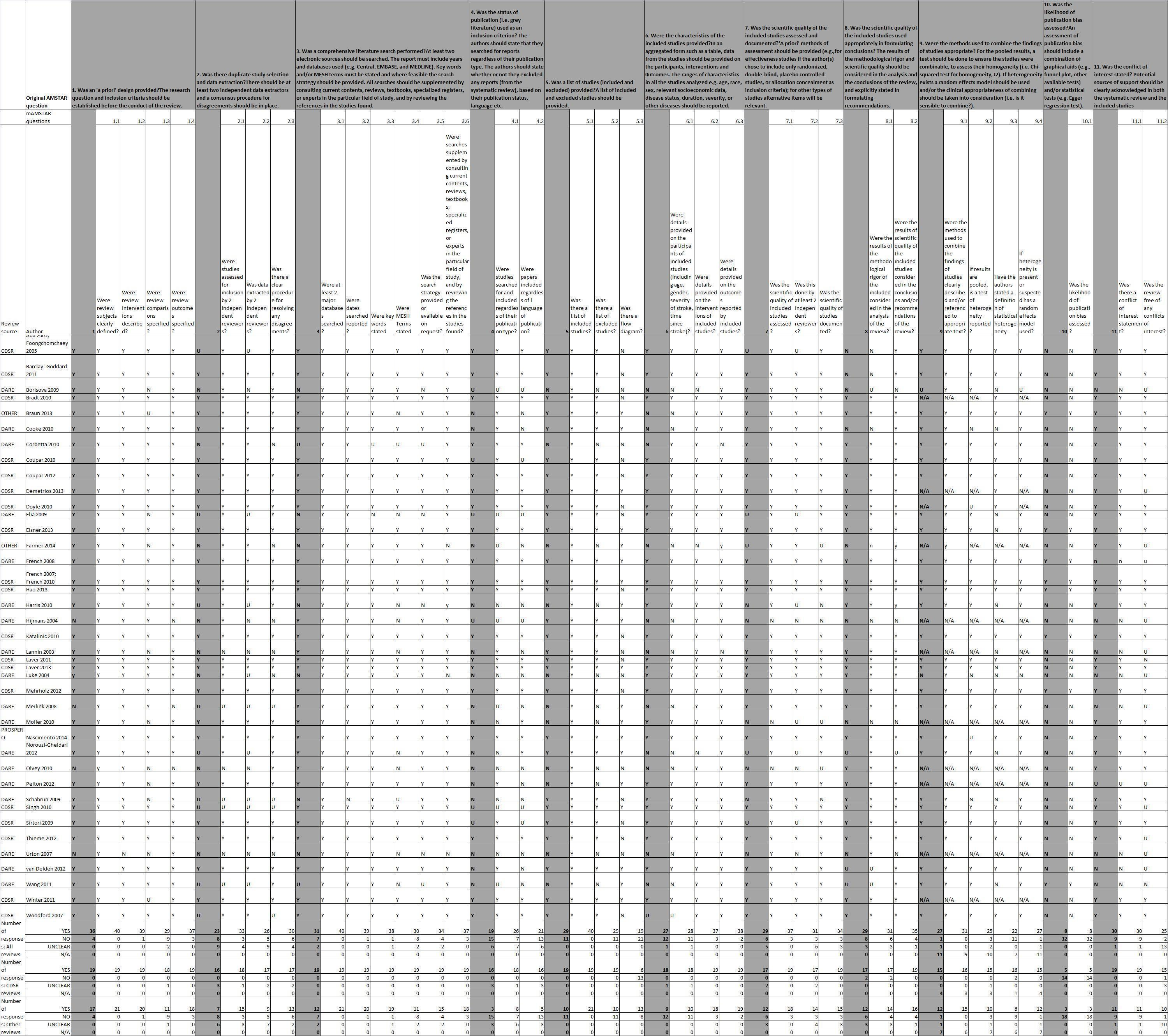
| Review (source) | Intervention | Date of search | Objective (as stated within review) | Types of studies included | Participants included | Interventions included | Comparisons included | Outcomes (as defined within review) | Number of studies included (number of participants included) |
| Ada 2005 (CDSR); Foongchomchaey 2005 (DARE) | Stretch or positioning | 22/03/2004 | To investigate the effects of supportive devices in preventing subluxation, repositioning the head of the humerus in the glenoid fossa,
decreasing pain, increasing function and adversely increasing contracture in the shoulder after stroke | RCTs, quasi‐randomised and controlled trials | Stroke | Supportive devices | Alternative supportive device or no support | Distance of subluxation (from x‐ray), pain, function, contracture | 4 (142) |
| Barclay‐Goddard 2011 (CDSR) | Mental practice | 24/11/2010 | To determine whether mental practice improves the outcomes of upper extremity rehabilitation for individuals living with the effects of stroke | RCTs | Stroke, UL functional deficits | Mental practice of upper extremity
movements or tasks alone or in combination with other therapies | No intervention; conventional intervention; placebo mental practice; or other novel therapies | Upper
extremity function: Arm and hand—e.g. Box and Block Test, Test Evaluant des Membres Supérieurs des Personnes Agées
(TEMPA), Action Research Arm Test, Motor Assessment Scale, upper extremity component, Frenchay Arm Test,
Wolf Motor Function Test, components of the Barthel Index or
the Functional Independence Measure. Hand function—Jebsen Test of Hand Function, Motor Assessment Scale Hand | 6 (119) |
| Borisova 2009 (DARE) | Stretch or positioning | 30/06/2005 | To assess the effectiveness of positioning on range of motion of the paretic shoulder following stroke | RCTs | Stroke | Positioning | Control | Range of motion | 5 (126) |
| Bradt 2010 (CDSR) | Music therapy | 25/02/2010 | To examine the effects of music therapy with standard care versus standard care alone or standard care combined with other therapies
on gait, upper extremity function, communication, mood and emotions, social skills, pain, behavioural outcomes, activities of daily
living and adverse events | RCTs, quasi‐RCTs | Acquired brain injury | Music therapy | Standard care or standard care with other therapies | Upper extremity function:measured by
hand grasp strength, frequency and duration of identified hand
function, spatiotemporal arm control Secondary outcomes:
Communication, mood and emotions, social skills and interactions, pain, behavioural outcomes, activities of daily living Adverse events (e.g. death, fatigue, falls) | 7 (184) |
| Braun 2013 (DARE) | Mental practice | 01/06/2012 | To investigate the beneficial and adverse effects of a mental practice intervention on activities, cognition and emotion in patients after stroke, patients with Parkinson’s disease or multiple sclerosis | RCTs | Stroke, Parkinson's or multiple sclerosis (but no studies with participants with multiple sclerosis found) | Mental practice as therapy or embedded in therapy | Control that allows assessment of the possible effects of mental practice | Measures of function, activity and participation | Stroke—14 (421) Parkinson's—2(60) |
| Cooke 2010 (DARE) | Exercise therapy | 01/10/2009 | To determine the strength of current evidence for provision of a
higher dose of the same types of exercise‐based therapy to enhance motor recovery after stroke | RCTs or quasi‐RCTs | Stroke | Experimental and control group interventions identical
except for dose described by duration and effort. Therapy dose could be described in terms
of time spent in therapy and/or of effort expended | See previous column—exercises but without increased duration | Motor impairment:
Motricity Index, muscle tone, joint range of
motion; co‐ordination, reaction time Motor activity:Modified
Rivermead Mobility Index, Action Research Arm Test,
Functional Ambulation Categories, Nine‐Hole Peg Test | 7 (680) |
| Corbetta 2010 (DARE) | CIMT (constraint‐ induced movement therapy) | 01/04/2010 | This article aims to present an update of the Cochrane review and to assess the effects of CIMT, modified CIMT and forced use on disability and arm motor function | RCTs and quasi‐RCTs | Stroke | CIMT, modified CIMT or forced use | Usual care | Disability:Functional Independence measure, Barthel Index Arm motor function:Action Research Arm Test, Wolf Motor Function Test, Emory Function Test, Motor Assessment Scale | 18 (674) |
| Coupar 2010 (CDSR) | Bilateral arm training | 28/08/2009 | To determine the effects of simultaneous bilateral training for improving arm function after stroke | RCTs | Stroke | Simultaneous bilateral training | Control, usual care | Performance in ADLs: functional movement of the upper limb;
Performance in extended activities of daily living: motor impairment of the arm | 18 (549) |
| Coupar 2012 (CDSR) | Service delivery | 21/05/2011 | To determine the effects of home‐based therapy programmes for upper limb recovery in patients with upper limb impairment following
stroke | RCTs | Stroke | Home‐based therapy for UL rehabilitation | Placebo, no intervention or usual care | ADLs and functional movement, extended ADLs, motor impairment | 4 (166) |
| Demetrios 2013 (CDSR) | Pharmacological | 01/09/2012 | To assess the effectiveness of multi‐disciplinary rehabilitation, following botulinum neurotoxin and other focal intramuscular treatments such as phenol, in improving
activity limitations and other outcomes in adults and children with poststroke spasticity. To explore what settings, types and intensities
of rehabilitation programmes are effective | RCTs | Adults and children with poststroke spasticity (clinical diagnosis) | Multi‐disciplinary rehabilitation after botulinum neurotoxin or other focal intramuscular treatments | Multi‐disciplinary rehabilitation | Passive function: Leeds Arm Spasticity Impact Scale, Disability Assessment Scale,
Arm Activity Measure Active function of the upper limb: e.g. Motor Activity Log (MAL) or Action Research Arm Test Active function of the lower limb: e.g. tests of walking speed, balance and gait
pattern Impairments—pain, spasm frequency, joint range
of movement, involuntary movements, measures of spasticity (Modified Ashworth Scale,
Tardieu Scale) Participation and impact on caregivers: WHO QoL‐BREF, Caregiver Strain
Index Adverse events | 3 (91) |
| Doyle 2010 (CDSR) | Sensory intervention | 16/09/2009 | To determine the effects of interventions that target upper limb sensory impairment after stroke | RCTs and controlled clinical trials | Stroke | For sensory impairment | No treatment,
conventional treatment, attention with placebo or with other interventions for sensory impairment | Functional use of the upper limb:
including Jebsen
Taylor Hand Function Test, Fugl‐Meyer, Modified Motor Assessment Scale,
Chedoke‐McMaster Motor Activity Log Scales (identifying perceived level of
use and satisfaction with level and quality of upper limb use) Activity limitations:
Barthel Index; Functional Independence Measure; Frenchay Activites Index; global dependency scales Participation: Stroke Impact Scale,
quality of life measures | 13 (467) |
| Elia 2009 (DARE) | Botulinum toxin injection by any route, including but not limited
to intramuscular, subcutaneous, intradermal and intra‐articular
routes | 01/09/2006 | The aim of this systematic review was to determine
whether botulinum neurotoxin reduces spasticity
or improves function in adult patients after stroke | All levels of evidence | Stroke | Intramuscular injections, botulinum neurotoxin A or botulinum neurotoxin B | | Ashworth Scale, Improvement of Global Assessment Scale (area under the curve of Ashworth scores), functional
disability, pain and quality of life measured by
validated scales; occurrence of serious adverse events | 11 (782) |
| Elsner 2013 (CDSR) | Transcranial direct current stimulation (tDCS) | May 2013 | To assess the effects of tDCS on generic activities of daily living and motor function in people with stroke | RCTs, first period of randomised cross‐over trials | Stroke | Active tDCS | Placebo, sham tDCS, no intervention or conventional rehabilitation | Primary outcome: Activities of daily living—Frenchay Activities Index, Barthel Index, Rivermead Activities of Daily Living Assessment, Modified Rankin Scale and Functional Independence Measure Secondary outcomes: Upper limb function—Action Research Arm Test, Fugl‐Meyer Score, Nine‐Hole Peg Test or Jebsen Taylor Hand Function Test. Muscle strength—grip force or motricity index Lower limb function | 15 (455) |
| Farmer 2014 (personal communication) | Assistive technologies, including electrical stimulation | 01/09/2011 | To identify and explore evidence for use of assistive technologies in poststroke upper limb rehabilitation | RCTs | Stroke | Assistive technologies including electrical stimulation (An assistive technology was defined as "a mechanical
or electrical device used in a functional task orientated training process which will have a systematic or rehabilitative effect on a person" and stated to include biofeedback, brain stimulation, constraint‐induced movement, neuromuscular electrical stimulation (NMES), robotics and virtual reality.) | Placebo, alternative treatments, usual care | Impairment: Range of motion, grip strength, subjective assessment of strength, Fugl‐Meyer Activity: Action Research Arm Test and Wolf Motor Function Test Partcipation: Motor Activity Log Amount of Use; Motor Activity Log Quality of Movement; Functional Independence Measure; Barthel index; Rankin Score and Stroke Impact Scale | 11 (474) |
| French 2007 (CDSR); French 2010 (DARE) | Repetitive task training | 16/10/2006 | To determine whether repetitive task training after stroke improves global, upper or lower limb function, and whether treatment effects are dependent on the amount, type or timing of practice | RCTs, controlled clinical trials | Stroke | Repetitive tasks training; an active motor sequence (multi‐joint motion) performed repetitively | Attention control, recreation, cognitive therapy, upper limb versus lower limb | Arm function: Motor Assessment Scale—Upper Limb Component, Action Research Arm Test, Frenchay Arm Test, Wolf Motor Function Test, Functional Test of the Hemiparetic Upper Extremity, Box and Block Test, Southern Motor Group Assessment Hand function: Motor Assessment Scale Hand; Jebsen Test of Hand Function, Peg Test Sitting balance/reach: Reaching Performance Scale, Functional Reach.
Lower limb function: walking distance, walking speed, functional ambulation, Timed Up and Go Test/Sit to Stand; Rivermead Motor Assessment, Sodring Motor Evaluation Scale Standing Balance/Reach: Berg Balance Scale, Sitting Equilibrium Index, Standing Equilibrium Index, Functional Reach
Global motor function: Motor Assessment Scale, Rivermead Motor Assessment Scale, Sodring Motor Evaluation Scale
Activities of daily living measures: Barthel Index, Functional Independence Measure, Modified Rankin Scale, Global Dependency Scale
Measures of task performance or impairment:
Motricity Index, Fugl‐Meyer Assessment, Sodring Motor Evaluation Scale Leg and Arm Subscales, Trunk Control Test
Measures of quality of life, health status, user satisfaction, carer burden, motivation or perceived improvement:e.g.
Nottingham Health Profile, SF‐36, Dartmouth Cooperative Chart
Adverse outcomes | 14 (659) |
| French 2008 (DARE) | Repetitive task training | 01/09/2006 | To determine whether repetitive
functional task practice (RFTP) after stroke improves
limb‐specific or global function or activities of daily
living, and whether treatment effects are dependent on
the amount of practice, or the type or timing of the
intervention. Also to provide estimates of the cost‐effectiveness
of RFTP | RCTs, quasi‐RCTs, cross‐over trials (first part) | Stroke | Repetitive task training | Usual practice or attention control, alternative training | Arm function: Action Research Arm Test; Motor Assessment Scale—Upper
Limb Component, Frenchay Arm Test, Wolf
Motor Function Test, Functional Test of the Hemiparetic Upper Extremity, Box and Block Test, Test Evaluant des
Membres Supérieurs des Personnes Agées, University of Maryland Arm
Questionnaire for Stroke, Motor Activity Log
Hand function: Motor Assessement Scale Hand; Jebsen Test of Hand
Function; Peg Test, Purdue Pegboard. Sitting Balance/Reach—Reaching Performance
Scale, Functional Reach | 31 (1078) |
| Hao 2013 (CDSR) | Repetitive transcranial magnetic stimulation (rTMS) | 23/04/2012 | To assess the efficacy and safety of rTMS for improving function in people with stroke | RCTs | Stroke (any age) | rTMS, rTMS added to standard treatment | Sham treatment, sham treatment added to baseline treatment, baseline treatment alone | ADLs: Barthel Index, Functional Independence Measure, Modified Rankin Motor function:Upper limb function—Motor Assessment Scale, Action Research Arm Test, Nine‐Hole Peg Test. Lower limb function—changes in stride length or speed, Timed Up and Go Test, Rivermead Motor Assessment Scale. Global motor function—Motor Assessment Scale, Rivermead Motor
Assessment Scale Death or disability Any other impairment improvement (e.g. visual, perceptual, depression, cognition, etc) | 19 (588) |
| Harris 2010 (DARE) | Exercise | 04/2009 | To examine the evidence
for strength training of the paretic upper limb in improving
strength, upper limb function and ADLs | RCTs | Stroke | Strength training (voluntary exercise against resistance) | No treatment, placebo, non‐strengthening intervention | Upper limb strength, upper limb function or ADLs | 13 (517) |
| Hijmans 2004 (DARE) | Stretch or positioning | 01/06/2003 | To assess the scientific base of elbow
orthoses | All designs considered | Elbow condition | Splinting | No comparisons prespecified | Range of motion, pain, grip strength | Stroke RCT—1 (18), Cohort—1 (16) |
| Katalinic 2010 (CDSR) | Stretch or positioning | 01/04/2009 | To determine the effects of stretch on contractures in people with, or at risk of, contractures | RCTs and controlled
clinical trials; parallel‐group designs, within‐subject
designs or cross‐over designs | • Neurological conditions (e.g. stroke, multiple sclerosis,
spinal cord injury, traumatic brain injury, Guillain‐Barré
syndrome, Parkinson’s disease)
• Advanced age (e.g. frailty);
• History of trauma or surgery (e.g. burns, joint replacement
surgery)
• Underlying joint or muscle pathology and disease processes
(e.g. inflammatory arthritis, osteoarthritis) | Stretch, stretch plus co‐intervention | No stretch, placebo or sham stretch, co‐intervention | Range of motion, torques, QoL, SF‐36, Tardieu, Modified Ashworth Scale, Functional Independence Measure, motor ability score | 35 (1391) |
| Lannin 2003 (DARE) | Stretch or positioning | 26/05/2003 | To assess the effectiveness of hand splinting on the hemiplegic
upper extremity following stroke | All designs considered | Stroke | Splinting | No comparisons prespecified | Functional use of hand, range of motion, tone, spasticity, oedema, pain | 21 (230) |
| Laver 2011 (CDSR) | Virtual reality | 30/03/2010 | To evaluate the effects of virtual reality and interactive video gaming on upper limb, lower limb and global motor function after stroke | RCTs | Stroke | Immersive or non‐immersive virtual reality | Alternative intervention, no Intervention | Upper limb function and activity:
Arm function and activity—Motor Assessment Scale (Upper Limb), Action Research
Arm Test, Wolf Motor Function Test;
Hand function and activity—Nine‐Hole Peg Test, Box and Block Test. Gait and balance function and activity:
Lower limb function and activity—walking distance, walking speed, Community
Walk Test, functional ambulation, Timed Up and Go Test;
Standing reach—Berg
Balance Scale and laboratory‐based force plate measures Global motor function: Motor Assessment Scale Secondary outcomes: Cognitive function—Trail Making Test, Useful Field of View Test; Activity limitation—
Functional Independence Measure (FIM), Barthel Index,
Activities‐Specific Balance; Confidence Scale, On‐Road Driving
Test;
Participation restriction and quality of life—SF‐36, EQ5D, Stroke Impact Scale or other patient‐reported outcomes;
Functional magnetic resonance
imaging (MRI) Adverse events: motion sickness, pain, injury, falls
and death | 19 (565) |
| Laver 2013 (CDSR) | Service delivery | 09/07/2013 | To evaluate the effects of telerehabilitation, in comparison with in‐person or no rehabilitation, on activities of daily living for people after
stroke. Secondary objectives included determining the effects of telerehabilitation on mobility, health‐related quality of life, upper
limb function, cognitive function or functional communication | RCTs | Stroke | Telerehabilitation | "In‐Person Rehabilitation" or no rehabilitation or alternative method of delivering telerehabilitation | Primary outcomes: Activities of daily living—Functional Independence Measure; Nottingham Extended Activities of Daily Living Secondary outcomes: Self‐care and domestic life;
mobility (e.g. Timed Up and Go Test, walking
speed, functional ambulation category); Patient satisfaction with the intervention—self‐reported health‐related quality of life; upper limb function (e.g. Action Research Arm Test, Wolf Motor Function Test, Fugl‐Meyer Upper Extremity
Measure); cognitive function (e.g. Mini
‐Mental State Examination, specific measures such as tests of
attention or executive functioning); Functional communication; Cost‐effectiveness. Adverse events | 10 (933) |
| Luke 2004 (DARE) | Exercise therapy | 2003 | To determine the effectiveness of the Bobath concept in reducing upper limb impairments, activity limitations and participation restrictions after stroke | RCTs, cross‐over and single case series | Stroke | Stated use of the Bobath concept
or neurodevelopmental therapy in isolation | A control for Bobath
intervention in the form of a group with no
intervention or a group with a comparison intervention,
or a baseline phase | Any outcome
measure reflecting change in upper limb impairment,
activity limitation or participation restriction | RCTs—5 (209) Cross‐over—1 (131) Single‐case study—2 (34) |
| Mehrholz 2012 (CDSR) | Robotics | 01/08/2011 | To assess the effectiveness of electromechanical and robot‐assisted arm training in improving generic activities of daily living, arm function and arm muscle strength in patients after stroke | RCTs | Stroke | Electromechanical and robot‐assisted arm training for recovery of arm function | Other rehabilitation or placebo interventions, or no treatment | ADLs (Barthel Index, Functional Independence Measure), Fugl‐Meyer, Motricity Index and other measures of arm function or strength | 19 (666) |
| Meilink 2008 (DARE) | Electrostimulation | 01/06/2006 | To assess whether EMG‐triggered neuromuscular electrical
stimulation (EMG‐NMES) applied to the extensor muscles of the forearm
improves hand function after stroke. | RCTs | Stroke | EMG‐NMES | Usual care | Reaction time, Fugl‐Meyer Assessment, Box and Block Test, peak velocity, deceleration time, Functional Independence Measure (self‐care), Action Research Arm Test, grip strength, Motricity Index, pinch and grip strength, elbow flexion/shoulder abduction, goniometry | 8 (157) |
| Molier 2010 (DARE) | Biofeedback | 01/03/2009 | To investigate the effects of different aspects and types of augmented feedback on motor functions and motor
activities of the hemiparetic arm after stroke | All levels of evidence | Stroke | Intervention augmented by biofeedback | Comparisons were not defined a priori but included practising movements without feedback or robotic guidance | Fugl‐Meyer, Composite Spasticity Index, Ashworth Scale, Test Evaluant des
Membres Supérieurs des Personnes Agée, Block and Box Test, Motor Power Score, Motor Status Score, Motor Assessment Scale, Jebsen Taylor Hand Test, ABILHAND, Purdue Pegboard Test, Chedoke McMaster, Wolf Motor Function Measure, Stroke Impact Scale, Functional Test of the Hemiparetic Upper Extremity | 23 (328): RCTs—8 (148) Cohort—10 (106) Matched pairs—2 (52) Not randomised—1 (16) Observational study—1 (5) Single case study—1 (1) |
| Nascimento 2014 (PROSPERO) | Electrical stimulation | December 2012 | To determine whether electrical stimulation is effective in increasing strength after stroke, and whether any benefits are maintained beyond the intervention period or carried over to activity | RCTs and controlled trials | Stroke | Cyclical electrical stimulation for strengthening | 1. No treatment, placebo, non‐strengthening interventions 2. Other strengthening interventions 3. Different modes of electrical stimulation | Strength: peak force generation Activity: Block and Box Test, Action Research Arm Test General activity: Barthel Index | 16 (638) |
| Norouzi‐Gheidari 2012 (DARE) | Robotics | 01/07/2010 | To find evidence regarding the effectiveness
of robot therapy compared with conventional therapy in improving motor
recovery and functional abilities of the paretic upper limb of
patients with stroke | RCTs | Stroke | Robot therapy | Conventional therapy | Fugl‐Meyer, Functional Independence Measure, Motor Power Scale, Motor Status Scale | 12 (383) |
| Olvey 2010 (DARE) | Pharmacological | 01/07/2010 | To review
studies focusing on contemporary pharmacological therapies
for upper limb spasticity after stroke | RCTs, open‐labelled non‐randomised or observational studies | Stroke | Pharmacological treatments for spasticity | Dose comparisons or placebo with or without other treatment | Spasticity (Ashworth Scale or Modified Ashworth Scale or Tardieu Scale), pain, Fugl‐Meyer Assessment, Functional Independence Measure, Barthel Index, Disability Assessment Scale, range of motion, health‐related quality of life | RCTs—23 (1039) Other—31 (1288) |
| Pelton 2012 (DARE) | Exercise | 04/2010 | To identify all existing interventions targeted at co‐ordination of arm and hand segments for reach‐to‐grasp
following stroke. To determine the effectiveness of current treatments for improving co‐ordination of reach‐to‐grasp
after stroke | All types of study design | Stroke | Treatment to develop co‐ordination of hand and arm during reach‐to‐grasp | | Specific measures of co‐ordination such
as movement velocity, acceleration, deceleration and movement
duration, maximum hand aperture and reaction time; Fugl‐Meyer Assessment | 8 (155) |
| Schabrun 2009 (DARE) | Sensory training | Not reported | We examined the volume and quality of the evidence available for
both passive and active sensory training following stroke | All types of study design | Stroke | Sensory retraining | | Jebsen Taylor Hand Function, Action Research Arm Test, Modified Ashworth Assessment Scale, Modified Motor Assessment Scale | 14 (296) |
| Singh 2010 (CDSR) | Pharmacological | 22/01/2010 | To assess the benefits and safety of botulinum toxin compared with placebo or alternative treatments in adults with shoulder pain | RCTs | Shoulder pain | Botulinum toxin injection by any route, including but not limited
to intramuscular, subcutaneous, intradermal and intra‐articular
routes | Placebo injection or another active treatment | Pain: measured on a visual analogue scale, numerical
rating scale or semi‐quantitative descriptive scale Adverse effects Function or disability: measured using validated shoulder‐specific
instruments (e.g. Constant Score, University of
California and Los Angeles Shoulder Scale (UCLA) or American
Shoulder and Elbow Surgeons Shoulder Score, Western Ontario Osteoarthritis of the Shoulder) General
disability measures: e.g. Health Assessment Questionnaire
Joint range of motion Quality of life: e.g.
Short‐Form 36 (SF‐36) | 6 (164) |
| Sirtori 2009 (CDSR) | Constraint‐induced movement therapy (CIMT) | 01/06/2008 | To assess the efficacy of CIMT, modified CIMT (mCIMT) or forced use (FU) for arm management in hemiparetic patients | RCTs and quasi‐RCTs | Stroke | CIMT, mCIMT or forced use | Other rehabilitation techniques or none | Arm motor function: perceived arm motor function, arm impairment, dexterity, quality of life | 19 (619) |
| Thieme 2012 (CDSR) | Sensory intervention | 08/06/2011 | To summarise the effectiveness of mirror therapy for improving motor function, activities of daily living, pain and visuospatial neglect in patients after stroke | RCTs and randomised cross‐over trials | Stroke | Mirror therapy | Any control intervention | Upper limb and hand function: Fugl‐Meyer, Action Reseach Arm Test, Wolf Motor Function Test, Brunnstrom Stages of Upper Extremity, Motricity Index Lower limb function: Functional Independence Measure, Barthel Index | 14 (567) |
| Urton 2007 (DARE) | Mixed | 06/2005 | To critically analyse the literature on effective interventions for upper extremity
hemiparesis following stroke | RCTs and CCTs | Stroke | For upper limb hemiparesis | | Fugl‐Meyer Assessment, Box and Block Test, Purdue Pegboard Test, Action Research Arm Test, Functional Independence Measure, TEMPA, Wolf Motor Function Test, grip strength, Caregiver Strain Index, Geriatric Depression Score, Ashworth Scale, Motor Activity Log and other study‐specific measures | 11 (269) |
| van Delden 2012 (DARE) | Bilateral arm training | 01/06/2011 | To compare the effects of unilateral and bilateral
training on upper limb function after stroke with regard to 2 key factors: severity of upper limb paresis and time of intervention post stroke | RCTs | Stroke up to 1 month = acute, 1‐6 months = subacute, after 6 months = chronic | Unilateral arm training; bilateral arm training | Alternative treatment | Wolf Motor Function Measure, Canadian Occupational Performance Measure, Fugl‐Meyer Assessment, Functional Independence Measure, Motor Activity Log, Stroke Impact Scale, Action Research Arm Test, Rivermead Motor Assessment, Nine‐Hole Peg Test, Modified Barthel Index, Nottingham Health Profile, Hospital Anxiety and Depression Scale, Motor Status Scale, Motor Assessment Scale, dynamometry, Rehabilitation Activities Profile, fMRI, additional kinematics | 9 (452) |
| Wang 2011 (DARE) | Mental practice | 10/2010 | To evaluate mental imagery on rehabilitation of functions in patients with stroke | RCTs | Stroke | Mental practice or mental imagery. Other clinical and rehabilitative treatments were the same as control group | Conventional stroke rehabilitation methods (such as physiotherapy and occupational therapy) | Upper limb function: Upper Limb Section of Fugl‐Meyer Assessment of Motor Recovery, Action Research Arm Test Other outcomes: Motor Assessment Scale, Modified Ashworth Scale, Upper Extremity Function Test, Functional independence Measure, Motor Activity Log, Color Trails Test, Task Performance Test, Motricity Index, The Arm Functional Test, simple test for evaluating hand function, Modified Barthel Index | 16 (652) (191 total participants for English papers, 461 total participants for Chinese papers) |
| Winter 2011 (CDSR) | Stretch or positioning | 22/03/2010 | To identify whether specific hands‐on therapeutic interventions enhance motor activity and function of the upper limb post stroke | RCTs | Stroke | Manual therapy techniques | Unclear | UL function: Action Research Arm Test, Motricity Index, Functional Independence Measure, Barthel Index | 3 (86) |
| Woodford 2007 (CDSR) | Biofeedback | 29/03/2006 | To assess the effects of EMG‐BFB for motor function recovery following stroke | RCTs and quasi‐RCTs | Stroke | EMG biofeedback with standard physiotherapy | Standard physiotherapy or standard physiotherapy and sham feedback | Range of motion, improvement in gait (stride length, speed, need for ambulation aids),
functional ability, electromyographic activity, muscle weakness | 13 (269) |