针刺治疗成人神经性疼痛
Abstract
研究背景
神经性疼痛可能由神经损伤引起,并且是中枢神经系统病变的继发改变。尽管已有许多临床试验,但是针对神经性疼痛的针刺治疗的有效性和安全性仍存在不确定性。
研究目的
本综述的目的是评价针刺治疗成人慢性神经性疼痛的镇痛效果和不良事件。
检索策略
我们于2017年2月14日检索了CENTRAL,MEDLINE,Embase,4个中文数据库,临床试验网和世界卫生组织(World Health Organization, WHO)国际临床试验注册平台(International Clinical Trials Registry Platform, ICTRP)。我们还交叉检索了纳入研究的参考文献列表。
标准/纳入排除标准
我们纳入那些用于成人神经性疼痛的,治疗时间持续8周或更长的比较针刺(单独给予或与其他疗法联合使用)与假针刺、其他阳性治疗或常规治疗的随机对照试验(Randomised controlled trials, RCTs)。我们检索了基于针刺入和刺激人体组织的针刺治疗性研究,并且排除了在没有针刺入的情况下刺激针刺穴位的其他方法。我们检索了临床实践中使用的手针、电针或其他针刺技术的研究(如温针,火针等)。
数据收集与分析
我们使用了Cochrane推荐的标准方法流程。主要结局是疼痛强度和疼痛缓解。次要结局是任何与疼痛相关的结果,包括部分改善、退出、受试者经历任何不良事件、严重不良事件和生活质量。对于二分类结局,我们计算危险比(risk ratio, RR)和95%置信区间(confidence intervals, CI),对于连续型结局,我们计算平均差(mean difference, MD)与95%CI。我们还计算了在恰当情况下获得额外收益需治疗的人数( number needed to treat for an additional beneficial outcome, NNTB)。我们使用随机效应模型合并所有资料,并使用GRADE评价证据质量,以生成“结果摘要”表。
主要结果
我们纳入了6项研究,涉及462名患有慢性周围神经性疼痛的受试者(442名完成试验的受试者(251名男性),平均年龄52至63岁)。纳入的研究招募了来自中国的403名受试者和来自英国的59名受试者。大多数研究存在高偏倚风险,包括样本量较小(每个治疗组少于50名受试者),所有研究都面临受试者和研究人员破盲。大多数研究的随机序列生成的偏倚风险不明确(6项研究中有4项),包括分组隐藏(6项中有5项)和选择性报告(所有纳入研究)。所有的研究都调查了手针,我们没有发现任何比较针刺与常规治疗的研究,也没有任何研究调查其他针刺技术(如电针,温针,火针)。
一项研究将针刺与假针刺进行了比较。我们不确定两种干预措施之间在减轻疼痛强度方面是否有任何差异(n=45;MD=‐0.4,95%CI [‐1.83, 1.03],非常低质量的证据)。两组均未达到“比轻度疼痛更轻” (针刺和假针刺组的视觉模拟评分(visual analogue scale, VAS,0‐10)平均评分分别为5.8和6.2,其中0意味着无痛)。关于生活质量的资料有限,表明两组之间没有明显差异。没有关于疼痛缓解、不良事件或其他预定次要结局的证据。
三项研究将针刺与其他疗法(甲钴胺联合尼莫地平和肌醇)进行了比较。与其他疗法相比,针刺可降低疼痛“无临床反应”的风险(n=209; RR=0.25,95%CI [0.12, 0.51]),但是,没有证据表明疼痛强度、疼痛缓解、不良事件或任何其他次要结局。
两项研究比较了针刺联合其他阳性疗法(甲钴胺和消渴痹通胶囊)与单独使用的其他阳性疗法。我们发现与单独接受其他治疗的组相比,针刺联合组的疼痛强度VAS评分较低(n=104;MD=‐1.02,95%CI [‐1.09, ‐0.95]),生活质量较高(n=104;MD=‐2.19,95%CI [‐2.39, ‐1.99])。然而,针刺组和对照组的平均VAS评分分别为3.23和4.25,表明两组均未达到“比轻度疼痛低”。此外,这一证据来自一项具有高偏倚风险和极小样本量的研究。我们没有发现关于疼痛缓解的证据,两组之间在其他参数上也没有明显差异,包括对疼痛相关的“无临床反应”和退出。没有关于不良事件的证据。
由于研究限制(性能,检测和损耗偏倚的高风险,以及由于研究规模小而混杂的高风险)或不精确,证据的整体质量非常低。我们对效应估计的信心有限,并且真实效果可能与估计的效果大不相同。
作者结论
由于可获得的资料有限,与假针刺或其他有效疗法相比,没有足够的证据支持或反驳使用针刺治疗神经性疼痛或任何特定的神经性疼痛病症。由于治疗持续时间不明确,有5项研究仍在进行中,有7项研究待分类,这些研究的结果可能会影响目前的研究结果。
PICO
Plain language summary
针刺治疗成人神经性疼痛
系统综述问题
针刺能够安全有效地治疗成人慢性神经性疼痛吗?
研究背景
神经性疼痛是由神经受损引起的复杂的慢性疼痛。它不同于从受损组织沿着健康神经传递的疼痛信息(例如,跌倒或切割伤、或膝关节炎)。普通人群中大约7%至10%的人患有神经性疼痛。针刺是一种通过将针刺入皮肤或下面的组织来治疗疾病的传统中医(Traditional Chinese medicine, TCM)技术。
在本系统综述中,我们致力于明确对患有神经性疼痛的成年人,是否可以通过针刺治疗来缓解疼痛,改善生活质量,并且比其他治疗方案引起的副作用更少。我们寻找比较针刺与假针刺的研究(假针刺是指使用钝针插入针筒而不是穿透皮肤或皮下组织)。我们还寻找针刺与常规治疗或与其他阳性治疗(如甲钴胺、尼莫地平、肌醇和消渴痹通胶囊)比较的研究。
研究特征
我们于2017年2月对相关临床试验进行了检索。我们纳入了6项手针研究:1项研究是针刺与假针刺比较;3项研究是针刺联合其他阳性疗法与单独阳性疗法比较;2项研究是比较单独使用针刺和其他阳性治疗比较。这6项研究纳入462名患有慢性周围神经性疼痛的成年人。受试者平均年龄在52至63岁之间。他们接受了8周或更长时间的治疗。我们没有发现任何研究比较针刺与常规治疗,也没有任何其他针刺技术的研究(如电针,温针,火针)。
主要结果和证据质量
与假针刺或其他疗法(如甲钴胺,尼莫地平,肌醇和消渴痹痛胶囊)相比,我们不确定手针对疼痛强度,疼痛缓解和生活质量的有益作用。关于针刺的潜在危害(副作用)缺乏证据。
我们使用四个级别来评价这些研究中的证据质量:非常低,低,中等或高。非常低质量的证据意味着我们对结果非常不确定。高质量的证据意味着我们对结果非常有信心。该系统综述中的证据质量非常低,主要是由于研究方式存在问题(例如受试者对治疗不知情,或假针刺组的更多受试者提前离开研究)。研究中还包括受试者样本很少的情况。此外,这些发现仅适用于老年人的外周神经性疼痛。
总的来说,我们没有足够的证据支持或反驳使用针刺治疗神经性疼痛。
Authors' conclusions
Summary of findings
| Acupuncture versus sham acupuncture for neuropathic pain in adults | ||||||
| Patient or population: adults with neuropathic pain Comparison: sham acupuncture | ||||||
| Outcomes | Sham acupuncture | Acupuncture | Relative effect | No of participants | Quality of the evidence | Comments |
| Participant‐reported pain intensity | Mean 6.2 | Mean 5.8 | The mean participant‐reported pain intensity in the intervention group was | 45 | ⊕⊝⊝⊝ | Acupuncture has no clinical significant beneficial effects on pain intensity compared to sham acupuncture. |
| Participant‐reported pain relief substantial (at least 50% pain relief over baseline) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participants experiencing any serious adverse event | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Quality of life | Mean 27.7 | Mean 37.7 | The mean bodily pain component of quality of life in the intervention groups was 10 higher | 45 | ⊕⊝⊝⊝ | Acupuncture has no beneficial effects on bodily pain compared to sham acupuncture. |
| CI: confidence interval; MD: mean difference; SF‐36: Short Form (36) Health Survey (SF‐36); VAS: visual analogue scale | ||||||
| GRADE Working Group grades of evidence | ||||||
| aGarrow 2014 recruited 59 participants initially; there were 14 withdrawals and only the 45 participants that completed treatment were included in the study's final results. | ||||||
| Acupuncture versus treatment as usual for neuropathic pain in adults | ||||||
| Patient or population: adults with neuropathic pain Comparison: treatment as usual | ||||||
| Outcomes | Sham acupuncture | Acupuncture | Relative effect (Not applicable) | No of participants | Quality of the evidence | Comments |
| Participant‐reported pain intensity | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participant‐reported pain relief | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participants experiencing any serious adverse event | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Quality of life | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| GRADE Working Group grades of evidence | ||||||
| Acupuncture versus other active therapy for neuropathic pain in adults | ||||||
| Patient or population: adults with neuropathic pain Comparison: other active therapy | ||||||
| Outcomes | Sham acupuncture | Acupuncture | Relative effect (Not applicable) | No of Participants | Quality of the evidence | Comments |
| Participant‐reported pain intensity | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participant‐reported pain relief | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participants experiencing any serious adverse event | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Quality of life | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| GRADE Working Group grades of evidence | ||||||
| Acupuncture combined with other active therapy versus other active therapy for neuropathic pain in adults | ||||||
| Patient or population: adults with neuropathic pain Comparison: other active therapy alone | ||||||
| Outcomes | Other active therapy | Acupuncture combined with other active therapy | Relative effect | No of participants | Quality of the evidence | Comments |
| Participant‐reported pain intensity | Mean 4.25 | Mean 3.23 | The mean participant‐reported pain intensity in the intervention groups was | 104 | ⊕⊝⊝⊝ | Acupuncture combined other active therapy has no clinical significant beneficial effects on pain intensity compared to other active therapy alone. |
| Participant‐reported pain relief substantial (at least 50% pain relief over baseline) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participants experiencing any serious adverse event | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Quality of life | Mean 35.17 | Mean 32.98 | The mean bodily pain component of quality of life in the intervention groups was 2.19lower | 104 | ⊕⊕⊝⊝ | Acupuncture combined other active therapy improved the quality of life compared to other active therapy alone. |
| CI: confidence interval; FACT/the GOG‐Ntx: Functional Assessment of Cancer Therapy/Gynaecologic Oncology Group/Neurotoxicity; MD: mean difference; VAS: Visual Analogue Scale | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded twice for study limitations (risk of bias) due to high risk of performance and detection bias. | ||||||
Background
We based the methods of this review on a template used to review drugs to relieve neuropathic pain. The aim is for all reviews to use the same methods, based on new criteria for what constitutes reliable evidence in chronic pain (Moore 2010a; Appendix 1).
Description of the condition
The 2011 International Association for the Study of Pain defined neuropathic pain as "pain caused by a lesion or disease of the somatosensory system" (Jensen 2011), based on a previously agreed definition (Treede 2008). Neuropathic pain may be caused by nerve damage, and is often followed by changes to the central nervous system (Moisset 2007). Pain can be severe and may be present for months or years. The origin of pain is complex (Apkarian 2011; Tracey 2011), occurring in approximately between 6.9% and 10% of the population worldwide (Van Hecke 2014). Many people with neuropathic pain conditions are significantly disabled and experience moderate or severe pain for many years.
Neuropathic pain is usually classified according to the cause of nerve injury. The common causes of neuropathic pain include painful diabetic neuropathy (PDN), postherpetic neuralgia (PHN), amputation (stump and phantom limb pain), neuropathic pain after surgery or trauma, trigeminal neuralgia, stroke or spinal cord injury, and HIV infection. Neuropathic pain is also divided into peripheral neuropathic pain, central neuropathic pain (brain and spinal cord), or mixed (peripheral and central) neuropathic pain. Subsequently, there is an ongoing debate regarding the efficacy of different drugs for central versus peripheral neuropathic pain (Finnerup 2015).
Systematic reviews have reported that the overall prevalence of neuropathic pain in the general population is between 7% and 10% (Moore 2014b; Van Hecke 2014). In individual countries, prevalence rates of 3.3% in Austria (Gustorff 2008), 6.9% in France (Bouhassira 2008), and up to 8% in the UK (Torrance 2006) have been reported. Reports regarding the occurrence of some forms of neuropathic pain, such as PDN and post‐surgical chronic pain (which is often neuropathic in origin), are increasing (Hall 2008).
The small number of cases of neuropathic pain has resulted in varying estimates of incidence between individual studies. Between 2002 and 2005 in the UK (per 100,000 person‐year observation) there were 28 incidences of PHN recorded (95% confidence interval (CI) 27 to 30), 27 cases of trigeminal neuralgia (95% CI 26 to 29), 0.8 for phantom limb pain (95% CI 0.6 to 1.1), and 21 incidences of PDN (95% CI 20 to 22) (Hall 2008). Other studies estimate the incidence of trigeminal neuralgia at 4 per 100,000 (Katusic 1991; Rappaport 1994), and 12.6 per 100,000 (Koopman 2009), with estimates of 3.9 per 100,000 for PHN in the Netherlands (Koopman 2009). One systematic review of chronic pain demonstrated that some neuropathic pain conditions, such as PDN, are more common than other neuropathic pain conditions, with prevalence rates up to 400 per 100,000 (McQuay 2007).
Neuropathic pain is difficult to treat effectively, with only a minority of people experiencing a clinically relevant benefit from any one intervention. A multidisciplinary approach is now advocated, with pharmacological interventions being combined with physical or cognitive interventions, or both. Conventional analgesics, such as paracetamol and nonsteroidal anti‐inflammatory drugs, are not thought to be effective, but are frequently used (Di Franco 2010; Vo 2009). Some people may derive some benefit from a topical lidocaine patch or low‐concentration topical capsaicin, although evidence about the benefits of these interventions is unproven (Derry 2012; Derry 2014). High‐concentration topical capsaicin may benefit some people with PHN (Derry 2013), and treatment using so‐called 'unconventional analgesics', such as antidepressants (duloxetine and amitriptyline) (Lunn 2014; Moore 2012a; Sultan 2008), or antiepileptics (gabapentin or pregabalin) (Moore 2009; Moore 2011a; Wiffen 2013), are often prescribed.
One overview of treatment guidelines pointed out some general similarities between recommendations, but guidelines overall remain inconsistent (O'Connor 2009). The proportion of people who achieve worthwhile pain relief (typically at least 50% pain intensity reduction; Moore 2013a) is small, and is generally only 10% to 25% more when compared with placebo. The numbers needed to treat for an additional beneficial outcome are usually between 4 and 10 (Kalso 2013; Moore 2013b). Therefore, neuropathic pain is not particularly different from other chronic pain conditions, with only a small proportion of trial participants experiencing a good response to treatment (Moore 2013b).
Chronic pain conditions comprised five of the 11 top‐ranking global conditions for years lived with disability in 2010 (Vos 2012), and are responsible for a considerable reduction in quality of life, loss of employment, and increased healthcare costs (Moore 2014b).
Description of the intervention
Acupuncture is sought and offered as a treatment for pain in many societies (Macpherson 2004; Zhao 2011). Acupuncture is defined as needle insertion and stimulation of somatic tissues for therapeutic purposes. Acupuncture points (or acupoints) are described in anatomical regions but have no anatomical or physiological substrate to define them. Inserting needles at acupuncture points often involves the targeting of tissues in specific anatomical locations. The existence of point specificity in acupuncture remains controversial (Choi 2012). Several clinical studies found that acupuncture at specific acupuncture points according to the traditional acupuncture theory have similar effects to the sham acupuncture points (including non‐specific acupoints or non‐acupuncture points) (Enblom 2012; Li 2012). Therefore, some researchers claimed that the location of the acupoints may not be as important as the stimulation techniques used as part of acupuncture treatment. However, there has also been some evidence to validate the acupoint specificity (Wang 2015; Yang 2014). Wang and colleagues demonstrated that the effectiveness of acupuncture for relieving visceral hypersensitivity was different at individual acupoints; the effects are more predominant at the acupoints on the stomach meridian (Wang 2015). Yang 2014 observed that the pattern of brain glucose metabolism change at the acupoint was pertinent and targeted, while at the non‐acupoint it was disordered and randomised. Meanwhile, some studies had shown that specific acupoints have sensitisation in a particular disease state, which can reflect the disease and be used to treat it by stimulation with a specialised needle (He 2017; Yan 2017). The main cause of this argument is that the essence of meridians and acupoints remains unclear, so it is difficult to design a standard method as a non‐active control. In the sham acupuncture used in relevant studies, it is difficult to avoid all the active ingredients of acupuncture methods. On the other hand, acupoint may be a three‐dimensional structure, including the dermal, muscular, and neural components, as well as connective tissue and chemical aspects, because the acupuncture signals induced by varying needling‐depth stimulation may be transmitted through different neural pathways (Chen 2013; Wu 2015). Classical point locations that are frequently used are guided by the Chinese meridian theory, which states that there are 361 acupoints situated on the surface of the body. Tender points are also used by clinical acupuncturists.
A number of different acupuncture techniques have been developed including traditional manual acupuncture (MA), electroacupuncture (EA), acupuncture point injection, transcutaneous electrical acupoint stimulation (TEAS), and laser acupuncture (which involves low‐intensity, non‐thermal laser irradiation to stimulate acupuncture points). In clinical practice, the MA and EA techniques are widely used. MA involves inserting acupuncture needles into the skin, which are then twisted by hand until a feeling of 'deqi' (a sensation of soreness, heaviness, numbness, or distension) occurs in the area surrounding the needles. The EA technique involves delivering a stimulating current to the acupuncture points using an electrical stimulator. Typical acupuncture treatment involves the needles being left in place for up to 30 minutes, with multiple treatment sessions over several weeks.
There is a lack of consensus regarding the benefits of MA and EA, with some studies showing EA to have a superior analgesic effect (Lang 2010; Schliessbach 2011; Zheng 2010), and other studies showing no difference in pain reduction for MA and EA (Ahn 2011; Plaster 2014). Disagreement also exists regarding the effects of prolonged acupuncture stimulation, with research suggesting it can result in therapeutic benefit, but can also result in habituation and tolerance that weakens the beneficial effects of acupuncture (Han 2011; Leung 2008; Li 2014). One study demonstrated that the mean level of serum nitric oxide in people with migraine decreased by 31% after five acupuncture treatments (P value < 0.05) (Gündüztepe 2014). Other research has suggested that acupuncture is most effective when combined with another treatment, rather than as a stand‐alone treatment (Lu 2011; Miao 2014).
How the intervention might work
The overwhelming data from basic science support the idea that acupuncture mediates its clinically relevant effects via nerves, usually, but not exclusively, in deep somatic tissue (Dhond 2008; Kim 2008; Zhang 2005). EA stimulates all fibre types, since all nerve impulses work through alterations in membrane potentials mediated via voltage‐gated channels. MA mediates a mechanical stimulus, and therefore will only stimulate mechanosensitive nerve endings (Toda 2002; Zhao 2008). Release of adenosine via both techniques may mediate a local inhibition of nociceptive fibres (Goldman 2010). Some evidence suggests that in the central nervous system acupuncture may produce an analgesic effect by the deactivation of limbic areas (Hui 2010; Shi 2015). Alternatively, descending inhibitory modulation may also be regulated by acupuncture to enable the modulation of pain (Takeshige 1992).
Why it is important to do this review
Acupuncture has been increasingly used to treat chronic pain (including neuropathic pain) and is considered to be one of the most popular types of complementary alternative medicine available in Western healthcare (Barnes 2008), with a survey showing that 13% of adults in Europe and Israel have used acupuncture to treat chronic pain (Breivik 2006). However, uncertainty remains regarding the effectiveness and safety of acupuncture treatments despite a number of clinical trials being undertaken.
This review will use the methodological standards outlined in the PaPaS Author and Referee Guidance for Pain Studies (PaPaS 2012), which includes a definition of a reduction in pain intensity of 50% or more to identify improvements in co‐morbid symptoms, quality of life, and function. This approach will assess the best available evidence to determine whether acupuncture provides beneficial treatment for neuropathic pain in adults.
Objectives
To assess the analgesic efficacy and adverse events of acupuncture treatments for chronic neuropathic pain in adults.
Methods
Criteria for considering studies for this review
Types of studies
We included relevant randomised controlled trials (RCTs) with a treatment duration of eight weeks or longer. We only included studies published in a journal, with the exception of online summaries of otherwise unpublished clinical trials and abstracts with sufficient data for analysis. We excluded studies that were non‐randomised or quasi‐randomised (e.g. allocation by odd or even date of birth), studies of experimental pain, case reports, and clinical observations.
Types of participants
Adults aged 18 years and above with one or more chronic neuropathic pain conditions including (but not limited to):
-
cancer‐related neuropathy;
-
central neuropathic pain;
-
complex regional pain syndrome (CRPS) Type II;
-
HIV neuropathy;
-
painful diabetic neuropathy (PDN);
-
phantom limb pain;
-
postherpetic neuralgia (PHN);
-
postoperative or traumatic neuropathic pain;
-
spinal cord injury;
-
trigeminal neuralgia.
If we found studies of participants with more than one type of neuropathic pain, we planned to analyse results according to the primary condition. We excluded studies of migraine and headache as they are the subject of another Cochrane Review (Chronicle 2004). In studies where people had a mixture of other types of pain and neuropathic pain, we included a study only if the majority of participants (greater than 80%) had neuropathic pain.
Types of interventions
Acupuncture either given alone or in combination with other therapies, with acupuncture therapy defined as needle insertion and stimulation of somatic tissues for therapeutic purposes. When acupuncture is given in combination with other therapies, the therapy given to the acupuncture group has to also be given to the control group. We included any stimulation based on needle insertion, for example, electrical stimulation (EA) and warm needling (involving the burning of mugwort on an acupuncture needle inserted in the skin or tissues below to heat the needle). We excluded other methods of stimulating acupuncture points without needle insertion (e.g. direct moxibustion, indirect moxibustion, heat‐sensitive moxibustion, moxa burner moxibustion, crude drug moxibustion, or natural moxibustion). Therefore, we included moxibustion with needle insertion but excluded any other types of moxibustion alone.
We compared:
-
acupuncture versus sham acupuncture;
-
acupuncture versus treatment as usual;
-
acupuncture versus other active therapies (anything that is a planned comparison, e.g. exercise or drug therapy).
-
acupuncture combined with other active therapy versus other active therapy
We excluded studies that compared different forms of acupuncture. We also excluded studies with acupuncture assigned to each investigated group (e.g. acupuncture alone versus acupuncture plus adjuvant treatment).
Types of outcome measures
Primary outcomes
-
Participant‐reported pain intensity at the end of treatment measured using a validated visual analogue scale (VAS) or categorical pain scale. We are particularly interested in the number of people who achieve 'no worse than mild pain' (Moore 2013a). We consider 3 out of 10 on a numerical rating scale, or 30/100 mm on a VAS, as 'no worse than mild pain' (Wiffen 2013).
-
Participant‐reported pain relief at the end of treatment measured using a validated VAS or categorical pain scale. Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) defines at least 30% pain relief over baseline as moderate pain relief, and at least 50% pain relief over baseline as substantial pain relief in chronic pain (Dworkin 2008).
Secondary outcomes
-
Any pain‐related outcome indicating some improvement
-
Withdrawals due to lack of efficacy, adverse events, and for any cause
-
Participants experiencing any adverse event
-
Participants experiencing any serious adverse event. Serious adverse events typically include any untoward medical occurrence or effect that at any dose results in death, is life‐threatening, requires hospitalisation or prolongation of existing hospitalisation, results in persistent or significant disability or incapacity, is a congenital anomaly or birth defect, is an 'important medical event' that may jeopardise the person, or may require an intervention to prevent one of the above characteristics or consequences.
-
Specific adverse events, particularly somnolence and dizziness
-
Quality of life
'Summary of findings' table
We included 'Summary of findings' tables to present the main findings for all comparisons in a transparent and simple tabular format. In particular, we included key information concerning the quality of evidence, the magnitude of effect of the interventions examined, and the sum of available data on the outcomes:
-
participant‐reported pain intensity measured using a VAS (including the number of participants who achieved 'no worse than mild pain');
-
pain relief (including the number of participants who achieved at least 50% pain relief from baseline);
-
serious adverse events;
-
quality of life (all scales reported).
We used the GRADE approach to assess the quality of evidence (Appendix 2; Schünemann 2011a, Schünemann 2011b; GRADEpro GDT 2015).
Search methods for identification of studies
Electronic searches
We searched the following databases on 14 February 2017, without language or date restrictions:
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, issue 2) via the Cochrane Register of Studies Online (CRSO);
-
MEDLINE (via Ovid) 1946 to Feb week 1 2017;
-
Embase (via Ovid) 1974 to 2017 week 07;
-
Chinese databases: Chinese BioMedical Literature Database (CBM); China National Knowledge Infrastructure (CNKI); Chongqing Weipu (VIP); Wanfang Database.
The search strategies for CENTRAL, MEDLINE and Embase can be found in Appendix 3, Appendix 4 and Appendix 5. The search strategies for the Chinese databases are presented in Appendix 6, Appendix 7, Appendix 8, and Appendix 9.
Searching other resources
We reviewed the bibliographies of any RCTs and review articles that we identified. We also searched the following clinical trial databases in February 2017: The metaRegister of Controlled Trials (mRCT) (www.controlled‐trials.com/mrct/), ClinicalTrials.gov (ClinicalTrials.gov), and World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/) to identify additional published or unpublished data. We did not contact investigators or study sponsors for unpublished studies.
Data collection and analysis
We performed separate analyses according to particular neuropathic pain conditions. We combined different neuropathic pain conditions in analyses for exploratory purposes only.
Selection of studies
We determined eligibility by reading the abstract of each study identified by the search. We excluded studies that clearly did not satisfy the inclusion criteria, and we obtained full copies of the remaining studies. Two review authors (TYC and JZ) read the studies independently and reached agreement by discussion. We did not anonymise the studies before assessment. We created a PRISMA flow chart (Moher 2009) and a 'Characteristics of included studies' table for each study, and noted the reasons for exclusion in the Characteristics of excluded studies tables.
Data extraction and management
Two review authors (ZYJ and YY) extracted data independently using a standard form and checked for agreement before entering the data into Review Manager 5 (RevMan 2014). Where a study was reported in more than one paper, we collated multiple reports of each study into a single data extraction form. We extracted data regarding the pain condition and number of participants treated, management of interventions, study design (placebo or active control), study duration and follow‐up, analgesic outcome measures, withdrawals, and adverse events (participants experiencing any adverse event or serious adverse event). We resolved any disagreement by discussion.
Assessment of risk of bias in included studies
Two review authors (HSC and SML) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), and adapted from those used by Cochrane Pregnancy and Childbirth (Derry 2012a), with any disagreements resolved by discussion.
-
Random sequence generation (checking for possible selection bias). We assessed the method used to generate the allocation sequence as low risk of bias (any truly random process, e.g. random number table or computerised random number generation) or unclear risk of bias (the method used to generate sequence not clearly stated). We would not assess high risk of bias on this domain because non‐randomised or quasi‐randomised studies were excluded directly.
-
Allocation concealment (checking for possible selection bias). The method used to conceal allocation to interventions prior to assignment determines whether intervention allocation could have been foreseen in advance, during recruitment, or changed after assignment. We assessed the methods as low risk of bias (e.g. telephone or central randomisation or consecutively numbered, sealed, opaque envelopes), unclear risk of bias (method not clearly stated), or high risk of bias.
-
Blinding of participants and outcome assessment (checking for possible performance and detection bias). During the acupuncture application, the acupuncturist knows the group to which the participants belonged, therefore, we assessed the methods used to blind participants and outcome assessors. We assessed the methods as low risk of bias (study states that it was blinded and describes the method used to achieve blinding for participants, e.g. identical acupuncture needles matched in appearance (Takakura 2013)), unclear risk of bias (study states that it was blinded but does not provide an adequate description of how it was achieved), or high risk of bias (no blinding or incomplete blinding).
-
Incomplete outcome data (checking for possible attrition bias due to the use of incomplete outcome data). We assessed the methods used to deal with incomplete data as low risk of bias (less than 10% of participants did not complete the study, or used appropriate modelling to impute missing data), unclear risk of bias (insufficient reporting of attrition), or high‐risk of bias (drop out is greater than 10% and used 'completer‐only' analysis).
-
Selective reporting (reporting bias due to selective outcome reporting). We assessed this as low risk of bias where the study protocol was available and all of the study's pre‐specified (primary and secondary) outcomes that were of interest in the review had been reported in the pre‐specified way, or if the study protocol was not available but it was clear that the published reports included all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon). We assessed this as high risk of bias when:
-
not all of the study's pre‐specified primary outcomes had been reported;
-
one or more primary outcomes was reported using measurements, analysis methods, or subsets of the data (e.g. subscales) that were not pre‐specified;
-
one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting was provided, such as an unexpected adverse event);
-
one or more outcomes of interest in the review were reported incompletely, so that they could not be entered in a meta‐analysis;
-
and the study report did not include results for a key outcome that was expected to have been reported for such a study.
-
-
Size of study (checking for possible biases confounded by small size). We assessed studies as being at low‐risk of bias (200 or more participants per treatment arm), unclear risk of bias (50 to 199 participants per treatment arm), or high‐risk of bias (fewer than 50 participants per treatment arm).
Measures of treatment effect
We calculated numbers needed to treat for additional beneficial outcomes as the reciprocal of the absolute risk reduction (ARR; McQuay 1998). For unwanted effects, the number needed to treat for an additional beneficial outcome (NNTB) became the number needed to treat for an additional harmful outcome (NNTH) and we calculated it in the same manner. For dichotomous outcomes, we calculated risk ratio (RR) with 95% CI; for continuous outcomes, we calculated mean difference (MD) with 95% CI.
Unit of analysis issues
For studies with multiple treatment arms and a single control arm, where the treatment arms were not combined for analysis, we split the number of control participants between comparisons.
The particular concern of cross‐over studies is the carry‐over effect. For the data extracted from a cross‐over study, we only used data from the first period, unless the data from both arms had been reported in a manner suitable for alternative methods of analysis (Higgins 2011).
However, there were no studies that had more than two available arms or with cross‐over design.
Dealing with missing data
We used intention‐to‐treat (ITT) analysis, and missing participants were assigned zero improvement wherever possible.
Assessment of heterogeneity
We dealt with methodological and clinical heterogeneity by combining studies with similar research design and examining similar conditions. We assessed statistical heterogeneity visually (L'Abbé 1987), and used the I2 statistic (Higgins 2003). We interpreted an I2 estimate greater than or equal to 75%, accompanied by a statistically significant Chi2 statistic, as evidence of substantial levels of heterogeneity (Deeks 2011), in which case we explored reasons for heterogeneity (Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
As described in the Cochrane Handbook for Systematic Reviews of Interventions (Sterne 2011), reporting biases occur when the reporting of research findings is influenced by the nature and direction of results. Funnel plots may be useful in investigating reporting biases but are of limited power to detect small‐study effects (Egger 1997). We would have employed funnel plots for outcomes if they had included 10 studies or more that reported relevant data.
Data synthesis
Due to the high possibility of heterogeneity for participants and interventions in this review, where possible we conducted meta‐analysis using a random‐effects model.
Subgroup analysis and investigation of heterogeneity
We planned to conduct subgroup analyses of different techniques of acupuncture practice (such as MA, EA, auricular acupuncture, and warm needling). We were unable to conduct this subgroup analysis, however, because all the included studies used MA. We also planned to conduct subgroup analysis of 'peripheral versus central pain' but we were unable to because there were insufficient data.
We will conduct these subgroup analysis in future updates if more data become available.
Sensitivity analysis
Where the data were sufficient, we conducted sensitivity analysis for primary outcomes to test the robustness of the results. As our measured outcomes were based on subjectively rated scales, we had planned to assess whether the quality of included studies influenced the pooled result by excluding studies with high risk of bias for blinding (performance and detection bias). We tested whether missing data influenced the results where the ITT analysis had been applied by assigning missing participants as zero improvement. We reported both sets of results and discussed them. However, we did not perform any sensitivity analysis due to insufficient data reported for primary outcomes in the included studies.
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies.
Results of the search
The initial search resulted in 5314 references in total, of which 4733 were identified from seven databases and 581 were identified through other sources. After checking for duplication, 3574 unique references remained. Upon inspection of the title and abstracts of these, we excluded a further 3521 references. We read the remaining 50 studies (with 53 references) in full, and we subsequently excluded 31 studies (with 34 references) with reasons (please refer to Figure 1 for further detail). Eight studies are awaiting assessment and five studies are ongoing. Eventually, we were able to include six studies in this review and five were included in the meta‐analysis.

Study flow diagram
Included studies
Six RCTs with 462 participants (442 completers) met the inclusion criteria for this review. The sample sizes ranged from 59 to 104 (see Characteristics of included studies).
Participants
Most of the participants (n = 403) were recruited from China (Han 2017; Han 2017a; Wang 2016; Zhang 2010; Zhao 2016). The remaining 59 participants in Garrow 2014 were recruited from the UK.
The average age of included participants ranged from 52 to 63 years of age, and included 251 men and 191 women. Two studies (Garrow 2014; Han 2017) did not report the age and gender of the dropouts (n = 20). The included participants were diagnosed with peripheral neuropathic pain. The 358 participants in five studies (Garrow 2014; Han 2017a; Wang 2016; Zhang 2010; Zhao 2016) were diagnosed with diabetic peripheral neuropathy. The remaining 104 participants in Han 2017 were diagnosed with chemotherapy‐induced peripheral neuropathy. Three studies (Garrow 2014; Han 2017; Han 2017a) did not report the length of illness of participants, while the remaining studies included participants with peripheral neuropathic pain for more than three months.
Interventions
One study (Wang 2016) had three treatment arms. We excluded one treatment arm in this study, as it did not meet our inclusion criteria. The remaining six studies had two treatment arms.
All six studies treated the intervention group with manual acupuncture (Garrow 2014; Han 2017; Han 2017a; Wang 2016; Zhang 2010; Zhao 2016). Manual acupuncture was used alone in four studies, compared with sham acupuncture (Garrow 2014) or Western medicine. Mecobalamin combined with nimodipine was used as a control in Han 2017a and Zhao 2016, and inositol was the control in Zhang 2010. Manual acupuncture combined with mecobalamin was administered in Han 2017, compared with mecobalamin used alone. Manual acupuncture combined with Xiaoke bitong capsule was administered in Wang 2016, compared with Xiaoke bitong capsule used alone.
The details for acupuncture points used in included studies are outlined in Table 1. The treatment duration of all included studies ranged from 8 to 12 weeks.
| Acupuncture points used | Study ID |
| Taixi (KI3); Hegu (LI4); Taichong (LR3); Sanyinjiao (SP6); Zusanli (ST36) | |
| Shenmai (B62); Zulinqi (GB41); Zhaohai (K6); Lieque (L7); Neiguan (P6); Houxi (SI3); Waiguan (SJ5); Gongsun (SP4) | |
| Feishu (BL13); Geshu (BL17); Feiyang (BL58); Zulinqi (GB41); Zhiyang (GV9); Shendao (GV11); Shenzhu (GV12); Dazhui (GV14); Taichong (LR3); Sanyinjiao (SP6); Xuehai (SP10); Tianshu (ST25); Zusanli (ST36); Xiangu (ST43) | |
| The main points: Huantiao (GB30); Yanglingquan (GB34); Sanyinjiao (SP6); Zusanli (ST36); The auxiliary points (selected 2‐3from following): Shenshu (BL23); Kunlun (BL60); Guanyuan (CV4); Qihai (CV6); Huantiao (GB30); Taixi (K3); Taichong (LIV3); Pishu (PL20) | |
| The main points: Ganshu (BL18); Pishu (BL20); Shenshu (BL23); Yishu; Feishu (BL58); Zusanli (ST36); Sanyinjiao (SP6), Taibai (SP3); Zutonggu; Qihai (CV6); Guanyuan (CV4); Fenglong(ST40) and Yanglingquan (GB34); The auxiliary points: Jianyu (LI15); Quchi (LI11); Shousanli (LI10); Hegu (LI4); Biguan (ST31); Futu (ST32); Liangqiu (ST34); Xiangu (ST43) and Neiting (ST 44); Added for blood stasis points: Geshu (BL17) and Xuehai (SP10); Added for severe numbness of the hands and feet points: Bafeng(EX‐LE10) and Baxie (EX‐UE9). |
Outcomes
Participant‐reported pain intensity at the end of treatment
Two studies measured participant‐reported pain intensity (Garrow 2014; Han 2017). Garrow 2014 measured pain intensity with a VAS from 0 to 100, so we transferred those data to 0 to 10 scale measurements. (See Table 2 for details of the scales used.)
| Outcomes | Scales | Description of scales | Relevant Studies |
| Participant‐reported pain intensity | Visual Analogue Scale (VAS) | The VAS is a visual analogue scale for pain intensity, in which 0 means no pain and 10 (or 100) means the worst pain ever experienced. | |
| Quality of life | Short Form (36) Health Survey (SF‐36) | The SF‐36 is a 36‐item, patient‐reported survey of patient health and consists of 8 scaled scores, which are the weighted sums of the questions in their section. Each scale is directly transformed into a 0‐100 scale on the assumption that each question carries equal weight. The lower the score, the more disability. The 8 sections are: vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning and mental health. Summary scores for the SF‐12, version 2 (SF‐12v2) health status measure are based on scoring coefficients derived for version 1 of the SF‐36. The higher score is better. | |
| Functional Assessment | The FACT/GOG‐Ntx questionnaire is used to investigate patients' daily activities and evaluate the degree of neuropathy. The questionnaire includes 7 questions about physical well‐being, 7 questions about social/family well‐being, 6 questions about emotional well‐being, 7 questions about functional well‐being and 9 questions about additional concerns. Where in each question, 0 = not at all and 4 = very much, lower is better. |
Participant‐reported pain relief at the end of treatment
No study reported this outcome.
Any pain‐related outcome indicating some improvement
Three studies (Han 2017a; Wang 2016; Zhao 2016) reported any pain‐related outcome, that was the number of participants who were judged to have 'no clinical response'. (See Characteristics of included studies for definition details.)
Withdrawal due to lack of efficacy, adverse effects or for any cause
Two studies reported withdrawals from the study (Garrow 2014; Han 2017) due to any cause.
Participants experiencing any adverse event
Only one study (Garrow 2014) reported participants experiencing any adverse event.
Participants experiencing any serious adverse event
No study reported this outcome.
Specific adverse events, particularly somnolence and dizziness
No study reported this outcome.
Quality of life
Two studies reported quality of life using different scales (Garrow 2014; Han 2017). (See Table 2 for details of scales used.)
Excluded studies
We excluded 31 studies (34 references) from this review for the following reasons (see Characteristics of excluded studies).
-
Issues relating to study design: we excluded six studies as they were not randomised controlled trials (Hu 2015; Schroeder 2012; Shen 2009; Tan 2004; Zhao 2009; Zheng 2014).
-
Issues relating to participants: we excluded five studies as the included participants were not adult patients with neuropathic pain (Chung 2016; Franca 2008; Koh 2013; MacPherson 2015; Tam 2007).
-
Issues relating to the intervention: two studies employed therapeutic methods that did not meet our criteria, like moxibustion or trigger‐point injection (Ay 2010; Lin 2004). We also excluded 12 studies (15 references) because the treatment duration was less than eight weeks (Chen 2007; Dyson‐Hudson 2007; Gao 2012; Itoh 2009; Itoh 2012; Liu 2013; Penza 2011; Sun 2014; Wang 2013; Zhang 2015; Zheng 2013; Zhu 2011).
-
Issues relating to comparison: we excluded five studies for this reason. Four studies reported acupuncture being given in combination with other therapies, but the same therapy was not given to the control group (Li 2010; Lin 2006; Zhang 2013; Zhou 2011). The fifth study was excluded as they compared different forms of acupuncture (Wang 2007).
-
In addition, we excluded one clinical trial (NCT01881932) as it was terminated with no published results.
Studies awaiting classification
See Characteristics of studies awaiting classification.
There were seven studies awaiting classification due to unclear treatment duration. The location of these studies were the USA (Maeda 2013), Germany (DRKS00010625) and China (chiCTR‐INR‐16009079; NCT02770963; NCT03048591; Shen 2016; Yue 2016). One study (Rivera 2010) based in Spain was not printed in English or Chinese and is awaiting translation.
Ongoing studies
See Characteristics of ongoing studies.
We identified five ongoing studies that started between 2007 and 2017 but had not been published. The location of these studies were the USA (NCT01163682; NCT02104466; NCT02831114), Korea (Shin 2011), and China (NCT02553863). Three studies (Shin 2011; NCT02104466; NCT02831114) were in the recruiting phase and the other two studies (NCT01163682; NCT02553863) had not yet started recruiting at the time of writing this review.
Risk of bias in included studies
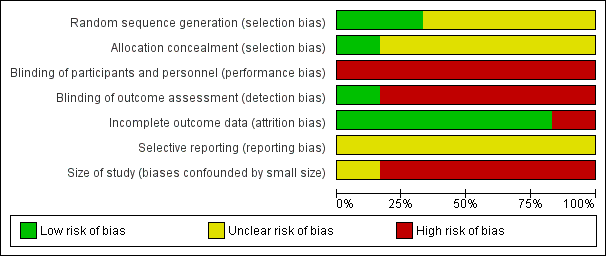
Details of these assessments are available in the 'Risk of bias' table corresponding to each study in the Characteristics of included studies tables, and are also presented in the 'Risk of bias' graph (Figure 2) and summary (Figure 3).
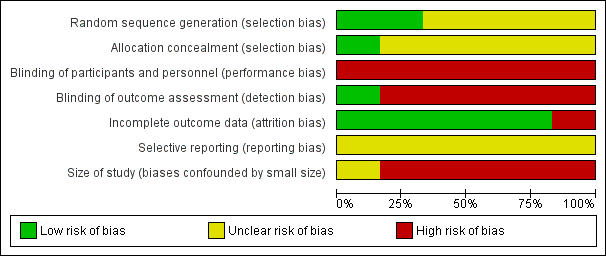
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
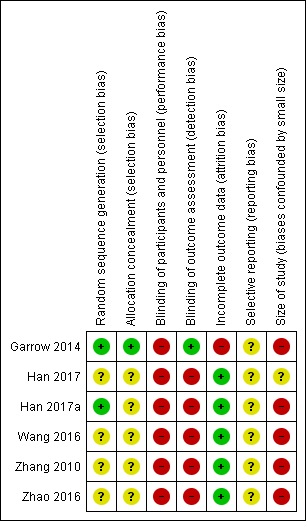
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study
Allocation
Random sequence generation
All six included studies reported some form of randomisation. Two studies reported adequate sequence generation and we rated them as low risk. The methods used to generate the allocation sequence included random number tables (Han 2017a), or computerised randomisation programs (Garrow 2014). The remaining four studies provided insufficient information to assess bias on this domain and we classified them as unclear risk of bias.
Allocation concealment
Only Garrow 2014 reported adequate allocation concealment. This study used sealed, opaque envelopes, managed by a person who was not involved with the study, to maintain allocation concealment. The remaining five studies did not provide enough information to rate this bias and so we classified them as unclear.
Blinding
We found all included studies had high risk of performance bias. For five studies (Han 2017; Han 2017a; Wang 2016; Zhang 2010; Zhao 2016), participants in one group received acupuncture and the other group did not. It would not have been possible to blind participants and healthcare professionals giving the treatment. In the study Garrow 2014 (acupuncture versus sham acupuncture), the treatment allocation was revealed to the acupuncturists but out of sight of the participants.
We also rated all included studies, except for one (Garrow 2014, low risk), as high risk of detection bias in that the primary outcomes (e.g. pain intensity) were subjective measures and were reported by the participants themselves. The unblinding of the participants is likely to influence the detection of true effect. However, in the study Garrow 2014, it is possible that the participants had been blinded.
Incomplete outcome data
We rated five studies as low risk of bias in this domain: four studies did not have missing outcome data (Han 2017a; Wang 2016; Zhang 2010; Zhao 2016); and we rated the other one study as low risk (Han 2017) due to the fact that the proportion of dropout was less than 10% and reasons for dropout were not relevant to the effect of intervention. The dropout rate was higher than 10% in the study Garrow 2014 (14/59, 23.7%) and the study author only analyzed data from completers, and so we rated this study as high risk of attrition bias.
Selective reporting
The study protocols were not available and we rated all studies to be at unclear risk of reporting bias.
Size of study (biases confounded by small size)
We judged five studies to be at a high‐risk of bias due to small sample size (fewer than 50 participants per treatment arm: Garrow 2014; Han 2017a; Wang 2016; Zhang 2010; Zhao 2016). We found the remaining study (Han 2017) to have an unclear risk of bias (52 participants per treatment arm).
Effects of interventions
See: Summary of findings for the main comparison Acupuncture versus sham acupuncture for neuropathic pain in adults; Summary of findings 2 Acupuncture versus treatment as usual for neuropathic pain in adults; Summary of findings 3 Acupuncture versus other active therapy for neuropathic pain in adults; Summary of findings 4 Acupuncture combined with other active therapy versus other active therapy for neuropathic pain in adults
Comparison 1: acupuncture versus sham acupuncture
For this comparison, we found only one relevant study (Garrow 2014) involving 59 participants receiving either manual acupuncture or sham acupuncture. However, only 45 participants completed the assessment and were included in the analysis for pain intensity and quality of life.
See summary of findings Table for the main comparison.
Primary outcomes
Participant‐reported pain intensity
Garrow 2014 found no clear difference on VAS score of pain intensity between the manual acupuncture and the sham acupuncture groups (n = 45; MD ‐0.40, 95% CI ‐1.83 to 1.03; Table 3). We judged the quality of evidence for this outcome to be very low. We downgraded the quality of evidence twice for very serious limitations to study quality due to high risk of performance and attrition bias (high withdraw rates, and unbalanced as well), and high risk of bias confounded by small study size; and once for imprecision due to wide 95% CIs.
| Acupuncture versus sham acupuncture | ||||||||||
| Outcome | Specific measurement | Study | Manual acupuncture group | Sham acupuncture group | Effect measure | Statistical test | ||||
| Mean | SD | Total | Mean | SD | Total | MD (95%CI) | P value | |||
| Pain intensity | VASa | 5.8 | 2.6 | 24 | 6.2 | 2.3 | 21 | ‐0.40 (‐1.83 to 1.03) | 0.58 | |
| Quality of life | SF‐36b: physical health score | 31.9 | 9.2 | 24 | 32.1 | 9.8 | 21 | ‐0.20 (‐5.78 to 5.38) | 0.94 | |
| SF‐36: mental health score | 39.2 | 14 | 24 | 35.7 | 12.6 | 21 | 3.50 (‐4.17 to 11.27) | 0.38 | ||
| SF‐36: bodily pain score | 37.7 | 27.4 | 24 | 27.7 | 16.9 | 21 | 10.00 (‐3.13 to 23.13) | 0.14 | ||
| Acupuncture + other active therapies versus other active therapies | ||||||||||
| Outcome | Specific measurement | Study | Acupuncture + other active therapies group | Other active therapies group | Effect measure | Statistical test | ||||
| Mean | SD | Total | Mean | SD | Total | MD (95%CI) | P value | |||
| Pain intensity | VAS | 3.23 | 0.17 | 52 | 4.25 | 0.197 | 52 | ‐1.02 (‐1.09 to ‐0.95) | < 0.00001 | |
| Quality of life | FACT/the GOG‐Ntxc | 32.98 | 0.542 | 52 | 35.17 | 0.518 | 52 | ‐2.19 (‐2.39 to ‐1.99) | < 0.00001 | |
MD: mean difference; SD: standard deviation
aVAS: Visual Analogue Scale (0‐10, lower is better)
bSF‐36: Short Form (36) Health Survey (0‐100, higher is better)
cFACT/the GOG‐Ntx: Functional Assessment of Cancer Therapy/Gynaecologic Oncology Group/ Neurotoxicity questionnaire (lower is better)
Participant‐reported pain relief
The study did not explicitly report this outcome, but the average VAS score of the manual acupuncture and sham acupuncture groups was 5.8 and 6.2 respectively, indicating that neither group achieved 'no worse than mild pain'.
Secondary outcomes
Any pain‐related outcome
The study did not report this outcome.
Withdrawals due to lack of efficacy, adverse events, and for any cause
The study reported that 14 participants withdrew from the study and were lost to follow‐up. Three of these withdrew due to adverse events. Fewer dropouts (n = 4) were reported in the manual acupuncture group than the sham acupuncture group (n = 10), but no clear differences were observed (n = 59; RR 0.44, 95% CI 0.16 to 1.25; NNTB = 6; Table 4). We judged the quality of evidence for this outcome to be very low. We downgraded the quality of evidence twice for very serious limitations to study quality due to high risk of performance and attrition bias, and high risk of bias confounded by small study size; and once for imprecision due to wide 95% CI.
| Acupuncture versus sham acupuncture | ||||||||
| Outcome | Study | Manual acupuncture group | Sham acupuncture group | Effect measure | Statistical test | |||
| Events | Total | Events | Total | RR (95%CI) | NNTB | P value | ||
| Withdraw from trial due to any cause | 4 | 28 | 10 | 31 | 0.44 (0.16 to 1.25) | NNTB = 6 | 0.53 | |
| Adverse events: any cases | 1 | 28 | 2 | 31 | 0.55 (0.05 to 5.78) | NNTB = 34 | 0.62 | |
| Acupuncture + other active therapies versus other active therapies | ||||||||
| Outcome | Study | Acupuncture + other active therapies group | Other active therapies group | Effect measure | Statistical test | |||
| Events | Total | Events | Total | RR (95%CI) | NNT | P value | ||
| Any pain‐related outcomes: no clinical response | 4 | 30 | 10 | 30 | 0.40 (0.14 to 1.14) | NNTB = 5 | 0.09 | |
| Withdraw from trial due to any cause | 3 | 52 | 3 | 52 | 1.00 (0.21 to 4.73) | NA | 1.00 | |
NA: not applicable; NNTB: number needed to treat for an additional beneficial outcome; RR: risk ratio
Participants experiencing any adverse event
The study did not find any notable differences between the manual acupuncture and sham acupuncture groups (n = 59; RR 0.55, 95% CI 0.05 to 5.78; NNTB = 34; Table 4). We judged the quality of evidence for this outcome to be very low. We downgraded the quality of evidence twice for very serious limitations to study quality due to high risk of performance and attrition bias, and high risk of bias confounded by small study size; and once for imprecision due to wide 95% CI.
Participants experiencing any serious adverse event
The study did not report this outcome.
Specific adverse events, particularly somnolence and dizziness
The study did not report this outcome.
Quality of life
The study found no clear differences on physical health score (n = 45; MD ‐0.20 95% CI ‐5.78 to 5.38), mental health score (n = 45; MD 3.50 95% CI ‐4.17 to 11.27) and bodily pain score (n = 45; MD 10.00 95% CI ‐3.13 to 23.13) (Table 3). We judged the quality of evidence for this outcome to be very low. We downgraded the quality of evidence twice for very serious limitations to study quality due to high‐risk of performance and attrition bias, and high risk of bias confounded by small study size; and once for imprecision due to wide 95% CI.
We did not perform subgroup analysis or sensitivity analysis in this comparison due to insufficient data.
Comparison 2: acupuncture versus treatment as usual
We found no studies reporting data for this comparison.
Comparison 3: acupuncture versus other active therapy
For this comparison, we found three relevant studies (Han 2017a; Zhang 2010; Zhao 2016; n = 209) that compared manual acupuncture with other active therapy. The other active therapies were mecobalamin combined with nimodipine, and inositol.
Primary outcomes
Participant‐reported pain intensity
No study reported this outcome.
Participant‐reported pain relief
No study reported this outcome.
Secondary outcomes
Any pain‐related outcome
The three relevant studies (Han 2017a; Zhang 2010; Zhao 2016) reported data for the number of participants with 'no clinical response'. There were fewer participants with no clinical response in the manual acupuncture group than in the 'Western medicine' group (n = 209; RR 0.25, 95% CI 0.12 to 0.51; NNTB = 4; Analysis 1.1). We judged the quality of evidence for this outcome to be very low. We downgraded the quality of evidence twice for very serious limitations to study quality due to high risk of performance and attrition bias, and high risk of bias confounded by small study size; and once for imprecision due to wide 95% CI.
Withdrawals due to lack of efficacy, adverse events, and for any cause
No study reported this outcome.
Participants experiencing any adverse event
No study reported this outcome.
Participants experiencing any serious adverse event
No study reported this outcome.
Specific adverse events, particularly somnolence and dizziness
No study reported this outcome.
Quality of life
No study reported this outcome.
We did not perform subgroup analysis or sensitivity analysis in this comparison due to insufficient data.
Comparison 4: acupuncture combined with other active therapy versus other active therapy
For this comparison, we found two relevant studies (Han 2017; Wang 2016; n = 164). The acupuncture technique that the studies employed was manual acupuncture. The other active therapies were mecobalamin, and Xiaoke bitong capsule.
See summary of findings Table 4.
Primary outcomes
Participant‐reported pain intensity
For this outcome, we found only one relevant study where pain was measured using VAS. Han 2017 reported that participants receiving manual acupuncture combined with mecobalamin had a lower VAS score of pain intensity than those receiving mecobalamin used alone (n = 104; MD ‐1.02, 95% CI ‐1.09 to ‐0.95; Table 3), but the average VAS score of the acupuncture and control groups were 3.23 and 4.25 respectively, indicating that neither group achieved 'no worse than mild pain'. We judged the quality of evidence for this outcome to be very low. We downgraded the quality of evidence twice for very serious limitations to study quality due to high risk of performance and detection bias, and once for imprecision due to wide 95% CI.
Participant‐reported pain relief
No study reported this outcome.
Secondary outcomes
Any pain‐related outcome
For this outcome, we found only one relevant study (Wang 2016) that reported data for number of participants showing 'no clinical response'. We did not observe clear differences between the compared groups (n = 60; RR 0.40, 95% CI 0.14 to 1.14; NNTB = 5; Table 4). We judged the quality of evidence for this outcome to be very low. We downgraded the quality of evidence twice for very serious limitations to study quality due to high risk of performance and detection bias, and once for imprecision due to wide 95% CI.
Withdrawals due to lack of efficacy, adverse events, and for any cause
For this outcome, we found only one relevant study (Han 2017). There was no clear differences on withdrawals due to any cause when comparing acupuncture combined with other active therapy versus other active therapy used alone (n = 104; RR 1.00, 95% CI 0.21 to 4.73; Table 4). We judged the quality of evidence for this outcome to be very low. We downgraded the quality of evidence twice for very serious limitations to study quality due to high risk of performance and detection bias, and once for imprecision due to wide 95% CI.
Participants experiencing any adverse event
No study reported this outcome.
Participants experiencing any serious adverse event
No study reported this outcome.
Specific adverse events, particularly somnolence and dizziness
No study reported this outcome.
Quality of life
One study (Han 2017) reported quality of life (the nervous system symptoms) assessed by Functional Assessment of Cancer Therapy/Gynaecologic Oncology Group/ Neurotoxicity (FACT/the GOG‐Ntx) questionnaire scores. Results showed that quality of life improved in the manual‐acupuncture combined with mecobalamin group compared with the mecobalamin‐alone group (n = 104; MD ‐2.19, 95% CI ‐2.39 to ‐1.99; Table 3). We judged the quality of evidence for this outcome to be low. We downgraded the quality of evidence twice for very serious limitations to study quality due to high risk of performance and detection bias.
We did not perform subgroup analysis or sensitivity analysis in this comparison due to insufficient data.
Assessment of reporting biases
None of the comparisons included 10 studies reporting the same outcome, so we did not produce a funnel plot to assess the reporting biases.
Discussion
Summary of main results
When acupuncture was compared with sham acupuncture for neuropathic pain in adults, this review identified limited data with very low‐quality evidence on pain intensity and quality of life, which showed no clear difference between groups (one study; summary of findings Table for the main comparison). The average VAS score of the manual acupuncture and sham acupuncture groups was 5.8 and 6.2 respectively, indicating that neither group achieved 'no worse than mild pain'. Evidence was not available on pain relief, serious adverse events or other pre‐defined secondary outcomes.
We did not find any study comparing acupuncture with treatment as usual.
When acupuncture alone was compared with other active therapy (mecobalamin combined with nimodipine, inositol), the manual acupuncture group had fewer participants with 'no clinical response' than those using mecobalamin combined with nimodipine, or inositol. Evidence was not available for primary outcomes or the remaining secondary outcomes.
When investigating acupuncture combined with other active therapy versus other active therapy used alone (mecobalamin, and Xiaoke bitong capsule), we found that participants who received the combination therapy had a lower VAS score on pain intensity and improved quality of life, than those who received other active therapy alone. However, the average VAS score of the acupuncture and control groups was 3.23 and 4.25 respectively, indicating that neither group achieved 'no worse than mild pain'. Furthermore, the evidence was obtained from a study with high risk of bias and a very small sample size (n = 104). There was no evidence about pain relief. We found no clear differences between groups on the remaining parameters, including 'no clinical response' withdrawals. However, we found no evidence about adverse events.
In general, no clear benefits or harms of acupuncture in neuropathic pain in adults were discernible due to the lack of robust evidence. Five studies are still ongoing and seven studies are awaiting classification due to unclear treatment duration, and the results of these studies may influence the current findings.
Overall completeness and applicability of evidence
Overall, the evidence is incomplete from several angles, including the participants, the interventions and the outcomes. All included participants were aged between 52 and 63 years (on average), and diagnosed with peripheral neuropathic pain; 77% of the participants were diagnosed with diabetic peripheral neuropathy, hence limiting the applicability of the findings. In terms of interventions, all included studies used manual acupuncture. Furthermore, other acupuncture techniques (such as EA, warm needling, fire needling) were not identified. Evidence for acupuncture compared with usual treatment was also lacking.
Most of the included studies did not report either or both of our two primary outcomes: no worse than mild pain and participant‐reported pain relief.
Five of the six studies were conducted in China, where acupuncture is more frequently practiced and culturally recognised than in other countries, hence this may further limit the applicability of the findings.
Quality of the evidence
Overall, the quality of the evidence is very low, downgraded for study limitations (high risk of performance, detection and attrition bias, and high risk of bias confounded by small study size) or imprecision. All included studies except Garrow 2014 had high‐risk of performance bias due to insufficient blinding of participants and personnel; as most of the outcomes were self‐reported (assessed by participants), detection bias is also high. The only study rated as low risk of detection bias stated that the participants were blinded (Garrow 2014). Five included studies had small sample sizes (fewer than 50 participants per treatment arm), and one study had high risk of attrition bias. Most studies did not clearly describe the method of random sequence generation and allocation concealment. We identified potential reporting bias as we were unable to obtain the protocols for many of the included studies. The quality of the evidence for most outcomes was compromised by small sample size and imprecise summary effects. We have very little confidence in the effect estimate and the true effect is likely to be substantially different from the estimate of effect.
Potential biases in the review process
We developed comprehensive search strategies and performed the search using both Chinese and English databases. However, we only included published data so it is possible that there is publication bias. Two reviewers screened studies and extracted the data independently, and it is less likely that this process could have introduced bias.
Agreements and disagreements with other studies or reviews
A previous systematic review assessed the effectiveness of complementary therapies for neuropathic and neuralgic pain (Pittler 2008) and found that the evidence was not sufficient to address whether acupuncture can relieve neuropathic or neuralgic pain. Two additional systematic reviews explored acupuncture for trigeminal neuralgia (TN) (Liu 2010) and post‐stroke shoulder pain (Lee 2016), respectively. Both reviews found that acupuncture had some effect for pain, however, the study duration was not limited in these reviews and the length of included studies in Lee 2016 was less than eight weeks. The authors found that all the eligible studies were of low quality and the results were inconclusive. The present review has very little evidence concerning acupuncture in neuropathic pain, and reached a similar conclusion to these previous reviews.

Study flow diagram
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study

Comparison 1 Acupuncture alone versus other active therapy, Outcome 1 Any pain‐related outcomes: no clinical response ‐ defined by original study.
| Acupuncture versus sham acupuncture for neuropathic pain in adults | ||||||
| Patient or population: adults with neuropathic pain Comparison: sham acupuncture | ||||||
| Outcomes | Sham acupuncture | Acupuncture | Relative effect | No of participants | Quality of the evidence | Comments |
| Participant‐reported pain intensity | Mean 6.2 | Mean 5.8 | The mean participant‐reported pain intensity in the intervention group was | 45 | ⊕⊝⊝⊝ | Acupuncture has no clinical significant beneficial effects on pain intensity compared to sham acupuncture. |
| Participant‐reported pain relief substantial (at least 50% pain relief over baseline) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participants experiencing any serious adverse event | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Quality of life | Mean 27.7 | Mean 37.7 | The mean bodily pain component of quality of life in the intervention groups was 10 higher | 45 | ⊕⊝⊝⊝ | Acupuncture has no beneficial effects on bodily pain compared to sham acupuncture. |
| CI: confidence interval; MD: mean difference; SF‐36: Short Form (36) Health Survey (SF‐36); VAS: visual analogue scale | ||||||
| GRADE Working Group grades of evidence | ||||||
| aGarrow 2014 recruited 59 participants initially; there were 14 withdrawals and only the 45 participants that completed treatment were included in the study's final results. | ||||||
| Acupuncture versus treatment as usual for neuropathic pain in adults | ||||||
| Patient or population: adults with neuropathic pain Comparison: treatment as usual | ||||||
| Outcomes | Sham acupuncture | Acupuncture | Relative effect (Not applicable) | No of participants | Quality of the evidence | Comments |
| Participant‐reported pain intensity | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participant‐reported pain relief | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participants experiencing any serious adverse event | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Quality of life | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| GRADE Working Group grades of evidence | ||||||
| Acupuncture versus other active therapy for neuropathic pain in adults | ||||||
| Patient or population: adults with neuropathic pain Comparison: other active therapy | ||||||
| Outcomes | Sham acupuncture | Acupuncture | Relative effect (Not applicable) | No of Participants | Quality of the evidence | Comments |
| Participant‐reported pain intensity | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participant‐reported pain relief | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participants experiencing any serious adverse event | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Quality of life | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| GRADE Working Group grades of evidence | ||||||
| Acupuncture combined with other active therapy versus other active therapy for neuropathic pain in adults | ||||||
| Patient or population: adults with neuropathic pain Comparison: other active therapy alone | ||||||
| Outcomes | Other active therapy | Acupuncture combined with other active therapy | Relative effect | No of participants | Quality of the evidence | Comments |
| Participant‐reported pain intensity | Mean 4.25 | Mean 3.23 | The mean participant‐reported pain intensity in the intervention groups was | 104 | ⊕⊝⊝⊝ | Acupuncture combined other active therapy has no clinical significant beneficial effects on pain intensity compared to other active therapy alone. |
| Participant‐reported pain relief substantial (at least 50% pain relief over baseline) | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Participants experiencing any serious adverse event | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported this outcome so no evidence to support or refute benefits of intervention. |
| Quality of life | Mean 35.17 | Mean 32.98 | The mean bodily pain component of quality of life in the intervention groups was 2.19lower | 104 | ⊕⊕⊝⊝ | Acupuncture combined other active therapy improved the quality of life compared to other active therapy alone. |
| CI: confidence interval; FACT/the GOG‐Ntx: Functional Assessment of Cancer Therapy/Gynaecologic Oncology Group/Neurotoxicity; MD: mean difference; VAS: Visual Analogue Scale | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded twice for study limitations (risk of bias) due to high risk of performance and detection bias. | ||||||
| Acupuncture points used | Study ID |
| Taixi (KI3); Hegu (LI4); Taichong (LR3); Sanyinjiao (SP6); Zusanli (ST36) | |
| Shenmai (B62); Zulinqi (GB41); Zhaohai (K6); Lieque (L7); Neiguan (P6); Houxi (SI3); Waiguan (SJ5); Gongsun (SP4) | |
| Feishu (BL13); Geshu (BL17); Feiyang (BL58); Zulinqi (GB41); Zhiyang (GV9); Shendao (GV11); Shenzhu (GV12); Dazhui (GV14); Taichong (LR3); Sanyinjiao (SP6); Xuehai (SP10); Tianshu (ST25); Zusanli (ST36); Xiangu (ST43) | |
| The main points: Huantiao (GB30); Yanglingquan (GB34); Sanyinjiao (SP6); Zusanli (ST36); The auxiliary points (selected 2‐3from following): Shenshu (BL23); Kunlun (BL60); Guanyuan (CV4); Qihai (CV6); Huantiao (GB30); Taixi (K3); Taichong (LIV3); Pishu (PL20) | |
| The main points: Ganshu (BL18); Pishu (BL20); Shenshu (BL23); Yishu; Feishu (BL58); Zusanli (ST36); Sanyinjiao (SP6), Taibai (SP3); Zutonggu; Qihai (CV6); Guanyuan (CV4); Fenglong(ST40) and Yanglingquan (GB34); The auxiliary points: Jianyu (LI15); Quchi (LI11); Shousanli (LI10); Hegu (LI4); Biguan (ST31); Futu (ST32); Liangqiu (ST34); Xiangu (ST43) and Neiting (ST 44); Added for blood stasis points: Geshu (BL17) and Xuehai (SP10); Added for severe numbness of the hands and feet points: Bafeng(EX‐LE10) and Baxie (EX‐UE9). |
| Outcomes | Scales | Description of scales | Relevant Studies |
| Participant‐reported pain intensity | Visual Analogue Scale (VAS) | The VAS is a visual analogue scale for pain intensity, in which 0 means no pain and 10 (or 100) means the worst pain ever experienced. | |
| Quality of life | Short Form (36) Health Survey (SF‐36) | The SF‐36 is a 36‐item, patient‐reported survey of patient health and consists of 8 scaled scores, which are the weighted sums of the questions in their section. Each scale is directly transformed into a 0‐100 scale on the assumption that each question carries equal weight. The lower the score, the more disability. The 8 sections are: vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning and mental health. Summary scores for the SF‐12, version 2 (SF‐12v2) health status measure are based on scoring coefficients derived for version 1 of the SF‐36. The higher score is better. | |
| Functional Assessment | The FACT/GOG‐Ntx questionnaire is used to investigate patients' daily activities and evaluate the degree of neuropathy. The questionnaire includes 7 questions about physical well‐being, 7 questions about social/family well‐being, 6 questions about emotional well‐being, 7 questions about functional well‐being and 9 questions about additional concerns. Where in each question, 0 = not at all and 4 = very much, lower is better. |
| Acupuncture versus sham acupuncture | ||||||||||
| Outcome | Specific measurement | Study | Manual acupuncture group | Sham acupuncture group | Effect measure | Statistical test | ||||
| Mean | SD | Total | Mean | SD | Total | MD (95%CI) | P value | |||
| Pain intensity | VASa | 5.8 | 2.6 | 24 | 6.2 | 2.3 | 21 | ‐0.40 (‐1.83 to 1.03) | 0.58 | |
| Quality of life | SF‐36b: physical health score | 31.9 | 9.2 | 24 | 32.1 | 9.8 | 21 | ‐0.20 (‐5.78 to 5.38) | 0.94 | |
| SF‐36: mental health score | 39.2 | 14 | 24 | 35.7 | 12.6 | 21 | 3.50 (‐4.17 to 11.27) | 0.38 | ||
| SF‐36: bodily pain score | 37.7 | 27.4 | 24 | 27.7 | 16.9 | 21 | 10.00 (‐3.13 to 23.13) | 0.14 | ||
| Acupuncture + other active therapies versus other active therapies | ||||||||||
| Outcome | Specific measurement | Study | Acupuncture + other active therapies group | Other active therapies group | Effect measure | Statistical test | ||||
| Mean | SD | Total | Mean | SD | Total | MD (95%CI) | P value | |||
| Pain intensity | VAS | 3.23 | 0.17 | 52 | 4.25 | 0.197 | 52 | ‐1.02 (‐1.09 to ‐0.95) | < 0.00001 | |
| Quality of life | FACT/the GOG‐Ntxc | 32.98 | 0.542 | 52 | 35.17 | 0.518 | 52 | ‐2.19 (‐2.39 to ‐1.99) | < 0.00001 | |
| MD: mean difference; SD: standard deviation | ||||||||||
| Acupuncture versus sham acupuncture | ||||||||
| Outcome | Study | Manual acupuncture group | Sham acupuncture group | Effect measure | Statistical test | |||
| Events | Total | Events | Total | RR (95%CI) | NNTB | P value | ||
| Withdraw from trial due to any cause | 4 | 28 | 10 | 31 | 0.44 (0.16 to 1.25) | NNTB = 6 | 0.53 | |
| Adverse events: any cases | 1 | 28 | 2 | 31 | 0.55 (0.05 to 5.78) | NNTB = 34 | 0.62 | |
| Acupuncture + other active therapies versus other active therapies | ||||||||
| Outcome | Study | Acupuncture + other active therapies group | Other active therapies group | Effect measure | Statistical test | |||
| Events | Total | Events | Total | RR (95%CI) | NNT | P value | ||
| Any pain‐related outcomes: no clinical response | 4 | 30 | 10 | 30 | 0.40 (0.14 to 1.14) | NNTB = 5 | 0.09 | |
| Withdraw from trial due to any cause | 3 | 52 | 3 | 52 | 1.00 (0.21 to 4.73) | NA | 1.00 | |
| NA: not applicable; NNTB: number needed to treat for an additional beneficial outcome; RR: risk ratio | ||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Any pain‐related outcomes: no clinical response ‐ defined by original study Show forest plot | 3 | 209 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.12, 0.51] |

