Intervenciones farmacológicas para el dolor abdominal recurrente en niños
Información
- DOI:
- https://doi.org/10.1002/14651858.CD010973.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 06 marzo 2017see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Problemas de desarrollo, psicosociales y de aprendizaje
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
-
Review design: AEM, SL
-
Review co‐ordination: AEM
-
Data collection:
-
Search strategy design: AEM, AB
-
Searches undertaken: AEM, AB
-
Search results screened: AEM, TVND, RAA, AB, JTC, RW
-
Retrieval of papers: AEM, AB
-
Paper screening and appraisal, and extraction of data: AEM, TVND, RAA, AB, JTC, RW
-
Writing to authors for additional information: AEM, AB, RAA, TVND
-
Entering the data into Review Manager 5: AEM, TVND, RAA, AB, JTC
-
-
Analysis of the data: AEM, TVND, RAA, AB, JTC, SL
-
Interpretation of the data:
-
Methodological perspective: AEM, TVND, RAA, AB, JTC
-
Clinical perspective: AEM, TVND, SL
-
Sources of support
Internal sources
-
National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care South West Peninsula (PenCLAHRC), UK.
Funds the work of the evidence synthesis team.
External sources
-
None, Other.
Declarations of interest
The work of the evidence synthesis team is funded by the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care South West Peninsula (PenCLAHRC). The Funder has had no role in the review itself.
Alice E Martin: none known.
Tamsin V Newlove‐Delgado: none known.
Rebecca A Abbott: none known.
Alison Bethel: none known.
Joanna Thompson‐Coon: none known.
Rebecca Whear: none known
Stuart Logan: none known.
The authors who practice clinical paediatrics are Alice E Martin and Stuart Logan. Alice is a Paediatric Trainee and works under the guidance of various consultant paediatricians. Stuart is a Consultant Paediatrician and treats children according to current best evidence, in light of their preference. There are therefore no conflicts of interest with this review.
Acknowledgements
We acknowledge the work of the original review authors: Angela Huertas‐Ceballos, Stuart Logan, Cathy Bennett, Sarah See, Colin Macarthur, and Morris Zwi. We would also like to acknowledge the work of the Cochrane Developmental, Psychosocial and Learning Problems Review Group, the editors, statistician, and peer reviewers who commented on early drafts of this review.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Mar 06 | Pharmacological interventions for recurrent abdominal pain in childhood | Review | Alice E Martin, Tamsin V Newlove‐Delgado, Rebecca A Abbott, Alison Bethel, Joanna Thompson‐Coon, Rebecca Whear, Stuart Logan | |
| 2014 Feb 14 | Pharmacological interventions for recurrent abdominal pain in childhood | Protocol | Alice E Martin, Tamsin V Newlove‐Delgado, Rebecca A Abbott, Alison Bethel, Joanna Thompson‐Coon, Vasilis Nikolaou, Stuart Logan | |
Differences between protocol and review
The differences between the protocol and the review are detailed in the Additional Methods Table in Appendix 2.
Rebecca Whear joined the team following the publication of the protocol.
Notes
This is a new review, which supersedes a previously published review (Huertas‐Ceballos 2008a).
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Adolescent; Child; Child, Preschool; Humans;
PICO
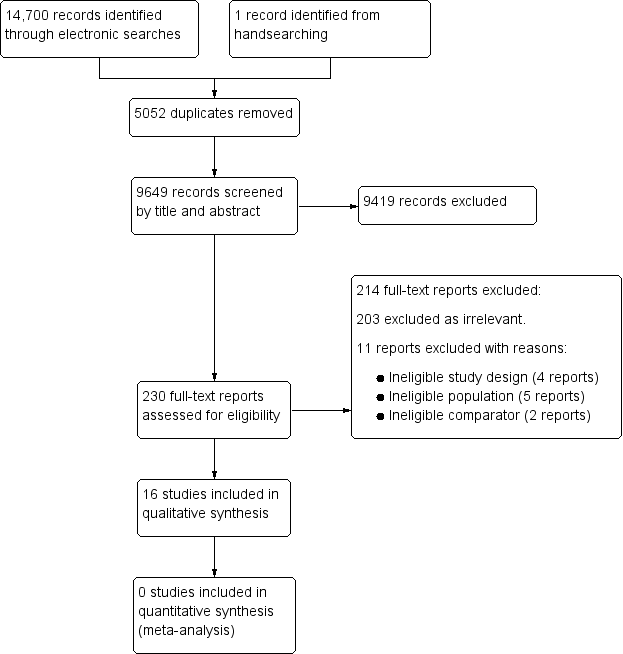
Study flow diagram.
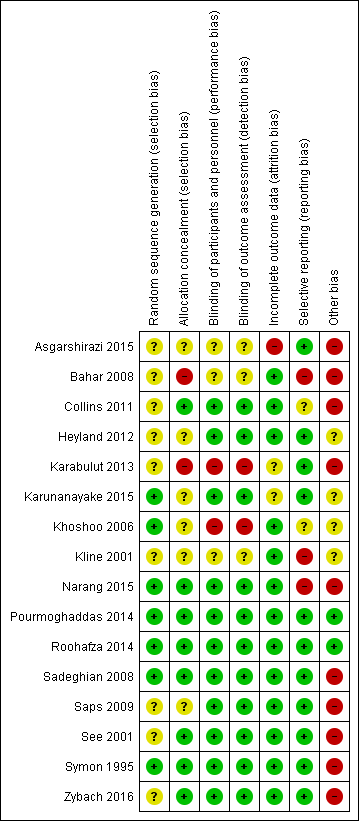
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
| Antispasmodics compared to placebo for recurrent abdominal pain | ||||||
| Patient or population: school‐aged children (5 to 18 years of age) with recurrent abdominal pain Settings: hospital paediatric outpatient clinics Intervention: antispasmodic drugs Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (SD) | Relative effect (95% CI) | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Intervention | |||||
| Pain duration (mean pain duration, assessed at 4 weeks) | The mean duration of pain in the control group was 6.17 (± 11.61). | The mean duration of pain in the intervention group was51.6 (± 23.74). | MD ‐25.4 (‐35.5 to ‐15.3) | 120 (1) | ⊕⊝⊝⊝ | No evidence of efficacy |
| Pain improvement (clinician judged, assessed at 2 weeks) | 9 of 21 children in the control group had an improvement in pain. | 15 of 21 children in the intervention group had an improvement in pain. | OR 3.33 (0.93 to 12.01) | 42 (1) | ⊕⊝⊝⊝ | No evidence of efficacy |
| Pain frequency (episodes of pain in 4 weeks, assessed after 4 weeks) | The mean number of episodes of pain in the control group was 21.6 (32.4). | The mean number of episodes of pain in the intervention group was10.3 (14). | MD 11.3 (2.4 to 20.1) | 132 (1) | ⊕⊝⊝⊝ | No evidence of efficacy |
| Pain improvement (self reported response to treatment, assessed at 4 weeks) | The response to treatment in the control group was 30.3%. | The response to treatment in the intervention group was 40.6%. | OR 1.6 (0.7 to 3.4) | 115 (1) | ⊕⊕⊝⊝ | No evidence of efficacy |
| *The basis for the assumed risk (e.g., the median control group risk across studies) is provided in footnotes. The corresponding risk is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded for low methodological quality due to single, small study; risk of bias from incomplete outcome data and differential loss of participants between groups. The placebo differed in preparation and dose timing compared to the intervention drug. | ||||||
| Domain | 'Risk of bias' judgement | ||
| Low | High | Unclear | |
| Selection bias | |||
| Random sequence generation | If the study details any of the following methods: (1) simple randomisation (such as coin‐tossing, throwing dice, or dealing previously shuffled cards, a list of random numbers, or computer‐generated random numbers); or (2) restricted randomisation such as blocked, ideally with varying block sizes or stratified groups, provided that within‐group randomisation is not affected | If the study details no randomisation or an inadequate method such as alternation, assignment based on date of birth, case record number, and date of presentation. These latter methods may be referred to as ‘quasi‐random’. | If there is insufficient detail to judge the risk of bias
|
| Allocation concealment | If the study details concealed allocation sequence in sufficient detail to determine that allocations could not have been foreseen in advance of, or during, enrolment | If the study details a method where the allocation is known prior to assignment | If there is insufficient detail to judge the risk of bias |
| Performance bias | |||
| Blinding of participants and personnel | If the study details a method of blinding participants and personnel. Detail would need to be sufficient to show that participants and personnel were unable to identify the therapeutic intervention from the control intervention. | If the methods detail that the participants or study personnel were not blinded to the study medication or placebo | If there is insufficient detail to judge the risk of bias |
| Detection bias | |||
| Blinding of outcome assessment | If the study details a blinded outcome assessment. This may only be possible for outcomes that are externally assessed. | If the outcome assessment is not blinded. We expect this may be unavoidable for self rated outcomes of unblinded interventions. | If there is insufficient detail to judge the risk of bias
|
| Attrition bias | |||
| Incomplete outcome data | If the study reports attrition and exclusions, including the numbers in each intervention group (compared with total randomised participants), reasons for attrition or exclusions, and any re‐inclusions; the impact of missing data is not believed to have altered the conclusions; and reasons for the missing data are acceptable | We may judge the risk of attrition bias to be high due to the amount, nature, or handling (such as per‐protocol analysis) of incomplete outcome data. | If there is insufficient detail to judge the risk of bias, e.g. if the number of children randomised to each treatment is not reported |
| Reporting bias | |||
| Selective reporting | If there is complete reporting of all outcome data. This will be determined based on comparison of the protocol and published study, if available. | If the reporting is selective so that some outcome data are not reported | If there is insufficient detail to judge the risk of bias, e.g. protocols are unavailable |
| Other sources of bias | |||
| Other bias | If the study is judged to be at low of risk of other potential sources of bias, such as no differential loss to follow‐up or an adequate washout period in cross‐over trials | If there are other sources of bias, such as differential loss to follow‐up or an inadequate washout period in cross‐over trials | If there is insufficient detail to judge the risk of bias |

