Estimulación magnética periférica repetitiva para el deterioro y la discapacidad en personas después de un accidente cerebrovascular
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Study characteristics | ||
| Methods | Study design: RCT Study grouping: parallel group | |
| Participants | Inclusion criteria: chronic unilateral, first‐ever stroke more than 12 months before the start of the study. Participants with stroke presented with paretic ankle muscles with spasticity (medical records), had a CT or MRI scan taken within the previous 5 years, and were able to walk independently (i.e. with no physical assistance) more than 10 m with or without an assistive device. Exclusion criteria: use of antispastic medication; past vertebral surgery; major circulatory, respiratory, or cardiac disease; neurological disease/deficit other than stroke; severe lower limb orthopaedic condition; or cognitive disorder Baseline characteristics Active rPMS (n = 9)
Sham rPMS (n = 9)
Baseline comparability between 2 groups: rPMS group was earlier from onset than sham group Loss to follow‐up: 0% | |
| Interventions | Intervention characteristics Active rPMS
Sham rPMS
Sham stimulation was applied using the same parameters but at a very low intensity. | |
| Outcomes | Muscle strength: dorsiflexion strength (kg)
| |
| Identification | Sponsorship source: Canadian Foundation for Innovation (CS) and studentships from the Fondsde la Recherche en Sante du Quebec (LDB, HMA) and the Canadian Institutes for Health Research (LDB, HMA) Country: Canada Setting: n/a Authors' names: Louis‐David Beaulieu, Hugo Masse‐Alarie, Brenda Brouwer, Cyril Schneider Institution: Laboratoire de Neurostimulation et Neurosciences Cliniques Email: [email protected] Address: Centre de recherche du CHU de Quebec, Axe Neurosciences RC‐9800, 2705 Boulevard Laurier, Quebec, QC G1V 4G2, Canada | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Low risk | To ensure blinding, all participants were informed at enrolment that they could receive real rPMS or sham stimulation over the paretic lower limb, but they were not provided with information about the location of the coil nor sensations induced by stimulation. |
| Blinding of outcome assessment (detection bias) | Low risk | Experimenters performing pre‐intervention and postintervention measures and analysis had to leave the room during the intervention, and remained blind to group allocation during the experiments and to times of measurement during analysis (i.e. pre‐intervention or postintervention) until completion of analyses. |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up 0% |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available. |
| Other bias | Low risk | No other biases |
| Study characteristics | ||
| Methods | Study design: RCT Study grouping: parallel group | |
| Participants | Inclusion criteria: hemiparesis caused by stroke or traumatic brain injury; spasticity of an upper extremity, with a score of 1 to 3 on the Tardieu Scale; age between 18 and 75 years Exclusion criteria: metal implant in the head or within the stimulation area; medically implanted device (cardiac pacemaker, cochlear implant, or medication pump); pregnancy; comorbidity with other neurodegenerative disorders or other neurological or orthopaedic disorders; increased intracranial pressure; unstable fracture of the paretic upper extremity Baseline characteristics Active rPMS plus rehabilitation (n = 31)
Sham rPMS plus rehabilitation (n = 32)
Baseline comparability between groups: only rPMS group included traumatic brain injury; rPMS group earlier from onset than sham group Loss to follow‐up: 0.05%; ITT analysis performed | |
| Interventions | Intervention characteristics Active rPMS plus rehabilitation
Sham rPMS plus rehabilitation
| |
| Outcomes | Activities of daily living: Barthel Index (scores range from 0 to 100)
Upper limb function: Fugl‐Meyer Assessment (scores range from 0 to 66)
Spasticity: Modified Tardieu Scale of elbow and wrist (scores range from 0 to 5)
| |
| Identification | Sponsorship source: n/a Country: Germany Setting: neurological rehabilitation hospital Authors' names: Carmen Krewer, Sandra Hartl, Friedemann Muller, Eberhard Koenig Institution: Schoen Klinik Bad Aibling, Motor Research Department, Bad Aibling, Germany Email: CKrewer@schoen‐kliniken.de Address: Schoen Klinik Bad Aibling, Kolbermoorer Strasse 72, D‐83043 Bad Aibling, Germany | |
| Notes |
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Low risk | Randomised allocation was done by an individual not involved in any other aspect of the study. |
| Blinding of participants and personnel (performance bias) | Low risk | Active coil makes typical discharge noises. Blinding of participants and personnel was sufficient. |
| Blinding of outcome assessment (detection bias) | Low risk | Trained therapists, blinded for treatment allocation, assessed each participant. |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up 5%; no differences in reasons for missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available. |
| Other bias | Low risk | No other biases |
| Study characteristics | ||
| Methods | Study design: cross‐over trial | |
| Participants | Inclusion criteria: single history of CNS lesion due to stroke or traumatic brain injury; lesion interval > 12 months; increased muscle tone, i.e. 1, 2, 3, or 4 on the Modified Ashworth Score (0 to 5) in affected wrist or finger joints; no volitional distal motor function of the affected arm, except for mass flexion; no metal implants or open wounds in the stimulation area; no deep vein thrombosis; no relevant oedema; no pacemaker; no preceding botulinum toxin injection within previous 6 months; signed written informed consent (approved by local ethics committee) Exclusion criteria: n/a Baseline characteristics Group 1 (active rPMS plus rehabilitation, sham rPMS plus rehabilitation) (n = 20)
Group 2 (sham rPMS plus rehabilitation, active rPMS plus rehabilitation) (n = 20)
Baseline comparability between groups: group 1 was younger than group 2 Loss to follow‐up: 0% | |
| Interventions | Intervention characteristics Active rPMS plus rehabilitation
Sham rPMS plus rehabilitation
| |
| Outcomes | Spasticity: Modified Ashworth Score of wrist and finger (scores range from 0 to 4)
| |
| Identification | Sponsorship source: n/a Country: Germany Setting: n/a Comments: Verein zur Förderung der Hirnforschung und Rehabilitation, e.V., Berlin Authors' names: Werner C, Schrader M, Wernicke S, Bryl B, Hesse S Institution: Medical Park Berlin Humboldtmühle, Neurological Rehabilitation, Charité, University Medicine Berlin, Germany Email: [email protected] Address: Medical Park Berlin Charité – University Medicine Berlin An der Mühle 2‐9, Berlin 13507, Germany | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was conducted with the help of a computer‐generated lot (www.randomizer.at). |
| Allocation concealment (selection bias) | Low risk | Before start of therapy, the subinvestigator of the study attached the rPMS or sham coil according to group assignment. |
| Blinding of participants and personnel (performance bias) | Low risk | This study used a sham coil delivered with an atypical clicking sound. Therapists who applied stimulation and muscle stretch were not aware of whether the coil used was the one intended for rPMS or sham. |
| Blinding of outcome assessment (detection bias) | Low risk | A rater, blinded to treatment allocation, assessed participants. |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up 0% |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available. |
| Other bias | Low risk | No other biases |
| Study characteristics | ||
| Methods | Study design: RCT Study grouping: parallel group | |
| Participants | 18 participants after stroke with spastic hemiparesis (mean age 60.8 years; 9 women, 9 men; 3 to 12 months after stroke) | |
| Interventions | Intervention characteristics Active rPMS
Sham rPMS
| |
| Outcomes | Upper limb function: angle of motion for hand extension and hand flexion (degree)
Upper limb function: Action Research Arm Test (scores range from 0 to 57 points)
Upper limb function: Bard and Hirschberg Score
Spasticity: Ashworth Score (scores range from 0 to 4)
Spasticity: Gerstenbrand Spasticity Rating Scale
| |
| Identification | Sponsorship source: n/a Country: Austria Setting: n/a Authors' names: Zifko UA, Morph M, Diem K, Havel PM, Struppler A Institution: Rehabilitationsklinik Pirawarth, Bad Pirawarth, Austria Email: n/a Address: n/a | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) | Unclear risk | The abstract states "double‐blind study". However, there was no information on blinding for personnel. |
| Blinding of outcome assessment (detection bias) | Low risk | The abstract states "double‐blind study". |
| Incomplete outcome data (attrition bias) | Unclear risk | Loss to follow‐up 11% |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available. |
| Other bias | Low risk | No other biases |
CNS: central nervous system
CT: computed tomography
ITT: intention‐to‐treat
MRI: magnetic resonance imaging
n/a: not applicable
RCT: randomised controlled trial
rPMS: repetitive peripheral magnetic stimulation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Unsuitable study design | |
| Unsuitable study design | |
| Unsuitable outcomes | |
| Insufficient information | |
| Unsuitable outcomes | |
| Unsuitable outcomes | |
| Unsuitable outcomes | |
| Unsuitable study design | |
| Unsuitable intervention | |
| Unsuitable study design | |
| Unsuitable study design | |
| Insufficient information |
Characteristics of studies awaiting classification [ordered by study ID]
| Methods | Unknown |
| Participants | Participants with stroke |
| Interventions | Low‐frequency magnetic fields |
| Outcomes | Spasticity |
| Notes |
| Methods | Comparative study |
| Participants | 42 participants with stroke (mean age 64 ± 1.0 years) |
| Interventions | 10 daily sessions of 1 Hz repetitive transcranial magnetic stimulation and repetitive peripheral magnetic stimulation |
| Outcomes | Motor Club Assessment Scale |
| Notes |
| Methods | Comparative study |
| Participants | 121 participants with ischaemic stroke in the acute period |
| Interventions | Technique of frequency‐modulated magnetolaser therapy |
| Outcomes | n/a |
| Notes |
n/a: not applicable
Characteristics of ongoing studies [ordered by study ID]
| Study name | The effects of repetitive peripheral magnetic stimulation on motor function and spasticity in patients with hemiparesis |
| Methods | RCT |
| Participants | Stroke, not specified as haemorrhage or infarction |
| Interventions | 20‐minute therapy sessions of rPMS plus an additional 20 minutes of occupational therapy, 2 times a day, 5 times a week, for 2 weeks vs sham stimulation |
| Outcomes | Primary outcome: function and spasticity of the paretic upper extremity. The Fugl‐Mayer assessment is used to assess function, and the Tardieu scale to assess spasticity. |
| Starting date | 21 April 2007 |
| Contact information | Eberhard Koenig, Schön Klinik Bad Aibling, Kolbermoorer Str. 72 83043 Bad Aibling, Germany |
| Notes | DRKS00000798 This trial was registered retrospectively. |
| Study name | The effect of repetitive peripheral magnetic stimulation in stroke‐rehabilitation: a randomised controlled trial |
| Methods | RCT |
| Participants | Inclusion criteria: subacute stroke (occurred no longer than 6 months previously); spastic hemiparesis of the upper limb (at least Modified Ashworth Scale 1); slight function in the fingers or hand (at least 1 point on the Fugl‐Meyer Test in subscore C) Exclusion criteria: epilepsy, implanted metal in the stimulation area, implanted medical devices, dysfunctional speech comprehension, pregnancy |
| Interventions | Stimulation intensity is adjusted individually for each participant, so that a joint movement results from the muscle contraction. Muscles of the upper arm and forearm are stimulated with a butterfly coil; the participant takes a sitting position with raised feet in the wheelchair or on a chair with backrest; the arm is placed to be stimulated or maintained by the therapist. |
| Outcomes | Primary outcome: group difference in the Fugl‐Meyer score 3 weeks poststimulation Secondary outcome: group difference in the Katz Index of Independence Activities of Daily Living Scale score after 6 months |
| Starting date | 23 September 2014 |
| Contact information | Kristin Pohl, Moritz Klinik Bad Klosterlausnitz, Hermann‐Sachse‐Strasse 46 07639 Bad Klosterlausnitz, Germany Email: kristin.pohl@moritz‐klinik.de |
| Notes | DRK00007722 |
| Study name | The effects of repetitive peripheral magnetic stimulation in patient with spastic hemiparesis after stroke: a randomised‐controlled study |
| Methods | RCT |
| Participants | Inclusion criteria: subacute stroke (occurred no longer than 6 months previously); spastic hemiparesis of the upper limb (at least Modified Ashworth Scale 1); slight function in the fingers or hand (at least 1 point on the Fugl‐Meyer Test in subscore C) Exclusion criteria: epilepsy, implanted metal in the stimulation area, implanted medical devices, dysfunctional speech comprehension, pregnancy |
| Interventions | Stimulation is 15 minutes daily for 3 weeks for a total of 15 sessions. Stimulation intensity is adjusted individually for each participant, so that a joint movement results from the muscle contraction. Muscles of the upper arm and forearm are stimulated with a butterfly coil. Participant takes a sitting position with raised feet in a wheelchair or on a chair with a backrest. The arm is then placed to be stimulated or maintained by the therapist. |
| Outcomes | Primary outcome: Fugl‐Meyer Test of the upper extremity, a test that evaluated the function of the affected upper extremity. This test will be performed directly after the end of the 3 weeks of intervention/control intervention. Secondary outcome: Katz Index of Independence Activities of Daily Living questionnaire. This questionnaire aims to identify dependence on performance of activities of daily living and will be performed 6 months after the end of the intervention/control intervention. |
| Starting date | 15 April 2015 |
| Contact information | Kristin Pohl, Moritz Klinik Bad Klosterlausnitz, Hermann‐Sachse‐Strasse 46 07639 Bad Klosterlausnitz, Germany Email: kristin.pohl@moritz‐klinik.de |
| Notes | DRKS00007899 |
| Study name | Dose–response of rPMS for upper limb hemiparesis after stroke |
| Methods | This is a multicentre, prospective, assessor‐blinded, dose–response RCT with 3 parallel groups. Study will be conducted from 20 January 2020 to 30 September 2022. This trial aims to clarify the dose–response of rPMS therapy when combined with intensive OT in chronic stroke patients with moderate to severe upper limb hemiparesis. 2 hospitals (the Jikei University Hospital and the Jikei University Daisan Hospital) have been registered as study sites. |
| Participants | Neither the patients nor the public were directly involved in the study design, patient recruitment, or conduct of the study. The obtained results will contribute to better clinical outcomes for stroke patients with upper limb hemiparesis. |
| Interventions | Eligible participants who provide written informed consent will be randomly assigned at a ratio of 1:2:2 to the control group, the group receiving 2400 daily pulses of rPMS (2400 pulses group), or the group receiving 4800 daily pulses of rPMS (4800 pulses group), respectively. Participants will be randomly assigned using a computer‐generated list of random numbers using blocked randomisation, and stratified by the Fugl Meyer Assessment (FMA) (< 20 or ≥ 20) and age (< 65 or ≥ 65 years old). The study researcher will report to the allocator by phone, and the assignment will then be reported to the investigator. The block sizes will not be disclosed to ensure allocation concealment. rPMS therapy and intensive OT will be initiated from the day after admission (Day 1). The evaluation will be conducted on Day 14, after 2 weeks of therapy. After the evaluation, the therapy will be repeated for another 2 weeks (Days 15 to 28). For the control group, 4800 pulses of rPMS therapy will be performed for relief measures after the evaluation (Day 14). Another evaluation will be conducted 2 weeks after therapy (Day 28). Participants will be discharged on Day 28, after a total of 4 weeks of admission. In addition, the immediate effect of rPMS therapy will be assessed at the time of admission and the first session of rPMS therapy. The long‐term effect and safety of the rPMS therapy will be checked 4 weeks after discharge. |
| Outcomes | The evaluations will be conducted at 1 week before admission; on day of admission (Day 0); 1 day after admission (Day 1); 2 weeks after admission (Day 14); 4 weeks after admission (Day 28); at the point of discontinuation; and 4 weeks after discharge. The primary outcome of the study is the difference in upper limb motor function (FMA) between Day 0 and Day 14. The secondary outcomes are differences in spasticity, active range of motion, motor evoked potential (MEP), and activities of daily living during the study period. |
| Starting date | 26 February 2020 |
| Contact information | Kinoshita S, Ikeda K, Yasuno S, Takahashi S, Yamada N, Okuyama Y, Sasaki N, Hada T, Kuriyama C, Suzuki S, Hama M, Ozaki N, Watanabe S, Abo M |
| Notes | jRCTs032190191 |
| Study name | Immediate effect of simple magnetic stimulation for upper limb spasticity: a randomised‐controlled trial |
| Methods | RCT |
| Participants | Inclusion criteria: adults after stroke with Modified Ashworth Scale score of 1+ or more in the metacarpophalangeal joint, wrist, or elbow flexor muscles Exclusion criteria: unstable condition and/or patients who used cardiac pacemaker |
| Interventions | 15 minutes of magnetic stimulation for spastic muscles |
| Outcomes | Primary outcome: changes in spasticity evaluated by the Modified Ashworth Scale Secondary outcomes: Modified Ashworth Scale score and subjective symptoms of participants at 24 hours before, just before, just after, 1 hour after, 24 hours after stimulation |
| Starting date | 1 November 2018 |
| Contact information | Hitoshi Kagaya, Fujita Health University Hospital, 1‐98 Dengakugakubo, Kutsukake, Toyoake, Aichi, Japan Email: hkagaya2@fujita‐hu.ac.jp |
| Notes | jRCTs042180014 |
| Study name | Prevention of shoulder subluxation in stroke patients with magnetic stimulation: a randomized controlled trial (PSSMS‐RCT) |
| Methods | RCT |
| Participants | Patients with hemiplegia after stroke with stable general condition, and aged 20 or older who gave informed consent |
| Interventions | 6 weeks of magnetic stimulation in addition to usual training: 20 minutes stimulation per day, 5 days per week plus physical and occupational therapy |
| Outcomes | Changes in humeral head position by X‐ray examination after 6‐week intervention. Changes in motor function, joint range of motion, muscle strength, and pain |
| Starting date | 20 September 2018 |
| Contact information | Saitoh Eiichi |
| Notes | jRCTs042180043 |
| Study name | Repetitive peripheral magnetic stimulation for patients with hemiplegia |
| Methods | RCT |
| Participants | Inclusion criteria: cerebral hemisphere damage, people who could walk independently, Modified Rankin Scale between 0 and 2 before onset Exclusion criteria: severe dementia, people with contraindications outlined in the guidelines for repetitive transcranial magnetic stimulation |
| Interventions | Repetitive peripheral magnetic stimulation + standard physical therapy |
| Outcomes | Knee extension strength, evaluation time: at the time of starting physical therapy, 1 week later, 2 weeks later, 1 month later, 2 months later Stroke Impairment Assessment Set, 10‐metre walking speed, Functional Independence Measure, quadriceps muscle thickness, acceleration during walking, Berg Balance Scale, Timed Up and Go Test, biochemical blood test, number of days until gait reacquisition, hospitalisation |
| Starting date | 1 October 2015 |
| Contact information | Keita Suzuki, Kawasaki University of Medical Welfare, Department of Rehabilitation, 288 Matsushima, Kurashiki, Okayama, Japan Email: [email protected]‐m.ac.jp |
| Notes | UMIN000018750 |
| Study name | Effect of pairing peripheral and transcranial magnetic stimulations triggered by actual movement on motor plasticity |
| Methods | Cross‐over trial |
| Participants | Inclusion criteria: people with chronic stroke (more than 3 months after onset) who were inpatients and outpatients of Tohoku University Hospital Exclusion criteria: people with metal in cranium, trauma or operation of brain, intracardiac lines, increased intracranial pressure, pregnancy, childhood, heart disease, cardiac pacemaker, medication pump, tricyclic antidepressants, neuroleptics, febrile convulsion, epilepsy, family history of epilepsy |
| Interventions | Subthreshold peripheral and transcranial magnetic stimulations with actual movement |
| Outcomes | Direction of transcranial magnetic stimulation‐induced upper limb movement of the paretic side, excitability of corticospinal tract |
| Starting date | 1 October 2015 |
| Contact information | Akihiko Asao, Tohoku University Graduate School of Medicine, Department of Physical Medicine and Rehabilitation, 2‐1 Seiryo‐machi, Aoba‐ku, Sendai, Miyagi, Japan Email: [email protected] |
| Notes | UMIN000019106 |
| Study name | Prevention of shoulder subluxation in stroke patients with magnetic stimulation: a randomised controlled trial |
| Methods | RCT |
| Participants | Inclusion criteria: people with hemiplegia after stroke with stable general condition, aged 20 years or older Exclusion criteria: history of epilepsy, cardiac pacemaker, difficulty in sitting position over 40 minutes, magnetic materials near the stimulation site, distance between acromion and humeral head more than 1/2 fingerbreadth, inpatients expected to discharge within 6 weeks, pregnant women |
| Interventions | 6 weeks of magnetic stimulation in addition to usual training: 20 minutes of stimulation per day, 5 days per week, plus physical and occupational therapy |
| Outcomes | Primary outcome: changes in humeral head position by X‐ray examination after 6‐week intervention Secondary outcomes: changes in motor function, joint range of motion, muscle strength, pain |
| Starting date | 1 April 2018 |
| Contact information | Kenta Fujimura, Fujita Health University, Faculty of Rehabilitation, School of Health Sciences, 1‐98 Dengakugakubo, Kutsukake, Toyoake, Aichi, Japan Email: rehabmed@fujita‐hu.ac.jp |
| Notes | UMIN000031957 |
OT: occupational therapy
RCT: randomised controlled trial
rPMS: repetitive peripheral magnetic stimulation
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Muscle strength at the end of treatment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1: rPMS versus sham, Outcome 1: Muscle strength at the end of treatment | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Activities of daily living at the end of treatment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 1: Activities of daily living at the end of treatment | ||||
| 2.2 Activities of daily living at the end of follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.2  Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 2: Activities of daily living at the end of follow‐up | ||||
| 2.3 Upper limb function at the end of treatment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.3  Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 3: Upper limb function at the end of treatment | ||||
| 2.4 Upper limb function at the end of follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.4  Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 4: Upper limb function at the end of follow‐up | ||||
| 2.5 Spasticity of the elbow at the end of treatment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.5  Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 5: Spasticity of the elbow at the end of treatment | ||||
| 2.6 Spasticity of the elbow at the end of follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.6  Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 6: Spasticity of the elbow at the end of follow‐up | ||||
| 2.7 Spasticity of the wrist at the end of treatment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.7  Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 7: Spasticity of the wrist at the end of treatment | ||||
| 2.8 Spasticity of the wrist at the end of follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.8  Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 8: Spasticity of the wrist at the end of follow‐up | ||||
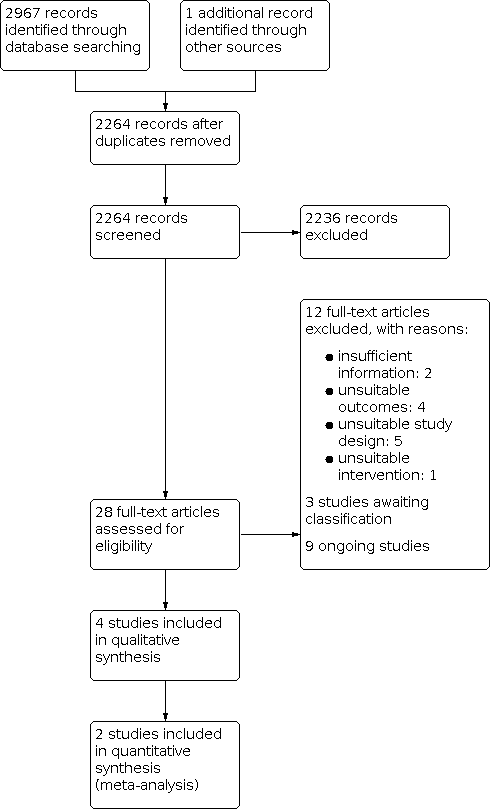
Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1: rPMS versus sham, Outcome 1: Muscle strength at the end of treatment

Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 1: Activities of daily living at the end of treatment

Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 2: Activities of daily living at the end of follow‐up

Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 3: Upper limb function at the end of treatment

Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 4: Upper limb function at the end of follow‐up

Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 5: Spasticity of the elbow at the end of treatment

Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 6: Spasticity of the elbow at the end of follow‐up

Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 7: Spasticity of the wrist at the end of treatment

Comparison 2: rPMS plus rehabilitation versus sham plus rehabilitation, Outcome 8: Spasticity of the wrist at the end of follow‐up
| Active rPMS only compared with sham rPMS in stroke | ||||||
| Patient or population: people with stroke Setting: not reported Intervention: active rPMS Comparison: sham rPMS | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with sham rPMS | Risk with rPMS | |||||
| Activities of daily living (ADLs) | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Upper limb function | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Lower limb function | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Spasticity (elbow) | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Spasticity (wrist) | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Muscle strength | Mean muscle strength 10.44 kg | MD 3 kg higher | ‐ | 18 | ⊕⊕⊝⊝ |
|
| Death | ‐ | ‐ | See comment | ‐ | ‐ | No trials reported this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; rPMS: repetitive peripheral magnetic stimulation. | ||||||
| GRADE Working Group grades of evidence | ||||||
| aOne study with small sample size; 95% CI overlaps zero. | ||||||
| Active rPMS only compared with no intervention in stroke | ||||||
| Patient or population: people with stroke Setting: not available Intervention: active rPMS Comparison: no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with no intervention | Risk with rPMS | |||||
| Activities of daily living (ADLs) | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Upper limb function | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Lower limb function | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Spasticity (elbow) | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Spasticity (wrist) | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Muscle strength | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Death | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI). CI: confidence interval; rPMS: repetitive peripheral magnetic stimulation. | ||||||
| GRADE Working Group grades of evidence | ||||||
| Active rPMS plus rehabilitation compared with sham rPMS plus rehabilitation in stroke | ||||||
| Patient or population: people with stroke Setting: neurological rehabilitation hospital Intervention: active rPMS plus rehabilitation Comparison: sham rPMS plus rehabilitation | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with sham rPMS plus rehabilitation | Risk with active rPMS plus rehabilitation | |||||
| Activities of daily living (ADLs) | Mean ADL score 50 | MD 3 lower (16.35 lower to 10.35 higher) | ‐ | 63 | ⊕⊕⊝⊝ |
|
| Upper limb function | Mean upper limb function score 13 | MD 2 higher | ‐ | 63 | ⊕⊕⊝⊝ |
|
| Lower limb function | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Spasticity (elbow) | Mean spasticity (elbow) score 1.41 | MD 0.41 lower | ‐ | 63 | ⊕⊕⊝⊝ |
|
| Spasticity (wrist) | Mean spasticity (wrist) score 2.13 | MD 0.2 lower | ‐ | 63 | ⊕⊕⊝⊝ |
|
| Muscle strength | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Death | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; rPMS: repetitive peripheral magnetic stimulation. | ||||||
| GRADE Working Group grades of evidence | ||||||
| aOne study with small sample size; 95% CI overlaps zero. | ||||||
| Active rPMS plus rehabilitation compared with rehabilitation only in stroke | ||||||
| Patient or population: people with stroke Setting: not available Intervention: active rPMS plus rehabilitation Comparison: rehabilitation only | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with rehabilitation only | Risk with active rPMS plus rehabilitation | |||||
| Activities of daily living (ADLs) | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Upper limb function | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Lower limb function | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Spasticity (elbow) | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Spasticity (wrist) | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Muscle strength | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| Death | ‐ | ‐ | See comment | ‐ | ‐ | No trials measured this outcome. |
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI). CI: confidence interval; rPMS: repetitive peripheral magnetic stimulation. | ||||||
| GRADE Working Group grades of evidence | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Muscle strength at the end of treatment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Activities of daily living at the end of treatment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.2 Activities of daily living at the end of follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.3 Upper limb function at the end of treatment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.4 Upper limb function at the end of follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.5 Spasticity of the elbow at the end of treatment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.6 Spasticity of the elbow at the end of follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.7 Spasticity of the wrist at the end of treatment Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.8 Spasticity of the wrist at the end of follow‐up Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |

