Видеоларингоскопия в сравнении с прямой ларингоскопией при интубации трахеи у детей (за исключением новорожденных)
Abstract
Background
Direct laryngoscopy is the method currently used for tracheal intubation in children. It occasionally offers unexpectedly poor laryngeal views. Indirect laryngoscopy involves visualizing the vocal cords by means other than obtaining a direct sight, with the potential to improve outcomes. We reviewed the current available literature and performed a meta‐analysis to compare direct versus indirect laryngoscopy, or videolaryngoscopy, with regards to efficacy and adverse effects.
Objectives
To assess the efficacy of indirect laryngoscopy, or videolaryngoscopy, versus direct laryngoscopy for intubation of children with regards to intubation time, number of attempts at intubation, and adverse haemodynamic responses to endotracheal intubation. We also assessed other adverse responses to intubation, such as trauma to oral, pharyngeal, and laryngeal structures, and we assessed vocal cord view scores.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and trial registers (www.clinicaltrials.gov and www.controlledtrials) in November 2015. We reran the search in January 2017. We added new studies of potential interest to a list of ‘Studies awaiting classification' and will incorporate them into formal review findings during the review update. We performed reference checking and citation searching and contacted the authors of unpublished data to ask for more information. We applied no language restrictions.
Selection criteria
We included only randomized controlled trials. Participants were children aged 28 days to 18 years. Investigators performed intubations using any type of indirect laryngoscopes, or videolaryngoscopes, versus direct laryngoscopes.
Data collection and analysis
We used Cochrane standard methodological procedures. Two review authors independently reviewed titles, extracted data, and assessed risk of bias.
Main results
We included 12 studies (803 children) in this review and meta‐analysis. We identified three studies that are awaiting classification and two ongoing studies.
Trial results show that a longer intubation time was required when indirect laryngoscopy, or videolaryngoscopy, was used instead of direct laryngoscopy (12 trials; n = 798; mean difference (MD) 5.49 seconds, 95% confidence interval (CI) 1.37 to 9.60; I2 = 90%; very low‐quality evidence). Researchers found no significant differences between direct and indirect laryngoscopy on assessment of success of the first attempt at intubation (11 trials; n = 749; risk ratio (RR) 0.96, 95% CI 0.91 to 1.02; I2 = 67%; low‐quality evidence) and observed that unsuccessful intubation (five trials; n = 263) was significantly increased in the indirect laryngoscopy, or videolaryngoscopy, group (RR 4.93, 95% CI 1.33 to 18.31; I2 = 0%; low‐quality evidence). Five studies reported the effect of intubation on oxygen saturation (n = 272; very low‐quality evidence). Five children had desaturation during intubation: one from the direct laryngoscopy group and four from the indirect laryngoscopy, or videolaryngoscopy, group.
Two studies (n = 100) reported other haemodynamic responses to intubation (very low‐quality evidence). One study reported a significant increase in heart rate five minutes after intubation in the indirect laryngoscopy group (P = 0.007); the other study found that the heart rate change in the direct laryngoscopy group was significantly less than the heart rate change in the indirect laryngoscopy, or videolaryngoscopy, group (P < 0.001). A total of five studies (n = 244; very low‐quality evidence) looked at evidence of trauma resulting from intubation. Investigators reported that only two children from the direct laryngoscopy group had trauma compared with no children in the indirect laryngoscopy, or videolaryngoscopy, group.
Use of indirect laryngoscopy, or videolaryngoscopy, improved the percentage of glottic opening (five trials; n = 256). Studies noted no significant difference in Cormack and Lehane score (C&L) grade 1 (three trials; n = 190; RR 1.06, 95% CI 0.93 to 1.21; I2 = 59%).
Authors' conclusions
Evidence suggests that indirect laryngoscopy, or videolaryngoscopy, leads to prolonged intubation time with an increased rate of intubation failure when compared with direct laryngoscopy (very low‐quality evidence due to imprecision, inconsistency, and study limitations). Review authors had difficulty reaching conclusions on adverse haemodynamic responses and other adverse effects of intubation, as only a few children were reported to have these outcomes. Use of indirect laryngoscopy, or videolaryngoscopy, might lead to improved vocal cord view, but marked heterogeneity between studies made it difficult for review authors to reach conclusions on this outcome.
PICO
Резюме на простом языке
Сравнение инструментов (устройств) с видеоподдержкой и без нее для интубации у детей
Актуальность
При необходимости общей анестезии детям иногда требуется ввести в горло специальную трубку. Этот процесс называется интубацией. К интубации прибегают также при чрезвычайных ситуациях – например, при травмах, сильном затруднении дыхания и сердечной недостаточности. Интубация обычно выполняется с помощью ларингоскопа, который позволяет приподнять язык для прямого обзора голосовых связок. Эта процедура называется прямой ларингоскопией. Непрямая ларингоскопия (видеоларингоскопия) выполняется с помощью новых устройств, которые показывают голосовые связки посредством видеокамеры, расположенной на кончике устройства.
Считается, что видеоларингоскопы (непрямые ларингоскопы) обеспечивают лучший обзор голосовых связок по сравнению с прямыми ларингоскопами. Однако пока остается неясным, облегчают ли они введение интубационной трубки.
Характеристика исследований
Мы изучили доказательства эффективности непрямой ларингоскопии (видеоларингоскопии) в сравнении с прямой ларингоскопией при интубации у детей в возрасте от 28 дней до 18 лет. Мы нашли 12 рандомизированных контролируемых испытаний (с участием 803 детей), соответствующих критериям включения. Доказательства актуальны на ноябрь 2015 года. Мы повторили поиск в январе 2017 года и при обновлении обзора включим еще 3 исследования, ожидающие классификации.
Основные результаты
Непрямая ларингоскопия (видеоларингоскопия) при интубации занимает больше времени и с большей вероятностью будет неудачной (доказательства очень низкого качества). Если первая попытка интубации была успешной, то существенной разницы между видео‐ и прямой ларингоскопией не наблюдалось (доказательства низкого качества). Лишь в нескольких исследованиях сообщали о влиянии интубации на возникновение неблагоприятных гемодинамических реакций, включая изменение кислородной сатурации и частоты сердечных сокращений, а также травм рта и трахеи. В связи с этим было трудно сделать вывод о неблагоприятном воздействии в целом (доказательства очень низкого качества). Непрямая ларингоскопия может обеспечивать лучший обзор голосовых связок.
Качество доказательств
Мы обнаружили существенные различия в результатах исследований, включенных в обзор, в частности – относительно оценки времени интубации, числа попыток интубации, числа неудачных интубаций, неблагоприятных эффектов, а также оценки обзора голосовых связок. Ни одно из включенных в обзор исследований не финансировалось производителем ларингоскопов, что снижает риск смещения. Качество исследований варьировало, и лишь некоторые из них отличались высоким качеством. В связи с этим качество доказательств в целом мы оценили как очень низкое.
Authors' conclusions
Summary of findings
| Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates) | ||||||
| Patient or population: tracheal intubation in children (excluding neonates) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with direct laryngoscopy | Risk with videolaryngoscopy | |||||
| Intubation time | Mean intubation time in the intervention group was 5.49 seconds higher (1.37 higher to 9.60 higher) | ‐ | 798 | ⊕⊝⊝⊝ | Risk of bias (unblinded), very serious heterogeneity (I2 = 90%), and clinically important increase not excluded | |
| Number of attempts at intubation and unsuccessful intubations | Study population | RR 0.96 | 749 | ⊕⊕⊝⊝ | Very serious heterogeneity (I2 = 67%) | |
| 26 per 1000 | 25 per 1000 | |||||
| Number of attempts at intubation and unsuccessful intubations | Study population | RR 4.93 | 263 | ⊕⊕⊝⊝ | Lack of blinding and no exclusion of a clinically trivial increase | |
| 37 per 1000 | 182 per 1000 | |||||
| Adverse haemodynamic response to endotracheal intubation | In 4 studies that reported occurrences of oxygen saturation < 95%, 5 cases happened in the videolaryngoscopy group and none in the direct laryngoscopy group. The fifth study shows a 97% mean saturation in the video group compared with 99% in the direct group | ‐ | 272 | ⊕⊝⊝⊝ | Very sparse data and serious concerns about unblinded reporting | |
| Adverse haemodynamic response to endotracheal intubation | One study reported a significant increase in heart rate after intubation with direct laryngoscopy, and the other study contradicted this and showed less of a change in heart rate in the direct group. A single study reported that systolic, diastolic, and mean arterial blood pressures were not significantly different between the 2 groups | ‐ | 100 | ⊕⊝⊝⊝ | Very sparse data and serious concerns about unblinded reporting | |
| Other adverse effects of intubation in children, including trauma to oral, pharyngeal, and laryngeal structures, assessed by visual or laryngoscopic examination | Only 2 children from the direct laryngoscopy group were reported to have evidence of trauma as a result of the intubation process compared with no children in the indirect laryngoscopy, or videolaryngoscopy, group | ‐ | 244 | ⊕⊝⊝⊝ | Very sparse data and serious concerns about unblinded reporting | |
| *Risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded three levels owing to serious concerns about study limitation, inconsistency, and indirectness bDowngraded two levels owing to serious inconsistency and study limitation cDowngraded two levels owing to serious imprecision and study limitation dDowngraded three levels owing to serious imprecision and serious inconsistency and study limitation eDowngraded three levels owing to study limitation and serious imprecision fDowngraded three levels owing to serious imprecision, study limitation, and inconsistency | ||||||
Background
Description of the condition
Airway management with or without tracheal intubation is a lifesaving procedure and is an important step in elective anaesthesia and cardiopulmonary resuscitation. It can, however, present a challenge, especially for the less experienced and non‐paediatric anaesthetist, as the paediatric airway is substantially different from the adult airway, and obstruction leads to rapid desaturation in small infants and children (Rasmussen 2009). In the operating theatre, tracheal intubation is usually applied after induction of anaesthesia to facilitate a secure airway in patients requiring neuromuscular paralysis and positive‐pressure ventilation (Zhao 2014).
A direct laryngoscope is the device most widely used to facilitate tracheal intubation (Scott 2009), but it is considered difficult to use by inexperienced personnel; it is reported that a 90% success rate requires 47 episodes of intubation practice (Mulcaster 2003). Problems with tracheal intubation were the most frequently recorded primary airway problem with difficult, delayed, and failed intubation, as were "can’t intubate can’t ventilate" scenarios (Woodall 2011).
Unfortunately, physical findings on examination of the airway discriminate poorly between potentially easy and difficult intubations (Shiga 2005), and direct laryngoscopy (DL) occasionally offers unexpectedly poor laryngeal views. Such difficulty, even if ultimately overcome, may result in multiple attempts at laryngoscopy and significant morbidity, such as desaturation, airway injuries, dental injuries, and cardiac arrest leading to neurological impairment. Rarely, such incidents may cause death (Cheney 1999).
Description of the intervention
Intubation was rarely performed in children before the 1940s, by which time our understanding of childhood physiology under anaesthesia had improved, and some specialist anaesthetic equipment for children had been developed (Costarino 2005). Indirect laryngoscopy involves visualizing the person's vocal cords by a means other than obtaining a direct line of sight. Classic examples are fibreoptic and indirect laryngoscopes, or videolaryngoscopes. The curvature of the blade and the special internal arrangement of the optical components allow visualization of the glottic plane without alignment of oral, pharyngeal, and tracheal axes, which may facilitate glottic exposure (Zhao 2014). Combining the fibreoptic bronchoscope and the laryngoscope led to the development of videolaryngoscopes, which provide a video‐based view of the glottic opening, with or without additional guidance of the tube towards the tracheal opening (Theiler 2013).
Many different types of indirect laryngoscopes facilitate intubation. Several manufacturers now have paediatric‐specific designs, and examples of indirect laryngoscopes, or videolaryngoscopes, that are available in the full complement of paediatric sizes include the following: the Storz videolaryngoscope, GlideScope, Truview, Pentax AWS, Airtraq, and the new McGrath paediatric size 2 videolaryngoscope that was recently introduced (Fiadjoe 2014). In general, these techniques offer the advantage of avoiding the need to align the optical axis in the pharynx and mouth to visualize the entrance of the larynx (Jungbauer 2009). However, it remains unclear if this approach translates into increased success with intubation (Griesdale 2012; White 2012).
How the intervention might work
Intubation in children is increasingly performed with indirect laryngoscopes, or videolaryngoscopes, and these are now emerging as important adjuncts in airway management. A video camera at the tip of the blade can potentially provide an increased angle and a magnified view of the glottis in normal and difficult paediatric airways (Vlatten 2009). Indirect laryngoscopes, or videolaryngoscopes, use magnifying mirrors, a light source, and a guide to facilitate visualization of the vocal cords and passing of the endotracheal tube. Specific to paediatric anaesthesia, it is more difficult for the trainer and the learner to share the same view during direct laryngoscopy. The excellent view and remote screen of the indirect laryngoscope, or videolaryngoscope, may therefore be particularly useful for training in these patients (MacNair 2009).
Many early paediatric indirect laryngoscopes, or videolaryngoscopes, were simply scaled down versions of the adult design. This resulted in poor views of the airway and failed intubations for infants and neonates (Fiadjoe 2014).
In adults, both mannequin and human studies have demonstrated that indirect laryngoscopy, or videolaryngoscopy, provides superior intubating conditions and requires a shorter learning curve (Vlatten 2012). Paediatric studies suggest that indirect laryngoscopy, or videolaryngoscopy, and direct laryngoscopy are equally suitable for facilitating intubation (Fiadjoe 2012; Kim 2011; Redel 2009; Vlatten 2012), but the time needed for intubation might be prolonged with videolaryngoscopy. A study in which investigators used paramedics, medical students, respiratory therapists, and nurses in the live situation of the operating room showed that indirect laryngoscopy, or videolaryngoscopy, has higher success rates and shorter times to intubation for adults (Jungbauer 2009). Moreover, available systematic reviews of adult intubation through videolaryngoscopy have shown some improvement in intubation outcomes (De Jong 2014; Griesdale 2012; Lu 2011; Su 2011). Furthermore, Lewis and colleagues published a protocol for a Cochrane systematic review that will assess the use of videolaryngoscopy in adult surgical patients (Lewis 2014).
Why it is important to do this review
Airway management and intubation are important in both elective and emergency situations for which a secure airway is required. The current practice is to use direct laryngoscopy to facilitate intubation; however, indirect laryngoscopy, or videolaryngoscopy, has the potential to facilitate successful intubation while improving intubation outcomes. Kim and associates reported that in children, videolaryngoscopy provided a view of the larynx equal to or better than that provided by the direct laryngoscope at the expense of longer intubation times (Kim 2008). Videolaryngoscopy is easier for investigators to use and results in a lower alteration in heart rate (Maharaj 2006; Riad 2012). To date, no systematic reviews have addressed the effects of indirect laryngoscopy, or videolaryngoscopy, on only paediatric intubation outcomes. A recent meta‐analysis that assessed both adults and children suggested that videolaryngoscopy is a good alternative to conventional direct laryngoscopy but included only a few paediatric studies (Su 2011).
Sun and coworkers concluded from a recent meta‐analysis including both children and neonates that videolaryngoscopies were associated with improved visualization of the glottis in children with normal airways or with potentially difficult airways, but with a significantly increased incidence of failed intubation (Sun 2014). Our review excludes neonatal intubations, as children in this age group have different airway anatomy and require different intubation techniques.
It is beyond the scope of this review to address the cost‐effectiveness and global health or policy‐based impact of this expensive and technology‐dependent intervention.
Objectives
To assess the efficacy of indirect laryngoscopy, or videolaryngoscopy, versus direct laryngoscopy for intubation of children with regards to intubation time, number of attempts at intubation, and adverse haemodynamic responses to endotracheal intubation. We also assessed other responses to intubation, such as trauma to oral, pharyngeal, and laryngeal structures, and we assessed vocal cord view scores.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomized controlled trials (RCTs) that compared intubation of children with indirect laryngoscopy, or videolaryngoscopy, versus direct laryngoscopy. We excluded mannequin‐simulated studies .
Types of participants
We included studies that assessed children 28 days to 18 years of age who needed to be intubated as an elective or emergency procedure. These intubations were done in the operating theatre or in a controlled anaesthetic environment.
Types of interventions
We included in this review all available studies that assessed tracheal intubation of children using any of the different types of indirect laryngoscope, or videolaryngoscope, as an intervention, compared with the control, which used a conventional method of intubation and the direct laryngoscope.
Types of outcome measures
Primary outcomes
-
Intubation time
-
Number of attempts at intubation and number of unsuccessful intubations
-
Adverse haemodynamic responses to endotracheal intubation, including changes in oxygen saturation, mean blood pressure, heart rate, and heart rhythm
Secondary outcomes
-
Other adverse effects of intubation in children, including trauma to oral, pharyngeal, and laryngeal structures assessed by visual or laryngoscopic examination
-
Vocal cord view score
Search methods for identification of studies
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL; 2015, Issue 11), MEDLINE (Ovid SP; 1946 to November 2015), Embase (Ovid SP; 1974 to November 2015), and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO; 1982 to November 2015). We reran the search in January 2017 and will address any studies of interest when we update the review. (See Appendix 2 for the search strategy that we used in this review.) We adapted the search terms used in MEDLINE for the other database sources.
We applied no language restrictions and obtained English translation of relevant studies when needed.
Searching other resources
We searched for unpublished ongoing clinical trials at the following websites ‐ www.clinicaltrials.gov and www.controlledtrials ‐ in November 2015. We reran the search in January 2017 and will incorporate any studies of interest when we update the review. We searched relevant conference proceedings, abstracts, and internal reports, and we contacted authors of studies for unpublished data or studies. We reviewed reference lists for other possible clinical trials and personal collections of articles when needed.
Data collection and analysis
Selection of studies
We followed standard methods of the Cochrane Anaesthesia, Critical and Emergency Care Review Group. Two review authors (IA and MM or DS) independently assessed titles and abstracts and, when needed, full texts of identified studies to determine eligibility for inclusion in this review. We resolved disagreements by consulting with a third review author (JL). We constructed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses) flow chart to record the number of papers retrieved and exclusions at each stage, along with reasons for inclusion or exclusion from the review (Moher 2009). We prepared the characteristics of included and excluded studies tables to present a summary of characteristics of relevant studies. We imposed no language restrictions
Data extraction and management
We obtained for assessment full‐text versions of all studies that may be included in the review. We used the form provided by the Cochrane Anaesthesia, Critical and Emergency Care Group for data extraction, which two review authors (IA and DS) independently completed for eligible trials (Appendix 5). We compared extracted data for any differences, which we assessed through further discussion of the full texts of included studies, and we compared study data with extracted data. This resulted in resolution of all disagreements between review authors. We entered the data into Review Manager 5 (RevMan 5.3) for further processing and analysis.
Assessment of risk of bias in included studies
Two review authors (IA and DS) independently assessed the risk of bias for each study, using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
We resolved disagreements by discussion or by consultation with a third review author (JL). We assessed risk of bias according to the following domains.
-
Random sequence generation (selection bias).
-
Allocation concealment (selection bias).
-
Blinding of participants and personnel (performance bias).
-
Blinding of outcome assessment (detection bias).
-
Incomplete outcome data (attrition bias).
-
Selective outcome reporting (reporting bias).
We graded each potential risk of bias as low, high, or unclear. We entered details of all judgements made regarding risk of bias assessment into the 'Risk of bias' tables included in the Characteristics of included studies tables.
Measures of treatment effect
We reported the risk ratio (RR) for dichotomous data and calculated the mean difference (MD) for continuous data. Some studies presented the results of continuous data as median, range or interquartile range, or both, so we calculated estimated means and standard deviations according to the method previously described by Hozo and colleagues (Hozo 2005).
Unit of analysis issues
We assessed only RCTs, using the participating child who needed intubation as the unit of analysis. We included no cluster‐randomized trials or cross‐over trials in this review.
Dealing with missing data
We contacted the authors of published studies for further clarification or for additional information when required. We used sensitivity analyses to explore the potential impact of missing data. We have highlighted all missing data within the Results section. We discussed in the review any drop‐out of children after randomization, to address implications and effects on results if applicable.
Assessment of heterogeneity
We anticipated heterogeneity of studies owing to the nature of the interventions provided. We assessed this using Chi2 and I2 statistics (Higgins 2002). We investigated significant heterogeneity by performing subgroup analyses.
Assessment of reporting biases
We contacted trial authors to request missing outcome data, when suspected. We performed sensitivity analyses to explore the impact of including studies with missing data in the overall assessment of results (Egger 1997). We examined funnel plots when we identified 10 or more studies reporting on a particular outcome, to investigate the potential of reporting and publication bias.
Data synthesis
We performed statistical analyses according to recommendations of the Cochrane Anaesthesia, Critical and Emergency Care Group. We used the Cochrane statistical package Review Manager 5 for data synthesis and analysis and reported all measures with 95% confidence intervals (CIs). As we expected heterogeneity between studies, we undertook a meta‐analysis with a random‐effects model and explored the influence of predefined subgroups if we found sufficient data.
Subgroup analysis and investigation of heterogeneity
We planned to conduct subgroup analyses, when data were available, based on the following.
-
Degree of airway difficulty.
-
Age of the child.
-
Skill level of the operator.
-
Type of videolaryngoscopy equipment used.
-
Emergency versus elective intubation.
Sensitivity analysis
We performed sensitivity analyses to explore the potential impact of missing data and any methodological heterogeneity. We omitted from the meta‐analysis studies with high risk of bias or variation in methods used one at a time to assess the effect on overall results. We assessed high risk of bias as described in the section entitled Risk of bias in included studies.
Summary of findings and GRADE
We used the principles of the GRADE system (Guyatt 2008) to assess the quality of the body of evidence associated with these specific outcomes.
-
Intubation time.
-
Number of attempts at intubation and number of unsuccessful intubations.
-
Adverse haemodynamic responses to endotracheal intubation in terms of oxygen saturation, mean blood pressure, and heart rate.
-
Other adverse effects of intubation in children, including trauma to oral, pharyngeal, and laryngeal structures, as assessed by visual or laryngoscopic examination.
We constructed summary of findings Table for the main comparison using GRADE software. Through the GRADE approach, we appraised the quality of a body of evidence according to the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. This technique accounted for within‐study risk of bias (methodological quality), directness of the evidence, precision of effect estimates, and risk of publication bias.
Results
Description of studies
Results of the search
We summarized search results in Figure 1.

Study flow (PRISMA) diagram of included and excluded studies. We reran the search in January 2017. We found three studies of interest. These studies were added to a list of ‘Studies awaiting classification' and will be incorporated into formal review findings during the review update.
We initially identified 1589 citations through searches of databases and specific websites. After screening by titles and abstracts, we first obtained full‐paper copies of 66 citations that were potentially eligible for inclusion in the review. From those studies, we excluded 51 articles for further duplication or irrelevant article methods and/or study populations. We excluded three additional studies for including different age groups and different study methods, as described in the Characteristics of excluded studies table. We included 12 studies (803 participants) in our review (Figure 1). We reran searches in November 2015. Among 134 new citations, we found no additional studies of interest. We reran the search again in January 2017, using new search terms, to include all studies while excluding duplicates. Among 959 new citations, we obtained full‐paper copies for 44 additional studies, from which we found three new studies of potential interest (243 participants). We added these three studies to a list of 'Studies awaiting classification' and will incorporate them into formal review findings during the review update. We will assess two ongoing studies when we update the review.
Included studies
We included in the review 12 eligible studies identified through the search (Ali 2013; Fiadjoe 2012; Inal 2010; Kim 2008; Kim 2011; MacNair 2009; Nileshwar 2010; Redel 2009; Riad 2012; Vlatten 2009; Vlatten 2012; White 2012). We summarized these studies in the Characteristics of included studies table.
Participants
We included in the review a total of 803 children, 28 days to 18 years of age. Participants were children who were scheduled for elective procedures. None of the included studies assessed emergency intubations. Anaesthetists, who were experts in direct laryngoscopy but had variable expertise in indirect laryngoscopy, performed all intubations. We included Fiadjoe 2012, which studied healthy infants younger than 12 months of age with normal craniofacial anatomy, but the age group was 5.5 ± 3.3 (mean ± SD) months, so the possibility that this study included infants younger than 28 days of age is very low. Inclusion of this study is unlikely to affect overall results of the review.
Interventions or comparisons
Different studies used different types of videolaryngoscopes. Four studies used the GlideScope videolaryngoscope (Fiadjoe 2012; Kim 2008; Kim 2011; Redel 2009). Four studies used the Airtraq videolaryngoscope (Ali 2013; Riad 2012; Vlatten 2012; White 2012). Inal 2010 used TruView EVO2, MacNair 2009 used Berci–Kaplan, Nileshwar 2010 used the Bullard laryngoscope, and Vlatten 2009 used the STORZ laryngoscope. Three studies included no muscle relaxant as part of their study protocol, but the implication of this for the intubation process was not clear (Redel 2009; Vlatten 2009; Vlatten 2012).
Excluded studies
We excluded three studies from this review, as study design (Tutuncu 2011) and population (Riveros 2013; Singh 2009) did not meet eligibility criteria for the intervention. We presented details in the Characteristics of excluded studies section.
Ongoing studies
We identified two ongoing studies and are awaiting dissemination of study results (Jamil 2015; Kim 2016). For further information, please see the Characteristics of ongoing studies table.
Studies awaiting classification
Three studies are awaiting classification (243 participants) (Cakirca 2016; Patil 2016; Vadi 2016). We will incorporate these studies into our formal review findings during the review update. For additional information, please see the Characteristics of studies awaiting classification table.
Risk of bias in included studies
Figure 2 and Figure 3 show risk of bias assessment across all 12 included studies. We have provided additional details in the risk of bias tables found in the Characteristics of included studies section.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We assessed low risk of selection bias for nine studies that provided sufficient details about randomization (Ali 2013; Fiadjoe 2012; Kim 2008; Kim 2011; Nileshwar 2010; Redel 2009; Vlatten 2009; Vlatten 2012; White 2012). We assessed low risk of allocation bias for only four studies that provided sufficient information (Inal 2010; Fiadjoe 2012; Kim 2011; Riad 2012).
Blinding
Personnel performing the intubation were not blinded to the type of device used across all 12 studies included in this review (Ali 2013; Inal 2010; Fiadjoe 2012; Kim 2008; Kim 2011; MacNair 2009; Nileshwar 2010; Redel 2009; Riad 2012; Vlatten 2009; Vlatten 2012; White 2012). Also, some outcomes were directly related to intubation, so we classified all 12 included studies as having high risk of bias. These outcomes included number of intubation attempts, vocal cord view score, and percentage of glottic opening score. Only two studies adopted good measures to reduce the risk of bias when assessing ‘time to intubate’ outcome measurements (Kim 2011; Vlatten 2012).
Incomplete outcome data
Seven of the included studies provided all of the results for randomized children (Ali 2013; Inal 2010; Kim 2008; Kim 2011; Redel 2009; Riad 2012; White 2012). However, five studies (Fiadjoe 2012; MacNair 2009; Nileshwar 2010; Vlatten 2009; Vlatten 2012) did not include in the analysis some of the children who had been recruited (no intention‐to‐treat analysis).
Selective reporting
All 12 included studies reported on all outcomes specified in the methods. Therefore, we assessed all 12 studies as having low risk of reporting bias.
Other potential sources of bias
We looked at funding by manufacturers as another source of bias; however, none of the studies reported in this review was funded by the manufacturer of an indirect laryngoscope, or videolaryngoscope.
Effects of interventions
See: Summary of findings for the main comparison
See summary of findings Table for the main comparison.
Comparison of indirect laryngoscopy, or videolaryngoscopy, versus direct laryngoscopy
All 12 eligible studies reported on this comparison. They included a total of 803 children from 28 days to 18 years of age. Types of indirect laryngoscopes, or videolaryngoscopes, used included GlideScope, Airtraq, TruView EVO2, Berci–Kaplan, Bullard, and STORZ. Two studies assessed simulated difficult airway scenarios by applying manual in‐line stabilization (Nileshwar 2010) or nasal intubation (Kim 2011). The remaining 10 studies evaluated orotracheal intubation in children with a presumed normal airway. Expert anaesthetists in direct laryngoscopy with variable experience in indirect laryngoscopy, or videolaryngoscopy, performed the intubations.
Primary outcomes
1. Intubation time
All 12 included studies reported intubation time. The pooled data synthesis included 798 children, and the definition of ‘intubation time’ varied between studies. Nine studies measured intubation time from introduction of the laryngoscope blade between the lips until first capnographic confirmation following intubation (Ali 2013; Fiadjoe 2012; Kim 2008; Kim 2011; MacNair 2009; Nileshwar 2010; Vlatten 2009; Vlatten 2012; White 2012).
Two studies (Inal 2010; Redel 2009) regarded intubation time as “time from the instrument entering the patient’s mouth until the time it was taken out after the placement of an endotracheal tube in the trachea”.
Riad 2012 reported intubation time as the period from termination of manual ventilation with a facemask to initiation of ventilation through the inserted endotracheal tube. Five studies presented results as median, range or interquartile range, or both (Fiadjoe 2012; Kim 2011; MacNair 2009; Vlatten 2009; Vlatten 2012), so we estimated mean and standard deviation according to the method described in Hozo 2005.
The pooled data synthesis and meta‐analysis for this outcome showed marked heterogeneity that needed further exploration. Analysis showed that children intubated by indirect laryngoscopy, or videolaryngoscopy, needed a longer time for intubation than those intubated by direct laryngoscopy (MD 5.49 seconds, 95% CI 1.37 to 9.60; I2 = 90%; very low‐quality evidence; Analysis 1.1; Figure 4).

Forest plot of comparison: 1 Indirect/videolaryngoscope versus conventional laryngoscope for intubation of children, outcome: 1.1 Intubation time.
Subgroup analysis
We undertook subgroup analysis by assessing the type of videolaryngoscope used. We could evaluate by subgroup analysis only ‘intubation time’ results from children intubated with GlideScope and Airtraq laryngoscopes. ‘Intubation time’ results from four studies that used the GlideScope laryngoscope (N = 403) showed no differences from total results (MD 5.12 seconds, 95% CI 0.45 to 9.80; I2 = 87%; Fiadjoe 2012; Kim 2008; Kim 2011; Redel 2009; Analysis 1.1; Figure 4). The four studies that assessed ‘intubation time’ with the Airtraq laryngoscope (n = 193) showed no significant differences between Airtraq and conventional laryngoscopy regarding this outcome (MD ‐0.81 seconds, 95% CI ‐16.59 to 14.96; I2 = 95%; Ali 2013; Riad 2012; Vlatten 2012; White 2012; Analysis 1.1; Figure 4). We could not group the remaining studies, as each used a different type of videolaryngoscope.
Sensitivity analysis
We performed a sensitivity analysis by omitting certain studies to assess the effect on overall results. Initially, we omitted Nileshwar 2010 from the pooled data synthesis (for high risk of bias and different methods, as recruited children had a simulated difficult airway scenario that was achieved by applying manual in‐line stabilization). This resulted in no differences in overall results with regards to heterogeneity (MD 4.20 seconds, 95% CI 0.74 to 7.66; I2 = 90%). Furthermore, we omitted from the meta‐analysis studies that used different definitions of intubation times and Kim 2011, which assessed nasal intubation; this revealed no differences in overall results in terms of heterogeneity (MD 5.43 seconds, 95% CI 1.06 to 9.8; I2 = 92%). Sensitivity analyses did not explain the marked heterogeneity among studies, hence it is difficult for review authors to provide conclusions on overall pooled average results for this outcome.
The funnel plot showed no evidence of publication bias for this outcome (Figure 5).

Funnel plot of comparison: 1 Indirect/videolaryngoscope versus conventional laryngoscope for intubation of children, outcome: 1.1 Intubation time.
2. Number of attempts at intubation and number of unsuccessful intubations
Eleven studies including 749 children evaluated success on the first attempt at intubation. Investigators found no significant differences between direct and indirect laryngoscopies (RR 0.96, 95% CI 0.91 to 1.02; I2 = 67%; low‐quality evidence; Ali 2013; Inal 2010; Kim 2008; Kim 2011; Fiadjoe 2012; MacNair 2009; Nileshwar 2010; Redel 2009; Vlatten 2009; Vlatten 2012; White 2012). We have summarized these results in Analysis 1.4. It was not possible for review authors to include outcome results from Riad 2012, as the actual numbers of events were not available. Five studies that included 263 children assessed unsuccessful intubation (failure after the second attempt at intubation or oxygen desaturation or both) and found that it was significantly increased in the indirect laryngoscopy, or videolaryngoscopy, group (RR 4.93, 95% CI 1.33 to 18.31; I2 = 0%; low‐quality evidence; Ali 2013; Kim 2011; MacNair 2009; Nileshwar 2010; Vlatten 2012).
We have summarized these results in Analysis 1.5.
Funnel plot inspection for success on the first attempt at intubation shows no evidence of asymmetry (Figure 6).

Funnel plot of comparison: 1 Indirect/videolaryngoscope versus conventional laryngoscope for intubation of children, outcome: 1.4 Successful first intubation attempts.
3. Adverse haemodynamic response to endotracheal intubation
3.1. Effect of intubation on oxygen saturation
Five studies including 272 children reported the effect of intubation on oxygen saturation (Inal 2010; Kim 2011; Nileshwar 2010; Vlatten 2009; Vlatten 2012; very low‐quality evidence).
Inal 2010 reported lowest oxygen saturation during intubation attempts as 99.4% ± 0.6% (mean ± SD) for the direct laryngoscopy group, compared with 97.6% ± 2.4% for the indirect laryngoscopy group. Investigators noted no desaturation (defined in the study as peripheral oxygen saturation < 90%). Kim 2011 found desaturation to < 95% in one case in the indirect laryngoscopy, or videolaryngoscopy, group compared with none in the direct laryngoscopy group, and Nileshwar 2010 reported four cases in the indirect laryngoscopy, or videolaryngoscopy, group. Vlatten 2009 and Vlatten 2012 reported that oxygen saturation did not drop to below 94% during intubation in any of the children in their studies.
3.2. Other haemodynamic responses
Only two studies that included 100 children reported effects of intubation on other haemodynamic responses (Inal 2010; Riad 2012; very low‐quality evidence).
Systolic blood pressure, diastolic blood pressure, and mean arterial pressure were not significantly different between the two groups studied by Riad 2012 (P = 0.86, 0.67, and 0.72, respectively), but investigators reported a significant increase in heart rate (HR) five minutes after intubation in the direct laryngoscopy group (P = 0.007). Inal 2010, on the other hand, showed that the HR change (difference before and after) in the direct laryngoscopy group was significantly lower than that in the indirect laryngoscopy group (P < 0.001) but did not provide actual data. No other studies reported these outcomes or reported heart rhythm as an outcome.
Secondary outcomes
1. Other adverse effects of intubation in children, including trauma to the airway and oral cavity
Five studies (total number of participants = 244; very low‐quality evidence) looked at evidence of trauma to the airway and oral cavity (Ali 2013; Inal 2010; Nileshwar 2010; Redel 2009; White 2012). Ali 2013 reported that only two children from the direct laryngoscopy group had evidence of trauma as a result of the intubation process compared with no children in the indirect laryngoscopy, or videolaryngoscopy, group.
2. Vocal cord view score (percentage of glottic opening (POGO) score)
Five of the reviewed studies, with a total of 256 children as participants, reported evaluation of the vocal cord view using a percentage score (Ali 2013; Fiadjoe 2012; Vlatten 2009; Vlatten 2012; White 2012).
We calculated estimates of means for studies for which results were presented as median, range, and/or interquartile range, as described earlier. Indirect laryngoscopy, or videolaryngoscopy, significantly improved the percentage of glottic opening (POGO) score in most of the studies reporting this outcome. Ali 2013 reported that the mean percentage of glottic opening was 97% in the indirect laryngoscopy group compared with 72% in the direct laryngoscopy group. The other studies yielded similar results: Fiadjoe 2012 reported a mean POGO of 90% for the indirect laryngoscopy group compared with 66.3% for the direct laryngoscopy group; and Vlatten 2009 provided a mean POGO of 95% for the indirect laryngoscopy group compared with 76.25% for the direct laryngoscopy group.
Vlatten 2012 reported a mean POGO of 97.5% of for the indirect laryngoscopy group compared with 75% for the direct laryngoscopy group, and White 2012 found no difference in POGO score reporting at 85% in both groups. We did not undertake meta‐analysis owing to the very skewed nature of the data reported, which would have made any estimate of confidence intervals unlikely to be true.
Vocal cord view score; laryngoscopic view according to Cormack and Lehane grade (C&L grade)
Six studies (including a total of 492 children as participants) evaluated vocal cord view scores according to Cormack and Lehane grade (C&L grade) (Inal 2010; Kim 2008; Kim 2011; MacNair 2009; Nileshwar 2010; Redel 2009). However, children who were enrolled in three of the studies had been assessed by both direct and indirect laryngoscopes, hence we omitted them from the pooled data synthesis (Kim 2008; Nileshwar 2010; MacNair 2009). Studies that evaluated the C&L view of grade 1 (3 trials; n = 190) observed no significant differences between direct and indirect laryngoscopy, or videolaryngoscopy (RR 1.06, 95% CI 0.93 to 1.21; I2 = 59%; Analysis 1.6). We included only 190 children in the final data synthesis for this outcome, so results should be interpreted with caution.
Subgroup analyses
None of the included studies provided sufficient data for assessment of the following subgroups: degree of airway difficulty; age of the child; skill level of the operator; and emergency versus elective intubation.
None of the intubations were done by inexperienced staff; only experienced anaesthetists performed all intubations on children with normal airways in all included studies. This was done in a controlled anaesthetic environment, and no emergency intubations were included. Children with difficult intubations and those with high risk of anaesthesia were excluded from these studies. Data were insufficient for analysis of subgroup outcome results according to age groups.
Discussion
Summary of main results
Airway complications are among the most common perioperative critical incidents in paediatric anaesthesia (Rasmussen 2009). Anaesthetists are increasingly turning to indirect laryngoscopy, or videolaryngoscopy, for both normal and difficult endotracheal intubations, mainly because videolaryngoscopy offers better views of the airway, particularly for patients who have previously undergone failed attempts at direct laryngoscopy (Fiadjoe 2014). Success with indirect laryngoscopy, or videolaryngoscopy, entails three main factors: patient factors (favourable anatomy, e.g. adequate mouth opening); provider factors (experience and skill with the device), and technical factors (e.g. optimal stylet bend angle, endotracheal tube (ETT) moulding, correct blade size selection). All of these must be optimized for smooth and successful intubation (Fiadjoe 2014).
This meta‐analysis assessed the following types of paediatric indirect laryngoscopes, or videolaryngoscopes: Airtraq, Bullard, Berci‐Kaplan, GlideScope, TruView, and Storz. Results of pooled data analysis show that intubation with indirect laryngoscopy, or videolaryngoscopy, was probably associated with improved visualization of the glottis, although the time to intubate was significantly prolonged when compared with direct laryngoscopy, and the quality of the evidence was very low. Of the 12 studies included in this meta‐analysis, one study compared children with simulated difficult airways; this was achieved by restricting cervical spine movements (Nileshwar 2010). Moreover, the current review shows that subgroup analysis performed to assess the types of videolaryngoscopy used studied small numbers of participants or identified significant heterogeneity among studies, which indicates uncertainty about the results.
Data were insufficient to permit conclusions about the overall effects of indirect laryngoscopy, or videolaryngoscopy, with regards to adverse effects. Only two children in this review were reported to have evidence of airway/oesophageal trauma, and one study (Ali 2013) reported this. A review article reported that five children from two studies had desaturation during the intubation process (Kim 2011; Nileshwar 2010). Furthermore, only two studies reported changes in heart rate during intubation (Inal 2010; Riad 2012), and no studies reported changes in heart rhythm.
Overall completeness and applicability of evidence
We identified 12 studies that assessed more than 800 children. All studies assessed intubation times as well as visualization of the glottis. Pooled results of assessment of these two outcomes would provide a fairly good estimate of the effect. However, the trials assessed had moderate to severe heterogeneity, which indicates uncertainty regarding overall results.
Quality of the evidence
We downgraded the quality of evidence from low to very low for the main outcomes, mainly owing to inconsistency, imprecision, and/or clinical variation. These variations in study results were not explained by subgroup analysis or sensitivity analysis.
Potential biases in the review process
To our knowledge, we have identified all available studies that assessed intubation in children with indirect laryngoscopy, or videolaryngoscopy, compared with the conventional method of intubation. We searched for ongoing trials and handsearched reference lists and grey literature to reduce the risk of publication bias. We reran the search in January 2017 and found three studies of interest (with a total of 243 participants). We added these studies to a list of ‘Studies awaiting classification' and will incorporate them into formal review findings during the review update. We extracted data only from full texts and included one study with a very low possibility that it included infants less than 28 days old, as the age group was reported as 5.5 ± 3.3 (mean ± SD) months (Fiadjoe 2012). Inclusion of this study is unlikely to affect overall review results. Given that the I2 statistic can be affected by several factors, leading to inconsistency, we believe that clinical variables within studies were the major factor that affected the overall value of the I2 statistic. In addition, imprecision as well as inconsistency between studies contributed to high value. We performed the analysis on outcomes using the high I2 statistic, but we acknowledged the low quality of evidence in summary of findings Table for the main comparison.
Agreements and disagreements with other studies or reviews
A recent meta‐analysis that compared the use of direct and indirect laryngoscopy in both paediatric and neonatal participants showed results similar to the findings of this review (Sun 2014). This meta‐analysis revealed that although videolaryngoscopes improved glottic visualization among paediatric patients, this was achieved at the expense of prolonged intubation time and increased failures (Sun 2014). Another meta‐analysis that compared direct and indirect laryngoscopy in both adults and children showed that the indirect laryngoscope, or videolaryngoscope, achieved a better view of the glottis, a similarly high rate of successful intubation, and shorter intubation time when difficulty was encountered (Su 2011). The systematic review and meta‐analysis of studies that included only adult participants showed that, compared with direct laryngoscopy, GlideScope videolaryngoscopy is associated with improved glottic visualization, particularly among patients with potential or simulated difficult airways (Griesdale 2012). In a pilot study that evaluated children known to have a difficult airway, use of the GlideScope videolaryngoscope, with and without laryngeal pressure, significantly improved Cormack and Lehane grade at laryngoscopy (Karsli 2010). The recent systematic review of assessment of videolaryngoscopy among neonates identified no completed studies for inclusion in the review (Lingappan 2015). Furthermore, Lewis and colleagues published a protocol for a systematic review on assessment of use of videolaryngoscopy in adult surgical patients (Lewis 2014).
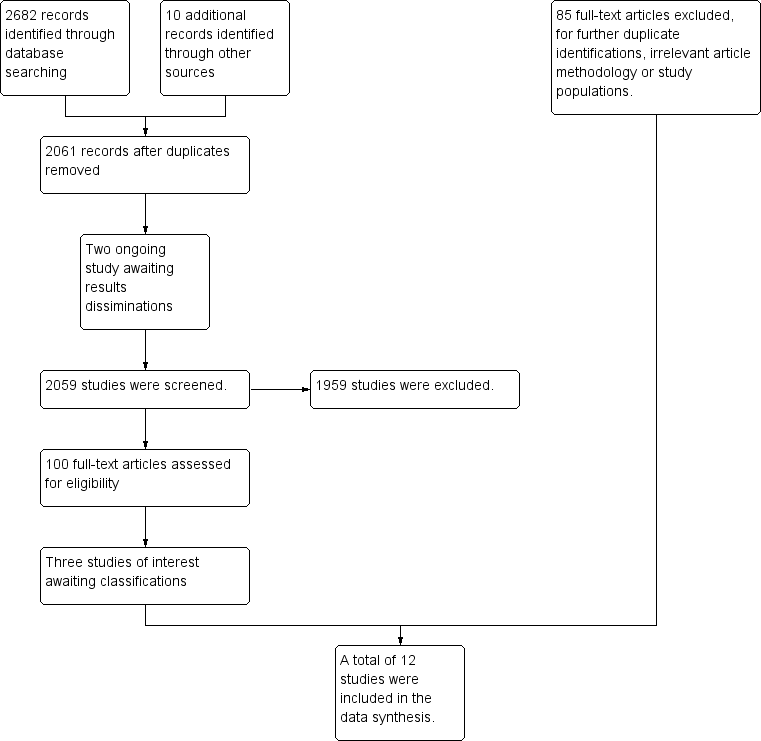
Study flow (PRISMA) diagram of included and excluded studies. We reran the search in January 2017. We found three studies of interest. These studies were added to a list of ‘Studies awaiting classification' and will be incorporated into formal review findings during the review update.
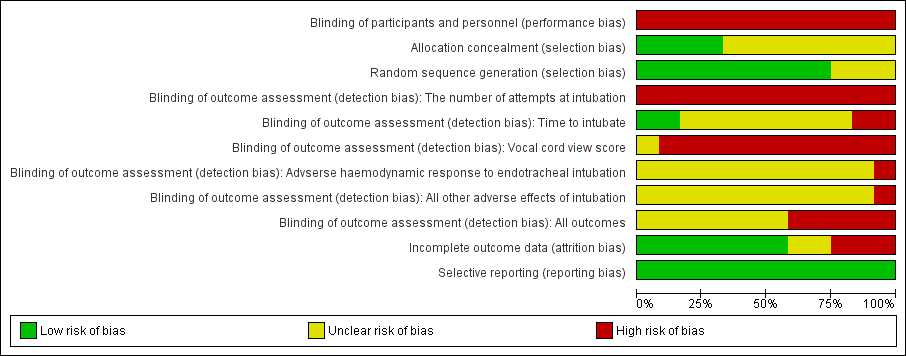
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Indirect/videolaryngoscope versus conventional laryngoscope for intubation of children, outcome: 1.1 Intubation time.

Funnel plot of comparison: 1 Indirect/videolaryngoscope versus conventional laryngoscope for intubation of children, outcome: 1.1 Intubation time.

Funnel plot of comparison: 1 Indirect/videolaryngoscope versus conventional laryngoscope for intubation of children, outcome: 1.4 Successful first intubation attempts.

Comparison 1 Indirect videolaryngoscope vs conventional laryngoscope for intubation of children, Outcome 1 Unsuccessful or more than 2 intubation attempts.

Comparison 1 Indirect videolaryngoscope vs conventional laryngoscope for intubation of children, Outcome 2 Intubation time ‐simulated difficult airway scenario study excluded.
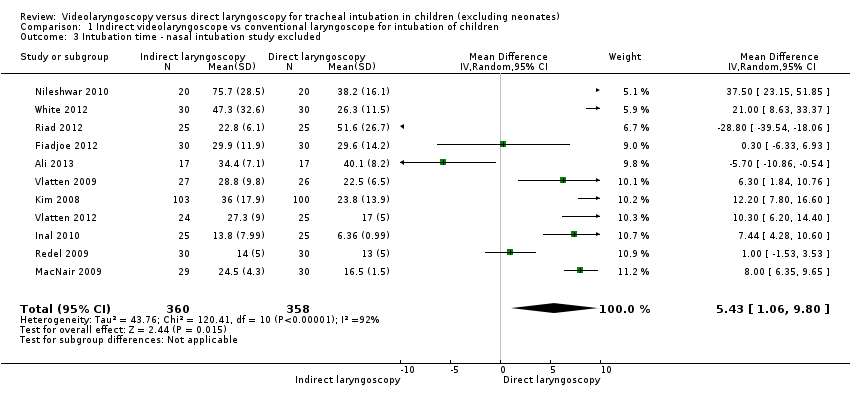
Comparison 1 Indirect videolaryngoscope vs conventional laryngoscope for intubation of children, Outcome 3 Intubation time ‐ nasal intubation study excluded.

Comparison 1 Indirect videolaryngoscope vs conventional laryngoscope for intubation of children, Outcome 4 Successful first intubation attempts.

Comparison 1 Indirect videolaryngoscope vs conventional laryngoscope for intubation of children, Outcome 5 Unsuccessful or more than 2 intubation attempts.

Comparison 1 Indirect videolaryngoscope vs conventional laryngoscope for intubation of children, Outcome 6 Vocal cords score: laryngoscopic view according to the Cormack and Lehane grade (C&L grade) ‐ grade 1 view.
| Videolaryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates) | ||||||
| Patient or population: tracheal intubation in children (excluding neonates) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with direct laryngoscopy | Risk with videolaryngoscopy | |||||
| Intubation time | Mean intubation time in the intervention group was 5.49 seconds higher (1.37 higher to 9.60 higher) | ‐ | 798 | ⊕⊝⊝⊝ | Risk of bias (unblinded), very serious heterogeneity (I2 = 90%), and clinically important increase not excluded | |
| Number of attempts at intubation and unsuccessful intubations | Study population | RR 0.96 | 749 | ⊕⊕⊝⊝ | Very serious heterogeneity (I2 = 67%) | |
| 26 per 1000 | 25 per 1000 | |||||
| Number of attempts at intubation and unsuccessful intubations | Study population | RR 4.93 | 263 | ⊕⊕⊝⊝ | Lack of blinding and no exclusion of a clinically trivial increase | |
| 37 per 1000 | 182 per 1000 | |||||
| Adverse haemodynamic response to endotracheal intubation | In 4 studies that reported occurrences of oxygen saturation < 95%, 5 cases happened in the videolaryngoscopy group and none in the direct laryngoscopy group. The fifth study shows a 97% mean saturation in the video group compared with 99% in the direct group | ‐ | 272 | ⊕⊝⊝⊝ | Very sparse data and serious concerns about unblinded reporting | |
| Adverse haemodynamic response to endotracheal intubation | One study reported a significant increase in heart rate after intubation with direct laryngoscopy, and the other study contradicted this and showed less of a change in heart rate in the direct group. A single study reported that systolic, diastolic, and mean arterial blood pressures were not significantly different between the 2 groups | ‐ | 100 | ⊕⊝⊝⊝ | Very sparse data and serious concerns about unblinded reporting | |
| Other adverse effects of intubation in children, including trauma to oral, pharyngeal, and laryngeal structures, assessed by visual or laryngoscopic examination | Only 2 children from the direct laryngoscopy group were reported to have evidence of trauma as a result of the intubation process compared with no children in the indirect laryngoscopy, or videolaryngoscopy, group | ‐ | 244 | ⊕⊝⊝⊝ | Very sparse data and serious concerns about unblinded reporting | |
| *Risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded three levels owing to serious concerns about study limitation, inconsistency, and indirectness bDowngraded two levels owing to serious inconsistency and study limitation cDowngraded two levels owing to serious imprecision and study limitation dDowngraded three levels owing to serious imprecision and serious inconsistency and study limitation eDowngraded three levels owing to study limitation and serious imprecision fDowngraded three levels owing to serious imprecision, study limitation, and inconsistency | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Unsuccessful or more than 2 intubation attempts Show forest plot | 12 | 798 | Mean Difference (IV, Random, 95% CI) | 5.49 [1.37, 9.60] |
| 1.1 Other videolaryngoscopes | 4 | 202 | Mean Difference (IV, Random, 95% CI) | 11.04 [4.62, 17.46] |
| 1.2 GlideScope videolaryngoscope | 4 | 403 | Mean Difference (IV, Random, 95% CI) | 5.12 [0.45, 9.80] |
| 1.3 Airtraq videolaryngoscope | 4 | 193 | Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐16.59, 14.96] |
| 2 Intubation time ‐simulated difficult airway scenario study excluded Show forest plot | 11 | 758 | Mean Difference (IV, Random, 95% CI) | 4.20 [0.74, 7.66] |
| 3 Intubation time ‐ nasal intubation study excluded Show forest plot | 11 | 718 | Mean Difference (IV, Random, 95% CI) | 5.43 [1.06, 9.80] |
| 4 Successful first intubation attempts Show forest plot | 11 | 749 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.91, 1.02] |
| 5 Unsuccessful or more than 2 intubation attempts Show forest plot | 5 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 4.93 [1.33, 18.31] |
| 6 Vocal cords score: laryngoscopic view according to the Cormack and Lehane grade (C&L grade) ‐ grade 1 view Show forest plot | 3 | 190 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.93, 1.21] |

