Ранняя аппендэктомия в сравнении с отсроченной при аппендикулярной флегмоне или абсцессе
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised controlled trial | |
| Participants | Country: India Study dates: from 1998 to 2001 Adults: not mentioned Appendiceal phlegmon: 60 (100%) Appendiceal abscess: 0 (0%) Participants with appendiceal mass determined on medical history, physical examination, and imaging results (e.g. ultrasonography, plain abdominal X‐ray) Exclusion criteria:
| |
| Interventions | Participants with appendiceal mass (N = 60) were randomly assigned to 3 groups Further details: open appendicectomy as soon as appendiceal mass resolved within the same admission Further details: initial conservative treatment followed by interval open appendicectomy 6 weeks later Group 3: conservative treatment without appendicectomy (n = 20).Group excluded from review | |
| Outcomes | Short‐term outcome measures (< 3 weeks): Operative time, operative difficulty, postoperative complications, length of hospital stay, and duration of time away from work. | |
| Notes | Funding source: no information provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no information provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) | High risk | Comment: it is not possible to blind the participants and healthcare providers unless sham surgery was provided, which may be unethical |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: no information provided |
| Incomplete outcome data (attrition bias) | Low risk | Comment: there were no postrandomisation dropouts |
| Selective reporting (reporting bias) | High risk | Comment: the trial protocol was not available. Some outcomes of interest in the review were not reported so that the trial was considered to be high risk of bias for selective reporting. |
| Differences in baseline characteristics | Low risk | Comment: there was no baseline imbalance in important characteristics. |
| Methods | Randomised controlled trial | |
| Participants | Country: USA Study dates: from 2006 to 2009 Adults: 0 (0%) Girls: 19 (47.5%) Appendiceal phlegmon: 0 (0%) Appendiceal abscess: 40 (100%) Inclusion criteria:
Exclusion criteria:
| |
| Interventions | Participants with appendiceal abscess (N = 40) were randomly assigned to 2 groups Further details: emergent (immediate) laparoscopic appendicectomy Group 2: delayed laparoscopic appendicectomy (n = 20) Further details: initial conservative treatment and percutaneous drainage of the abscess (when possible), followed by interval laparoscopic appendicectomy approximately 10 weeks later | |
| Outcomes | Mortality, total hospital stay, total hospital costs, and quality of life (Pediatric Quality of Life Scale‐Version 4.0) | |
| Notes | Funding source: no information provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no information provided |
| Allocation concealment (selection bias) | Unclear risk | Quote: "[t]he randomisation sequence was accessed to identify the next allotment" Comment: no information provided about the method of allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Comment: it is not possible to blind the participants and healthcare providers unless sham surgery was provided, which may be unethical |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: no information provided |
| Incomplete outcome data (attrition bias) | Low risk | Comment: there were no postrandomisation dropouts |
| Selective reporting (reporting bias) | Low risk | Comment: the study protocol is available. All of the study's pre‐specified outcomes were reported |
| Differences in baseline characteristics | Low risk | Comment: no baseline imbalance in important characteristics |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| A non‐randomised study | |
| A non‐randomised study | |
| Randomised controlled trial about perforated appendicitis without appendiceal abscess | |
| A non‐randomised study | |
| A non‐randomised study | |
| A non‐randomised study | |
| A non‐randomised study | |
| A non‐randomised study |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Overall morbidity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1 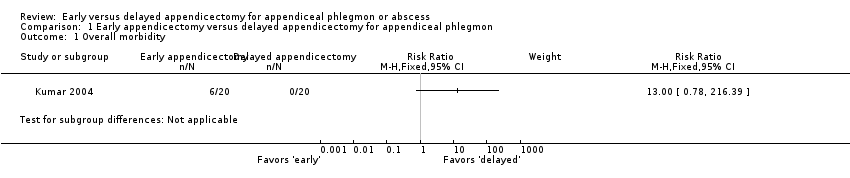 Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 1 Overall morbidity. | ||||
| 2 Wound infection Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 2 Wound infection. | ||||
| 3 Faecal fistula Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 3 Faecal fistula. | ||||
| 4 Total length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 4 Total length of hospital stay (days). | ||||
| 5 Time away from normal activities (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 5 Time away from normal activities (days). | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Early appendicectomy versus delayed appendicectomy for appendiceal abscess, Outcome 1 Total length of hospital stay (days). | ||||
| 2 Quality of life (score on a scale from 0‐100) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.2  Comparison 2 Early appendicectomy versus delayed appendicectomy for appendiceal abscess, Outcome 2 Quality of life (score on a scale from 0‐100). | ||||

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
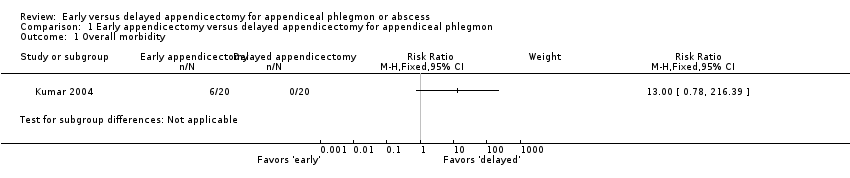
Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 1 Overall morbidity.

Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 2 Wound infection.
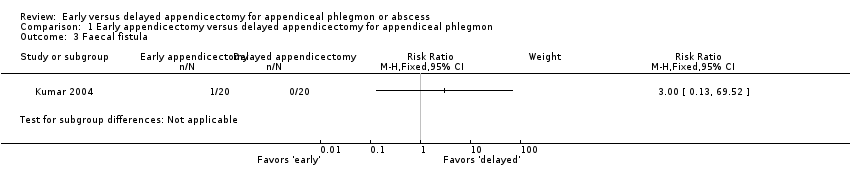
Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 3 Faecal fistula.

Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 4 Total length of hospital stay (days).
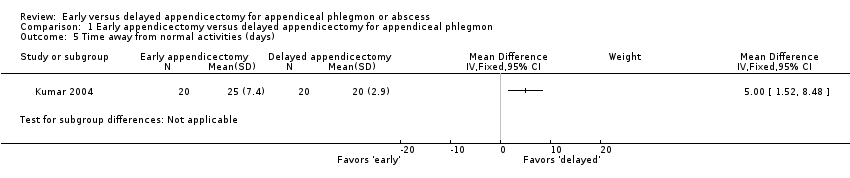
Comparison 1 Early appendicectomy versus delayed appendicectomy for appendiceal phlegmon, Outcome 5 Time away from normal activities (days).

Comparison 2 Early appendicectomy versus delayed appendicectomy for appendiceal abscess, Outcome 1 Total length of hospital stay (days).

Comparison 2 Early appendicectomy versus delayed appendicectomy for appendiceal abscess, Outcome 2 Quality of life (score on a scale from 0‐100).
| Early versus delayed open appendicectomy for appendiceal phlegmon | ||||||
| Patient or population: paediatric and adult patients with appendiceal phlegmon | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed appendicectomy | Early appendicectomy | |||||
| Overall morbidity Median follow‐up: 33,5 months | 0 per 1000 | 300 per 1000 | RR 13.00 | 40 | ⊕⊝⊝⊝ | — |
| Wound infection Median follow‐up: 33,5 months | 0 per 1000 | 200 per 1000 | RR 9.00 | 40 | ⊕⊝⊝⊝ | — |
| Faecal fistula Median follow‐up: 33,5 months | 0 per 1000 | 50 per 1000 | RR 3.00 | 40 | ⊕⊝⊝⊝ | — |
| Mortality Median follow‐up: 33,5 months | See comment | See comment | Not estimable | 40 | ⊕⊕⊝⊝ | There was no mortality in either group. |
| Total length of hospital stay (days) Follow‐up: 3 weeks | The mean total length of hospital stay in the delayed appendicectomy group was 14.7 days | The mean total length of hospital stay in the early appendicectomy group was 6.7 days higher | MD 6.70 (2.76 to 10.64) | 40 | ⊕⊝⊝⊝ | — |
| Time away from normal activities (days) Median follow‐up: 33,5 months | The mean time away from normal activities in the delayed appendicectomy group was 20 days | The mean time away from normal activities in the early appendicectomy group was 5 days higher | MD 5.00 (1.52 to 8.48) | 40 | ⊕⊝⊝⊝ | — |
| Quality of life Median follow‐up: 33,5 months | Not reported | |||||
| Pain (days) Follow‐up: 3 weeks | Not reported | |||||
| *The basis for the assumed risk was the control group proportion in the study. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded one level for serious risk of bias. | ||||||
| Early versus delayed laparoscopic appendicectomy for appendiceal abscess | ||||||
| Patient or population: paediatric participants with appendiceal abscess Setting: secondary and tertiary care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Delayed appendicectomy | Early appendicectomy | |||||
| Overall morbidity | Not reported | |||||
| Wound infection | Not reported | |||||
| Faecal fistula | Not reported | |||||
| Mortality Follow‐up: 12 weeks | See comment | See comment | Not estimable | 40 | ⊕⊝⊝⊝ | There was no mortality in either group. |
| Total length of hospital stay (days) Follow‐up: 12 weeks | The mean total length of hospital stay in the delayed appendicectomy group was 6.7 days | The mean total length of hospital stay in the early appendicectomy group was 0.2 days lower | MD −0.20 (−3.54 to 3.14) | 40 | ⊕⊝⊝⊝ | — |
| Time away from normal activities (days) | Not reported | |||||
| Quality of life (Pediatric Quality of Life Scale‐Version 4.0, a scale of 0 to 100 with higher values indicating better quality of life) Follow‐up: 12 weeks | The mean quality of life score in the delayed appendicectomy group was 84.37 points | The mean quality of life score in the early appendicectomy group was 12.40 points higher | MD 12.40 (9.78 to 15.02) | 40 | ⊕⊝⊝⊝ | We considered the observed mean difference in quality of life score to be clinically significant. |
| Pain (days) | Not reported | |||||
| *The basis for the assumed risk was the control group proportion in the study. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded two levels due to very serious imprecision (small sample size). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Overall morbidity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2 Wound infection Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Faecal fistula Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4 Total length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5 Time away from normal activities (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total length of hospital stay (days) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2 Quality of life (score on a scale from 0‐100) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |

