up. Data were collected at multiple intervals but was not reported except at the one‐year interval. This was a conference abstract and attempts to contact the authors were unsuccessful and a full paper of the study has not been published. |
| Incomplete outcome data (over 6 months) (attrition bias) | Unclear risk | Comment: It is unclear in the publication the flow through of participants from baseline, to randomisation, to outcome measurement at follow‐up. The numbers of participants randomised to each group are not provided and no information is provided on whether all of these participants continued through the study to the 12 month follow‐up. Data were reported for the one year follow‐up; however, there is no reporting of the number of randomised versus followed‐up participants, or dropouts, at this time point. This was a conference abstract and attempts to contact the authors were unsuccessful and a full paper of the study has not been published. |
| Selective reporting (reporting bias) | High risk | Comment: the conference abstract does not contain a detailed methods section. It is unclear whether selective outcome reporting occurred. Also without a trial protocol, it is unclear whether other outcomes were assessed but not reported. In addition, no standard deviations or p‐values for the outcomes are reported in the abstract. |
| Other bias (outcomes appropriately analysed) | Unclear risk | Comment: it is unclear in the results whether the number of ruptures that occurred was per person, digit or tendon. A unit of analysis error may have occurred, but this is unclear. |
| Study characteristics | ||
| Methods | Study Design: parallel group randomised trial* Setting: single‐centre; Welsh Plastic Surgery Centre, UK Unit of randomisation: participant Unit of analysis: unclear | |
| Participants | Details of sampling frame: Total eligible: not reported Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: 112 participants Passive: not reported Controlled passive: not reported Sex distribution: not reported Age: not reported Flexor tendon zone: not reported Inclusion criteria:
Exclusion criteria:
Surgical technique: Strickland (1985) repairs in zones I to III. Characteristics of participants lost to follow‐up and included in analysis: Total available for follow‐up: not reported Total drop‐outs: not reported Total analysed: 80 participants (interim analysis) Passive: not reported Controlled passive: not reported | |
| Interventions | Intervention 1: Early passive exercise regimen (modified Duran protocol) Components of the intervention: exercise regimen: early passive flexion without rubber band traction, controlled passive mobilisation regimen (cited as using the modified Duran, Strickland and Glogovac regimen 1990). Isolated and composite passive flexion in the orthosis without the rubber band traction, and both active and passive extension within the orthosis. Dose: not reported Frequency of administration: not reported Intervention 2: Early controlled passive exercise regimen (modified Kleinert protocol) Components of the intervention: exercise regimen: early controlled passive flexion using rubber band traction, controlled passive flexion with active extension regimen (modified Kleinert Regime, May et al 1992). Active extension exercises and fingers were maintained in passive flexion using rubber band traction orthosis. The rubber band traction allowed the passive movements to be controlled. Dose: not reported Frequency of administration: not reported Both groups: Components of the intervention: participants were seen within 72 hours of surgery prior to leaving the hospital, and subsequently continued physiotherapy under supervision on an out‐patient basis. In addition, participants were reviewed on a weekly basis by medical staff. Dose: not reported Frequency of administration: not reported | |
| Outcomes | Outcomes were measured at 3 and 6 month intervals; additional active ROM was recorded at 6 weeks.
| |
| Funding and conflicts of interest statements | Funding source: not reported Conflicts of interest: not reported | |
| Notes | *This was a conference proceeding reporting an interim analysis. Hence, very little information was reported in the publication. The authors were contacted to provide more information about the study methods and results, but no response from the authors was received. No other publications on this study were found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A prospective, randomised study was set up at the Welsh Regional Plastic Surgery Centre in July 1992." Comment: there is insufficient information to determine whether the randomisation sequence was adequately generated. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "A prospective, randomised study was set up at the Welsh Regional Plastic Surgery Centre in July 1992." Comment: information was insufficient to reveal the adequacy of allocation concealment. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: due to the nature of the interventions, it is unlikely that the participants or intervention personnel were blinded to the intervention. However, no self‐reported measures were reported. However, since this was a conference abstract outcomes there is insufficient information to make a judgement. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: there is insufficient information to determine whether the outcome assessors were blinded, or not, to the group assignments. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Unclear risk | Comment: there is no information provided about the flow of participants through the study, reasons for exclusions, attrition or for being excluded from the analysis. |
| Incomplete outcome data (3 to 6 months) (attrition bias) | Unclear risk | Comment: there is no information is provided about the flow of participants through the study, reasons for exclusions, attrition or for being excluded from the analysis. |
| Selective reporting (reporting bias) | High risk | The only data reported are quote: "combination of Kleinert and Strickland grading (So et al, 1990). Statistical analysis carried out on the first 80 patients using the paired students t test shows no significant difference in outcome." Comment: no means, standard deviations of p‐values are reported. Very little data are provided in this conference proceeding. |
| Other bias (outcomes appropriately analysed) | Unclear risk | Comment: insufficient information is provided in the publication to determine whether a unit of analysis error may have occurred, or whether standardised methods for measuring the outcome were used. |
| Study characteristics | ||
| Methods | Study design: parallel group randomised controlled trial Setting: single‐centre; Hand surgery unit, Uludag University Medical Faculty, Bursa, Turkey Unit of randomisation: participant Unit of analysis: digit | |
| Participants | Details of sampling frame: Total eligible: not reported Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: 25 participants (41 digits) Laser group: 13 participants (21 digits) Control group: 12 participants (20 digits) Sex distribution: Randomised: 15 males; 10 females Laser group: 8 males; 4 females* Control group: 6 males; 6 females* Age: mean ± SD (range): 23.75 (range: 7 to 43) years Laser group: 23.75 ± 2.56 years Control group: 24.0 ± 3.03 years Flexor tendon zone: Zone I: 4 (Group 1: 2; Group 2: 2) Zone II: 13 (Group 1: 6; Group 2: 7) Zone III: 8 (Group 1: 3; Group 2: 5) Zone IV: 3 (Group 1: 3; Group 2: 0) Zone V: 11 (Group 1: 6; Group 2: 5) Inclusion criteria:
Exclusion criteria:
Surgical technique for flexor tendon repair: No details reported. Characteristics of participants lost to follow‐up/drop‐outs and included in analysis: Total available for follow‐up: 25 (41 digits) Total drop‐outs: 2 tendon ruptures were excluded Total analysed: 23 (39 digits) | |
| Interventions | Intervention: Low level laser therapy (LLLT) Components of the intervention: laser: following a whirlpool treatment, laser was applied to four different points with 1 cm intervals along the injury zone. The head of the instrument was held perpendicular to and in slight contact with the skin. Technical description of the laser device: the infrared‐27 GaAs diode laser instrument (Roland Series Elettronica Pagani) with the wavelength of 904 nm, frequency range of 5–7000 Hz, and maximum power of 27 W, 50 W, or 2734 W. Dose: frequency: 100 Hz for 130 second duration Frequency of administration: once per day for 10 weekdays during a two‐week period. Control: Placebo Components of the intervention: placebo laser treatment was given by using the same instrument as the intervention group, and placing its head in the same way on the hand but not turning it on. Dose: 130 second duration Frequency of administration: once per day for 10 weekdays during a two‐week period. Both groups: Components of the intervention: orthosis: modified Kleinert orthosis with a palmar pulley was applied to the injured hand of each patient three days after surgery. Exercise regimen: Washington exercise regimen was implemented for 12 weeks post‐operatively. Additional components: whirlpool (35 °C was applied to the injured hand of the patient for 15 minutes) and laser commenced from days 8 to 21. Dose: not reported Frequency of administration: not reported | |
| Outcomes | Outcomes were assessed weekly up to 12 weeks:
| |
| Funding and conflicts of interest statements | Funding source: not reported | |
| Notes | * There is an inconsistency in the number of males and females in each group compared with the total number reported in the paper. Authors were contacted for clarification, but no response was received. **Not an outcome of interest for this review No clinical trial registration found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: correspondence received from the authors states that "it was a randomised controlled study. The patients were randomised into two groups using random‐number table." Comment: an adequate methods was used to generate the randomisation sequence. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The patients were assigned into two groups by a second observer other than the one who made the evaluation throughout the study." Comment: tt appears that someone who was not involved in the treatments assigned the groups. However, there is still insufficient information to determine who this person was and whether an adequate method was used to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: study is described as "a placebo‐controlled double‐blind prospective study model". Comment: participants are likely to have been blinded to the intervention as the placebo group received the same treatment without the machine being switched on. It may not have been possible for the personnel (treaters) providing the intervention to be blinded due to the nature of the intervention, if they were required to change the settings on the laser machine. However, since none of the self‐reported outcomes are outcomes of interest for this review, risk of bias is likely not have occurred. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: study is also described as " a placebo‐controlled double‐blind prospective study model". Comment: it is not clearly reported at what level the blinding occurred. Due to the nature of the intervention, the participants were likely to have been blinded. It is unlikely that the care providers were blinded as they would need to set the parameters on the laser machine. It is unclear whether participants were provided with any information from the treating personnel that would make them perceive the laser they received as superior to the placebo. However, since the self‐reported measures were also not outcomes of interest for this review, this is unlikely to have biased the results. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The patients were assigned into two groups by a second observer other than the one who made the evaluation throughout the study." Study is also described as " a placebo‐controlled double‐blind prospective study model". Comment: it appears that the person who conducted outcome evaluations was blinded to the intervention. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Unclear risk | Comment: one exclusion reported in each group due to tendon rupture, but no attrition due to drop‐out mentioned in either group. Although not reported, this does not mean that it did not occur. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all data for the outcomes mentioned in the methods section are reported in the results section. Also without a trial protocol, it is unclear whether other outcomes were assessed but not reported. |
| Other bias (outcomes appropriately analysed) | Unclear risk | Comment: too little information is provided in the publication to know whether a unit of analysis error may have occurred. Outcomes are reported for digits and it is unclear if grip strength was measured per participant or per digit and how this was accounted for in the analysis. There is also a discrepancy in the number of participants reported in total (25 patients) and the total in gender distribution (24 patients). |
| Study characteristics | ||
| Methods | Study Design: parallel group randomised controlled trial Setting: single‐centre; Department of Plastic Surgery, 15 Khordad Hospital of Shahid Beheshti University of Medical Sciences, Tehran, Iran; 2015 to 2016 Unit of randomisation: participant Unit of analysis: participant | |
| Participants | Details of sampling frame: Total eligible: not reported Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: 97 participants (114 fingers) Laser: 39 participants (46 fingers) Control: 58 participants (68 fingers) Sex distribution: not reported at baseline Age: not reported at baseline Flexor tendon zone: not reported at baseline Inclusion criteria:
Exclusion criteria:
Surgical technique: All tendons were repaired with four‐strand repairs. Primary repair was performed under general or regional anaesthesia, 6 to 24 hours following the patient’s admission. The surgery protocol under loop magnification was Brunner incision, repairing flexor tendons by four‐strand modified Kessler core suture method; periphery running suture was performed with 4/0 Nylon, and digital nerve repairing with 10/0 Nylon in 32 patients. Characteristics of participants lost to follow‐up/drop‐outs and included in analysis: Total drop‐outs: 20 participants, all in control group Total available for 4‐week follow‐up: 77 participants (92 fingers) Total available for 4‐week follow‐up: laser group: 39 participants (46 fingers) Total available for 4‐week follow‐up: control group: 38 participants (46 fingers) Sex distribution at follow‐up: 60 males; 17 females Laser: 31 males; 8 females Control: 29 males; 9 females Mean ± SD age: Laser: 27.85 +/‐ 9.26 Control: 26.72 +/‐ 9.69 Flexor tendon zone distribution: Zone I: 6 (Laser: 2; Control: 4) Zone II: 67 (Laser: 37; Control: 30) Zone III: 19 (Laser: 5; Control: 14) | |
| Interventions | Intervention: Low level laser therapy (LLLT) Components of the intervention: LLLT as commenced at day two post‐surgery, within the plaster brace. Technical specification of the LLLT device: Mustang 2000 Laser device (Technical Co., Moscow, Russia) with two probes of red (KLO4) and infrared laser (LO7). The laser probes were placed over the repairing site in the contact method. Red and infrared laser were used to accelerate tendon healing. Dose: the setting for the red laser was continuous mode, 660 nm, and 2 J/cm2. Infrared laser in pulsed mode, wave 810 nm, 100 Hz, 5.85 J/Cm2. Specification for the LLLT applied: Peak power output 15 W; power density 15 W/cm2; wave length 890 nm; pulse frequency 100 Hz; spot size 0.002 cm2; pulsed duration 130 ns; duration of exposure for each point 60 sec; energy density 5.85 J/cm2. Frequency of administration: 2 to3 times per week, for 10 sessions over four‐week period. Control: Placebo Components of the intervention: placebo low level laser therapy with the power off. Dose: placebo dose with machine off. Frequency of administration: 2 to 3 times per week, for 10 sessions over a four‐week period. Both groups: Components of the intervention: orthosis: plaster brace with 10 degrees wrist, 90 degrees MCP joint and zero degrees IP joint flexion. Exercise regimen: Kleinert rehabilitation regimen was started within the first 24 hours. Dose: orthosis: full time for four weeks. Exercise regimen: not reported Frequency of administration: orthosis: full time for four weeks. Exercise regimen: not reported | |
| Outcomes | Outcome assessment was recorded at four weeks.
| |
| Funding and conflicts of interest statements | Funding source: Vice Chancellor for research Shahid Beheshti University of Medical Sciences Conflicts of interest: none declared | |
| Notes | Trial registered: IRCT2017050233783N1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " Using the unequal treatment allocation method, patients were randomly divided into two groups… We used the stratified block randomisation scheme with an allocation ratio of 0.6:0.4 to determine the unequal sample size…" |
| Allocation concealment (selection bias) | Unclear risk | Comment: it is unclear how the allocation sequence was concealed, if at all, until the intervention was assigned. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: although not explicitly stated in the publication, the clinical trials registry states that the study was "double‐blinded". However, there is insufficient information in the publication to know at which level this blinding occurred. Due to the nature of the interventions, it is possible that the participants could have been blinded to the interventions, but this was not explicitly stated. It is also possible that the personnel (treaters) were blinded but this was not explicitly stated. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: although not explicitly stated, the clinical trials registry states that the study was "double‐blinded". However, there is insufficient information in the publication to know at which level this blinding occurred. Due to the nature of the interventions, it is possible that the participants could have been blinded to the interventions, but this was not explicitly stated. It is also possible that the care providers were blinded but this was not explicitly stated. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The two observers, blind to the LLLT group, assessed the data independently." |
| Incomplete outcome data (less than 3 months) (attrition bias) | High risk | Quote: "Of 58 patients in the control group, 20 patients did not come back for follow up and 38 patients were treated with involvement of total 46 fingers. None has attended a hand therapy clinic" |
| Selective reporting (reporting bias) | Low risk | Comment: all data for the outcomes mentioned in the methods and clinical trials registry are reported in the results section. It appears that earlier weekly data may have been collected and not reported. However, it is unlikely that this impacts our judgement of the clinical effectiveness of the treatment. |
| Other bias (outcomes appropriately analysed) | Unclear risk | Comment: it is unclear whether a unit of analysis error for the range of motion measures has occurred, as it reports participants but this is a digit level measurement. |
| Study characteristics | ||
| Methods | Study design: parallel group randomised trial Setting: single‐centre; Department of Orthopaedic Surgery, Oslo, Norway Unit of randomisation: participant Unit of analysis: digit and participant (where appropriate) | |
| Participants | Details of sampling frame: Total eligible: 53 patients (73 fingers) Total excluded pre‐randomisation: 0 patients Baseline characteristics: Total randomised: 53 participants (73 fingers) Active flexion: 24 participants (39 fingers) Controlled passive: 29 participants (33 fingers) Sex distribution: 36 males; 14 females Active flexion: 18 males; 4 females Controlled passive: 18 males; 10 females Age: mean (range): Active: 37 years (18 to 66 years) Controlled passive: 40 years (19 to 72 years) Flexor tendon zone: Zone I: 18 (Active: 12; Control: 6) Zone II: 47 (Active: 25; Control: 22) Zone III: 4 (Active: 0; Control: 4) Inclusion criteria:
Exclusion criteria:
Surgical technique: Tendon repairs were performed one to four days after injury. The wound was extended in a zig‐zag fashion and the sheath was opened in the palmar midline with limited pulley release at the site of the repair. The FDP tendon was directly repaired with a two‐strand core suture in a side‐locking loop configuration using 3‐0 braided poly blend polyethylene (FiberWire; Arthrex Co., Naples, FL, USA). The repair was completed with a running epitendinous suture with 5‐0 monofilament nylon (Dermalon; Covidien Ltd, Mansfield, MA, USA) in an interlocking horizontal mattress suture fashion. This repair configuration is similar to the Silfverskold repair, with the differences in use of FiberWire as the suture material and locking loops of the core suture placed on the side instead of the volar surface of the tendon and in use of Dona’s interlocking horizontal mattress suture instead of cross‐stitches in making peripheral sutures. In cases with avulsion or a distal tendon stump too short for placement of a suture, the tendon was reattached with transverse intraosseous loop technique. The core suture was identical to the end‐to‐end repair. Characteristics of participants lost to follow‐up/drop‐outs: Total drop‐outs: 8 participants (9 fingers) Total excluded from analysis for 12 months follow‐up: 8 participants (9 fingers) Active flexion: 4 participants (2 ruptures and 2 lost to follow‐up) Controlled passive: 4 participants (1 rupture and 3 lost to follow‐up) Total available for 12 months follow‐up: 45 participants (63 fingers) Active flexion: 20 participants (34 fingers) Controlled passive: 25 participants (29 fingers) Number of digits included in analyses*: 1 month: active flexion: 37; controlled passive: 42 2 months: active flexion: 36; controlled passive: 32 3 months: active flexion: 36; controlled passive: 31 6 months: active flexion: 32; controlled passive: 30 12 months: active flexion: 34; controlled passive: 29 | |
| Interventions | Intervention: Active flexion plus controlled passive exercise regimen Components of intervention: exercise regimen: additional warm up exercises from day 1 post surgery with additional active extension and passive flexion hourly, followed by active unresisted finger flexions with the rubber bands released. Standard care as below. Dose: 10 repetitions of active extension/passive flexion; 10 to 20 active flexion. Frequency of administration: every waking hour for four weeks (starting from day one post‐surgery). Control: Controlled passive exercise regimen (modified Kleinert protocol) As described below. Both groups: Components of the intervention: dressings: bandages removed on first post‐operative day and spray on dressing applied. Orthosis: standardised dorsal blocking plaster orthosis applied in 0 to 20 degrees wrist flexion and 50 to 80 degrees MCP joint flexion. Splint extended to PIP joint distally. Rubber bands were attached to the nails of the injured finger and pulley placed in the palm (as per modified Kleinert regimen). Exercise regimen: weeks 1 to 4: full passive flexion using other hand, and active extension. Six weeks: active flexion exercises initiated for Standard care group and continued for Intervention group. Graded functional use: Simple activities of daily living (ADL) allowed at six weeks and gradual increasing in load to allow full gripping at 12 weeks. Dose: orthosis: worn full time for four weeks. Exercise regimen: 20 to 30 repetitions each exercise. Graded functional use: not reported. Frequency of administration: orthosis: worn full time for four weeks. Exercise regimen: every waking hour. Graded functional use: not reported. | |
| Outcomes | Outcomes were assessed at 1, 2, 3, 6, 12 months after surgery:
| |
| Funding and conflicts of interest statements | Funding source: none received | |
| Notes | The unit of analysis was fingers for the appropriate outcome measures, and participants for appropriate outcomes measures. No clinical trial registration found. Additional data was provided by correspondence from the authors including a data table for AROM, grip and pinch strengths, and VAS ADLs with means and SDs for 1, 2, 3, 6 and 12 months. *Analyses were conducted per digit. We used the number of digits as described in Table 3 of the publication for all our analyses conducted in RevMan. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We randomised with closed envelopes without any external identification, concealing the allocation until opening. At inclusion, every patient chose an envelope, which was opened after the repair was completed and the orthosis with rubber bands was applied,"; and correspondence received from authors: "The envelops were mixed like cards, then the patients themselves chose one from the deck of envelops, that means the sequence was random." Comment: it appears that the sequence was generated in a random manner. |
| Allocation concealment (selection bias) | Low risk | Quote: "We randomised with closed envelopes without any external identification, concealing the allocation until opening. At inclusion, every patient chose an envelope, which was opened after the repair was completed and the orthosis with rubber bands was applied." Comment: allocation was concealed in opaque envelopes. An adequate method was used to conceal the allocation sequence. |
| Blinding of participants and personnel (performance bias) | High risk | Comment: given the nature of the interventions, participants were not blind to treatment, and may have had different expectations about the benefits of each intervention to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) | High risk | Comment: non‐blinded participants who may have had different expectations about the benefits of the intervention they received when assessing functional use. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Two therapists (not blinded to group allocation) performed the registrations." Comment: the therapists who conducted the outcome assessments were not blinded to group allocation. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Low risk | Comment: information is provided about the flow of participants through the study, reasons for exclusions, attrition or for being excluded from the analysis. Loss to follow‐up was minimal and unlikely to have influenced the study findings. |
| Incomplete outcome data (3 to 6 months) (attrition bias) | Low risk | Comment: information is provided about the flow of participants through the study, reasons for exclusions, attrition or for being excluded from the analysis. Loss to follow‐up was minimal and unlikely to have influenced the study findings. |
| Incomplete outcome data (over 6 months) (attrition bias) | Low risk | Comment: information is provided about the flow of participants through the study, reasons for exclusions, attrition or for being excluded from the analysis. Loss to follow‐up was minimal and unlikely to have influenced the study findings. |
| Selective reporting (reporting bias) | Unclear risk | Comment: all outcome measures reported in the methods section were reported in the results section of the publication. However, without a trial protocol, it is unclear whether other outcomes were assessed but not reported. |
| Other bias (outcomes appropriately analysed) | High risk | Comment: it appears that an unit of analysis error has occurred for the measurement of grip strength. Authors reported that they analysed all outcomes per finger digit, however grip strength is a participant level variable. No further sources of bias were found. Furthermore, grip and pinch strength were measured as a percentage of the contralateral side with no controlling for hand dominance. |
| Study characteristics | ||
| Methods | Study Design: parallel group randomised trial Setting: single‐centre; Department of Hand Surgery, Copenhagen University Hospital, Denmark Unit of randomisation: participant Unit of analysis: participant (only contributed one digit) | |
| Participants | Details of sampling frame: Total eligible: not reported Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: 39 participants (39 digits; 39 tendons) Active: 19 tendons (thumb and digits) Passive: 20 tendons (thumb and digits) Sex distribution: not reported Age: not reported Flexor tendon zone: Zone I: 7 (includes one FPL) Zone II: 32 (includes 5 FPL) Inclusion criteria:
Exclusion criteria:
Surgical technique for the flexor repair: Primary tendon repair was performed within three days of injury. Each group received a different surgical technique. Active group: modified Kessler suture (Ti‐cron 4.0) Passive group: grasping suture (Prolene 2.0) and external pull‐out knot technique. Characteristics of participants lost to follow‐up/drop‐outs and included in analysis: Total drop‐outs: 6 (lost to follow‐up: 3; tendon ruptures: 3) Total excluded from analysis: 6 (lost to follow‐up: 3; tendon ruptures: 3) | |
| Interventions | Intervention 1: Active flexion plus active extension exercise regimen (plus modified Kessler suture surgical technique) Components of the intervention: this group's flexor tendon was repaired with a modified Kessler suture (Ti‐cron 4.0). Exercise regimen: early active controlled mobilisation, active extension and active flexion exercises (described as the May et al. protocol, but no citation or further description provided) Dose: not reported Frequency of administration: not reported Intervention 2: Passive flexion plus active extension exercise regimen (plus grasping suture and external pull‐out knot surgical technique) Components of the intervention: this group's flexor tendons were repaired with a grasping suture (Prolene 2.0) and external pull‐out knot technique. Exercise regimen: early passive exercise regimen, active extension and passive flexion exercises (described as the Mantero protocol, but no citation of further description provided). Dose: not reported Frequency of administration: not reported | |
| Outcomes | Outcomes were measured at one‐year post surgery:
| |
| Funding and conflicts of interest statements | Funding source: not reported Conflicts of interest: not reported | |
| Notes | This was a conference proceeding. Hence, very little information was reported in the publication. The authors were contacted to provide more information about the study methods and results, but no response from the authors was received. No clinical trials registration or publication of the full trial was found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "This study was conducted as a prospective randomised design…..." Comment: there is insufficient information in the publication to judge whether the allocation sequence was generated in a random manner. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "This study was conducted as a prospective randomised design…..." Comment: there is insufficient information in the publication to judge whether the allocation sequence was adequately concealed prior to the randomisation. |
| Blinding of participants and personnel (performance bias) | Low risk | Comment: due to the nature of the interventions, it is not likely that the participants or the intervention personnel would have been blinded to the intervention. However, none of the outcomes were self‐reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: there is insufficient information to determine whether the outcome assessors were blinded to the intervention. |
| Incomplete outcome data (over 6 months) (attrition bias) | Unclear risk | Comment: the conference abstract details that six participants were either lost to follow‐up or had tendon ruptures and therefore were not included in the one year follow‐up. It is not reported which group these drop‐outs occurred in and whether this biased the results. |
| Selective reporting (reporting bias) | Unclear risk | Comment: the outcomes and methods for measurement are not detailed in the methods section of the conference abstract. It is unclear whether selective outcome reporting occurred. Also, without a trial protocol, it is unclear whether other outcomes were assessed but not reported. |
| Other bias (outcomes appropriately analysed) | High risk | Comment: groups received different surgical interventions that may have biased the results in favour of one group over another. As it appears that each participant only contributed one digit, it does not appear that an unit of analysis error has occurred. No further sources of bias were identified. |
| Study characteristics | ||
| Methods | Study design: parallel group randomised controlled trial Setting: single‐centre; Service of Hand Surgery and Microsurgery, Clinica SOS Mao, Porto Alegre, Brazil Unit of randomisation: participant Unit of analysis: unclear | |
| Participants | Details of sampling frame: Total eligible: not reported Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: 84 participants (84 digits; 152 tendons) Sex distribution: not reported Age: mean (range): Group 1: 32 (20 to 64) years Flexor tendon zone: zone II: 84 digits Inclusion criteria:
Exclusion criteria:
Surgical technique for the flexor tendon repair: Surgery was performed under axillary block and tourniquet. Brunner’s zigzag palmar incisions. Tendon repair was a combined Kessler’s modified technique using 3‐0 synthetic monofilament. A2, A3, A4 pulleys were preserved. Tendon sheath was not sutured. Arterial and nerve injuries, when present, were repaired with 9‐0 synthetic monofilament. All surgeries were performed 7 to 21 days after traumatic injury. Characteristics of participants lost to follow‐up/drop‐outs and included in analysis: Total available for follow‐up: not reported Total drop‐outs: not reported Total analysed: not reported | |
| Interventions | Intervention: Active exercise regimen Components of the intervention: exercise regimen: early active mobilisation initiated at 12 hours after tendon repair ‐ active flexion/extension exercises. Orthosis: dorsal splint protection (as per both groups). After re‐operation for an adverse event, the patient was then placed again on the same exercise regimen. Participants were reviewed weekly during the first month and post‐operative follow‐up ranged from 12 to 36 months. Dose: 10 repetitions of each movement. Frequency of administration: every waking hour for 16 hours per day. Intervention: Immobilisation regimen Components of the intervention: hand immobilised with a dorsal splint for three weeks; as per both groups (detailed below) Both groups: Components of the intervention: hand immobilised in a dorsal orthosis positioned in 30 to 60 degrees wrist flexion and the MCP joints in 90 degrees flexion with the IP joints extended. The orthosis was removed at week 3 post‐surgery. Participants were seen weekly at the clinic during the first month. Dose: orthosis: worn full time Frequency of administration: orthosis: worn full time for three weeks | |
| Outcomes | Outcomes were recorded at a minimum of 12 months (mean 22 months, range 12 to 36 months) post‐surgery:
| |
| Funding and conflicts of interest statements | Funding source: not reported | |
| Notes | There is some difficulty identifying the unit of analysis for the analysis: e.g. tenolysis unit of analysis is “cases”. We have assumed that since each participant only offered one digit to the study that a case represents both digit and person. The number of participants in each group was calculated manually from the data provided in the publication. No clinical trial registration found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were prospectively randomised, and divided into two groups." Comment: there is insufficient information in the publication to judge whether the allocation sequence was generated in a random manner. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were prospectively randomised, and divided into two groups." Comment: there is insufficient information in the publication to judge whether the allocation sequence was adequately concealed until the interventions were assigned. |
| Blinding of participants and personnel (performance bias) | High risk | Comment: given the nature of the interventions, participants were not blind to treatment, and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: it is not reported whether the outcome assessors were blinded to the intervention, or who the outcome assessors were. |
| Incomplete outcome data (over 6 months) (attrition bias) | Unclear risk | Comment: it is unclear in the publication the flow through of participants from baseline, to randomisation, to outcome measurement at 12 months. It is unclear whether the number of participants reported includes any drop‐outs. |
| Selective reporting (reporting bias) | High risk | Comment: all outcome measures reported in the methods section were reported in the results section of the publication. However, without a trial protocol, it is unclear whether other outcomes were assessed but not reported. Further, no means or standard deviations for the range of movement measurements were reported. |
| Other bias (outcomes appropriately analysed) | Unclear risk | Comment: randomisation occurred at the participant level. However, it is sometimes unclear whether some of the outcomes were reported at the tendon level (some participants had two tendons repaired) or at the participant or digit level. Therefore, a unit of analysis error may have occurred. |
| Study characteristics | ||
| Methods | Study Design: parallel group randomised controlled trial Setting: single‐centre; Department of Plastic Surgery, Netherlands; 2003 to 2005 Unit of randomisation: participant Unit of analysis: unclear | |
| Participants | Details of sampling frame: Total eligible: not reported Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: 28 participants Sex distribution: not reported at baseline Age: not reported at baseline Flexor tendon zone: not reported Inclusion criteria:
Exclusion criteria:
Surgical technique: not reported Characteristics of participants lost to follow‐up/drop‐outs and included in analysis: Total available for follow‐up: 25 participants Total drop‐outs: 0 Total crossed over group: 1 participant allocated motor imagery was crossed over to the control Total analysed: 25 participants Intervention (baseline/follow‐up) n = 13/12* Control (baseline/follow‐up) n = 12/13* Sex distribution at follow‐up: Motor imagery: 9 males; 3 females Control: 9 males; 4 females Age: mean ± SD (range) at follow‐up: Motor imagery: 36.1 ± 11.3 years Control: 31.1 ± 10.0 years | |
| Interventions | Intervention: Motor imagery (MI) Components of the intervention: participants were instructed to perform active flexion and extension movements mentally during the immobilisation period. The instructions were as follows: “Try to imagine as vividly as possible that you slowly clench your fingers and bend the wrist of your splinted hand. Host this image for 3 seconds. Next, imaging that you straighten your wrist and stretch your fingers. Repeat these imaginary movements 10 times (1 session).” Participants entered the actual number of sessions they performed on a form at the end of each day. Dose: each imagined movement was performed 10 times held for three seconds Frequency of administration: 8 sessions per day Control: Standard care hand therapy There are no actual specific details of what the control group was provided but it is assumed that they received the treatment that both groups were provided (below), and no additional treatments were provided. Both groups: Participants of both groups underwent their regular treatment. Components of the intervention: orthosis: relative immobilisation using a Kleinert orthosis. with a wrist band to enable the fingers to be held in a flexed position. Exercise regimen: during the first four weeks postoperatively, only passive flexion of the finger joints was allowed. At 4 to 6 weeks: place‐and‐hold exercises were also practiced: exercises in which the patient flexes their fingers passively with the help of the hand. The fingers are released and the patient is to hold the fingers in the flexed position. Dose:orthosis: 6 weeks full‐time wear; wrist band worn only at night. Frequency of administration: exercise regimen: not reported | |
| Outcomes | Outcomes were assessed at 6, 7, 8, 10, and 12 weeks postoperatively
| |
| Funding and conflicts of interest statements | Funding source: not reported | |
| Notes | Participants of the motor imagery group had significantly more injured tendons per person (2.3 ± 0.5) compared with the control group (1.5 ± 1.0). One participant allocated motor imagery was found to have a low VMIQ score (< 72) and was crossed‐over into the control group. However, the participant flow diagram in the trial report does not make this clear. *There also appears to be an error in Figure 1 (page 555) of the trial report with respect to the number of participants at baseline and follow‐up in each group. This could reflect that one participant was crossed‐over from the motor imagery group to the control group; but this is not made clear. No clinical trial registration found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After inclusion, subjects were admitted at random to either the control group of the motor imagery group…." Comment: it is unclear how the random sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "After inclusion, subjects were admitted at random to either the control group of the motor imagery group…." Comment: it is unclear how the random allocation sequence was concealed until the interventions were assigned. |
| Blinding of participants and personnel (performance bias) | High risk | Comment: given the nature of the interventions, participants were not blind to treatment, and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) | High risk | Comment: non‐blinded participants, who may have had different expectations about the benefits of the intervention they received self‐reported some outcomes. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: there is insufficient information to determine whether the outcome assessor was blinded to the intervention group. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Unclear risk | Comment: there are some discrepancies with the PRISMA flow chart numbers and the numbers of participants at baseline and 12 week follow‐up in the publication. It is unclear how any dropouts were accounted for in the analysis. |
| Selective reporting (reporting bias) | High risk | Comment: in the methods section, most outcomes were recorded at 6, 7, 8 and 10 weeks. However, only the 12 week data are reported in the publication. Also, without a trial protocol, it is unclear whether other outcomes were assessed but not reported. Means and standard deviations for main outcomes were also not reported. |
| Other bias (outcomes appropriately analysed) | High risk | Comment: it is unclear whether a unit of analysis error may have occurred with the pinch strength measurements: in the methods it states that pinch strength was measured for each digit, and for a number of participants more than one tendon was damaged. |
| Study characteristics | ||
| Methods | Study design: parallel group randomised trial Setting: multi‐centre; eight hand surgery centres, Washington, USA Unit of randomisation: participant Unit of analysis: participant and digit (as appropriate) | |
| Participants | Details of sampling frame: Total eligible: 103 participants (119 digits) Total excluded pre‐randomisation: 0 participants (0 digits) Baseline characteristics: Total randomised: 103 participants (119 digits) Place and hold group: 52 participants (61 digits) Controlled passive group: 51 participants (58 digits) Sex distribution: not reported at baseline Age: not reported at baseline Flexor tendon zone: zone II: 119 digits Inclusion criteria:
Exclusion criteria:
Surgical technique: Patients had operation within 48 hours of injury. Skin incision left to discretion of surgeon – most were Bruner incision for oblique lacerations, mid‐axial incisions for transverse lacerations. All repairs were 4‐strand using Strickland technique with 3‐0 polyester for two core sutures, and 6‐0 monofilament Prolene for running epitendinous suture. No repair of the tendon sheath was done. The two slips of the FDS were repaired with a simple core Kessler sutures with 3‐0 polyester. When nerves were injured, they were repaired with microsurgery. All participants had zone II repairs– multiple fingers. Characteristics of participants lost to follow‐up/drop‐outs and included in analysis: Total available for 12‐month follow‐up: 93 (106 digits) Place and hold group: 47 participants (54 digits) Controlled passive group: 46 participants (52 digits) Total analysed (excluding tendon ruptures): 89 participants (102 digits) at 12‐month follow‐up Place and hold group: 46 patients (52 digits) Controlled passive group: 44 patients (50 digits) Sex distribution at follow up: 63 males; 30 females Age: mean (range) at follow up: Mean 29 years (15 to 51 years) Place and hold: 28 (16 to 51) years Controlled passive: 32 (15 to 49) years | |
| Interventions | Intervention 1: Place and hold exercise regimen 72 hours to 4 weeks post‐surgery: Components of the intervention: exercise regimen: place and hold and passive exercise programmes using a hinged orthosis (specific for the exercise regimen) that allows for wrist extension while still maintaining the MCP joints in flexion initiated on day 3 post‐surgery. Participant completed place and hold exercise regimen within the orthosis ‐ passively, the wrist is placed into 30 degrees extension, while fingers are pushed passively intro flexion; participant gently contracts the finger flexors to attempt to hold the flexed position, and then relaxes and allows the wrist to drop into flexion and the fingers to extend. Orthosis: between therapy sessions, patients were managed with a static dorsal blocking orthosis that maintained the wrist and MCPJs in flexion. Dose: each place and hold exercise is held for five seconds. Number of repetitions not reported. Orthosis: dorsal blocking splint is worn full time between exercise sessions. Frequency of administration: exercise regimen: Hourly. Orthosis: dorsal blocking splint is worn between exercise sessions. 2 to 4 weeks: Components of the intervention: exercise regimen: place and hold and passive exercises that were now performed without the tenodesis orthosis. Orthosis: between therapy sessions, participants continue to wear dorsal blocking orthosis. Dose: each place and hold exercise is held for five seconds. Number of repetitions not reported. Orthosis: dorsal blocking splint is worn full time between exercise sessions. Frequency of administration: exercise regimen: hourly. Orthosis: dorsal blocking splint is worn between exercise sessions. 4 weeks: Components of the intervention: exercise regimen: tenodesis exercises without an orthosis. Active movement from full fist, to hook fist to straight fist to full finger extension commenced. Orthosis: between therapy sessions, participants continue to wear dorsal blocking orthosis. Dose: each place and hold exercise is held for five seconds. Number of repetitions not reported. Orthosis: dorsal blocking splint is worn full time between exercise sessions. Frequency of administration: exercise regimen: not reported. Orthosis: dorsal blocking splint is worn between exercise sessions. 5 weeks: Components of the intervention: exercise regimen: week 4 exercises plus active wrist and finger flexion following by wrist and finger extension. Orthosis: between therapy sessions, participants continue to wear dorsal blocking orthosis. Dose: number of repetitions not reported. Orthosis: dorsal blocking splint is worn full time between exercise sessions. Frequency of administration: exercise regimen: not reported. Orthosis: dorsal blocking splint is worn between exercise sessions. 6 weeks: Components of the intervention: exercise regimen: active finger flexion exercises with joint blocking are added to the regimen. Buddy taping may be applied to facilitate flexion. Orthosis: discontinue wear. Dose: exercise regimen: not reported Frequency of administration: exercise regimen: not reported 7 weeks: Components of the intervention: exercise regimen: passive extension exercises and extension splints may be used when indicated. Dose: as needed. Frequency of administration: as needed. 9 weeks: Components of the intervention: light strengthening commenced. Dose: not reported. Frequency of administration: not reported. 10 to 14 weeks: Components of the intervention: progressive strengthening programme to regain pre‐operative strength. Unrestricted activity allowed at 14 weeks. Dose: not reported. Frequency of administration: not reported. Intervention 2: Controlled passive exercise regimen Combined protocols from both the Duran (passive exercise program) and Kleinert (rubber band traction) passive motion rehabilitation program allowed patients to come out of the rubber‐band traction to perform the passive Duran therapy with the therapist. Only the injured digit was placed in the Kleinert rubber‐band traction. 24 hours to 3 weeks: Components of the intervention: orthosis: long arm dorsal blocking orthosis. Exercise regimen: all participants commenced an active extension and passive flexion exercise regimen. Oedema management: participants were provided with compressive wraps within 24 to 72 hours post‐surgery. Dose: orthosis: full‐time wear for 72 hours. Exercise regimen: not reported. Oedema management: not reported. Frequency of administration: orthosis: full‐time wear from immediately post‐surgery until commenced hand therapy (within 72 hours). Exercise regimen: not reported. Oedema management: not reported 3 to 6 weeks: Components of the intervention: exercise regimen: place and hold exercises commenced. Orthosis: rubber band traction applied to a dorsal blocking orthosis and wrist position changed to neutral. Dose: not reported Frequency of administration: not reported 6 to 9 weeks: Components of the intervention: exercise regimen: passive extension of isolated joints, combined joint finger extension exercises with wrist flexed. and light function commenced. Orthosis: wean from dorsal blocking splint. Dose: not reported Frequency of administration: not reported 9 to 12 weeks: Components of the intervention: exercise regimen: blocking exercises for PIP and DIPJs, progressive resistive exercises. Orthosis: commence static progressive splinting and/or gentle extension splinting for joint contractures as needed. Dose: not reported Frequency of administration: not reported 12 to 14 weeks: Components of the intervention: light to moderate resistive activities. Dose: not reported Frequency of administration: not reported 16 weeks: No precautions Both groups: 24 to 72 hours post‐surgery: Components of the intervention: orthosis: Long arm dorsal blocking orthosis. Exercise regimen: all participants commenced an active extension and passive flexion exercise regimen. Oedema management: participants were provided with compressive wraps within 24 to 72 hours post‐surgery. Dose: orthosis: full‐time wear for 72 hours. Exercise regimen: not reported. Oedema management: not reported. Frequency of administration: orthosis: full‐time wear from immediately post‐surgery until commenced hand therapy (within 72 hours). Exercise regimen: not reported. Oedema management: not reported. (Full protocol available in the appendix of the publication) | |
| Outcomes | Outcomes measured at 6, 12, 26, 52 weeks:
| |
| Funding and conflicts of interest statements | Funding source: Orthopaedic Research and Education Foundation (external funding agency) | |
| Notes | No clinical trial registration found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Each centre had a research coordinator who enrolled the patients and randomised the treatments. The research coordinator performed the randomisation by drawing a card indiscriminately from an envelope with an equal number of cards labelled active or passive before the patient started therapy." Comment: the randomisation sequence appears to have been generated using an adequate method. |
| Allocation concealment (selection bias) | Low risk | Quote: the research coordinator performed the randomisation by drawing a card indiscriminately from an envelope with an equal number of cards labelled active or passive before the patient started therapy." Comment: the allocation sequence appears to have been adequately concealed prior to assignment of interventions. |
| Blinding of participants and personnel (performance bias) | High risk | Comment: insufficient information to determine from the publication. However, given the nature of the interventions (participation in an exercise programme with orthoses), participants could not be blinded to treatment, and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) | High risk | Comment: non‐blinded participants, who may have had different expectations about the benefits of the intervention they received self‐reported some outcomes. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "The therapist who performed the therapy also recorded the measurements of motion, sensation and dexterity so they could not be blinded…" Comment: the outcomes assessors were not blinded to the group allocations. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Unclear risk | Comment: only range of motion data were collected at the six week time point. It is unclear whether this is a complete data set or participants were lost to attrition at these time points, as the number of participants included in the assessments are not reported. Just because it is not reported we can not assume it is a full data set. |
| Incomplete outcome data (3 to 6 months) (attrition bias) | Unclear risk | Comment: it is unclear how many participants were loss to follow‐up at 3 and 6 month evaluation. Only range of motion was measured at the 3 and 6 month evaluation. |
| Incomplete outcome data (over 6 months) (attrition bias) | Low risk | Quote: "Ten patients (13 digits) were lost to follow up, resulting in 93 patients and 106 injured digits who completed the 12‐month follow up evaluation." Comment: the number of participants and digits lost to follow‐up were reported. However, it is unclear how these participants differed to those who were analysed at the earlier time points for range of motion, or how these drop outs may have affected the data. Although, the loss to follow‐up appears to be accounted for the 12 months evaluation at which time the majority of the outcomes were measured. |
| Selective reporting (reporting bias) | Unclear risk | Comment: the outcomes were reported as per the pre‐specified methods section. However, without a trial protocol, it is unclear whether other outcomes were assessed but not reported. |
| Other bias (outcomes appropriately analysed) | Low risk | Comment: it is unlikely that a unit of analysis error occurred as outcomes reported per person are reported as such (e.g. DASH, dexterity measures, satisfaction). Range of motion was calculated per digit. The authors disclosed funding for the project; however, it does not appear that this would have influenced the results in any way as it appears to have been from a non‐commercial granting agency. No further sources of risk of bias were identified. |
| Study characteristics | ||
| Methods | Study Design: randomised trial Setting: single‐centre; Department of Plastic and Reconstructive Surgery of Nizam’s Institute of Medical Sciences, Hyderabad, India Unit of randomisation: participant Unit of analysis: unclear | |
| Participants | Details of sampling frame: Total eligible: 46 participants (digits: not reported) Total excluded pre‐randomisation: 16 participants (digits: not reported) Baseline characteristics: Total randomised: 30 participants (digits: not reported) Place and hold: 15 participants (digits: not reported) Passive: 15 participants (digits: not reported) Sex distribution: not reported Age: not reported Flexor tendon zone: zone V: 46 participants Inclusion criteria:
Exclusion criteria:
Surgical technique for flexor tendon repair: Not reported Characteristics of participants lost to follow‐up/drop‐outs and included in analysis Total lost to follow up/drop‐outs: 0 participants Total available for 12‐week follow‐up: 30 participants (digits: not reported) Total analysed: 30 participants (digits: not reported) | |
| Interventions | Intervention 1: Early place and hold progressed to tendon gliding exercise regimen (multiple treatments) Week 1 to 3: Place and hold exercise regimen Components of the intervention: orthosis: dorsal blocking splint (wrist in 20° to 30°, MCP in 50° to 70°, IPJs in extension). Exercise regimen: within the orthosis: (1) active PIP and DIP joint extension; (2) isolated passive PIP and DIP flexion, followed by composite passive finger exercise; (3) place and hold exercise. Dose: exercise regimen: (1) 50 repetitions; (2) 5 to 10 repetitions; (3) 2 to 5 repetitions Frequency of administration: exercise regimen: hourly Weeks 4 to 5: Graduated tendon gliding exercise regimen Components of the intervention: orthosis: ceased early only if there is poor movement/scarring. Exercise regimen: (1) MCP joint blocked in flexion and gentle progressive IP joint extension; (2) FDS/FDP tendon gliding; (3) upgrade at five weeks to include non‐resistive blocking exercises Dose: exercise regimen: not reported Frequency of administration: exercise regimen: not reported Week 6: Full passive stretching exercise regimen Components of the intervention: orthosis: ceased. Exercise regimen: passive stretching exercise regimen for all joints Dose: exercise regimen: not reported Frequency of administration: exercise regimen: not reported Intervention 2: Early passive progressed to active exercise regimen (multiple treatments) Week 1 to 3: Passive exercise regimen Components of the intervention: orthosis: dorsal blocking splint (wrist in 40 to 50 degrees, MCP 50 to 70 degrees, IPJs in extension). Exercise regimen: within the orthosis: passive exercise to all IP joints Dose: exercise regimen: not reported Frequency of administration: exercise regimen: hourly Week 4 to 6: active exercise regimen Components of the intervention: exercise regimen: active MCP and IP joint exercises Dose: exercise regimen: not reported Frequency of administration: exercise regimen: hourly Both groups: Components of the intervention: orthosis: each group received a dorsal blocking splint but at different wrist positions. Orthosis was discarded at four weeks unless there was excellent motion and in this case, orthosis was work for an additional 1 to 2 weeks. Exercise regimen: shoulder and elbow (no forearm) in all planes; (2) At week 4 ‐ active wrist exercises. Oedema reduction: elevation. Pain relief: TENS. Scar care: at week 3 (massage inside orthosis). Electrical stimulation: to promote tendon glide. Graded functional activity and strengthening regimen: commenced at week 6 and progressed to normal function by week 12. Dose: orthosis: full time for six weeks. Exercise regimen: not reported. Oedema reduction: not reported. TENS: not reported. Scar care: not reported. Electrical stimulation: not reported. Graded functional activity: not reported. Frequency of administration: orthosis: worn full time. Scar care: during therapy sessions (unknown frequency). Oedema reduction: not reported. TENS: not reported. Electrical stimulation: not reported. Graded functional activity and strengthening regimen: not reported. NB: There is insufficient information in the publication to determine when the exercise regimen commenced during the first week post‐operation. | |
| Outcomes | Outcomes were measured at 4 and 12 weeks:
| |
| Funding and conflicts of interest statements | Funding source: self‐funded | |
| Notes | Outcomes were reported as differences between the 12th week and baseline measures or 4th week and baseline for range of motion (TAM). Participants contributed one or more tendons to the studies. The number of digits reported and the unit of analysis for each outcome is not reported. There is also insufficient information to determined the unit of analysis from the publication. A unit of analysis error may have occurred. No clinical trials registration found. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " Thirty subjects who fit the criteria were selected and randomly divided into two groups of 15 each by lottery method…" |
| Allocation concealment (selection bias) | Unclear risk | Comment: there is insufficient information to determine how the random allocation sequence was concealed until the interventions were assigned. Clarification from the authors has been requested but was not received at the time of publication. Although a lottery method was used, it is unclear when the randomisation using this method occurred. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: " Patients were blinded for being in either of the groups." |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: it is not reported who conducted the outcome assessments and whether they were blinded to the participant's intervention assignment. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Low risk | Quote: "No tendon ruptures or subject drop‐outs were recorded." Comment: there was no attrition. Data were reported on a complete data set. |
| Selective reporting (reporting bias) | High risk | Comment: all outcomes described in the methods section of the paper are reported in the results section of the paper. No clinical trials registry was identified in the publication. Data are reported as the improvement from the first ROM measurement taken at week 1 to week 12, and then compared between groups. Baseline measurements are not reported nor does it state whether these were accounted for in the analysis. Mean and standard deviation scores for the different time points are not reported. |
| Other bias (outcomes appropriately analysed) | High risk | Comment: it is unclear whether a unit of analysis error may have occurred as the numbers of participants, hands and digits in each group included in the analysis are not reported. The authors had no conflicts of interest or funding sources. No further sources of bias detected. Outcomes were not appropriately analysed and were reported in a way that was not able to be interpreted in a meaningful way by the review authors. |
| Study characteristics | ||
| Methods | Study Design: parallel group randomised trial Setting: France Unit of randomisation: participant Unit of analysis: unclear | |
| Participants | Details of sampling frame: Total eligible: not reported Total excluded pre‐randomisation: not reported Baseline characteristics: Total randomised: 35 participants (digits: not reported) Active group: 16 participants Controlled passive group: 19 participants Sex distribution: not reported Age: mean: 35 years Flexor tendon zone: zone II: 35 participants Inclusion criteria:
Exclusion criteria:
Surgical technique: Primary repair was performed as an emergency procedure using a 4/0 absorbable Tsuge core suture and a peripheral epitenon running suture (6/0 Prolene). Characteristics of participants lost to follow‐up/drop‐outs and included in analysis Total lost to follow up/drop‐outs: not reported Total available for follow‐up: not reported Total analysed: not reported | |
| Interventions | Intervention 1: Early active flexion plus passive exercise regimen (Strickland and Small protocol) Components of the intervention: exercise regimen: Passive flexion, active flexion and active extension within the orthosis using the Strickland exercise regimen. Authors cited these papers for their intervention protocol, Strickland 2000; Small 1989. Dose: exercise regimen: not reported Frequency of adminstration: exercise regimen: not reported Intervention 2: Controlled passive exercise regimen (modified Kleinert protocol) Components of the intervention: exercise regimen: controlled passive mobilisation using rubber band traction. Authors stated using the Kleinert protocol as referenced in Kleinert (Kleinert 1967). Dose: exercise regimen: not reported Frequency of administration: exercise regimen: not reported Both groups: Components of the intervention: rehabilitation started at three days post‐operation for both groups (other intervention components not reported). Dose: exercise regimen: not reported Frequency of administration: exercise regimen: not reported | |
| Outcomes | Outcomes were measured at 8, 12 and 24 weeks:
| |
| Funding and conflicts of interest statements | Funding source: not reported | |
| Notes | This was a conference proceeding. Hence, very little information was reported in the publication. No other publications of the trial were found. The authors were contacted to provide more information about the study methods and results, but no response from the authors was received. Insufficient information is provided in the publication to determine whether or not a unit of analysis error may have occurred. However, very little data are included in the abstract. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "This prospective randomised study was designed to compare two methods of early mobilisation (Kleinert versus Strickland protocol) after primary repair of flexor tendons." Comment: there is insufficient information in the publication to judge whether the allocation sequence was generated in a random manner. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "This prospective randomised study was designed to compare two methods of early mobilisation (Kleinert versus Strickland protocol) after primary repair of flexor tendons." Comment: there is insufficient information in the publication to judge whether the allocation sequence was adequately concealed prior to the randomisation. |
| Blinding of participants and personnel (performance bias) | High risk | Comment: given the nature of the interventions, participants were not blind to treatment, and may have had different expectations about the benefits of each intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: it is not reported whether the outcome assessors were blinded to the intervention. |
| Incomplete outcome data (less than 3 months) (attrition bias) | Unclear risk | Comment: the participant flow was not reported and is unclear. It is unclear whether the number of participants reported were those that were randomised into the study and/or those available at follow‐up. Clarification from the authors has been requested but was not received at the time of publication. |
| Incomplete outcome data (3 to 6 months) (attrition bias) | Unclear risk | Comment: the participant flow was not reported and is unclear. It is unclear whether the number of participants reported were those that were randomised into the study and/or those available at follow‐up. Clarification from the authors has been requested but was not received at the time of publication. |
| Selective reporting (reporting bias) | High risk | Comment: the outcomes mentioned in the methods section are not fully reported in the results section of the conference abstract. Also, without a trial protocol, it is unclear whether other outcomes were assessed but not reported. Fingertip to palm distances and percentages of patients receiving fair or poor outcomes are not reported. Adverse events and mean duration for inability to work are reported for overall participants and not for the individual groups. |
| Other bias (outcomes appropriately analysed) | Unclear risk | Comment: very limited information is given in the conference abstract regarding the number of digits and tendons contributed to the study for each participant. The unit of analysis is unclear. |
ADL: activities of daily living; AROM: active range of motion; CPM: continuous passive motion; CRPS: complex regional pain syndrome; DASH: Disabilities of the Arm, Shoulder and Hand questionnaire; DIP: distal interphalangeal; FDP: flexor digitorum profundus; FDS: flexor digitorum superficialis; FPL: flexor pollicis longus; IF: index flexion; IP: interphalangeal; IPJ: interphalangeal joint; LF: little flexion; LLLT: low level laser therapy; MCP: metacarpophalangeal; MF: middle flexion; MI: motor imagery; NR: not reported; OT: occupational therapist; PAH: place and hold; PDS: polydioxanone suture;PIP: proximal interphalangeal; RCT: randomised controlled trial; RF: ring flexion; ROM: range of motion; RTW: return to work; SD: standard deviation; TAM: total active motion; VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not a randomised trial. | |
| Not a randomised trial. | |
| Not a randomised trial. | |
| Study never started recruitment and was abandoned. | |
| No separate analysis for participants with flexor tendon injuries. Not our outcome of interest (compliance). | |
| Study never started recruitment and was abandoned. | |
| Not a randomised trial. | |
| Not a randomised trial. | |
| Not a randomised trial. | |
| Not a randomised trial. | |
| Included participants had traumatic hand injuries involving bone or/and flexor tendon. No separate analysis for participants with flexor tendon injuries. | |
| Not a randomised trial. |
Characteristics of studies awaiting classification [ordered by study ID]
| Methods | Experimental study, design unclear |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Intervention 1: Controlled active extension x 12/hour. Passive flexion maintained using the Kleinert splint. Intervention 2: Passive flexion and passive extension, performed in a dorsal blocking orthosis. |
| Outcomes | Primary outcomes
Secondary outcomes
|
| Notes | It is unclear whether the study was a randomised trial. We received two emails from the trial authors, one stating that this is a randomised trial, and one stating that this was NOT a randomised trial. We are awaiting further clarification from the authors. |
| Methods | Randomised parallel group controlled trial |
| Participants | 62 children with injury of hand flexor tendon |
| Interventions | Intervention: Rehabilitation exercises by occupational therapy with comprehensive analysis, case treatment, genearch (spl) training and learning from playing Control: Routine comprehensive training |
| Outcomes | Not known |
| Notes | We identified this article post‐editorial review. This article needs to be translated from Chinese. Some information is included in Pedro (https://search.pedro.org.au/search‐results/record‐detail/11056). |
| Methods | Randomised parallel group intervention trial; blinded outcome assessor |
| Participants | Details of sampling frame: Total eligible: 86 Total randomised: 31 Active intervention group: 17 Passive intervention group: 14 Total analysed: 14 (17 participants dropped out of the trial and/or were not able to be reached for follow‐up) Active Intervention group analysed: 6 Passive intervention group analysed: 8 Sex distribution: 23 males; 8 females Active group: 13 males; 4 females Passive group: 10 males; 4 females Mean ± SD (range) age: Active group: 30 (18 to 50) years Passive group: 29 (20 to 41) years Inclusion criteria:
Exclusion criteria:
Surgical technique: Four strand tendon repair, using a 3/0 braided material, oversewn with a continuous nylon 6/0 suture. Setting: Single centre trial, Occupational Therapy Hand Service Department, within a tertiary academic state hospital (Tygerberg Hospital, Cape Town, South Africa) |
| Interventions | Intervention 1: Active rehabilitation Components of the intervention: Exercise regimen: Controlled graded active digital flexion. Dose: Graded programme. Frequency of administration: 5 to 6 45‐minute sessions over 8 to 10 weeks Intervention 2: Passive rehabilitation Components of the intervention: Exercise regimen: Modified Duran protocol focusing on passive digital flexion. Active finger flexion is not introduced until 4 to 5 weeks post repair. Dose: Graded programme. Frequency of administration: 5 to 6 45‐minute sessions over 8 to 10 weeks Both groups: Components of the intervention: Orthosis: Dorsal orthosis (position: wrist in neutral to 20 degrees extension, MCP joints in 80 degrees flexion, IPJs in full extension). |
| Outcomes | Outcome data were collected at eight weeks post‐surgery.
|
| Notes | This was a pilot feasibility trial and hence was not powered to test the effectiveness of the interventions. |
| Methods | Parallel group quasi‐randomised clinical trial |
| Participants | Details of sampling frame: Total eligible: 240 patients (252 tendons) Total excluded pre‐randomisation: Not reported Total randomised: 240 patients (252 tendons) Intervention group: 48 patients (67 tendons) Control group: 192 patients (185 tendons) Sex distribution: 186 males; 54 females Intervention group: 36 males; 12 females Control group: 150 males; 42 females Mean ± SD (range) age: Intervention group: 30.6 ± 8 years Control group: 33 ± 12 years Inclusion criteria:
Exclusion criteria:
Surgical technique: Four strand tendon repair Setting: Single centre trial, Tehran Khordad Hospital, Iran |
| Interventions | Intervention Group: Patients were mobilised at day 14 after surgery, performed active movements and underwent physiotherapy for three months. Control Group: Patients were immobilised for four weeks after surgery. From four weeks, active movements and physiotherapy were done for three months (similar to intervention group). |
| Outcomes |
|
| Notes | The control group has 192 patients with only 185 tendons. We assume this is an error in reporting as there cannot be more number of patients than tendons. There also is a big difference in participant numbers between the two groups. This study does not appear to be randomised (no evidence in support of this description); imbalance in the numbers allocated; incorrect data and percentages that don't compute to whole numbers indicate these data are incorrect. We are awaiting clarification from the authors. |
DASH: Disability of the Arm, Shoulder and Hand; IPJ: interphalangeal joint;FDP: flexor digitorum profundus;FDS: flexor digitorum superficialis; MCP: metacarpophalangeal;
Characteristics of ongoing studies [ordered by study ID]
| Study name | A randomised control trial comparing the functional outcomes in patients with post tendon repair mobilised by conventional hand therapy versus assistive device. |
| Methods | Randomised, parallel group, active controlled trial, interventional design. |
| Participants | Target sample size: 120 participants Inclusion criteria:
Exclusion criteria:
Setting: Department of Orthopaedics, Kasturba Medical College, Manipal, India. |
| Interventions | Intervention 1: Mobilisation with assistive device Intervention 2: Mobilisation with conventional hand therapy Both groups will have intervention provided for a period of three months and two sessions daily one in the morning and one in the evening each session will be for a period of 60 minutes. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | 1 January 2019 |
| Contact information | Ashwath Acharya Phone: 8217736961 Email: [email protected] |
| Notes | WHO Clinical trials registry: CTRI/2019/01/016821 URL: www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=29865 |
| Study name | Comparison of active and passive rehabilitation on outcomes of the flexor tendons repair in zone II of the hand. |
| Methods | Parallel group single blinded randomised controlled trial. |
| Participants | Sample size: 20 participants
Exclusion criteria:
Setting: Hazrat Fatima Hospital, Seyed Jamaleddin Asadabadi Ave, Tehran, Iran (Islamic Republic of). |
| Interventions | Intervention 1: Active rehabilitation. Full range of active flexion and extension of the operated finger under supervision of the occupational therapist; three movements in one session per day for three weeks. Intervention 2: Passive rehabilitation. Full range of passive flexion of the finger (rubber band) and active extension by the patient under supervision of the occupational therapist; three movements in three sessions per day for three weeks. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | 6 November 2013 |
| Contact information | Mohammad Javad Fatemi Phone: +98 21 8871 7272 Email: [email protected] |
| Notes | WHO clinical trials registry: IRCT201310138177N8. URL: en.irct.ir/trial/8628. |
| Study name | The investigation of the effect of two methods of early active and passive motion on hand function and satisfaction in patients with flexor tendon injury in zone I and II. |
| Methods | Randomised double blinded parallel group interventional study design. |
| Participants | Target sample size: 30 participants Inclusion criteria:
Exclusion criteria:
Setting: School of Rehabilitation, Shahid Shahnazari Street, Madar Square, Mirdamad Blvd, Tehran 15459‐13487 Tehran, Iran (Islamic Republic of). |
| Interventions | Intervention 1: "The clients will be referred to the occupational therapist within 24‐24 hours after surgery. In this group, regular rehabilitation programs and the Strickland protocol will be implemented. The treatment sessions will be performed by the therapist for 45 minutes, 3 days a week for 8 weeks. In this method, two splints are used: 1: Dorsal Block Splint, which is made of plaster, and wrist joint in 20 degrees of flexion, metacarpophalangeal at 50 degrees of flexion and interphalangeal in the extension and used most of the time, 2: Splint is a thermoplastic training. The wrist part is hinged and allows full flexion to the wrist, metacarpophalangeal and interphalangeal joints, but limits the wrist at 30 degrees of extension, metacarpophalangeal at 60 degrees and interphalangeal at 25 degrees of flexion. Week 4‐0: Every hour the exercises will be performed by 15 times repetitive exercises in orthosis Dorsal Block and the flexion Place and hold practice with 15 repetitions in orthosis, These exercises will be presented in writing and videos recorded for them at home. Week 8‐4: orthosis training will be lifted, but orthosis Dorsal Block will be covered except during training, and exercises will be done every 2 hours. At 6‐5 weeks, the blocking and hook fist exercises will be performed. 7‐8 weeks of progressive resistance exercises and daily routine activities will be added. At week 14, complete resistance exercises and heavy daily activities will be performed." Intervention 2: "The client will be referred to the occupational therapist within 24‐24 hours after surgery. A therapist will be performed a traditional rehabilitation program modified Duran protocol of 40 minutes, three days per week, for eight weeks. In this group, a dorsal block orthosis will be used, which will place the wrist joint at 20° flexion and metacarpophalangeal at 50° flexion and allowing the interphalangeal joints to be fully extended." |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | 14 August 2018 |
| Contact information | Laleh Lajevardi Phone: +98 21 2222 8051 Email: [email protected] |
| Notes | WHO Clinical trials registry: IRCT20150721023277N7. URL: en.irct.ir/trial/28585. We were unsuccessful in our attempts to obtain more information on this study. |
| Study name | Mobile application for improving rehabilitation after flexor tendon repair |
| Methods | Parallel group randomised controlled trial. |
| Participants | Sample size: 101 participants
Exclusion criteria:
Setting: Karolinska Institutet, Sweden. |
| Interventions | Control Group : Standard treatment. Rehabilitation according to early active motion. Experimental Group: Standard treatment and intervention (smart phone application). Intervention group also received a smart phone app including; exercise videos, push‐notifications for exercise, exercise diary, written information on the surgery, rehabilitation, questions and answers. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | 1 March 2017 |
| Contact information | Marianne Arner and Jonas Svingen Email: [email protected] Phone: +46709360278 |
| Notes | WHO Clinical trials registry: NCT03812978. URL: https://clinicaltrials.gov/show/NCT03812978. |
| Study name | The Manchester Short Splint in the rehabilitation of zone II flexor tendon repairs |
| Methods | Parallel group randomised controlled trial. |
| Participants | Sample size: 60 participants
Exclusion criteria:
Setting: Manchester University NHS Foundation Trust, Manchester, United Kingdom. |
| Interventions | Intervention: Device: Short splint that permits maximal wrist flexion and up to 45° of wrist extension with a block to 30° of MCP joint extension. Active control: Device: Traditional long splint which is a forearm‐based dorsal thermoplastic splint that immobilises the wrist in neutral position with a block to 30° of MCP joint extension. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | 1 June 2015 |
| Contact information | Vivien Lees, Bradley Tallon Email: [email protected]; [email protected] Phone: 0161 291 6648;01612915757 |
| Notes | WHO Clinical trials registry: NCT03850210. URL: https://clinicaltrials.gov/show/NCT03850210. |
| Study name | Electromyographic (EMG) biofeedback training in Zone I‐III flexor tendon injuries |
| Methods | Parallel group randomised controlled trial |
| Participants | Sample size: 22 participants
Exclusion criteria:
|
| Interventions | Intervention: EMG biofeedback training + modified Duran protocol, same physiotherapist three times a week for 12 weeks Control: modified Duran protocol, same physiotherapist three times a week for 12 weeks |
| Outcomes | Primary outcomes:
|
| Starting date | 10 October 2016 |
| Contact information | Umut Eraslan & Ali Kitis, Pamukkale University, Turkey |
| Notes | Clinicaltrials.gov: https://clinicaltrials.gov/ct2/show/NCT04237415 This trial was retrospectively reported. This study has a reported completion date of 21 March 2019. |
| Study name | Primary flexor tendon repair in zone I and II: a prospective randomised trial of passive mobilisation with place‐and‐hold, compared with true active motion therapy |
| Methods | Parallel group randomised intervention trial; blinded outcome assessor |
| Participants | Sample size: 64 participants
Exclusion criteria:
|
| Interventions | Intervention 1: Active rehabilitation: Participant sees an occupational therapist 1 to 3 days after surgery. An orthosis is fabricated to immobilise the wrist and work as an extension block for the MCP joints, and is worn day and night for 4 weeks. Another splint that immobilises the DIP and PIP joints is work whenever the participant is not exercising. During active exercise the participant follows a strict protocol with both active and passive training and increasing number of repetitions for 3 months. |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | 14 July2014 |
| Contact information | Jan Friden, Professor, Sahlgrenska University Hospital, Sweden |
| Notes | clinicaltrials.gov: This trial was retrospectively reported. This study has a reported completion date of 30 August 2018. |
AISEQ: Athlete Injury Self Efficacy Questionnaire; DIP: distal interphalangeal; EMG: electromyography FDP: flexor digitorum profundus;FDS: flexor digitorum superficialis; MCP: metacarpophalangeal; PIP: proximal interphalangeal; SIRAS: Sport Injury Adherence Scale
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | |||||||||||||||||||||||||||||||||||||||
| 1.1 Self‐reported function for ADL using a VAS (0 to 10; higher = better) Show forest plot | 1 | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||
| Analysis 1.1
Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 1: Self‐reported function for ADL using a VAS (0 to 10; higher = better) | |||||||||||||||||||||||||||||||||||||||||||
| 1.2 Self‐reported function using VAS for ADLs (0 to 10; higher scores = better); secondary analyses Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| Analysis 1.2  Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 2: Self‐reported function using VAS for ADLs (0 to 10; higher scores = better); secondary analyses | |||||||||||||||||||||||||||||||||||||||||||
| 1.2.1 ADL VAS at 2 months (0=worst; 10=best) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.2.2 ADL VAS at 3 months (0=worst; 10=best) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.2.3 ADL VAS at 6 months (0=worst; 10=best) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.2.4 ADL VAS at 12 months (0=worst; 10=best) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.3 Active finger range of motion (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| Analysis 1.3  Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 3: Active finger range of motion (degrees) | |||||||||||||||||||||||||||||||||||||||||||
| 1.3.1 Total Active Movement at 1 month (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.3.2 Total Active Movement at 2 months (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.3.3 Total Active Movement at 3 months (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.3.4 Total Active Movement at 6 months (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.3.5 Total Active Movement at 12 months (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.4 Finger range of movement ‐ Poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| Analysis 1.4  Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 4: Finger range of movement ‐ Poor outcome | |||||||||||||||||||||||||||||||||||||||||||
| 1.4.1 Strickland classification at 1 month | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.4.2 Strickland classification at 2 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.4.3 Strickland classification at 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.4.4 Strickland classification at 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.4.5 Strickland classification at 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.4.6 Tang classification at 1 month | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.4.7 Tang classification at 2 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.4.8 Tang classification at 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.4.9 Tang classification at 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.4.10 Tang classification at 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.5 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| Analysis 1.5  Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 5: Adverse events | |||||||||||||||||||||||||||||||||||||||||||
| 1.5.1 Tendon rupture | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.5.2 Complex Regional Pain Syndrome | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.5.3 Wound dehiscence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.5.4 Transitory swelling + tenderness | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.5.5 Any adverse event | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.6 Strength (% of the contralateral hand or digit) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| Analysis 1.6  Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 6: Strength (% of the contralateral hand or digit) | |||||||||||||||||||||||||||||||||||||||||||
| 1.6.1 Grip Strength at 3 months (% of the contralateral hand) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.6.2 Grip Strength at 6 months (% of the contralateral hand) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.6.3 Grip Strength at 12 months (% of the contralateral hand) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.6.4 Pinch Strength at 3 months (% of the contralateral digit) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.6.5 Pinch Strength at 6 months (% of the contralateral digit) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| 1.6.6 Pinch Strength at 12 months (% of the contralateral digit) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2: Early active flexion + active extension exercise regimen (+ modified Kessler suture surgical technique) versus passive flexion + active extension exercise regimen (+ grasping suture and external pull‐out knot surgical technique), Outcome 1: Adverse events | ||||
| 2.1.1 Tendon ruptures | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1.2 Scar adhesions requiring surgery (Tenolysis) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Range of movement at 12+ months: poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3: Active exercise regimen versus immobilisation regimen, Outcome 1: Range of movement at 12+ months: poor outcome | ||||
| 3.1.1 IFSSH criteria | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1.2 Strickland criteria | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.2  Comparison 3: Active exercise regimen versus immobilisation regimen, Outcome 2: Adverse events | ||||
| 3.2.1 Tendon ruptures | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.2.2 Movement restrictions indicating need for tenolysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.2.3 Secondary surgery (actual or indicated) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Grip strength at 12 weeks (% difference between normal and affected hands) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.1  Comparison 4: Early place and hold progressed to tendon gliding exercise regimen versus early passive progressed to active exercise regimen, Outcome 1: Grip strength at 12 weeks (% difference between normal and affected hands) | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 5.1 Function (self‐reported): DASH scores (0 to 100; higher score = more disability) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.1  Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 1: Function (self‐reported): DASH scores (0 to 100; higher score = more disability) | ||||
| 5.1.1 DASH at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1.2 DASH at 52 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.2 Range of movement (Total Active Movement) (degrees) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.2  Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 2: Range of movement (Total Active Movement) (degrees) | ||||
| 5.2.1 At 8 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.2.2 At 52 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.3 Range of movement (Strickland Criteria) at 8 weeks: Poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.3  Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 3: Range of movement (Strickland Criteria) at 8 weeks: Poor outcome | ||||
| 5.4 Adverse events Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.4  Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 4: Adverse events | ||||
| 5.4.1 Tendon rupture | 3 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.19, 3.50] |
| 5.4.2 Scar adherence | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.04 [0.00, 0.66] |
| 5.4.3 Flexion contracture of the DIP joint | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.02, 0.88] |
| 5.4.4 Flexion contracture of the PIP joint | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.15, 1.48] |
| 5.4.5 FDS tendon lag | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.06, 0.98] |
| 5.4.6 FDP tendon lag | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.04, 0.62] |
| 5.5 Function (observed): Jebsen Taylor at 52 weeks (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.5  Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 5: Function (observed): Jebsen Taylor at 52 weeks (seconds) | ||||
| 5.6 Function (observed): Purdue pegboard at 52 weeks (pegs) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.6  Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 6: Function (observed): Purdue pegboard at 52 weeks (pegs) | ||||
| 5.7 Satisfaction with hand function (0 to 10: complete satisfaction) at 6 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.7  Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 7: Satisfaction with hand function (0 to 10: complete satisfaction) at 6 months | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 6.1 Adverse event (tendon rupture) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.1  Comparison 6: Unrestricted activity at 8 weeks post‐surgery versus unrestricted activity at 10 weeks, Outcome 1: Adverse event (tendon rupture) | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 7.1 Function (self‐reported): DASH scores (0 to 100; higher score = more disability) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.1  Comparison 7: Exoskeleton versus physiotherapy, Outcome 1: Function (self‐reported): DASH scores (0 to 100; higher score = more disability) | ||||
| 7.1.1 DASH at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1.2 DASH at 18 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2 Active finger range of motion of PIP joint (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.2  Comparison 7: Exoskeleton versus physiotherapy, Outcome 2: Active finger range of motion of PIP joint (degrees) | ||||
| 7.2.1 PIP joint range of motion at 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2.2 PIP joint range of motion at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2.3 PIP joint range of motion at 18 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.3 Active finger range of motion of DIP joint (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.3  Comparison 7: Exoskeleton versus physiotherapy, Outcome 3: Active finger range of motion of DIP joint (degrees) | ||||
| 7.3.1 DIP joint range of motion at 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.3.2 DIP joint range of motion at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.3.3 DIP joint range of motion at 18 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.4 Active finger range of motion (Total Active Movement) (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.4  Comparison 7: Exoskeleton versus physiotherapy, Outcome 4: Active finger range of motion (Total Active Movement) (degrees) | ||||
| 7.4.1 TAM at 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.4.2 TAM at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.4.3 TAM at 18 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.5 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 7.5  Comparison 7: Exoskeleton versus physiotherapy, Outcome 5: Adverse events | ||||
| 7.5.1 Tendon rupture | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.5.2 CRPS (complex regional pain syndrome) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.6 Strength at 18 weeks Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 7.6  Comparison 7: Exoskeleton versus physiotherapy, Outcome 6: Strength at 18 weeks | ||||
| 7.6.1 Grip strength (kg) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.6.2 Pinch strength (kg) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 8.1 Active finger range of motion (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.1  Comparison 8: Continuous passive motion device versus controlled passive progressed to active exercise regimen (Modified Kleinert), Outcome 1: Active finger range of motion (degrees) | ||||
| 8.1.1 TAM at > 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.2 Range of movement at > 6 months (Strickland criteria) ‐ poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.2  Comparison 8: Continuous passive motion device versus controlled passive progressed to active exercise regimen (Modified Kleinert), Outcome 2: Range of movement at > 6 months (Strickland criteria) ‐ poor outcome | ||||
| 8.3 Adverse event Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 8.3  Comparison 8: Continuous passive motion device versus controlled passive progressed to active exercise regimen (Modified Kleinert), Outcome 3: Adverse event | ||||
| 8.3.1 Tendon rupture at >6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.3.2 Infection at >6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 9.1 Improvement in active range of movement (Difference between 3 and 12 weeks; Total Active Motion measured in degrees) Show forest plot | 1 | 131 | Mean Difference (IV, Fixed, 95% CI) | 26.47 [19.70, 33.24] |
| Analysis 9.1  Comparison 9: Ultrasound versus control, Outcome 1: Improvement in active range of movement (Difference between 3 and 12 weeks; Total Active Motion measured in degrees) | ||||
| 9.1.1 1MHz; 0.7W/cm2 increased to 1w/cm2 | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 31.50 [19.94, 43.06] |
| 9.1.2 1 MHz; 0.3w/cm2 increased to 1.0w/cm2 | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 23.80 [11.89, 35.71] |
| 9.1.3 3Mhz; 0.5w/cm2 increased to 0.7w/cm2 | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 23.90 [12.20, 35.60] |
| 9.2 Active finger range of motion (Strickland classification) at 3 months ‐ Poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 9.2  Comparison 9: Ultrasound versus control, Outcome 2: Active finger range of motion (Strickland classification) at 3 months ‐ Poor outcome | ||||
| 9.3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 9.3  Comparison 9: Ultrasound versus control, Outcome 3: Adverse events | ||||
| 9.3.1 Tendon rupture at 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.3.2 Wound dehiscence <3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 10.1 Active finger range of motion (Total active motion (degrees)) at 12 weeks Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 10.1  Comparison 10: Low‐level laser therapy versus placebo control, Outcome 1: Active finger range of motion (Total active motion (degrees)) at 12 weeks | ||||
| 10.2 Range of movement at 12 weeks: poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 10.2  Comparison 10: Low‐level laser therapy versus placebo control, Outcome 2: Range of movement at 12 weeks: poor outcome | ||||
| 10.2.1 Strickland scoring system at 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.3 Adverse events Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 10.3  Comparison 10: Low‐level laser therapy versus placebo control, Outcome 3: Adverse events | ||||
| 10.3.1 Tendon rupture | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.3.2 Wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.4 Grip strength at 12 weeks (% lost using uninjured hand as comparison) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 10.4  Comparison 10: Low‐level laser therapy versus placebo control, Outcome 4: Grip strength at 12 weeks (% lost using uninjured hand as comparison) | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 11.1 Strength (kg) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 11.1  Comparison 11: Motor imagery versus control, Outcome 1: Strength (kg) | ||||
| 11.1.1 Grip strength (kg) at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1.2 Pinch strength (kg) at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
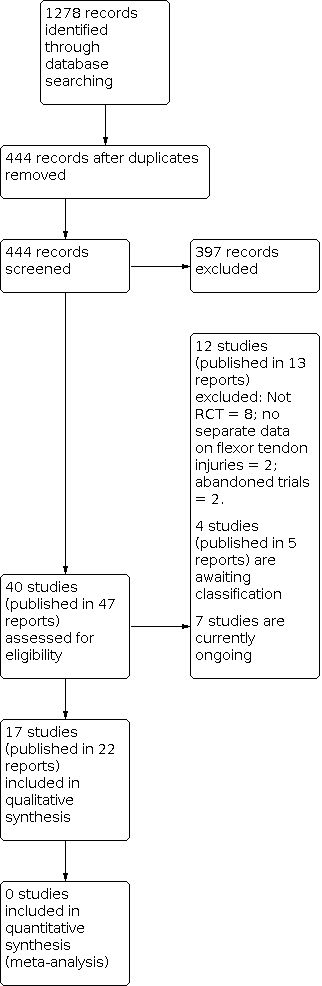
Diagram showing the flow of studies through the study selection process

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Self‐reported function for ADL using a VAS (0 to 10; higher = better) | ||||||
| Study | Follow‐up | Active Median (IQR) | Active N (digits) | Control Median; IQR | Control N (digits) | Reported P value |
|---|---|---|---|---|---|---|
| Rigo 2017 | At 2 months | 7.2 (3.0) | 36 | 6.5 (3.1) | 32 | P = 0.204 |
| At 3 months | 7.3 (3.6) | 36 | 7.7 (3.0) | 31 | P = 0.850 | |
| At 6 months | 8.8 (1.5) | 32 | 8.5 (3.5) | 30 | P = 0.942 | |
| At 12 months | 9.3 (1.2) | 34 | 8.8 (2.0) | 29 | P = 0.113 | |
Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 1: Self‐reported function for ADL using a VAS (0 to 10; higher = better)

Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 2: Self‐reported function using VAS for ADLs (0 to 10; higher scores = better); secondary analyses

Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 3: Active finger range of motion (degrees)

Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 4: Finger range of movement ‐ Poor outcome

Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 5: Adverse events

Comparison 1: Early active flexion plus controlled passive exercise regimen versus early controlled passive exercise regimen (modified Kleinert protocol), Outcome 6: Strength (% of the contralateral hand or digit)

Comparison 2: Early active flexion + active extension exercise regimen (+ modified Kessler suture surgical technique) versus passive flexion + active extension exercise regimen (+ grasping suture and external pull‐out knot surgical technique), Outcome 1: Adverse events

Comparison 3: Active exercise regimen versus immobilisation regimen, Outcome 1: Range of movement at 12+ months: poor outcome

Comparison 3: Active exercise regimen versus immobilisation regimen, Outcome 2: Adverse events

Comparison 4: Early place and hold progressed to tendon gliding exercise regimen versus early passive progressed to active exercise regimen, Outcome 1: Grip strength at 12 weeks (% difference between normal and affected hands)

Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 1: Function (self‐reported): DASH scores (0 to 100; higher score = more disability)

Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 2: Range of movement (Total Active Movement) (degrees)

Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 3: Range of movement (Strickland Criteria) at 8 weeks: Poor outcome

Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 4: Adverse events

Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 5: Function (observed): Jebsen Taylor at 52 weeks (seconds)

Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 6: Function (observed): Purdue pegboard at 52 weeks (pegs)

Comparison 5: Place and hold exercise regimen versus Controlled passive exercise regimen, Outcome 7: Satisfaction with hand function (0 to 10: complete satisfaction) at 6 months

Comparison 6: Unrestricted activity at 8 weeks post‐surgery versus unrestricted activity at 10 weeks, Outcome 1: Adverse event (tendon rupture)

Comparison 7: Exoskeleton versus physiotherapy, Outcome 1: Function (self‐reported): DASH scores (0 to 100; higher score = more disability)

Comparison 7: Exoskeleton versus physiotherapy, Outcome 2: Active finger range of motion of PIP joint (degrees)

Comparison 7: Exoskeleton versus physiotherapy, Outcome 3: Active finger range of motion of DIP joint (degrees)

Comparison 7: Exoskeleton versus physiotherapy, Outcome 4: Active finger range of motion (Total Active Movement) (degrees)

Comparison 7: Exoskeleton versus physiotherapy, Outcome 5: Adverse events

Comparison 7: Exoskeleton versus physiotherapy, Outcome 6: Strength at 18 weeks

Comparison 8: Continuous passive motion device versus controlled passive progressed to active exercise regimen (Modified Kleinert), Outcome 1: Active finger range of motion (degrees)

Comparison 8: Continuous passive motion device versus controlled passive progressed to active exercise regimen (Modified Kleinert), Outcome 2: Range of movement at > 6 months (Strickland criteria) ‐ poor outcome

Comparison 8: Continuous passive motion device versus controlled passive progressed to active exercise regimen (Modified Kleinert), Outcome 3: Adverse event

Comparison 9: Ultrasound versus control, Outcome 1: Improvement in active range of movement (Difference between 3 and 12 weeks; Total Active Motion measured in degrees)

Comparison 9: Ultrasound versus control, Outcome 2: Active finger range of motion (Strickland classification) at 3 months ‐ Poor outcome

Comparison 9: Ultrasound versus control, Outcome 3: Adverse events

Comparison 10: Low‐level laser therapy versus placebo control, Outcome 1: Active finger range of motion (Total active motion (degrees)) at 12 weeks

Comparison 10: Low‐level laser therapy versus placebo control, Outcome 2: Range of movement at 12 weeks: poor outcome

Comparison 10: Low‐level laser therapy versus placebo control, Outcome 3: Adverse events

Comparison 10: Low‐level laser therapy versus placebo control, Outcome 4: Grip strength at 12 weeks (% lost using uninjured hand as comparison)

Comparison 11: Motor imagery versus control, Outcome 1: Strength (kg)
| Addition of active flexion exercises to controlled passive exercise regimen for rehabilitation following surgery for flexor tendon injuries of the hand | ||||||
| Patient or population: participants undergoing rehabilitation following surgery for flexor tendon injuries of the handa | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Early controlled passive exercise regimen (modified Kleinert protocol) | Early active flexion plus early controlled passive exercise regimen | |||||
| Functional assessment using a patient reported outcome measure: Follow‐up: 6 months | Study population | ‐ | 62 fingers (1 RCT) | ⊕⊝⊝⊝ | The study reporting this outcome reported median and interquartile ranges. It found no evidence of a difference between the two groups (reported P = 0.942). It is very unlikely that a difference of 0.3 on an 11 point scale is clinically important. | |
| See comment. Median 8.5, IQR 3.5 | See comment. | |||||
| Functional assessment using a patient reported outcome measure: Follow‐up: 12 months | Study population | ‐ | 63 fingers | ⊕⊝⊝⊝ | The study reporting this outcome reported median and interquartile ranges. It found no evidence of a difference between the two groups (reported P = 0.113). It is very unlikely that a difference of 0.5 on an 11 point scale is clinically important | |
| See comment. Median 8.8, IQR 2.9 | See comment. | |||||
| Active finger range of motion | Study population | ‐ | 63 fingers | ⊕⊝⊝⊝ | This difference is not meaningful and could have been due to error in measurement: for goniometric measurement, the minimal detectable difference is between 12 and 30 degrees with a standard error of measurement ranging from 4 to 11 degrees per joint (Reissner 2019). | |
| Mean AROM in the control group was 134 degrees | MD 3 degrees higher | |||||
| Active finger range of motion | Study population | ‐ | 63 fingers | ⊕⊝⊝⊝ | This difference is not meaningful and could have been due to error in measurement: for goniometric measurement, the minimal detectable difference is between 12 and 30 degrees with a standard error of measurement ranging from 4 to 11 degrees per joint (Reissner 2019). | |
| Mean AROM in the control group was 140 degrees | MD 9 degrees higher | |||||
| Adverse events: participants incurring one or more adverse events Follow‐up: 12 months | Study population | RR 0.58 (0.23 to 1.44) | 69 fingers (1 RCT) | ⊕⊝⊝⊝ | The 15 adverse events comprised 3 tendon ruptures, 6 wound dehiscence, 1 complex regional pain syndrome and 5 transitory swelling and tenderness of the tendon sheaf. | |
| 282 per 1000 | 164 per 1000 (65 lower to 406 higher) | |||||
| Adverse event (tendon rupture) | Study population | RR 1.73 | 69 fingers | ⊕⊝⊝⊝ | All three tendon ruptures (4.3%) underwent secondary surgery. | |
| 31 per 1000 | 54 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aThe majority (68%) were zone II flexor tendon repairs; the rest being zone I and III. dDowngraded one level due to serious indirectness reflecting the reflecting the uncertain nature of the outcome. eDowngraded two levels due to very serious imprecision reflecting the small number of events. | ||||||
| Active exercise regimen compared with an immobilisation regimen following surgery for flexor tendon injuries of the hand | ||||||
| Patient or population: participants undergoing rehabilitation following surgery for flexor tendon injuries of the handa | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Immobilisation regimen for three weeks | Active exercise regimen commenced within one day post‐surgery | |||||
| Functional assessment using a patient reported outcome measure | See comment. | See comment. | Not estimable | ‐ | See comment. | Outcome was not reported |
| Functional assessment using a patient reported outcome measure | See comment. | See comment. | Not estimable | ‐ | See comment. | Outcome was not reported |
| Range of movement | See comment. | See comment. | Not estimable | ‐ | See comment. | Outcome was not reported |
| Range of movement | Study population | RR 0.08 | 84 | ⊕⊝⊝⊝ | Poor outcome is < 25% of normal. The 7 (15%) cases of poor range of finger movement were all in the immobilisation group | |
| 149 per 1000 | 12 per 1000 | |||||
| Adverse events: participants incurring one or more adverse events | See comment. | See comment. | Not estimable | 84 | See comment | Outcome was not reported. Only tendon rupture and indication for tenolysis data provided; see below. |
| Adverse events requiring (or indicated for) surgery | Study population | RR 0.64 | 84 | ⊕⊝⊝⊝ | All five cases of tendon rupture (13.5% of 37) needing surgical repair occurred after 2 weeks in the active mobilisation group and all 10 cases of range of motion deficiency (21.3% of 47) indicating scar adhesion and need for tenolysis occurred in the immobilisation group. | |
| 213 per 1000 | 137 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group (in this table, this is directly based on the study population) and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aAll were zone II flexor tendon repairs. bDowngraded two levels for very serious risk of bias reflecting detection bias (no blinding of outcome assessors), potential selection bias and attrition bias. cDowngraded one level for serious indirectness reflecting the unsatisfactory nature of the outcome. dDowngraded one level because of low number of events and wide confidence intervals for this outcome. eThese complications reflect the anticipated complications of early active mobilisation (early re‐rupture) and immobilisation (scar adhesions and contractures). It is uncertain whether tenolysis was actually done for those participants with range of motion deficit in the immobilisation group. | ||||||
| Place and hold exercise versus controlled passive exercise following surgery for flexor tendon injuries of the hand | ||||||
| Patient or population: participants undergoing rehabilitation following surgery for flexor tendon injuries of the handa | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Controlled passive exercise regimen | Place and hold exercise regimen | |||||
| Functional assessment using a patient reported outcome measure: assessed with DASH questionnaire (0 to 100; higher scores = worse disability) | Study population | Not estimable | 26 | ⊕⊝⊝⊝ | The study reporting this outcome reported median and interquartile ranges, finding no evidence of a difference between the two groups (reported P = 0.62). | |
| See comment. Median 15, IQR 10 to 30 | See comment. Median 23, IQR 2 to 26 | |||||
| Functional assessment using a patient reported outcome measure: | Study population | ‐ | 89 | ⊕⊝⊝⊝ | These differences are not clinically important. The recommended minimal clinically important difference for DASH is 15 (DASH/QuickDASH). | |
| Mean DASH score was 3.1 | Mean DASH score was 1.1 lower (2.77 lower to 0.57 higher) | |||||
| Range of movement | See comment. | See comment. | Not estimable | ‐ | See comment. | Outcome was not reported |
| Range of movement | Study population | ‐ | 89 (102 digits) | ⊕⊝⊝⊝ | ||
| Mean ROM was 128 degrees | Mean ROM was 28 degrees higher | |||||
| Adverse events: participants incurring one or more adverse events | See comment. | See comment. | Not estimable | 84 | See comment. | This outcome was not reported by the three trials testing this comparison. Only tendon rupture (see next) was commonly reported. One trial (26 participants), reporting by tendon or digit (36 digits), also reported on scar adherence (reported only in the controlled passive group), flexion contracture at the DIP and PIP joints and tendon lag; very low certainty evidence for all individual complications. |
| Adverse events requiring (or indicated for) surgery | Study populationsh | RR 0.81 | 196 tendons | ⊕⊝⊝⊝ | These data were limited to tendon rupture. We considered that all 7 tendon ruptures (3.6% of 196 tendons) would have required surgery.j | |
| 40 per 1000 | 33 per 1000 (8 to 140) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group (in this table, this is directly based on the study population) and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aThe majority were zone II flexor tendon repairs; one of the three studies making this comparison also included 7 zone I injuries and 7 zone III injuries. bAll exercises started at 3 days from surgery. The place and hold exercise regimens varied among the three studies. In two studies, the exercises were carried out with a dorsal orthosis and in one study, the dorsal orthosis was removal when doing the exercises cAll exercises started at 3 days from surgery. The controlled passive exercise regimens varied among the three studies. However, rubber band traction was common to all three. dDowngraded two levels for very serious risk of bias reflecting lack of blinding (performance and detection bias) eDowngraded one level for serious imprecision. fDowngraded one level for serious imprecision, also reflecting the potential 'ceiling' effect as the mean values were very low and thus cannot discriminate between the two groups. gDowngraded one level for serious imprecision as the data are presented for tendons not participants. hControl group risk was devised from the summed data from the three studies. These results were not available for participants rather than tendons. iDowngraded two levels for very serious imprecision reflecting a very low number of events and wide confidence interval for this outcome. jWe did not include the 14 cases of scar adherence (70% of 20 tendons) reported in the controlled passive group of one trial because the outcome was not defined and no details of the extent or consequences were provided. | ||||||
| Database | Period Searched | Date Searched | Number of hits |
|---|---|---|---|
| Cochrane Bone, Joint and Musculoskeletal Trials (BJMT) Specialised Register | 18 June 2019 | 18 June 2019 | 26 |
| CENTRAL | August 2020, Issue 8 | 11 August 2020 | 208 |
| MEDLINE | January 1946 to August 2020 | 10 August 2020 | 462 |
| Embase | January 1980 to June 2019 | 18 June 2019 | 227 |
| CINAHL PLUS | January 1937 to June 2019 | 18 June 2019 | 63 |
| AMED | January 1985 to August 2020 | 10 January 2017 | 75 |
| ClinicalTrials.gov | 11 August 2020 | 79 | |
| WHO International Clinical Trials Registry Platform (ICTRP) | 18 June 2019 | 138 |
| Study | Country | Setting | Recruited Participants; Digits; Tendons | Final follow‐up Participants; Digits; Tendons | Zones | Age (years) Mean (Range) | Male | Female |
|---|---|---|---|---|---|---|---|---|
| Egypt | Rehabilitation Department | 33; NR; 45 | 26; NR; 36 | I‐III | 26.8 (15‐60)a | 21a | 5a | |
| Sweden | NR | 96; 106; NR | 82; 91; 118 | II | 37a | 54a | 28a | |
| Iran | Hand therapy clinic | 54; 64; 108 | 54; 64; 108 | II | 28.5 (13‐50) | 37 | 17 | |
| India | Hospital | 106; 139; NR | 100; 131; NR | II | G1: NR (10‐45)a G2: 35 (22‐50)a | 89a | 11a | |
| USA | Multi‐centre hospital | 51; 60; 102b | 51; 60; 102 | II | 29.4a | NR | NR | |
| Germany | Physiotherapy clinic | 62; NR;NR | 59; NR; NR | II | 29.5 (18‐60) | 44 | 18 | |
| Sweden | NR | 100; 108; NR | NR; NR; NR | II | NR | NR | NR | |
| UK | Plastic surgery centre | 112; NR; NR | 80; NR; NR | I‐III | NR | NR | NR | |
| Turkey | Hand surgery centre | 25; 41; NR | 23; 39; NR | I‐V | 24 (7‐43) | 15 | 10 | |
| Iran | Plastic surgery centre | 97; 114; 114 | 77; 92; 92 | I‐III | 27a | 60a | 17a | |
| Norway | Orthopaedic surgery centre | 53; 73; 73 | 45; 63; 63 | I‐III | 38.7 (18‐72)c | 36c | 14c | |
| Denmark | Hand surgery centre | 39; 39; 39 | 33; 33; 33 | I‐II | NR | NR | NR | |
| Brazil | Hand surgery centre | 84; NR; 152 | NR; NR; NR | II | 34 (18‐66) | NR | NR | |
| Netherlands | Plastic surgery centre | 28; NR; NR | 25; NR; NR | All | 33.5a | 18a | 7a | |
| USA | Multi‐centre hand surgery centre | 103; 119; 238 | 89; 102; 204 | II | 29 (15‐51)a | 63a | 30a | |
| India | Plastic surgery centre | 30; NR; NR | 30; NR; NR | V | NR | NR | NR | |
| France | NR | 35; NR; NR | NR; NR NR | II | 35 | NR | NR | |
| NR: Not reported; G1: Group 1; G2: Group 2 aOnly reported at follow‐up (not at baseline) bParticipants were only eligible if they were available for the 6 month follow‐up. Thus, this number is likely to have been much higher than reported here. cExcludes 3 participants who experienced tendon ruptures after randomisation. | ||||||||
| Study ID | Function: patient‐reported | Active ROM | Adverse event | Passive ROM | Strength | Return to work | Function: objective measure | Quality of life | Satisfaction |
|---|---|---|---|---|---|---|---|---|---|
| X | X | X | X | ||||||
| X | X | X | X | X | |||||
| X | X | ||||||||
| X | X | X | |||||||
| X | X | ||||||||
| X | X | X | X | X | |||||
| X | X | ||||||||
| X | X | ||||||||
| X | X | X | |||||||
| X | X | X | |||||||
| X | X | X | X | ||||||
| X | X | X | |||||||
| X | X | ||||||||
| X | X | X | |||||||
| X | X | X | X | X | X | ||||
| X | X | X | |||||||
| X | X | X |
| Classification system | Outcome (% motion achieved) | Excellent | Good | Fair or satisfactory | Poor | Failure |
| Strickland‐Glogovac | % active PIP + DIP ROM (active flexion ‐ extension deficit) compared to contralateral side or 175 degrees* | 85% to 100% | 70% to 84% | 50% to 69% | 0% to 49% | Not applicable |
| ROM (in degrees) | > 150 | 125 to 149 | 90 to 124 | < 90 | Not applicable | |
| Strickland or Modified Strickland | % active PIP + DIP ROM (active flexion ‐ extension deficit) compared to contralateral side or 175 degrees* | 75% to 100% | 50% to 74% | 24% to 49% | 0% to 24% | Not applicable |
| ROM (in degrees) | > 132 | 88 to 131 | 45 to 87 | < 44 | Not applicable | |
| Tang*** | % active PIP + DIP ROM compared to contralateral side or 175 degrees* | 90% to 100% | 70% to 89% | 50% to 69% | 30% to 49% | < 30% |
| IFSSH | % Total active motion compared to total passive motion** | 75% to 100% | 50% to 74% | 24% to 49% | 0% to 24% | Not applicable |
| Total Active Motion | % active MCP + PIP + DIP ROM (active flexion ‐ extension deficit) compared to contralateral side | Normal | > 75% | 50% to 75% | < 50% | < pre‐surgery |
| DIP: distal interphalangeal; IFFSH: International Federation of Societies for Surgery of the Hand; MCP: metacarpophalangeal; ROM: range of movement; PIP: proximal interphalangeal *The sum of active ROM of the PIP and DIP joints is calculated in degrees. This is done by adding the flexion achieved at the PIP and DIP joints and subtracting any extension deficits from the total. Motion is reported as a % of the contralateral side. It is assumed that 175 degrees is the sum of motion of the normal PIP and DIP joints of the unaffected side. % motion achieved = ((PIP + DIP flexion) ‐ (PIP + DIP extension deficit)) X 100 divided by 175. ** % motion achieved = (Total active motion X 100) divided by Total passive motion. ***According to Tang, the excellent and good scores are further divided into plus and minus sub‐grades based on their grip strength and quality of motion (investigator’s subjective judgement of the coordination, visual arc and speed of motion). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Self‐reported function for ADL using a VAS (0 to 10; higher = better) Show forest plot | 1 | Other data | No numeric data | |
| 1.2 Self‐reported function using VAS for ADLs (0 to 10; higher scores = better); secondary analyses Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.1 ADL VAS at 2 months (0=worst; 10=best) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.2 ADL VAS at 3 months (0=worst; 10=best) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.3 ADL VAS at 6 months (0=worst; 10=best) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.2.4 ADL VAS at 12 months (0=worst; 10=best) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3 Active finger range of motion (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3.1 Total Active Movement at 1 month (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3.2 Total Active Movement at 2 months (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3.3 Total Active Movement at 3 months (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3.4 Total Active Movement at 6 months (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.3.5 Total Active Movement at 12 months (degrees) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.4 Finger range of movement ‐ Poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.1 Strickland classification at 1 month | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.2 Strickland classification at 2 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.3 Strickland classification at 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.4 Strickland classification at 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.5 Strickland classification at 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.6 Tang classification at 1 month | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.7 Tang classification at 2 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.8 Tang classification at 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.9 Tang classification at 6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.4.10 Tang classification at 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.5 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.5.1 Tendon rupture | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.5.2 Complex Regional Pain Syndrome | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.5.3 Wound dehiscence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.5.4 Transitory swelling + tenderness | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.5.5 Any adverse event | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.6 Strength (% of the contralateral hand or digit) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.6.1 Grip Strength at 3 months (% of the contralateral hand) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.6.2 Grip Strength at 6 months (% of the contralateral hand) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.6.3 Grip Strength at 12 months (% of the contralateral hand) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.6.4 Pinch Strength at 3 months (% of the contralateral digit) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.6.5 Pinch Strength at 6 months (% of the contralateral digit) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.6.6 Pinch Strength at 12 months (% of the contralateral digit) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1.1 Tendon ruptures | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1.2 Scar adhesions requiring surgery (Tenolysis) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Range of movement at 12+ months: poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1.1 IFSSH criteria | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1.2 Strickland criteria | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.2.1 Tendon ruptures | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.2.2 Movement restrictions indicating need for tenolysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.2.3 Secondary surgery (actual or indicated) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Grip strength at 12 weeks (% difference between normal and affected hands) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 5.1 Function (self‐reported): DASH scores (0 to 100; higher score = more disability) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1.1 DASH at 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1.2 DASH at 52 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.2 Range of movement (Total Active Movement) (degrees) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.2.1 At 8 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.2.2 At 52 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.3 Range of movement (Strickland Criteria) at 8 weeks: Poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.4 Adverse events Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.4.1 Tendon rupture | 3 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.19, 3.50] |
| 5.4.2 Scar adherence | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.04 [0.00, 0.66] |
| 5.4.3 Flexion contracture of the DIP joint | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.02, 0.88] |
| 5.4.4 Flexion contracture of the PIP joint | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.15, 1.48] |
| 5.4.5 FDS tendon lag | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.06, 0.98] |
| 5.4.6 FDP tendon lag | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.04, 0.62] |
| 5.5 Function (observed): Jebsen Taylor at 52 weeks (seconds) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.6 Function (observed): Purdue pegboard at 52 weeks (pegs) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.7 Satisfaction with hand function (0 to 10: complete satisfaction) at 6 months Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 6.1 Adverse event (tendon rupture) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 7.1 Function (self‐reported): DASH scores (0 to 100; higher score = more disability) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1.1 DASH at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1.2 DASH at 18 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2 Active finger range of motion of PIP joint (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2.1 PIP joint range of motion at 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2.2 PIP joint range of motion at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.2.3 PIP joint range of motion at 18 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.3 Active finger range of motion of DIP joint (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.3.1 DIP joint range of motion at 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.3.2 DIP joint range of motion at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.3.3 DIP joint range of motion at 18 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.4 Active finger range of motion (Total Active Movement) (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.4.1 TAM at 6 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.4.2 TAM at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.4.3 TAM at 18 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.5 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.5.1 Tendon rupture | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.5.2 CRPS (complex regional pain syndrome) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.6 Strength at 18 weeks Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.6.1 Grip strength (kg) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.6.2 Pinch strength (kg) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 8.1 Active finger range of motion (degrees) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1.1 TAM at > 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.2 Range of movement at > 6 months (Strickland criteria) ‐ poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.3 Adverse event Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.3.1 Tendon rupture at >6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.3.2 Infection at >6 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 9.1 Improvement in active range of movement (Difference between 3 and 12 weeks; Total Active Motion measured in degrees) Show forest plot | 1 | 131 | Mean Difference (IV, Fixed, 95% CI) | 26.47 [19.70, 33.24] |
| 9.1.1 1MHz; 0.7W/cm2 increased to 1w/cm2 | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 31.50 [19.94, 43.06] |
| 9.1.2 1 MHz; 0.3w/cm2 increased to 1.0w/cm2 | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 23.80 [11.89, 35.71] |
| 9.1.3 3Mhz; 0.5w/cm2 increased to 0.7w/cm2 | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 23.90 [12.20, 35.60] |
| 9.2 Active finger range of motion (Strickland classification) at 3 months ‐ Poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.3.1 Tendon rupture at 3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.3.2 Wound dehiscence <3 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 10.1 Active finger range of motion (Total active motion (degrees)) at 12 weeks Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.2 Range of movement at 12 weeks: poor outcome Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.2.1 Strickland scoring system at 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.3 Adverse events Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.3.1 Tendon rupture | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.3.2 Wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.4 Grip strength at 12 weeks (% lost using uninjured hand as comparison) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 11.1 Strength (kg) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1.1 Grip strength (kg) at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1.2 Pinch strength (kg) at 12 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |

