Anticonceptivos orales combinados: riesgo de infarto de miocardio y de accidente cerebrovascular isquémico
Información
- DOI:
- https://doi.org/10.1002/14651858.CD011054.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 27 agosto 2015see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Regulación de la fertilidad
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
REJR, OMD and FMH developed the study design. TS provided statistical expertise. AA and WML provided clinical expertise. REJR drafted the protocol. OMD and FMH edited the protocol. REJR and FMH independently selected the publications and extracted the data. REJR interpreted the data and drafted the manuscript. FMH, OMD, TS, AA and WML critically reviewed drafts of the manuscript.
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
Netherlands Heart Foundation, Netherlands.
Dr Willem Lijfering is a postdoctoral researcher for the Netherlands Heart Foundation (2011T012). This organization did not play a role in the design and conduct of this study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Declarations of interest
REJR declares no conflict of interest.
FMH declares no conflict of interest.
WML declares no conflict of interest.
TS declares no conflict of interest.
AA declares no conflict of interest.
OMD declares no conflict of interest.
Acknowledgements
We thank Carol Manion, Reference Librarian at FHI360, Durham, USA, and Jan W. Schoones, Walaeus Library, LUMC, Leiden, NL for developing the search strategies.
Version history
| Published | Title | Stage | Authors | Version |
| 2015 Aug 27 | Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke | Review | Rachel E.J. Roach, Frans M Helmerhorst, Willem M. Lijfering, Theo Stijnen, Ale Algra, Olaf M Dekkers | |
| 2014 Mar 30 | Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke | Protocol | Rachel E.J. Roach, Frans M Helmerhorst, Willem M. Lijfering, Ale Algra, Olaf M Dekkers | |
Differences between protocol and review
During data extraction we noticed that the age cut‐off for women included in the analyses differed per study. Some studies had an upper age limit of 45 years, whereas other studies had an upper limit of 60 or no upper age limit at all. In this review, we chose to include (mostly) pre‐menopausal women, and so chose an age cut‐off of 50 years. We did this by including studies that included women up to 50 years of age, and, where possible, also by extracting data on women < 50 years from studies that included older women.
In the protocol, Roach 2014, we stated that we would assess the risk of myocardial infarction or ischemic stroke for first, second and third generation contraceptive preparations in our analysis on COC generation, and also for preparations containing drospirenone. In the review we have now added cyproterone acetate to this sentence, as this is also a commonly used type of progestagen that cannot be assigned to a generation.
Information on how each generation of COC pill was classified was not present in the protocol 'Methods' section. This information is important as oral contraceptive generations can be classified in more than one way. We have added the definitions to the Types of interventions section.
We aimed to investigate the risk of reporting bias in a funnel plot. However, as our review included various different types of analysis (overall risk, and risk according to generation, estrogen dose and progestagen type), and four different types of bias were assessed along with confounding, making a funnel plot was not feasible. Instead, we presented the risk of bias in the review text, a 'Risk of bias' table and a 'Risk of bias' summary figure.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Case‐Control Studies;
- Cohort Studies;
- Contraceptives, Oral, Combined [*adverse effects];
- Estrogens [administration & dosage, *adverse effects];
- Myocardial Infarction [*chemically induced];
- Observational Studies as Topic;
- Progestins [administration & dosage, *adverse effects];
- Risk Assessment;
- Stroke [*chemically induced];
Medical Subject Headings Check Words
Female; Humans;
PICO

Study flow diagram.
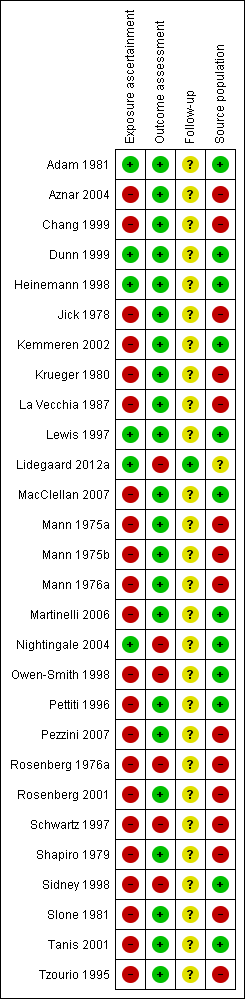
Risk of bias in the 28 included articles (reporting on 24 included studies). Green: low risk; red: high risk; yellow: unclear risk.
Regarding Lidegaard 2012a "Source population": not applicable as this was a population study.

Effect of myocardial infarction and/or stroke in oral contraceptive users versus non‐users.

Effect of myocardial infarction and/or stroke in oral contraceptive users versus non‐users stratified per generation
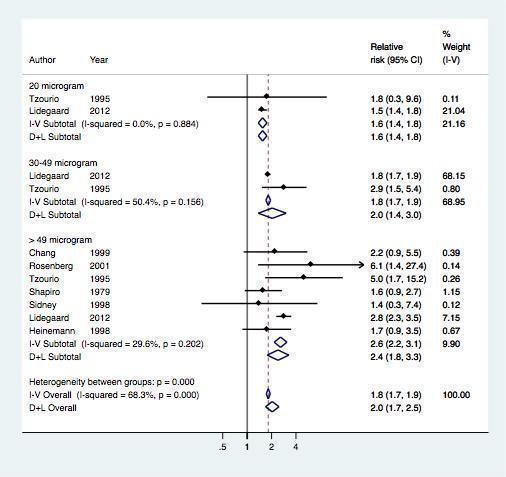
Effect of myocardial infarction and/or stroke in oral contraceptive users versus non‐users stratified by estrogen dose
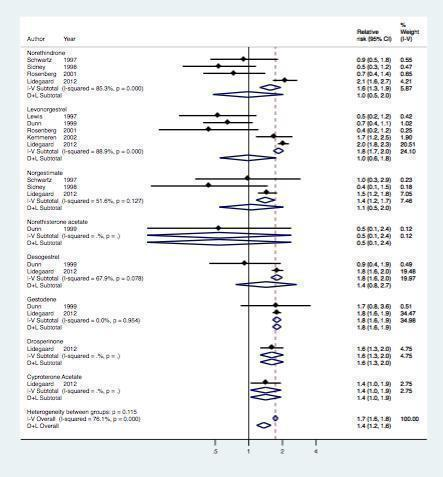
Effect of myocardial infarction and/or stroke in oral contraceptive users versus non‐users stratified per prosgestagen type
| Study | P ublication year | Study design | Outcomea |
| 1981 | Case control | Myocardial infarction | |
| 2004 | Case control | Ischemic stroke | |
| 1999 | Case control | Ischemic stroke | |
| 1999 | Case control | Myocardial infarction | |
| 1998/1997 | Case control | Both | |
| 1978 | Case control | Myocardial infarction | |
| 2002/2001 | Case control | Both | |
| 1981 | Case control | Myocardial infarction | |
| 1987 | Case control | Myocardial infarction | |
| 2012 | Cohort | Both | |
| 2007 | Case control | Ischemic stroke | |
| 1975/1976 | Case control | Myocardial infarction | |
| 1975 | Case control | Myocardial infarction | |
| 2006 | Case control | Ischemic stroke | |
| 2004 | Nested case control | Ischemic stroke | |
| 1998 | Case control | Ischemic stroke | |
| 1997 | Case control | Ischemic stroke | |
| 2007 | Case control | Ischemic stroke | |
| 1976 | Case control | Myocardial infarction | |
| 2001 | Case control | Myocardial infarction | |
| 1998 | Case control | Ischemic stroke | |
| 1998 | Case control | Myocardial infarction | |
| 1981/1981 | Case control | Myocardial infarction | |
| 1995 | Case control | Ischemic stroke | |
| aDenotes both myocardial infarction and ischemic stroke. | |||
| Study | Design | Outcome | Non‐use Event (n)/Total (n) | 1st generation Event (n)/Total (n) | 2nd generation Event (n)/Total (n) | 3rd generation Event (n)/Total (n) |
| Case‐control | Myocardial infarction | 386/1853 | — | 20/139 | 20/81 | |
| Case‐control | Ischemic stroke | 101/669 | 7/38 | 52/225 | 32/142 | |
| Case‐control | Ischemic stroke | 125/397 | 14/28 | 27/62 | 8/41 | |
| Cohort | Both | * | * | * | * | |
| Case‐control | Myocardial infarction | 591/3301 | 11/79 | 4/46 | 2/17 | |
| Case‐control | Ischemic stroke | 52/476 | 4/36 | 1/15 | — | |
| Case‐control | Myocardial infarction | 255/1159 | 8/60 | 3/27 | — | |
| Case‐control | Myocardial infarction | 146/714 | 11/42 | 59/232 | 20/130 | |
| Abbreviations: COC: combined oral contraceptives; n: number. * Adjusted effect estimates extracted | ||||||
| Study | Design | Outcome | Non‐use Event (n)/Total (n) | 20 µg E2 Event (n)/Total (n) | 30 to 49 µg E2 Event (n)/Total (n) | ≥ 50 µg E2 Event (n)/Total (n) |
| Case‐control | Ischemic stroke | 42/188 | — | — | 9/23 | |
| Case‐control | Ischemic stroke | 96/353 | — | — | 15/38 | |
| Cohort | Both | * | * | * | * | |
| Case‐control | Myocardial infarction | 591/3301 | — | — | 4/7 | |
| Case‐control | Myocardial infarction | 205/1812 | — | — | 18/107 | |
| Case‐control | Myocardial infarction | 255/1159 | — | — | 2/7 | |
| Case‐control | Ischemic stroke | 25/135 | 2/7 | 30/76 | 8/15 | |
| Abbreviations: µg: micrograms; E2: ethinylestradiol; n: number. * Adjusted effect estimates extracted | ||||||
| Study | Design | Outcome | Event (n)/Total (n) | ||||||||
| Non‐use | Norethindron | Levonorgestrel | Norethisterone acetate | Desogestrel | Gestodene | Norgestimate | Drospirenone | Cyproterone acetate | |||
| Case‐control | Myocardial infarction | 386/1853 | — | 18/123 | 2/16 | 9/46 | 11/35 | — | — | — | |
| Case‐control | Ischemic stroke | 101/669 | — | 52/225 | — | — | — | — | — | ||
| Case‐control | Myocardial infarction | 125/397 | — | 8/41 | — | — | — | — | — | — | |
| Cohort | Both | * | * | * | — | * | * | * | * | * | |
| Case‐control | Myocardial infarction | 591/ 3301 | 11/79 | 4/46 | — | — | — | — | — | — | |
| Case‐control | Ischemic stroke | 156/ 921 | 10/64 | — | — | — | — | 4/24 | — | — | |
| Case‐control | Myocardial infarction | 255/ 1159 | 8/60 | — | — | — | — | 3/27 | — | — | |
| Abbreviations: n: number. * Adjusted effect estimates extracted | |||||||||||
| Study | Crude OR (95% CI) | Adjusted OR (95% CI) | Adjustment variables per study |
| 1.8 (1.3 to 2.5) | 2.8 (1.8 to 4.5) | Age, hypertension, body mass index, lipid levels, diabetes, smoking, alcohol, family history of stroke, duration of COC use, study centre | |
| 2.1 (0.7 to 7.1) | 1.8 (0.3 to 11.5) | Age, geographic area, marital status, education, social class, smoking, alcohol and coffee consumption, parity, age at menopause, diabetes, hypertension, obesity, hyperlipidemia, family history of ischemic heart disease | |
| 2.3 (1.5 to 3.8) | 2.3 (1.4 to 3.8) | Age, educational level, hypertension, hypercholesterolemia, obesity, smoking | |
| 1.6 (0.9 to 2.9) | 2.3 (1.2 to 4.6) | Heart disease, diabetes, hypertension, previous venous thrombosis, migraine, alcohol, smoking | |
| 2.9 (1.0 to 8.7) | 2.9 (0.9 to 9.6) | Social class, smoking status, history of hypertension | |
| 1.0 (0.5 to 1.9) | 1.2 (0.5 to 2.6) | Hypertension, diabetes, smoking, race, body mass index | |
| Abbreviations: OR: odds ratio; COC: combined oral contraception. | |||

