Videolaringoscopia versus laringoscopia directa para pacientes adultos que requieren intubación traqueal
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 99 Inclusion criteria: body mass index between 30 and 50 kg/m2; orotracheal intubation required for elective surgery Exclusion criteria: no details Baseline characteristics: Pentax AWS Age: 50 (SD ± 12) Gender M/F: 11/39 BMI: 41.2 (SD ± 4.4) ASA II: 15 ASA III: 32 ASA IV: 3 Mallampati 1: 21 Mallampati 2: 18 Mallampati 3: 7 Mallampati 4: 4 Macintosh Age: 49 (SD ± 14) Gender M/F: 10/39 BMI: 42.5 (SD ± 5.9) ASA II: 7 ASA III: 40 ASA IV: 2 Mallampati 1: 14 Mallampati 2: 21 Mallampati 3:13 Mallampati 4: 0 Country: USA Setting: hospital | |
| Interventions | Pentax AWS (n = 50) vs Macintosh blade (n = 49) Macintosh laryngoscope with a #4 blade | |
| Outcomes | Continuous outcomes: Time to intubation: defined as time from start of first attempt of insertion of laryngoscope until a capnogram signal was obtained. Median (Q1, Q3) time: Pentax 38 (31, 50) seconds vs Macintosh 26 (22, 29) seconds. Adjusted for Mallampati and ASA status: hazard ratio 0.35, 95% confidence interval 0.23 to 0.55, P < 0.001. No evidence of a learning curve on time to intubation with the Pentax AWS based on analysis of sequence quartiles Ease of intubation on a scale of 0 to 100 (0 as easiest): VLS 52 (SD ± 31), Mac 40 (SD ± 28); P = 0.02 CL glottic view reported with CL 1 and 2: grouped as good; CL 3 and 4: grouped as poor. Data not reported for this outcome Dichotomous outcomes: Laryngeal/airway trauma Sore throat Successful first attempt No. of attempts: 1 to 3 | |
| Notes | Baseline characteristics: more women than men in each group. More ASA II in Pentax group, more ASA III in Macintosh group. More Mallampati scores of 1 in Pentax group, more Mallampati scores of 2 in Macintosh group Conclusions of study authors: Although Pentax AWS often provided a superb glottic view, time required for intubation was longer than for Macintosh. Success was better with Mactinosh blade. AWS should not be substituted routinely for a conventional Macintosh #4 blade in morbidly obese patients. Funding/declarations of interest: supported by internal funds; Pentax on loan from manufacturers for duration of the study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was based on computer‐generated, random‐block codes" |
| Allocation concealment (selection bias) | Low risk | Quote: "sequentially numbered opaque envelopes" Comment: assumed envelope was sealed |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "it was impossible to blind the operator to the device being used" Comment: this will affect all outcomes for this domain. |
| Blinding of outcome assessment (detection bias) | High risk | Comment: Observers who looked at blood staining and postoperative sore throat were blinded to group allocation. However, it was not possible to blind outcome assessors to primary outcomes. |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Of 105 randomized patients, 4 did not complete the study because of cancellation of surgery or because the laryngoscopist could not arrive to the operating room on time, and 2 patients in the Pentax group had missing primary outcomes" Comment: few losses, unlikely to introduce any bias |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | High risk | Quote: "All patients’ tracheas were intubated by 1 of 2 attending anesthesiologists, each of whom had previously used the Pentax AWS 5 to 10 times before the study began" Comment: it is likely that the balance of experience will favour the Macintosh group |
| Baseline characteristics | Low risk | Quote: "patients in the Pentax group were more likely to have better ASA physical status and better Mallampati scores (absolute standardized difference 0.25)" Comment: small difference unlikely to be clinically relevant |
| Funding sources | Unclear risk | Comment: supported by internal funds; Pentax on loan from manufacturers for duration of study |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 50 Inclusion criteria: normal intraocular pressure, scheduled for ophthalmic surgery requiring tracheal intubation Exclusion criteria: no details Baseline characteristics: described as comparable but no details given; abstract only Country: Saudi Arabia Setting: hospital | |
| Interventions | GlideScope vs Macintosh blade | |
| Outcomes | Continuous outcomes: Duration of intubation Other outcomes: MAP and HR, plus intraocular pressure | |
| Notes | Additional: email sent to authors to request additional details; additions made to risk of bias tables following study author response Funding/declarations of interest: none (confirmed by study authors in email) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned" Comment: Email information from study authors states use of sealed envelopes |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: abstract only; insufficient details but no blinding assumed |
| Incomplete outcome data (attrition bias) | Unclear risk | Comment: abstract only; insufficient details |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Comment: Email information from study authors states intubators had 5 years' experience with GlideScope and up to 20 years' experience with Macintosh blade |
| Baseline characteristics | Unclear risk | Comment: no details |
| Funding sources | Low risk | Comment: Email information from study authors states no additional funding used for study |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 100 Inclusion criteria: all patients scheduled for elective bariatric surgery, BMI > 35 kg/m2 and age > 18 and < 60 years Exclusion criteria: severe mental illness, ongoing alcohol or substance abuse, previous difficult intubation, patient considered by the anaesthesiologist to require a different procedure of anaesthesia or intubation (e.g. fibreoptic intubation) than prescribed by the study protocol Baseline characteristics: GlideScope Age: 42 SD ± 10 (range 21–60) Gender M/F: 15/35 BMI: 42 SD ± 6 (range 35–62) Mallampati ≥ 3: 11 Height (cm): 171 SD ± 10 (range 150–195) Weight (kg): 125 SD ± 10 (range 92–190) Macintosh Age: 41 SD ± 8 (range 28–59) Gender M/F: 9/31 BMI: 41 SD ± 5 (range 35–56) Mallampati 3: 16 Height (cm): 172 SD ± 7 (range 157–194) Weight (kg): 122 SD ± 18 (range 90–167) Country: Denmark Setting: hospital | |
| Interventions | GlideScope (n = 50) vs Macintosh blade (n = 50) GlideScope participants in ramped position; #4 blade used; stylet bent at 90 degrees, as per manufacturer guidelines Macintosh participants in ramped position; #3 or #4 blade at the intubator’s discretion; hockey‐stick‐shaped stylets | |
| Outcomes | Continuous outcomes: Time to intubation (time from gripping the laryngoscope until registration of expired CO2): GlideScope (median (range)): 48 (22‐148); Mac 32 (17‐209) Difficulty of intubation: no difference in subjective difficulty of intubation, but IDS scores significantly lower in GlideScope group; median IDS score: GlideScope group 1 (0–4); Mac 2 (0–7) (P = 0.01) Dichotomous outcomes: Failed intubation: defined as not achieving intubation in maximum 2 attempts Hypoxia: defined as oxygen desaturation < 93% Laryngeal/airway trauma: defined as mucosal injury, airway bleeding, dental trauma Sore throat/hoarseness (assessed at 1 hour post extubation on a VAS): sore throat present in 40% in GlideScope group vs 42% in Macintosh group No. of attempts: 4 participants in Macintosh group required more than 1 attempt at intubation vs 1 in GlideScope group (P = 0.36). Two of the 4 participants in the Macintosh group proved impossible to intubate within 2 attempts with direct laryngoscopy (i.e. failed intubation) and were subsequently intubated with the GlideScope with no problem. CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: all intubations performed by 1 of 5 certified nurse anaesthetists or 2 anaesthesiologists, all with prior experience with at least 20 GlideScope intubations and with wide experience in anaesthetizing obese patients Funding/declarations of interest: departmental funding only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated random numbers" |
| Allocation concealment (selection bias) | Low risk | Quote: "sealed opaque envelopes packed by an outside investigator" Comment: does not state that envelopes are sequentially numbered, but low risk of bias assumed with use of outside investigator |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: no attempt to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "One hundred consecutive patients were enrolled after which the trial was ended as planned. All eligible patients gave consent to participate, none were excluded or failed to complete, and all were included in the final analysis" |
| Selective reporting (reporting bias) | Low risk | Comment: copy of protocol on clinicaltrials.gov sought and compared with published trial (clinical trials ID NCT00917033); all outcomes reported |
| Experience of intubator | Low risk | Quote: "All intubations were performed by one of five certified nurse anaesthetists or two anaesthesiologists all with prior experience from at least 20 GS (GlideScope) intubations and with wide experience in anesthetizing obese patients" |
| Baseline characteristics | Low risk | Quote: "The patients in the two groups were comparable with regards to demographic and airway characteristics" |
| Funding sources | Low risk | Comment: departmental funding only |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 36 Inclusion criteria: patients between 20 and 80 years of age, ASA I or II, scheduled to undergo elective surgery requiring intubation Exclusion criteria: risk factors for cardiopulmonary disease, predicted or history of difficult intubation (cervical spine abnormality, restricted neck mobility), gastric aspiration Baseline characteristics: Pentax AWS Age: 61.7 (SD ± 8.8) Gender M/F: 8/10 Height (m): 160.0 (SD ± 8.6) Weight (kg): 59.7 (SD ± 14.1) Mallampati 1: 10 Mallampati 2: 8 Mallampati 3: 0 Macintosh Age: 56.7 (SD ± 17.3) Gender M/F: 13/5 Height (m): 163.9 (SD ± 7.1) Weight (kg): 63.5 (SD ± 11.3) Mallampati 1: 8 Mallampati 2: 9 Mallampati 3: 1 Country: Japan Setting: hospital | |
| Interventions | Pentax AWS (n = 18) vs Macintosh (n = 18) A pillow was placed under the participant's head, and an appropriately sized semirigid cervical collar was fitted around the neck to simulate limited neck movements. Macintosh blade #3 or #4 | |
| Outcomes | Continuous outcomes: Time for tracheal intubation: defined as time when the airway device was handed to the anaesthesiologist to time when the presence of carbon dioxide was confirmed in the exhaled breath on the vital sign monitor Difficulty of intubation: IDS score distribution: AWS score of 0 in 14 participants, score of 1 in 3 participants; Mac score of 0 in 1 participant, score of 1 in 5 participants, score of 2 in 3 participants, 3 in 4 participants, 4 in 3 participants, 5 in 1 participant Dichotomous outcomes: Failed intubation (1 failure in AWS group due to insufficient interincisor space compared with thickness of the blade; 1 failure in Mac group due to tooth injury; failures excluded from CL data) Laryngeal/airway trauma (lip injury, blood on device) Participant reported sore throat (pharyngeal pain) Hoarseness No. of attempts: 1 to 4 CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: In all cases, laryngoscopy was performed by 1 anaesthesiologist experienced in the use of both devices Funding/declarations of interest: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: described as randomized but no additional details given |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: time measured by independent observer, but not possible to blind observer for other outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Comment: one participant from each group had failed intubation, and subsequent analyses of outcomes did not include these missing participants. However, losses were few |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Comment: all laryngoscopies performed by 1 anaesthetist experienced with both devices |
| Baseline characteristics | Low risk | Comment: baseline characteristics equivalent |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 80 Inclusion criteria: pregnant patients undergoing caesarean section surgery under general anaesthesia Exclusion criteria: presence of cardiovascular, hepatic, renal or neuromuscular disease, non‐co‐operation, restricted neck movements, retrognathia, ASA score of III or IV, Mallampati score of 4, history of airway‐related surgery, emergency surgery. Additionally, patients who had more than 2 of the following criteria were excluded: Mallampati score of 3, maximal mouth‐opening capacity < 35 mm, thyromental distance < 65 mm Baseline characteristics: McGrath Age: 27.55 (SD ± 3.82) Height (cm): 162.9 (SD ± 6.15) Weight (kg): 77.90 (SD ± 13.71) BMI: 29.45 (SD ± 5.6) ASA I: 28 ASA II: 12 Mallampati 1: 19 Mallampati 2: 19 Mallampati 3: 2 Macintosh Age: 29.25 (SD ± 4.41) Height (cm): 160.8 (SD ± 6.0) Weight (kg): 72.32 (SD ± 9.82) BMI: 27.98 (SD ± 3.22) ASA I: 24 ASA II: 16 Mallampati 1: 21 Mallampati 2: 19 Mallampati 3: 0 Country: Turkey Setting: hospital | |
| Interventions | McGrath series 5 (n = 40) vs Macintosh (n = 40) McGrath blade: use of stylet to guide tube during videolaryngoscopy Macintosh blade #3 or #4 | |
| Outcomes | Continuous outcomes: Time for tracheal intubation: defined as time from anaesthesiologist taking the laryngoscope in his hand until first upward deflection on the capnograph after connection of the anaesthetic ventilation system to the tracheal tube POGO Dichotomous outcomes: Failed intubation Laryngeal/airway trauma: no palatoglossal arch nor dental injuries in either group Successful first attempt CL glottic view: 1 to 4 Other outcomes: haemodynamic outcomes | |
| Notes | Funding/declarations of interest: none apparent | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "sealed‐envelope technique" Comment: no additional details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: assumed no attempts made to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Quote: "All intubations were performed by an experienced anesthesiologist" |
| Baseline characteristics | Low risk | Quote: "There was no significant difference in the demographic data and preprocedural intubation conditions between the groups" |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 109 Inclusion criteria: age ≥ 18 years and requiring emergency tracheal intubation in the prehospital setting only during the day shift Exclusion criteria: none given Baseline characteristics: Pentax AWS Age: 74.4 (SD ± 13.6) Gender M/F: 34/22 Cardiac arrest participants: 54/56 Macintosh Age: 74.1 (SD ± 13.0) Gender M/F: 38/15 Cardiac arrest participants: 47/53 Country: Japan Setting: prehospital; paramedics/physicians travel together in ambulance to calls | |
| Interventions | Pentax AWS (n = 56) vs Macintosh (n = 53) A suction device and Magill forceps were available for use at any time | |
| Outcomes | Continuous outcomes: Difficulty of tracheal intubation(measured on IDS): median IDS (IQR): Pentax 0 (0‐1); Mac 1 (0‐2) Number of attempts (before switching from AWS to Macintosh): 0 in 3 cases, 1 in 14 cases, 2 in 1 case, 3 in 2 cases; data not reported for switching from Macintosh to AWS (Note: In 3 cases, the alternative device was used before the procedure was even started) Time for tracheal intubation (measured from insertion of the blade between the teeth to confirmation of endotracheal tube placement by capnograph. If intubation failed and the device for intubation was changed, time was measured from insertion on the first attempt to success on the second or successive attempts): median time (IQR) seconds: Pentax 155 (71–216); Mac 120 (60–170) Dichotomous outcomes: Failed intubation Successful first attempt Other: ultimate success of intubation (if intubation achieved within 600 seconds, even if change of device had taken place): Pentax 54/56; Mac 53/53 | |
| Notes | Experience of intubator: 6 physicians had previously worked as anaesthetists with an estimated range of 15 to 30 AWS intubations or > 100 Macintosh intubations per year. The remaining 5 had at least 50 Macintosh experiences but relatively fewer experiences with AWS intubation (but had received manikin training sessions) Funding/declarations of interest: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "allocation was changed in a serial manner and was controlled by personnel at the physician car system center" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The operators were told which of the two devices had been allocated to them to use only when en route to the incident in the ambulance" |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind physician |
| Blinding of outcome assessment (detection bias) | High risk | Comment: all outcomes assessed by physician who was not blinded. Some potential for bias in the outcomes as operators were encouraged to complete intubation as quickly as possible, even if it was achieved by switching devices. Operators could be biased to familiar equipment; therefore change to an alternative device made frequently |
| Incomplete outcome data (attrition bias) | High risk | Quote: "Of 121 patients enrolled in this study, 12 were excluded due to missing data, age < 18 years, or problems with the device used, leaving 109 for final analysis" Comment: high level of losses; no explanation about what problems with the device led to the exclusion of some patients |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Quote: "6 physicians had generally performed N 100 intubations per year as they had previously worked as anesthetists. The number of AWS intubations they have performed is not precisely known, but is estimated to be in the range of 15 to 30 AWS intubations per physician per year. The remaining 5 physicians had done an anesthesia rotation and had performed at least 50 intubations, but with relatively fewer experiences with AWS intubation" Comment: some variety of experience among personnel; unclear if these personnel were balanced between intervention and comparison groups |
| Baseline characteristics | Low risk | Comment: most baseline characteristics equivalent, except for differences in types of cases |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 296 Inclusion criteria: patients with objective predictors of potentially difficult tracheal intubation: reduced cervical motion from pathological condition or cervical spine precautions (limited capacity to flex or extend the neck or managed with a cervical collar, but with negative imaging), Mallampati classification score of 3 or 4, reduced mouth opening (< 3 cm), history of difficult direct laryngoscopy Exclusion criteria: a documented easy tracheal intubation (success on first attempt), history of failed intubation and failed bag‐mask ventilation, known unstable cervical spine injury, age < 18 years, presentation for an emergency surgical procedure Baseline characteristics: C‐MAC Age: 54 (SD ± 14) Gender M/F: 74/75 BMI: 34 (SD ± 10) ASA I: 3 ASA II: 60 ASA III: 80 ASA IV: 6 Macintosh Age: 55 (SD ± 15) Gender M/F: 83/64 BMI: 34 (SD ± 10) ASA I: 2 ASA II: 53 ASA III: 87 ASA IV: 5 Country: US Setting: hospital | |
| Interventions | C‐MAC (n = 149) vs Macintosh (n = 147) External laryngeal manipulation, use of gum‐elastic bougie | |
| Outcomes | Continuous outcomes: Number of attempts: no details on number of attempts provided in the paper Time for tracheal intubation: defined as time between blade insertion into the mouth and inflation of the endotracheal tube cuff Dichotomous outcomes: Failed intubation: defined as removal of laryngoscope from the mouth, then device selected at discretion of anaesthetist. Data taken only when an alternative device had been used Laryngeal/airway trauma Patient‐reported sore throat Hypoxia: defined as oxygen desaturation < 90% Successful first attempt: defined as confirmation of endotracheal tube placement by end‐tidal carbon dioxide with a single blade insertion CL view achieved: 1 to 4 Success also given per providers:anaesthesiologists: C‐MAC 9/10, Mac 10/12; per residents: C‐MAC 64/67, Mac 78/91; per CRNAs: C‐MAC 65/72, Mac 36/44 | |
| Notes | Experience of intubator: C‐MAC: anaesthesiologist 10; resident 67; CRNA (supervised) 72; Macintosh: anaesthesiologist 12; resident 91; CRNA (supervised) 44 Funding/declarations of interest: supported by an investigator‐initiated grant (no. 00520743‐2) from Karl Storz Endoscopy‐America Additional: contact made with study author to confirm denominator figures in Table 3; email response in file | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed in a 1:1 allocation ratio via specialized computer software" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Individual randomization cards were placed in concealed envelopes" Comment: unclear if envelope was opaque, numbered or sealed |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Both the study team and the anesthesia team remained blinded until the patient entered the operating room" Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "One of the investigators or a study nurse followed each patient into the operating room to record the relevant intubation and post intubation data" Comment: for patient reported outcomes; no details of whether other outcome assessors were blinded or not |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Three hundred patients were consented and enrolled in this randomized controlled study. There were four randomization failures that were excluded from analysis" Comment: losses too few to create bias |
| Selective reporting (reporting bias) | Low risk | Quote: "pre‐registered online as NCT00956592" Comment: clinical trial register protocol sourced; protocol outcomes comparable with study‐reported outcomes |
| Experience of intubator | High risk | Quote: "In three cases, the anesthesia team deviated from randomization to DL (Macintosh) and intubated with a video laryngoscope because of provider preference" Comment: does not state whether all operators had equivalent experience with C‐MAC, but it is known that some operators preferred a particular device. Also, the level of qualification of the operators differed between devices, with more resident anaesthetists using the Macintosh, and more CRNAs using the C‐MAC |
| Baseline characteristics | Low risk | Comment: baseline characteristics largely comparable |
| Funding sources | High risk | Comment: supported by an investigator‐initiated grant (no. 00520743‐2) from Karl Storz Endoscopy‐America |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 68 Inclusion criteria: > 18 years, ASA I or II, scheduled for elective thoracic surgery Exclusion criteria: rapid sequence induction, anticipated difficult airway, contraindication against use of double‐lumen tube Baseline characteristics: X‐lite Age: 41.8 (SD ± 9) Gender M/F: 28/6 BMI: 24 (SD ± 2.9) ASA I: 23 ASA II: 11 Mallampati 1: 26 Mallampati 2: 8 Macintosh Age: 44.6 (SD ± 10) Gender M/F: 29/5 BMI: 22.98 (SD ± 2.19) ASA I: 20 ASA II: 14 Mallampati 1: 24 Mallampati 2: 10 Country: Morrocco Setting: hospital | |
| Interventions | X‐lite videolaryngoscope (n = 34) vs Macintosh (n = 34) Stylet used in both groups Double‐lumen tube used in both groups | |
| Outcomes | Continuous outcomes: Time for tracheal intubation (from insertion of blade into mouth to capnography reading) Dichotomous outcomes: Failed intubation: defined as not successful after 3 attempts followed by intubation with alternative device Laryngeal/airway trauma (dental trauma, oesophageal or vocal cord trauma or bleeding) Hypoxia No. of attempts: 1 to 2 CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: intubator with at least 5 years' experience, including experience with X‐lite. No experience with double‐lumen tube with X‐lite Funding/declarations of interest: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: computer‐generated randomization |
| Allocation concealment (selection bias) | Unclear risk | Comment: numbers concealed in envelopes until moment of intubation; no additional details about envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: assumed outcome assessors were not blinded from outcomes measured in theatre |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | High risk | Comment: Anaesthetist had more than 5 years' experience with use of DLT and training in the use of X‐lite but no experience in use of X‐lite with double‐lumen tube. No details of experience with Macintosh provided |
| Baseline characteristics | Low risk | Comment: baseline characteristics comparable |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 70 Inclusion criteria: > 18 years old, ASA I or II, scheduled for elective thyroid surgery Exclusion criteria: anticipated difficult intubation, limited interdental distance, limited cervical mobility, limited thyromental difficulty or Mallampati 4. Those needing rapid sequence induction, those with gastro‐oesophageal reflux, hiatus hernia, diabetes, obesity Baseline characteristics: X‐lite Age: 43.5 (SD ± 11.1) Gender M/F: 11/24 Height (cm): 172.7 (SD ± 3.4) Weight (kg): 71.1 (SD ± 8.3) BMI: 23.9 (SD ± 2.9) ASA I: 28 ASA II: 7 Mallampati 1: 16 Mallampati 2: 13 Mallampati 3: 5 Mallampati 4: 1 Macintosh Age: 48.8 (SD ± 12.7) Gender M/F: 8/27 Height (cm): 172.1 (SD ± 3.7) Weight (kg): 73.9 (SD ± 8.2) BMI: 25.0 (SD ± 3.1) ASA I: 25 ASA II: 10 Mallampati 1: 15 Mallampati 2: 10 Mallampati 3: 8 Mallampati 4: 2 Country: Morrocco Setting: hospital | |
| Interventions | X‐lite videolaryngoscope (n = 35) vs Macintosh (n = 35) External laryngeal manoeuvres used, with gum‐elastic bougie Macintosh blade #3 | |
| Outcomes | Continuous outcomes: Difficulty of tracheal intubation: IDS scores for difficulty of tracheal intubation ‐ X‐lite 0: 13/35; 1 to 5: 20/35; > 5: 2/35; Mac 0: 7/35; 1 to 5 19/35; > 5: 9/35) Time for tracheal intubation: defined as sum of times for glottic visualization plus time from glottic visualization to tracheal intubation Dichotomous outcomes: Failed intubation (1 participant in Macintosh group was intubated with Airtraq after 3 attempts with Macintosh) Laryngeal/airway trauma (blood on scope; "no dental or laryngeal trauma was noted in either group") Hypoxia: defined as oxygen saturation < 92% CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: 3 intubators with experience of more than 500 intubations with Macintosh and more than 60 with X‐lite Funding/declarations of interest: none Addtional: study also included use of Airtraq scope ‐ excluded from this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: computer‐generated randomization |
| Allocation concealment (selection bias) | Unclear risk | Comment: concealed in envelopes, but no additional details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: outcome assessors independent but not possible to blind assessors in theatre |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no losses after randomization |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Comment: although intubators had less experience with X‐lite, they were still sufficiently experienced in both devices |
| Baseline characteristics | Low risk | Comment: baseline characteristics comparable |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 78 Inclusion criteria: patients scheduled for elective CABG Exclusion criteria: patients with renal, hepatic disease, bleeding diathesis, diabetes mellitus, Mallampati score of 3 or 4, history of a difficult intubation and ASA class IV Baseline characteristics: GlideScope Age: 57.28 (SD ± 9.91) Gender M/F: 23/17 Height (cm): 163.73 (SD ± 10.15) Weight (kg): 71.45 (SD ± 12.16) Mallampati 1: 21 Mallampati 2: 16 Mallampati 3: 3 Mallampati 4: 0 Macintosh Age: 58.58 (SD ± 10.87) Gender M/F: 29/9 Height (cm): 165.47 (SD ± 8.10) Weight (kg): 72.26 (SD ± 15.47) Mallampati 1: 25 Mallampati 2: 12 Mallampati 3: 1 Mallampati 4: 0 Country: Iran Setting: hospital | |
| Interventions | GlideScope (n = 40) vs Macintosh (n = 38) Use of stylet in both groups when required Macintosh blade #3 or #4 | |
| Outcomes | Continuous outcomes: Number of attempts Time for tracheal intubation: defined as time from opening mouth to filling the tube cuff ‐ measured in seconds Dichotomous outcomes: Failed intubation Respiratory complications Laryngeal/airway trauma Patient‐reported sore throat (sore throat and odynophagia reported together) Successful first attempt | |
| Notes | Experience of intubator: experienced, but no details on level of experience Funding/declarations of interest: none apparent | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using online software (http://www.graphpad.com/quickcalcs/randomize1.cfm), patients were randomly allocated" Comment: computer generated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details given |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: no mention of blinding; unlikely as timing of intubation was involved |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Two patients were excluded because of long postoperative intubation period" Comment: low number unlikely to cause bias |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Quote: "all of tracheal intubations were performed by experienced anesthesiologists" Comment: no information on whether amount of experience with each device was equivalent |
| Baseline characteristics | Low risk | Comment: baseline characteristics comparable |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 30 Inclusion criteria: adult patients scheduled for elective surgery under general anaesthesia, aged > 18 years to < 65 years, ASA I or II Exclusion criteria: patient likely to be difficult to intubate according to SIAARTI recommendations Baseline characteristics: GlideScope followed by Macintosh Age: 44 (SD ± 11) Gender M/F: 8/7 BMI: 25.5 (SD ± 3) Macintosh followed by GlideScope Age: 41 (SD ± 12) Gender M/F: 8/7 BMI: 26.4 (SD ± 2.8) Country: Italy Setting: hospital | |
| Interventions | GlideScope (n = 15) vs Macintosh (n = 15) GlideScope blade #4; "hockey stick" stylet used in GlideScope group Macintosh blade #3 or #4 | |
| Outcomes | Continuous outcomes: Time for tracheal intubation: defined as time from insertion of blade between incisors until tube cuff was inflated Dichotomous outcomes: Failed intubation Laryngeal/airway trauma ("no injuries or dental damage were recorded") "All were successfully intubated" ‐ but no definition of success given | |
| Notes | Experience of intubator: 1 intubator experienced in both techniques; > 100 intubations with each device Funding/declarations of interest: department funding only; no conflicts of interest Additional: Study aimed to measure forces but also reported data on relevant outcomes. Study authors have not reported on CL grades, although this information is included in the Methods section. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: use of a random number generator |
| Allocation concealment (selection bias) | Unclear risk | Quote: "numbered coded vehicles was the method used to achieve allocation concealment" Comment: not clear what this means and whether this is sufficient |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: participants blinded to group assignment, but intraoperative data collected by non‐blinded anaesthetists and caregivers |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought. Methods section stated that CL grades were recorded, but they were not reported in the Results section |
| Experience of intubator | Low risk | Comment: 1 intubator experienced in both techniques; > 100 intubations with each device |
| Baseline characteristics | Low risk | Comment: baseline characteristics comparable |
| Funding sources | Low risk | Comment: departmental funding only |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 150 Inclusion criteria: ASA I to III scheduled for elective surgery in supine position with general anaesthesia, requiring tracheal intubation Exclusion criteria: pathology of the upper respiratory or alimentary tract known or suspected, a rapid sequence induction indicated, an awake intubation appropriate because of a suspected or known difficult airway Baseline characteristics: C‐MAC3 Age: median (range) 54 (20‐74) Gender M/F: 10/27 Height (cm): median (range) 168 (150‐186) Weight (kg): median (range) 76 (54‐98) BMI: median (range) 27 (20‐40) Mallampati 1: 8 Mallampati 2: 23 Mallampati 3: 6 Mallampati 4: 0 Macintosh Age: median (range) 49 (23‐82) Gender M/F: 21/29 Height (cm): median (range) 170 (156‐196) Weight (kg): median (range) 81 (60‐179) BMI: median (range) 27 (20‐63) Mallampati 1: 16 Mallampati 2: 20 Mallampati 3: 13 Mallampati 4: 1 C‐MAC4 Age: median (range) 46 (34‐72) Gender M/F: 11/7 Height (m): median (range) 173 (163‐188) Weight (kg): median (range) 82 (54‐150) BMI: median (range) 27 (20‐40) Mallampati 1: 4 Mallampati 2: 6 Mallampati 3: 7 Mallampati 4: 1 C‐MAC4/SBT Age: median (range) 58 (27‐79) Gender M/F: 28/17 Height (cm): median (range) 173 (155‐193) Weight (kg): median (range) 78 (48‐135) BMI: median (range) 27 (19‐44) Mallampati 1: 9 Mallampati 2: 21 Mallampati 3: 15 Mallampati 4: 0 Country: Germany Setting: hospital | |
| Interventions | C‐MAC 3 (n = 37) vs C‐MAC4 (n = 18) vs C‐MAC/STB (n = 45) vs Macintosh (50) Participants underwent 3 separate laryngoscopies with Macintosh or #3 or #4 C‐MAC blade. After 50 participants, C‐MAC #4 was changed to a straight blade technique (C‐MAC/STB). Order of laryngoscopies was determined by randomization. Macintosh blade #3 or #4 | |
| Outcomes | Continuous outcomes: Time for tracheal intubation: defined as time from touching tube to performing successful endotracheal placement Dichotomous outcomes: Failed intubation: defined as intubated with alternative device owing to limited glottic visualization Laryngeal/airway trauma (any palatoglossal arch or dental injury) Number of intubation attempts: 1 to 3 CL glottic view: not possible to interpret data from graphs | |
| Notes | Experience of intubator: 1 of 3 anaesthesiologists with ≥ 8 years' experience (after training with manikins for C‐MAC scope) Funding/declarations of interest: equipment supplied by Storz manufacturer. One study author is a member of the Storz advisory team and receives grant support for airway management studies. Additional: cross‐over study with 3 arms, changed to 4 arms part of the way through the study. High risk of bias was introduced with changing of the protocol part of the way through | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: computer generated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | High risk | Comment: protocol changed part of the way through the study ‐ data not provided before and after protocol change. Therefore, not possible to assess whether high levels of bias were introduced by the decision. An additional group was introduced part of the way through the study, which led to exclusion of some participants from C‐MAC groups |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Comments: 1 of 3 anaesthesiologists with ≥ 8 years' experience (after training with manikins for C‐MAC scope). Although personnel are described as experienced, the level of experience with C‐MAC is unclear |
| Baseline characteristics | Low risk | Comment: baseline characteristics reported according to intubating device; some differences in male and female ratios between groups, but not anticipated to make a difference |
| Funding sources | High risk | Comment: equipment supplied by Storz manufacturer. One study author is a member of the Storz advisory team and receives grant support for airway management studies |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 60 Inclusion criteria: ASA I or II, scheduled to undergo general anaesthesia between the ages of 15 and 60 years Exclusion criteria: thyroid‐to‐chin length ≤ 5 cm, Mallampati class ≥ 3, mouth opening < 3 cm, restriction in neck extension or protruding front teeth, predicted to be difficult in intubation. Also, airway difficulty score > 8, including the evaluation criteria mentioned above, were predicted to be difficult to intubate Baseline characteristics: GlideScope Age: 39.5 (SD ± 13.4) Gender M/F: 16/14 Height (cm): 166.0 (SD ± 8.2) Weight (kg): 64.5 (SD ± 9.2) Macintosh Age: 43.0 (SD ± 14.9) Gender M/F: 15/15 Height (cm): 162.8 (SD ± 10.5) Weight (kg): 61.2 (SD ± 11.7) Country: Korea Setting: hospital | |
| Interventions | GlideScope (n = 30) vs Macintosh (n = 30) Macintosh blade #3 Use of cricoid pressure by assistant in both groups | |
| Outcomes | Continuous outcomes: Difficulty of tracheal intubation (airway difficulty score (ADS) on VAS by anaesthesiologist: 0 is most easy and 10 is most difficult. GlideScope 6.7 (SD ± 0.9); Macintosh 6.6 (SD ± 0.6)) Improved visualization (POGO score (%): GlideScope 89.6 (SD ± 20.0); Macintosh 67.6 (SD ± 24.7), P < 0.05) Time for tracheal intubation (measured in seconds): defined as time from when anaesthesiologist grabbed handle to when tube passed vocal cords | |
| Notes | Experience of intubator: all intubations performed by 1 anaesthetist ‐ fully experienced and familiar with GlideScope Funding/declarations of interest: none apparent Note: Some participants were younger than 18 years of age and were not separated in the data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "All patients were randomly allocated" Comment: no additional details |
| Allocation concealment (selection bias) | Unclear risk | Comment: no mention of concealment method |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: all outcomes assessed during intubation period were assumed to be not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: protocol not sought |
| Experience of intubator | Low risk | Quote: "study was carried out by a fully experienced anesthesiologist familiar with the GVL (GlideScope)" |
| Baseline characteristics | Low risk | Quote: "no statistical differences in age, sex, height, weight and ADS between the two groups" |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over design | |
| Participants | Total number of participants: 44 Inclusion criteria: undergoing elective surgery under general anaesthetic with tracheal intubation, ≥ 1 risk factor for a difficult laryngoscopy (from unpublished data: ASA I to III; over 18 years of age; requiring single‐lumen tracheal intubation) Exclusion criteria: (from unpublished data: rapid sequence induction or other alternative intubation methods indicated; known or suspected oral, pharyngeal or laryngeal masses. Or, if patients had poor dentition, symptomatic gastro‐oesophageal reflux, cervical spine instability, unstable hypertension, coronary artery disease, cerebral disease, lack of resources available to conduct the procedure on scheduled date of surgery) Baseline characteristics (taken from unpublished data): Intubation with GlideScope Age: 56.5 (SD ± 11.6) Gender (M/F): 11/13 Height (cm): 165.3 (SD ± 12.1) Weight (kg): 79.9 (SD ± 15.1) BMI (kg/m2): 29.2 (SD ± 4.6) Mallampati ≥ 3: 24 Intubation with Macintosh Age: 54.0 (SD ± 11.2) Gender (M/F): 12/8 Height (cm): 167.0 (SD ± 8.6) Weight (kg): 74.7 (SD ± 13.4) BMI (kg/m2): 26.8 (SD ± 4.3) Mallampati ≥ 3: 20 Country: Toronto, Ohio, USA Setting: hospital | |
| Interventions | GlideScope (n = 24) vs Macintosh (n = 20) | |
| Outcomes | Continuous outcomes: Time for tracheal intubation: defined as time from when laryngoscope passed between the participant's teeth to when laryngoscopy enabled placement of a styletted tracheal tube at, not through, laryngeal inlet. Results reported as median (IQR) seconds: GlideScope 30 (22‐47); Macintosh 18 (14‐28) Dichotomous outcomes: Failed intubation: defined as when laryngoscope was withdrawn beyond the teeth or lasting longer than 60 seconds | |
| Notes | Experience of intubator: laryngoscopists experienced in both devices on ≥ 25 occasions (from unpublished manuscript) Funding/declarations of interest: none apparent Comments: study authors provided unpublished manuscript of study on email request. Data above and in risk of bias table were taken from this manuscript. Study of forces, includes relevant outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: computer‐generated randomization code |
| Allocation concealment (selection bias) | Unclear risk | Comment: randomization revealed immediately before induction of anaesthesia (but no other details on how it was concealed) |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: outcome assessors and data analysts blinded to forces outcome but this outcome not relevant for this review. Assumed other outcome assessments were not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Comment: few losses after randomization due to study equipment failure, but data still collected for all outcomes when possible |
| Selective reporting (reporting bias) | Low risk | Comment: copy of protocol on clinicaltrials.gov sought and compared with published trial (clinical trials ID NCT01814176). All outcomes were reported |
| Experience of intubator | Low risk | Comment: laryngoscopists experienced in both devices, with use of GlideScope on at least ≥ 25 occasions |
| Baseline characteristics | Low risk | Comment: baseline characteristics comparable |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 59 Inclusion criteria: 40 to 60 years of age, untreated hypertension, undergoing elective surgery Exclusion criteria: blood pressure > 180/110 mmHg, predicted difficult airway, history of drug abuse, dehydration, history of other cardiovascular disease, history of consumption of any drugs known to affect cardiovascular system, diabetes mellitus, end‐organ damage due to hypertension Baseline characteristics: GlideScope Age: 54.82 (SD ± 5.76) Gender (M/F): 19/11 Weight (kg): 72.14 (SD ± 9.72) Macintosh Age: 57.82 (SD ± 4.83) Gender (M/F): 15/14 Weight (kg): 66.25 (SD ± 6.15) Country: Iran Setting: hospital | |
| Interventions | GlideScope (n = 30) vs Macintosh (n = 29) | |
| Outcomes | Continuous outcomes: Time for tracheal intubation: defined as time from grasping endotracheal tube until passing tube through vocal cords | |
| Notes | Experience of intubator: all intubations performed by 1 experienced anaesthesiology resident Funding/declarations of interest: none apparent Additional: Study aimed to assess haemodynamic changes but included relevant outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: randomized using permutated blocks |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessor for relevant outcome |
| Incomplete outcome data (attrition bias) | Low risk | Comment: only 1 exclusion; not likely to affect outcome data |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Quote: "The patients were intubated by a single experienced anesthesiology resident" Comment: no details on whether experience is equivalent with both devices |
| Baseline characteristics | Low risk | Comment: baseline characteristics comparable |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 203 Inclusion criteria: scheduled for elective surgery Exclusion criteria: pathology of the neck, upper respiratory tract or upper alimentary tracts, at risk of pulmonary aspiration of gastric contents Total baseline characteristics: Age: mean 57 (SD ± 16) (range 18–86) Gender M/F: 117/86 Height (cm): mean 160 (SD ± 9) (range 130–181) Weight (kg): mean 61 (SD ± 12) (range 34–105) BMI: mean 24 (SD ± 3.9) (range 16–37) ASA I: 62 ASA II: 140 ASA III: 1 Mallampati 1: 154 Mallampati 2: 40 Mallampati 3: 8 Mallampati 4: 1 Country: Japan Setting: hospital Participant's head and neck stabilized by assistants using in‐line manual method | |
| Interventions | Pentax AWS vs Macintosh Macintosh blade #3 or #4. Use of gum‐elastic bougie allowed in Macintosh group | |
| Outcomes | Continuous outcomes: Improved visualization Time for tracheal intubation (for Macintosh, time from tracheal tube passing gap between upper and lower incisors to confirmation of carbon dioxide waveforms after tracheal intubation; for Pentax, time from touching tracheal tube (attached to scope) to confirmation of carbon dioxide waveforms) Dichotomous outcomes: Failed intubation: defined as not complete within 120 seconds, then tried with another device. Some inconsistencies within study report with denominator figures for successful tracheal intubation. CL glottic view: 1 to 4 | |
| Notes | Funding/declarations of interest: 1 study author given an honorarium from manufacturer for writing a lecture and was loaned an AWS for the study. Other departments had to provide their own | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The order was randomized by tossing a coin" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: no blinding possible |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no loss of participants |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Comment: no details of operator experience |
| Baseline characteristics | Unclear risk | Comment: not divided by group, as cross‐over design |
| Funding sources | High risk | Comment: one study author given an honorarium from manufacturer for writing a lecture and was loaned an AWS for the study. Other departments had to provide their own |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel design | |
| Participants | Total number of participants: 60 Inclusion criteria: ASA I to III, scheduled for elective surgical procedure requiring tracheal intubation Exclusion criteria: no details Baseline characteristics not included in abstract Country: Ireland Setting: hospital | |
| Interventions | McGrath vs Macintosh Type of McGrath not specified in the paper Optimization manoeuvres used in both groups as required (readjustment of head, use of bougie, use of external laryngeal manipulation and use of second assistant) | |
| Outcomes | Continuous outcomes: Tme for tracheal intubation (reported in study without SD) Difficulty of intubation Dichotomous outcomes: Successful first attempt Larngeal/airway trauma (dental trauma) CL glottic view: 1 to 3 Number of attempts: 1 to 3 | |
| Notes | Experience of intubator: experience with McGrath on ≥ 5 occasions. Ten anaesthetists in total. Does not say if stratified Funding/declarations of interest: 1 McGrath VLS on loan from manufacturer Other: published only as an abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: participants described as "randomly assigned", but no additional details |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "All data were collected by an independent unblinded observer" |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Quote: "Ten anaesthetists, who had received prior instruction and had experienced use of the McGrath videolaryngoscope on at least five previous occasions" Comment: unclear if this is sufficient equivalent experience |
| Baseline characteristics | Low risk | Quote: "There were no significant differences in baseline characteristics between the groups" |
| Funding sources | Unclear risk | Comment: 1 McGrath VLS on loan from manufacturer |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 40 Inclusion criteria: over 16 years of age requiring urgent tracheal intubation in the critical care unit Exclusion criteria: requirement for immediate endotracheal intubation (within 5 minutes) as anticipated by the ICU team, spontaneous breathing endotracheal intubation technique or cervical spine precautions, history of (or anticipated) difficult intubation, previous cardiac arrest or cardiopulmonary instability (oxygen saturation 90% or systolic blood pressure 80 mmHg despite oxygen or fluid and vasopressor therapy), prior clinical deterioration requiring immediate tracheal intubation while awaiting randomization or deemed inappropriate for enrolment by the attending physician (e.g. patient considered unsuitable for either technique) Baseline characteristics: GlideScope Age: 68 (SD ± 16) Gender M/F: 15/5 BMI: 26 (SD ± 4) Mallampati 1: 5 Mallampati 2: 6 Mallampati 3: 2 Mallampati 4: 1 Macintosh Age: 61 (SD ± 16) Gender M/F: 13/7 BMI: 24 (SD ± 6) Mallampati 1: 3 Mallampati 2: 4 Mallampati 3: 3 Mallampati 4: 0 Note: 16 participants were not tested for their Mallampati score. Country: Canada Setting: hospital, ICU or emergency department | |
| Interventions | GlideScope (n = 20) vs Macintosh (n = 20) GlideScope blade #4; site of intubation ICU (19), ward (1), ED (0) Macintosh blade #3 or #4; site of intubation ICU (14), ward (3), ED (3) | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from when tip of laryngoscope entered the participant's mouth until detection of end‐tidal carbon dioxide waveform on capnography) Dichotomous outcomes: Failed intubation (unsuccessful on first attempt and required use of alternative device). Data presented for failure of first attempts. Not possible to combine data with those of other studies. In the GlideScope group, 5 of 12 (42%) first attempts failed, resulting in use of the Macintosh for subsequent attempts. In the Macintosh group, only 1 of 13 (5%) first attempts failed, resultingin use of the GlideScope for subsequent attempts (P = 0.03). The supervisor took over in 8 of 12 (67%) failed first attempts with Macintosh (data missing from 1 participant) compared with 4 of 12 (33%) in the GlideScope group (P = 0.22). Mortality (30 days) Successful first attempt CL glottic view: 1 to 4 (results reported for 19 participants only) No. of attempts: 1 to 4 Time for successful intubation, median (IQR): GlideScope 221 (103‐291), Mac 156 (67‐220), P = 0.15 | |
| Notes | Experience of intubator: all inexperienced in endotracheal intubation, defined as fewer than 5 endotracheal intubations in the preceding 6 months (medical students, or PGY 1‐4) Supervisor could take over if initial attempt exceeded 1 minute. Funding/declarations of interest: Canadian Anesthesiologists' Society 2009 Research Award; Clinician Scientist Award from Vancouver Coastal Health Research Institute Additional: pilot study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: random allocation table in permutated blocks of 4 |
| Allocation concealment (selection bias) | Low risk | Comment: numbered opaque sealed envelopes opened by research co‐ordinator at time of randomization |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: research co‐ordinators not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Comment: data for CL scores not reported for 1 participant in each group |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Comment: both groups included inexperienced operators |
| Baseline characteristics | Low risk | Comment: baseline characteristics comparable |
| Funding sources | Low risk | Comment: Canadian Anesthesiologists' Society 2009 Research Award; Clinician Scientist Award from Vancouver Coastal Health Research Institute |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 120 Inclusion criteria: 18 to 65 years of age, either gender, ASA I or II undergoing elective cervical spine surgery for cervical compressive myelopathy Exclusion criteria: risk factors for difficult mask ventilation, gastric aspiration (obesity, pregnancy), difficult airway such as previous neck surgery and mouth opening < 3 cm Baseline characteristics: C‐MAC + stylet Age: 40 (SD ± 12) Gender M/F: 25/5 BMI: 23.1 (SD ± 2.6) ASA I: 22 ASA II: 8 Mallampati 1: 4 Mallampati 2: 14 Mallampati 3: 12 Macintosh + stylet Age: 39 (SD ± 16) Gender M/F: 26/4 BMI: 21.6 (SD ± 2.1) ASA I: 21 ASA II: 9 Mallampati 1: 6 Mallampati 2: 11 Mallampati 3: 13 C‐MAC non‐stylet Age: 39 (SD 16) Gender M/F: 24/6 BMI: 21.6 (SD 2.7) ASA I: 23 ASA II: 7 Mallampati 1: 6 Mallampati 2: 15 Mallampati 3: 9 Macintosh non‐stylet Age: 41 (SD 16) Gender M/F: 28/2 BMI: 22.0 (SD 2.4) ASA I: 25 ASA II: 5 Mallampati 1: 4 Mallampati 2: 15 Mallampati 3: 11 Country: India Setting: hospital | |
| Interventions | C‐MAC with stylet (n = 30) vs Macintosh with stylet (n = 30) vs C‐MAC non‐stylet (n = 30) vs Macintosh non‐stylet (n = 30) Gum‐elastic bougies used if required Additional: The neck of all participants was immobilized with MILS by holding the sides of the neck and the mastoid processes, thus preventing flexion/extension or rotational movements of the head and neck. | |
| Outcomes | Continuous outcomes: Difficulty of tracheal intubation: measured on IDS; reported as median (IQR): C‐MAC + stylet 2 (1‐3); Macintosh + stylet 3 (2‐4); C‐MAC non‐stylet 4 (2‐6); Macintosh non‐stylet 3 (2‐8) Time for tracheal intubation: defined as time from insertion of laryngoscope blade between the teeth until ETT was placed through the vocal cords, as evidenced by visual confirmation; reported as median (IQR): C‐MAC + stylet 27 (23‐31); Macintosh + stylet 34 (22‐53); C‐MAC non‐stylet 52 (28‐76); Macintosh non‐stylet 34 (22‐70) Dichotomous outcomes: Failed intubation: defined as an attempt in which the trachea was not intubated, or that required longer than 120 seconds to perform Laryngeal/airway trauma (upper lip trauma, tooth damage, soft tissue bleeding, supraglottic trauma) Successful first attempt CL glottic view: 1 to 3 No. of attempts: 1 to 2 | |
| Notes | Experience of intubator: 1 of 2 anaesthesiologists experienced in the use of both laryngoscopes in patients requiring MILS, having done > 50 intubations with each device before the study Funding/declarations of interest: none apparent | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated randomization" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Data were collected by a single independent observer" Comment: not possible for all outcomes to be blinded;unclear if independent observer is blinded |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Four patients were excluded because of alternative intubation techniques preferred by the attending anesthesiologist" Comment: small number excluded prior to randomization |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "two anesthesiologists...experienced in the use of both laryngoscopes in patients requiring MILS, having done more than 50 such intubations with each device before this study" |
| Baseline characteristics | Low risk | Comment: baseline characteristics comparable |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over design ‐ participants intubated with both types of scopes in random order | |
| Participants | Total number of participants: 14 Inclusion criteria: adults undergoing elective surgery requiring general anaesthesia and oral endotracheal intubation, patients who were likely to be easy to intubate, Mallampati airway class 1 or 2, thyromental distance ≥ 6.0 cm, sternomental distance ≥ 12.5 cm, age 18 to 80 years, height between 1.52 and 1.83 m, BMI ≤ 30 kg/m2 Exclusion criteria: maxillary incisors that were loose or in poor condition; previous difficult intubation; any cervical spine anatomical abnormalities such as disc disease, instability, myelopathy and/or any previous cervical spine surgery; symptomatic gastro‐oesophageal reflux or reactive airway disease; any history of coronary artery disease or cerebral aneurysm; any history of vocal cord and/or glottic disease or dysfunction; preoperative systolic blood pressure > 180 mmHg or diastolic blood pressure > 80 mmHg; ASA > III Baseline characteristics: reported for all participants, not by group Age: 47 (SD ± 20) Gender M/F: 9/5 BMI: 25.9 (SD ± 2.6) ASA I: 3 ASA II: 11 Mallampati 1: 8 Mallampati 2: 6 Country: USA Setting: hospital | |
| Interventions | Airtraq vs Macintosh Airtraq used with video camera attachment | |
| Outcomes | Continuous outcomes: Time for tracheal intubation (definition not given): not included in meta‐analysis but study authors report results as mean (± SD): Airtraq 19.6 (± 7.0); Macintosh 21.6 (± 7.8) Dichotomous outcomes: Success of intubation (not included in meta‐analysis because of increased risk of bias due to study design, but study authors report that all intubations were successful except for 1 in a participant intubated with a Macintosh blade) Glottic view (POGO scores: "POGO scores at stage 3 were less during intubations with the Macintosh than with Airtraq, based on both anaesthesiologist report (P = 0.0007) and video analysis (P = 0.0002)") Adverse effects, but not reported by group. "On postoperative day 7, two patients reported very mild voice changes that were intermittent and nonbothersome" | |
| Notes | Experience of intubator: 2 study anaesthesiologists, both with more than 27 years' experience of direct laryngoscopy and ≥ 50 successful intubations with Airtraq Funding/declarations of interest: supported by a National Institutes of Health grant Additional: study designed to measure forces but includes relevant outcomes for this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: use of an independent biostatistician to develop randomization sequence |
| Allocation concealment (selection bias) | Low risk | Comment: use of sealed opaque envelopes with matching patient identification number |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors to relevant outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Comment: only 1 loss; reasons for loss reported |
| Selective reporting (reporting bias) | Low risk | Comment: registered with clinicaltrials.gov NCT01369381; protocol sourced and appears equivalent to full published report |
| Experience of intubator | Low risk | Comment: 2 study anaesthesiologists, each with more than 27 years' experience of direct laryngoscopy and ≥ 50 successful intubations with Airtraq |
| Baseline characteristics | Unclear risk | Comment: more women than men enrolled in the study; unclear if this affects results. All participants underwent laryngoscopy with each scope; therefore baseline characteristics were not presented separately |
| Funding sources | Low risk | Comment: supported by a National Institutes of Health grant |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 200 Inclusion criteria: ASA I or II undergoing general anaesthesia using tracheal intubation Exclusion criteria: history of previous difficult intubation, cervical spine fracture or cervical spine instability Baseline characteristics: Baseline characteristics not sufficiently supplied in short report. Author quote: "Patients were comparable with respect to age, weight and height" Country: Japan Setting: hospital | |
| Interventions | Pentax AWS (n = 100) vs Macintosh (n = 100) | |
| Outcomes | Continuous outcome: Time for tracheal intubation Dichotomous outcomes: Successful first attempt No. of attempts: 1 to 3 | |
| Notes | Experience of intubator: 26 non‐anaesthesia residents, with median clinical training of 5 weeks (range 1‐24 weeks) Funding/declarations of interest: none Additional: limited detail ‐ short report only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: computer random number table |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "an independent observer recorded the duration of tracheal intubation attempts" Comment: independent but not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no losses reported |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Comment: 26 residents, all with equivalent limited experience |
| Baseline characteristics | Low risk | Comment: described by study authors as comparable |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 521 Inclusion criteria: required general anaesthesia with tracheal intubation for surgery Exclusion criteria: history of previous difficult intubation, cervical spine fracture or cervical spine instability Baseline characteristics: Pentax AWS Age: 53 (SD ± 16) Height (cm): 159 (SD ± 9) Weight (kg): 59 (SD ± 12) BMI: 23 (SD ± 4) Macintosh Age: 54 (SD ± 17) Height (cm): 159 (SD ± 9) Weight (kg): 59 (SD ± 11) BMI: 23 (SD ± 4) Country: Japan Setting: hospital | |
| Interventions | Pentax AWS (n = 265) vs Macintosh (n = 256) | |
| Outcomes | Continuous outcomes: Time for tracheal intubation: defined as time from interruption of intermittent positive‐pressure ventilation to connection of the endotracheal tube to an anaesthesia circuit. If the first intubation attempt failed, duration of the subsequent attempt was added to time of the first attempt to secure the airway. Dichotomous outcomes: Successful first attempt No. of attempts: 1 to 4 | |
| Notes | Experience of intubator: all medical residents with anaesthesia training of 9 (SD 6) weeks, 48 operators in total, supervised by anaesthesiologist, available for verbal information if necessary Funding/declarations of interest: departmental funding only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned via table of random numbers as generated by a personal computer" Comment: However, study authors also state: "availability of the Pentax‐AWS was slightly limited compared with the standard Macintosh laryngoscope." Unclear if this may have introduced bias |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details given |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: all outcomes were assessed during intubation process; therefore not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | High risk | Quote: "each participant had taken part in a smaller number of intubations with the Pentax‐AWS than the Macintosh laryngoscope" Comment: all operators had limited experience |
| Baseline characteristics | Low risk | Comment: baseline characteristics equivalent |
| Funding sources | Low risk | Comment: departmental funding only |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 60 Inclusion criteria: adult patients, ASA I or II, requiring a DLT for thoracic surgery Exclusion criteria: risk of regurgitation and pulmonary aspiration, history of gastro‐oesophageal reflux, pregnancy, scheduled tracheostomy and planned postoperative ventilation in ICU, a potentially difficult laryngoscopy as suggested by limited neck extension (< 35°), distance between tip of the patient’s mandible and thyroid notch < 7 cm, sternomental distance < 12.5 cm with the head fully extended and the mouth closed Baseline characteristics: GlideScope Age: 40.1 (SD ± 18.7) Gender M/F: 7/23 Height (cm): 168 (SD ± 6.8) Weight (kg): 60.1 (SD ± 9.5) BMI: 21.3 (± 3.4) ASA I: 14 ASA II: 16 Mallampati 1: 1 Mallampati 2: 27 Mallampati 3: 2 Macintosh Age: 37.2 (SD ± 15.4) Gender M/F: 11/19 Height (cm): 165.6 (SD ± 8.4) Weight (kg): 62. 4 (SD ± 12) BMI: 23.0 (± 5.6) ASA I: 12 ASA II: 18 Mallampati 1: 3 Mallampati 2: 27 Mallampati 3: 0 Country: Taiwan Setting: hospital | |
| Interventions | GlideScope (n = 30) vs Macintosh (n = 30) BURP manoeuvre used when required Use of double‐lumen tubes for all participants | |
| Outcomes | Continuous outcome: Time of intubation (time of DLT insertion calculated from time when the laryngoscope passed between participant's lips until 3 complete cycles of end‐tidal carbon dioxide displayed on the capnograph) Dichotomous outcomes: Laryngeal/airway trauma (blood on the device or oral bleeding) Patient‐reported sore throat (combined data for mild/moderate/severe classifications). Hoarseness data also presented but not reported in this review Successful first attempt No. of attempts: 1 to 3 or more | |
| Notes | Experience of intubator: 2 experienced anaesthetists with experience of ≥ 300 tracheal intubations with each device Funding/declarations of interest: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly assigned" Comment: no mention of method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "opening a sealed envelope" Comment: no mention if opaque |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: some outcomes were assessed by an independent observer, but study authors did not state whether this person was blinded. For theatre outcomes, assumed the assessor was not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Low risk | Comment: clinical trial register protocol sourced (unique identifier: NCT 014249605). Protocol outcomes comparable with study‐reported outcomes |
| Experience of intubator | Low risk | Quote: "two experienced anaesthesiologists with experience of at least 300 tracheal intubations with each device" |
| Baseline characteristics | Unclear risk | Comment: more men in Macintosh group. Impact of this difference is uncertain |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over design | |
| Participants | Total number of participants: 128 Inclusion criteria: age > 18 years, ASA I to III, full upper dentition at front Exclusion criteria: requiring awake fibreoptic intubation, with known laryngeal pathology or at risk of pulmonary aspiration Baseline characteristics: reported according to device with which participants were intubated McGrath Series 5 Age: 42.3 (SD ± 14.0) Gender M/F: 35/29 BMI: 28.5 (SD ± 5.0) ASA I: 21 ASA II: 37 ASA III: 6 Mallampati 1: 30 Mallampati 2: 26 Mallampati 3: 7 Mallampati 4: 1 Macintosh Age: 42.5 (SD ± 13.1) Gender M/F: 25/39 BMI: 27.9 (SD ± 6.0) ASA I: 23 ASA II: 39 ASA III: 2 Mallampati 1: 24 Mallampati 2: 34 Mallampati 3: 6 Mallampati 4: 0 Country: Australia Setting: hospital | |
| Interventions | McGrath Series 5 (n = 64) vs Macintosh (n = 64) Alternative device was used initially to record laryngoscopic view, then was removed. Device to which participants were randomized was then used to re‐record laryngoscopic view, then intubation was performed | |
| Outcomes | Continuous outcomes: Time of intubation: defined as time from when laryngoscope entered the mouth until first capnographic square wave Intubation difficulty score: reported as median (IQR (range)): McGrath 0 (0‐3 (0‐7)); Macintosh 2 (0‐3 (0‐7)); P = 0.0024 Dichotomous outcomes: Failed intubation Sore throat/hoarseness Laryngeal/airway trauma (dental damage, blood on blade, mucosal laceration, other airway trauma) CL glottic view: reported as differences between intubations with each device. Study authors state that view was worse when Macintosh was used as opposed to McGrath laryngoscope | |
| Notes | Experience of intubator: experienced anaesthetists; all were "clinically familiar with both devices and had undergone training in the use of the McGrath Series 5 before the start of the trial" Funding/declarations of interest: no external funding received Additional: manual in‐line stabilization performed on all participants | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "group allocation was achieved using a computer‐generated randomisation list and sealed envelopes" |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: no details of blinding; assumed no attempts were made |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Comment: experienced anaesthetists with at least 10 years' experience, described as clinically familiar with both devices and trained in use of McGrath before start of the trial. No further description of the degree of clinical experience to establish whether experience was sufficient and equivalent for each device |
| Baseline characteristics | Unclear risk | Comment: some differences in balance of gender between groups. Impact of this difference is uncertain |
| Funding sources | Low risk | Comment: no external funding sources |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 59 Inclusion criteria: ASA I or II, 18 to 65 years of age, scheduled for elective surgery requiring tracheal intubation Exclusion criteria: known or predicted difficult airway, obesity (BMI > 35 kg/m2), coronary artery or reactive airway disease, history of alcohol or substance abuse or gastro‐oesophageal reflux Baseline characteristics: GlideScope Age: median (IQR (range)) 46 (36‐50 (19‐59)) Height (cm): 158.0 (SD ± 5.9) Weight (kg): 56.9 (SD ± 11.9) ASA I: 16 ASA II: 13 Mallampati 1: 25 Mallampati 2: 4 Macintosh Age: median (IQR (range)) 38 (34‐45 (24‐51)) Height (cm): 155.8 (SD ± 5.8) Weight (kg): 57.7 (SD ± 11.3) ASA I: 16 ASA II: 14 Mallampati 1: 22 Mallampati 2: 8 Country: Singapore Setting: hospital | |
| Interventions | GlideScope (n = 29) vs Macintosh (n = 30) This study compared the median effective concentration of anaesthetic required for optimal intubating conditions for each device. Bias was introduced by this study design. Investigators provided data on difficulty of intubation | |
| Outcomes | Continuous outcomes: Difficulty of tracheal intubation Subjective data for difficulty of intubation included 5 variables (jaw relaxation, laryngoscopy, vocal cord, coughing, movement) recorded on scales. Median (IQR (range) ‐ GlideScope 8 (6‐0 (5‐12)); Mac 7 (6‐11 (5‐14) Study author quote: "There was no difference in the total intubation scores" | |
| Notes | Funding/declarations of interest: none apparent | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated list using the sealed envelope method" |
| Allocation concealment (selection bias) | Unclear risk | Comment: envelopes used, but no additional details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: outcome assessed by intubator |
| Incomplete outcome data (attrition bias) | High risk | Quote: "If the anaesthetist was unable to grade the intubating condition during the first attempt, the patient was excluded and subsequent airway management was performed according to the anaesthetist’s discretion The patient was replaced so that there would be 30 patients in each group" Comment: 5 exclusions due to inability to grade intubating conditions; may have introduced bias to results |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Comment: no information about experience of intubators |
| Baseline characteristics | Unclear risk | Comment: baseline characteristics largely equivalent. However, the mean age of participants in the Macintosh group is younger; unclear if this could result in easier intubations |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 200 Inclusion criteria: > 18 years old, recruited if modified Mallampati score was 3 or 4, history of a difficult intubation and mouth opening ≥ 2 cm Exclusion criteria: ASA ≥ IV, undergoing rapid sequence induction Baseline characteristics: Berci‐Kaplan VLS ‐ C‐MAC Age: 56.8 (range 18‐88) Height (cm): 172 (SD ± 10) Weight (kg): 83.2 (SD ± 20.8) Mallampati 1: 0 Mallampati 2: 1 Mallampati 3: 76 Mallampati 4: 23 Mallampati 4: 23 Macintosh Age: 54.2 (range 18‐94) Height (cm): 172 (SD ± 9) Weight (kg): 78.7 (SD ± 19.4) Mallampati 1: 0 Mallampati 2: 2 Mallampati 3: 87 Mallampati 4: 11 Country: Germany Setting: hospital | |
| Interventions | Berci‐Kaplan VLS (n = 100) vs Macintosh (n = 100) Optimizing manoeuvres used included external manipulation of the larynx (BURP manoeuvre), use of a gum‐elastic bougie (Eschmann stylet) and changes in head positioning. | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from when participant's mouth was opened until cuff of tube was inflated Dichotomous outcomes: Failed intubation CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: All intubations were performed by 2 experienced anaesthetists with 13 and 17 years of experience in clinical anaesthesia and at least 3 years of experience in difficult intubations Funding/declarations of interest: departmental funding only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐based randomization list" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details provided |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors for the included outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Quote: "All intubations were performed by two experienced anaesthesiologists with 13 and 17 yr of experience in clinical anaesthesia and at least 3 yr of experience in difficult intubations" Comment: no information on whether experience was equivalent for each device |
| Baseline characteristics | Low risk | Comment: comparable baseline characteristics |
| Funding sources | Low risk | Comment: departmental funding only |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 30 Inclusion criteria: scheduled for elective CABG Exclusion criteria: risk factors for gastric aspiration, difficult intubation or both (Mallampati class 3 or 4; thyromental distance < 6 cm; interincisor distance < 3.5 cm), left main coronary artery disease, poor left ventricular function, conduction abnormality, use of a permanent pacemaker Baseline characteristics: Pentax AWS Age: 59 (SD ± 8) Weight (kg): 62 (SD ± 5) Mallampati 1: mean 1.57 (SD ± 0.5) Macintosh Age: 55 (SD ± 8) Weight (kg): 65 (SD ± 10) Mallampati 1: mean 1.01 (SD ± 0.8) Country: India Setting: hospital | |
| Interventions | Pentax (n = 15) vs Macintosh (n = 15) Macintosh blade #3 in female, #4 in male patients | |
| Outcomes | Continuous outcome: Time for tracheal intubation (in seconds): defined as time from picking up laryngoscopy to when the blade was removed from the mouth after successful intubation | |
| Notes | Experience of intubator: 3 consultant anaesthetists who learnt and performed at least 20 intubations with the new device in the clinical setting, before the study Funding/declarations of interest: none apparent Additional: aim to look at haemodynamic changes for patients with CABG; reports time for intubation as only relevant outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The allocation sequence was generated by random number tables" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Data were collected by an independent unblinded observer" |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "Tracheal intubation was performed in each patient by one of the three consultant anaesthesiologists who learnt and performed at least 20 intubations with the new device in the clinical setting, prior to the study" |
| Baseline characteristics | Low risk | Quote: "The demographic data, incidence of hypertension, serum creatinine, LV ejection fraction, and Mallampatti score were similar in both the groups" |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 60 Inclusion criteria: adult patients scheduled for elective surgery requiring general anaesthesia with endotracheal intubation and with ASA I to III Exclusion criteria: gastro‐oesophageal reflux disease, with abnormal physical status of the upper airway (e.g. after C‐spine trauma), C‐spine previously operated on, oropharyngeal or hypopharyngeal tumours, macroglossia, mandibular retrusion, other known airway difficulties Baseline characteristics: GlideScope Age: 61 (SD ± 15) Gender M/F: 13/17 Height (cm): 169 (SD ± 9) Weight (kg): 82 (SD ± 7) BMI: 28.8 (SD ± 3.5) Mallampati 1: 5 Mallampati 2: 19 Mallampati 3: 6 Macintosh Age: 63 (SD ± 12) Gender M/F: 19/11 Height (cm): 172 (SD ± 8) Weight (kg): 84 (SD ± 12) BMI: 28.3 (SD ± 5.8) Mallampati 1: 9 Mallampati 2: 17 Mallampati 3: 4 Country: Germany Setting: hospital | |
| Interventions | GlideScope (n = 30) vs Macintosh (n = 30) GlideScope blade #4, Macintosh blade #3 or #4 External laryngeal pressure allowed to improve glottic view in both groups | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from beginning of laryngoscopy to successful placement of ET tube; median (min/max): VLS 53 (28 ‐ 210) seconds; Mac 24 (min/max12 ‐ 75) seconds Dichotomous outcome: Failed intubation (3 participants randomized to the conventional group in which conventional intubation failed, intubation could be successfully performed with videolaryngoscopy) | |
| Notes | Experience of intubator: 33 laryngoscopists participated in the study; GlideScope experience of all participating anaesthesiologists: mean 9.9 (SD ± 8.6) intubations. The GlideScope had been available for 6 months before this investigation Funding/declarations of interest: travel grant from Verathon Europe. Study authors declare no conflicts of interest Other information: all anaesthesiologists were instructed to avoid moving the C‐spine to minimize C‐spine movements during laryngoscopy, but head and neck were not immobilized | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Immediately after induction of anesthesia, the patients were randomly assigned" Comment: no details on method of randomization |
| Allocation concealment (selection bias) | Unclear risk | Quote: "sealed envelope randomization" Comment: insufficient details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: attempts at blinding for some study outcomes, but not possible to blind for relevant review outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "All enrolled patients were able to be included in further evaluation" |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | High risk | Quote: "Thirty‐three laryngoscopists participated in the study; the GlideScope experience of all participating anesthesiologists was a mean of 9.9 (± 8.6) intubations. The GlideScope had been available for a period of 6 months before this investigation" Comment: large number of participating physicians with differing skill levels |
| Baseline characteristics | Low risk | Quote: "no significant differences in biometric data" |
| Funding sources | High risk | Comment: travel grant from Verathon Europe. Study authors declare no conflicts of interest. |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 46 Inclusion criteria: aged 20 years or older, undergoing uvulopalatopharyngoplasty under general anaesthesia; diagnosis of obstructive sleep apnoea, confirmed by polysomnography, but otherwise healthy; ASA I or II Exclusion criteria: loosened teeth or mouth opening < 18 mm; any pathology in the neck, pharynx or larynx; risk factor for aspiration of gastric contents; history of hypersensitivity to an anaesthetic drug Baseline characteristics: Pentax AWS Age: 45.8 (range 23–62) Gender M/F: 16/6 BMI: 25.6 (SD ± 3.5) ASA I: 11 ASA II: 11 Mallampati 1: 0 Mallampati 2: 5 Mallampati 3: 10 Mallampati 4: 7 Macintosh Age: 43.7 (range 19‐64) Gender M/F: 19/4 BMI: 25.8 (SD ± 3.2) ASA I: 9 ASA II: 14 Mallampati 1: 4 Mallampati 2: 9 Mallampati 3: 6 Mallampati 4: 4 Country: Republic of Korea Setting: hospital | |
| Interventions | Pentax AWS (n = 23) vs Macintosh (n = 23) With the AWS, a well‐lubricated tracheal tube was attached to a channel on the right side of the tube before insertion. When the Macintosh laryngoscope was used, a gum‐elastic bougie could be used. | |
| Outcomes | Continuous outcomes: Time for tracheal intubation Difficulty of intubation: IDS scores Dichotomous outcomes: Failed intubation: defined as an attempt in which the trachea was not intubated or an attempt that took > 60 seconds to complete Laryngeal/airway trauma (visible trauma to lip or oral mucosa, bleeding, or dental trauma) Successful first attempt No. of attempts: 1 or 2 CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: both anaesthetists experienced > 3 years of clinical anaesthesia, and had performed > 500 and ≥ 100 tracheal intubations with the Macintosh laryngoscope and the AWS, respectively. Funding/declarations of interest: none | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly allocated into either the Macintosh group or AWS group" Comment: no additional details |
| Allocation concealment (selection bias) | Unclear risk | Quote: "sealed envelope method" Comment: insufficient details |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "it was impossible to blind both the operator and the observer to the device being used" |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "An independent, but unblinded observer collected all data in every case of this trial" |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "In a total of 46 patients enrolled, one patient in the AWS group was excluded because of a change in surgical plan" Comment: low level of loss should not affect results |
| Selective reporting (reporting bias) | Low risk | Quote: "studies and registration in clinicaltrials.gov (Unique Identifier: NCT01428570)" Comment: protocol sourced and outcomes comparable with reported study outcomes |
| Experience of intubator | Low risk | Quote: "Before this study, both anaesthetists experienced >3 yr of clinical anaesthesia, and had performed >500 and at least 100 tracheal intubations with the Macintosh laryngoscope and the AWS in patients, respectively" |
| Baseline characteristics | Unclear risk | Quote: "randomization of this study was not fully achieved. Even though the best efforts of randomization were made, more patients with higher Mallampati classification were included in the AWS group. This could be attributed to the limited number of patients recruited. However, the AWS was shown to overcome such a disadvantage" Comment: differences in baseline characteristics in the Mallampati scores. Impact of this difference is uncertain |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 100 Inclusion criteria: scheduled for various surgical procedures requiring tracheal intubation as part of anaesthesia, 18 years of age or older, ASA I to III Exclusion criteria: increased risk of pulmonary aspiration, cervical spine pathology or anticipated airway difficulties (i.e. Mallampati grade 4 or thyromental distance 6 cm) Baseline characteristics: Pentax AWS Age: 60 (SD ± 19) Gender M/F: 20/30 Height (cm): 158 (SD ± 9) Weight (kg): 56 (SD ± 10) Mallampati 1: 26 Mallampati 2: 17 Mallampati 3: 7 Mallampati 4: 0 Macintosh Age: 53 (SD ± 18) Gender M/F: 28/22 Height (cm): 162 (SD ± 2) Weight (kg): 58 (SD ± 10) Mallampati 1: 28 Mallampati 2: 14 Mallampati 3: 8 Mallampati 4: 0 Country: Japan Setting: hospital | |
| Interventions | Pentax (n = 50) vs Macintosh (n = 50) Macintosh blade #3 | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from picking up the laryngoscope to confirmation of tracheal intubation by capnography. In the event that tracheal intubation was accomplished after 1 or 2 failed attempts, times for all individual intubation attempts were totalled to calculate intubation time. Improved visualization (with POGO) Dichotomous outcomes: Failed intubation: defined as unsuccessful after 3 attempts, then change of device used. Any single insertion of Airway scope or Macintosh laryngoscope into the participant's mouth was considered an intubation attempt. Laryngeal/airway trauma (mucosal trauma, i.e. blood detected on the devices, dental injury) Hypoxia CL glottic view: 1 to 4 No. of attempts: 1 to 3 | |
| Notes | Funding/declarations of interest: instruments loaned from manufacturers. No financial support Additional: All participants had laryngoscopy performed with Macintosh #3 in normal position to obtain grades, then table was moved up alongside normal operating table for anaesthetist to kneel on to simulate ground position. Laryngoscopic view was taken again with #3 Macintosh, then intubation was performed in randomized groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was based on computer‐generated codes" |
| Allocation concealment (selection bias) | Low risk | Quote: "maintained in sequentially numbered, opaque envelopes until just before experimental intubation" |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Both investigators were blinded to the laryngeal view obtained by the other, and to the results of laryngoscopy performed under optimal conditions before group assignment" Comment: not possible to blind anaesthetists to primary outcomes |
| Blinding of outcome assessment (detection bias) | High risk | Comment: both investigators were blinded to the laryngeal view obtained by the other, and to the results of laryngoscopy performed under optimal conditions before group assignment. Not possible to blind other outcome data |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Quote: "The investigator... had previously performed 150 intubations using the Airway Scope in an optimal intubation condition, but none at the ground level" |
| Baseline characteristics | Unclear risk | Quote: "Morphometric and airway assessment data of patients assigned to either the Airway Scope or the Macintosh laryngoscope were similar" Comment: more males in Macintosh group. Impact of this difference is uncertain |
| Funding sources | Unclear risk | Comment: instruments loaned from manufacturers. No financial support |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 44 Inclusion criteria: no details given Exclusion criteria: younger than 18 years of age, requiring other than blade #3 of laryngoscope, ASA ≥ IV, requiring surgery of the face or throat Baseline characteristics: Cross‐over design. Baseline characteristics not divided by type of scope but by gender Female Age: 50 (SD ± 16) BMI: 26.8 (SD ± 5.5) ASA I: 11 ASA II: 12 ASA III: 1 Mallampati 1: 7 Mallampati 2: 14 Mallampati 3: 2 Mallampati 4: 1 Male Age: 56 (SD ± 13) BMI: 302 (SD ± 8.5) ASA I: 3 ASA II: 14 ASA III: 3 Mallampati 1: 10 Mallampati 2: 8 Mallampati 3: 2 Mallampati 4: 0 Country: The Netherlands Setting: hospital | |
| Interventions | Storz VLS (type not specified by study authors) vs Macintosh Cross‐over design with 2 scopes; each participant having both scopes (in a randomized order) with 2 anaesthetists | |
| Outcomes | Dichotomous outcomes: Failed intubation Laryngeal/airway trauma (injuries or dental damage) CL glottic view: 1 to 4. Not possible to extract data for this outcome (presented as correlation data with Mallampati scores) | |
| Notes | Funding/declarations of interest: none Additional: unclear whether 3 participants were lost during the study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: patients randomly selected to participate. Order of blades randomly decided. No additional details |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: assumed not blinded ‐ no details |
| Incomplete outcome data (attrition bias) | High risk | Comment: some apparent loss, not explained ‐ 3 missing participants from VLS group. Unexplained discrepancies in tables |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "Ten anesthesiolgists (4 specialists, 6 residents), all familiar with the videolaryngoscope (minimum 30 uses) and classical intubation practices, participated in the study" |
| Baseline characteristics | Low risk | Comment: comparable baseline characteristics |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over with 4 scopes | |
| Participants | Total number of participants: 50 Inclusion criteria: selected from a population of elective surgical patients. No additional details provided Exclusion criteria: younger than 18 years of age, requiring other than a #3 blade Macintosh laryngoscope, ASA ≥ IV, without both upper and lower teeth, requiring surgery of the face and/or throat Baseline characteristics: GlideScope Age: 56 (SD ± 17) Gender M/F: 6/19 BMI: 25 (SD ± 4) ASA I: 10 ASA II: 15 ASA III: 0 Macintosh Age: 54 (SD ± 16) Gender M/F: 10/15 BMI: 26 (SD ± 4) ASA I: 9 ASA II: 14 ASA III: 2 McGrath Series 5 Age: 55 (SD ± 16) Gender M/F: 4/21 BMI: 26 (SD ± 5) ASA I: 9 ASA II: 14 ASA III: 2 V‐Mac Storz Berci DCI Age: 52 (SD ± 16) Gender M/F: 10/15 BMI: 25 (SD ± 3) ASA I: 9 ASA II: 14 ASA III: 2 Country: The Netherlands Setting: hospital | |
| Interventions | GlideScope (n = 25); McGrath Series 5 (n = 25); VMac (n = 25); Macintosh (n = 25). Total N = 50 Participants randomly assigned to receive a pair of scopes in random order | |
| Outcomes | Continuous outcomes: Time for tracheal intubation: measured as time between picking up the ETT and positioning the tube directly anterior to the vocal cords at < 30 seconds, 30 to 60 seconds, > 60 seconds. Intubation time was measured as the sum of all attempts. Not possible to use these data, as not similar to other data in the review. Study author quote: "The time taken to complete the placement of the ETT with the McGrath™ scope (Aircraft Medical) was significantly different from the other blades, with a greater proportion of the attempts requiring more than 30 s. There was also a statistically significant difference in time taken for the procedure between the Macintosh (Karl Storz) and GlideScope® blades (Verathon Inc), with the GlideScope® blade (Verathon Inc) having more attempts requiring between 30 and 60 s. No further differences in insertion time were significant" Dichotomous outcomes: Failed intubation: defined as more than 4 attempts or > 120 seconds Laryngeal/airway trauma Successful first attempt No. of attempts: 1 to 4 CL glottic view: 1 to 3 | |
| Notes | Experience of intubator: all laryngoscopies were performed by available staff members (only senior residents and specialists), all of whom were experienced in anaesthesia and use of the VLS studied. All staff members received an introductory VLS course in the hospital’s airway skills lab and had used each VLS a minimum of 50 times before this study. Funding/declarations of interest: none apparent | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: participants randomly assigned to set of 2 blades, which were used in randomized order. No details of randomization method provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: outcome assessors were independent but it was not possible to blind them from group allocation |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Comment: large number of anaesthetists in the study; all described as having equivalent training |
| Baseline characteristics | Unclear risk | Comment: more males in Macintosh and Berci DCI group. Impact of this difference is uncertain |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 40 Inclusion criteria: 18 to 60 years old, ASA I or II, scheduled for elective surgery that was expected to take 1 to 2 hours Exclusion criteria: known cardiovascular disease, diabetes, endocrine disease, allergies to any medications; anatomical characteristics associated with a difficult airway, such as unstable teeth, mouth opening < 3 cm, limited neck extension Baseline characteristics: Pentax AWS Age: 38.9 (SD ± 13.3) Gender M/F: 12/8 Height (cm): 168 (SD ± 9.3) Weight (kg): 64.9 (SD ± 8.2) BMI: 23.0 (SD ± 2.6) Macintosh Age: 35.5 (SD ± 10.5) Gender M/F: 11/9 Height (cm): 166.5 (SD ± 9.8) Weight (kg): 66.0 (SD ± 14.9) BMI: 23.6 (SD ± 3.9) Country: Korea Setting: hospital | |
| Interventions | Pentax AWS (n = 20) vs Macintosh (n = 20) | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from when the tip of the blade passes the incisors until the tip of the blade passes out of the incisors after insertion of the tracheal tube Dichotomous outcome: Patient‐reported sore throat: measured at different time points; mild to moderate sore throat measured 30 minutes after extubation. Not possible to interpret data presented for sore throat at 30 minutes. No sore throat observed 24 hours after extubation in either group | |
| Notes | Experience of intubator: single anaesthesiologist who was an expert in both intubation procedures Funding/declarations of interest: none apparent Additional: "If tracheal intubation failed at the first attempt or if a patient’s Cormack‐Lehane score was greater than three, the patient was immediately excluded from the study" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients were randomly assigned to the two groups" Comment: no additional details |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind time to intubation outcome. However, nurses assessed sore throat in PACU and were blinded |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "single anesthesiologist who was an expert in both intubation procedures" |
| Baseline characteristics | Low risk | Quote: "There was no significant difference between the two groups in demographic data" |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 60 Inclusion criteria: ASA I or II admitted for elective gynaecological procedures, Mallampati grades 1 and 2 Exclusion criteria: risk of aspiration, evidence of a potentially difficult airway Baseline characteristics: GlideScope Age: 39 (SD ± 13) Height (cm): 158.3 (SD ± 4.5) Weight (kg): 57.8 (SD ± 10.5) ASA I: 23 ASA II: 7 Mallampati 1: 25 Mallampati 2: 5 Macintosh Age: 40 (SD ± 10) Height (cm): 157.5 (SD ± 4.7) Weight (kg): 58.2 (SD ± 8.9) ASA I: 28 ASA II: 2 Mallampati 1: 26 Mallampati 2: 4 Country: Singapore Setting: hospital | |
| Interventions | GlideScope (n = 30) vs Macintosh (n = 30) Stylet used in both groups | |
| Outcomes | Continuous outcomes: Difficulty of tracheal intubation: Median difficulty score for GlideScope group was 20 (range 0‐90) and for Macintosh group 10 (range 0‐70). Time for tracheal intubation: defined as time from anaesthetist picking up device to when capnography confirmed correct placement of the tube. Intubation time was broken down by level of experience of the intubator. Dichotomous outcomes: Failed intubation: defined as inability to secure airway in 3 attempts Laryngeal/airway trauma Successful first attempt No. of attempts: 1 to 2 CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: 20 anaesthetists in the department with varying degrees of experience with GlideScope (from complete novice to more than 10 successful experiences) Funding/declarations of interest: none Addtional: in‐line manual stabilization of head and neck to simulate difficult airway | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: described as randomized with sealed envelopes. Insufficient details |
| Allocation concealment (selection bias) | Unclear risk | Comment: sealed envelopes. No further details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: outcome assessors independent ‐ but not described as blinded for any outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | High risk | Comment: differing levels of experience of intubators, all detailed by study authors. Not clear whether experience of intubators was evenly distributed for each device |
| Baseline characteristics | Low risk | Comment: comparable baseline characteristics |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 170 Inclusion criteria: adults scheduled for elective open thoracic surgery requiring double‐lumen tube insertion for 1‐lung ventilation Exclusion criteria: limited mouth opening, ASA III or IV, age < 18 years, history of known difficult airway Baseline characteristics: CEL‐100 Age: 58.2 (SD ± 9.6) Gender M/F: 55/28 Height (cm): 162.5 (SD ± 7.5) Weight (kg): 60.9 (SD ± 8.9) BMI: 22.9 (SD ± 2.7) ASA I: 60 ASA II: 16 ASA III: 7 Mallampati 1: 40 Mallampati 2: 36 Mallampati 3: 7 Mallampati 4: 0 Macintosh Age: 57.6 (SD ± 9.4) Gender M/F: 52/30 Height (cm): 163.1 (SD ± 7.3) Weight (kg): 61.2 (SD ± 8.3) BMI: 23.1 (SD ± 2.8) ASA I: 59 ASA II: 17 ASA III: 6 Mallampati 1: 45 Mallampati 2: 31 Mallampati 3: 6 Mallampati 4: 0 Country: China Setting: hospital | |
| Interventions | CEL‐100 videolaryngoscope (n = 85) vs Macintosh (n = 85) CEL‐100 from Connell energy Technology Co. Ltd, Shanghai, China Use of stylet, and external laryngeal pressure if required | |
| Outcomes | Continuous outcomes: Difficulty of tracheal intubation: subjectively assessed from 0: easy, to 100: difficult IDS scores: median (IQR) 0 = easy, 100 = difficult. CEL‐100 0 (0‐0 (0‐60)); Macintosh 15 (0‐30 (0‐80)) Time for tracheal intubation: defined as time from insertion of laryngoscope blade into the mouth until first upstroke of the capnograph trace; If more than 1 intubation attempt was required, successful intubation time was the sum of the times for each attempt and did not include the time interval between attempts). Median (IQR) ‐ CEL‐100 45 (38‐55); Mac 51 (40‐61) out of 83 and 82 participants Dichotomous outcomes: Failed intubation: defined as failure after 3 attempts for either device with trachea intubated with a single‐lumen tube or managed according to ASA difficult airway guidelines. Participants were then excluded from the study. Laryngeal/airway trauma (oral mucosal bleeding) Patient‐reported sore throat (or hoarseness, reported on first postoperative day) Hypoxia: oxygen saturation < 95% ‐ reported as hypoxaemia. "No episodes in either group" Successful first attempt No. of attempts: 1 or > 2 CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: all intubations were performed by 3 experienced anaesthetists who had each performed at least 30 successful double‐lumen tube insertions using the CEL‐100 device Funding/declarations of interest: none Additional: use of double‐lumen tube in both groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated codes" |
| Allocation concealment (selection bias) | Low risk | Quote: "maintained in sequentially numbered opaque envelopes" |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "All postoperative data were collected by one independent observer who was blinded to the study randomisation" Comment: some outcomes, such as time for intubation, could not be blinded because of the nature of the intervention |
| Incomplete outcome data (attrition bias) | Low risk | Comment: 5 participants excluded from further analysis owing to failure of intubation. Low number, therefore low risk of bias |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "All the intubations were performed by three experienced anaesthetists who had each performed at least 30 successful double‐lumen tube insertions using the CEL‐100 device" |
| Baseline characteristics | Low risk | Quote: "Patients’ characteristics, pre‐operative airway assessments and the tubes used in the study were similar in both groups" |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 80 Inclusion criteria: adult patients, ASA physical status II or III, scheduled for elective coronary artery bypass surgery requiring endotracheal intubation and intra‐arterial blood pressure monitoring Exclusion criteria: obesity (BMI > 35 kg/m2), chronic obstructive pulmonary disease, history of difficult intubation, mouth opening < 3 cm, inadequate neck mobility or left ventricular ejection fraction < 45% Baseline characteristics: Cross‐over design, all reported together Age: 66.2 (SD ± 10.2) Gender M/F: 55/25 Height (cm): 172 (SD ± 9) Weight (kg): 80.9 (SD ± 15.5) BMI: 27.0 (SD ± 4) ASA I: 0 ASA II: 67 ASA III: 13 Mallampati 1: 34 Mallampati 2: 41 Mallampati 3: 5 Mallampati 4: 0 Countries: Belgium and The Netherlands Setting: hospital | |
| Interventions | Storz C‐MAC vs Macintosh, cross‐over in randomized order Extra manoeuvres to optimize visualization of the glottis entrance (BURP). A stylet or a gum‐elastic bougie was used to facilitate intubation. | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time between picking up the ETT and visual passage of the tube until vocal cords were between the 2 black line markings on the distal end of the ETT. However, data were not reported by study authors. Dichotomous outcomes: Failed intubation Laryngeal/airway trauma (reported for palatoglossal arch or dental injury) Patient‐reported sore throat: Only 3 participants, who had an effective airway time longer than 50 seconds, reported postoperative minor, self‐limiting sore throat, which did not require treatment. Study authors did not state to which group these participants were assigned. No. of attempts: counted as each approach of the endotracheal tube (ETT) to the glottis entrance. If after 2 attempts the participant could not be intubated, a stylet or a gum‐elastic bougie was used to facilitate intubation. However, no data were reported by study authors for this outcome. | |
| Notes | Funding/declarations of interest: none apparent Additional: Only data on failed intubation could be extracted for this study. All other outcomes were not relevant or were wrongly reported for our review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "We performed a randomized cross‐over study, in which each patient received sequential treatments in a random order" Comment: participants selected a sealed card. Insufficient details |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details given |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "attending anaesthesiologist was not blinded to the type of laryngoscope used" |
| Blinding of outcome assessment (detection bias) | High risk | Comment: sore throat assessed by blinded investigator but not possible to blind personnel to primary outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought. Data not reported for number of attempts |
| Experience of intubator | Unclear risk | Comment: no details of anaesthetist experience |
| Baseline characteristics | Unclear risk | Comment: no baseline characteristics by group owing to cross‐over design |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 120 Inclusion criteria: ASA I to III, aged 16 years or older, undergoing surgical procedures requiring tracheal intubation Exclusion criteria: risk factors for gastric aspiration, difficult intubation or both (Mallampati class 3 or 4; thyromental distance < 6 cm; interincisor distance < 3.5 cm); history of relevant drug allergy Baseline characteristics: GlideScope Age: 45.03 (range 23‐80) Gender M/F: 8/22 BMI: 26.5 (SD ± 3.3) ASA median (IQR): 2 (1‐2) Mallampati 1: 10 Mallampati 2: 20 Pentax AWS Age: 43.9 (range 20‐68) Gender M/F: 11/19 BMI: 26.0 (SD ± 6.0) ASA median (IQR): 2 (1‐2) Mallampati 1: 12 Mallampati 2: 18 Truview EVO2 Age:43.2 (range 21‐83) Gender M/F: 20/10 BMI: 25.3 (SD ± 3.5) ASA median (IQR): 2 (1‐2) Mallampati 1: 14 Mallampati 2: 16 Macintosh Age: 50.8 (range 18‐82) Gender M/F: 11/19 BMI: 25.7 (SD ± 4.1) ASA median (IQR): 2 (1‐2) Mallampati 1: 13 Mallampati 2: 17 Country: Ireland Setting: hospital | |
| Interventions | GlideScope (n = 30) vs Pentax AWS (n = 30) vs Truview EVO2 (n = 30) vs Macintosh (n = 30) Truview EVO2 was used with camera attachment and therefore was included in this review. Stylet was used for GlideScope and Truview EVO2 laryngoscopes. ETT was placed in side channel of Pentax AWS before intubation attempt. Bougie, cricoid pressure, and second assistant were used for all scopes. Macintosh blade #3 was used in females and #4 in males | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from insertion of the blade between the teeth until the ETT was placed through the vocal cords Dichotomous outcomes: Failed intubation: defined as trachea not intubated, or took > 60 seconds; maximum of 3 attempts, then manual in‐line axial stabilization discontinued and Macintosh blade used Laryngeal/airway trauma (blood on laryngoscope blade, minor laceration, dental or other airway trauma) Successful first attempt No. of attempts: 1 to 3 CL glottic view: 1 to 4 IDS scores: 0 to 7 | |
| Notes | Experience of intubator: each investigator had performed at least 50 intubations with each device in manikins, and at least 20 intubations with each device in the clinical setting Funding/declarations of interest: Both Pentax and Truview were provided by manufacturers. Departmental funding only Additional: all participants underwent manual in‐line axial stabilization | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "allocation sequence was generated by random number tables" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "allocation concealed in sealed envelopes, which were not opened until patient consent had been obtained" Comment: insufficient details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "All data were collected by an independent unblinded observer" |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "Tracheal intubation was performed in each patient by one of the three anaesthetists... Each investigator had performed at least 50 intubations with each device in manikins, and at least 20 intubations in the clinical setting with each device" |
| Baseline characteristics | Unclear risk | Quote: "There were no significant differences in patient characteristics or baseline airway parameters between the groups, with the exception of a greater number of male patients in the Truview EVO2 group" Comment: higher mean age of participants in the Macintosh group and differences in ratio of male to female participants between groups. Unclear if this made intubations more difficult in this group |
| Funding sources | Unclear risk | Comment: both Pentax and Truview were provided by manufacturers. Departmental funding only |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 60 Inclusion criteria: ASA I to III, aged 16 years or older, undergoing general anaesthesia for surgery and requiring tracheal intubation Exclusion criteria: risk factors for gastric aspiration, difficult intubation (Mallampati class 3 or 4; thyromental distance < 6 cm; interincisor distance < 3.5 cm) or both, history of relevant drug allergy Baseline characteristics: Pentax AWS Age: 50.4 (range 23‐82) Gender M/F: 13/17 BMI: 26.9 (SD ± 4.1) Macintosh Age: 47.4 (range 18‐78) Gender M/F: 18/12 BMI: 26.3 (SD ± 4.9) Country: Ireland Setting: hospital | |
| Interventions | Pentax AWS (n = 30) vs Macintosh (n = 30) | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from insertion of blade between the teeth until tracheal tube was placed through the vocal cords. Median (IQR): AWS 11 (9‐13); Macintosh 11 (9‐15) Dichotomous outcomes: Failed intubation (defined as an attempt in which the trachea was not intubated, or that required > 120 seconds to perform) Laryngeal/airway trauma (blood on laryngoscope blade, minor laceration, dental or other airway trauma) Successful first attempt No. of attempts: 1 to 3 CL glottic view: 1 to 4 IDS score: 0 to 7 | |
| Notes | Experience of intubator: 1 of 3 anaesthetists who were familiar with each of the devices. Each investigator had performed, with each device, at least 50 intubations in manikins and at least 20 intubations in the clinical setting Funding/declarations of interest: Pentax AWS supplied by manufacturer. Departmental funding only Additional: study also included an LMA CTrach laryngoscope, which does not meet our inclusion criteria; therefore, we have not included data for this arm. All participants were given manual in‐line axial stabilization | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "allocation sequence was generated by random number tables" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "allocation concealed in sealed envelopes, which were not opened until patient consent had been obtained" Comment: insufficient details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "data were collected by an independent unblinded observer" |
| Incomplete outcome data (attrition bias) | Low risk | Comment: data for CL scores not available for 3 patients in the Macintosh group, but overall few losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "one of the three anaesthetists...who were familiar with each of the devices. Each investigator had performed, with each device, at least 50 intubations in manikins and at least 20 intubations in the clinical setting" |
| Baseline characteristics | Unclear risk | Quote: "There were no significant differences in characteristics or baseline airway parameters between the groups" Comment: more males in Macintosh group. Impact of this difference is uncertain |
| Funding sources | Unclear risk | Comment: Pentax AWS supplied by manufacturer. Departmental funding only |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 75 Inclusion criteria: ASA I to III, aged 16 years or older, deemed on preoperative assessment by the primary anaesthetist to be at increased risk for difficult laryngoscopy, undergoing surgical procedures requiring tracheal intubation Exclusion criteria: risk factors for gastric aspiration, history of relevant drug allergy Baseline characteristics: GlideScope Age: 55 (range 22‐85) Gender M/F: 13/12 BMI: 34.4 (SD ± 10.7) Mallampati 1: 0 Mallampati 2: 0 Mallampati 3: 20 Mallampati 4: 5 Pentax AWS Age: 60 (range 29‐84) Gender M/F: 14/11 BMI: 33.4 (SD ± 7.2) Mallampati 1: 0 Mallampati 2: 1 Mallampati 3: 21 Mallampati 4: 3 Macintosh Age: 54 (range 26‐85) Gender M/F: 16/9 BMI: 33.6 (SD ± 9.4) Mallampati 1: 0 Mallampati 2: 0 Mallampati 3: 19 Mallampati 4: 6 Country: Ireland Setting: hospital | |
| Interventions | GlideScope (n = 25) vs Pentax AWS (n = 25) vs Macintosh (n = 25) Use of bougie, external laryngeal manipulation, second assistant for all 3 scopes Stylet used in GlideScope bent into hockey stick curve Macintosh blade #3 in females; #4 in males | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from insertion of the blade between the teeth until the TT was placed through the vocal cords. Time for successful attempt: median (IQR): AWS 15 (8‐31); GlideScope 17 (12‐31); Macintosh 13 (8‐23) Dichotomous outcomes: Failed intubation Laryngeal/airway trauma (minor: visible trauma to lip or oral mucosa or blood on the laryngoscope) Successful first attempt No. of attempts: 1 to 3 CL glottic view: 1 to 4 IDS score: 0 to 8 or > 8 | |
| Notes | Note more obese patients (BMI > 30) in all 3 groups Experience of intubator: each anaesthetist had performed more than 500 intubations with the Macintosh laryngoscope and at least 100 intubations with the Pentax AWS and GlideScope in manikins, and 50 intubations with the Pentax AWS and GlideScope in the clinical setting, before this study Funding/declarations of interest: Pentax provided by manufacturers. Departmental funding only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "random number tables" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "allocation concealed in sealed envelopes" Comment: insufficient details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "All data were collected by an independent unblinded observer" |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no losses reported in CONSORT figure |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "Each anaesthetist had performed more than 500 intubations with the Macintosh laryngoscope and at least 100 intubations with the Pentax AWS and GlideScope in manikins, and 50 intubations with the Pentax AWS and GlideScope in patients" |
| Baseline characteristics | Low risk | Comment: comparable baseline characteristics, although slightly higher number of males in Macintosh group |
| Funding sources | Unclear risk | Quote: "Pentax Ltd provided the Pentax AWS device and disposable blades free of charge for use in the study" |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 13 Inclusion criteria: aged 41 to 68 years, ASA I or II, scheduled to undergo elective surgery requiring general anaesthesia with tracheal intubation Exclusion criteria: previous neck surgery, possible pregnancy, difficult intubation anticipated, without incisor teeth Baseline characteristics: Cross‐over design with baseline characteristics reported together for 11 participants (2 excluded owing to technical difficulties) Age: 50 (range 41‐68) Gender M/F: 7/4 Height (cm): 161 (range 150‐175) Weight (kg): 55 (range 41‐75) Mallampati 1: 10 Mallampati 2: 1 Mallampati 3: 0 Mallampati 4: 0 Country: Japan Setting: hospital | |
| Interventions | Pentax AWS vs Macintosh | |
| Outcomes | Continuous outcomes: Improved visualization ("Assessment of the glottic view during laryngoscopy by Cormack–Lehane grading resulted in a score of 1 with the AWS and a score of 2 with the Macintosh laryngoscope in all patients") Time for tracheal intubation: defined as time when the Macintosh laryngoscope or the AWS passed the central incisors to time when the tip of the tracheal tube passed through the glottis | |
| Notes | Experience of intubator: Study authors stated, "The operator was familiar with both devices, and his technique was consistent"; however, no further information was provided to reveal level of experience Funding/declarations of interest: Airway scope provided by manufacturer Additional: video‐fluoroscopic study. Head immobilised with blocks and restraining bands | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: described as randomized, no additional details |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details given |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: assumed outcome assessor not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Two of the 13 patients were excluded from the study because of technical difficulties" Comment: moderate loss |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Comment: no details on amount of experience with Pentax |
| Baseline characteristics | Unclear risk | Comment: cross‐over design; baseline characteristics not divided by group |
| Funding sources | Unclear risk | Quote: "The AirWay Scope was provided by Pentax Corporation" |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 24 Inclusion criteria: aged 18 to 82 years, ASA I or II, scheduled to undergo elective surgery requiring general anaesthesia with tracheal intubation Exclusion criteria: previous neck surgery, possible pregnancy, unstable C‐spine, difficult intubation anticipated, without incisors Baseline characteristics: AWS Age: 50.8 (range 27‐82) Gender M/F: 6/6 Height (cm): 162.0 (SD ± 7.1) Weight (kg): 58.0 (SD ± 6.5) Mallampati 1: 8 Mallampati 2: 4 Mallampati 3: 0 Mallampati 4: 0 Macintosh Age:48.1 (range 24‐63) Gender M/F: 6/6 Height (cm): 161.6 (SD ± 10.2) Weight (kg): 56.5 (SD ± 13.6) Mallampati 1: 8 Mallampati 2: 4 Mallampati 3: 0 Mallampati 4: 0 Country: Japan Setting: hospital | |
| Interventions | Pentax AWS (n = 12) vs Macintosh (n = 12) | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time when the laryngoscope or the AWS passed the central incisors to time when the anaesthetist withdrew the device from the participant's mouth after tracheal intubation Dichotomous outcome: CL glottic view: 1 to 4 | |
| Notes | Funding/declarations of interest: Pentax AWS supplied by manufacturer Additional: study also included a group using a McCoy laryngoscope, which was not eligible for inclusion in this review; therefore, we did not extract data for this group. Fluoroscopic comparisons, but some relevant outcome data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: described as randomized with no additional details |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: assumed outcome assessors not blinded |
| Incomplete outcome data (attrition bias) | High risk | Comment: 5 withdrawals. Most resulted from problems with recording data during laryngoscopies. High attrition rate |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Comment: no details |
| Baseline characteristics | Low risk | Comment: comparable baseline characteristics |
| Funding sources | Unclear risk | Comment: Pentax AWS supplied by manufacturer |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 90 Inclusion criteria: ASA I to III, aged 16 years or older, undergoing surgical procedures requiring tracheal intubation Exclusion criteria: risk factors for gastric aspiration, difficult intubation or both (Mallampati class 3 or 4; thyromental distance < 6 cm; interincisor distance < 3.5 cm), history of relevant drug allergy Baseline characteristics: C‐MAC Age: 54 (SD ± 20) Gender M/F: 10/20 BMI: 29 (SD ± 5) Mallampati 1: 11 Mallampati 2: 19 Mallampati > 2: 0 Macintosh Age: 58 (SD ± 20) Gender M/F: 19/12 BMI: 28 (SD ± 7) Mallampati 1: 12 Mallampati 2: 18 Mallampati > 2: 1 Airtraq Age: 52 (SD ± 19) Gender M/F: 14/15 BMI: 28 (SD ± 4) Mallampati 1: 13 Mallampati 2: 16 Mallampati > 2: 0 Country: Ireland Setting: hospital | |
| Interventions | C‐MAC (n = 30) vs Airtraq (n = 29) vs Macintosh (n = 31) | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from insertion of the blade between the teeth until the anaesthetist had obtained the best possible view of the vocal cords Dichotomous outcomes: Failed intubation: defined as an attempt in which the trachea was not intubated, or in which the device was abandoned and another device was used Laryngeal/airway trauma (blood on laryngoscope blade/minor laceration/dental or other airway trauma) Successful first attempt No. of attempts: 1 to 3 CL glottic view: 1 to 3 IDS score: 0 to 8 or > 8 | |
| Notes | Experience of intubator: 1 anaesthetist experienced in the use of all 3 laryngoscopes Funding/declarations of interest: Storz C‐MAC and Airtraq supplied by manufacturers. Departmental funding only Additional: Airtraq is used, with camera attached as a videolaryngoscope. Participants' neck immobilized in both groups through manual in‐line axial stabilization | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "allocation sequence was generated using online randomization software" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "allocation concealed in sealed envelopes, which were not opened until patient consent had been obtained" Comment: insufficient detail |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "All data were collected by an independent unblinded observer" Comment: despite use of independent assessors, not possible to blind assessors from outcomes measured in theatre |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "A total of 90 patients consented to participate in the study. One patient, who had been randomized to the C‐MAC group, was not subsequently entered into the study due to a change in the choice of anaesthetic technique" Comment: low level of loss |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "The trachea was then intubated by one anaesthetist...experienced in the use of all three laryngoscopes" |
| Baseline characteristics | Unclear risk | Comment: more males in Macintosh group. Impact of this difference is uncertain. |
| Funding sources | Unclear risk | Quote: "Storz Ltd provided the C‐MAC device, and Prodol Ltd provided the Airtraq devices free of charge for use in the study" |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 300 Inclusion criteria: ASA I or II, MET > 4, scheduled for elective surgery under general anaesthesia in the supine position Exclusion criteria: age < 18 years or > 60 years; any anatomical abnormality in the head, neck or face; any ENT, neck or thoracic surgery; smoking history; edentulous patients; estimated surgery time > 4 hours; any clinical evidence of active pulmonary disease; common cold during recent 2 weeks; limited mouth opening or neck extension Baseline characteristics: GlideScope Age: 39.1 (SD ± 7.6) Gender M/F: 67/83 ASA I: 125 ASA II: 25 Mallampati 1: 71 Mallampati 2: 48 Mallampati 3: 18 Mallampati 4: 13 Macintosh Age: 40.2 (SD ± 7.2) Gender M/F: 70/80 ASA I: 127 ASA II: 23 Mallampati 1: 85 Mallampati 2: 40 Mallampati 3: 17 Mallampati 4: 8 Country: Iran Setting: hospital | |
| Interventions | GlideScope (n = 150) vs Macintosh (n = 150) GlideScope blade #4; Macintosh blade #3 for women and #4 for men | |
| Outcomes | Continuous outcome: Time for tracheal intubation: no definition reported Dichotomous outcomes: Failed intubation Patient‐reported sore throat | |
| Notes | Experience of intubator: 1 anaesthetist in both groups Funding/declarations of interest: university funding only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "block randomization method" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details given |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "Patients and the anesthesia resident, who evaluated the patients postoperatively, were blinded" Comment: blinding for sore throat outcome but not for intubation time or failed intubation outcome |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought. Study authors did not report data for failed intubation. |
| Experience of intubator | Unclear risk | Comment: 1 anaesthetist in both groups but no details of experience |
| Baseline characteristics | Unclear risk | Quote: "The two groups were comparable with respect to; age, sex, ASA class, and duration of operation" Comment: baseline demographics presents more participants with higher Mallampati score in the intervention group |
| Funding sources | Low risk | Comment: university funding only |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 40 Inclusion criteria: ASA I or II, adult patients between 20 and 65 years old, undergoing elective mastectomy or minor orthopaedic surgery in supine position Exclusion criteria: hypertension, hypotension, cardiovascular disease, or arteriosclerosis; known history of a previous difficult tracheal intubation Baseline characteristics: Pentax Age: 41.0 (SD ± 13.8) Gender M/F: 5/15 Height (cm): 157.1 (SD ± 12.0) Weight (kg): 55.3 (SD ± 11.6) Macintosh Age: 41.7 (SD ± 13.8) Gender M/F: 4/16 Height (cm): 159.0 (SD ± 12.1) Weight (kg): 54.1 (SD ± 10.6) Country: Japan Setting: hospital | |
| Interventions | Pentax AWS (n = 20) vs Macintosh (n = 20) Macintosh blade #3 or #4 for women, #4 or #5 for men | |
| Outcomes | Continuous outcome: Time for tracheal intubation: recorded as interval from the time the device was inserted (Macintosh laryngoscope or AWS) into the oropharynx to the time when the device was removed from the oral cavity Dichotomous outcomes: Failed intubation: defined as inability to place the tracheal tube into the trachea on the first attempt in the Macintosh group Patient‐reported sore throat: reported at 24 hours postoperatively. Graded on a 4‐point scale; no sore throat, mild, moderate or severe sore throat | |
| Notes | Experience of intubator: all intubating procedures were performed by a single anaesthetist who had 2 years' experience with Macintosh blades and at least 50 experiences with the AWS. Funding/declarations of interest: Grants‐in‐Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan to Koichi Nishikawa (No. 20390412) Additional: note bias introduced by exclusion criteria (study author quote: "Patients in whom there was failure to intubate and those requiring more than 30 seconds to achieve tracheal intubation were excluded from this study") | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "The patients were interviewed in a standard fashion by a blinded investigator" Comment: not possible to blind outcome assessors for primary outcome, although investigator blinded for assessment of sore throat |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "No patient was excluded from analysis according to the exclusion criteria" |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "All intubating procedures were performed by a single anesthesiologist who had 2 years experience with Macintosh blades and at least 50 times experience with the AWS" |
| Baseline characteristics | Low risk | Quote: "There were no significant differences in terms of patient characteristics" |
| Funding sources | Low risk | Comment: Grants‐in‐Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan to Koichi Nishikawa (No. 20390412) |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 54 Inclusion criteria: ASA I or II, undergoing elective surgical procedures Exclusion criteria: no details Baseline characteristics: Cross‐over design with baseline characteristics reported together, not by scope Age: 53.4 (SD ± 15.4) Gender M/F: 27/27 Height (cm): 168 (SD ± 10) Weight (kg): 82.6 (SD ± 18.2) BMI: 29.3 (SD ± 6.0) Country: Canada Setting: hospital | |
| Interventions | McGrath vs Macintosh Type of McGrath device not specified | |
| Outcomes | Continuous outcomes: Improved visualization (measured with POGO) Time for tracheal intubation Dichotomous outcomes: Failed intubation Patient‐reported sore throat CL glottic view: 1 to 4 | |
| Notes | Funding/declarations of interest: none apparent Additional: simulated difficult laryngoscope with manual in‐line immobilization Abstract only. Not possible to contact study author, as no contact information provided in abstract. Sufficient information in Methods and Results sections for inclusion in the review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: randomized but no additional details. Abstract only |
| Allocation concealment (selection bias) | Unclear risk | Comment: abstract only. No details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind anaesthetist to primary outcome |
| Incomplete outcome data (attrition bias) | Unclear risk | Comment: abstract only. No details |
| Selective reporting (reporting bias) | Unclear risk | Comment: abstract only. No details |
| Experience of intubator | Unclear risk | Comment: no details |
| Baseline characteristics | Unclear risk | Comment: cross‐over design. Baseline characteristics not presented by group |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel design | |
| Participants | Total number of participants: 95 Inclusion criteria: scheduled for elective surgery under general anaesthesia, ASA I or II, aged 18 to 60 years Exclusion criteria: hypertension, lung disease, cardiovascular disease, cervical spine disease, gastro‐oesophageal reflux disease, predicted difficult intubation/laryngoscopy, history of regular drug intake, allergy to anaesthetic medications, oxygen desaturation during intubation ≤ 94%, intubation failures Baseline characteristics: GlideScope Age: 36.1 (SD ± 11.6) Gender M/F: 20/26 Height (cm): 167.5 (SD ± 8.9) Weight (kg): 69.7 (SD ± 9.1) BMI (kg/m2): 24.9 (SD ± 3.5) Macintosh Age: 33.7 (SD ± 10.6) Gender M/F: 18/31 Height (cm): 165.9 (SD ± 7.5) Weight (kg): 66.2 (SD ± 9.8) BMI (kg/m2): 24.1 (SD ± 3.3) Country: Iran Setting: hospital | |
| Interventions | GlideScope (n = 46) vs Macinotsh (n = 49) Macintosh blade #3 for women and #4 for men | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from insertion of scope until tracheal tube positioned between vocal cords Dichotomous outcome: Intubation failure: defined as more than one attempt needed to achieve successful intubation, intubations needing > 30 seconds, need for another person to complete the procedure | |
| Notes | Funding/declarations of interest: supported in part by grant from Iran University of Medical Sciences Additional: study aimed to consider haemodynamic changes, but also reported on relevant outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: generated by random allocation table in permutated blocks of 4 |
| Allocation concealment (selection bias) | Low risk | Quote: "The numbered opaque sealed envelopes that contained patient allocation were opened at the time of randomization" |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Comment: study exclusion criteria were such that some patients were excluded because of intubation failure. For this review, we included in our outcome data the number of excluded patients due to intubation failure |
| Selective reporting (reporting bias) | Unclear risk | Comment: clinical trials identification number supplied (IRCT201111264969N4) but protocol not sourced |
| Experience of intubator | Low risk | Comment: about 4 years' experience with Macintosh and 20 successful intubations with GlideScope |
| Baseline characteristics | Low risk | Comment: comparable baseline characteristics |
| Funding sources | Unclear risk | Comment: supported in part by grant from Iran University of Medical Sciences |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 20 Inclusion criteria: scheduled to undergo an elective interventional neuroradiological procedure under general anaesthesia Exclusion criteria: incapable of informed consent, clinical or radiological evidence of C‐spine abnormalities, requiring rapid sequence induction or an induction without a neuromuscular blocking drug Baseline characteristics: None reported Country: Canada Setting: hospital | |
| Interventions | GlideScope vs Macintosh GlideScope blade size "large"; Macintosh blade #3 or #4 | |
| Outcomes | Dichotomous outcome: CL glottic view: 1 to 3 | |
| Notes | Experience of intubator: all intubations were performed by 2 senior anaesthesiology residents who had performed both laryngoscopy techniques at least 30 times at the beginning of the study. Funding/declarations of interest: none apparent Additional: a trained assistant, positioned at the participant's head, maintained MILS of the C‐spine throughout airway manoeuvres by grasping the mastoid processes bilaterally with the fingertips while cupping the occiput in the palms of the hands Study powered as comparison of spine movement during intubation with MILS, but has relevant outcomes Long study period with few participants | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomization table" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "of blinding, since both the operators performing the laryngoscopies and the image assessors knew which technique was being executed, blinding being impossible to perform in the former and extremely difficult to achieve in the latter" Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "All intubations were performed by two senior anesthesiology residents...having performed both laryngoscopy techniques at least 30 times at the beginning of the study" |
| Baseline characteristics | Unclear risk | Comment: none reported |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 29 Inclusion criteria: ASA I or II, aged over 18 years, undergoing elective surgical procedures requiring tracheal intubation Exclusion criteria: rapid sequence intubation or another intubation method indicated; known or suspected oral, pharyngeal or laryngeal masses; poor dentition, symptomatic gastro‐oesophageal reflux, cervical spine instability, unstable hypertension, coronary artery disease, cerebral disease or asthma; resources not available for procedure to be conducted on the scheduled date of surgery Baseline characteristics: not reported by group because of cross‐over design Age: 47.9 (SD ± 14.4) Gender M/F: 14/9 BMI < 30/30‐35 kg/m2: 19/4 ASA I: 12 ASA II: 11 Mallampati 1: 7 Mallampati 2: 11 Mallampati 3: 5 Country: Canada Setting: hospital | |
| Interventions | GlideScope vs Macintosh Macintosh blade #3, GlideScope blade size unknown | |
| Outcomes | Continuous outcome: Time for tracheal intubation Dichotomous outcome: Successful first attempt | |
| Notes | Experience of intubator: anaesthesia staff that included specialists, fellows and third‐ and fifth‐year anaesthesia trainees with experience in using the GlideScope on more than 25 occasions. Funding/declarations of interest: none apparent Additional: stylets used for both | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: computer‐generated codes used |
| Allocation concealment (selection bias) | Unclear risk | Comment: randomization codes revealed before induction, but no additional details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Comment: personnel with varying levels of anaesthetic experience. All had experience in using GlideScope on more than 25 occasions. |
| Baseline characteristics | Unclear risk | Comment: cross‐over design, characteristics not presented in groups |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 70 Inclusion criteria: aged over 18 years, undergoing elective surgical procedures requiring endobronchial intubation with a left‐sided DLT Exclusion criteria: history of previous failed or difficult tracheal intubation, difficult tracheal intubation anticipated (2 risk factors of Mallampati score ≥ 3, incisor gap < 3.5 cm, thyromental distance < 6.5 cm, reduced neck extension and flexion), alternative method of tracheal intubation indicated (e.g. rapid sequence intubation), contraindication to a left DLT, contraindication to 1‐lung ventilation, anticipated difficult bag‐mask ventilation of the lungs, BMI > 40 kg/m2 Baseline characteristics: GlideScope Age: 59 (SD ± 12) Gender M/F: 15/20 BMI: 26 (SD ± 5) ASA II: 8 ASA III: 24 Mallampati 1: 15 Mallampati 2: 13 Mallampati 3: 7 Macintosh Age: 62 (SD ± 14) Gender M/F: 18/17 BMI: 26 (SD ± 4) ASA II: 5 ASA III: 29 Mallampati 1: 22 Mallampati 2: 11 Mallampati 3: 2 Country: Canada Setting: hospital | |
| Interventions | GlideScope vs Macintosh Macintosh and GlideScope blade size unknown | |
| Outcomes | Continuous outcome: Time for tracheal intubation Dichotomous outcomes: Failed intubation Laryngeal/airway trauma Patient‐reported sore throat Successful first attempt Difficulty of intubation (use of numerical rating scale ranging from 1 (none) to 10 (severe)) | |
| Notes | Experience of intubator: study centre performs more than 1500 thoracic cases per annum, and the GlideScope has been the primary video‐laryngoscope since 2001. All anaesthetists were specialists or fellows who regularly perform thoracic anaesthesia and regularly use the GlideScope for tracheal intubation. However, most staff had used the GlideScope for DLT insertion only around 3 to 6 times. Funding/declarations of interest: none apparent Additional: stylet used to shape DLT to replicate GlideScope or Macintosh blades, dependent on device used See also abstract reports of same study (Van Rensburg 2013a and Van Rensburg 2013b). In these abstracts, study authors reported duration of first intubation as GlideScope 77 seconds (44) compared with Macintosh 51 seconds (61). They do not state whether this is a mean value (SD). Also in these abstracts, study authors stated different percentages for success of first intubation (74% vs 88%, unclear which figure relates to which scope). For the purpose of this review, we have taken data from the full report, not from the abstracts | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was computer‐generated" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "revealed to the anaesthetist and research staff after the airway assessment and immediately before induction of anaesthesia" Comment: additional details required |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors for some reported outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses after randomization |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | High risk | Comment: operators were experienced in use of both laryngoscopes but had very limited experience with a GlideScope blade for DLT intubations |
| Baseline characteristics | Low risk | Quote: "Baseline characteristics and pre‐operative airway assessments were similar in both groups" |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 200 Inclusion criteria: undergoing elective surgery under general anaesthesia Exclusion criteria: no details Baseline characteristics: No details, described as comparable in both groups Country: India Setting: hospital | |
| Interventions | GlideScope (N = 100) vs Macintosh (N = 100) | |
| Outcomes | Continuous outcomes: Time for tracheal intubation Improved visualization (POGO scores): scores taken initially with all participants and again at laryngoscopy attempt, which included intubation. This review used POGO scores from second laryngoscopy. Intubation difficulty score: data presented as mean (SD): GlideScope 0.4 (± 0.7); Macintosh 1.2 (± 1.3), P < 0.05 Dichotomous outcomes: Number of attempts (no data presented in abstract) CL glottic view: study authors' quote: "the difference in CL grades during final laryngoscopy between the two groups was statistically highly significant (P < 0.001)". No data presented in abstract, not stated in which direction this result is significant Adverse events: study authors' quote: "the incidence of adverse events was similar in two groups (P > 0.05)". No data presented in abstract | |
| Notes | Funding/declarations of interest: no details Additional: abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: participants described as randomly assigned, but no additional details in abstract |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: no details given but not possible to blind assessors to many included outcomes |
| Incomplete outcome data (attrition bias) | Unclear risk | Comment: no details reported in abstract |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Comment: no details of experience reported in abstract |
| Baseline characteristics | Unclear risk | Comment: described as comparable but no data presented |
| Funding sources | Low risk | Comment: no details reported in abstract, assumed no funding |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 120 Inclusion criteria: at least 18 years of age, ASA ≤ 3, ≥ 1 positive predictor of a difficult airway, Mallampati score ≥ 2 Exclusion criteria: refusal of participation, indication for rapid sequence induction, known difficult facemask ventilation Baseline characteristics: Macintosh blade Height (cm): 170 (SD ± 9) Weight (kg): 77(SD ± 17) Age: 66 (SD ± 13) Gender M/F: 21/19 ASA I: 3 ASA II: 23 ASA III: 14 Mallampati 1: 0 Mallampati 2: 23 Mallampati 3: 17 Mallampati 4: 0 DCI video laryngoscope Height (cm): 172 (SD ± 12) Weight (kg): 78 (SD ± 15) Age: 63 (SD ± 15) Gender M/F: 21/19 ASA I: 4 ASA II: 28 ASA III: 8 Mallampati 1: 0 Mallampati 2: 23 Mallampati 3: 16 Mallampati 4: 1 GlideScope Height (cm): 173 (SD ± 10) Weight (kg): 83 (SD ± 13) Age: 66 (SD ± 10) Gender M/F: 26/14 ASA I: 2 ASA II: 29 ASA III: 9 Mallampati 1: 0 Mallampati 2: 22 Mallampati 3: 16 Mallampati 4: 2 Country: Germany Setting: hospital | |
| Interventions | Repeated laryngoscopy comparing Macintosh, Storz DCI laryngoscopy and GlideScope Macintosh blade #3 for male female, #4 for tall participants GlideScope standard adult/large blade used in all DCI fixed blade size | |
| Outcomes | Continuous outcome: Time for tracheal intubation Dichotomous outcomes: Failed intubation Hypoxia No. of attempts: 1 to 3 CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: investigation was carried out by 2 board‐certified anaesthetists. Both were familiar with all the laryngoscopes investigated (50 intubations each) Funding/declarations of interest: videolaryngoscopes supplied by manufacturers | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomized sequence" Comment: no additional details |
| Allocation concealment (selection bias) | Unclear risk | Quote: "allocation of patients by opening of a sealed envelope" Comment: no additional details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "In total, 120 patients were enrolled in this study; none had to be excluded for data analysis" |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "The investigation was carried out by two board‐certified anaesthetists... Both were familiar with all the laryngoscopes investigated (≥ 50 intubations each)" |
| Baseline characteristics | Unclear risk | Quote: "There were no significant differences between groups with regard to patients’ characteristics and predictors of a difficult airway" Comment: more male participants in GlideScope group, and higher mean weight reported for this group. Impact of these differences is uncertain |
| Funding sources | Unclear risk | Comment: videolaryngoscopes supplied by manufacturers |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 96 Inclusion criteria: scheduled for elective ENT surgery requiring tracheal intubation, ≥ 1 of the following: Mallampati score ≥ 2, reduced mobility of the atlanto‐occipital joint (≤ 15°), mouth opening < 4 cm, thyromental distance < 6 cm Exclusion criteria: refusal of participation, age < 18 years and ASA > III, indication for rapid sequence induction, known difficult facemask ventilation, hypopharyngeal or laryngeal tumours with risk of bleeding or swelling Baseline characteristics: GlideScope Age: 59 (SD ± 13) Gender M/F: 8/24 Height (cm): 177 (SD ± 11) Weight (kg): 81 (SD ± 14) ASA I: 0 ASA II: 21 ASA III: 11 Mallampati 1: 1 Mallampati 2: 16 Mallampati 3: 13 Mallampati 4: 2 Macintosh Age: 59 (SD ± 16) Gender M/F:16/16 Height (cm): 171 (SD ± 94) Weight (kg): 76 (SD ± 16) ASA I: 2 ASA II: 19 ASA III: 11 Mallampati 1: 0 Mallampati 2: 20 Mallampati 3: 9 Mallampati 4: 3 C‐MAC D‐blade Age: 51 (SD ± 19) Gender M/F: 7/25 Height (cm): 176 (SD ± 10) Weight (kg): 81 (SD ± 17) ASA I: 3 ASA II: 21 ASA III: 8 Mallampati 1: 1 Mallampati 2: 16 Mallampati 3: 11 Mallampati 4: 4 Country: Germany Setting: hospital | |
| Interventions | Intervention characteristics: Randomized repeated laryngoscopy was performed with Macintosh, GlideScope and C‐MAC D‐Blade. Intubation with final device Macintosh #3 blade was used routinely for female and male participants; blade #4 was used only for tall individuals. GlideScope large blade was used in all intubations. C‐MAC D‐blade was used in all intubations. Additional difficult airway equipment: stylets were used. In hockey stick shape for GlideScope and C‐MAC, moderate curve for Macintosh | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from touching ETT to inflating cuff Dichotomous outcomes: Failed intubation CL glottic view: 1 to 4 Successful first attempt No. of attempts: 1 to 3 | |
| Notes | Experience of intubator: investigation was carried out by 3 board certified anaesthetists familiar with all laryngoscopes (> 50 intubations each) Funding/declarations of interest: Volker Doerges (study author) reported his membership in the Karl Storz advisory board and involvement in the development of C‐MAC. Also, manufacturers supplied the scopes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomized sequence" Comment: no additional details of method used |
| Allocation concealment (selection bias) | Unclear risk | Quote: "sealed envelope" Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors for relevant outcomes |
| Incomplete outcome data (attrition bias) | Low risk | Comment: 1 participant excluded from GlideScope group owing to problems with facemask. No other exclusions |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "The investigation was carried out by three board certified anaesthetists...familiar with all laryngoscopes (≥ 50 intubations each)" |
| Baseline characteristics | Unclear risk | Quote: "Except for distribution between the sexes, there were no significant differences between groups regarding demographic data and predictors of a difficult airway" Comment: participants in C‐MAC group slightly younger. Impact of this difference is uncertain |
| Funding sources | High risk | Comment: One study author is a member of the Karl Storz advisory board and was involved in the development of C‐MAC. Also, manufacturers supplied the scopes |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 50 Inclusion criteria: no details Exclusion criteria: no details Baseline characteristics: McGrath Age: 55.5 (SD ± 17.0) Gender M/F: 18/7 BMI: 27 (SD ± 4.2) Macintosh Age: 52.7 (SD ± 14.3) Gender M/F: 15/10 BMI: 29.2 (SD ± 4.9) Country: UK Setting: hospital | |
| Interventions | McGrath vs Macintosh in parallel trial Type of McGrath device not specified in abstract Blade sizes not specified | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from insertion of laryngoscope to first appearance of carbon dioxide on capnograph trace Dichotomous outcomes: Failed intubation Successful first attempt No. of attempts: 1 to 3 | |
| Notes | Funding/declarations of interest: none apparent Additional: cervical spine immobilisation maintained with rigid cervical collar Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "single‐blinded, randomised controlled trial" Comment: no details. Abstract only |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details. Abstract only |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Unclear risk | Comment: no details. Abstract only |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Comment: no details |
| Baseline characteristics | Low risk | Comment: comparable baseline characteristics |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 40 Inclusion criteria: ASA I or II, normotensive patients, aged 18 to 65 years, scheduled for elective surgery requiring tracheal intubation Exclusion criteria: receiving medications known to affect blood pressure or heart rate, Mallampati classification 3 or 4, anticipated difficult airway Baseline characteristics: GlideScope Age: 38.9 (SD ± 10.9) Gender M/F: 17/3 BMI: 26.6 (SD ± 4.1) Macintosh Age: 43.7 (SD ± 16.1) Gender M/F: 9/11 BMI: 25.0 (SD ± 3.8) Country: Canada Setting: hospital | |
| Interventions | GlideScope vs Macintosh Macintosh #3 blade used GlideScope blade not specified Stylet was used to stiffen tracheal tube to conform with the angle of the blade for the GlideScope group. No external manipulation of the larynx was performed in either group | |
| Outcomes | Continuous outcomes: Number of attempts Time for tracheal intubation: defined as time from insertion of intubating device into the oral cavity to inflation of the endotracheal tube cuff Dichotomous outcomes: Failed intubation Patient‐reported sore throat (graded as none (no sore throat), moderate (similar to that noted with a cold) and severe (more severe than a cold)) Hoarseness graded as none (no hoarseness), moderate (obvious to observer) and severe (aphonia) | |
| Notes | Experience of intubator: Intubations were performed by a single anaesthetist who had performed more than 50 intubations with each device and was well experienced in all 3 techniques of tracheal intubation. Funding/declarations of interest: none apparent Additional: a Trachlight was included in this study, although data were not recorded, as Trachlight did not meet our criteria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "a computerized random‐number generator" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "An unblinded observer noted the number of intubation attempts" Quote: "The severity of postoperative sore throat and hoarseness were assessed in the recovery room by a second observer blinded to the intubation technique" Comment: attempts made by investigators to blind outcome assessors when possible; however, not possible to blind assessors to primary outcome of failed intubation |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "All 60 patients were successfully intubated" Comment: no losses reported in CONSORT diagram |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "Intubations were performed by a single anaesthesiologist, who had performed more than 50 intubations with each device and is well experienced in all three techniques of tracheal intubations" |
| Baseline characteristics | Unclear risk | Quote: "There was a statistically significant difference in sex distribution among the groups with more men in the GlideScope group" Comment: unclear how this difference may have affected the results |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 200 Inclusion criteria: presenting for surgery requiring tracheal intubation Exclusion criteria: raised intracranial pressure, known airway pathology or cervical spine injury, requiring rapid sequence induction Baseline characteristics: GlideScope Age: 52 (range 20‐87) Gender M/F: 32/68 Height (cm): 166 (SD ± 12) Weight (kg): 75 ( SD ± 21) ASA I: 27 ASA II: 44 ASA III & IV: 24 Mallampati 1: 52 Mallampati 2: 36 Mallampati 3: 11 Mallampati 4: 1 Macintosh Age: 54 (range 20‐87) Gender M/F: 38/62 Height (cm): 165 (SD ± 12) Weight (kg): 73 (SD ± 17) ASA I: 26 ASA II: 45 ASA III & IV: 21 Mallampati 1: 50 Mallampati 2: 41 Mallampati 3: 9 Mallampati 4: 0 Country: Canada Setting: hospital | |
| Interventions | GlideScope vs Macintosh #3 Macintosh blade used GlideScope size not mentioned | |
| Outcomes | Continuous outcome: Time for intubation: defined as time from insertion of device until end‐tidal carbon dioxide was detected Dichotomous outcomes: Failed intubation: defined as failure after 3 attempts, then change to another blade Successful first attempt No. of attempts: 1 and > 1 CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: intubations were performed by 5 different anaesthetists, all of whom were experienced in anaesthesia (> 10 years' experience) and use of the GlideScope (20 intubations) before the study. Funding/declarations of interest: none Additional: after approximately 3 minutes, all participants underwent an initial direct laryngoscopy, which was scored according to the CL grading system with the Macintosh laryngoscope and a size 3 blade. This was performed by a separate anaesthetist, who was neither 1 of the intubators nor involved with the participant's overall care. Then participants were allocated to randomized groups for intubation with given scope | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patients were allocated by computer‐generated randomization in blocks of six" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Five patients from the pilot study were excluded from the final TTI (time to intubate) analysis. Four of these patients required multiple attempts at intubation, and the recorded TTI included interim bag‐and‐mask time and did not reflect true intubation time; one of these patients was in the DL group (Macintosh) (C&L grade 2) and three were in the GS group (Glidescope) (one each of C&L grade 1, 2, and 3)" Comment: only small number of exclusions; unlikely to affect results and full explanations given |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "The intubations were performed by five different anaesthetists, all of whom were experienced in anaesthesia (> 10 yr experience) and the use of the GlideScope (> 20 intubations) prior to the study" |
| Baseline characteristics | Low risk | Quote: "Patient characteristics and the airway parameters were similar in the two groups" |
| Funding sources | Low risk | Comment: none |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 200 Inclusion criteria: scheduled for elective anaesthesia Exclusion criteria: no details given. Abstract only Baseline characteristics: No details given in abstract. Study authors state, "Patient profiles such as height and body weight were similar in both groups" Country: Japan Setting: hospital | |
| Interventions | Pentax AWS vs Macintosh (denominator figures not given by group) | |
| Outcomes | Continuous outcome: Time for tracheal intubation: no definition given. AWS 19 seconds (SD ± 9); Macintosh 18 seconds (SD ± 8) Dichotomous outcome: Successful first attempt: "All intubations were successful at the first attempt"; however, numbers of participants per group not provided | |
| Notes | Funding/declarations of interest: departmental funding only (response to email request) Additional: abstract only. Email request sent to study authors to request additional information; responses noted in risk of bias table | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomly assigned to group" Comment: insufficient details |
| Allocation concealment (selection bias) | Unclear risk | Comment: use of sealed envelope technique (response to email request). Insufficient detail |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: data analysed by independent assessor (response to email request) but assumed that people measuring outcomes were not blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Comment: no details |
| Selective reporting (reporting bias) | Unclear risk | Comment: no details |
| Experience of intubator | Low risk | Comment: experience of at least 100 intubations with the Macintosh and 50 intubations with the Pentax AWS (response to email request) |
| Baseline characteristics | Unclear risk | Comment: no baseline characteristics reported |
| Funding sources | Low risk | Comment: departmental funding only (response to email request) |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 69 Inclusion criteria: ASA I to III, scheduled for elective non‐obstetrical surgery in the lateral position requiring general anaesthesia with tracheal intubation Exclusion criteria: BMI > 30 kg/m2, cervical spine abnormality, pharyngolaryngeal disorder, anticipated difficult airway, increased risk of aspiration Baseline characteristics: Pentax AWS Age: 68.3 (range 30‐83) Gender M/F: 12/23 Height (cm): 156 (SD ± 9) Weight (kg): 55.9 (SD ± 12.1) Macintosh Age: 67.6 (range 32‐88) Gender M/F: 8/26 Height (cm): 154 (SD ± 9) Weight (kg): 55.0 (SD ± 12.8) Country: Japan Setting: hospital | |
| Interventions | Pentax AWS (n = 35) vs Macintosh (n = 34) External laryngeal manipulation and adjustment of participant's head and neck position were performed as necessary Stylet was used for intubation in the Macintosh group | |
| Outcomes | Continuous outcomes: Difficulty of tracheal intubation. Intubation difficulty score as median (IQR range): VLS 0 (0‐0); Mac 0 (0‐2) Time for tracheal intubation: defined as time from insertion of blade between the teeth until tracheal tube cuff was passed through vocal cords. Median (IQR range): VLS 14 (9‐19), Mac 29 (20‐31) Dichotomous outcomes: Failed intubation: defined as failure to intubate within 60 seconds. Required intubation with alternative device or change to lateral position Successful first attempt No. of attempts: 1 CL glottic view: 1 to 3 | |
| Notes | Experience of intubator: 2 anaesthetists experienced more than 5000 intubations with the Macintosh laryngoscope and more than 300 intubations with the AWS in the supine position. However, as they had few experiences in the lateral position, they practised tracheal intubation in this position with a mannequin. Funding/declarations of interest: departmental funding only Additional: all participants in lateral position for intubation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients were randomly assigned into two groups using a sealed envelope technique" Comment: insufficient detail |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Comment: only 1 loss after randomization due to cancellation of surgery |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Unclear risk | Comment: 2 anaesthetists experienced with both laryngoscopes in the supine position. Although they had fewer experiences in the lateral position, they had practised intubation in this position with a mannequin |
| Baseline characteristics | Unclear risk | Quote: "There were no significant differences in demographic data" Comment: some differences noted in ratio of male to female participants. Impact of these differences is uncertain. |
| Funding sources | Low risk | Comment: departmental funding only |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 88 Inclusion criteria: ASA I or II, scheduled for elective surgery under general anaesthesia requiring tracheal intubation Exclusion criteria: required rapid sequence induction, history of previous difficult direct laryngoscopy and required awake tracheal intubation, unable or unwilling to provide informed consent, uncontrolled hypertension, history of ischaemic heart disease without optimal control of symptoms, history of acute or recent stroke or myocardial infarction, cervical spine instability or cervical myelopathy, symptomatic asthma or reactive airway disease requiring daily pharmacological treatment for control of symptoms, history of gastric reflux Baseline characteristics: McGrath Series 5 Age: 52 (SD ± 13) Gender M/F: 18/26 BMI: 29.3 (SD ± 6.5) ASA I: 22 ASA II: 22 Mallampati 1: 14 Mallampati 2: 22 Mallampati 3: 7 Mallampati 4: 1 Macintosh Age: 54 (SD ± 16) Gender M/F: 20/24 BMI: 28.2 (SD ± 6.2) ASA I: 13 ASA II: 31 Mallampati 1: 24 Mallampati 2: 17 Mallampati 3: 2 Mallampati 4: 1 Country: Canada Setting: hospital | |
| Interventions | McGrath Series 5 (n = 44) vs Macintosh (n = 44) McGrath blade equivalent to #3; Macintosh blade #3 Stylet used in all participants Cross‐over groups labels: McGrath = Macintosh then McGrath; Macintosh = McGrath then Macintosh | |
| Outcomes | Continuous outcomes: Improved visualization (POGO: 82 (23) for McGrath; 13 (23) for Macintosh) Time for tracheal intubation: defined as time from insertion of the laryngoscope into the oral cavity until its removal Dichotomous outcomes: Failed intubation (tracheal tube could not be placed owing to difficulty viewing the glottis) Laryngeal/airway trauma (mucosal bleeding) Patient‐reported sore throat Successful first attempt CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: each of the consultant anaesthetists involved in the study had previously practised with the McGrath video laryngoscope using a manikin until subjectively comfortable with the device Funding/declarations of interest: departmental funding. McGrath scopes supplied by Vitaid Canada. One investigator is a consultant for a McGrath distributor Additional: manual in‐line stabilization used to simulate difficult airway | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no details |
| Allocation concealment (selection bias) | Unclear risk | Quote: "A sealed envelope was opened, revealing to which of two study groups the patient had been randomly assigned" Comment: no further details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: assumed other outcome assessors not blinded to devices used |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no apparent losses |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | High risk | Quote: "Each of the consultant anaesthetists involved in the study had previously practised with the McGrath videolaryngoscope using a manikin until subjectively comfortable with the device" Comment: assumed therefore that experience was greater in Macintosh group |
| Baseline characteristics | Unclear risk | Comment: some differences in ASA scores and Mallampati scores ‐ unclear how this might affect the results. Otherwise baseline characteristics comparable |
| Funding sources | High risk | Comment: departmental funding. McGrath scopes supplied by Vitaid Canada. One investigator is a consultant for a McGrath distributor |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 400 Inclusion criteria: scheduled for elective gynaecological, orthopaedic, breast or aesthetic surgery in tertiary maternity and women’s hospital, consented to general anaesthesia and tracheal intubation Exclusion criteria: pregnant, ASA IV, aged < 21 or > 80 years, weight < 30 kg, BMI > 40 kg/m2, limited mouth opening (< 2.5 cm), respiratory tract pathology, preoperative sore throat, high risk of regurgitation or aspiration, allergy to any study medication Baseline characteristics: GlideScope Age: 43.4 (SD ± 11.2) Height (cm): 157.1 (SD ± 6.5) Weight (kg): 61.1 (SD ± 11.8) BMI: 24.7 (SD ± 4.6) Mallampati 1: 28 Mallampati 2: 43 Mallampati 3: 26 Mallampati 4: 3 Pentax AWS Age: 37.0 (SD ± 10.5) Height (cm): 158.2 (SD ± 6.3) Weight (kg): 59.7 (SD ± 13.9) BMI: 23.7 (SD ± 5.2) Mallampati 1: 48 Mallampati 2: 35 Mallampati 3: 17 Mallampati 4: 0 C‐MAC Age: 41.5 (SD 12.3) Height (cm): 157.9 (SD 6.2) Weight (kg): 60.7 (SD 14.1) BMI: 24.3 (SD 5.6) Mallampati 1: 52 Mallampati 2: 33 Mallampati 3: 12 Mallampati 4: 3 Macintosh Age: 39.6 (SD ± 9.9) Height (m): 157.4 (SD ± 5.7) Weight (kg): 58.87 (SD ± 12.7) BMI: 23.6 (SD ± 4.2) Mallampati 1: 46 Mallampati 2: 32 Mallampati 3: 19 Mallampati 4: 3 Country: Singapore Setting: tertiary maternity and women's unit | |
| Interventions | GlideScope (n = 100) vs Pentax AWS (n = 100) vs C‐MAC (n = 100) vs Macintosh (n = 100) For participants assigned to GlideScope, tracheal tube was preloaded with the manufacturer’s preconfigured stylet; if intubation after first or second attempt was not feasible with the Airway Scope, C‐MAC or conventional Macintosh laryngoscope, use of a stylet or bougie was left to the preference of the anaesthetist | |
| Outcomes | Continuous outcomes: Difficulty of tracheal intubation, ease of insertion of the blade and tracheal tube (as subjectively assessed from 0: easy, to 100: difficult): median (IQR (range)): AWS 0 (0‐8.75 (0‐60)); C‐MAC 10 (0‐20 (0‐90)); GlideScope 0 (0‐20 (0‐80)); Macintosh 0 (0‐20 (0‐90)) Improved visualization: quality of the view (subjectively assessed from 0: good, 100: bad) Time for tracheal intubation: defined as interval from insertion of the laryngoscope blade into the mouth to inflation of the tracheal tube cuff Dichotomous outcomes: Failed intubation: required more than 3 attempts, or exceeded 120 seconds Laryngeal/airway trauma (mucosal bleeding, lip bleeding, dental trauma) Patient‐reported sore throat: postoperative sore throat and above laryngeal/airway trauma recorded in recovery room Hypoxia Successful first attempt No. of attempts: 1 to 3 CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: all intubations were performed by experienced anaesthetists who had performed > 30 intubations with each of the devices being tested Funding/declarations of interest: no external funding | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated random number table" |
| Allocation concealment (selection bias) | Low risk | Quote: "After recruitment, the enrolling investigator opened a sealed opaque envelope that concealed group allocation in the anaesthetic induction room" |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Participants were blinded to their group allocation" Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "An independent data collector recorded the observed manoeuvres used to optimise the laryngeal view" Comment: some outcomes assessed by independent observer, but not possible for observer to be blinded |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Four hundred patients were successfully recruited and there were no dropouts" |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "All intubations were performed by experienced anaesthetists who had performed > 30 intubations with each of the devices being tested" |
| Baseline characteristics | Unclear risk | Comment: most baseline characteristics comparable. Some differences in Mallampati scores in GlideScope and C‐MAC groups ‐ unclear how this might affect the results |
| Funding sources | Low risk | Comment: no external funding |
| Study characteristics | ||
| Methods | Randomized controlled trial Cross‐over | |
| Participants | Total number of participants: 18 Inclusion criteria: ASA physical status I to III, age 18 to 75 years, elective non‐cardiac surgery requiring general anaesthesia with endotracheal intubation Exclusion criteria: gastro‐oesophageal reflux disease, body mass index > 35 kg/m2, possibility of pregnancy, previous neck surgery, unstable C‐spine, difficult airway Baseline characteristics: GlideScope and Macintosh Age: 40 (SD ± 13) Gender M/F: 5/13 Height (cm): 167 (SD ± 8) Weight (kg): 70 (SD ± 14) ASA I: 3 ASA II: 12 ASA III: 3 Mallampati 1: 8 Mallampati 2: 8 Mallampati 3: 1 Mallampati 4: 1 Country: Canada Setting: hospital | |
| Interventions | GlideScope and Macintosh | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined from time when the blade or stylet passed the central incisors to when the ETT was positioned at the vocal cords | |
| Notes | Experience of intubator: all laryngoscopies were performed by 1 person to minimize interoperator variability. Before this study, intubator had performed > 50 intubations with the GlideScope and > 500 intubations with the Macintosh laryngoscope Funding/declarations of interest: supported, in part, by the 2004 Canadian Anesthesia Society Additional: this study included a Lightwand group, which was not included in this analysis. Fluoroscopic study but with relevant outcomes for tracheal intubation time; therefore included. While awake, participants were placed on the operating room table with a rigid board under their torso to simulate field spinal precautions, or on the table on which trauma patients are placed in the emergency room. Manual in‐line stabilization was then simulated by taping the patient’s head into the Mayfield horseshoe. The head was taped circumferentially around the forehead | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: use of computer‐generated numbers |
| Allocation concealment (selection bias) | Unclear risk | Quote: "sealed envelopes" Comment: no additional details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors for the relevant outcome measured |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Near the end of the study, the radiology department suffered simultaneous failure of the main and back‐up servers, and data for 11 patients were lost. As a result, an additional 7 patients were recruited before analysis, allowing 36 patients to be analyzed in the groups assigned" Comment: explanation given for losses; additional recruitment attempted |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "All laryngoscopies were performed by one person to minimize interoperator variability. Before this study, (intubator) had performed 50 intubations with..the GlideScope and 500 intubations using the Macintosh laryngoscope" |
| Baseline characteristics | Unclear risk | Comment: cross‐over study; baseline characteristics not divided by group |
| Funding sources | Low risk | Comment: supported, in part, by the 2004 Canadian Anesthesia Society |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 120 Inclusion criteria: aged 18 years, undergoing elective surgery, anaesthesia plan consisting of routine tracheal intubation under general anaesthesia performed by a first‐year trainee anaesthetist and supervised by a senior colleague Exclusion criteria: other intubation techniques planned, rapid sequence induction indicated Baseline characteristics: McGrath Series 5 Age: Median 48 (range 21‐84) Gender M/F: 17/43 Height (m): median 1.66 (range 1.50–1.89) Weight (kg): median 71.0 (range 50.0–116.4) BMI: median 25.7 (range 16.1‐39.5) Mallampati 1: 29 Mallampati 2: 29 Mallampati 3: 2 Mallampati 4: 0 Macintosh Age: median 60.5 (range 21‐84) Gender M/F: 19/41 Height (m): median 1.64 (range 1.48–1.90) Weight (kg): median 69.8 (range 44.0–106.5) BMI: median 25.2 (range 17.3‐47.2) Mallampati 1: 32 Mallampati 2: 27 Mallampati 3: 1 Mallampati 4: 0 Country: Scotland Setting: hospital | |
| Interventions | McGrath Series 5 vs Macintosh | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time between anaesthetist taking the laryngoscope in his hand until effective ventilation was initiated via the tracheal tube. Median (range): VLS 47.0 (25‐202); Mac 29.5 (15‐121) Dichotomous outcomes: Failed intubation Laryngeal/airway trauma (trama/blood in airway after intubation). However, 3 participants in the Macintosh group had undergone surgery, which could have accounted for blood at successful first attempt CL glottic view: 1 to 4 | |
| Notes | Experience of intubator: all 4 anaesthetists who performed tracheal intubation had undergone between 6 and 12 months of anaesthesia training during the study. All had achieved the Royal College of Anaesthetists initial competency in general anaesthesia with tracheal intubation and had also received training in use of the McGrath laryngoscope. This followed a standard competency‐based model, initially with a manikin, followed by 10 successful intubations in clinical practice Funding/declarations of interest: none. Scopes bought with charitable foundation fund Additional: When a Macintosh laryngoscope was used, a stylet or other intubation aid was used at the discretion of the anaesthetist, as were other aspects of the anaesthetic protocol. A shaped stylet (Mallinckrodt satin slip intubating stylet) was inserted into the tracheal tube for intubation with the McGrath laryngoscope because the view of the glottis is indirect | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The randomization sequence was generated in advance by the study’s statistical advisor" Comment: insufficient details on how randomization was completed |
| Allocation concealment (selection bias) | Low risk | Quote: "Sequentially numbered opaque envelopes were used to conceal the sequence and were opened only on arrival of the patient in the anaesthetic room" |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists. Study was described as single‐blinded; therefore we have assumed participants were blinded |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "All patients in the Macintosh group were intubated successfully, but in one patient in the McGrath group, a Macintosh laryngoscope had to be used because of battery failure in the McGrath during intubation. Time to intubation was also not recorded for this patient owing to an error with the stopwatch" |
| Selective reporting (reporting bias) | Low risk | Comment: Clinical trial register protocol sourced (unique identifier: NCT00633867). Protocol outcomes comparable with study reported outcomes |
| Experience of intubator | Unclear risk | Comment: all 4 anaesthetists had undergone 6 to 12 months of training to include manikin training in use of the McGrath blade. Unclear whether this is equivalent to use of the Macintosh |
| Baseline characteristics | Unclear risk | Quote: "Both groups were comparable apart from a greater median age in the Macintosh group (60.5 vs 48.0 yr)" Comment: Impact of this difference is uncertain; intubation may be more difficult with older participants in the Macintosh group. |
| Funding sources | Low risk | Comment: no external funding. Scopes were bought with charitable foundation fund |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 159 Inclusion criteria: aged 18 to 65, scheduled for regular escharectomy under general anaesthesia with a hypermetabolic state due to burn injury (occurring < 1 month from surgery), ASA II or III, second‐ or third‐degree burns over 25% of body surface Exclusion criteria: loose teeth, craniocervical or cervical injury or malformation, arteriosclerosis, uncontrolled hypertension, myocardial infarction, cerebrovascular disease, class 4 of Mallampati, existing endotracheal intubation, bandages due to burns on the face or neck, difficulties in manual ventilation Baseline characteristics: Pentax‐AWS Age: 45.5 (SD ± 10.4) Gender M/F: 37/13 Height (cm): 167.0 (SD ± 9.3) Weight (kg): 66.6 (SD ± 16.0) ASA II: 34 ASA III: 16 Mallampati 1: 8 Mallampati 2: 32 Mallampati 3: 10 Type of surgery: escharectomy Macintosh Age: 47.4 (SD ± 10.5) Gender M/F: 38/12 Height (cm): 166.4 (SD ± 9.6) Weight (kg): 65.9 (SD ± 11.5) ASA II: 37 ASA III: 13 Mallampati 1: 6 Mallampati 2: 29 Mallampati 3: 15 Type of surgery: escharectomy Country: Korea Setting: theatre | |
| Interventions | Pentax‐AWS vs Macintosh Macintosh blade #3 (for females) and #4 (for males) After second attempt, cricoid pressure was applied in Pentax group, and cricoid pressure and a stylet in Macintosh group | |
| Outcomes | Continuous outcome: Time for tracheal intubation: defined as time from moment when the blade of the laryngoscope passed the incisor to moment when it was outside the oral cavity after endotracheal intubation) Dichotomous outcomes: Failed intubation Patient‐reported sore throat (measured on 4‐point scale including none, reported on asking, self‐reported, affecting voice/hoarseness. For this review, data were transferred to dichotomous, sore throat or not. Measured at 24 hours postoperatively Successful first attempt No. of attempts: 1 to 3 Improved visualization: with POGO scale. Measured in units of 10%. VLS: 97% (SD ± 4%); Mac 48% (SD ± 29%) | |
| Notes | Experience of intubator: all endotracheal intubations were performed by a resident in the Department of Anesthesiology & Pain Medicine who had more than 3 years of experience in endotracheal intubation with the Macintosh laryngoscope and had performed more than 50 procedures with the Pentax‐AWS Funding/declarations of interest: none apparent Additional: In case of failure of the first attempt, second attempt was performed after manual ventilation with 100% oxygen for 30 seconds. After the second attempt, cricoid pressure was applied in Group P (Pentax‐AWS). In Group M (Macintosh) after the second attempt, cricoid pressure and a stylet were used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "simple random sampling with 50 subjects each group" Comment: concerns about randomization methods. Insufficient detail given. Paper says that an additional 59 were randomized to the Macintosh group |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | High risk | Comment: 59 participants from Macintosh group were excluded owing to failed intubation on first attempt; therefore, no data for sore throat or time outcomes |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Quote: "All endotracheal intubations were performed by a resident in the Department of Anesthesiology & Pain Medicine, with over 3 years of experience in endotracheal intubation using the Macintosh laryngoscope and with more than 50 procedures using the Pentax‐AWS" |
| Baseline characteristics | High risk | Quote: "There were no differences in gender, age, height, body weight, ASA physical status classification, Mallampati class distribution, thyromental distance, range of burn injury, and the presence and the degree of sore throat 24 hours after operation between Group M and Group P (Table 1)" Comment: However, baseline data given only for 50 participants in each group. Not a total of 159. Number of participants reported does not match that throughout the study. Macintosh group was sometimes reported as including 109 participants and sometimes as including 50. |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 57 Inclusion criteria: adults, ASA I, scheduled for elective plastic surgery during general anaesthesia requiring orotracheal intubation Exclusion criteria: receiving medications known to affect blood pressure or heart rate, predicted difficult airways Baseline characteristics: GlideScope Age: 28.2 (SD ± 9.5) Gender M/F: 11/17 Height (cm): 165.4 (SD ± 6.1) Weight (kg): 61.4 ( SD ± 11.9) Macintosh Age: 32.3 (SD ± 11) Gender M/F: 9/18 Height (cm): 165.1 (SD ± 6.9) Weight (kg): 61.7 (SD ± 13.6) Country: People's Republic of China Setting: hospital | |
| Interventions | GlideScope vs Macintosh Macintosh #3 blade | |
| Outcomes | Continuous outcome: Time for tracheal intubation: from termination of manual ventilation with a facemask to restart of ventilation through a tracheal tube Dichotomous outcomes: Failed intubation Successful first attempt No. of attempts: 1 to 3 | |
| Notes | Experience of intubator: all intubation procedures were performed by a single anaesthesiologist experienced in using a Macintosh and a GlideScope Funding/declarations of interest: none apparent Additional: External laryngeal compression was applied if necessary. After visualization of the glottis, a precurved styletted tracheal tube was inserted into the glottis. Two participants were excluded from statistical analysis of data, both from the GlideScope group; 1 case failed on the first attempt because of poor laryngeal view caused by fogging of the camera lens; the other case failed because of difficult immobilization of the GlideScope blade owing to the lubricant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "allocated by a sequence of random numbers" Comment: insufficient detail |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetists |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | Low risk | Comment: 2 participants excluded from statistical analysis, with explanations provided |
| Selective reporting (reporting bias) | Unclear risk | Comment: published protocol not sought |
| Experience of intubator | Low risk | Comment: 1 anaesthetist experienced in both devices |
| Baseline characteristics | Low risk | Quote: "There were no significant differences in demographic data between the two groups" |
| Funding sources | Low risk | Comment: none apparent |
| Study characteristics | ||
| Methods | Randomized controlled trial Parallel group | |
| Participants | Total number of participants: 623 Inclusion criteria: all patients who required tracheal intubation in the trauma resuscitation unit during the study period were assessed for eligibility. Indications for intubation followed Eastern Association for the Surgery of Trauma guidelines; included airway obstruction, hypoventilation, severe hypoxia, cognitive impairment (Glasgow Coma Scale score ≤ 8) and haemorrhagic shock. Altered mental status, combativeness and extreme pain were additional criteria. Exclusion criteria: minors, suspected laryngeal trauma or extensive maxillofacial injury requiring an immediate surgical airway, known or strongly suspected spinal cord injury with awake flexible fibre‐optic intubation indicated, cardiac arrest on arrival, those who died in the trauma resuscitation unit Baseline characteristics: GlideScope Age: 42 (range 18‐119) Gender M/F: 216/87 Macintosh Age: 43 (range 18‐94) Gender M/F: 244/76 Country: Baltimore, Maryland, USA Setting: shock trauma centre | |
| Interventions | GlideScope vs Macintosh No mention of blade sizes | |
| Outcomes | Continuous outcome: Time for intubation: defined as interval between when the laryngoscope was inserted into the participant's mouth and when it was fully removed. Mean (95% confidence intervals) 71.0 (65.3‐76.7); 56.5 (51.1‐62) Dichotomous outcomes: Mortality (30 days) Successful first attempt | |
| Notes | Experience of intubator: emergency medicine or anaesthesiology residents with a minimum of 1 year of previous intubation experience performed most procedures under the direct supervision of an attending trauma anaesthesiologist. Remaining intubations were performed by the attending anaesthesiologist or by a nurse anaesthetist under attending guidance. Funding/declarations of interest: intramural research funding from University of Maryland School of Medicine Program in Trauma Additional: GlideScope had been in routine use at the study institution for 2 years before initiation of the trial. All participants were given rapid sequence induction. Re: mortality data, study authors state, "When post hoc analysis was performed on a much smaller cohort of patients, there was an observed higher mortality rate for the subgroup of patients with severe head injuries (head AIS score > 3) who were randomized to intubation with GVL (GlideScope) (22 [30%] of 73) versus DL (Macintosh) (16 [14%] of 112) (p = 0.047). This association between mortality and use of the GlideScope remained significant even when controlling for patient characteristics such as admission physiology, mechanism of injury, and injury severity" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no details other than "randomly assigned". A large number of exclusions followed randomization at the discretion of the anaesthetist. However, analysis confirmed lack of selection bias |
| Allocation concealment (selection bias) | Unclear risk | Comment: equipment and study forms (airway kit) were kept in the bag until participant was selected. Insufficient details |
| Blinding of participants and personnel (performance bias) | High risk | Comment: not possible to blind anaesthetist |
| Blinding of outcome assessment (detection bias) | High risk | Comment: not possible to blind outcome assessors |
| Incomplete outcome data (attrition bias) | High risk | Comment: large number of participants excluded at anaesthetist's discretion |
| Selective reporting (reporting bias) | Low risk | Comment: protocol sourced and outcomes comparable with reported study outcomes. Clinical trials identifier: NCT01235065 |
| Experience of intubator | Unclear risk | Comment: GlideScope had been in routine use at the institution for 2 years. All personnel had at least 1 year of experience in intubation. However, it is unclear from this description whether personnel had sufficient equivalent experience with the GlideScope |
| Baseline characteristics | Unclear risk | Comment: few baseline characteristics were reported |
| Funding sources | Low risk | Comment: intramural research funding from University of Maryland School of Medicine Program in Trauma |
# = number; ADS = airway difficulty score; AIS = abbreviated injury score; ASA = American Society of Anesthesiologists (physical status classification); BMI = body mass index; BURP = 'backwards, upwards, rightward pressure'; CABG = coronary artery bypass graft; CL or C & L = Cormack and Lehane (Cormack 1984); C‐MAC/SBT = C‐MAC device with straight blade; CRNA = certified registered nurse anaesthetist; DLT = double‐lumen tube; ED = emergency department; ENT = ear, nose and throat; ETT = endotracheal intubation; HR = heart rate; ICU = intensive care unit; ID = identification; IDS = intubation difficulty score; IQR = interquartile range; Mac = Macintosh; MAP = mean arterial pressure; MET = metabolic equivalents; M/F = male/female; MILS = manual in‐line stablilization; min/max = minimum/maximum; no. = number; PACU = postanaesthesia care unit; POGO = percentage of glottic opening; Q1, Q3 = quartile range 1, quartile range 3; SD = standard deviation; SIAARTI = The National Congress of the Italian Society of Anaesthesiology and Intensive Care Medicine; USA = United States of America; VAS = visual analogue scale; VLS = videolaryngoscope.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Difference in lumen tubes between groups | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Paediatric population | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Bullard study ‐ no details of whether Bullard was used as a videolaryngoscope | |
| Not compared against a Macintosh blade | |
| Truview EVO2 study ‐ no details of whether Truview EVO2 was used as a videolaryngoscope | |
| Truview EVO2 study ‐ no details of whether Truview EVO2 was used as a videolaryngoscope | |
| Not compared against a Macintosh blade | |
| Participants not undergoing general anaesthesia | |
| Truview EVO2 study ‐ no details of whether Truview EVO2 was used as a videolaryngoscope | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Not compared against a Macintosh blade | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Not compared against a Macintosh blade | |
| Bullard study ‐ no details of whether a Bullard was used as a videolaryngoscope | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Participants not undergoing general anaesthesia | |
| Nasotracheal intubation | |
| Does not include review outcomes | |
| Nasotracheal intubation | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Nasotracheal intubation | |
| RCT, cross‐over design. GlideScope vs Macintosh, patients with ASA I or II scheduled for gynaecological procedures. Does not report relevant review outcomes | |
| Nasotracheal intubation | |
| Nasotracheal intubation | |
| Nasotracheal intubation | |
| Not compared against a Macintosh blade | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Not compared against a Macintosh blade | |
| Nasotracheal intubation | |
| Not compared against a Macintosh blade | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| RCT, parallel design. GlideScope vs Macintosh (total N = 200). Does not measure relevant outcomes | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Not compared against a Macintosh blade | |
| Nasogastric tube insertion | |
| Nasotracheal intubation | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Not compared against a Macintosh blade | |
| Not compared against a Macintosh blade | |
| Not compared against a Macintosh blade | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Not compared against a Macintosh blade | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Not compared against a Macintosh blade | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| WuScope study ‐ fibreoptic not video device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Not compared against a Macintosh blade | |
| Not compared against a Macintosh blade | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Abstract from 2006. Insufficient detail to include and no contact details for study author | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Airtraq study ‐ no details of whether Airtraq was used with a camera device | |
| Bullard study ‐ no details of whether Bullard was used as a videolaryngoscope | |
| Unclear whether Optiscope was used with a video camera |
ASA = American Society of Anesthesiologists (physical status classification); RCT = randomized controlled trial.
Characteristics of studies awaiting classification [ordered by study ID]
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: adult patients, ASA I and II, normal intraocular pressure |
| Interventions | GlideScope vs Macintosh. Total N = 50 |
| Outcomes | No relevant outcomes reported in abstract |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: adult patients, normal intraocular pressure, scheduled for ophthalmic surgery requiring tracheal intubation |
| Interventions | GlideScope vs Macintosh. Total N = 50 but no denominator figures by group |
| Outcomes | Time to tracheal intubation |
| Notes | Abstract only with insufficient details. Awaiting publication of full text |
| Methods | Quasi‐randomized controlled trial Parallel design |
| Participants | Included: patients requiring emergency intubation |
| Interventions | GlideScope vs Macintosh. Total N = 97 |
| Outcomes | Success of intubation Successful first attempt Time to intubation |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients without features of difficult airway, requiring general anaesthesia and tracheal intubation |
| Interventions | C‐MAC vs Macintosh. Total N = 90 |
| Outcomes | CL grades Time to intubation Intubation attempts |
| Notes | MILS to simulate difficult airway Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients undergoing elective caesarean section by general anaesthesia requiring tracheal intubation |
| Interventions | GlideScope vs Macintosh. Total N = 70 |
| Outcomes | Time to intubation |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients with normal airway |
| Interventions | Truview and McGrath Series 5 vs Macintosh. Total N = 126 |
| Outcomes | Time to intubate Difficulty of intubation Failure to intubate |
| Notes | Anaesthetists divided into groups depending on level of experience Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: no details |
| Interventions | Airtraq vs Macintosh. Total N = 80 |
| Outcomes | Time to intubate POGO Ease of intubation |
| Notes | Does not state in abstract whether Airtraq was used with video camera Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: ASA I or II without difficult airway |
| Interventions | C‐MAC vs Macintosh. Total = 100 |
| Outcomes | Time to intubation Number of attempts CL grades |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: adult patients, ASA I to III |
| Interventions | C‐MAC indirect view vs C‐MAC direct view. Total N = 50 |
| Outcomes | Time to tracheal intubation |
| Notes | Study identified during peer review process. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: adult patients, ASA I to III |
| Interventions | Truview EVO2 and Airtraq vs Macintosh. Total N = 150 |
| Outcomes | Time to tracheal intubation |
| Notes | Does not state in abstract whether Airtraq was used with video camera Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: ASA I to III, scheduled to undergo surgery |
| Interventions | Pentax AWS vs Macintosh. Total N = 30 |
| Outcomes | Time to tracheal intubation |
| Notes | Abstract only with no outcomes denominator figures. Awaiting publication of full text |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: mild to moderate obesity (BMI = 28‐35) |
| Interventions | GlideScope vs Macintosh. Total N = 100 but no denominator figures by group |
| Outcomes | Time to tracheal intubation |
| Notes | Abstract only with insufficient details of outcomes. Awaiting publication of full text |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: adult patients |
| Interventions | Airtraq vs Macintosh. Total N = 40 |
| Outcomes | Time to intubation |
| Notes | Use of double‐lumen tube Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients scheduled for cardiovascular surgery |
| Interventions | Pentax AWS vs Mactintosh. Total N = 40 |
| Outcomes | Intubation success Time to tracheal intubation CL glottic view |
| Notes | Abstract only with insufficient detail to allow inclusion. No study author contact details with abstract |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: adults undergoing tracheal intubation in ICU |
| Interventions | Videolaryngoscope vs direct laryngoscopes (types not specified in abstract). Total N = 150 |
| Outcomes | Successful first attempt Time to intubation Glottic view |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: adult patients scheduled for elective surgery under 1‐lung ventilation, ASA I to III |
| Interventions | McGrath vs Macintosh. Total N = 50 Type not specified in abstract |
| Outcomes | Number of attempts Time to intubation POGO scores |
| Notes | Use of double‐lumen tube Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients without cervical spine abnormality |
| Interventions | McGrath vs Macintosh. Total N = 50 Type of McGrath not stated in abstract |
| Outcomes | Unknown |
| Notes | Data taken from English abstract. Requires full translation to establish whether relevant outcomes were measured |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients undergoing elective orthopaedic surgery that did not involve cervical spine procedure |
| Interventions | McGrath Series 5 vs Macintosh. Total N = 22 |
| Outcomes | Time to intubation Glottic view Successful intubation Number of attempts |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients scheduled to undergo general anaesthesia with tracheal intubation |
| Interventions | HPHJ‐A videolaryngoscope (n = 50) vs Macintosh (n = 50) |
| Outcomes | Time for tracheal intubation Number of attempts CL glottic view: 1 to 4 |
| Notes | Data taken from English abstract and English baseline characteristics table. Requires full translation to establish risk of bias and for data related to time outcomes |
| Methods | Randomized controlled trial Cross‐over design |
| Participants | Included: ASA I to III, no signs of predictable difficult intubation Country: Italy |
| Interventions | Glidescope vs Macintosh. Total N = 300 |
| Outcomes | Dichotomous outcomes: Intubation success Number of attempts: 1 to 2 CL grades: 1 to 4 |
| Notes | Abstract only. Results available but numbers are inconsistent; contact with study authors required to confirm results. No contact details therefore, awaiting publication of full text |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients scheduled for video‐assisted thoracoscopic surgery for pulmonary resection requiring left‐sided double‐lumen tube insertion |
| Interventions | Airtraq and GlideScope vs Macintosh |
| Outcomes | Failure to intubate Time to intubation Sore throat, dental injury, mucosal bleeding |
| Notes | Use of double‐lumen tube Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Age 18 to 80 years ASA I to III Presenting for elective surgery Requires general anaesthesia Present as a possible difficult intubation (≥ 1 of the following): history of difficult intubations, morbid obesity, small mouth opening (< 3 fingerbreadths), limited neck mobility, Mallampati classes II and III, short thyromental distance (< 6 cm) |
| Interventions | Storz DCI videolaryngoscope vs Macintosh |
| Outcomes | 5‐Scale score of glottic view Time and number of attempts required Level of difficulty Degree of irritation of the pharynx, epiglottis and arytenoids Vital signs, oxygen saturation and end‐tidal carbon dioxide |
| Notes | Registered at clinicaltrials.gov. Listed as completed, but no results posted and have not been able to source completed study |
| Methods | Randomized controlled trial Parallel design |
| Participants | Elective adult surgical patient requiring tracheal anaesthesia Males and females ASA I to III Age 18 years of age and older |
| Interventions | Airtraq AWS and Storz DCI and GlideScope and McGrath vs Macintosh |
| Outcomes | Percentage distribution of Cook's modification of Cormack‐Lehane's grading system. Each study subject will receive a grade of 1, 2A, 2B, 3A, 3B or 4 in the Cook classification Intubation time: measured from entry of the device into the oral cavity until confirmation of proper placement of tracheal tube, as judged by an exhaled tidal volume > 200 mL and the presence of end‐tidal carbon dioxide (CO2) Success rate: number of attempts required for successful intubation by an attending anaesthesiologist Maximal neck extension: using atlanto‐occipital joint extension scale Ease of intubation: judged by laryngoscopist on a 5‐point rating scale: 5 is excellent, 1 is poor Complication rate: All complications will be recorded, with special attention given to common complications, such as upper airway and dental trauma Interincisor distance: maximal mouth opening necessary for intubation Laryngoscopist's comments: pertinent device‐specific clinical comments Vital signs (blood pressure, heart rate, mean arterial pressure, and pulse oximeter rate) |
| Notes | Registered at clinicaltrials.gov. Listed as completed, but no results posted and have not been able to source completed study. No contact made with study authors |
| Methods | RCT, cross‐over design |
| Participants | Elective non‐cardiac surgery requiring intubation Adults ASA I to III BMI < 35 |
| Interventions | Airtraq vs Macintosh |
| Outcomes | Cervical spine movement Time to Intubation |
| Notes | Registered at clinicaltrials.gov. Listed as completed, but no results posted and have not been able to source completed study. No contact made with study authors |
| Methods | Randomized controlled trial Parallel design |
| Participants | Adults 18 years and over Scheduled for elective surgery Anaesthetic plan would normally include oral intubation with a Macintosh laryngoscope blade by a junior anaesthetist Valid informed consent |
| Interventions | Pentax AWS vs Macintosh |
| Outcomes | Is there a clinically significant difference in the time taken to successfully intubate the trachea? Is there a difference in the intubation difficulty score? |
| Notes | Registered at clinicaltrials.gov. Status listed as unknown but estimated completion date registered as September 2012. No results posted and have not been able to source completed study No contact made with study authors |
| Methods | Randomized controlled trial |
| Participants | Patients with documented BMI > 35 kg/m2 Scheduled to undergo inpatient surgery procedures under general anaesthesia. Willingness and ability to sign an informed consent document 18 to 80 years of age ASA II to III adults of either sex |
| Interventions | Karl Storz Video‐Mac and GlideScope and McGrath vs Macintosh |
| Outcomes | Intubation time using a stop watch Glottis visualization using CL and POGO score |
| Notes | Registered at clinicaltrials.gov. Listed as completed, but no results posted and have not been able to source completed study. No contact made with study authors |
| Methods | Randomized controlled trial Parallel design |
| Participants | Any adult patient booked for elective surgery requiring orotracheal intubation with a double‐lumen endotracheal tube. |
| Interventions | GlideScope Groove vs Macintosh |
| Outcomes | Duration of Intubation Number of intubation attempts Number of failures to intubate Use of external laryngeal pressure Laryngoscopic grade distribution: CL grade observed during laryngoscopy Presence of sore throat: graded on postoperative day 2 as none, mild, moderate or severe |
| Notes | Registered at clinicaltrials.gov. Status listed as unknown, but estimated completion date registered as December 2014. No results posted and have not been able to source completed study. No contact made with study authors |
| Methods | Randomized controlled trial Parallel design |
| Participants | Elective procedure requiring oral tracheal tube intubation Over 16 years of age Airway assessment suggests to the anaesthetist that a standard Macintosh laryngoscope approach to intubation would be appropriate |
| Interventions | McGrath vs Macintosh |
| Outcomes | Intubation difficulty score Time to intubation Number and types of alternative techniques used Perception of force used Complications Ease of intubation Failure to intubate |
| Notes | Registered at clinicaltrials.gov. Listed as completed, but no results posted and have not been able to source completed study. No contact made with study authors |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: adult patients, thoracic surgery requiring 1‐lung ventilation |
| Interventions | McGrath Series 5 videolaryngoscope vs Macintosh |
| Outcomes | Intubation time measured with a stopwatch, defined as time from insertion of blade into the mouth to withdrawal of blade Number of successful intubations at first attempt |
| Notes | Registered at clinicaltrials.gov. Listed as completed, but no results posted and have not been able to source completed study. No contact made with study authors |
| Methods | Randomized controlled trial Cross‐over design |
| Participants | Included: ASA I to III with non‐anticipated difficult airways |
| Interventions | McGrath Series 5, C‐MAC, GlideScope and Macintosh. Total N = 141 |
| Outcomes | No relevant outcomes reported in abstract |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: female patients, ASA I to III, 18 to 65 years of age, BMI > 30 kg/m2 |
| Interventions | McGrath Series 5 vs Macintosh. Total = 84 |
| Outcomes | CL grades Intubation difficulty Time to intubation |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients scheduled for bariatric surgery, BMI > 35 kg/m2 |
| Interventions | GlideScope vs Macintosh. Total N = 100 |
| Outcomes | Time to intubation Intubation difficulty Number of attempts CL grades Sore throat, hoarseness |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients requiring urgent tracheal intubation |
| Interventions | GlideScope vs Macintosh. Total N = 117 |
| Outcomes | Success of first intubation Rates of complications |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients without predictors of difficult tracheal intubation |
| Interventions | McGrath vs Macintosh. Number of participants not specified Type of McGrath not specified |
| Outcomes | Difficulty of intubation Time to intubation |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update. Unclear if this is an RCT |
| Methods | No English abstract available for additional details |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Title suggests possible inclusion, but paper requires translation from Chinese |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients with predicted good glottic view |
| Interventions | McGrath Series 5 vs Macintosh. Total N = 96 |
| Outcomes | Time to intubate CL grades |
| Notes | Use of double‐lumen tube Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: morbidly obese patients (BMI > 35 kg/m2) scheduled for general, gynaecological and bariatric surgery |
| Interventions | GlideScope and LMA CTrach TM vs Macintosh. Total N = 90 |
| Outcomes | Intubation difficulty score Time to intubate Overall success rate Number of attempts CL grades |
| Notes | Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
| Methods | Randomized controlled trial Parallel design |
| Participants | Included: patients scheduled for surgery under general anaesthesia |
| Interventions | Airtraq vs Macintosh. Total N = 149 |
| Outcomes | Successful intubation CL grades Time to intubate |
| Notes | Does not state in abstract whether Airtraq is used with video camera Study identified during January 2016 search. Review of full text required to assess eligibility during next update |
ASA = American Society of Anesthesiologists (physical status classification); BMI = body mass index; CL = Cormack and Lehane (Cormack 1984); MILS = manual in‐line stabilization; POGO = percentage of glottic opening; RCT = randomized controlled trial
Characteristics of ongoing studies [ordered by study ID]
| Study name | Comparison of the Macintosh, King Vision®, GlideScope® and Airtraq® laryngoscopes in routine airway management |
| Methods | RCT, parallel design |
| Participants | ASA I or II Aged 18 to 65 years Scheduled for elective minor surgery Under general anaesthesia Female |
| Interventions | King Vision, GlideScope, Airtraq, Macintosh |
| Outcomes | Time to tracheal intubation: time when the investigated laryngoscope passes the central incisors to time when the tip of the tracheal tube passes through the glottis Laryngoscopic view: best view during laryngoscopy (using Cormack and Lehane classification) Ease of intubation on a 100‐mm visual analogue scale (0 for much ease and 100 for extremely difficult) Number of intubation attempts Number of optimization manoeuvres: If intubation was unsuccessful at the first attempt, took longer than 180 seconds, or if desaturation noted on the pulse oximeter (defined as SpO2 < 93%) [14], intubation attempt will be stopped, and the lungs will be ventilated with an oxygen‐volatile anaesthetic mixture for 3 minutes. Second attempt will be allowed with randomly allocated airway device Duration of laryngoscopy: time from holding of the investigated laryngoscope to appearance as the first upward deflection on the capnograph Haemodynamic parameters: heart rate, systolic and mean blood pressures |
| Starting date | September 2013 |
| Contact information | Mohamed R El Tahan, MD; [email protected] |
| Notes |
| Study name | King Vision and cervical spines movement |
| Methods | RCT, cross‐over design |
| Participants | Sixteen participants, ASA I or II Aged 18 to 65 years Scheduled for elective minor surgery Under general anaesthesia |
| Interventions | King Vision, Macintosh |
| Outcomes | Cervical spine movement Time to intubation: time when the investigated laryngoscope passes the central incisors to time when the tip of the tracheal tube passed through the glottis Laryngoscopic view: glottic view during laryngoscopy will be assessed according to the Cormack‐Lehane grading system: Grade 1, full view; Grade 2, only arytenoid cartilages visible; Grade 3, only epiglottis visible; Grade 4, epiglottis not visible Ease of intubation: rate ease of intubation on a 100‐mm visual analogue scale (0 for much ease and 100 for extremely difficult). Number of intubation attempts Number of optimization manoeuvres |
| Starting date | October 2013 |
| Contact information | Mohamed R El Tahan, MD; [email protected] |
| Notes | Listed as ongoing study at clinicaltrials.gov |
| Study name | Evaluation of videolaryngoscopes in difficult airway (SWIVITII) |
| Methods | RCT, parallel design |
| Participants | Elective surgery with general anaesthesia requiring intubation > 18 years old ASA I to III |
| Interventions | Airtraq, King Vision, AP Advance, Macintosh |
| Outcomes | First attempt intubation success rate Side effects: sore throat, bleeding, dental injuries |
| Starting date | February 2014 |
| Contact information | Lorenz G Theiler, MD; [email protected] |
| Notes |
| Study name | Comparison of Indirect and Direct Laryngoscopy in Obese Patients |
| Methods | RCT, parallel design |
| Participants | Obese adult patients (BMI > 35 kg/m2) for elective bariatric surgery |
| Interventions | Storz C‐MAC, Macintosh |
| Outcomes | POGO (percentage of glottic opening) score at maximum laryngeal view for 3 laryngoscopes (Macintosh, Storz C‐MAC, standard and D‐blade) Subjective "ease of intubation" Time to intubate |
| Starting date | January 2013 |
| Contact information | Peter Charters. Aintree University Hospital |
| Notes |
| Study name | McGrath Mac videoLaryngoscope vs Macintosh laryngoscope (MGM‐Eval) |
| Methods | RCT, parallel design |
| Participants | Adult patients scheduled for general anaesthesia with orotracheal intubation |
| Interventions | McGrath Mac videolaryngoscope vs Macintosh |
| Outcomes | Ease of tracheal intubation Ease of intubation measured on the Intubation Difficulty Scale Time to obtain first capnogram (seconds) Score of Cormak and Lehane modified by Yentis POGO (percentage of glottic opening) score Rate of use of alternative techniques for intubation Rate of oesophageal intubation Incidence of arterial oxygen desaturation (SpO2 < 92%) Rate of failure of tracheal intubation Rate of haemodynamic abnormality Postoperative throat pain Postoperative hoarseness Questionnaire of Salditt−Isabel |
| Starting date | November 2014 |
| Contact information | Marc Fischler, MD; m.fischler@hopital‐foch.org |
| Notes |
| Study name | Rapid Sequence Intubation at the Emergency Department |
| Methods | RCT, parallel design |
| Participants | Patients requiring emergency rapid sequence intubation at the emergency department Male and female participants 18 years to 99 years of age Written confirmation by a physician not involved in this study Written informed consent by the participant (obtained afterwards) Participant not showing remarkable rejection in participation in this study |
| Interventions | C‐MAC videolaryngoscope, Macintosh |
| Outcomes | Success rate defined as successful placement of endotracheal tube within the trachea Time to intubation defined as time between insertion of the videolaryngoscope/Macintosh blade into the mouth until detection of end‐tidal CO2 Laryngoscopic view: Cormack and Lehane score Number of intubation attempts Unrecognized oesophageal intubation Ease of intubation (1‐5): (1) very easy, (2) easy, (3) somewhat difficult, (4) difficult, (5) impossible Violations of the teeth: number of patients; teeth will be inspected for potential damage and documented accordingly Necessity of using additional, alternative airway devices for successful intubation (if randomized airway device failed): number of participants requiring alternate device Maximum drop of saturation: SpO2 will be measured continuously and documented accordingly |
| Starting date | November 2014 |
| Contact information | Kurt Ruetzler, MD; [email protected] |
| Notes |
| Study name | Videolaryngoscopes for Double Lumen Tube Intubations |
| Methods | RCT, parallel design |
| Participants | ASA II/III Elective thoracic procedures Adult Estimated 120 participants |
| Interventions | Airtraq, GlideScope, King Vision, Macintosh |
| Outcomes | Time to duration of endobronchial intubation: defined as time from when the laryngoscope entered between the participant's lips until successful DLT placement (regardless of the number of attempts) Best obtained glottis view during laryngoscopy using Cormack and Lehane direct view or 'video assisted view' seen on the video display screen Ease of endobronchial intubation on a visual analogue score (VAS) of ease of endobronchial intubation (0 for much ease and 100 for extremely difficult) Number of optimization manoeuvres Number of 'backwards upwards rightwards pressure' (BURP) manoeuvre Failure rate for double‐lumen tube intubation Sore throat on a VAS from 0, indicating 'none', to 10, 'severe' sore throat Hoarseness on numerical scale observed by the anaesthesiologist (0: absent, 1: subjective, or 3: aphonic) |
| Starting date | January 2015 |
| Contact information | Mohamed R El Tahan, MD; [email protected] |
| Notes |
ASA = American Society of Anesthesiologists (physical status classification); BMI = body mass index; DLT = double‐lumen tubes; RCT = randomized controlled trial; VAS = visual analogue scale.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Failed intubation Show forest plot | 38 | 4127 | Odds Ratio (M‐H, Random, 95% CI) | 0.35 [0.19, 0.65] |
| Analysis 1.1  Comparison 1: VLS versus Macintosh, Outcome 1: Failed intubation | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Hypoxia Show forest plot | 8 | 1319 | Odds Ratio (M‐H, Random, 95% CI) | 0.39 [0.10, 1.44] |
| Analysis 2.1  Comparison 2: VLS versus Macintosh, Outcome 1: Hypoxia | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Mortality Show forest plot | 2 | 663 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.65, 1.82] |
| Analysis 3.1  Comparison 3: VLS versus Macintosh, Outcome 1: Mortality | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Laryngeal/airway trauma Show forest plot | 29 | 3110 | Odds Ratio (M‐H, Random, 95% CI) | 0.68 [0.48, 0.96] |
| Analysis 4.1  Comparison 4: VLS versus Macintosh, Outcome 1: Laryngeal/airway trauma | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 5.1 Patient‐reported sore throat Show forest plot | 17 | 2392 | Odds Ratio (M‐H, Random, 95% CI) | 0.82 [0.56, 1.19] |
| Analysis 5.1  Comparison 5: VLS versus Macintosh, Outcome 1: Patient‐reported sore throat | ||||
| 5.1.1 Postanaesthesia care unit | 10 | 1548 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.73, 1.38] |
| 5.1.2 Postoperative day 1 | 8 | 844 | Odds Ratio (M‐H, Random, 95% CI) | 0.54 [0.27, 1.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 6.1 Hoarseness Show forest plot | 6 | 527 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.36, 0.88] |
| Analysis 6.1  Comparison 6: VLS versus Macintosh, Outcome 1: Hoarseness | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 7.1 Successful first attempt Show forest plot | 36 | 4731 | Odds Ratio (M‐H, Random, 95% CI) | 1.27 [0.77, 2.09] |
| Analysis 7.1  Comparison 7: VLS versus Macintosh, Outcome 1: Successful first attempt | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 8.1 Number of attempts Show forest plot | 28 | 6692 | Odds Ratio (M‐H, Random, 95% CI) | 1.06 [0.68, 1.66] |
| Analysis 8.1  Comparison 8: VLS versus Macintosh, Outcome 1: Number of attempts | ||||
| 8.1.1 1 attempt | 28 | 3346 | Odds Ratio (M‐H, Random, 95% CI) | 1.25 [0.68, 2.31] |
| 8.1.2 2 to 4 attempts | 28 | 3346 | Odds Ratio (M‐H, Random, 95% CI) | 0.89 [0.47, 1.70] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 9.1 Time for tracheal intubation Show forest plot | 37 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 9.1  Comparison 9: VLS versus Macintosh, Outcome 1: Time for tracheal intubation | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 10.1 Intubation difficult score (IDS) Show forest plot | 7 | 568 | Odds Ratio (M‐H, Random, 95% CI) | 7.13 [3.12, 16.31] |
| Analysis 10.1  Comparison 10: VLS versus Macintosh, Outcome 1: Intubation difficult score (IDS) | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 11.1 Improved visualization Cormack & Lehane (CL) 1 Show forest plot | 22 | 2240 | Odds Ratio (M‐H, Random, 95% CI) | 6.77 [4.17, 10.98] |
| Analysis 11.1  Comparison 11: VLS versus Macintosh, Outcome 1: Improved visualization Cormack & Lehane (CL) 1 | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 12.1 Improved visualization Cormack & Lehane (CL) 1 to 4 Show forest plot | 22 | 4480 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.54, 1.87] |
| Analysis 12.1  Comparison 12: VLS versus Macintosh, Outcome 1: Improved visualization Cormack & Lehane (CL) 1 to 4 | ||||
| 12.1.1 CL 1 to 2 | 22 | 2240 | Odds Ratio (M‐H, Random, 95% CI) | 5.42 [3.70, 7.95] |
| 12.1.2 CL 3 to 4 | 22 | 2240 | Odds Ratio (M‐H, Random, 95% CI) | 0.18 [0.13, 0.27] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 13.1 Improved visualization POGO Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 13.1  Comparison 13: VLS versus Macintosh, Outcome 1: Improved visualization POGO | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 14.1 Failed intubation by scope Show forest plot | 33 | 3916 | Odds Ratio (M‐H, Random, 95% CI) | 0.40 [0.21, 0.75] |
| Analysis 14.1  Comparison 14: VLS versus Macintosh, Outcome 1: Failed intubation by scope | ||||
| 14.1.1 GlideScope | 16 | 1306 | Odds Ratio (M‐H, Random, 95% CI) | 0.57 [0.25, 1.32] |
| 14.1.2 Pentax AWS | 11 | 1086 | Odds Ratio (M‐H, Random, 95% CI) | 0.24 [0.05, 1.20] |
| 14.1.3 McGrath | 5 | 466 | Odds Ratio (M‐H, Random, 95% CI) | 1.18 [0.06, 23.92] |
| 14.1.4 C‐MAC | 8 | 1058 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.15, 0.68] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 15.1 Failed intubation by airway difficulty Show forest plot | 34 | 3383 | Odds Ratio (M‐H, Random, 95% CI) | 0.35 [0.18, 0.65] |
| Analysis 15.1  Comparison 15: VLS versus Macintosh, Outcome 1: Failed intubation by airway difficulty | ||||
| 15.1.1 Predicted not difficult | 19 | 1743 | Odds Ratio (M‐H, Random, 95% CI) | 0.61 [0.22, 1.67] |
| 15.1.2 Predicted difficult | 6 | 830 | Odds Ratio (M‐H, Random, 95% CI) | 0.28 [0.15, 0.55] |
| 15.1.3 Simulated difficult | 9 | 810 | Odds Ratio (M‐H, Random, 95% CI) | 0.18 [0.04, 0.77] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 16.1 Failed intubation by experience of personnel Show forest plot | 22 | 2273 | Odds Ratio (M‐H, Random, 95% CI) | 0.29 [0.13, 0.67] |
| Analysis 16.1  Comparison 16: VLS versus Macintosh, Outcome 1: Failed intubation by experience of personnel | ||||
| 16.1.1 Personnel experienced with both devices | 17 | 1927 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.13, 0.75] |
| 16.1.2 Personnel less experienced with VLS | 5 | 346 | Odds Ratio (M‐H, Random, 95% CI) | 0.20 [0.02, 2.56] |
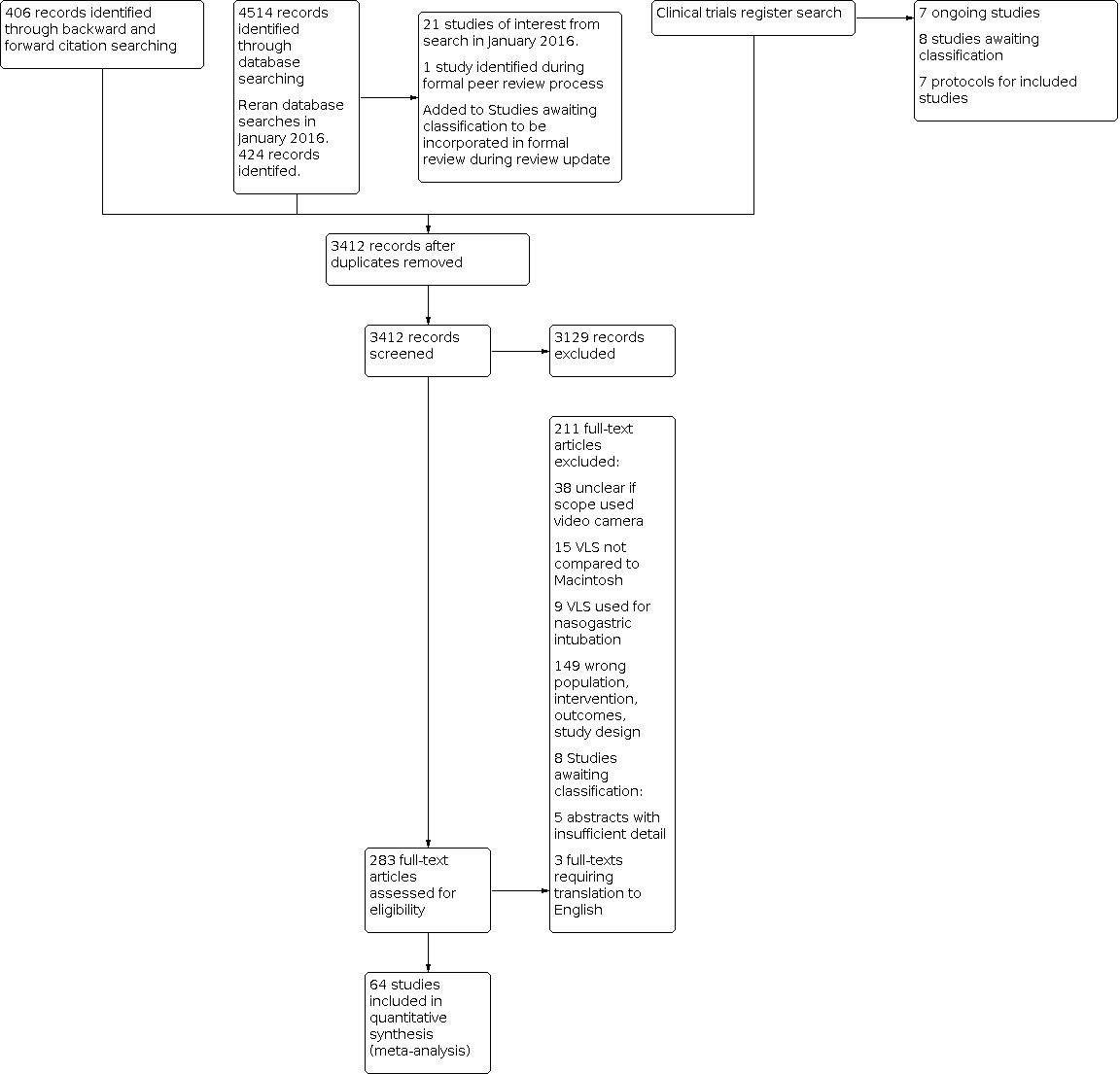
Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Funnel plot of comparison: 1 Failed intubation, outcome: 1.1 Failed intubation.

Comparison 1: VLS versus Macintosh, Outcome 1: Failed intubation

Comparison 2: VLS versus Macintosh, Outcome 1: Hypoxia

Comparison 3: VLS versus Macintosh, Outcome 1: Mortality

Comparison 4: VLS versus Macintosh, Outcome 1: Laryngeal/airway trauma

Comparison 5: VLS versus Macintosh, Outcome 1: Patient‐reported sore throat

Comparison 6: VLS versus Macintosh, Outcome 1: Hoarseness

Comparison 7: VLS versus Macintosh, Outcome 1: Successful first attempt

Comparison 8: VLS versus Macintosh, Outcome 1: Number of attempts

Comparison 9: VLS versus Macintosh, Outcome 1: Time for tracheal intubation

Comparison 10: VLS versus Macintosh, Outcome 1: Intubation difficult score (IDS)

Comparison 11: VLS versus Macintosh, Outcome 1: Improved visualization Cormack & Lehane (CL) 1

Comparison 12: VLS versus Macintosh, Outcome 1: Improved visualization Cormack & Lehane (CL) 1 to 4

Comparison 13: VLS versus Macintosh, Outcome 1: Improved visualization POGO

Comparison 14: VLS versus Macintosh, Outcome 1: Failed intubation by scope

Comparison 15: VLS versus Macintosh, Outcome 1: Failed intubation by airway difficulty

Comparison 16: VLS versus Macintosh, Outcome 1: Failed intubation by experience of personnel
| Videolaryngoscopy compared with direct laryngoscopy for tracheal intubation | ||||||
| Patient or population: patients requiring tracheal intubation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Direct laryngoscopy | Videolaryngoscopy | |||||
| Failed intubation | Study population | OR 0.35 | 4127 | ⊕⊕⊕⊝ | Downgraded by 1 level. See footnote. | |
| 94 per 1000 | 35 per 1000 | |||||
| Moderate | ||||||
| Hypoxia | Study population | OR 0.39 | 1319 | ⊕⊝⊝⊝ | Downgraded by 3 levels. See footnotes. | |
| 58 per 1000 | 23 per 1000 | |||||
| Moderate | ||||||
| Serious respiratory complications | See comment | See comment | Not estimable | 78 | ⊕⊝⊝⊝ | Insufficient data to complete meta‐analysis. Downgraded by 2 levels. See footnotes. |
| Mortality | Study population | OR 1.09 | 663 | ⊕⊝⊝⊝ | Downgraded by 3 levels. See footnotes. | |
| 106 per 1000 | 114 per 1000 | |||||
| Very low | ||||||
| Proportion of successful first attempts | Study population | OR 0.79 | 4731 | ⊕⊕⊕⊝ | Downgraded by 1 level. See footnotes. | |
| 831 per 1000 | 795 per 1000 | |||||
| Moderate | ||||||
| Sore throat | Study population | OR 1.00 | 1548 | ⊕⊕⊕⊝ | Downgraded by 1 level. See footnotes. | |
| 250 per 1000 | 289 per 1000 | |||||
| Moderate | ||||||
| Time for tracheal intubation | See comment | See comment | Not estimable | 4488 | ⊕⊝⊝⊝ | High level of statistical heterogeneity between studies; therefore meta‐analysis not completed. Downgraded by 3 levels. See footnotes. |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aNot possible to blind intubator to device. Downgraded for study limitations. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Failed intubation Show forest plot | 38 | 4127 | Odds Ratio (M‐H, Random, 95% CI) | 0.35 [0.19, 0.65] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Hypoxia Show forest plot | 8 | 1319 | Odds Ratio (M‐H, Random, 95% CI) | 0.39 [0.10, 1.44] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Mortality Show forest plot | 2 | 663 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.65, 1.82] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Laryngeal/airway trauma Show forest plot | 29 | 3110 | Odds Ratio (M‐H, Random, 95% CI) | 0.68 [0.48, 0.96] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 5.1 Patient‐reported sore throat Show forest plot | 17 | 2392 | Odds Ratio (M‐H, Random, 95% CI) | 0.82 [0.56, 1.19] |
| 5.1.1 Postanaesthesia care unit | 10 | 1548 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.73, 1.38] |
| 5.1.2 Postoperative day 1 | 8 | 844 | Odds Ratio (M‐H, Random, 95% CI) | 0.54 [0.27, 1.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 6.1 Hoarseness Show forest plot | 6 | 527 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.36, 0.88] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 7.1 Successful first attempt Show forest plot | 36 | 4731 | Odds Ratio (M‐H, Random, 95% CI) | 1.27 [0.77, 2.09] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 8.1 Number of attempts Show forest plot | 28 | 6692 | Odds Ratio (M‐H, Random, 95% CI) | 1.06 [0.68, 1.66] |
| 8.1.1 1 attempt | 28 | 3346 | Odds Ratio (M‐H, Random, 95% CI) | 1.25 [0.68, 2.31] |
| 8.1.2 2 to 4 attempts | 28 | 3346 | Odds Ratio (M‐H, Random, 95% CI) | 0.89 [0.47, 1.70] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 9.1 Time for tracheal intubation Show forest plot | 37 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 10.1 Intubation difficult score (IDS) Show forest plot | 7 | 568 | Odds Ratio (M‐H, Random, 95% CI) | 7.13 [3.12, 16.31] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 11.1 Improved visualization Cormack & Lehane (CL) 1 Show forest plot | 22 | 2240 | Odds Ratio (M‐H, Random, 95% CI) | 6.77 [4.17, 10.98] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 12.1 Improved visualization Cormack & Lehane (CL) 1 to 4 Show forest plot | 22 | 4480 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.54, 1.87] |
| 12.1.1 CL 1 to 2 | 22 | 2240 | Odds Ratio (M‐H, Random, 95% CI) | 5.42 [3.70, 7.95] |
| 12.1.2 CL 3 to 4 | 22 | 2240 | Odds Ratio (M‐H, Random, 95% CI) | 0.18 [0.13, 0.27] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 13.1 Improved visualization POGO Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 14.1 Failed intubation by scope Show forest plot | 33 | 3916 | Odds Ratio (M‐H, Random, 95% CI) | 0.40 [0.21, 0.75] |
| 14.1.1 GlideScope | 16 | 1306 | Odds Ratio (M‐H, Random, 95% CI) | 0.57 [0.25, 1.32] |
| 14.1.2 Pentax AWS | 11 | 1086 | Odds Ratio (M‐H, Random, 95% CI) | 0.24 [0.05, 1.20] |
| 14.1.3 McGrath | 5 | 466 | Odds Ratio (M‐H, Random, 95% CI) | 1.18 [0.06, 23.92] |
| 14.1.4 C‐MAC | 8 | 1058 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.15, 0.68] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 15.1 Failed intubation by airway difficulty Show forest plot | 34 | 3383 | Odds Ratio (M‐H, Random, 95% CI) | 0.35 [0.18, 0.65] |
| 15.1.1 Predicted not difficult | 19 | 1743 | Odds Ratio (M‐H, Random, 95% CI) | 0.61 [0.22, 1.67] |
| 15.1.2 Predicted difficult | 6 | 830 | Odds Ratio (M‐H, Random, 95% CI) | 0.28 [0.15, 0.55] |
| 15.1.3 Simulated difficult | 9 | 810 | Odds Ratio (M‐H, Random, 95% CI) | 0.18 [0.04, 0.77] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 16.1 Failed intubation by experience of personnel Show forest plot | 22 | 2273 | Odds Ratio (M‐H, Random, 95% CI) | 0.29 [0.13, 0.67] |
| 16.1.1 Personnel experienced with both devices | 17 | 1927 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.13, 0.75] |
| 16.1.2 Personnel less experienced with VLS | 5 | 346 | Odds Ratio (M‐H, Random, 95% CI) | 0.20 [0.02, 2.56] |

