Malla o injertos transvaginales comparados con reparación con tejido autólogo para el prolapso vaginal
Información
- DOI:
- https://doi.org/10.1002/14651858.CD012079Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 09 febrero 2016see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Ginecología y fertilidad
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
All review authors contributed to writing the protocol. Four review authors (C Maher, C Schmid, B Feiner, K Baessler) assessed the relevance and eligibility of studies for inclusion in the review and then assessed the quality of included studies. Four review authors (C Maher, C Schmid, K Baessler, B Feiner) independently extracted data from trial reports, interpreted the results, and contributed to the writing of the draft version of the review.
Sources of support
Internal sources
-
Cochrane, UK.
Cochrane Review Support Programme: Pelvic organ prolapse reviews
External sources
-
National Institute for Health Research (NIHR), UK.
This project was supported by the NIHR, via Cochrane Infrastructure funding to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, the NIHR, the NHS or the Department of Health.
Declarations of interest
The lead review author, Christopher Maher, is an author of two trials of pelvic prolapse (Maher 2004a; Maher 2011)
The other review authors declare that they have no conflicts of interest.
Acknowledgements
We acknowledge the work of Elisabeth J Adams and Suzanne Hagen as coauthors on the original review, and Charis Glazener as coauthor on the original review and update. The authors of the 2016 update would like to thank Sheila Wallace, Information Specialist of the Cochrane Incontinence Review Group, for designing the search strategy and running the searches for this review. We are also grateful for the assistance of Helen Nagels and Cindy Farquhar of the Cochrane Gynaecology and Fertility Group in the preparation of this new review.
Version history
| Published | Title | Stage | Authors | Version |
| 2024 Mar 13 | Transvaginal mesh or grafts or native tissue repair for vaginal prolapse | Review | Ellen Yeung, Kaven Baessler, Corina Christmann-Schmid, Nir Haya, Zhuoran Chen, Sheila A Wallace, Alex Mowat, Christopher Maher | |
| 2016 Feb 09 | Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse | Review | Christopher Maher, Benjamin Feiner, Kaven Baessler, Corina Christmann‐Schmid, Nir Haya, Jane Marjoribanks | |
Differences between protocol and review
This review is the result of updating the review 'Surgical management of pelvic organ prolapse in women'. As a result of the update, we decided to split the review into six reviews.
This review should be read as part of a series of six Cochrane reviews relating to the surgical management of prolapse including:
-
Surgery for women with anterior compartment prolapse.
-
Surgery for women with posterior compartment prolapse.
-
Surgery for women with apical compartment prolapse.
-
Continence outcomes in pelvic organ prolapse surgery.
-
Transvaginal grafts or mesh compared with native tissue repair for vaginal prolapse.
-
Perioperative interventions at prolapse surgery.
Differences from the published review methods were a reduction in the number of outcomes and limiting this review to studies that compared native tissue with mesh (absorbable and permanent) and biological grafts.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Surgical Mesh;
- Absorbable Implants;
- Awareness;
- Randomized Controlled Trials as Topic;
- Recurrence;
- Reoperation [statistics & numerical data];
- Secondary Prevention [statistics & numerical data];
- Urinary Incontinence, Stress [surgery];
- Uterine Prolapse [prevention & control, psychology, *surgery];
- Vagina [*surgery];
Medical Subject Headings Check Words
Female; Humans;
PICO

PRISMA study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Forest plot of comparison: 1 Any transvaginal permanent mesh versus native tissue repair, outcome: 1.1 Awareness of prolapse (1 to 3 years).

Forest plot of comparison: 3 Biological repair versus native tissue repair, outcome: 3.1 Awareness of prolapse (1 to 3 years).

Funnel plot of comparison: 1 Any transvaginal permanent mesh versus native tissue repair, outcome: 1.3 Recurrent prolapse (any) at 1 to 3 years.

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 1 Awareness of prolapse (1‐3 years).

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 2 Repeat surgery (1‐3 years).

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 3 Recurrent prolapse (any) at 1‐3 years.

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 4 Injuries bladder or bowel.

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 5 Objective failure of anterior compartment (cystocoele).

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 6 Objective failure of posterior compartment (rectocoele).

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 7 POPQ assessment (any mesh).

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 8 Bladder function: de novo stress urinary incontinence (1‐3 years).
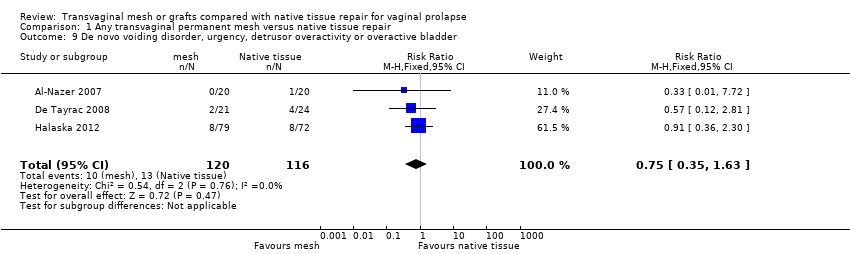
Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 9 De novo voiding disorder, urgency, detrusor overactivity or overactive bladder.

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 10 De novo dyspareunia (1‐3 years).

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 11 Sexual function (1‐3 years).

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 12 Quality of life: continuous data (1‐2 years):.

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 13 Quality of life: dichotomous data "much or very much better".

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 14 Operating time (minutes).

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 15 Blood transfusion.

Comparison 1 Any transvaginal permanent mesh versus native tissue repair, Outcome 16 Length of stay in hospital (days).

Comparison 2 Absorbable mesh versus native tissue repair, Outcome 1 Awareness of prolapse (2 year review).

Comparison 2 Absorbable mesh versus native tissue repair, Outcome 2 Repeat surgery for prolapse (2 years).
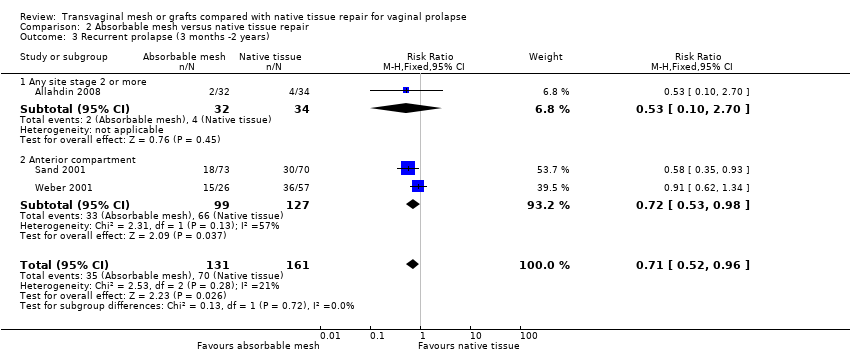
Comparison 2 Absorbable mesh versus native tissue repair, Outcome 3 Recurrent prolapse (3 months ‐2 years).

Comparison 2 Absorbable mesh versus native tissue repair, Outcome 4 Death.

Comparison 2 Absorbable mesh versus native tissue repair, Outcome 5 Objective failure of anterior compartment (cystocoele).

Comparison 2 Absorbable mesh versus native tissue repair, Outcome 6 Objective failure of posterior compartment (rectocoele).
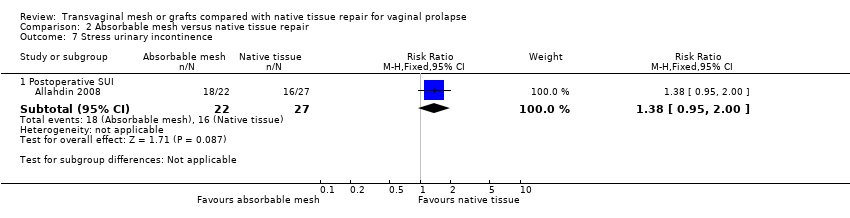
Comparison 2 Absorbable mesh versus native tissue repair, Outcome 7 Stress urinary incontinence.

Comparison 2 Absorbable mesh versus native tissue repair, Outcome 8 Quality of life (2 years).

Comparison 3 Biological repair versus native tissue repair, Outcome 1 Awareness of prolapse (1‐3 year).
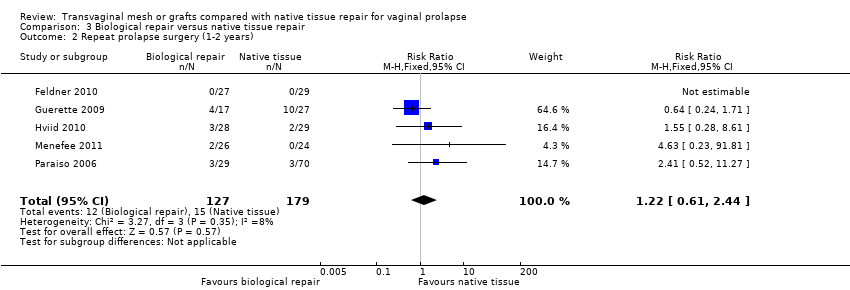
Comparison 3 Biological repair versus native tissue repair, Outcome 2 Repeat prolapse surgery (1‐2 years).

Comparison 3 Biological repair versus native tissue repair, Outcome 3 Recurrent prolapse (1 year).

Comparison 3 Biological repair versus native tissue repair, Outcome 4 Injuries to bladder or bowel.

Comparison 3 Biological repair versus native tissue repair, Outcome 5 Objective failure of anterior compartment (cystocele).

Comparison 3 Biological repair versus native tissue repair, Outcome 6 Objective failure of posterior compartment (rectocele).

Comparison 3 Biological repair versus native tissue repair, Outcome 7 POPQ assessment.

Comparison 3 Biological repair versus native tissue repair, Outcome 8 De novo urinary stress incontinence.

Comparison 3 Biological repair versus native tissue repair, Outcome 9 De novo voiding disorders, urgency, detrusor overactivity or overactive bladder.

Comparison 3 Biological repair versus native tissue repair, Outcome 10 De novo dyspareunia (1 year).

Comparison 3 Biological repair versus native tissue repair, Outcome 11 Sexual function (1 year).

Comparison 3 Biological repair versus native tissue repair, Outcome 12 Quality of life (1 year).

Comparison 3 Biological repair versus native tissue repair, Outcome 13 Operating time (minutes).

Comparison 3 Biological repair versus native tissue repair, Outcome 14 Blood transfusion.
| Any transvaginal permanent mesh versus native tissue repair for vaginal prolapse | ||||||
| Population: women with vaginal prolapse | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Native tissue repair | Any transvaginal permanent mesh | |||||
| Awareness of prolapse review 1 to 3 years | 188 per 1000 | 124 per 1000 | RR 0.66 (0.54 to 0.81) | 1614 (12 RCTs) | ⊕⊕⊕⊝ | |
| Repeat surgery ‐ prolapse review 1 to 3 years | 32 per 1000 | 17 per 1000 | RR 0.53 | 1675 | ⊕⊕⊕⊝ | |
| Repeat surgery ‐ continence surgery | 26 per 1000 | 28 per 1000 (16 to 48) | RR 1.07 (0.62 to 1.83) | 1284 (9 RCTs) | ⊕⊕⊝⊝ | |
| Repeat surgery ‐ surgery for prolapse, SUI, or mesh exposure review 1 to 3 years | 48 per 1000 | 114 per 1000 | RR 2.40 | 867 | ⊕⊕⊕⊝ | |
| Recurrent prolapse review 1 to 3 years | 381 per 1000 | 152 per 1000 | RR 0.40 | 2494 | ⊕⊕⊝⊝ | I2 = 73% |
| Bladder injury | 5 per 1000 | 21 per 1000 | RR 3.92 | 1514 | ⊕⊕⊕⊝ | |
| De novo dyspareunia (pain during sexual intercourse) review 1 to 3 years | 95 per 1000 | 88 per 1000 | RR 0.92 | 764 | ⊕⊕⊝⊝ | |
| De novo stress urinary incontinence review 1 to 3 years | 96 per 1000 | 133 per 1000 | RR 1.39 | 1512 | ⊕⊕⊝⊝ | |
| Quality of life review 1 to 2 years | The mean quality of life in the mesh groups was 0.05 standard deviations higher (0.20 lower to 0.30 higher). This is an imprecise finding that is consistent with a small benefit in either group, or else no difference between the groups | 665 (7 studies) | ⊕⊝⊝⊝ very low1, 2,4 | I2 = 60% | ||
| *The basis for the assumed risk is the median control group risk across studies The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level due to serious risk of bias: most of the studies were at unclear or high risk of bias associated with poor reporting of methods, including failure by many to describe satisfactory methods of allocation concealment or blinding. A minority of studies did not report use of blinding at all. 2Downgraded one level due to serious imprecision: findings compatible with benefit in either group or with no clinically meaningful difference between the groups. 3Downgraded one level due to serious imprecision: findings compatible with benefit in native tissue group or with no clinically meaningful difference between the groups. 4Downgraded one level due to serious inconsistency: substantial statistical heterogeneity. | ||||||
| Absorbable mesh versus native tissue repair for vaginal prolapse | ||||||
| Population: women with vaginal prolapse Control: native tissue repair | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Native tissue repair | Absorbable mesh | |||||
| Awareness of prolapse at 2 years | 724 per 1000 | 760 per 1000 | RR 1.05 | 54 | ⊕⊝⊝⊝ | |
| Repeat surgery for prolapse (stage 2 or more) at 2 years | 125 per 1000 | 59 per 1000 | RR 0.47 | 66 | ⊕⊝⊝⊝ | |
| Recurrent prolapse at 3 months to 2 years | 429 per 1000 | 304 per 1000 | RR 0.71 | 292 | ⊕⊕⊝⊝ | |
| Bladder injury | Not reported in the included studies | |||||
| De novo dyspareunia (pain during sexual intercourse) review 1 to 3 years | Not reported in the included studies | |||||
| Stress urinary incontinence at 2 years | 593 per 1000 | 818 per 1000 | RR 1.38 | 49 | ⊕⊝⊝⊝ | |
| Quality of life at 2 years | The mean quality of life score was the same in both groups, when measured using a severity score of 1 to 10 (mean difference 0, 95% CI ‐2.82 to 2.82) | 54 | ⊕⊝⊝⊝ | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level due to serious risk of attrition bias: at two years 18% not included in analysis. | ||||||
| Biological repair versus native tissue repair for vaginal prolapse | ||||||
| Population: women with vaginal prolapse Control: native tissue repair | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Native tissue repair | Biological repair | |||||
| Awareness of prolapse at 1 to 3 years | 105 per 1000 | 102 per 1000 | RR 0.97 | 777 | ⊕⊕⊝⊝ | |
| Repeat prolapse surgery 1 to 2 years | 43 per 1000 | 52 per 1000 | RR 1.22 | 306 | ⊕⊕⊝⊝ | |
| Recurrent prolapse at 1 year | 295 per 1000 | 277 per 1000 | RR 0.94 | 587 | ⊕⊝⊝⊝ | |
| Bladder injury | Not estimable as only 1 event occurred (in the native tissue group) | 137 (1 study) | ||||
| Bowel injury | Not estimable as only 1 event occurred (in the biological repair group) | 137 (1 study) | ||||
| De novo dyspareunia (pain during sexual intercourse) review 1 to 3 years | 177 per 1000 | 150 per 1000 | RR 0.85 | 37 | ⊕⊝⊝⊝ | |
| De novo urinary stress incontinence at 1 year | Not estimable ‐ no events occurred | 56 | ||||
| Quality of life at 1 year | The mean quality of life in the biological repair group was 0.05 standard deviations lower (0.48 lower to 0.38 higher). This is an imprecise finding that is consistent with a small benefit in either group, or else no difference between the groups | 84 | ⊕⊝⊝⊝ | |||
| *The basis for the assumed risk is the median control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level due to serious risk of bias: four of the studies at high or unclear risk of bias associated with blinding status. 7Downgraded one level due to serious risk of bias: blinding status unclear. 8Downgraded two levels due to very serious imprecision: single small study, only six events. 9Downgraded one level due to serious risk of attrition bias, and a further two levels due to very serious imprecision: only 84 participants. | ||||||
| Study ID | Repair events | Repair total | Exposure events | Exposure total |
| Ali 2006 abstract | 0 | 43 | 3 | 46 |
| 0 | 23 | 1 | 21 | |
| 0 | 182 | 21 | 183 | |
| 0 | 60 | 5 | 62 | |
| 0 | 81 | 18 | 88 | |
| 0 | 39 | 2 | 40 | |
| 0 | 54 | 4 | 44 | |
| 0 | 72 | 16 | 79 | |
| 0 | 33 | 5 | 32 | |
| 0 | 35 | 2 | 33 | |
| 0 | 24 | 2 | 28 | |
| 0 | 38 | 2 | 37 | |
| 0 | 96 | 18 | 104 | |
| Qatawneh 2013 | 0 | 63 | 4 | 53 |
| 0 | 42 | 3 | 43 | |
| Thijs 2010 abstract | 0 | 48 | 9 | 48 |
| 0 | 20 | 3 | 20 | |
| 0 | 51 | 2 | 53 | |
| 0 | 84 | 14 | 83 | |
| Total | 134 | 1097 |
| Study ID | Repair events | Repair total | Exposure events | Exposure total |
| Ali 2006 abstract | 0 | 43 | 3 | 46 |
| 0 | 23 | 1 | 21 | |
| 0 | 182 | 21 | 183 | |
| 0 | 39 | 2 | 40 | |
| 0 | 54 | 4 | 44 | |
| 0 | 35 | 2 | 33 | |
| 0 | 24 | 2 | 28 | |
| 0 | 38 | 2 | 37 | |
| 0 | 96 | 18 | 104 | |
| Qatawneh 2013 | 0 | 63 | 4 | 53 |
| 0 | 42 | 3 | 43 | |
| Thijs 2010 abstract | 0 | 48 | 9 | 48 |
| 0 | 20 | 3 | 20 | |
| 0 | 51 | 2 | 53 | |
| Total | 76 | 753 |
| Study ID | Repair events | Repair total | Exposure events | Exposure total |
| 0 | 60 | 5 | 62 | |
| 0 | 81 | 18 | 88 | |
| 0 | 72 | 16 | 79 | |
| 0 | 33 | 5 | 32 | |
| 0 | 84 | 14 | 83 | |
| Total | 58 | 344 |
| Study ID | Surgery for mesh exposure | Total number of women in mesh group |
| 6 | 186 | |
| 3 | 62 | |
| 7 | 88 | |
| 4 | 66 | |
| 2 | 40 | |
| 2 | 44 | |
| 10 | 79 | |
| 3 | 32 | |
| 2 | 33 | |
| 2 | 37 | |
| 14 | 104 | |
| Qatawneh 2013 | 4 | 53 |
| 5 | 78 | |
| 3 | 43 | |
| 2 | 36 | |
| 7 | 42 | |
| Thijs 2010 abstract | 4 | 48 |
| 3 | 20 | |
| 2 | 53 | |
| 5 | 83 | |
| Total | 100 | 1227 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Awareness of prolapse (1‐3 years) Show forest plot | 12 | 1614 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.54, 0.81] |
| 1.1 Anterior compartment:mesh vs native tissue | 9 | 1172 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.51, 0.84] |
| 1.2 Multicompartment: mesh vs native tissue | 4 | 442 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.46, 0.97] |
| 2 Repeat surgery (1‐3 years) Show forest plot | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Prolapse | 12 | 1675 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.31, 0.88] |
| 2.2 Continence surgery | 9 | 1284 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.62, 1.83] |
| 2.3 Surgery for prolapse, SUI or mesh exposure | 7 | 867 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.40 [1.51, 3.81] |
| 3 Recurrent prolapse (any) at 1‐3 years Show forest plot | 21 | 2494 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.30, 0.53] |
| 3.1 Anterior compartment repair: mesh versus native tissue | 15 | 1748 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.26, 0.40] |
| 3.2 Multi‐compartment repair: mesh versus native tissue | 6 | 746 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.40, 0.87] |
| 4 Injuries bladder or bowel Show forest plot | 11 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Bladder injury | 11 | 1514 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.92 [1.62, 9.50] |
| 4.2 Bowel injury | 1 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.26 [0.13, 78.81] |
| 5 Objective failure of anterior compartment (cystocoele) Show forest plot | 13 | 1406 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.36, 0.55] |
| 5.1 Anterior compartment repair: mesh versus native tissue | 9 | 1004 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.28, 0.47] |
| 5.2 Multi‐compartment repair: mesh versus native tissue | 4 | 402 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.51, 1.06] |
| 6 Objective failure of posterior compartment (rectocoele) Show forest plot | 3 | 226 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.29, 1.42] |
| 6.1 Mesh vs native tissue | 3 | 226 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.29, 1.42] |
| 7 POPQ assessment (any mesh) Show forest plot | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Point Ba POPQ | 10 | 1125 | Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.27, ‐0.59] |
| 7.2 Point C POPQ | 8 | 925 | Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐1.13, 0.23] |
| 7.3 Point Bp | 7 | 832 | Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.34, 0.44] |
| 7.4 total vaginal length | 5 | 611 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.25, 0.40] |
| 8 Bladder function: de novo stress urinary incontinence (1‐3 years) Show forest plot | 12 | 1512 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.39 [1.06, 1.82] |
| 8.1 Anterior compartment: mesh vs native tissue | 8 | 1205 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [1.00, 2.11] |
| 8.2 Multi compartment : mesh vs native tissue | 4 | 307 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.90, 1.92] |
| 9 De novo voiding disorder, urgency, detrusor overactivity or overactive bladder Show forest plot | 3 | 236 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.35, 1.63] |
| 10 De novo dyspareunia (1‐3 years) Show forest plot | 11 | 764 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.58, 1.47] |
| 10.1 Anterior compartment: mesh vs native tissue | 8 | 643 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.60, 1.93] |
| 10.2 Multicompartment: mesh vs native tissue | 3 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.29, 1.42] |
| 11 Sexual function (1‐3 years) Show forest plot | 7 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 PISQ score | 7 | 857 | Mean Difference (IV, Fixed, 95% CI) | ‐0.13 [‐0.40, 0.13] |
| 12 Quality of life: continuous data (1‐2 years): Show forest plot | 7 | 665 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.20, 0.30] |
| 12.1 PQOL end score | 3 | 331 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.31, 0.49] |
| 12.2 Pelvic floor impact questionnaire end score | 4 | 334 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.34, 0.37] |
| 13 Quality of life: dichotomous data "much or very much better" Show forest plot | 1 | 168 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.80, 1.25] |
| 13.1 PGI‐I | 1 | 168 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.80, 1.25] |
| 14 Operating time (minutes) Show forest plot | 13 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Anterior compartment: mesh vs native tissue | 10 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Multicompartment: mesh vs native tissue | 3 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Blood transfusion Show forest plot | 6 | 723 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.88, 2.72] |
| 16 Length of stay in hospital (days) Show forest plot | 7 | 953 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.30, 0.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Awareness of prolapse (2 year review) Show forest plot | 1 | 54 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.77, 1.44] |
| 2 Repeat surgery for prolapse (2 years) Show forest plot | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.09, 2.40] |
| 3 Recurrent prolapse (3 months ‐2 years) Show forest plot | 3 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.52, 0.96] |
| 3.1 Any site stage 2 or more | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.10, 2.70] |
| 3.2 Anterior compartment | 2 | 226 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.53, 0.98] |
| 4 Death Show forest plot | 2 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 absorbable mesh versus native tissue repair | 2 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Objective failure of anterior compartment (cystocoele) Show forest plot | 2 | 226 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.53, 0.98] |
| 5.1 Anterior compartment repair: absorbable mesh versus native tissue | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.62, 1.34] |
| 5.2 Multi‐compartment repair: absorbable mesh versus native tissue | 1 | 143 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.35, 0.93] |
| 6 Objective failure of posterior compartment (rectocoele) Show forest plot | 1 | 132 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.40, 3.19] |
| 6.1 Multi‐compartment repair: absorbable mesh versus native tissue | 1 | 132 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.40, 3.19] |
| 7 Stress urinary incontinence Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Postoperative SUI | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.95, 2.00] |
| 8 Quality of life (2 years) Show forest plot | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐2.82, 2.82] |
| 8.1 VAS QoL | 1 | 54 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐2.82, 2.82] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Awareness of prolapse (1‐3 year) Show forest plot | 7 | 777 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.65, 1.43] |
| 1.1 Anterior compartment repair: biological graft vs native tissue | 4 | 429 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.45, 1.23] |
| 1.2 Multicompartment repair: biological graft vs native tissue | 1 | 126 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.55 [1.04, 19.92] |
| 1.3 Posterior compartment repair: biological graft vs native tissue | 2 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.41, 1.94] |
| 2 Repeat prolapse surgery (1‐2 years) Show forest plot | 5 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.61, 2.44] |
| 3 Recurrent prolapse (1 year) Show forest plot | 7 | 587 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.60, 1.47] |
| 3.1 Anterior compartment repair: biological graft vs native tissue | 5 | 369 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.54, 1.05] |
| 3.2 Posterior compartment repair: biological graft vs native tissue | 2 | 218 | Risk Ratio (M‐H, Random, 95% CI) | 2.09 [1.18, 3.70] |
| 4 Injuries to bladder or bowel Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 bladder injury | 1 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.01, 8.40] |
| 4.2 bowel injury | 1 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.13 [0.13, 75.57] |
| 5 Objective failure of anterior compartment (cystocele) Show forest plot | 6 | 570 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.46, 0.96] |
| 6 Objective failure of posterior compartment (rectocele) Show forest plot | 3 | 283 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.39, 3.51] |
| 7 POPQ assessment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Ba POPQ | 1 | 56 | Mean Difference (IV, Fixed, 95% CI) | ‐0.5 [‐0.98, ‐0.02] |
| 7.2 Point C | 1 | 56 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐1.28, 0.08] |
| 7.3 Bp POPQ | 1 | 56 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.27, 0.47] |
| 7.4 total vaginal length | 1 | 56 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.06, 1.14] |
| 8 De novo urinary stress incontinence Show forest plot | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 De novo voiding disorders, urgency, detrusor overactivity or overactive bladder Show forest plot | 2 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.29, 2.26] |
| 10 De novo dyspareunia (1 year) Show forest plot | 1 | 37 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.20, 3.67] |
| 11 Sexual function (1 year) Show forest plot | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐2.33, 4.33] |
| 11.1 PISQ | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐2.33, 4.33] |
| 12 Quality of life (1 year) Show forest plot | 2 | 84 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.48, 0.38] |
| 12.1 PQOL score | 1 | 56 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.42, 0.63] |
| 12.2 PFDI‐20 | 1 | 28 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐1.11, 0.39] |
| 13 Operating time (minutes) Show forest plot | 4 | 232 | Mean Difference (IV, Fixed, 95% CI) | 10.34 [6.31, 14.36] |
| 14 Blood transfusion Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.13 [0.14, 32.90] |

