Profilaxis con antibióticos para la reparación de la episiotomía después del parto vaginal
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Quasi‐randomised controlled trial | |
| Participants | 80 women with normal labour and episiotomy in 1 public hospital, recruited between October 1988 and September 1989. | |
| Interventions | Intervention arm received oral chloramphenicol 500 mg 4 times daily for 72 hours after episiotomy repair. Control arm received no treatment. | |
| Outcomes | A total of 73 women included in analysis, 34 in intervention arm and 39 in control arm. Outcomes measured included episiotomy dehiscence (wound rupture without signs of infection), episiotomy infection (pain, heat, redness, or purulent discharge and wound rupture), and puerperal endometritis assessed at 10 days postpartum (defined as 2 of the following; fever, hypogastric pain, uterine involution, abnormal lochia). | |
| Notes | Florianopolis, Brazil. Exclusion of 7 women lost to follow‐up at 10 days postpartum. All women were from low socioeconomic class. All women attended by registrars. Funding: not reported. Conflicts of interest: not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomised according to protocol number (even and odd numbers) |
| Allocation concealment (selection bias) | High risk | Allocation concealment based on protocol number |
| Blinding of participants and personnel (performance bias) | High risk | Not double‐blinded. Control arm received no treatment |
| Blinding of outcome assessment (detection bias) | Unclear risk | Unknown. No information on whether physicians who evaluated the women at 10 days postpartum were blinded to the treatment allocation. |
| Incomplete outcome data (attrition bias) | High risk | 6 women in intervention group and 1 in control group were missing for follow‐up, but no differences reported in baseline characteristics among those followed‐up. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other sources of bias noted. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Episiotomy infection with wound dehiscence Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.28] |
| Analysis 1.1  Comparison 1 Comparison 1. Antibiotic prophylaxis versus no treatment, Outcome 1 Episiotomy infection with wound dehiscence. | ||||
| 2 Episiotomy wound dehiscence without infection Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.29, 2.34] |
| Analysis 1.2  Comparison 1 Comparison 1. Antibiotic prophylaxis versus no treatment, Outcome 2 Episiotomy wound dehiscence without infection. | ||||
| 3 Episiotomy wound dehiscence (overall with or without infection) Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.20, 1.35] |
| Analysis 1.3  Comparison 1 Comparison 1. Antibiotic prophylaxis versus no treatment, Outcome 3 Episiotomy wound dehiscence (overall with or without infection). | ||||
| 4 Incidence of puerperal infection (endometritis) Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 1.4 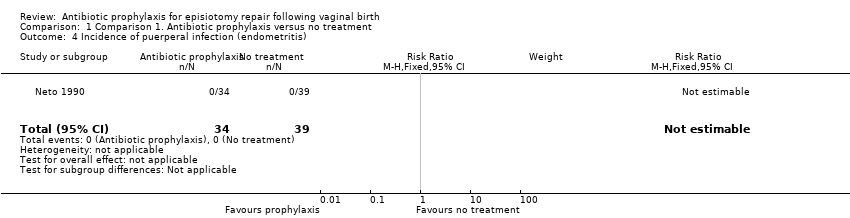 Comparison 1 Comparison 1. Antibiotic prophylaxis versus no treatment, Outcome 4 Incidence of puerperal infection (endometritis). | ||||

Study flow diagram
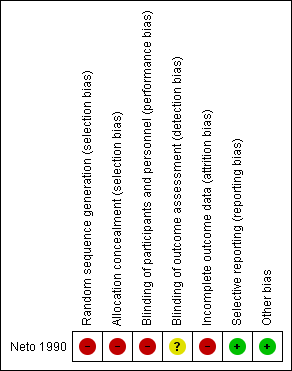
Risk of bias summary: review authors' judgements about each 'risk of bias' domain

Comparison 1 Comparison 1. Antibiotic prophylaxis versus no treatment, Outcome 1 Episiotomy infection with wound dehiscence.

Comparison 1 Comparison 1. Antibiotic prophylaxis versus no treatment, Outcome 2 Episiotomy wound dehiscence without infection.
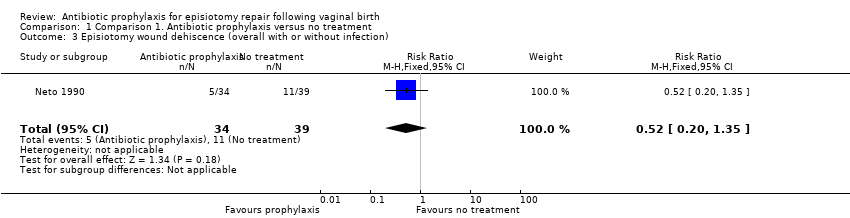
Comparison 1 Comparison 1. Antibiotic prophylaxis versus no treatment, Outcome 3 Episiotomy wound dehiscence (overall with or without infection).

Comparison 1 Comparison 1. Antibiotic prophylaxis versus no treatment, Outcome 4 Incidence of puerperal infection (endometritis).
| Antibiotic prophylaxis compared to no treatment for episiotomy repair following vaginal birth | ||||||
| Patient or population: women with episiotomy repair following vaginal birth Settings: public hospital, Brazil Intervention: antibiotic prophylaxis with oral chloramphenicol 500 mg four times daily for 72 hours after episiotomy repair Comparison: no treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Risk with no treatment | Risk with antibiotic prophylaxis | |||||
| Incidence of episiotomy wound infection with wound dehiscence | Study population | RR 0.13 | 73 | ⊕⊝⊝⊝ | ||
| 103 per 1000 | 14 per 1000 | |||||
| Incidence of episiotomy wound dehiscence without wound infection | Study population | RR 0.82 | 73 | ⊕⊝⊝⊝ | ||
| 179 per 1000 | 151 per 1000 | |||||
| Incidence of puerperal infection (endometritis) | Study population | not estimable | 73 | ⊕⊝⊝⊝ | There were no events in either group. | |
| 0 per 1000 | 0 per 1000 | |||||
| Incidence of severe maternal infectious morbidity | Study population | ‐ | 0 | ‐ | trial did not measure this outcome | |
| ‐ | ‐ | |||||
| Discomfort or pain at episiotomy wound site | ‐ | ‐ | ‐ | 0 | ‐ | trial did not measure this outcome |
| Women's satisfaction with care | ‐ | ‐ | ‐ | 0 | ‐ | trial did not measure this outcome |
| Adverse effects of antibiotics | Study population | ‐ | 0 | ‐ | trial did not measure this outcome | |
| ‐ | ‐ | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 One study with very serious design limitations (‐2) | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Episiotomy infection with wound dehiscence Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.28] |
| 2 Episiotomy wound dehiscence without infection Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.29, 2.34] |
| 3 Episiotomy wound dehiscence (overall with or without infection) Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.20, 1.35] |
| 4 Incidence of puerperal infection (endometritis) Show forest plot | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

