نقش درمان فارماکولوژیک عوامل خطرساز عروقی برای کاهش مرگومیر و حوادث قلبیعروقی در بیماران مبتلا به آنوریسم آئورت شکمی
چکیده
پیشینه
پروفیلاکسی دارویی ثابت شده خطر حوادث قلبیعروقی را در افراد مبتلا به بیماری انسدادی شریانی آترواسکلروتیک (atherosclerotic occlusive arterial disease) به خطر میاندازد. با این حال، نقش پروفیلاکسی در افراد مبتلا به آنوریسم آئورت شکمی (abdominal aortic aneurysm; AAA) هنوز معلوم نیست. مطالعات متعدد نشان دادهاند که با وجود ترمیم موفقیتآمیز، افرادی که دارای AAA هستند نرخ بقای کمتری نسبت به کنترلهای سالم دارند. افراد مبتلا به AAA با شیوع بیشتر بیماری کرونری قلبی و خطر حوادث قلبیعروقی روبهرو هستند. علیرغم این ارتباط، در مورد اثربخشی پروفیلاکسی دارویی در کاهش خطر قلبیعروقی در افراد مبتلا به AAA اطلاعات کمی در دست است. این نسخه بهروز از یک مرور کاکرین است که در سال 2014 منتشر شد.
اهداف
تعیین اثربخشی طولانیمدت داروهای آنتیپلاکت، آتیهیپرتانسیو یا کاهنده چربی بر کاهش مرگومیر و حوادث قلبیعروقی در افراد مبتلا به آنوریسم آئورت شکمی.
روشهای جستوجو
برای بهروزکردن این مرور، متخصص اطلاعات عروق در کاکرین (CIS)؛ پایگاه ثبت تخصصی عروق در کاکرین (14 اپریل 2016) را جستوجو کرد. علاوه بر این، CIS پایگاه ثبت مرکزی کارآزماییهای کنترل شده کاکرین (CENTRAL) (شماره 3، 2016) و پایگاههای ثبت کارآزماییها (14 اپریل 2016) را جستوجو کرد، فهرست منابع مقالات مرتبط را نیز بررسی کردیم.
معیارهای انتخاب
کارآزماییهای تصادفیسازی و کنترل شده که در آنها افراد مبتلا به AAA بهطور تصادفی به یکی از درمانهای پروفیلاکتیک در برابر دیگری، یک رژیم متفاوت از همان دمران، یک دارونما (placebo)، یا عدم درمان اختصاص یافتند، واجد شرایط برای ورود به این مرور بودند. پیامدهای اولیه شامل مورتالیتی به هر علتی و مرگومیر قلبیعروقی بود.
گردآوری و تجزیهوتحلیل دادهها
دو نویسنده مرور بهطور مستقل از هم مطالعات را برای ورود انتخاب و ارزیابی کیفیت و استخراج دادهها را کامل کردند. هرگونه اختلافنظری را با مباحثه حل کردیم. فقط یک مطالعه دارای معیارهای ورود به این مرور بود، بنابراین نتوانستیم متاآنالیز انجام دهیم.
نتایج اصلی
هیچ مطالعه جدیدی معیارهای ورود به نسخه بهروز این مرور را نداشت. یک کارآزماییهای تصادفیسازی و کنترل شده در این مرور پیدا کردیم. زیر‐گروهی از شرکتکنندگان مبتلا به AAA متوپرولول (metoprolol) (N = 111) یا دارونما (N = 116) دریافت کردند. هیچ شواهد روشنی وجود نداشت که نشان دهد متوپرولول میتواند مورتالیتی به هر علتی (نسبت شانس (OR): 0.17؛ 95% فاصله اطمینان (CI): 0.02 تا 1.41)، مرگومیر قلبیعروقی (OR: 0.20؛ 95% CI؛ 0.02 تا 1.76)، مرگومیر در اثر AAA (OR: 1.05؛ 95% CI؛ 0.06 تا 16.92) کاهش میدهد یا حوادث قلبیعروقی غیر‐کشنده (OR: 1.44؛ 95% CI؛ 0.58 تا 3.57) را در طول 30 روز پس از جراحی افزایش میدهد. علاوه بر این، طی شش ماه پس از جراحی، تاثیرات تخمینی با مزایا و آسیبها برای مورتالیتی به هر علتی (OR: 0.71؛ 95% CI؛ 0.26 تا 1.95)، مرگومیر قلبیعروقی (OR: 0.73؛ 95% CI؛ 0.23 تا 2.39) و حوادث قلبیعروقی غیر‐کشنده (OR: 1.41؛ 95% CI؛ 0.59 تا 3.35) هماهنگی داشت. عوارض جانبی دارویی برای کل جمعیت مطالعه گزارش شد و برای زیر‐گروهی از شرکتکنندگان مبتلا به AAA در دسترس نبود. این مطالعه را بهطور کلی در معرض خطر پائین سوگیری (bias) در نظر گرفتیم. کیفیت شواهد را برای همه پیامدها پائین در نظر گرفتیم. سطح کیفیت شواهد را به دلیل عدم دقت کاهش دادیم، زیرا فقط یک مطالعه با تعداد کمی از شرکتکنندگان در دسترس بود، تعداد حوادث اندک بودند و نتایج با مزایا و آسیبها همسو و سازگار بود.
نتیجهگیریهای نویسندگان
با توجه به محدود بودن تعداد کارآزماییهای وارد شده، شواهد کافی برای نتیجهگیری کردن در مورد اثربخشی پروفیلاکسی بیماری قلبیعروقی در کاهش مرگومیر و حوادث قلبیعروقی در افراد مبتلا به AAA وجود ندارد. کارآزماییهای تصادفیسازی و کنترل شده بیشتری که با کیفیت خوب انجام شوند و بسیاری از انواع پروفیلاکسی را با پیگیری طولانیمدت مورد بررسی قرار بدهند، پیش از اتخاذ نتیجهگیریهای درست، مورد نیاز است.
PICO
خلاصه به زبان ساده
درمان دارویی عوامل خطرساز عروقی برای کاهش مرگومیر و عوارض قلبیعروقی در افراد مبتلا به آنوریسم آئورت شکمی
پیشینه
آنوریسم آئورت شکمی (abdominal aortic aneurysm; AAA) یک وضعیت بالقوه تهدید کننده زندگی است که در آن آئورت بزرگ شده و در نهایت میتواند منجر به خونریزی گستردهای شود. دستورالعملهای فعلی توصیه میکنند که AAAهای 55 میلیمتر یا بیشتر باید به روش جراحی، ترمیم شوند، چون در این اندازه، خطر پارهشدگی بیش از خطر ترمیم جراحی است. AAAها بین اندازههای 30 تا 54 میلیمتر پر‐خطر نیستند و بهطور کلی توسط اسکنهای منظم برای بررسی بزرگتر شدن مورد بررسی قرار میگیرند. پژوهشهای اخیر نشان داده که حتی پس از ترمیم آنوریسم، نرخ بقا در افراد مبتلا به AAA بدتر از افراد بدون AAA است. در بیشتر موارد، علت مرگومیر یک رویداد قلبیعروقی، مانند حمله قلبی یا سکته مغزی است. شرایطی نظیر فشار خون بالا یا کلسترول بالا خطر مرگومیر قلبیعروقی را افزایش میدهند. با این حال، هر دو شرایط را میتوان از طریق درمان دارویی معکوس کرد. با توجه به افزایش خطر مرگومیر با AAA، تعیین اینکه کدام درمان دارویی در پیشگیری از مرگومیر قلبیعروقی در افراد مبتلا به AAA موثرتر بوده، مهم است.
در این مرور، محققانی از کاکرین، اثربخشی درمان دارویی را در درمان عوامل خطرساز عروقی و کاهش مرگومیرها و حوادث و مرگومیرهای قلبیعروقی در افراد مبتلا به AAA بررسی کردند.
ویژگیهای مطالعه و نتایج کلیدی
پس از جستوجو برای همه مطالعات مرتبط (تا 14 اپریل 2016)، یک مطالعه را پیدا کردیم که در آن یک زیر‐گروه از 227 فرد مبتلا به AAA، بتا‐بلاکر متوپرولول (beta‐blocker metoprolol) (داروهایی را که فشار خون را کاهش میدهند) یا یک دارونما (placebo) (درمان ساختگی) دریافت کردند. نتایج این مطالعه برای همه علل مرگومیر و مرگومیر ناشی از بیماریهای قلبیعروقی یا بیماریهای قلبیعروقی غیر‐کشنده در 30 روز یا شش ماه پس از ترمیم AAA غیر‐دقیق است. عوارض جانبی دارو برای کل جمعیت مطالعه گزارش شد و برای زیر‐گروهی از شرکتکنندگان مبتلا به AAA در دسترس نبود.
کیفیت شواهد
ما این مطالعه را بهطور کلی در معرض خطر پائین سوگیری (bias) قضاوت کردیم. کیفیت شواهد را پائین در نظر گرفتیم زیرا فقط یک مطالعه کوچک را در مرور وارد کردیم، رویدادهای کمی گزارش شده بود و نتیجه آن با مزیت و آسیب همسو و سازگار بود.
انجام مطالعات بزرگ و طولانیتر برای شناسایی بهترین درمان موثر است. در حال حاضر افراد مبتلا به AAA طیف گستردهای را از درمانهای فارماکولوژیک شامل داروهای آنتیپلاکت، داروهای آنتی‐هیپرتانسیو و داروهای کاهش دهنده چربی دریافت میکنند. کارآزماییهای آینده باید داروهای موجود را تست کنند تا بتوانند موثرترین استراتژی را پیدا کنند، چه با یک داروی واحد باشد یا ترکیبی از درمانها. علاوه بر این، مقبولیت چنین مداخلاتی باید مورد ارزیابی قرار گیرد و مطالعات آینده باید عوارض جانبی همراه با این داروها و تاثیر آنها را بر کیفیت زندگی اندازهگیری کنند.
Authors' conclusions
Summary of findings
| Metoprolol compared to placebo for reducing mortality and cardiovascular events in patients with abdominal aortic aneurysm (AAA) | ||||||
| Patient or population: patients of any age with AAA less than 30 mm in diameter | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with metoprolol | |||||
| All‐cause mortality, 30 days1 | Study population | OR 0.17 | 227 | ⊕⊕⊝⊝ | — | |
| 52 per 1000 | 9 per 1000 | |||||
| Cardiovascular death, 30 days3 | Study population | OR 0.20 | 227 | ⊕⊕⊝⊝ | — | |
| 43 per 1000 | 9 per 1000 | |||||
| AAA‐related death, 30 days4 | Study population | OR 1.05 | 227 | ⊕⊕⊝⊝ | — | |
| 9 per 1000 | 9 per 1000 | |||||
| Nonfatal cardiovascular event, 30 days5 | Study population | OR 1.44 | 227 | ⊕⊕⊝⊝ | — | |
| 78 per 1000 | 108 per 1000 | |||||
| All‐cause mortality, 6 months1 | Study population | OR 0.71 | 227 | ⊕⊕⊝⊝ | — | |
| 86 per 1000 | 63 per 1000 | |||||
| Cardiovascular death, 6 months3 | Study population | OR 0.73 | 227 | ⊕⊕⊝⊝ | — | |
| 60 per 1000 | 45 per 1000 | |||||
| AAA‐related death, 6 months4 | See comments | See comments | See comments | See comments | The incidence of AAA‐related death was not measured at six months. | |
| Nonfatal cardiovascular event, 6 months5 | Study population | OR 1.41 | 227 | ⊕⊕⊝⊝ | — | |
| 86 per 1000 | 117 per 1000 | |||||
| *The risk with placebo was the average risk in the placebo group (i.e. the number of participants with events divided by total number of participants of the placebo group included in the meta‐analysis). The risk in the metoprolol group (and its 95% CI) is based on the assumed risk in the placebo group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Death from all causes. | ||||||
Background
Description of the condition
An abdominal aortic aneurysm (AAA) is an abnormal dilatation of the aorta as it passes below the renal arteries to the point of bifurcation, where it forms the left and right common iliac arteries. The clinical definition of AAA varies, although a maximum infrarenal measurement (a measurement taken below the renal artery branches) of ≥ 30 mm is commonly used (Wanhainen 2008). The prevalence of AAA is six times greater in men than in women (Pleumeekers 1995), with one study demonstrating a prevalence of 1.3% in women and 7.6% in men (Scott 2002). Apart from male gender, other risk factors for AAA include smoking, increased age, and family history of AAA (Blanchard 2000). Conclusive evidence from several studies has shown smoking to be associated with AAA (Badger 2009; Greenhalgh 2008; Wilmink 1999). One study, Wilmink 1999, estimated that the risk of AAA is seven times higher in smokers and three times higher in ex‐smokers compared with age‐matched nonsmokers, and another study reported that 90% of participants with AAA were smokers (Greenhalgh 2008). Increased age has been consistently shown as a significant risk factor (Lloyd 2010; Singh 2001). One population‐based study of 6386 men and women reported no AAA in participants younger than 48 years of age, but from this age onward the prevalence increased linearly in both men and women (Singh 2001). Family history is another known risk factor for AAA. One study reported that 9% to 12% of first‐degree relatives of a participant with an AAA will develop an aneurysm (van Vlijmen‐van Keulen 2002).
The decision to operate on an AAA is made when the risk of rupture is greater than the risk associated with the operation, and burden of co‐morbidity is increasingly important (Ohrlander 2011). The UK Small Aneurysm Trial estimated that the annual rupture rate is 0.3% for AAAs that are less than 4 cm in diameter, 1.5% for 4.0 cm to 4.9 cm AAAs, and 6.5% for 5.0 cm to 5.9 cm AAAs (Brown 1999). In general, the American Heart Association and the UK Aneurysm Screening Programme recommend that patients with infrarenal AAAs measuring ≥ 55 mm should undergo repair to eliminate the risk of rupture (Hirsch 2005). AAAs can be repaired using an open or endovascular approach. Open repair with graft placement is a major procedure and may be preferred when patients are fit because complications are fewer and patients do not routinely require follow‐up. Endograft repair involving stent placement (EVAR) is associated with a lower postoperative risk and is therefore considered when the patient is a high surgical risk or has coexisting medical conditions. The major risks in repairing an AAA are perioperative cardiac events, infection, and death. The 30‐day mortality has been estimated at 5% in elective open surgical AAA repair compared with 1.7% with EVAR (Greenhalgh 2004; Prinssen 2004). However, a recent study showed no significant difference in survival at five years in participants who had undergone open repair compared with EVAR (Brown 2011). Patients with an infrarenal AAA of 30 mm to 54 mm are monitored by ultrasound or computed tomography (CT) scans every three, six, or 12 months for detection of possible expansion and the need for repair. These patients are considered for statin therapy to reduce vascular risk, decrease the risk of rupture and reduce aneurysm growth rates (Davis 2008). Angiotensin‐converting enzyme (ACE) inhibitors and angiotensin receptor blockers have also been proposed to reduce aneurysmal growth (Hackam 2006).
Studies have shown that even after successful surgical repair of an AAA, participants had a poorer survival rate than healthy controls (de Bruin 2014; De Martino 2013; Timmers 2013). A Dutch cohort study measured a survival rate of 59% 10 years after open AAA repair, and patients had a poorer health‐related quality of life than age‐matched controls (Timmers 2013). Another Dutch study compared statin use in patients undergoing AAA repair and found that while statins were associated with fewer cardiovascular deaths, several risk factors remained that were associated with poor survival after AAA repair including age of greater than 70 years, a history of cardiac disease, and moderate to severe tobacco use (de Bruin 2014). A further study of 2637 participants undergoing AAA repair determined that although five‐year survival rates were similar between open and EVAR repair groups, advanced age ≥ 75 years, coronary artery disease, unstable angina or recent myocardial infarction (MI), oxygen‐dependent chronic obstructive pulmonary disease, and an estimated glomerular filtration rate of less than 30 mL/min/1.73 m2 were associated with poor survival at five years (De Martino 2013).
A recent study conducted in Australia demonstrated an association between AAA thrombus volume and subsequent cardiovascular events (Parr 2011). AAA thrombus products are released into the circulation where they have the potential to stimulate leukocytes and produce other changes that might promote atherosclerotic plaque activation and acute coronary and cerebrovascular events (Morange 2006; Parry 2009; Smith 2005; Takagi 2009).
AAA size and growth are associated with local generation of inflammation markers such as interleukin‐6, matrix metalliproteinase‐2 (MMP‐2), and MMP‐9 (Schouten 2006). Inflammation also seems to be important in perioperative adverse cardiac events. Larger AAA size is independently associated with an increased incidence of perioperative cardiovascular complications after elective infrarenal AAA repair (Schouten 2006).
Description of the intervention
Pharmacological therapy to reduce cardiovascular risk factors such as hypertension and hypercholesterolaemia. Examples of pharmacological therapy are antiplatelet therapy (e.g. aspirin, clopidogrel, ticlopidine, cilostazol, or any other antiplatelet drugs), antihypertensive drugs (e.g. calcium channel blockers, angiotensin‐converting enzyme (ACE) inhibitors, beta‐blockers (β‐blockers), or any other antihypertensive drugs) and lipid‐lowering therapy (e.g. statins).
How the intervention might work
As people with AAA have increased cardiovascular risks, pharmacological therapy may reduce cardiovascular mortality and nonfatal cardiovascular events.
Why it is important to do this review
Three Cochrane systematic reviews on the effectiveness of surgical treatment of AAA have been conducted. Badger 2014 and Paravastu 2014 both compared endovascular versus open surgical repair for AAA, while Filardo 2015 examined immediate repair versus routine ultrasound surveillance. Another published Cochrane review, Rughani 2012, examined the effectiveness of medical treatments in terms of the expansion rate of small abdominal aortic aneurysms. However, these reviews have focused on treatment of AAA and ruptured AAA rather than on treatment of vascular risk factors associated with cardiovascular mortality in participants with AAA.
Acquired risk factors such as hypertension and hypercholesterolaemia are often reversible through pharmacological therapy. Given the increased risk of mortality with AAA, it is important to determine which prophylaxis is most effective in preventing cardiovascular death in people with AAA. To date, no systematic review has been conducted to study the effectiveness of medical treatments in reducing cardiovascular mortality in people with AAA. This review sought to provide evidence on the most effective medical treatment for this important problem.
This is an update of a Cochrane review first published in 2014.
Objectives
To determine the long‐term effectiveness of antiplatelet, antihypertensive or lipid‐lowering medication in reducing mortality and cardiovascular events in people with abdominal aortic aneurysm (AAA).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials in which participants with abdominal aortic aneurysm (AAA) were randomly allocated to one prophylactic treatment versus another, a different regimen of the same treatment, a placebo, or no treatment. We planned to include published studies and studies in progress, if preliminary results were available. Non‐English studies were eligible and we sought translations, where appropriate, for inclusion in the review.
Types of participants
Men and women of any age with AAA of less than 30 mm in diameter as measured by standardised techniques such as ultrasound examination or CT. We also included participants who had undergone endovascular or open surgical repair for AAA. In participants who had an AAA repair, the time period included in this review was the postoperative rather than the surveillance phase. We only included mixed population studies where data on the subset of participants with AAA were available.
Types of interventions
-
Antiplatelet therapy (e.g. aspirin, clopidogrel, ticlopidine, cilostazol, or any other antiplatelet drugs).
-
Antihypertensive drugs (e.g. calcium channel blockers, angiotensin‐converting enzyme (ACE) inhibitors, beta‐blockers (β‐blockers), or any other antihypertensive drugs).
-
Lipid‐lowering therapy (e.g. statins).
-
Combination treatment (e.g. antiplatelet drug plus antihypertensive or statin) versus single treatment.
-
Combination treatment versus no treatment.
Where possible, we planned to compare one intervention with another treatment, a different regimen of the same treatment, placebo, or no treatment. We included any type, method, duration, timing, mode of delivery, and dose of medical treatment. We excluded studies in which participants were not treated with a specific regimen but were given numerous medications as it would not be possible to attribute outcomes or side effects to one particular regimen.
This review concerns medical interventions in which the principal actions are to modify cardiovascular risk factors. Therefore, we did not include any alternative treatments for which the primary purpose was to treat the aneurysm itself, for example to reduce growth rates or prevent rupture, or both.
Types of outcome measures
Primary outcomes
-
All‐cause mortality.
-
Cardiovascular mortality (fatal myocardial infarction (MI), fatal stroke, other vascular deaths).
Secondary outcomes
-
AAA‐related death.
-
Nonfatal cardiovascular events (nonfatal MI, nonfatal stroke, or transient ischaemic attack).
-
Major amputation.
-
Quality of life.
-
Drug‐related morbidity.
-
Drug‐related mortality.
We excluded outcomes that were specific to the aneurysm itself (for example, change in size or rupture rates).
Search methods for identification of studies
We sought translations of any trials that were not in the English language.
Electronic searches
For this update the Cochrane Vascular Information Specialist (CIS) searched the following databases for relevant trials.
-
The Cochrane Vascular Specialised Register (14 April 2016).
-
The Cochrane Central Register of Controlled Trials (CENTRAL (2016, Issue 3)) via the Cochrane Register of Studies Online.
See Appendix 1 for details of the search strategy the CIS used to search CENTRAL.
The Cochrane Vascular Specialised Register is maintained by the CIS and is constructed from weekly electronic searches of MEDLINE Ovid, Embase Ovid, CINAHL, AMED, and through handsearching relevant journals. The full list of the databases, journals and conference proceedings which have been searched, as well as the search strategies used, are described in the Specialised Register section of the Cochrane Vascular module in the Cochrane Library (www.cochranelibrary.com).
The CIS searched the following trial databases for details of ongoing and unpublished studies using the terms abdominal aneurysm (14 April 2016):
-
World Health Organization International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/).
-
ClinicalTrials.gov (http://clinicaltrials.gov/).
-
ISRCTN Register (www.isrctn.com/).
See Appendix 2 for details of the search strategies.
Searching other resources
We reviewed the reference lists of relevant studies.
Data collection and analysis
Selection of studies
One review author (LR) used the selection criteria to identify trials for inclusion and assessed the titles and abstracts of all identified studies for relevance and design. The second review author (EA) independently confirmed this selection, and we resolved any disagreements through discussion. We obtained the full‐text articles of any potentially relevant studies. Two review authors independently assessed the full‐text articles. We resolved any disagreements by discussion. We listed all studies excluded after full‐text assessment in a 'Characteristics of excluded studies' table. We planned to include any studies that were published in duplicate only once in the review. We constructed a PRISMA diagram to illustrate the study selection process.
Data extraction and management
Two review authors (LR, EA) independently extracted the data. We recorded information about the trial design; AAA definition and measurement methods; baseline characteristics of participants; treatment type, method, duration, timing, mode of delivery, and dose. We reported all‐cause mortality and cardiovascular mortality data as the primary outcome measures. Also, we collected information on non‐cardiovascular events and adverse events in accordance with the secondary outcome measures. We planned to contact the study authors for further information if we required clarification. We resolved any disagreements in data extraction and management by discussion.
Assessment of risk of bias in included studies
Two review authors (LR, EA) independently used the Cochrane 'Risk of bias' assessment tool, Higgins 2011, to assess the risk of bias in the included study). This tool provides a protocol for judgements on sequence generation, allocation methods, blinding, incomplete outcome data, selective outcome reporting, and any other relevant biases. We resolved any disagreements by discussion.
Measures of treatment effect
We planned to base the analysis on intention‐to‐treat data from the individual clinical trials. As the primary and secondary outcomes are all binary measures, we computed odds ratios (ORs) using a fixed‐effect model. We calculated the 95% confidence intervals (CIs) of the effect sizes.
Unit of analysis issues
The unit of analysis was the individual participant. However, as the trial involved repeat measurements on participants at different points in time, it was prone to unit of analysis errors (Deeks 2011). Therefore, for the purpose of this review, we chose cardiovascular mortality at five years as the primary endpoint. We planned to include outcomes at longer follow‐up periods as secondary outcomes if reported.
Dealing with missing data
We sought information about dropouts, withdrawals, and other missing data. If not reported, we attempted to contact the study authors.
Assessment of heterogeneity
The inclusion of studies on a wide range of medical treatments was likely to result in a high degree of heterogeneity. We therefore planned to assess the heterogeneity between pooled studies by using the Chi2 test regarding the characteristics and quality of included studies (Deeks 2011).
We planned to perform the Chi2 test to assess heterogeneity in identified subgroups, and we planned to use the I2 statistic to measure the degree of inconsistency between studies. An I2 statistic result of greater than 50% may represent moderate to substantial heterogeneity (Deeks 2011). Only one study met the inclusion criteria for the review and therefore it was not necessary to measure the heterogeneity between studies.
Assessment of reporting biases
We planned to assess reporting biases such as publication bias using funnel plots (Sterne 2011). As only one study met the inclusion criteria of this review, which was at a low risk of reporting bias, we did not perform this.
Data synthesis
Two review authors (LR, EA) independently extracted the data. One review author (LR) entered the data into Review Manager 5 (RevMan 5) (RevMan 2014). The second review author (EA) cross‐checked data entry, and we resolved any discrepancies by consulting the source publication.
We used a fixed‐effect model to meta‐analyse the data.
Subgroup analysis and investigation of heterogeneity
Where possible, we planned to analyse clinically relevant subgroups based on drug and participant groupings including the following.
-
Diameter of aneurysm.
-
Type of repair (e.g. endovascular versus surgical).
-
Type of repair (e.g. endovascular or surgical) versus no repair.
-
Diabetes.
-
Year of publication.
However, as only one study with 227 participants met the inclusion criteria, it was not possible to perform subgroup analyses.
Sensitivity analysis
We planned to conduct a sensitivity analysis by excluding studies at a high risk of bias to measure the effect on the results. However, as there was only one included study we were unable to conduct a sensitivity analysis.
'Summary of findings' table
We presented the main findings of the review results concerning the quality of evidence, the magnitude of effect of the interventions examined, and the sum of available data for all‐cause mortality, cardiovascular mortality, AAA‐related death, and nonfatal cardiovascular events in a 'Summary of findings' table, according to the GRADE principles as described by Higgins 2011 and Atkins 2004. We used the GRADEprofiler Guideline Development Tool (GRADEpro GDT) software to assist in the preparation of the 'Summary of findings' table (GRADEpro GDT 2014).
Results
Description of studies
Results of the search
See Figure 1.
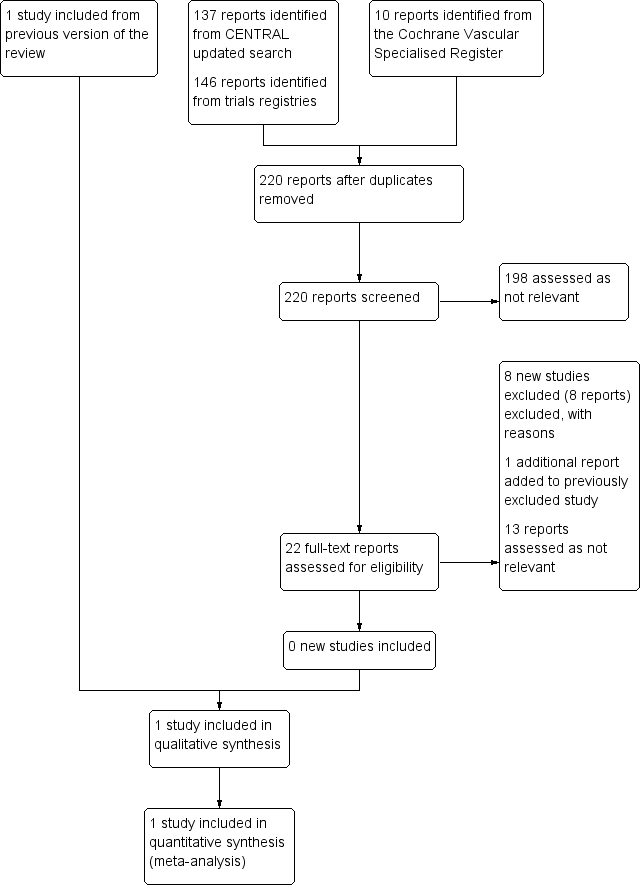
Study flow diagram.
Included studies
See the 'Characteristics of included studies' table.
No new studies met the inclusion criteria for this update.
The review includes one study (Yang 2006). Yang 2006 is a double‐blind, randomised, placebo‐controlled trial that measured the effects of metoprolol on the incidence of cardiac complications at 30 days and six months after vascular surgery. The study included 496 participants who underwent procedures including abdominal aortic repair and infrainguinal or axillofemoral revascularisation. A subgroup of 227 participant had an abdominal aortic repair. Although the trial authors did not present outcome data for the abdominal aortic aneurysm (AAA) subgroup in the full report, we obtained these data through personal communication with the study author and statistician. Of the 227 AAA participants, 111 were randomised to metoprolol and 116 were randomised to a placebo. The doses of metoprolol were as follows: 100 mg in participants weighing ≥ 75 kg, 50 mg for participants weighing between 40 mg and 75 kg, and 25 mg for those weighing ≤ 40 kg. Beta‐blocker therapy was commenced preoperatively on the day of surgery and continued for the duration of the hospital stay. Within two hours postsurgery, the study drug was administered orally or intravenously for 15 minutes (metoprolol 1 mg/mL or saline at 0.2 mL/kg, diluted with 20 mL of saline). Study medication was continued intravenously every six hours or orally twice a day for five days or until hospital discharge, whichever occurred sooner. Intravenous study drug was converted to oral as soon as the participant tolerated oral intake. The trial performed 30‐day and six‐month follow‐ups by telephone for discharged participants. Yang 2006 defined the primary outcome as a composite of cardiac complications at 30 days postoperation including: cardiac death, nonfatal myocardial infarction (MI), congestive heart failure (CHF), unstable angina, and dysrhythmia requiring treatment, defined as atrial fibrillation or ventricular dysrhythmias. In the presence of more than one outcome, the first outcome was recorded. Secondary study outcomes included study drug discontinuation (due to bronchospasm, hypotension, or bradycardia), amputation, and intraoperative hypotension or bradycardia.
Excluded studies
See the 'Characteristics of excluded studies' table.
For this update we excluded seven completed studies (Ashes 2013; Berwanger 2015; Kouvelos 2011; Qu 2014; Schouten 2011; Xia 2014; Xia 2015), and one ongoing study (NCT01225094).
In total, we excluded 17 studies from the review (Ashes 2013; Berwanger 2015; Cesanek 2008; DECREASE Study; Durazzo 2004; Kouvelos 2011; Kouvelos 2013; Mackey 2006; Mangano 1996; NCT01225094; Neilipovitz 2012; POBBLE Trial; POISE Study; Qu 2014; Schouten 2011; Xia 2014; Xia 2015). Two studies, Durazzo 2004 and POBBLE Trial, had AAA subgroups but did not present specific outcome data for these participant. The author of one study, Durazzo 2004, confirmed through personal communication that these data were not available. We were unable to contact the authors of the POBBLE Trial. Ten studies did not report AAA subgroups (Ashes 2013; Berwanger 2015; Cesanek 2008; Kouvelos 2011; Mangano 1996; POISE Study; Qu 2014; Schouten 2011; Xia 2014; Xia 2015). Authors of the POISE Study confirmed that outcome data for AAA participants were not available, but the other nine study authors did not respond (Ashes 2013; Berwanger 2015; Cesanek 2008; Kouvelos 2011; Mangano 1996; Qu 2014; Schouten 2011; Xia 2014; Xia 2015). One study, Mackey 2006, was not a randomised controlled trial but a prospective study that measured the incidence of myocardial injury in vascular surgery patients. In two studies participants were taking co‐medications and therefore we could not attribute the results to one particular drug (Kouvelos 2013; Neilipovitz 2012). We excluded the DECREASE Study as the integrity of the data was questionable. In a report released by Erasmus MC Follow‐Up Committee in 2012, the principal investigator admitted that written informed consent was not obtained for every participant and that the data were collected in a negligent manner (Erasmus MC Follow‐Up Committee 2012). Finally, one ongoing study tested the effects of curcumin, a natural health product (NCT01225094).
Risk of bias in included studies
See the 'Risk of bias' table in the 'Characteristics of included studies' section, and Figure 2.
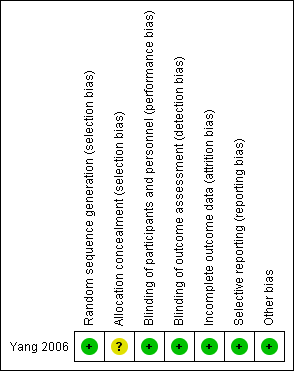
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.
Allocation
A study statistician performed random sequence generation in blocks of four and therefore we judged the study to be at a low risk of selection bias. However, the study authors did not report the methods used to conceal allocation of treatment and therefore the risk of selection bias was unclear.
Blinding
All study participants, investigators, caretakers and data outcome evaluators of Yang 2006 were blinded to treatment. Furthermore, blinding was maintained throughout the study, even if study medication was discontinued.
Incomplete outcome data
The two treatment groups in Yang 2006 were well‐balanced with respect to baseline characteristics, completion of the study protocol, and discontinuation of treatment. Furthermore, the study authors accounted for and reported on all missing data.
Selective reporting
The authors of Yang 2006 specified their hypothesis using results from previously published work. They clearly stated their primary and secondary outcomes and reported data on all outcomes.
Other potential sources of bias
We considered the Yang 2006 study to be at low risk of other potential sources of bias.
Effects of interventions
As only one study, Yang 2006, met the inclusion criteria, we were unable to pool data or perform a meta‐analysis. Therefore, we reported the individual estimates from the study in a narrative synthesis. The included study did not measure mortality at five years but at two shorter time points of 30 days and six months postoperation. Results indicated no clear evidence that metoprolol reduced all‐cause or cardiovascular mortality at 30 days: the incidence of all‐cause mortality was 1/111 in the metoprolol group and 6/116 in the placebo group (odds ratio (OR) 0.17, 95% confidence interval (CI) 0.02 to 1.41) while the incidence of cardiovascular mortality at 30 days was 1/111 and 5/116 in the metoprolol and placebo groups respectively (OR 0.20, 95% CI 0.02 to 1.76). One participant in each treatment group died of causes related to AAA (OR 1.05, 95% CI 0.06 to 16.92). Nonfatal cardiovascular events occurred in 12/111 in the metoprolol group and 9/116 in the placebo group at 30 days (OR 1.44, 95% CI 0.58 to 3.57). At six months, metoprolol did not significantly reduce the rate of all‐cause mortality (OR 0.71, 95% CI 0.26 to 1.95) or cardiovascular deaths (OR 0.73, 95% CI 0.23 to 2.39). The incidence of AAA‐related death was not measured at six months. The incidence of nonfatal cardiovascular events was similar between the two treatment groups at six months (OR 1.41, 95% CI 0.59 to 3.35). For these outcomes, we downgraded the quality of the evidence to low. The quality of evidence was downgraded due to imprecision, as only one study with a small number of participants met the inclusion criteria, the number of events was low, and the result was consistent with benefit and harm. No participant had to undergo an amputation. Quality of life was not reported.
Yang 2006 reported on adverse events in the form of study drug discontinuation (due to bronchospasm, hypotension, or bradycardia) and intraoperative hypotension or bradycardia. However, data on study drug discontinuation and the incidence of intraoperative hypotension or bradycardia were not available for the subgroup of AAA participants. In the overall study of 496 participants, the study authors reported that the incidence of intraoperative complications was significantly higher in the metoprolol group (P < 0.01). Hypotension occurred in 54% of metoprolol participants (46% required treatment) compared to 41% of placebo participants (34% required treatment). Bradycardia occurred in 35% and 10% of metoprolol and placebo participants, respectively, of whom 22% and 7% required treatment. However, given that these outcomes are based on a population of participants who had undergone vascular surgery for other conditions, we cannot generalise the results to participants with AAA.
Discussion
Summary of main results
Only one study fulfilled the inclusion criteria of this review. The study was a randomised controlled trial in which 496 participants undergoing non‐cardiac vascular surgery received either metoprolol or placebo (Yang 2006). We received data on a subgroup of 227 participants who underwent AAA repair from the study author. Results of the study indicate that metoprolol is not associated with a reduction in the rate of all‐cause or cardiovascular mortality at either 30 days or six months. No participant had to undergo an amputation. Quality of life was not reported. Adverse drug effects were reported for the whole study population and were not available for the subgroup of participants with AAA. We downgraded the quality of the evidence due to imprecision, as only one study with a small number of participants met the inclusion criteria, the number of events was low, and the result was consistent with benefit and harm.
Overall completeness and applicability of evidence
Currently, there is a severe lack of evidence concerning the effectiveness of pharmacological prophylaxis in the prevention of cardiovascular events in AAA patients. The one included study was relatively small and tested one beta‐blocker against a placebo at 30 days and six months follow‐up. Therefore, the results of this study are not widely applicable to the AAA population and the follow‐up period was relatively short to study mortality and cardiovascular events in such participants. Recent evidence has questioned whether beta‐blockers are of any perioperative value and suggests they may be harmful (Bolsin 2013). As there are many different drugs available, it is important to test these drugs, not just against a placebo but also against each other. Furthermore, it is important to establish if a combination of drugs would yield a better outcome than one drug alone.
Quality of the evidence
The quality of reporting in the single included study was good. With the exception of failing to report the methods used to conceal allocation of treatments, the study authors provided adequate information on the process of randomisation and blinding. As such, we deemed the study to be at a low risk of selection, performance, and detection bias. Additionally, the study authors accounted for all missing data and reported data on all primary and secondary outcomes, and therefore minimised the chances of attrition and performance bias. For all outcomes, we downgraded the quality of the evidence to low. We downgraded the quality of evidence for imprecision, as there was only one included study with a small number of participants, the number of events was small, and the confidence intervals (CI) indicated both benefit and harm.
Potential biases in the review process
We, the authors of this Cochane review, were neither involved in the included study nor in any of the excluded studies. Furthermore, we do not have any commercial or other conflict of interest. The search was as comprehensive as possible and two review authors independently assessed all studies for inclusion. We are confident that we have included all relevant studies and attempted to reduce bias in the review process. However, the possibility remains that we may have missed studies that have not been published.
Agreements and disagreements with other studies or reviews
This is an update of a Cochrane review first published in 2014 and the first systematic review to measure the effectiveness of pharmacological prophylaxis in reducing cardiovascular morbidity and mortality in AAA patients. One prospective study of AAA participants who were followed up over a median of 4.7 years determined that, in those who survived AAA repair, beta‐blocker use was associated with a significantly lower incidence of all‐cause mortality (hazard ratio (HR) 0.6, 95% CI 0.5 to 0.9) and cardiovascular mortality (HR 0.7, 95% CI 0.4 to 0.9) (Kertai 2004). After adjusting for clinical risk factors and beta‐blocker use, the same study showed that long‐term use of statins showed a reduction in both all‐cause and cardiovascular mortality (HR 0.4, 95% CI 0.3 to 0.6; and HR 0.3, 95% CI 0.2 to 0.6 respectively). Therefore, it would appear that statins reduce cardiovascular risk regardless of beta‐blocker use. However, this was a prospective cohort study with no randomisation and therefore likely to be at high risk of bias.
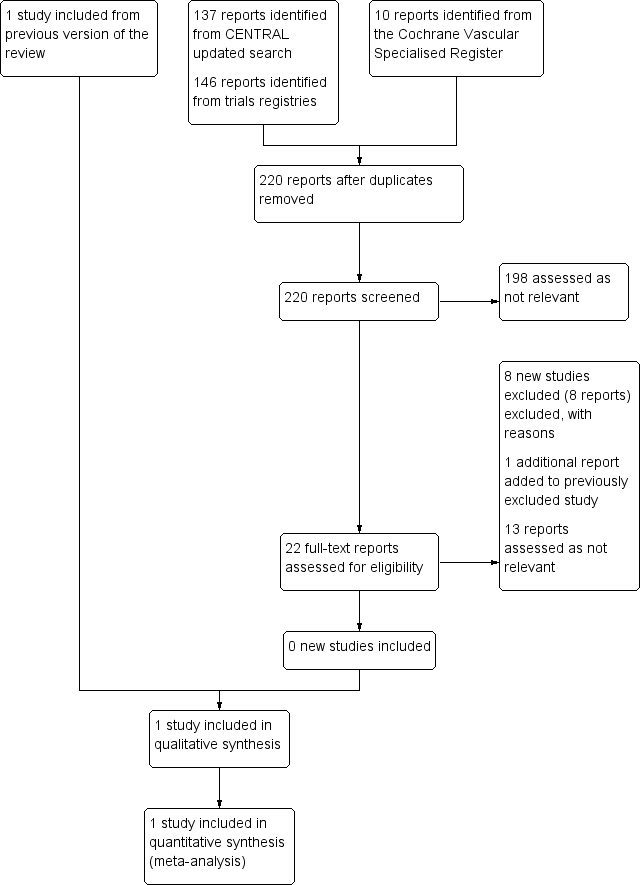
Study flow diagram.

'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.

Comparison 1 Metoprolol versus placebo, Outcome 1 All‐cause mortality, 30 days.

Comparison 1 Metoprolol versus placebo, Outcome 2 Cardiovascular death, 30 days.

Comparison 1 Metoprolol versus placebo, Outcome 3 AAA‐related death, 30 days.

Comparison 1 Metoprolol versus placebo, Outcome 4 Nonfatal cardiovascular event, 30 days.

Comparison 1 Metoprolol versus placebo, Outcome 5 All‐cause mortality, 6 months.
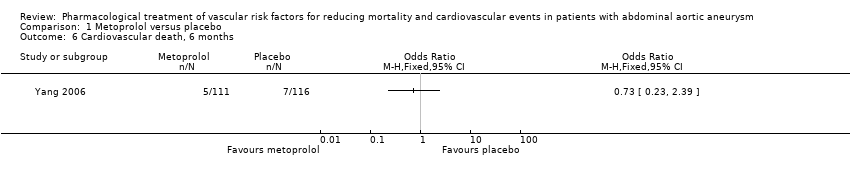
Comparison 1 Metoprolol versus placebo, Outcome 6 Cardiovascular death, 6 months.

Comparison 1 Metoprolol versus placebo, Outcome 7 Nonfatal cardiovascular event, 6 months.
| Metoprolol compared to placebo for reducing mortality and cardiovascular events in patients with abdominal aortic aneurysm (AAA) | ||||||
| Patient or population: patients of any age with AAA less than 30 mm in diameter | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with metoprolol | |||||
| All‐cause mortality, 30 days1 | Study population | OR 0.17 | 227 | ⊕⊕⊝⊝ | — | |
| 52 per 1000 | 9 per 1000 | |||||
| Cardiovascular death, 30 days3 | Study population | OR 0.20 | 227 | ⊕⊕⊝⊝ | — | |
| 43 per 1000 | 9 per 1000 | |||||
| AAA‐related death, 30 days4 | Study population | OR 1.05 | 227 | ⊕⊕⊝⊝ | — | |
| 9 per 1000 | 9 per 1000 | |||||
| Nonfatal cardiovascular event, 30 days5 | Study population | OR 1.44 | 227 | ⊕⊕⊝⊝ | — | |
| 78 per 1000 | 108 per 1000 | |||||
| All‐cause mortality, 6 months1 | Study population | OR 0.71 | 227 | ⊕⊕⊝⊝ | — | |
| 86 per 1000 | 63 per 1000 | |||||
| Cardiovascular death, 6 months3 | Study population | OR 0.73 | 227 | ⊕⊕⊝⊝ | — | |
| 60 per 1000 | 45 per 1000 | |||||
| AAA‐related death, 6 months4 | See comments | See comments | See comments | See comments | The incidence of AAA‐related death was not measured at six months. | |
| Nonfatal cardiovascular event, 6 months5 | Study population | OR 1.41 | 227 | ⊕⊕⊝⊝ | — | |
| 86 per 1000 | 117 per 1000 | |||||
| *The risk with placebo was the average risk in the placebo group (i.e. the number of participants with events divided by total number of participants of the placebo group included in the meta‐analysis). The risk in the metoprolol group (and its 95% CI) is based on the assumed risk in the placebo group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Death from all causes. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 All‐cause mortality, 30 days Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Cardiovascular death, 30 days Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 AAA‐related death, 30 days Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Nonfatal cardiovascular event, 30 days Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 All‐cause mortality, 6 months Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Cardiovascular death, 6 months Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Nonfatal cardiovascular event, 6 months Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

